Abstract
Objective
To gain a better understanding of the complex patterns of causes that contribute to death due to multiple sclerosis (MS) by assessing the relationship between MS and other causes of death listed on death certificates.
Methods
Multiple cause of death data for all adult deaths (aged ≥18 years) in British Columbia, Canada, between 1986 and 2013 were accessed. All causes, as listed on the death certificate, whether underlying or contributing, were considered “any mention” causes. The associations between mention of MS on the death certificate and mention of other causes of death were examined by logistic regression, adjusted for age, sex, and calendar year (Bonferroni-corrected α level = 0.002). Findings were also sex-stratified.
Results
Among 771,288 deaths, MS was mentioned on 2,153 certificates. If MS was mentioned (versus not mentioned), there was a greater chance that specific conditions contributed to the death: respiratory infection (adjusted odds ratio [aOR], 3.03 [95% confidence interval (CI), 2.73–3.36]), aspiration pneumonia (aOR, 7.15 [95% CI, 6.23–8.22]), urinary tract infection (UTI) (aOR, 10.2 [95% CI, 8.7–12.0]), other infection including sepsis (aOR, 1.34 [95% CI, 1.15–1.56]), and skin disease (aOR, 5.06 [95% CI, 3.96–6.46]). Sex differences existed for urinary tract infection (men: aOR, 14.9 [95% CI, 11.5–19.3]; women: aOR, 8.00 [95% CI, 6.53–9.81]) and chronic respiratory disease (men = aOR, 1.36 [95% CI, 1.14–1.63]; women = aOR, 0.97 [95% CI, 0.84–1.13]).
Conclusions
Deaths attributed to MS were commonly caused by infection (especially respiratory and urinary tract–related); conditions associated with advanced disability and immobility, such as aspiration pneumonia; and chronic respiratory disease in men. All are potentially modifiable; interventions that reduce the frequency or severity of these complications could improve survival in MS.
Although the management of multiple sclerosis (MS) has substantially changed with the advent of new disease-modifying therapies, a diagnosis of MS is still associated with a reduced life expectancy.1,2 Furthermore, comorbidities, particularly ischemic heart disease, diabetes mellitus, and chronic lung conditions, are associated with worse disability outcomes and shorter survival in MS.3 MS is rarely fatal as a cause of death by itself4; therefore, other causes, including those that directly result from complications of MS, are expected to explain the increased mortality risk. A better understanding of these causes would inform both clinical management and research into interventions that might affect survival.
According to international standards,5 a death certificate should specify the underlying cause of death (e.g., ischemic heart disease) and the conditions arising from it that led directly to death (e.g., ischemic heart disease leading to myocardial infarction and cardiac arrest). The death certificate often also includes the mode of death listed as the immediate cause; using the previous example, this would be cardiac arrest that resulted from myocardial infarction and ischemic heart disease. Finally, the certificate includes other significant conditions that contributed to the death, even though they are not considered to be in the direct chain of events leading to the death.5 Multiple cause of death (MCOD) data6 include all listed causes, and have been used to examine the contribution of different causes to deaths in some chronic disease.7–16 They have been underused, despite their potential value. Because comorbidities and complications of MS are common, MCOD analysis can provide much-needed insight into the broader reasons for death due to MS.8,11
We identified causes that contributed to deaths attributed to MS using MCOD data from all adult deaths in British Columbia, Canada, over a 28-year period.
Methods
MCOD data for all adult deaths (≥18 years of age) registered in British Columbia, Canada, from 1986 to 2013 inclusive were provided by the province's Vital Statistics Agency.17 In addition to the underlying and all contributing causes, sex and dates of birth and death were accessed.
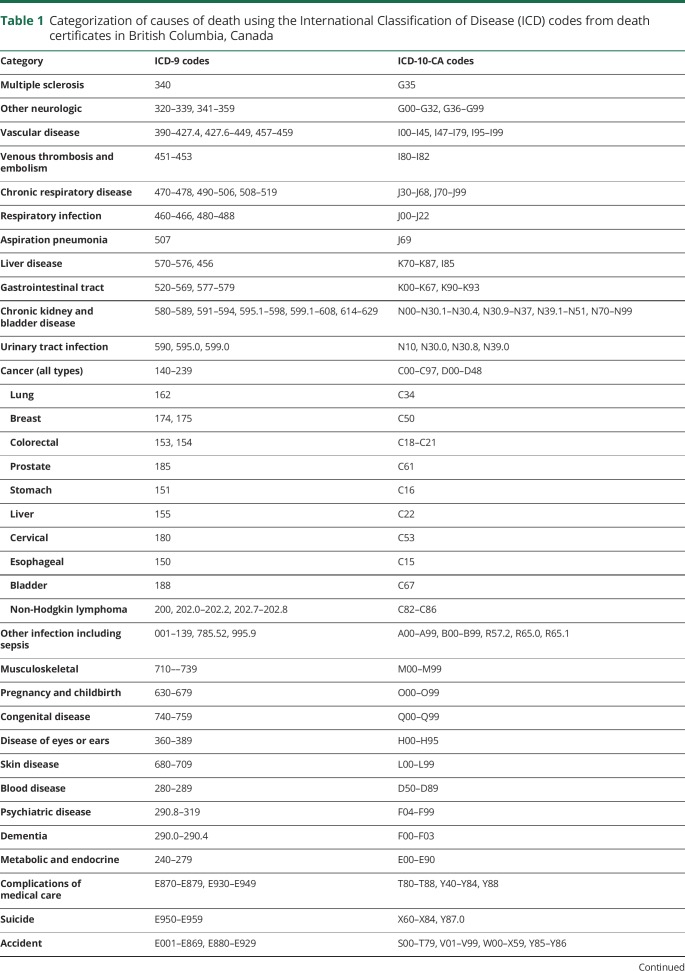
The underlying and contributing causes of death, as determined by the physician and listed on the death certificates, were provided in the form of ICD codes (version 9 or 10 depending on the year of death).18,19 We grouped all possible diseases and conditions into specific causes as follows: MS; other neurologic disease; vascular disease (which included cardiovascular disease, cerebrovascular disease, and peripheral vascular disease); venous thrombosis and embolism; chronic respiratory disease; respiratory infection; aspiration pneumonia; liver disease; gastrointestinal disease; noninfectious kidney and bladder disease; urinary tract infection; cancer; other infection including sepsis; musculoskeletal disease; pregnancy and childbirth; congenital disease (surviving into adulthood); disease of eyes or ears; skin disease; blood disorder; psychiatric disease; dementia; metabolic and endocrine disturbance; complications of medical and surgical care; suicide; accident; homicide; and other cause. In addition, cancer as a cause of death was further categorized into the 10 most prevalent types of cancer as defined by the World Cancer Research Fund: lung, breast, colorectal, prostate, stomach, liver, cervical, esophageal, bladder, and non-Hodgkin lymphoma.20 The mode of death (i.e., cardiac arrest, respiratory arrest, coma) was not included as a cause of death for our analysis. The ICD codes used to categorize cause of death are detailed in table 1.
Table 1.
Categorization of causes of death using the International Classification of Disease (ICD) codes from death certificates in British Columbia, Canada
We calculated the proportion of deaths that were attributed to MS as the underlying cause and the proportion for which MS was mentioned as the underlying or a contributing cause (“any mention”). The ratio of any mention of MS to mention of MS as the underlying cause of death was calculated by age at death (<40; 40–49; 50–59; 60–69; 70–79; ≥80 years). We also calculated the proportion of all deaths and the proportion of MS deaths (i.e., any mention of MS) attributed to each of the other causes. Only the causes that were mentioned together with MS on at least 6 death certificates were analyzed in order to avoid extrapolating from a small number of events and to comply with data privacy requirements of the British Columbia Ministry of Health and British Columbia Vital Statistics Agency. Logistic regression models were used to assess the association of any mention of MS with any mention of each of the other causes of death in comparison to any mention of the same cause without MS. Odds ratios (ORs) were adjusted for age at death (as a continuous variable), sex, and exact calendar year of death. Sex-stratified analyses, similarly adjusted for age and calendar year, were also performed. A Bonferroni correction was applied for multiple comparisons, resulting in a threshold for statistical significance of p < 0.002 for 23 comparisons.
Statistical analyses were conducted using R version 3.4.2 (R Foundation for Statistical Computing, Vienna, Austria) and SAS version 7.1 (SAS Institute, Inc., Cary).
Standard protocol approvals, registrations, and patient consents
This study was approved by the University of British Columbia's Clinical Research Ethics Board. Access to administrative data from British Columbia was approved by the BC Ministry of Health and the BC Vital Statistics Agency Data Stewardship Committees, and facilitated by Population Data BC (popdata.bc.ca/).
Data sharing
The Vital Statistics data that were used for this study were accessed through Population Data BC (popdata.bc.ca/) and reside on a limited access secure research environment. For legal and ethical reasons, the data cannot leave this secure research environment.
Results
A total of 771,288 adult death certificates were accessed; of these, 366,254 (47.5%) were for women. The mean age at death for the population of decedents was 74.5 years: 77.8 years for women and 71.5 years for men.
MS as a cause of death
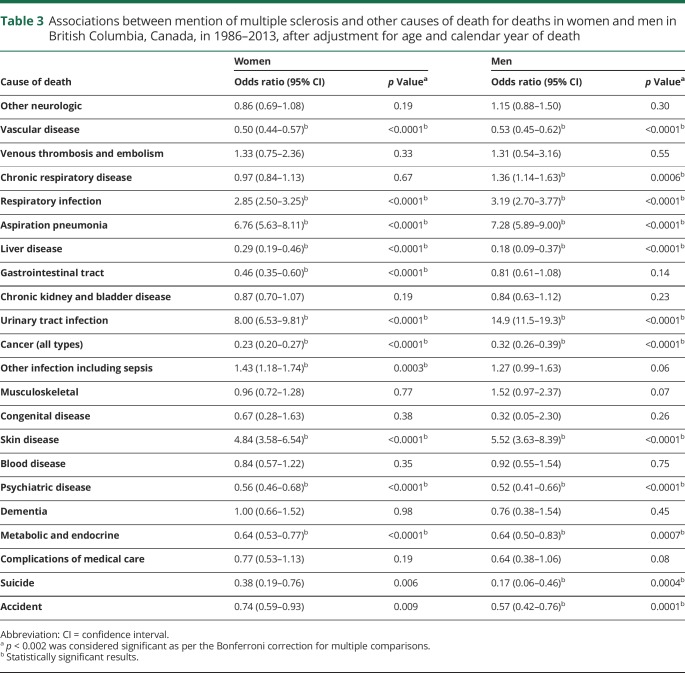
MS was mentioned as either the underlying or a contributing cause of death on 2,153 certificates; of these, 1,868 (86.8%) included at least 1 additional cause. Approximately twice as many death certificates for women (1,359/366,254 [0.37%]) included a mention of MS compared to death certificates for men (794/405,034 [0.20%]). However the proportion of all deaths with a mention of MS during any one calendar year between 1986 and 2013 varied between 0.19% and 0.39%. For deaths attributed to MS (any mention), the mean age at death was 64.8 years. MS was recorded as the underlying cause of death on 1,267 certificates; the mean age at these deaths was 62.6 years. The ratio of any mention of MS to MS as the underlying cause of death increased with age, from 1.3 for deaths occurring under 50 years of age to 2.1 for deaths at age 80 or older (figure 1).
Figure 1. The number of deaths with multiple sclerosis (MS) as the underlying cause compared to the number with any mention of MS, by age at death in British Columbia, Canada (1986–2013).
The numbers above each column represent the ratio of MS as the underlying cause to any mention of MS.
All causes of death
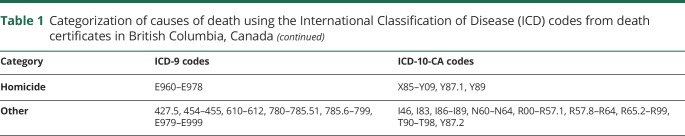
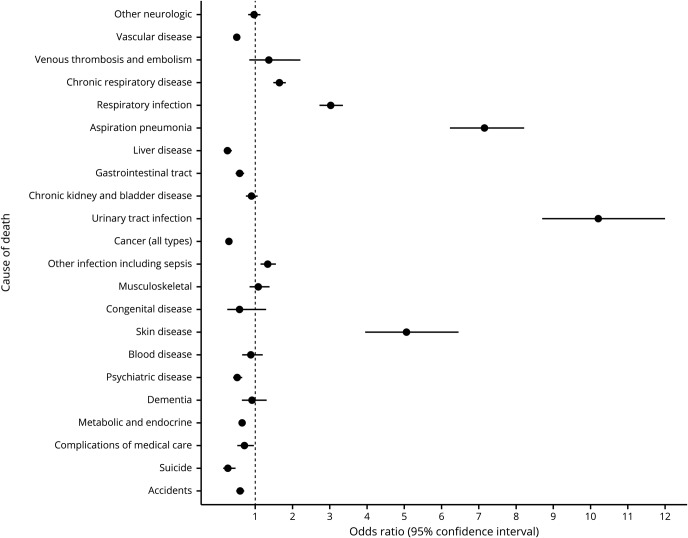
The most frequently mentioned cause of death overall was vascular disease (n = 388,750), followed by cancer (n = 246,765) and chronic respiratory disease (n = 140,695). These 3 categories were also the most commonly reported in conjunction with MS (vascular disease with MS: n = 556; cancer with MS: n = 303; chronic respiratory disease with MS: n = 500). Aside from MS, the least common causes of death among all decedents of British Columbia were pregnancy (n = 98), disease of eyes and ears (n = 2,074), and homicide (n = 2,351) (table 2); all 3 of these causes were excluded from further analysis because they were mentioned together with MS in fewer than 6 deaths.
Table 2.
Deaths by mentioned cause in British Columbia, Canada, for all decedents, by sex, and for deaths attributed to multiple sclerosis (MS) (1986–2013)
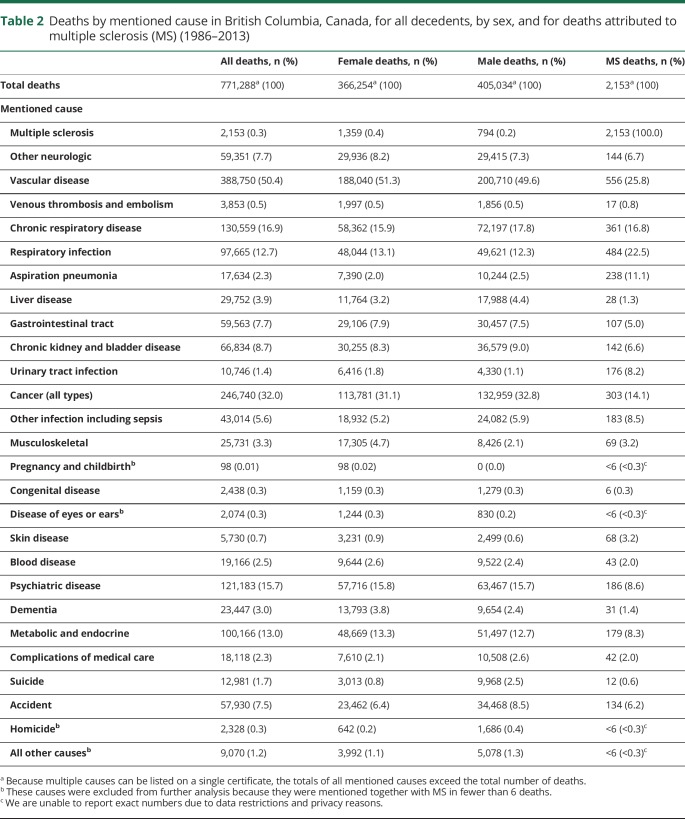
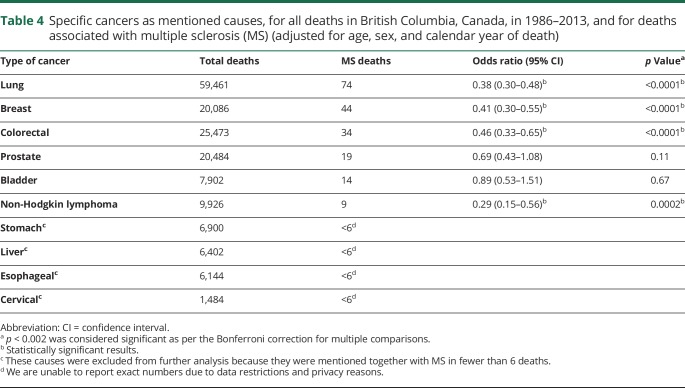
Compared to deaths with no mention of MS, those that were due to MS were more likely (p < 0.002) to be caused by urinary tract infection (adjusted OR [aOR], 10.2 [95% confidence interval (CI), 8.7–12.0]), aspiration pneumonia (aOR, 7.15 [95% CI, 6.23–8.22]), skin disease (aOR, 5.06 [95% CI, 3.96–6.46]), respiratory infection (aOR, 3.03 [95% CI, 2.73–3.36]), chronic respiratory disease (aOR, 1.65 [95% CI, 1.49–1.83]), and other infection including sepsis (aOR, 1.34 [95% CI, 1.15–1.56]). Of the 68 death certificates that mentioned both MS and skin disease, the majority (90%) referred specifically to pressure sores and chronic ulcers. Several causes were less likely to be mentioned together with MS, including vascular disease, liver disease, gastrointestinal disease, cancer (all types combined), metabolic or endocrine disturbance, psychiatric disease, accident, and suicide (figure 2). All remaining causes were just as likely to be mentioned with MS as without MS. Generally, the direction and size of the estimates were similar when men and women were assessed separately (table 3). However, the association between death due to MS and death due to urinary tract infection was greater for men than for women (men: aOR, 14.9 [95% CI, 11.5–19.3]; women: aOR, 8.00 [95% CI, 6.53–9.81]). In men only, deaths due to MS were more likely to be also due to chronic respiratory disease (men: aOR, 1.36 [95% CI, 1.14–1.63]; women: aOR, 0.97 [95% CI, 0.84–1.13]).
Figure 2. Odds ratios (ORs) and 95% confidence intervals for mention of each cause together with multiple sclerosis (MS), relative to mention of each cause without MS, British Columbia, Canada (1986–2013), after adjustment for age, sex, and calendar year of death.
The dotted line represents an OR of 1.0. An OR to the right of the dotted line represents an increased association of the cause of death with mention of MS on the death certificate. An OR to the left of the dotted line represents a reduced association of the cause of death with mention of MS.
Table 3.
Associations between mention of multiple sclerosis and other causes of death for deaths in women and men in British Columbia, Canada, in 1986–2013, after adjustment for age and calendar year of death
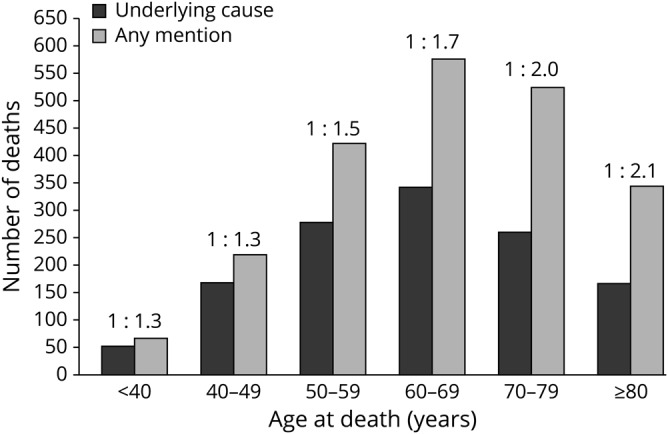
Deaths due to cancer
Of the 10 types of cancer examined, the most frequently reported was lung (n = 59,461), and the least frequent was cervical (n = 1,484). For each of cervical, stomach, liver, and esophageal cancer, there were fewer than 6 mentions of these cancers together with MS on the death certificate; these were excluded from further analysis. There were no positive associations between MS as a cause of death and any type of cancer. Rather, death due to MS was negatively associated with all cancers, although not all associations reached significance (table 4).
Table 4.
Specific cancers as mentioned causes, for all deaths in British Columbia, Canada, in 1986–2013, and for deaths associated with multiple sclerosis (MS) (adjusted for age, sex, and calendar year of death)
Discussion
In this study of 771,288 adult deaths recorded over almost 3 decades in British Columbia, Canada, we found that fewer than 1% of deaths were attributed to MS, either as the underlying or a contributing cause. The average age at deaths caused by MS was 10 years younger than that for all adult deaths in the province. However, MS was rarely cited as the only cause; more frequently, other causes contributed to the death, which highlights the value of MCOD data. The major contributing causes were aspiration pneumonia, respiratory infection, respiratory disease, urinary tract infection, other infection including sepsis, and skin disease (typically pressure ulcers). Conversely, there was no evidence of increased association between other causes and MS, including cancer.
The majority of findings were consistent for men and women. However, the association between death due to MS and urinary tract infection, while large in both, appeared stronger in men than women. Urinary tract infections are more common in women than men in the general population21; our results indicate that the increase in deaths due to urinary tract infection is relatively greater for MS deaths in men than in women, although urinary tract infections make an important contributions to MS deaths in both sexes. Chronic respiratory disease was associated with deaths attributed to MS for men but not for women. There have been inconsistent findings regarding the relationship between chronic respiratory disease and MS; however, it seems to emerge in people with MS at a younger age than it does in the general population,22 and might be associated with more rapid MS-related disability.23 There is evidence that the incidence of chronic respiratory disease is similar for women and men with MS, and that it is more prevalent in women22; its role in MS mortality warrants further consideration and research.
Almost twice as many deaths among women were attributed to MS than among men, which is in line with the observed sex differences in MS incidence.24,25 The role of MS in the death varied by age; MS was more likely to be cited as the underlying cause for deaths occurring at a younger age. With increasing age, other conditions were more likely to be cited as the underlying cause. While this concurs with the increased comorbidity risk with increasing age that is observed in the general population, the rate of this age-related increase in risk of comorbidity has been shown to be higher in MS26; our findings underscore the importance of comorbidities in MS as contributing factors to death.
Neurologic disorders, including MS, are associated with a substantial burden of disability and mortality on a global scale.27 MS itself confers an increased hazard of death relative to the general population.2,28–30 However, except for rare and aggressive variants,31 MS alone is rarely fatal. MCOD data can provide a more complete picture because they provide information on all conditions that the certifying physician considered clinically relevant to the death,7,11,32 therefore facilitating a broader understanding of the multiple complex events and conditions that contribute to the higher mortality risk in MS.
Overall, for the British Columbia population of decedents, 1,267 (59%) of the 2,153 death certificates that mentioned MS cited it as the underlying cause. This is comparable to the proportion reported by a study of death certificates in the United Kingdom, where MS was the underlying cause in 52%–70% of deaths attributed to MS, with these proportions varying over time.11 While few studies have accessed MCOD data, our findings concur with, but also extend beyond, a prior study from the United States that examined deaths due to MS over a shorter, 12-year period. Similar to our observations over 28 years, pressure ulcers, urinary tract infection, pneumonia, and septicemia were more likely to contribute to deaths due to MS when compared to deaths that were not attributed to MS.9 However, we also found that aspiration pneumonia was of particular importance, contributing to more than 10% of the deaths due to MS. This clinically well-recognized but often understudied condition occurs when food or drink enters the lungs, causing infection,33 and has not been specifically reported in the few MCOD studies conducted to date.9,11 While aspiration pneumonia risk can be elevated for people with advanced neurologic disease generally, our findings confirm its importance in contributing to death due to MS.
British Columbia, Canada, is one of the few jurisdictions worldwide with availability of large population-based administrative data and detailed MCOD information. The access to this population-based MCOD data from all adult death certificates registered in the province over almost 3 decades is a significant strength of our study. Such a large population of decedents provided stability for the reference groups even when stratified by age, sex, and calendar year of death, and also allowed us to assess relatively rare causes of death. Our study of deaths attributed to MS in the general population is the first of its kind from Canada.
Using MCOD data, we have identified additional important contributing conditions including urinary tract infection, skin ulcers, respiratory infections, and aspiration pneumonia. These conditions were not typically cited as underlying causes, but represented significant contributions to MS-related death: urinary tract infection, for example, contributed to 8% of deaths attributed to MS but fewer than 2% of all deaths. People with MS are at higher risk of urinary tract infection due to neurogenic bladder, urinary retention, and incomplete emptying, or frequent use of catheters.34 Pressure ulcers, which contributed to 3% of deaths attributed to MS, can develop as a consequence of immobility with prolonged periods of pressure on a single area of skin, and may also lead to sepsis and fatal infection.9,35 Respiratory infection is a common cause of death; it contributed to 12.7% of all deaths, but this contribution increased to 22.5% for deaths attributed to MS. Increased levels of frailty and a diagnosis of chronic disease (such as MS) are associated with poorer outcomes in respiratory infection.36 It is important to note that these conditions (which are often the consequences of severe disability) are not necessarily independent; one death due to MS can be attributed to more than one of these conditions. This again underlines the value of MCOD data to identify all causes contributing to death.
There were a number of deaths for which MS was less likely to be mentioned as a contributing cause, specifically those attributed to vascular disease, liver and gastrointestinal disease, common types of cancer, metabolic disturbance, psychiatric disease, accident, and suicide. The most likely explanation is that many of these conditions, but particularly cancer and suicide, are typically considered sufficient and independent causes of death, and are more likely to be reported alone on a death certificate regardless of the presence of other conditions or comorbidities at the time of death.7,32,37 Rather than implying that people with MS are less likely to die of these causes, it is more likely that the certifying physicians consider deaths due to these causes in persons with a diagnosis of MS to be unrelated to their MS.
The limitations of death certificate data should be considered. First, it is important to recognize that this study assessed deaths attributed to MS on the death certificates rather than deaths among those diagnosed with MS. Previous studies have shown that MS is mentioned on the death certificate in 70%–80% of deaths among people with MS38–40; it is assumed that the certifying clinician does not consider MS of relevance to the remaining deaths. Reliable completion of the death certificate is dependent on the physician's training and knowledge of the patient's history. Underestimation or overestimation of the true role of other causes in MS-related deaths may occur if, for example, a physician misses a contributing condition or has preconceived ideas about the relationship between causes. Population-based MCOD data can provide information about causes that are believed by the certifying physician to contribute to deaths attributed to MS. However, these data cannot provide answers to questions regarding causes of death (as recorded on death certificates) among people who have been diagnosed with MS, for whom MS may not be mentioned at all.39 Questions regarding causes of death among people with MS are better addressed by cohort studies, in which survival and cause-specific mortality can be compared to that of the general population.41,42 Findings from population-based MCOD data complement those from MS cohort studies, which often include clinic-based samples or rely on a single underlying cause of death.
We found that respiratory disease, respiratory infection, aspiration pneumonia, urinary tract infection, other infection including sepsis, and skin disease (specifically pressure ulcers) contributed to MS deaths more frequently than they did to deaths not due to MS. While our findings imply that the complications of severe disability make a substantial contribution to mortality in MS, many of these conditions may be preventable or amenable to modification. The analysis of MCOD data is a useful approach towards a more complete understanding of the reasons for premature mortality in MS.
Acknowledgment
The authors thank the British Columbia Ministry of Health and British Columbia Vital Statistics Agency for approval and support with access to provincial data and Population Data British Columbia for facilitating approval and use of the data. All inferences, opinions, and conclusions drawn in this report are those of the authors and do not reflect the opinions or policies of the Data Steward(s).
Glossary
- aOR
adjusted odds ratio
- CI
confidence interval
- ICD
International Classification of Diseases
- MCOD
multiple cause of death
- MS
multiple sclerosis
- OR
odds ratio
Appendix. Authors
Study funding
Supported by the Canadian Institutes of Health Research (MOP-82738; PI: Tremlett) and the US National MS Society (RG:5064-A-5; PI: Tremlett).
Disclosure
K. Harding was funded by an MS Society of Canada fellowship and has received research support from Novartis for work that is unrelated to this study. F. Zhu, M. Alotaibi, and T. Duggan report no disclosures relevant to the manuscript. H. Tremlett is the Canada Research Chair for Neuroepidemiology and Multiple Sclerosis; has current research support from the National Multiple Sclerosis Society, the Canadian Institutes of Health Research, the Multiple Sclerosis Society of Canada, and the Multiple Sclerosis Scientific Research Foundation; and in the last 5 years, has received research support from the Multiple Sclerosis Society of Canada (Don Paty Career Development Award), the Michael Smith Foundation for Health Research (Scholar Award), and the UK MS Trust, and speaker honoraria and/or travel expenses to attend CME conferences from the Consortium of MS Centres (2013, 2018), the National MS Society (2014, 2016, 2018), ECTRIMS (2013, 2014, 2015, 2016, 2017, 2018, 2019), Biogen Idec (2014), and the American Academy of Neurology (2013, 2014, 2015, 2016, 2019). All speaker honoraria are either declined or donated to an MS charity or to an unrestricted grant for use by H.T.’s research group. E. Kingwell reports no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Kingwell E, van der Kop M, Zhao Y, et al. Relative mortality and survival in multiple sclerosis: findings from British Columbia, Canada. J Neurol Neurosurg Psychiatry 2012;83:61–66. [DOI] [PubMed] [Google Scholar]
- 2.Koch-Henriksen N, Laursen B, Stenager E, Magyari M. Excess mortality among patients with multiple sclerosis in Denmark has dropped significantly over the past six decades: a population based study. J Neurol Neurosurg Psychiatry 2017;88:626–631. [DOI] [PubMed] [Google Scholar]
- 3.Marrie RA, Elliott L, Marriott J, et al. Effect of comorbidity on mortality in multiple sclerosis. Neurology 2015;85:240–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goodin DS, Corwin M, Kaufman D, et al. Causes of death among commercially insured multiple sclerosis patients in the United States. PLoS One 2014;9:e105207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Medical Certification of Cause of Death: Instructions for Physicians on Use of International Form of Medical Certificate of Cause of Death. Geneva, Switzerland: 1979. Available at: apps.who.int/iris/bitstream/handle/10665/40557/9241560622.pdf. Accessed February 22, 2018. [Google Scholar]
- 6.Israel RA, Rosenberg HM, Curtin LR. Analytical potential for multiple cause-of-death data. Am J Epidemiol 1986;124:161–179. [DOI] [PubMed] [Google Scholar]
- 7.Wilkins K, Wysocki M, Morin C, Wood P. Multiple causes of death. Health Rep 1997;2:19–29. [Google Scholar]
- 8.Wilkins K, Parsons GF, Gentleman JF, Forbes WF. Deaths due to dementia: an analysis of multiple-cause-of-death data. Chronic Dis Can 1999;20:26–35. [PubMed] [Google Scholar]
- 9.Redelings MD, McCoy L, Sorvillo F. Multiple sclerosis mortality and patterns of comorbidity in the United States from 1990 to 2001. Neuroepidemiology 2006;26:102–107. [DOI] [PubMed] [Google Scholar]
- 10.Redelings MD, Wise M, Sorvillo F. Using multiple cause-of-death data to investigate associations and causality between conditions listed on the death certificate. Am J Epidemiol 2007;166:104–108. [DOI] [PubMed] [Google Scholar]
- 11.Goldacre MJ, Duncan M, Griffith M, Turner MR. Trends in death certification for multiple sclerosis, motor neuron disease, Parkinson's disease and epilepsy in English populations 1979-2006. J Neurol 2010;257:706–715. [DOI] [PubMed] [Google Scholar]
- 12.Park J, Peters PA. Mortality from diabetes mellitus, 2004 to 2008: a multiple-cause-of-death analysis. Health Rep 2014;25:12–16. [PubMed] [Google Scholar]
- 13.Jamilloux Y, Maucort-Boulch D, Kerever S, et al. Sarcoidosis-related mortality in France: a multiple-cause-of death analysis. Eur Respir J 2016;48:1700–1709. [DOI] [PubMed] [Google Scholar]
- 14.Barbieri M, Désesquelles A, Egidi V, et al. Obesity-related mortality in France, Italy, and the United States: a comparison using multiple cause-of-death analysis. Int J Public Health 2017;62:623–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kiadaliri AA, Rosengren BE, Englund M. Fracture-related mortality in southern Sweden: a multiple cause of death analysis, 1998-2014. Injury 2018;49:236–242. [DOI] [PubMed] [Google Scholar]
- 16.Patel O, Syamlal G, Wood J, Dodd KE, Mazurek JM. Asthma mortality among persons aged 15-64 years, by industry and occupation: United States, 1999–2016. MMWR Morb Mortal Wkly Rep 2018;67:60–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.British Columbia Vital Statistics Agency [creator]. 2015, Vital Statistics Deaths: V2: Population Data BC: Data Extract. BC Vital Statistics Agency, 2015. Available at: www.popdata.bc.ca/data. Accessed November 14, 2017. [Google Scholar]
- 18.National Center for Health Statistics. International Classification of Diseases, Ninth Revision, Clinical Modification. 1999. Available at: www.cdc.gov/nchs/icd/icd9cm.htm. Accessed November 14, 2017.
- 19.World Health Organisation. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. 2016. Available at: apps.who.int/classifications/icd10/browse/2016/en. Accessed November 14, 2017. [Google Scholar]
- 20.World Cancer Research Fund. Worldwide Cancer Data Online, 2017. Available at: www.wcrf.org/int/cancer-facts-figures/worldwide-data. Accessed February 28, 2018. [Google Scholar]
- 21.Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med 2002;113(1A suppl):5S–13S 5S–13S. [DOI] [PubMed] [Google Scholar]
- 22.Marrie RA, Patten S, Tremlett H, et al. Chronic lung disease and multiple sclerosis: incidence, prevalence, and temporal trends. Mult Scler Relat Disord 2016;8:86–92. [DOI] [PubMed] [Google Scholar]
- 23.Kirby S, Brown M, Murray T, et al. Progression of multiple sclerosis in patients with other autoimmune diseases. Mult Scler J 2005;11:S28–S29. [Google Scholar]
- 24.Weinshenker BG, Bass B, Rice GP, et al. The natural history of multiple sclerosis: a geographically based study: I: clinical course and disability. Brain 1989;112:133–146. [DOI] [PubMed] [Google Scholar]
- 25.Visser EM, Wilde K, Wilson JF, Yong KK, Counsell CE. A new prevalence study of multiple sclerosis in Orkney, Shetland and Aberdeen City. J Neurol Neurosurg Psychiatry 2012;83:719–724. [DOI] [PubMed] [Google Scholar]
- 26.Marrie RA, Reider N, Stuve O, et al. The incidence and prevalence of comorbid gastrointestinal, musculoskeletal, ocular, pulmonary, and renal disorders in multiple sclerosis: a systematic review. Mult Scler 2015;21:332–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.GBD 2015 Neurological Disorders Collaborator Group. Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol 2017;16:877–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manouchehrinia A, Tanasescu R, Tench CR, Constantinescu CS. Mortality in multiple sclerosis: meta-analysis of standardised mortality ratios. J Neurol Neurosurg Psychiatry 2016;87:324–331. [DOI] [PubMed] [Google Scholar]
- 29.Burkill S, Montgomery S, Hajiebrahimi M, Hillert J, Olsson T, Bahmanyar S. Mortality trends for multiple sclerosis patients in Sweden from 1968 to 2012. Neurology 2017;89:555–562. [DOI] [PubMed] [Google Scholar]
- 30.Lunde HMB, Assmus J, Myhr KM, BL, Grytten N. Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry 2017;88:621–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Capello E, Mancardi G. Marburg type and Balò's concentric sclerosis: rare and acute variants of multiple sclerosis. Neurol Sci 2004;25(4 suppl):S361–S363. [DOI] [PubMed] [Google Scholar]
- 32.Fedeli U, Zoppini G, Goldoni CA, Avossa F, Mastrangelo G, Saugo M. Multiple causes of death analysis of chronic diseases: the example of diabetes. Popul Health Metr 2015;13:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DiBardino DM, Wunderink RG. Aspiration pneumonia: a review of modern trends. J Crit Care 2015;30:40–48. [DOI] [PubMed] [Google Scholar]
- 34.Phé V, Pakzad M, Curtis C, et al. Urinary tract infections in multiple sclerosis. Mult Scler J 2016;22:855–861. [DOI] [PubMed] [Google Scholar]
- 35.Redelings MD, Lee NE, Sorvillo F. Pressure ulcers: more lethal than we thought? Adv Skin Wound Care 2005;18:367–372. [DOI] [PubMed] [Google Scholar]
- 36.Segaloff HE, Petrie JG, Malosh RE, et al. Severe morbidity among hospitalised adults with acute influenza and other respiratory infections: 2014–2015 and 2015–2016. Epidemiol Infect 2018;146:1350–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mackenbach JP, Kunst AE, Lautenbach H, Oei YB, Bijlsma F. Competing causes of death: a death certificate study. J Clin Epidemiol 1997;50:1069–1077. [DOI] [PubMed] [Google Scholar]
- 38.Brønnum-Hansen H. Trends in survival and cause of death in Danish patients with multiple sclerosis. Brain 2004;127:844–850. [DOI] [PubMed] [Google Scholar]
- 39.Hirst C, Swingler R, Compston DAS, Ben-Shlomo Y, Robertson NP. Survival and cause of death in multiple sclerosis: a prospective population-based study. J Neurol Neurosurg Psychiatry 2008;79:1016–1021. [DOI] [PubMed] [Google Scholar]
- 40.Smestad C, Sandvik L, Celius E. Excess mortality and cause of death in a cohort of Norwegian multiple sclerosis patients. Mult Scler J 2009;15:1263–1270. [DOI] [PubMed] [Google Scholar]
- 41.Ragonese P, Aridon P, Salemi G, D'Amelio M, Savettieri G. Mortality in multiple sclerosis: a review. Eur J Neurol 2008;15:123–127. [DOI] [PubMed] [Google Scholar]
- 42.Scalfari A, Knappertz V, Cutter G, Goodin DS, Ashton R, Ebers GC. Mortality in patients with multiple sclerosis. Neurology 2013; 81:184–192. [DOI] [PMC free article] [PubMed] [Google Scholar]