Abstract
Objective
To compare the proportion of APOE ε4 genotype carriers in aphasic vs amnestic variants of Alzheimer disease (AD).
Method
The proportion of APOE ε4 carriers was compared among the following 3 groups: (1) 42 patients with primary progressive aphasia (PPA) and AD pathology (PPA/AD) enrolled in the Northwestern Alzheimer Disease Center Clinical Core; (2) 1,418 patients with autopsy-confirmed AD and amnestic dementia of the Alzheimer type (DAT/AD); and (3) 2,608 cognitively normal controls (NC). The latter 2 groups were compiled from the National Alzheimer Coordinating Center database. Logistic regression models analyzed the relationship between groups and APOE ε4 carrier status, adjusting for age at onset and sex as needed.
Results
Using NC as the reference and adjusting for sex and age, the DAT/AD group was 3.97 times more likely to be APOE ε4 carriers. Adjusting for sex and age at symptom onset, the DAT/AD group was 2.46 times as likely to be carriers compared to PPA/AD. There was no significant difference in the proportion of APOE ε4 carriers for PPA/AD compared to NC. PPA subtypes included 24 logopenic, 10 agrammatic nonfluent, and 8 either mixed (n = 5) or too severe (n = 3) to subtype. The proportion of carriers and noncarriers was similar for logopenic and agrammatic subtypes, both having fewer carriers.
Conclusion
The proportion of APOE ε4 carriers was elevated in amnestic but not aphasic manifestations of AD. These results suggest that APOE ε4 is an anatomically selective risk factor that preferentially increases the vulnerability to AD pathology of memory-related medial temporal areas rather than language-related neocortices.
The single most common clinical manifestation of sporadic Alzheimer disease (AD) is an amnestic multidomain dementia also known as dementia of the Alzheimer type (DAT). However, AD can also present as aphasic, visuospatial, and frontal behavioral-type dementias.1 All clinical presentations share the common denominator of neuritic β-amyloid (Aβ) plaques and neurofibrillary tangles (NFT) but in variable neuroanatomical distributions. In DAT, NFT are most numerous in memory-related medial temporal areas, from where they spread into adjacent neocortices, in keeping with the Braak and Braak2 progression pattern. Nonamnestic syndromes have different NFT distributions. For example, an aphasic variant of AD known as primary progressive aphasia (PPA) can be associated with tangle counts more numerous in left hemisphere language areas than in hippocampal and entorhinal cortices.3 In visuospatial variants (i.e., posterior cortical atrophy), the tangles can be most abundant in occipital areas and the superior colliculus, whereas the frontal behavioral type dementia variant can display tangles most prominent in frontal cortex.4,5 The determinants of this heterogeneity remain mysterious.
Next to age, the ε4 allele of APOE is the strongest risk factor for AD. The generality of this relationship was questioned by our early work on patients with PPA with positive AD biomarkers where we showed that APOE ε4 is not an equally robust risk factor.6,7 This finding suggested that the ε4-based vulnerability to AD might offer clues to the mechanisms of clinical heterogeneity in AD. However, in our previous investigations, postmortem verification of AD pathology was not obtained for all cases. Furthermore, analyses had not been controlled for sex and age at onset, 2 factors shown to influence the APOE ε4 effect.8,9 The present study addressed these prior limitations by requiring autopsy confirmation of AD in the PPA and DAT groups and by controlling comparisons for sex and age at symptom onset.
Methods
The brain bank of the Northwestern Alzheimer's Disease Center (ADC) has a total of 52 postmortem autopsy samples obtained from individuals with a clinical diagnosis of PPA and a neuropathologic diagnosis of AD. Ten cases were excluded from further study for various reasons: APOE not yet available (n = 1), very limited clinical information and no APOE (n = 6), or a second important primary neuropathologic finding (Lewy body disease [n = 2]; frontotemporal lobar degeneration with TDP-43 inclusions [n = 1]). Of the remaining 42, 13 had only AD neuropathologic change; 29 had a secondary finding deemed not pathologically significant. Of these 29, 17 had evidence of nonocclusive cerebrovascular disease; an additional 4 had vascular disease with an infarct or microinfarcts in nonstrategic areas; another 7 had limbic or amygdala Lewy bodies, brainstem Lewy bodies, or medial temporal TDP in addition to nonocclusive vascular disease. The remaining case had limbic Lewy bodies and hippocampal sclerosis with TDP.
The 42 cases in the sample all had been followed in the Northwestern ADC Clinical Core, funded by the National Institute on Aging, where they had donated blood for APOE genotyping and underwent annual follow-up clinical examinations. Those enrolled after 2005 were followed by the ADC Uniform Data Set (UDS)10–13 and committed to brain donation after death. In addition, those enrolled after 2007 had also participated in the Northwestern PPA Program, where they had extensive neuropsychological testing to make the root diagnosis of PPA and establish the aphasia subtype according to the 2011 guidelines.14 Cases enrolled prior to 2011 were diagnosed by detailed review of clinical charts and clinical consensus according to the new guidelines. All neuropathologic diagnoses were made using criteria established in the ADC program.15,16
Two comparison groups were identified from the National Alzheimer Coordinating Center (NACC) database, a national repository for data collected by the ADCs. One group consisted of cases with a primary clinical diagnosis of typical amnestic DAT (i.e., primary presumptive etiologic diagnosis of Alzheimer dementia),1,17 neuropathologic diagnosis of AD (i.e., Braak stages III–VI and moderate or frequent neuritic plaques, or intermediate to high likelihood of AD neuropathologic change), APOE genotyping, and age at onset within the range of the PPA sample (46–80 years, n = 1,418). All participants had been followed prospectively with the UDS during their lifetime. The second group consisted of cognitively healthy controls who were required to have remained cognitively normal for at least 5 consecutive yearly UDS visits prior to inclusion in the present study, and with age at the fifth UDS visit (index age) within the same range as the PPA sample (n = 2,608). Control cases were not required to have had brain autopsy due to relatively small sample size (supplementary material available at doi.org/10.5061/dryad.69qg1c0).
All participants in the studies from which data were acquired had given informed consent to participate in the parent studies in protocols approved by the institutional review boards of the parent institutions. Informed consent had included agreement to share data.
Data analysis
Differences in demographics between groups were tested with t tests and χ2 tests. We used logistic regression models to examine whether APOE ε4 carrier vs noncarrier status was associated with disease group. Unadjusted and adjusted logistic regression analyses were conducted. We ran the following 3 separate multivariable logistic regression models: (1) PPA/AD vs normal controls, (2) DAT/AD vs normal controls, and (3) PPA/AD vs DAT/AD. Multivariable models that included normal controls adjusted for sex, age at symptom onset for the disease group, and age at fifth UDS visit for the normal controls (i.e., index age). The multivariable model comparing PPA/AD with DAT/AD adjusted for sex and age at onset of symptoms.
Data availability
Anonymized data will be shared on request from qualified investigators.
Results
Table 1 shows descriptive statistics for all groups. Although the range of symptom onset age was similar in the PPA/AD and DAT/AD groups, the mean onset age was lower for PPA/AD (p < 0.001). In addition, the proportion of men and women differed between the normal control group and each clinical group (both p < 0.001) but not between the PPA/AD and DAT/AD groups (p = 0.33). PPA/AD and DAT/AD groups were populated mostly by men. See supplementary material at doi.org/10.5061/dryad.69qg1c0 for a more detailed breakdown of the case samples by age.
Table 1.
Descriptive statistics of patient and control groups
Adjusting for sex and age, the DAT/AD group was 3.97 times more likely to be an APOE ε4 carrier compared to normal controls (95% confidence interval [CI] 3.42–4.59; table 2). Using PPA/AD as the reference group, members of the DAT/AD group were 2.46 times more likely to be APOE ε4 carriers after adjusting for sex and age at onset (95% CI 1.31–4.70; table 2). There was no difference in the proportion of APOE ε4 carriers between PPA/AD and normal controls (odds ratio 1.05, 95% CI 0.54–2.00; table 2). Both logopenic and agrammatic PPA subtypes had fewer carriers than noncarriers (table 3).
Table 2.
Unadjusted and adjusted odds ratios (ORs) and 95% confidence intervals (CIs) of APOE ε4 carriers
Table 3.
Distribution of carriers vs noncarriers in primary progressive aphasia (PPA) clinical subtypes

To determine whether unequal participant numbers could influence our conclusions, a subsequent analysis was run (table e-1, doi.org/10.5061/dryad.69qg1c0), where we matched by sex and age at onset of symptoms (or age at fifth UDS visit for cognitively normal controls). The matched samples had a similar proportion of ε4 carriers compared to unmatched samples.
Discussion
APOE ε4 is a major genetic risk factor for AD, especially for its typical amnestic form. In other clinical presentations of AD neuropathology, most notably PPA, it does not appear to carry similar weight. In the present study, based on autopsy-confirmed cases and controlling for sex and age at symptom onset, we confirmed with even greater analytical rigor that individuals with PPA and AD neuropathology do not have a disproportionate representation of APOE ε4 carriers when compared with either cognitively healthy controls or individuals with amnestic dementia and AD neuropathology. In addition, both the logopenic and agrammatic subtypes had significantly fewer carriers than noncarriers.
The role of APOE ε4 in Alzheimer pathogenesis is not fully understood. Some have attributed the underlying mechanism to enhancing Aβ processing or deposition, others to tau phosphorylation, and others to neuroplasticity.18 One analysis of data from the Alzheimer’s Disease Neuroimaging Initiative investigated the relationship between APOE ε4 and cognitive and neuroanatomical measures in individuals with mild DAT and positive AD biomarkers. In that study, carriers had greater deficits on memory tests and greater atrophy in medial temporal structures than noncarriers, while noncarriers had worse scores on nonmemory tests and greater atrophy in frontoparietal cortices.19 Even in cognitively normal APOE ε4 carriers compared with noncarriers, there is evidence for marginally smaller hippocampal volumes.20 It appears therefore that APOE ε4 increases the vulnerability to AD in an anatomically selective fashion that targets the medial temporal limbic structures. A better understanding of this effect could help to identify at least one mechanism that underlies the anatomical diversity and clinical heterogeneity of neurodegenerative entities such as AD.
One caveat is the relatively small sample of individuals with PPA and postmortem AD. However, this sample was highly curated and worked up in detail, leaving little doubt as to the stringency of clinical diagnosis. Another caveat is the high percentage of APOE ε4 carriers in the DAT/AD group (65.7%) and in the cognitively normal control group (32.7%). The NACC database collects data from specialized research centers and attracts a different sample than do population-based studies. In fact, the frequencies we report are in line with data reported in one Alzheimer’s Disease Neuroimaging Initiative study.21 That carrier rates in AD can vary substantially was demonstrated in a meta-analysis of prevalence rates globally, where it was shown that prevalence rate was 47.21% for population-based studies, 58.68% for autopsy studies, and 63.47% for randomized clinical trials.22
The risk conferred by APOE ε4 on the typical amnestic dementia due to AD pathology does not appear to hold true for other clinical phenotypes of the disease. This conclusion encompasses agrammatic as well as logopenic forms of PPA.
Glossary
- Aβ
β-amyloid
- AD
Alzheimer disease
- ADC
Alzheimer's Disease Center
- CI
confidence interval
- DAT
dementia of the Alzheimer type
- NACC
National Alzheimer Coordinating Center
- NFT
neurofibrillary tangles
- PPA
primary progressive aphasia
- UDS
Uniform Data Set
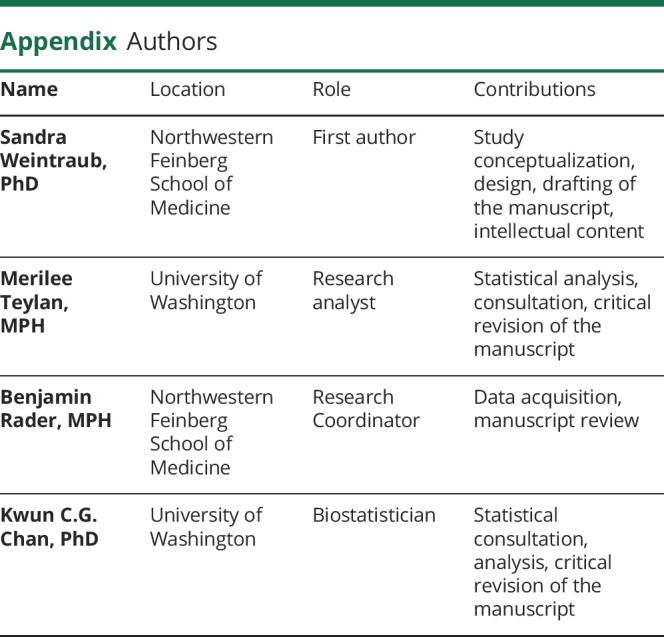
Appendix. Authors

Study funding
Study funded by grants from the National Institute of Neurologic Disorders and Stroke (NS085770), the National Institute on Deafness and Other Communication Disorders (R01 DC008552), National Institute of Neurologic Diseases and Stroke (R01 NS075075), and the National Institute on Aging (AG013854, AGO56258). The NACC database is funded by NIA/NIH grant U01 AG016976. NACC data are contributed by the NIA-funded ADCs: P30 AG019610 (PI Eric Reiman, MD), P30 AG013846 (PI Neil Kowall, MD), P50 AG008702 (PI Scott Small, MD), P50 AG025688 (PI Allan Levey, MD, PhD), P50 AG047266 (PI Todd Golde, MD, PhD), P30 AG010133 (PI Andrew Saykin, PsyD), P50 AG005146 (PI Marilyn Albert, PhD), P50 AG005134 (PI Bradley Hyman, MD, PhD), P50 AG016574 (PI Ronald Petersen, MD, PhD), P50 AG005138 (PI Mary Sano, PhD), P30 AG008051 (PI Thomas Wisniewski, MD), P30 AG013854 (PI M. Marsel Mesulam, MD), P30 AG008017 (PI Jeffrey Kaye, MD), P30 AG010161 (PI David Bennett, MD), P50 AG047366 (PI Victor Henderson, MD, MS), P30 AG010129 (PI Charles DeCarli, MD), P50 AG016573 (PI Frank LaFerla, PhD), P50 AG005131 (PI James Brewer, MD, PhD), P50 AG023501 (PI Bruce Miller, MD), P30 AG035982 (PI Russell Swerdlow, MD), P30 AG028383 (PI Linda Van Eldik, PhD), P30 AG053760 (PI Henry Paulson, MD, PhD), P30 AG010124 (PI John Trojanowski, MD, PhD), P50 AG005133 (PI Oscar Lopez, MD), P50 AG005142 (PI Helena Chui, MD), P30 AG012300 (PI Roger Rosenberg, MD), P30 AG049638 (PI Suzanne Craft, PhD), P50 AG005136 (PI Thomas Grabowski, MD), P50 AG033514 (PI Sanjay Asthana, MD, FRCP), P50 AG005681 (PI John Morris, MD), P50 AG047270 (PI Stephen Strittmatter, MD, PhD).
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Braak H, Braak E. Staging of Alzheimer-related cortical destruction. Int Psychogeriatr 1997;9:257–261; discussion 269–272. [PubMed] [Google Scholar]
- 3.Gefen T, Gasho K, Rademaker A, et al. Clinically concordant variations of Alzheimer pathology in aphasic versus amnestic dementia. Brain 2012;135:1554–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hof PR, Vogt BA, Bouras C, Morrison JH. Atypical form of Alzheimer's disease with prominent posterior cortical atrophy: a review of lesion distribution and circuit disconnection in cortical visual pathways. Vis Res 1997;37:3609–3625. [DOI] [PubMed] [Google Scholar]
- 5.Johnson JK, Head E, Kim R, Starr A, Cotman CW. Clinical and pathological evidence for a frontal variant of Alzheimer disease [see comments]. Arch Neurol 1999;56:1233–1239. [DOI] [PubMed] [Google Scholar]
- 6.Rogalski E, Sridhar J, Rader B, et al. Aphasic variant of Alzheimer disease: clinical, anatomic, and genetic features. Neurology 2016;87:1337–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rogalski EJ, Rademaker A, Harrison TM, et al. ApoE E4 is a susceptibility factor in amnestic but not aphasic dementias. Alzheimer Dis Assoc Disord 2011;25:159–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farrer LA, Cupples LA, Haines JL, et al. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease: a meta-analysis: APOE and Alzheimer Disease Meta Analysis Consortium [see comments]. Jama 1997;278:1349–1356. [PubMed] [Google Scholar]
- 9.Blacker D, Haines JL, Rodes L, et al. ApoE-4 and age at onset of Alzheimer's disease: the NIMH genetics initiative. Neurology 1997;48:139–147. [DOI] [PubMed] [Google Scholar]
- 10.Morris JC, Weintraub S, Chui HC, et al. The Uniform Data Set (UDS): clinical and cognitive variables and descriptive data from Alzheimer Disease Centers. Alzheimer Dis Assoc Disord 2006;20:210–216. [DOI] [PubMed] [Google Scholar]
- 11.Beekly DL, Ramos EM, Lee WW, et al. The National Alzheimer's Coordinating Center (NACC) database: the Uniform Data Set. Alzheimer Dis Assoc Disord 2007;21:249–258. [DOI] [PubMed] [Google Scholar]
- 12.Besser L, Kukull W, Knopman DS, et al. Version 3 of the National Alzheimer's Coordinating Center's Uniform Data Set. Alzheimer Dis Assoc Disord 2018;32:351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weintraub S, Besser L, Dodge HH, et al. Version 3 of the Alzheimer Disease Centers' neuropsychological test battery in the Uniform Data Set (UDS). Alzheimer Dis Assoc Disord 2018;32:10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gorno-Tempini ML, Hillis AE, Weintraub S, et al. Classification of primary progressive aphasia and its variants. Neurology 2011;76:1006–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hyman BT, Phelps CH, Beach TG, et al. National Institute on Aging-Alzheimer's Association guidelines for the neuropathologic assessment of Alzheimer's disease. Alzheimers Dement 2012;8:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montine TJ, Phelps CH, Beach TG, et al. National Institute on Aging-Alzheimer's Association guidelines for the neuropathologic assessment of Alzheimer's disease: a practical approach. Acta Neuropathol 2012;123:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan E. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer's disease. Neurology 1984;34:939–944. [DOI] [PubMed] [Google Scholar]
- 18.Nathan BP, Jiang Y, Wong GK, Shen F, Brewer GJ, Struble RG. Apolipoprotein E4 inhibits, and apolipoprotein E3 promotes neurite outgrowth in cultured adult mouse cortical neurons through the low-density lipoprotein receptor-related protein. Brain Res 2002;928:96–105. [DOI] [PubMed] [Google Scholar]
- 19.Wolk DA, Dickerson BC; Alzheimer's Disease Neuroimaging Initiative. Apolipoprotein E (APOE) genotype has dissociable effects on memory and attentional-executive network function in Alzheimer's disease. Proc Natl Acad Sci USA 2010;107:10256–10261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reiman EM, Uecker A, Caselli RJ, et al. Hippocampal volumes in cognitively normal persons at genetic risk for Alzheimer's disease. Ann Neurol 1998;44:288–291. [DOI] [PubMed] [Google Scholar]
- 21.Schuff N, Woerner N, Boreta L, et al. MRI of hippocampal volume loss in early Alzheimer's disease in relation to ApoE genotype and biomarkers. Brain 2009;132:1067–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crean S, Ward A, Mercaldi CJ, et al. Apolipoprotein E epsilon4 prevalence in Alzheimer's disease patients varies across global populations: a systematic literature review and meta-analysis. Dement Geriatr Cogn Disord 2011;31:20–30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data will be shared on request from qualified investigators.




