Abstract
The obese population is particularly challenging to the spine surgeon in all phases of care. A narrative literature review was performed to review difficulties in spine surgery on the obese patient population and techniques for mitigation. We specifically aimed to assess several topics with regard to this population: patient selection and pre-operative care; intra-operative and surgical techniques; and post-operative care, outcomes, and complications. The literature review demonstrated that obese patients are at increased surgical risk with spine surgery due to a variety of factors at all stages of intervention. Pre-operatively, obese patients have worse outcomes with physical therapy and present technical difficulties for injections. Transport to a hospital, imaging, resuscitation, and intubation are all challenged by increased body habitus. Intraoperatively, obese patients have increased operative times, blood loss, surgical site infections, and nerve palsies. Patient positioning and intraoperative imaging may be limited. Surgery itself may be technically challenging due to body habitus and minimally invasive techniques are becoming more prevalent in this population. Postoperatively, several studies demonstrate that obese patients have inferior outcomes compared to non-obese counterparts. Patient selection is key for elective interventions, and appropriate infrastructure aids in the ultimate outcomes for both elective and non-elective surgical treatments. Overall, obese patients present several challenges to the spine surgeon, and certain precautions can be undertaken preoperatively, intraoperatively, and postoperatively to mitigate the associated risks to and to optimize outcomes.
Keywords: narrative review, spine surgery, obesity, complications, body mass index (BMI)
Introduction
Obese patients present challenges in all phases of spine-related care and spinal surgery: preoperatively, intraoperatively, and postoperatively. With an increasing prevalence of obesity and an association between obesity and back pain, surgeons will see increasing numbers of obese patients with spine pathologies [1–3]. As Jakoi et al. demonstrate, the prevalence of patients with both lumbar degenerative disc disease and obesity has increased more than 5 times relative to the prevalence of patients with degenerative disc disease without obesity [4]. Obese patients undergoing surgery, however, are at increased risk of perioperative complications, morbidity, and mortality [5–19]. Increased body mass index (BMI) has been demonstrated to affect outcomes in all age groups. Studies have shown that obese adolescents undergoing spinal fusion for adolescent idiopathic scoliosis and obese adults undergoing spinal deformity surgery do worse than their non-obese counterparts [20,21].
Obesity is a growing epidemic that is starting to gain more attention in the spine literature. An increasing number of studies are being published that document the significantly increased risk of operating on the obese patient [5–19]. Puvanesarajah et al., for example, demonstrated that obese and morbidly obese patients older than 65 years undergoing lumbar fusion had significantly higher odds of experiencing a major medical complication, wound infection, wound dehiscence, and thirty-day readmission, as well as incurring longer length of stay and in-hospital costs [12]. Phan et al. likewise determined that morbidly obese patients undergoing posterior cervical fusion had increased risk of venous thromboembolism, and those undergoing anterior lumbar interbody fusion had increased risk for 30-day readmissions [16,17]. Burks et al. demonstrated that obesity is associated with increased rates of incidental durotomy in lumbar spine surgery [15]. The spine surgeon, thus, can encounter complications pre-operatively before an incision is made, intra-operatively, and/or post-operatively. This paper reviews the challenges of managing spine pathology in obese patients, and provides some tips to try to mitigate the risks.
Literature Review
Preoperative, intraoperative, and postoperative issues with obese patients undergoing spine surgery were explored. Pubmed and google scholar searches were performed using keywords “obesity,” “obese,” “spine,” and “surgery.” Article abstracts were assessed for relevancy. Secondary review of bibliographies of applicable articles were reviewed for additional relevant articles. Tertiary searches were done to answer additional questions in relation to perioperative care in this patient population.
Pre-operative challenges
Elective Surgery
Obesity is a modifiable risk factor that has been shown to be associated with several spinal disorders across various age and sex groups [22]. Conservative treatment for elective cases may include physical therapy, injections, nonsteroidal anti-inflammatory drugs (NSAIDs), and muscle relaxants. Analysis of the Spine Patient Outcomes Research Trial (SPORT) demonstrated that obese (BMI ≥30) patients with lumbar stenosis undergoing non-operative treatment did worse with regards to Oswestry Disability Index (ODI) and the bodily pain and physical function domains of the SF-36 when compared to patients with BMI<30 [23]. Similarly, obese patients with degenerative spondylolisthesis had similar SF-36 bodily pain scores but less improvement in the SF-36 physical function and ODI scores compared to their non-obese counterparts [23]. With regards to physical therapy, obesity has been shown to be an independent predictor of treatment failure [24]. Transforaminal epidural steroid injections (TFESI) are another effective conservative treatment option for lumbar disc herniation and radicular pain relief [25]. However, the obese patient population presents challenges with regards to fluoroscopy due to potentially difficult visualization of landmarks and need for longer needles. Cushman et al. demonstrated that obese patients had significantly longer mean fluoroscopy times and radiation doses during lumbar TFESIs [26].
Weight reduction in itself can have an effect on back pain, as Khoueir et al. demonstrated that substantial weight loss after bariatric surgery may be associated with moderate reductions in preexisting back pain at early-follow-up [27]. Similarly, Lidar et al. demonstrated bariatric surgery and weight reduction is associated with a significant decrease in low back pain, radicular pain, and marked increase in L4–5 intervertebral disk height [28]. Pre-operative weight loss may prevent a percentage of patients from requiring spine procedures, and perhaps bariatric surgery, in the setting of elective spine surgery, should be utilized to optimize outcomes. One case report, for example, illustrated a super obese patient who had improvement in his myelopathy following bariatric surgery, suspected secondary to a change in spinal alignment [29]. Jain et al., additionally, demonstrated that patients undergoing bariatric surgery before elective posterior lumbar fusion had lower rates of respiratory failure, urinary tract infection, acute renal failure, infection, overall medical complications, and lower hospital length of stay compared to obese patients with BMI over 40 [30].
Bariatric surgery and its relation to spine outcomes is not without controversy, however, as some studies have demonstrated bariatric surgery results in a greater risk of osteoporosis, reduced bone mineral density (BMD), Vitamin D deficiency, and an increased risk of spinal fractures [5]. Shanbhogue et al. determined that bone loss and deterioration of bone strength in the hip and spine continue into the years after gastric bypass, despite weight stabilization and maintenance of metabolic parameters [31]. The potential risk of reduced bone mineral density must be weighed against the potential benefit of reduced axial back pain [32]. Perhaps targeted pre-operative evaluations, such as the subcutaneous lumbar spine (SLS) index, can help stratify the risk of surgery in an obese patient to determine which course of action a surgeon should take, particularly in those with viable non-operative options [33].
Non-elective surgery
As Rosenfeld et al. describe, several logistical challenges exist for morbidly obese patients even prior to arrival to a hospital [34]. Patients sustaining trauma or being found down are often delayed in transport and transfer to an appropriate trauma level of care institution as often times special transport equipment is not readily available. It is not uncommon for emergency medical services to inquire about patient weight and size prior to arriving on the scene for better planning [35]. Traditional stretchers have average size limitations of 270–318kg but modifications have been developed for the larger patient. Specially designed ambulances may need to be utilized. Additionally, rotary or small fixed-wing aircraft have weight and size constraints which may limit transfer to that by road only. Smaller EMS helicopters for example, carry patients with a maximum of 135 kg while fixed-wing aircraft have limits of 260kg [35]. Additional challenges include obtaining intravenous access (may require intra-osseous access), measuring appropriate blood pressure due to inadequately sized cuffs, or applying appropriate cervical spine immobilization due to an ill-fitting collar. In that case, taped towel rolls may be applied to each side of the head for stabilization.
Upon arrival to an institution, obese individuals face several imaging limitations [36,37]. MRI may be not possible in this patient population, which is generally dependent upon the patient’s weight (due to table weight limits) as well as maximum girth (due to limitations of closed MRI dimensions). Furthermore, computed tomography (CT) scans may be of limited utility in these groups. Bony anatomy in CT scan may be difficult to visualize due to excess soft tissue or averaging artifact, and even CT myelogram may be of limited utility in this population (Figure 1). Limited or non-existent pre-operative imaging may lead to incorrect diagnoses, poor surgical planning, and overall increased surgical risk. Discussion with patient and family regarding these limitations and their effect on surgical planning are necessary. Alternatives to surgery are similarly limited. If the bariatric spine patient is to be treated with an orthotic, it may be difficult to obtain one that is appropriately sized. Due to excess soft adipose tissue, obese patients have additional protection of visceral organs; the energy, however, is transmitted to the axial and appendicular osseous structures and obese patients are more likely to sustain pelvic or extremity fractures [37].
Figure 1.
Super obese patients present limitations in pre- and post-operative imaging as well as patient positioning. A. Myelogram demonstrates poor penetration due to body habitus. MRI was not possible due to excessive body girth. B. Tape was used to manage skin folds. C. Post-operative films after a C3–7 laminectomy and fusion based upon the presumption of levels of stenosis due limited imaging (seen in A) in the classic clinical setting of myelopathy.
Anesthetic Issues
If surgery is indicated, obese patients present particular challenges in relation to anesthesia [38,39]. Obesity is associated with cardiac and pulmonary hypertension, ventricular deficiency, heart disease, and obstructive sleep apnea amongst other co-morbidities, and particular attention needs to be paid in the pre-operative evaluation. Obese trauma patients generally have higher base deficits than non-obese counterparts and are often under-resuscitated due to fluid and blood products not adjusted for their size [37]. At times pre-operative optimization is needed with BiPAP ventilation or respiratory physiotherapy. Intubation is more difficult due to increased neck circumference and poor visibility of the oropharynx, and may require fiberoptic assistance. Prone positioning adds additional risk of airway loss, and itself is challenging in the obese population. Douglass et al. describe awake fiberoptic intubation and awake prone positioning to overcome difficulties in transferring an anesthetized bariatric patient into the prone position [39]. Additional limitations in the morbidly obese include more difficult mechanical ventilation due to a restrictive chest wall, less accurate monitoring, easier dislodgement of endotracheal tubes, and increased susceptibility to airway edema and obstruction [34]. Lateral position may improve cardiovascular issues as the pannus is displaced away from the diaphragm and inferior vena cava [37]. Post-operatively, residual accumulation of anesthetics in the adipose tissue may affect ease of extubation, and a planned extubation may be required in the intensive care unit.
Operative challenges
Cao et al. performed a meta-analysis demonstrating that obesity is associated with longer operative times, greater post-operative blood loss, higher risk of surgical site infections, and higher risk of nerve injuries in lumbar spine surgery [40]. Lingutla et al. similarly performed a systematic review and meta-analysis of lumbar spine fusion in obese and non-obese patients and found greater intra-operative blood loss, longer duration of surgeries, and more complications in the obese patients [8].
Several studies illustrate that increased BMI is associated with increased blood loss or transfusion risk. Onyekwelu et al. demonstrated higher blood product requirement and extended hospital stay in obese patients requiring lumbar fusion [41]. Shamji et al. found that higher BMI to be associated with increased transfusion requirements and likelihood of discharge to assisted living after thoracolumbar spine fusion [42]. Longer operating time may be the etiology of greater intra-operative blood loss, or due to increased venous bleeding due to increased intra-abdominal or intra-thoracic pressures. The surgeon should be prepared and have additional blood ready for high-risk patients or can consider use of the Cell Saver (Haemonetics Corp). Meta-analyses and systematic reviews have also demonstrated that tranexamic acid (TXA) reduces perioperative blood loss and blood transfusions, and should be utilized in appropriate cases [43,44]. Neuromonitoring may also be more difficult in obese patients; needles need to be long enough to reach the muscle and higher BMI has been shown to be associated with false positive alerts with transcranial motor-evoked potential (TcMEP) monitoring [45].
A majority of studies reveal an association between obesity and surgical site infections. Olsen et al. performed a retrospective study to assess risk factors for surgical site infections in spine surgery and found morbid obesity with BMI >35 to be an independent risk factor [19]. Spine surgeons operating on high risk populations can take special measures to limit post-operative wound complications. Multicenter studies, systematic reviews, and meta-analyses have demonstrated that intra-wound, prophylactic vancomycin powder decreases the risk of developing surgical site infections, although some studies express concern about its effects on increasing the incidence of gram-negative and polymicrobial surgical site infections or potential for pseudoarthrosis [46–50]. Copious irrigation with antimicrobial solution (e.g., bacitracin or povidone-iodine in saline), multilayer closure to obliterate the dead space, placement of postoperative drains, occlusive dressings, post-operative antibiotics, and nasal/body decontamination have also been described as potential interventions to limit infections, although the evidence is limited [51–53].
Obese patients may require unique operative room set-up and positioning [37]. Multiple people—i.e., lift teams—are required for positioning, both for sake of the patient and the healthcare providers; in fact, some states have passed legislature pertaining to manual patient lifting [54]. Obese individuals may exceed the weight limits of the spine-capable operative tables, which often vary from 500–1000 pounds. In these instances, it may be possible to utilize a setup with two flat Jackson beds, belted together, with a Wilson frame strapped straddling both beds if the Wilson frame has a higher weight rating (Figure 2). Care must be taken, however, to ensure that the weight limit of the Wilson frame is not exceeded. Alternatively, the patient may be placed on large gel rolls (e.g. under sternum and pelvis). One challenge in prone positioning is the accommodation of an obese abdomen (or in some cases a large ventral hernia). The inability to position patients with a free-hanging abdomen may lead to increased intra-abdominal pressure and subsequently increased epidural venous pressure and bleeding during surgery. Although some patients can fit on a single Jackson frame, which can accommodate the abdomen, care must be taken to place additional padding around the sides of the frame to prevent skin pressure breakdown. While these techniques can accommodate the weight of such patients, one limitation includes difficulty safely positioning the head and neck, which are often far above the level of the bed due to abdominal obesity. One option is to suspend the neck in tongs hooked up to 8–10 pounds of traction, which allows neutral positioning of the head and neck without placing the face in a standard padded head holder, decreasing not only the risk for pressure sores to the face, but also decreasing intraocular pressure and potentially the risk of postoperative vision loss [55]. Particular care must be paid to appropriate padding, particularly of the extremities, as morbidly obese patients, especially those with BMI greater than 40, are at an increased risk of positioning-related peripheral neuropathy [7]. Finally, due to body habitus and positioning modifications, the patient may be relatively unstable on the bed; the use of wide silk tape can help secure the patient in place.
Figure 2.
Positioning issues when a patient outweighs the table maximum weight. Two Jackson tables may be utilized with the patient centered on a Wilson frame strapped to both. Several straps hold the two beds together and extra material is necessary to support the head which is elevated off the table surface. Extra padding is used to accommodate the pannus and to maintain spinal alignment. Multiple people are required to position. The C-arm is arced overhead as it cannot be positioned around both beds and patient.
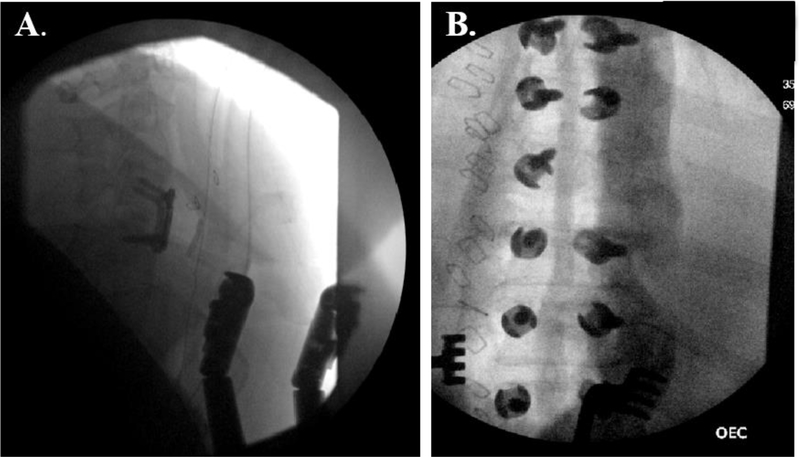
Fluoroscopy is well known to be more difficult in obese patient populations [36]. Compromised intra-operative imaging due to excess soft tissue may lead to difficult visualization (Figure 3) or, worse, wrong level surgery. AP views may be required to localize the surgical levels to provide a targeted incision if possible. Similarly, AP views may be useful in incision planning to find midline, when the midline is not palpable or otherwise apparent, nor will it reliably be at the apparent center of the field due to drift of the patient on the bed. Intra-operative CT or navigation may be considered in patients where radiography is central to instrumentation, although image quality is generally significantly degraded in more obese individuals and any specialized tables required for the use of navigation may have insufficient weight limits. Additionally, intra-operative O-arm devices or CT scanners may not have a large enough aperture to accommodate some patients. Flipping the C-arm over the operative table may be required as its diameter will not accommodate going around a double-table set up (Figure 2). Fluoroscopy images may need to be taken in an oblique nature if a true lateral is unable to be obtained due to size limitations. This, however, requires the surgeon to be familiar with the appearance of normal anatomic structures in the infrequently-used oblique projection, which may limit image utility. Furthermore, the difficulty of operating across such a wide field should not be underestimated. It may be required to deem the bottom (or sides lateral to the patient) of the operative table as “non-sterile” and either lean or kneel on any available space alongside the patient (keeping in mind this addition also factors into the total weight limit of the two beds). In both anterior and posterior cervical surgery, consideration should be given to a steep incline of the bed in order to both help ventilation and to utilize gravity to pull the excess tissue away from the operative field and improve radiographic images. Wide silk tape may be used to help straighten skin folds and keep the peri-incisional skin relatively taut, although too much traction may lead to skin breakdown.
Figure 3:
Poor quality intra-operative images in super obese patients increase the difficulty of spine surgery.
Significantly obese patients additionally provide technical surgical limitations, with poor operative corridors, poor visualization, and possibly suboptimal instrumentation if the surgical field is limited. Longer incisions may be required. Longer instruments (e.g., bayoneted bipolar forceps or Kerrisons) may alleviate some difficulty in working in deep incisions. Weitlaners utilized vertically and stacked may be reasonable retraction when exposure width is limited as compared to depth (i.e., cervical spine). The use of self-retaining abdominal retractor frame systems, with their relatively long blades, may be beneficial for posterior spinal exposures in obese patients. Additionally, Phan et al. have demonstrated lower fusion rates in obese (60%) compared to normal-weight (88.2%) and overweight patients (76%) [56]. Bone autograft harvesting can be technically challenging, so allograft or substitute may need to be used. These patients are clearly in a demographic to benefit from minimally invasive surgery (MIS) techniques; however, it has been our preference to not do such cases percutaneously (and have had to abort such attempts), purely due to the difficulty of securing adequate radiographic anatomical markers without excessive radiation to the surgical team. When considering percutaneous screw placement, one useful technique is creating a midline incision down to fascia and inserting Jamshidi needles through fascial incisions rather than skin incisions, in order to minimize parallax effects, improve maneuverability of the Jamshidis, and in order to accommodate the length of the Jamshidi, which may be insufficient for some obese patients. In this instance, AP views may need to be obtained with saline irrigation in the wound. The anterior retroperitoneal approach is also feasible in the overweight or obese cohort; obese patients have been shown to have increased durations of surgery and longer lengths and depths of incisions, but similar vascular and infectious complications compared to patients of normal weight [57,58].
Recent studies have demonstrated good results with MIS techniques, although obese patients may have increased surgery time, increased complications and less clinical benefits compared to non-obese counterparts [59–61]. Bohl et al., for example, demonstrated that greater BMI is an independent risk factor for undergoing a revision procedure following a single level MIS lumbar discectomy [62]. MIS techniques, compared to conventional open procedures, however, may provide similar outcomes while decreasing incision length, blood loss, operative time, and length of stay [63]. Adogwa et al. reviewed patients with BMI >30 and demonstrated similar improvement in pain, functional disability, and complication rates when comparing elective open versus MIS-transforaminal lumbar interbody fusion (TLIF) for degenerative disc disease or Grade I spondylolisthesis with central or foraminal stenosis who failed medical management [64]. Similar TLIF results were seen by Lau et al. in which obese patients had equivalent clinical outcomes and complication rates compared patients with normal weight [65]. Lastly, Park et al. demonstrated similar complication risks when comparing patients over and under BMI of 25 undergoing MIS spine surgery [66]. MIS techniques, however, have steep learning curves with potential for difficult access to the spine pathology, greater working distances, and poor imaging quality; therefore, proper surgical training, suitable patient selection, and careful choice of surgical materials is important [60,67].
Post-operative issues, complications, and outcomes
Post-operatively, it is important to mobilize bariatric patients as soon as is safe and possible. Additional people and equipment may be necessary to decrease risk of injury to the patient and healthcare employees; motorized ceiling lifts and “lift teams” have been shown to decrease the rate of hospital-acquired pressure ulcers, decrease patient handling-related employee injuries, and improve employee satisfaction while decreasing hospital costs [68]. A multidisciplinary team, including nutritionists, dieticians, social workers, and physical and occupational therapists should be involved. Obese patients are at an increased risk of venous thromboembolism, which is further compounded in trauma patients [34]. Sequential compression devices, if able to be fitted appropriately, along with appropriate weight-adjusted dosing of LMWH prophylaxis help reduce incidence of deep venous thrombosis and pulmonary embolism. For high risk patients, (e.g., obese patient with spinal cord injury), prophylactic vena cava filters or initiation of anticoagulation may be warranted and has been done at our institution.
Several studies suggest that post-operative outcomes are inferior in the obese population compared to the non-obese population. Giannadakis et al. determined that non-obese patients had more improvement in back and leg pain and had shorter surgeries in the setting of decompressive surgery for lumbar spinal stenosis [69]. Onyekwelu et al. similarly demonstrated slightly worse back pain scores at 2 years post-operatively in obese patients requiring lumbar decompression without fusion [41]. Elsayed et al. demonstrated that both obese and non-obese patients had significant improvements in pain scores after lumbar decompressive surgery for stenosis, but obese patients continued to report greater pain at 3 months post-operatively that later resolved by 12 months [70]. Bohl et al. demonstrated increased need for revision surgeries in patients with greater BMI and, lastly, Wilson et al. demonstrated that increased BMI was associated with increased post-operative disability in patients undergoing surgery for degenerative cervical myelopathy [62,71].
It is unclear whether obese patients undergoing surgery experience greater weight loss post-operatively. Joseph at al. demonstrated that patients undergoing a successful transforaminal lumbar interbody fusion (TLIF) procedure with improved function and pain scores did not have significant change in weight post-operatively [72]. Akins et al., however, demonstrated that obese and extremely obese patients undergoing lumbar spine fusions experienced more significant weight loss compared to non-obese patients, perhaps due to improvements in back pain and increased physical activity, or perhaps due to the fact they had more excess weight to lose [73].
It is important to note that not all studies demonstrate significant differences between obese and non-obese patients. Pereira et al. found no differences in surgical site infections, surgical complications, and re-operation rates due to BMI in the setting of degenerative lumbar spine disease [74]. Buerba et al. did not find increased complication rates after anterior or posterior cervical fusion in the 30 day post-operative period with larger BMI, a conclusion echoed by Narain et al. demonstrating comparable surgical outcomes, narcotics consumption, and hospital costs among different BMI classes undergoing anterior cervical discectomy and fusion (ACDF) [75,76]. Lingutla et al. performed a systematic review and meta-analysis of lumbar spine fusion in obese and non-obese patients and found no difference in pain and functional outcomes [8]. Chotai et al. studied the effect of obesity on cost per quality-adjusted life years gained following ACDF surgery in elective degenerative pathology; the authors found no significant differences in post-discharge health-care resource utilization, direct cost, in- direct cost, and total cost between obese and non-obese patients at post-operative 1-year and 2-year follow-up [77]. Finally, several studies demonstrate similar outcomes between obese and non-obese patients when utilizing minimally invasive techniques [61,66,78].
The ability to compensate for positive sagittal malalignment is different between obese and non-obese patients, with the obese population employing more lower extremity compensatory mechanisms as opposed to pelvic mechanisms [79]. Different compensatory mechanisms, in addition to various co-morbidities often associated with obesity, may be just some of the reasons the obese and non-obese populations have different responses to surgery, all factors the spine surgeon must be cognizant of. MIS (e.g., via tubular systems) or percutaneous techniques—by decreasing the amount of surgical incision, dead space, and potential paraspinal muscle damage via retraction—may decrease blood loss, accelerate post-operative recovery and mobilization, hospital stay, and overall perioperative morbidity [80–83]. As such, the authors propose that if spine surgery is indicated on an obese patient and bariatric surgery is not an option or has already been utilized, that anterior cervical or MIS/percutaneous approaches be employed when reasonable (Figure 4). Figure 5 summarizes the various ways to mitigate pre-operative, intra-operative, and post-operative challenges when caring for obese patients.
Figure 4.
Flow sheet depicting a general decision tree regarding an obese patient who presents with spine pathology.
Figure 5.
Maximizing surgical outcomes in obese patients: various ways to mitigate preoperative, intra-operative, and post-operative challenges.
Conclusions
Obese patients present several challenges to the spine surgeon. Certain precautions can be undertaken pre-operatively, intra-operatively, and post-operatively to mitigate the associated risks to and to optimize outcomes.
Acknowledgments
Research reported in this manuscript was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 2U54GM104942-02. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Leboeuf-Yde C, Kyvik KO, Bruun NH. Low back pain and lifestyle. Part II--Obesity. Information from a population-based sample of 29,424 twin subjects. Spine 1999;24:779–83; discussion 783–4. [DOI] [PubMed] [Google Scholar]
- [2].Hellsing A-L, Bryngelsson I-L. Predictors of Musculoskeletal Pain in Men. Spine 2000;25:3080–6. doi: 10.1097/00007632-200012010-00016. [DOI] [PubMed] [Google Scholar]
- [3].Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief 2015:1–8. doi: 10.1017/S1368980017000088. [DOI] [PubMed] [Google Scholar]
- [4].Jakoi AM, Pannu G, D’Oro A, Buser Z, Pham MH, Patel NN, et al. The clinical correlations between diabetes, cigarette smoking and obesity on intervertebral degenerative disc disease of the lumbar spine. Asian Spine Journal 2017;11:337–47. doi: 10.4184/asj.2017.11.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Epstein NE. More risks and complications for elective spine surgery in morbidly obese patients. Surgical Neurology International 2017;8:66. doi: 10.4103/sni.sni_49_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Marquez-Lara A, Nandyala S V., Sankaranarayanan S, Noureldin M, Singh K. Body Mass Index as a Predictor of Complications and Mortality After Lumbar Spine Surgery . Spine 2014;39:798–804. doi: 10.1097/BRS.0000000000000232. [DOI] [PubMed] [Google Scholar]
- [7].Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR, et al. Obesity and spine surgery: relation to perioperative complications. Journal of Neurosurgery: Spine 2007;6:291–7. doi: 10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- [8].Lingutla KK, Pollock R, Benomran E, Purushothaman B, Kasis A, Bhatia CK, et al. Outcome of lumbar spinal fusion surgery in obese patients: A systematic review and meta-Analysis. Bone and Joint Journal 2015;97-B:1395–404. doi: 10.1302/0301-620X.97B10.35724. [DOI] [PubMed] [Google Scholar]
- [9].Bono OJ, Poorman GW, Foster N, Jalai CM, Horn SR, Oren J, et al. Body mass index predicts risk of complications in lumbar spine surgery based on surgical invasiveness. Spine Journal 2018. doi: 10.1016/j.spinee.2017.11.015. [DOI] [PubMed] [Google Scholar]
- [10].Castle-Kirszbaum MD, Tee JW, Chan P, Hunn MK. Obesity in Neurosurgery: A Narrative Review of the Literature. World Neurosurgery 2017;106:790–805. doi: 10.1016/j.wneu.2017.06.049. [DOI] [PubMed] [Google Scholar]
- [11].Flippin M, Harris J, Paxton EW, Prentice HA, Fithian DC, Ward SR, et al. Effect of body mass index on patient outcomes of surgical intervention for the lumbar spine. Journal of Spine Surgery 2017;3:349–57. doi: 10.21037/jss.2017.06.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Puvanesarajah V, Werner BC, Cancienne JM, Jain A, Pehlivan H, Shimer AL, et al. Morbid Obesity and Lumbar Fusion in Patients Older Than 65 Years. Spine 2017;42:122–7. doi: 10.1097/BRS.0000000000001692. [DOI] [PubMed] [Google Scholar]
- [13].Buerba RA, Fu MC, Gruskay JA, Long WD, Grauer JN. Obese Class III patients at significantly greater risk of multiple complications after lumbar surgery: An analysis of 10,387 patients in the ACS NSQIP database. Spine Journal 2014;14:2008–18. doi: 10.1016/j.spinee.2013.11.047. [DOI] [PubMed] [Google Scholar]
- [14].Higgins DM, Mallory GW, Planchard RF, Puffer RC, Ali M, Gates MJ, et al. Understanding the Impact of Obesity on Short-term Outcomes and In-hospital Costs After Instrumented Spinal Fusion. Neurosurgery 2016;78:127–32. doi: 10.1227/NEU.0000000000001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Burks CA, Werner BC, Yang S, Shimer AL. Obesity Is Associated With an Increased Rate of Incidental Durotomy in Lumbar Spine Surgery. Spine 2015;40:500–4. doi: 10.1097/BRS.0000000000000784. [DOI] [PubMed] [Google Scholar]
- [16].Phan K, Lee NJ, Kothari P, Kim JS, Cho SK. Risk Factors for Readmissions Following Anterior Lumbar Interbody Fusion. Spine 2016:5–30. doi: 10.1097/BRS.0000000000001677. [DOI] [PubMed] [Google Scholar]
- [17].Phan K, Kothari P, Lee NJ, Virk S, Kim JS, Cho SK. Impact of Obesity on Outcomes in Adults Undergoing Elective Posterior Cervical Fusion. Spine 2017;42:261–6. doi: 10.1097/BRS.0000000000001711. [DOI] [PubMed] [Google Scholar]
- [18].McGuire KJ, Khaleel MA, Rihn JA, Zhao W, Weinstein JN, Israel B, et al. The Effect of High Obesity on Outcomes of Treatment for Lumbar Spinal Conditions. Spine 2014;39:1975–80. doi: 10.1097/BRS.0000000000000577.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Olsen M a, Mayfield J, Lauryssen C, Polish LB, Jones M, Vest J, et al. Risk factors for surgical site infection in spinal surgery. Journal of Neurosurgery: Spine 2003;98:149–55. doi: 10.3171/spi.2003.98.2.0149. [DOI] [PubMed] [Google Scholar]
- [20].De la Garza Ramos R, Nakhla J, Nasser R, Schulz JF, Purvis TE, Sciubba DM, et al. Effect of body mass index on surgical outcomes after posterior spinal fusion for adolescent idiopathic scoliosis. Neurosurgical Focus 2017;43:E5. doi: 10.3171/2017.7.FOCUS17342. [DOI] [PubMed] [Google Scholar]
- [21].Amin RM, Raad M, Jain A, Sandhu KP, Frank SM, Kebaish KM. Increasing Body Mass Index is Associated with Worse Perioperative Outcomes and Higher Costs in Adult Spinal Deformity Surgery. Spine 2017:1. doi: 10.1097/BRS.0000000000002407. [DOI] [PubMed] [Google Scholar]
- [22].Green BN, Johnson CD, Haldeman S, Griffith E, Clay MB, Kane EJ, et al. A scoping review of biopsychosocial risk factors and co-morbidities for common spinal disorders. Plos One 2018;13:e0197987. doi: 10.1371/journal.pone.0197987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Rihn JA, Radcliff K, Hilibrand AS, Anderson DT, Zhao W, Lurie J, et al. Does obesity affect outcomes of treatment forfor lumbar stenosis Spine (Phila Pa 1976) Author Manuscript. Author manuscript; available in PMC 2013 November 01.. 2012 November 1; 37(23): 1933–1946. doi: 10.1097/BRS.0b013e31825e21b2. and degenerative spond 2013;37:1933–46. doi:10.1097/BRS.0b013e31825e21b2.Does. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Eleswarapu AS, Divi SN, Dirschl DR, Mok JM, Stout C, Lee MJ. How effective is physical therapy for common low back pain diagnoses? Spine 2016;41:1325–9. doi: 10.1097/BRS.0000000000001506. [DOI] [PubMed] [Google Scholar]
- [25].Manchikanti L, Buenaventura RM, Manchikanti KN, Ruan X, Gupta S, Smith HS, et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician 2012;15:E199–245. [PubMed] [Google Scholar]
- [26].Cushman D, Mattie R, Curtis B, Flis A, McCormick ZL. The effect of body mass index on fluoroscopic time and radiation dose during lumbar transforaminal epidural steroid injections. Spine Journal 2016;16:876–83. doi: 10.1016/j.spinee.2016.03.041. [DOI] [PubMed] [Google Scholar]
- [27].Khoueir P, Black MH, Crookes PF, Kaufman HS, Katkhouda N, Wang MY. Prospective assessment of axial back pain symptoms before and after bariatric weight reduction surgery. Spine Journal 2009;9:454–63. doi: 10.1016/j.spinee.2009.02.003. [DOI] [PubMed] [Google Scholar]
- [28].Lidar Z, Behrbalk E, Regev GJ, Salame K, Keynan O, Schweiger C, et al. Intervertebral disc height changes after weight reduction in morbidly obese patients and its effect on quality of life and radicular and low back pain. Spine 2012;37:1947–52. doi: 10.1097/BRS.0b013e31825fab16. [DOI] [PubMed] [Google Scholar]
- [29].Takenaka S, Mukai Y, Hosono N, Kaito T. Improvement of thoracic myelopathy following bariatric surgery in an obese patient 2018:10–3. doi: 10.1136/bcr-2017-223629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Jain D, Berven SH, Carter J, Zhang AL, Deviren V. Bariatric surgery before elective posterior lumbar fusion is associated with reduced medical complications and infection. Spine Journal 2018. doi: 10.1016/j.spinee.2018.01.023. [DOI] [PubMed] [Google Scholar]
- [31].Shanbhogue V V, Støving RK, Frederiksen KH, Hanson S, Brixen K, Gram J, et al. Bone structural changes after gastric bypass surgery evaluated by HR-pQCT: A two-year longitudinal study. European Journal of Endocrinology 2017;176:685–93. doi: 10.1530/EJE-17-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Epstein N Bariatric bypasses contribute to loss of bone mineral density but reduce axial back pain in morbidly obese patients considering spine surgery. Surgical Neurology International 2017;8:13. doi: 10.4103/2152-7806.198740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Shaw K, Chen J, Sheppard W, Alazzeh M, Park H, Park D, et al. Use of the subcutaneous lumbar spine (SLS) index as a predictor for surgical complications in lumbar spine surgery. The Spine Journal 2018. doi: 10.1016/j.spinee.2018.04.018. [DOI] [PubMed] [Google Scholar]
- [34].Rosenfeld HE, Limb R, Chan P, Fitzgerald M, Bradley WPL, Rosenfeld JV. Challenges in the surgical management of spine trauma in the morbidly obese patient: A case series. Journal of Neurosurgery: Spine 2013;19:101–9. doi: 10.3171/2013.4.SPINE12876. [DOI] [PubMed] [Google Scholar]
- [35].Lombardi R, Stephenson J. Bariatric patients and aeromedical retrieval. Journal of the Australian Society of Aerospace Medicine 2012;7:22–5. [Google Scholar]
- [36].Le NTT, Robinson J, Lewis SJ. Obese patients and radiography literature: What do we know about a big issue? Journal of Medical Radiation Sciences 2015;62:132–41. doi: 10.1002/jmrs.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Spitler CA, Hulick RM, Graves ML, Russell G V., Bergin PF. Obesity in the Polytrauma Patient. Orthopedic Clinics of North America 2018;49:307–15. doi: 10.1016/j.ocl.2018.02.004. [DOI] [PubMed] [Google Scholar]
- [38].Baxi V, Budhakar S. Anesthesia management of a morbidly obese patient in prone position for lumbar spine surgery. Journal of Craniovertebral Junction and Spine 2010;1:55–7. doi: 10.4103/0974-8237.65483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Douglass J, Fraser J, Andrzejowski J. Awake intubation and awake prone positioning of a morbidly obese patient for lumbar spine surgery. Anaesthesia 2014;69:166–9. doi: 10.1111/anae.12387. [DOI] [PubMed] [Google Scholar]
- [40].Cao J, Kong L, Meng F, Zhang Y, Shen Y. Impact of obesity on lumbar spinal surgery outcomes. Journal of Clinical Neuroscience 2016;28:1–6. doi: 10.1016/j.jocn.2015.10.034. [DOI] [PubMed] [Google Scholar]
- [41].Onyekwelu I, Glassman SD, Asher AL, Shaffrey CI, Mummaneni P V., Carreon LY. Impact of obesity on complications and outcomes: a comparison of fusion and nonfusion lumbar spine surgery. Journal of Neurosurgery: Spine 2016;26:[Epub ahead of print]. doi: 10.3171/2016.7.SPINE16448. [DOI] [PubMed] [Google Scholar]
- [42].Shamji MF, Parker S, Cook C, Pietrobon R, Brown C, Isaacs RE. Impact of body habitus on perioperative morbidity associated with fusion of the thoracolumbar and lumbar spine. Neurosurgery 2009;65:490–8. doi: 10.1227/01.NEU.0000350863.69524.8E. [DOI] [PubMed] [Google Scholar]
- [43].Zhang Y, Liu H, He F, Chen A, Yang H, Pi B. Does Tranexamic Acid Improve Bleeding, Transfusion, and Hemoglobin Level in Patients Undergoing Multilevel Spine Surgery? A Systematic Review and Meta-Analysis. World Neurosurgery 2019;127:289–301. doi: 10.1016/j.wneu.2019.02.170. [DOI] [PubMed] [Google Scholar]
- [44].Cheriyan T, Maier SP, Bianco K, Slobodyanyuk K, Rattenni RN, Lafage V, et al. Efficacy of tranexamic acid on surgical bleeding in spine surgery: A meta-analysis. Spine Journal 2015;15:752–61. doi: 10.1016/j.spinee.2015.01.013. [DOI] [PubMed] [Google Scholar]
- [45].Kim DH, Zaremski J, Kwon B, Jenis L, Woodard E, Bode R, et al. Risk factors for false positive transcranial motor evoked potential monitoring alerts during surgical treatment of cervical myelopathy. Spine 2007;32:3041–6. doi: 10.1097/BRS.0b013e31815d0072. [DOI] [PubMed] [Google Scholar]
- [46].Khan NR, Thompson CJ, DeCuypere M, Angotti JM, Kalobwe E, Muhlbauer MS, et al. A meta-analysis of spinal surgical site infection and vancomycin powder. Journal of Neurosurgery Spine 2014;21:1–10. doi: 10.3171/2014.8.SPINE1445. [DOI] [PubMed] [Google Scholar]
- [47].Kang DG, Holekamp TF, Wagner SC, Lehman RA. Intrasite vancomycin powder for the prevention of surgical site infection in spine surgery : a systematic literature review. The Spine Journal 2019;15:762–70. doi: 10.1016/j.spinee.2015.01.030. [DOI] [PubMed] [Google Scholar]
- [48].Bakhsheshian J, Dahdaleh NS, Lam SK, Savage JW, Smith ZA. The Use of Vancomycin Powder In Modern Spine Surgery : Systematic Review and Meta-Analysis of the Clinical Evidence. World Neurosurgery 2014;83:816–23. doi: 10.1016/j.wneu.2014.12.033. [DOI] [PubMed] [Google Scholar]
- [49].Gande A, Rosinski A, Cunningham T, Bhatia N, Lee Y. Selection pressures of vancomycin powder use in spine surgery : a meta-analysis. The Spine Journal 2019;19:1076–84. doi: 10.1016/j.spinee.2019.01.002. [DOI] [PubMed] [Google Scholar]
- [50].Devin CJ, Chotai S, McGirt MJ, Vaccaro AR, Youssef JA, Orndorff DG, et al. Intrawound Vancomycin Decreases the Risk of Surgical Site Infection After Posterior Spine Surgery: A Multicenter Analysis. Spine 2018;43:65–71. doi: 10.1097/BRS.0000000000001371. [DOI] [PubMed] [Google Scholar]
- [51].Yamada K, Abe H, Higashikawa A, Tonosu J, Kuniya T, Nakajima K, et al. Evidence-based care bundles for preventing surgical site infections in spinal instrumentation surgery. Spine 2018;43:1765–73. doi: 10.1097/BRS.0000000000002709. [DOI] [PubMed] [Google Scholar]
- [52].Andrew Glennie R, Dea N, Street JT. Dressings and drains in posterior spine surgery and their effect on wound complications. Journal of Clinical Neuroscience 2015;22:1081–7. doi: 10.1016/j.jocn.2015.01.009. [DOI] [PubMed] [Google Scholar]
- [53].Yao R, Tan T, Tee JW, Street J. Prophylaxis of surgical site infection in adult spine surgery: A systematic review. Journal of Clinical Neuroscience 2018;52:5–25. doi: 10.1016/j.jocn.2018.03.023. [DOI] [PubMed] [Google Scholar]
- [54].Hudson MA. Texas passes first law for safe patient handling in America: landmark legislation protects health-care workers and patients from injury related to manual patient lifting. Journal of Long-Term Effects of Medical Implants 2005;15:559–66. [DOI] [PubMed] [Google Scholar]
- [55].Emery SE, Daffner SD, France JC, Ellison M, Grose BW, Hobbs GR, et al. Effect of head position on intraocular pressure during lumbar spine fusion. Journal of Bone and Joint Surgery - American Volume 2014;97:1817–23. doi: 10.2106/JBJS.O.00091. [DOI] [PubMed] [Google Scholar]
- [56].Phan K, Rogers P, Rao PJ, Mobbs RJ. Influence of obesity on complications, clinical outcome and subsidence following anterior lumbar interbody fusion (ALIF): prospective observational study. World Neurosurgery 2017;107:334–41. doi: 10.1016/j.wneu.2017.08.014. [DOI] [PubMed] [Google Scholar]
- [57].Lucas F, Emery E, Dudoit T, Berger L. Influence of Obesity on Access-Related Complications During Anterior Lumbar Spine Interbody Fusion. World Neurosurgery 2016;92:229–33. doi: 10.1016/j.wneu.2015.12.104. [DOI] [PubMed] [Google Scholar]
- [58].Peng CWB, Bendo JA, Goldstein JA, Nalbandian MM. Perioperative outcomes of anterior lumbar surgery in obese versus non-obese patients. Spine Journal 2009;9:715–20. doi: 10.1016/j.spinee.2009.04.023. [DOI] [PubMed] [Google Scholar]
- [59].IV JC, Jackson T. Minimally invasive lumbar discectomy in obese patients. Neurosurgery 2007;61:539–44. doi: 10.1227/01.NEU.0000280020.84758.E7. [DOI] [PubMed] [Google Scholar]
- [60].Kapetanakis S, Gkantsinikoudis N, Chaniotakis C, Charitoudis G, Givissis P. Percutaneous Transforaminal Endoscopic Discectomy for the Treatment of Lumbar Disc Herniation in Obese Patients: Health-Related Quality of Life Assessment in a 2-Year Follow-Up. World Neurosurgery 2018;113:e638–49. doi: 10.1016/j.wneu.2018.02.112. [DOI] [PubMed] [Google Scholar]
- [61].Wang T, Han C, Jiang H, Tian P. The Effect of Obesity on Clinical Outcomes After Minimally Invasive Surgery of the Spine: A Systematic Review and Meta-Analysis. World Neurosurgery 2018;110:e438–49. doi: 10.1016/j.wneu.2017.11.010. [DOI] [PubMed] [Google Scholar]
- [62].Bohl DD, Ahn J, Mayo BC, Massel DH, Tabaraee E, Sershon RA, et al. Does greater body mass index increase the risk for revision procedures following a single-level minimally invasive lumbar discectomy? Spine 2016;41:816–21. doi: 10.1097/BRS.0000000000001340. [DOI] [PubMed] [Google Scholar]
- [63].Tomasino A, Parikh K, Steinberger J, Knopman J, Boockvar J, Härtl R. Tubular microsurgery for lumbar discectomies and laminectomies in obese patients: Operative results and outcome. Spine 2009;34:664–72. doi: 10.1097/BRS.0b013e3181b0b63d. [DOI] [PubMed] [Google Scholar]
- [64].Adogwa O, Carr K, Thompson P, Hoang K, Darlington T, Perez E, et al. A prospective, multi-institutional comparative effectiveness study of lumbar spine surgery in morbidly obese patients: Does minimally invasive transforaminal lumbar interbody fusion result in superior outcomes? World Neurosurgery 2015;83:860–6. doi: 10.1016/j.wneu.2014.12.034. [DOI] [PubMed] [Google Scholar]
- [65].Lau D, Ziewacz J, Park P. Minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis in patients with significant obesity. Journal of Clinical Neuroscience 2013;20:80–3. doi: 10.1016/j.jocn.2012.07.004. [DOI] [PubMed] [Google Scholar]
- [66].Park P, Upadhyaya C, Garton HJFK. the Impact of Minimally Invasive Spine Surgery on Perioperative Complications in Overweight or Obese Patients. Neurosurgery 2008. March;62(3):693–9; Discussion 693–9 2008;62:693–9. doi: 10.1227/01.NEU.0000297115.62323.CE. [DOI] [PubMed] [Google Scholar]
- [67].Bae JS, Lee S-H. Transforaminal full-endoscopic lumbar discectomy in obese patients. International Journal of Spine Surgery 2016. doi: 10.14444/3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Walden CM, Bankard SB, Cayer B, Floyd WB, Garrison HG, Hickey T, et al. Mobilization of the obese patient and prevention of injury. Annals of Surgery 2013;258:646–50; discussion 650–1. doi: 10.1097/SLA.0b013e3182a5039f. [DOI] [PubMed] [Google Scholar]
- [69].Giannadakis C, Nerland US, Solheim O, Jakola AS, Gulati M, Weber C, et al. Does Obesity Affect Outcomes after Decompressive Surgery for Lumbar Spinal Stenosis? A Multicenter, Observational, Registry-Based Study. World Neurosurgery 2015;84:1227–34. doi: 10.1016/j.wneu.2015.06.020. [DOI] [PubMed] [Google Scholar]
- [70].Elsayed G, Davis MC, Dupépé EC, McClugage SG, Szerlip P, Walters BC, et al. Obese (Body Mass Index >30) Patients Have Greater Functional Improvement and Reach Equivalent Outcomes at 12 Months Following Decompression Surgery for Symptomatic Lumbar Stenosis. World Neurosurgery 2017;105:884–94. doi: 10.1016/j.wneu.2017.06.072. [DOI] [PubMed] [Google Scholar]
- [71].Wilson JR, Tetreault LA, Schroeder G, Harrop JS, Prasad S, Vaccaro A, et al. Impact of Elevated Body Mass Index and Obesity on Long-term Surgical Outcomes for Patients With Degenerative Cervical Myelopathy. Spine 2017;42:195–201. doi: 10.1097/BRS.0000000000001859. [DOI] [PubMed] [Google Scholar]
- [72].Joseph JR, Farooqui Z, Smith BW, Kahn EN, Liu X, La Marca F, et al. Does clinical improvement of symptomatic degenerative lumbar disease impact obesity? Journal of Neurosurgery: Spine 2017;26:705–8. doi: 10.3171/2016.11.SPINE16973. [DOI] [PubMed] [Google Scholar]
- [73].Akins PT, Inacio MCS, Bernbeck JA, Harris J, Chen YX, Prentice HA, et al. Do obese and extremely obese patients lose weight after lumbar spine fusions? Analysis of a cohort of 7303 patients from the kaiser national spine registry. Spine 2018;43:22–7. doi: 10.1097/BRS.0000000000002456. [DOI] [PubMed] [Google Scholar]
- [74].Pereira BJA, De Holanda CVM, Ribeiro CAA, De Moura SM, De Carvalho Galv??o PE, Quidute BSQ, et al. Impact of body mass index in spinal surgery for degenerative lumbar spine disease. Clinical Neurology and Neurosurgery 2014;127:112–5. doi: 10.1016/j.clineuro.2014.09.016. [DOI] [PubMed] [Google Scholar]
- [75].Buerba R a, Fu MC, Grauer JN. Anterior and posterior cervical fusion in patients with high body mass index are not associated with greater complications. The Spine Journal : Official Journal of the North American Spine Society 2014;14:1643–53. doi: 10.1016/j.spinee.2013.09.054. [DOI] [PubMed] [Google Scholar]
- [76].Narain AS, Hijji FY, Haws BE, Kudaravalli KT, Yom KH, Markowitz J, et al. Impact of body mass index on surgical outcomes, narcotics consumption, and hospital costs following anterior cervical discectomy and fusion. Journal of Neurosurgery: Spine 2018;28:160–6. doi: 10.3171/2017.6.SPINE17288. [DOI] [PubMed] [Google Scholar]
- [77].Chotai S, Sielatycki JA, Parker SL, Sivaganesan A, Kay HL, Stonko DP, et al. Effect of obesity on cost per quality-adjusted life years gained following anterior cervical discectomy and fusion in elective degenerative pathology. Spine Journal 2016;16:1342–50. doi: 10.1016/j.spinee.2016.06.023. [DOI] [PubMed] [Google Scholar]
- [78].Senker W, Stefanits H, Gmeiner M, Trutschnig W, Weinfurter I, Gruber A. Does Obesity Affect Perioperative and Postoperative Morbidity and Complication Rates After Minimal Access Spinal Technologies in Surgery for Lumbar Degenerative Disc Disease. World Neurosurgery 2018;111:e374–85. doi: 10.1016/j.wneu.2017.12.075. [DOI] [PubMed] [Google Scholar]
- [79].Jalai CM, Diebo BG, Cruz DL, Poorman GW, Vira S, Buckland AJ, et al. The impact of obesity on compensatory mechanisms in response to progressive sagittal malalignment. Spine Journal 2017;17:681–8. doi: 10.1016/j.spinee.2016.11.016. [DOI] [PubMed] [Google Scholar]
- [80].Stevens KJ, Spenciner DB, Griffiths KL, Kim KD, Zwienenberg-Lee M, Alamin T, et al. Comparison of minimally invasive and conventional open posterolateral lumbar fusion using magnetic resonance imaging and retraction pressure studies. Journal of Spinal Disorders & Techniques 2006;19:77–86. doi: 10.1097/01.bsd.0000193820.42522.d9. [DOI] [PubMed] [Google Scholar]
- [81].Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine 2007;32:537–43. doi: 10.1097/01.brs.0000256473.49791.f4. [DOI] [PubMed] [Google Scholar]
- [82].Ntoukas V, Muller A. Minimally invasive approach versus traditional open approach for one level posterior lumbar interbody fusion. Minimally Invasive Neurosurgery : MIN 2010;53:21–4. doi: 10.1055/s-0030-1247560. [DOI] [PubMed] [Google Scholar]
- [83].Scheufler K-M, Dohmen H, Vougioukas VI. Percutaneous Transforaminal Lumbar Interbody Fusion for the Treatment of Degenerative Lumbar Instability. Operative Neurosurgery 2007;60:203–13. doi: 10.1227/01.NEU.0000255388.03088.B7. [DOI] [PubMed] [Google Scholar]