Abstract
Tuberculous granuloma in the middle ear is an unusual entity. Herein, we report a case with short presentation of otitis media with mastoid abscess but with a CT scan showing widespread bone destruction. The cause was determined to be middle ear tuberculosis. Awareness of this entity is important, as it may cause a delay in referral to an otorhinolaryngology specialist and, subsequently, a delay in initiating treatment. Therefore, it should be considered in the differential diagnosis, especially when the usual treatment fails to produce the desired result.
Keywords: Cholesteatoma, Middle ear tuberculosis, Granuloma, Otitis media
Introduction
Otorrhea with mastoid abscess is commonly associated with pathology in the middle ear. The accompanying presentations may include hearing impairment, a recent history of ear infection, or the presence of granulation tissue from the middle ear that can be visible from the ear canal. The progression of the disease can lead to more devastating conditions, such as destruction of the middle ear conductive apparatus, facial paralysis, cochlear involvement with labyrinthitis, and intracranial dissemination of infection. However, failure of the standard treatment for acute otitis media should raise some suspicion of middle ear tuberculosis (TB) as a differential diagnosis. Tuberculosis is a puzzling infectious disease which may remain undiagnosed or cause confusion with other middle ear conditions like acute otitis media or even chronic otitis media with or without cholesteatoma. An atypical aggressive infection warrants further investigations for definitive diagnosis and treatment.
Case report
A 17-year-old man presented with a non-foul-smelling, yellowish discharge and post-auricular swelling of the right ear for two weeks. It was associated with otalgia, reduced hearing, and nocturnal fever. He had visited a private general practitioner and had completed one course of oral antibiotics prior to presentation at our clinic. However, his condition remained unresolved. There was no history of prolonged cough or loss of appetite or weight. He denied any history of night sweats or contact with a TB patient.
On examination, the vital signs were normal. There was a 7 x 4 cm fluctuant, soft, and tender swelling with no sinus or punctum pushing the right pinna antero-inferiorly. Otoscopic examination of the right ear showed posterior sagging of the canal with granulation tissue deep to it. The tympanic membrane was not visualized. The left ear examination was normal. A tuning fork test revealed negative Rinne on the right side while positive on the left. A Weber test was lateralized to the right, indicating right conductive hearing loss. The facial nerve was intact bilaterally and there were no signs of intracranial complications. There were no palpable lymph nodes.
A blood test showed high erythrocyte rate (80 mm/h). However, tuberculosis screening was unremarkable. He tested negative for hepatitis B and C as well as HIV. Chest x-ray was normal. Pure Tone Audiometry (PTA) showed severe to profound mixed hearing loss of the right ear with normal hearing on the left. Patient was started on intravenous ciprofloxacin and incision and drainage drained 8 ml of pus. Nevertheless, the culture came back as no growth.
The high-resolution CT scan (HRCT) revealed non-enhancing soft tissue density inside the external auditory canal, mesotympanum, and mastoid cavity on the right. There was erosion of the ossicles, the posterior, superior, and inferior walls of the auditory canal, and the mastoid bone (Fig. 1a). Otherwise, the cochlear and semicircular canals were intact. The proximal part of the tympanic segment and the anterior genu of the facial nerve were obliterated. There was a thinning of the bony area of the right tegmen tympani (Fig. 1b).
Fig. 1a (Left): Axial view of the HRCT of the temporal bone showing non-enhancing soft tissue density mass and bony erosions in the right temporal bone.
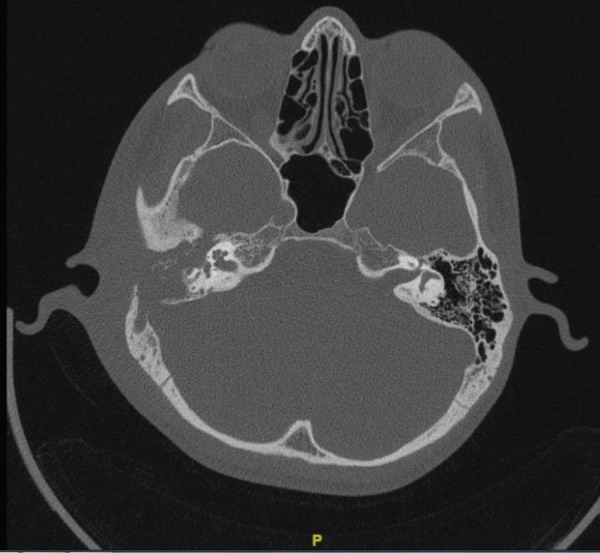
Fig. 1b (Right): Axial view of the HRCT of the temporal bone showing non-enhancing soft tissue density mass and bony erosions in the right temporal bone.
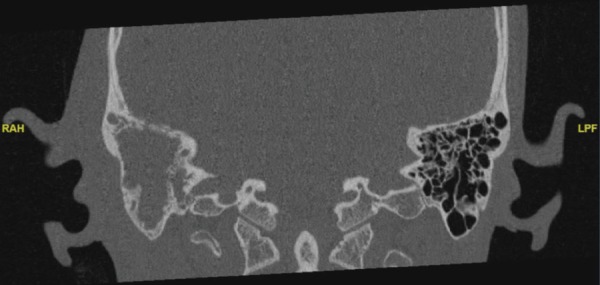
The left temporal bone structures were normal. The impressions from the radiological findings were in keeping with right cholesteatoma.
Right-modified radical mastoidectomy was carried out a week later as the patient did not respond well with the antibiotic. Intraoperatively, the right tegmen tympani and the right sigmoid sinus as well as the ossicles and the posterior wall of external auditory canal were noted to be eroded. Pus was sent for culture, sensitivity, and acid-fast bacilli (AFB) tests. The soft tissue from the mesotympanum was sent for histopathological examination (HPE).
The patient was discharged well on day two after the operation. Subsequently, the HPE was reported as tuberculous granuloma. However, the AFB test was negative. The patient was then treated as having extra-pulmonary TB with the regime of ethambutol, isoniazid, rifampicin, and pyrazinamide for nine months. The patient was seen well with no ear discharge during his follow-up at 8 months after completing the TB treatment.
Discussion
Otorrhea is a common presentation to the otorhinolaryngology clinic. Diagnosis of otorrhea with mastoid abscess is mostly limited to acute otitis media or chronic otitis media with or without cholesteatoma. The combination of microbiological, histopathological, and radiological findings guided by a thorough history and physical examination is important for achieving an accurate diagnosis.
Tuberculous otitis media is not a common disease, especially in an immunocompetent person. It is even rarer to occur as a primary infection. The findings of soft tissue density in the middle ear with extensive bony erosion on HRCT of the temporal bone of our patient was suggestive of cholesteatoma, but the short history of ear symptoms causing complications is not its typical presentation. Similar aggressiveness of the disease has also been reported in a few case reports.1,2 Cavallin and Munoz suggested diagnosis of tuberculous otomastoiditis when there is CT evidence of widespread bone destruction without clinical signs of aggressive infection.1
In our case, the AFB smear was negative for Mycobacterium tuberculosis (MTB). Garg et al. reported a very low sensitivity of MTB detected from pus AFB as compared to realtime polymerase chain reaction (RT-PCR).3 They have found that RT-PCR detected MTB in 28.6% of the cases with a negative AFB smear.
The diagnosis of tuberculosis in our case was made based on the histology report. In the same manner, Maniu et al. reported three cases of tympanomastoidectomy done under the suspicion of otitis media with cholesteatoma that were proven to be granulomatous lesions based on microscopic examination of the affected tissue.4 The common features in their report were the presence of severe granulation tissue filling the mastoid cavity and middle ear during surgery in the absence of cholesteatoma.
Primary tuberculosis of the middle ear is rarely encountered. In the literature, there are a few articles that report on this condition.5,6 The condition should be suspected when the usual treatment fails to produce the desired result. Histopathological assessment is always a crucial step for an accurate diagnosis in addition to microbiological and radiological assessments.
Conclusion
Middle ear tuberculosis should be considered in a patient who presents with otorrhea accompanied by an atypical aggressive infection. Histopathological examination is critical in accurately diagnosing this condition.
References
- 1.Cavallin L, Muren C. CT findings in tuberculous mastoiditis. A case report. Acta Radiol. 2000;41:49–51. [PubMed] [Google Scholar]
- 2.Munoz A, Ruiz-Contreras J, Jimenez A, Mate I, Calvo M, Villafruela M, et al. Bilateral tuberculous otomastoiditis in an immunocompetent 5-year old child: CT and MRI findings. Eur Radiol. 2009;19:1560–3. doi: 10.1007/s00330-008-1130-7. [DOI] [PubMed] [Google Scholar]
- 3.Garg P, Garg MK, Agarwal N. Comparison of histopathology, acid fast bacillus smear and real-time polymerase chain reaction for detection of Mycobacterium tuberculosis in anal fistula in 161 patients: A prospective controlled trial. Int J Mycobacteriol. 2016;5(Suppl 1):S208–9. doi: 10.1016/j.ijmyco.2016.09.055. [DOI] [PubMed] [Google Scholar]
- 4.Maniu AA, Harabagiu O, Damian LO, et al. Mastoiditis and facial paralysis as initial manifestations of temporal bone systemic diseases - the significance of the histopathological examination. Rom J Morphol Embryol. 2016;57:243–8. [PubMed] [Google Scholar]
- 5.Araujo MF, Pinheiro TG, Raymundo IT, et al. Tuberculous otitis media. J Int Adv Otol. 2011;7:413–7. [Google Scholar]
- 6.Bruschini L, Ciabotti A, Berrettini S. Chronic tuberculosis otomastoiditis: A case report. J Int Adv Otol. 2016;12:219–21. doi: 10.5152/iao.2016.2097. [DOI] [PubMed] [Google Scholar]


