Abstract
Introduction : Atopic eczema (AE) is a common inflammatory skin dermatosis that is increasing in prevalence. However, it can present in various clinical presentations, which leads to challenges in the diagnosis and treatment of the condition, especially in a primary care setting. The Clinical Practice Guidelines on the Management of Atopic Eczema was developed by a multidisciplinary development group and approved by the Ministry of Health Malaysia in 2018. It covers the aspects of diagnosis, severity assessment, treatment, and referral.
Keywords: atopic eczema, diagnosis, assessment, treatment, education
Introduction
Atopic eczema (AE) or atopic dermatitis is a complex, chronic, and recurrent inflammatory itchy skin disorder. In the majority of cases, it starts to develop in early childhood and may persist into adulthood. The prevalence is as high as 20% in some countries. In Malaysia, the prevalence has increased from 9.5% in 1995 to 12.6% in 2003. AE has various clinical manifestations in different age groups. This makes the diagnosis a challenge, leading to misdiagnosis and mistreatment. Therefore, it is paramount to have evidence-based clinical practice guidelines (CPG) for effective and safe management.
Clinical Presentation
AE has both acute and chronic clinical presentations. Acute eczema is characterized by papulovesicular eruption with erythema, weeping, edema, and excoriation, whereas chronic eczema is characterized by lichenification and dry skin (xerosis).
Diagnosis
AE is diagnosed clinically and not by any specific laboratory investigation. The following criteria is used for the diagnosis of AE.
The U.K. Working Party's Diagnostic Criteria for Atopic Dermatitis.
Patient must have an itchy skin condition (or parental report of scratching or rubbing in a child) plus 3 or more of the following:
history of involvement of the skin creases such as folds of elbows, behind the knees, fronts of ankles, or around the neck (including cheeks in children under 10)
a personal history of asthma or hay fever (or history of atopic disease in a first-degree relative in children under 4)
a history of generally dry skin in the last year
visible flexural eczema (or eczema involving the cheeks/forehead and outer limbs in children under 4)
onset under the age of 2 (not used if child is under 4)
Severity Assessment
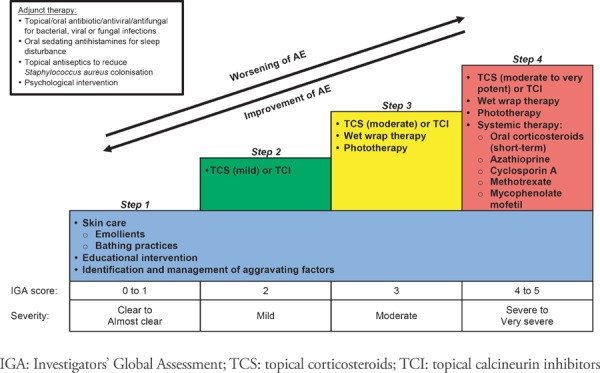
Assessment of disease severity and quality of life should be used in the management of atopic eczema. The preferred tools are the following:
Investigator's Global Assessment (IGA)
Dermatology Life Quality Index/Children's Dermatology Life Quality Index (DLQI/CDLQI)
Investigator's Global Assessment (IGA).
| Score | Description |
|---|---|
| 0 = Clear | No inflammatory signs of AD |
| 1 = Almost clear | Just-perceptible erythema and just-perceptible papulation/infiltration |
| 2 = Mild disease | Mild erythema and mild papulation/infiltration |
| 3 = Moderate disease | Moderate erythema and moderate papulation/infiltration |
| 4 = Severe disease | Severe erythema and severe papulation/infiltration |
| 5 = Very severe disease | Severe erythema and severe papulation/infiltration with oozing/crusting |
Aggravating/Triggering Factors
Various factors may worsen AE, which include the following:
aeroallergen (e.g., house dust mites, animal's dander)
physical irritants (e.g., nylon, wool, detergents, sweat)
environmental factors (e.g., extreme temperature)
microbial colonization/infection (e.g., Staphylococcus aureus)
patient factors (e.g., pregnancy, stress)
food
The influence of food allergy on the clinical course of AE remains unclear. Food may worsen AE in children less than two years old, especially milk, eggs, and peanuts. In the prevention of AE, hydrolyzed formulas should not be offered to infants in preference to breast milk.
Topical Therapy
Topical therapy is the mainstay of treatment in AE. This includes emollients, topical antiinflammatory agents, and topical antiseptic/antimicrobial agents.
Emollient/moisturizer
Emollient therapy is the mainstay of management in AE in all age groups of patients and in all stages of the disease, from mild to severe. It improves the epidermal barrier function and dryness, leading to a reduction in pruritus. Its application decreases the usage of topical corticosteroids.
Emollients are available in different formulations (ointments, creams, lotions, gels, and aerosol sprays). Ointments (e.g., petrolatum) are greasy in nature, whereas creams and lotions contain water and are more user-friendly and acceptable cosmetically. Creams (e.g., aqueous cream and urea cream), lotions, and gels contain preservatives to protect against microbial growth in the presence of water. There is no reliable evidence to show that one emollient is more effective than another. Generally, emollients are safe to be used in AE.
In infants with first-degree relatives with atopy, daily use of an emollient significantly reduces the risk of developing AE.
Topical corticosteroids
Topical corticosteroids (TCS) are the first-line anti-inflammatory agents for AE in both children and adults. They should be used to treat flares in AE. The choice of TCS depends on the following factors:
age of the patient
site of skin lesions
chronicity of skin lesions
severity of skin inflammation
The use of TCS should be monitored every 3–6 months to determine response and potential side effects.
TCS are categorised into four classes according to their potencies:
Class I (very potent; clobetasol propionate 0.05% cream/ointment)
Class II (potent; betamethasone valerate 0.1% cream/ointment, mometasone furoate 0.1% cream/ointment, fluticasone propionate 0.05% cream)
Class III (moderate; clobetasone butyrate 0.05% cream/ointment)
Class IV (mild; hydrocortisone acetate 1% cream/ointment)
Practical guides for TCS application are the following:
TCS should be used concomitantly with emollients.
Fingertip unit can be used as a guide to the amount of TCS required for affected sites.
Choice of vehicle of TCS depends on the affected sites (i.e., gel for scalp; cream for face, genital and flexural areas; ointment for palm and sole).
Choice of potency of TCS depends on the clinical severity of eczema (i.e., potent to very potent TCS ointment for thick lesions and mild to moderate TCS cream for thin lesions).
After resolution of eczema flares, discontinuation of TCS application should be done gradually to avoid rebound (i.e., twice a day followed by once a day, then 1–3 times a week before complete discontinuation).
After resolution of eczema flares, proactive therapy (mild TCS application intermittently once or twice a week) can be used to maintain remission.
Topical calcineurin inhibitors
Topical calcineurin inhibitors (TCIs), e.g., tacrolimus and pimecrolimus, are non-steroidal immune-modulating agents and may be considered for treatment of flares in AE. They are licensed for the treatment of children older than two years of age.
Systemic Therapy
Systemic therapy includes adjunctive treatment (e.g., antihistamines and systemic antibiotics) and specific treatment of AE (e.g., immunomodulating agent and biologics). Specific systemic treatments should be used only in severe cases of AE in patients where other management options have failed or are not appropriate and where AE has a significant impact on quality of life.
Antihistamines
Itch is a common symptom in AE, and sedating antihistamines may be considered as a short-term measure at bedtime in AE patients with sleep disturbance. The medication should not be used as a monotherapy or as a substitute topical therapy in AE.
Immunomodulating agents
Corticosteroids, cyclosporin A, methotrexate, azathioprine, mycophenolate mofetil, intravenous immunoglobulin, and interferon gamma are some of the immunomodulating agents used in AE. These agents are used in moderate to severe AE which are uncontrolled after optimization of topical treatment and/or phototherapy. They are also considered in chronic AE where quality of life is substantially impacted. A referral to a dermatologist should be considered when patients require immunomodulating agents.
Antimicrobials
Routine use of topical and systemic antimicrobials among patients with non-infected AE is not recommended. They may be considered when there is clinical evidence of infection.
Antiseptics at appropriate dilutions, e.g., potassium permanganate, triclosan, or chlorhexidine, may be used as an adjunct therapy to decrease bacterial load in patients who have recurrent infected AE.
In a local setting, short-term antiseptic agents may be used for weepy lesions in AE:
diluted potassium permanganate solution as bath/soak over the limbs and trunk
normal saline dab/wash over the face
Long-term continuous use of antiseptics should be avoided.
Educational Interventions
Educational and psychological interventions are used as an adjunct to conventional therapy in the management of AE. Patient education plays an important role in the self-management of AE. The use of a written eczema action plan (WEAP) may enhance patients' understanding and empower patients/caregivers to better manage their condition, thus reducing the frequency and severity of fl ares and the frequency of clinical encounters.
WRITTEN ECZEMA ACTION PLAN.
| NAME: | GREEN = GO : Use preventive measures YELLOW = CAUTION : Use lower strength medications RED = FLARE : Use higher strength medications and consult your doctor |
| GREEN | ECZEMA UNDER CONTROL |

|
REGULAR DAILY SKIN CARE
|
| YELLOW | ECZEMA WORSENING |
|
SKIN CARE DURING WORSENING
|
| RED | FLARE |
 |
SKIN CARE DURING FLARE
|
Referral
Referral to a dermatology service may be needed in the management of AE. The urgency of referral is dependent upon various factors. Referrals may be classified as either urgent or non-urgent.
- Urgent referral (within 24 hours)
- AE with clinical suspicion of eczema herpeticum (eczema with widespread herpes simplex infection)
- AE with severe skin bacterial infection that requires intravenous antibiotics
- AE with acute erythroderma where the eczema is affecting more than 80% of the body surface area
- Non-urgent referral
- Diagnostic uncertainty
- Severe or uncontrolled eczema:
- requirement of potent and very potent TCS
- frequent infections
- poor sleep or excessive scratching
- treatment failure with appropriate topical therapy regimen
- Parental concern
- Need for treatment demonstration/education
- Involvement of sites that are difficult to treat
- Psychological disturbance on the patient or family
A summary of the management of AE is illustrated in the following algorithm.
Acknowledgement
Details of the evidence supporting the above statements can be found in Clinical Practice Guidelines on the Management of Atopic Eczema 2018, available on the following websites: http://www.moh.gov.my (Ministry of Health Malaysia) and http://www.acadmed.org.my (Academy of Medicine). Corresponding organization: CPG Secretariat, Health Technology Assessment Section, Medical Development Division, Ministry of Health Malaysia; contactable at htamalaysia@moh.gov.my.


