To the Editor:
The 2019 novel coronavirus disease COVID-19, originally responsible for a cluster of pneumonia cases in Wuhan, China, has now become a global pandemic according to the World Health Organisation (WHO) with 132,758 cases and 4955 deaths globally as of 13 March 2020 [1]. Common symptoms of COVID-19 include fever, cough, dyspnoea and malaise. The disease is thought to spread via respiratory droplets among persons in close contact and possibly from contaminated surfaces [2]. Reports have also suggested that the virus can cause conjunctivitis and may be transmitted by aerosol contact with conjunctiva [3]. Ophthalmology practitioners may be susceptible to infection due to close patient proximity during slit lamp examination and the potential contamination of instruments [4].
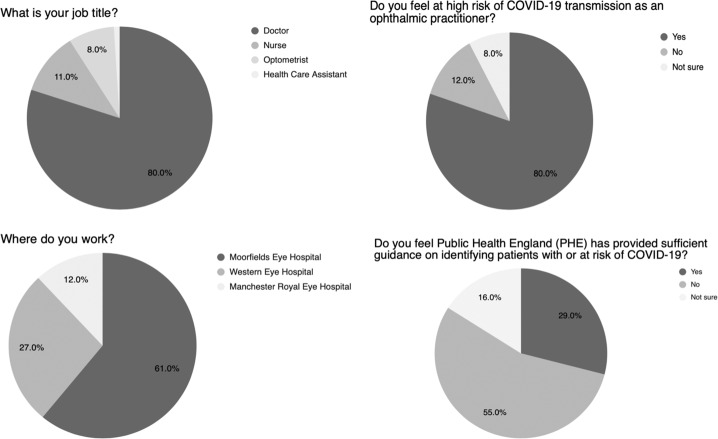
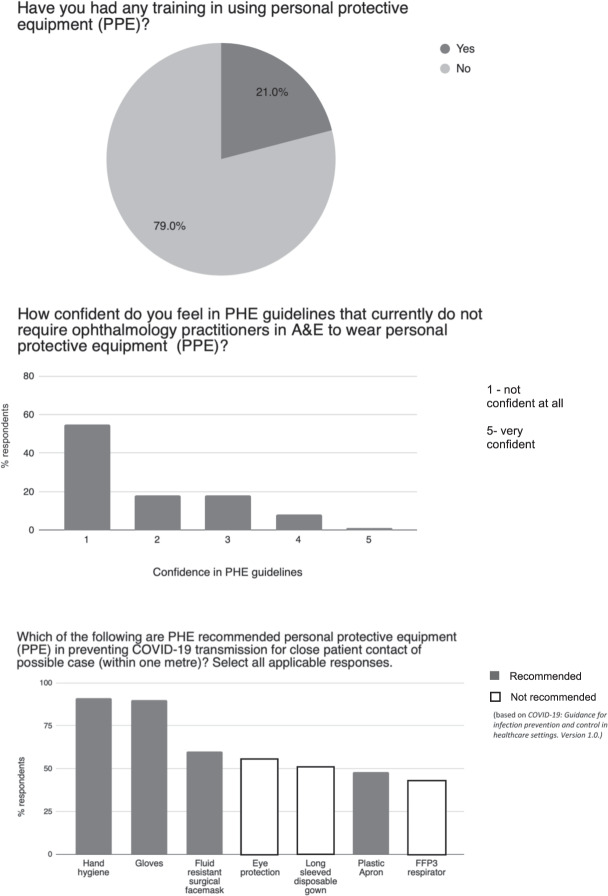
We conducted a self-administered anonymous survey (Google Forms) disseminated by email of ophthalmology doctors, nurses, optometrists and healthcare assistants employed at Moorfields Eye Hospital, Western Eye Hospital and Manchester Royal Eye Hospital from 10 March 2020 to 12 March 2020 to assess perception of COVID-19 exposure risk, understanding and confidence in current Public Health England (PHE) guidelines for identifying possible COVID-19 cases, knowledge of Personal Protective Equipment (PPE) recommendations and training in its usage when managing such cases. There was also a free text option for additional comments. A total of 100 practitioners completed the survey comprising doctors (80%), optometrists (11%), nurses (8%) and healthcare assistants (1%). Eighty percent of respondents felt at high risk of COVID-19 transmission at work, 12% did not and 8% were not sure. Most respondents felt published guidelines were not sufficient for identifying patients with or at risk of COVID-19 (Fig. 1). Respondents generally had poor confidence in guidelines which did not require ophthalmology practitioners in A&E to routinely wear PPE, and the majority had not had training in its use. There was a lack of understanding of recommended PPE for close patient contact with possible cases (Fig. 2). Several respondents raised concerns about the very close proximity of 20–30 cm to patients during slit lamp examinations and the need for effective triage for non-urgent eye problems. One respondent raised concerns about the lack of guidance for managing patients presenting to standalone eye units with suspected COVID-19 requiring emergency ophthalmic surgery.
Fig. 1. Demographics of survey respondents, perceived risk of COVID-19 transmission and confidence in PHE COVID-19 guidelines.
Survey of ophthalmology practitioners working in A&E.
Fig. 2.
Knowledge and confidence of using PPE among ophthalmology practitioners in A&E.
Our survey demonstrates a lack of confidence in and understanding of COVID-19 PHE guidance amongst ophthalmic practitioners, together with significant anxiety regarding exposure risk in the ophthalmic setting. Reflecting this, standalone eye hospitals have started to introduce their own protective equipment measures outside of PHE and RCOphth guidance such as acetate slit lamp screens and FFP3 respirators for all clinical staff in A&E. This lack of coordination amongst units risks generating further confusion for staff and patients. Given the rapidly evolving situation, effective dissemination of and adherence to regularly updated PHE guidelines is prudent to instil confidence amongst practitioners and to ensure a co-ordinated evidence-based response across the ophthalmic workforce. Revisiting strategies applied within the ophthalmic setting during previous novel coronavirus outbreaks such as SARS-CoV may well reduce transmission and save lives [5].
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Amal Minocha, Sing Yue Sim
References
- 1.World Health Organisation (WHO). Coronavirus disease 2019 (COVID-2019) Situation Report-53. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200313-sitrep-53-covid-19.pdf?sfvrsn=adb3f72_2.
- 2.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;102433. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 3.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS‐CoV‐2 infection. J Med Virol. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 4.Li J-PO, Lam DSC, Chen Y, Ting DSW. Novel Coronavirus disease 2019 (COVID-19): The importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104:297–8. doi: 10.1136/bjophthalmol-2020-315994. [DOI] [PubMed] [Google Scholar]
- 5.Chan W-M, Liu DTL, Chan PKS, Chong KKL, Yuen KSC, Chiu TYH, et al. Precautions in ophthalmic practice in a hospital with a major acute SARS outbreak: an experience from Hong Kong. Eye. 2006;20:283–9. doi: 10.1038/sj.eye.6701885. [DOI] [PMC free article] [PubMed] [Google Scholar]