Abstract
The novel severe acute respiratory syndrome coronavirus-2 pandemic is a global health problem, which started to affect China by the end of 2019. In Europe, Italy has faced this novel disease entity (named novel coronavirus disease [COVID-19]) first and severely. COVID-19 represents a significant hurdle for public health services and a potential harm for patients with cancer. The Collegio Italiano dei Primari Oncologi Medici (CIPOMO) is an Italian association of head physicians in oncology departments, which promotes working and research activities in oncology on a national basis. In the midst of the epidemic in Italy, the CIPOMO promoted a national survey aiming to evaluate the impact of COVID-19 on clinical activity of oncologists and the implementation of containment measures of COVID-19 diffusion. Overall, 122 head physicians participated in this survey, with a homogeneous distribution on the national territory. Results show that the following measures for oncologic patients have been promptly implemented through the whole country: use of protective devices, triage of patients accessing the hospital, delay of non-urgent visits and use of telemedicine. Results of this survey suggest that Italian oncology departments have promptly set a proactive approach to the actual emergency. Oncologists need to preserve the continuum of care of patients, as the benefit of ensuring a well-delivered anti-cancer treatment plan outweighs the risk of COVID-19 infection. International cooperation is an important starting point, as heavily affected nations can serve as an example to find out ways to safely preserve health activity during the pandemic.
Keywords: Cancer, Infection, Coronavirus, Pandemic, Health care, Oncology
Highlights
-
•
The novel coronavirus disease is a global health problem.
-
•
Patients with cancer are at risk of infections due to several predisposing factors.
-
•
Delaying oncologic procedures can compromise the efficacy of treatment itself.
-
•
Oncologists face the need to preserve their patients' continuum of care.
-
•
Proactive containment measures can protect both patients and medical activity.
1. Introduction
On 11th March 2020, the World Health Organisation declared the novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) outbreak a pandemic [1]. By the end of February 2020, Italy was experiencing the rapid spread of the virus, which started to affect the north of the country with a daily increase in the number of cases and consequent deaths [2]. In Italy, data regarding the diffusion of the novel coronavirus disease (COVID-19), caused by SARS-CoV-2, confirmed its higher lethality than that observed in China and worldwide (9% vs 4.3%) [3].
Following the Chinese model, containment measures to reduce the risk of COVID-19 in Italy have been promptly activated and implemented. The first national decree, issued on 8th March, instituted a containment zone concerning the most affected areas of the country (the so-called Red Zone, which at that time included 3 regions in the north of Italy: Lombardia, Emilia Romagna and Veneto). In the following days, a series of decrees have extended increasingly strict measures to the whole national territory. The main provisions included forbidding all gatherings of people, restricting movements of people within and outside the hometown, except for circumstances of necessity, and encouraging employees to work from home. In this circumstance, health workers cannot take any leave and are asked to suspend all non-urgent activities. All planned surgeries are postponed, to give over intensive care beds to the treatment of patients with COVID-19, and hospitals had to create new intensive care places by converting operating and anaesthetic rooms. Table 1 outlines the key milestones of COVID-19 diffusion.
Table 1.
Timeline of the key stages of COVID-19 diffusion in Italy.
| 31st December 2019 | The Municipal Health Services in Wuhan (China) report to the WHO a cluster of patients with pneumonia of unknown etiologic agent in the city of Wuhan, in the Chinese province of Hubei. |
| 9th January 2020 | Chinese authorities make a preliminary determination of a novel (or new) coronavirus (SARS-CoV-2), as the causal agent of the severe acute respiratory syndrome, named COVID-19. Chinese investigators conduct gene sequencing of the virus, using an isolate from one positive patient sample, making diagnostic tests promptly available worldwide. |
| 22nd January 2020 | The Italian Ministry of Health sets up a task force to coordinate interventions on the Italian territory, together with international responsible institutions. A surveillance system for suspected cases is established. |
| 30th January 2020 | Two Chinese tourists hospitalised for respiratory tract infection, in Rome, are the first confirmed cases of COVID-19 detected in Italy. Regional Health Authorities implement measures to track contacts of the two subjects. All contacts resulted negative for COVID-19. Italian government decides to interrupt all air connections with China. The WHO declares COVID-19 diffusion in China a public health emergency. |
| 31st January 2020 | The Italian Council of Ministers declares national public health emergency condition. |
| 21st February 2020 | The Italian National Institute of Health confirms the first case of local transmission of COVID-19 infection in a 38-year-old patient in Codogno. |
| 28th February 2020 | The WHO raises the threat definition for COVID-19 epidemic at a ‘high level’ of threatening for the global health. |
| 8th-9th March 2020 | A national decree institutes a containment zone concerning the most affected areas of the country, located in the north of Italy (Lombardia, Emilia Romagna and Veneto). The main provisions include forbidding all gatherings of people; restricting movements of people within and outside the hometown, except for circumstances of necessity; encouraging employees to work from home. Health workers cannot take any leave and are asked to suspend all non-urgent activities; all planned surgeries are postponed, to give over intensive care beds to the treatment of patients with COVID-19. |
| 10th March 2020 | The Italian Ministry of Health issues recommendations for oncologic and onco-haematologic patients, providing protective measures for off-therapy patients and those receiving systemic treatment. Oncologists are required to postpone follow up visits, in order to reduce patients' access to hospitals. Patients with thoracic tumours and those who underwent pulmonary resection are to be considered a subgroup of high-risk patients. |
| 11th March 2020 | The Italian Council of Ministers urgently sets increasingly strict containment measures to the whole national territory. The WHO declares the novel SARS-CoV-2 outbreak a pandemic. |
| 13th March 2020 | Three Italian scientific associations (AIOM, CIPOMO and COMU) release an official document for the management of oncologic and onco-haematologic activities during COVID-19 pandemic. The WHO declares Europe is becoming the new epicentre of COVID-19 pandemic. |
AIOM, Associazione Italiana di Oncologia Medica; CIPOMO, Collegio Italiano dei Primari Oncologi Medici Ospedalieri; COMU, Collegio degli Oncologi Medici Universitari; COVID-19, novel coronavirus disease; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2; WHO, World Health Organisation.
This pandemic represents a significant harm for patients with cancer, who are at high risk of infections due to several predisposing factors [4]. Moreover, most treatment procedures in oncology cannot be delayed without compromising the efficacy of treatment itself. In Italy, specific indications on oncologic patients’ management were given on 10th March, mainly regarding caution measures to reduce the risk of infection (i.e. use of personal protective equipment, practice social distancing). While encouraging physicians to postpone follow-up visits, indications were given to guarantee oncologic services even within the Red Zone to maintain the continuum of care. At the present time, data regarding diffusion and management of COVID-19 in oncologic patients are scarce [5,6]. Such emergency has led Italian oncologists to join forces, with the aim to find a way not to compromise the continuum of care of patients and to preserve safe everyday clinical practice.
The Italian college of directors of the National Health System (NHS) of the Hospital Department of Medical Oncology (Collegio Italiano dei Primari Oncologi Medici Ospedalieri [CIPOMO]) gathers the heads of all the NHS hospital medical oncology departments, including general hospitals, city hospitals and cancer centres. This association safeguards and promotes working and research activities in oncology on a national basis. In the midst of the epidemic in Italy, the CIPOMO promoted a national survey aiming to evaluate the impact of COVID-19 on clinical activity of oncologists and the implementation of containment measures of COVID-19 diffusion.
Here, we present the results of this survey, providing an overview of the COVID-19 epidemic in Italy and assessing potential interventions to overcome this critical situation.
1.1. Survey characteristics and results
The survey includes a total of 27 questions, which are divided in 3 sections: the first section assesses the routine use of preventive measures (e.g. vaccinations) in oncologic patients, the second contains questions regarding COVID-19 diffusion containment measures adopted before the enactment of national decrees in this regard and the third and last section assesses the diffusion of COVID-19 in oncology units and its impact on working activity, after national decrees on containment measures were adopted. A complete original version of the survey is provided in Supplementary Material 1.
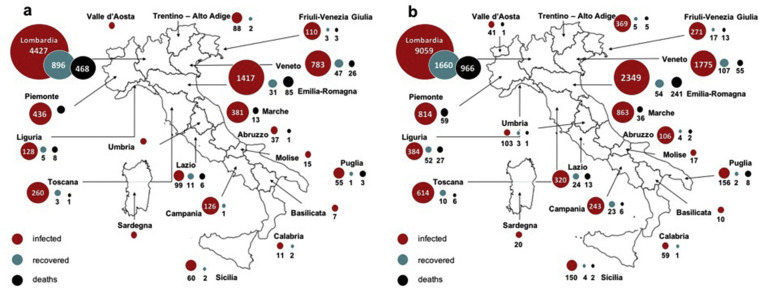
The survey was launched online on 12th March 2020 and closed on 15th March 2020. Fig. 1 displays the COVID-19 diffusion in Italy at the beginning and end of the present survey. At the time of the survey initiation, most of COVID-19 cases were gathered in the Red Zone. Overall, 122 head physicians of oncology departments participated in the survey, with an 84% survey completion rate. Results of the survey sections are displayed in Table 2, Table 3, Table 4 . In Italy there is a universalistic NHS, with an individual administration further subdivided among 20 regions which are geographically distributed in north, centre and south (including the islands). For this reason, results are presented as follows: all regions (n = 122); Red Zone (n = 39); in the north of Italy, excluding the Red Zone (n = 26); in the centre of Italy (n = 18) and in the south of Italy and islands (n = 25). To simplify consultation and interpretation of results, Table 2, Table 3, Table 4 contain answers to multiple choice questions of the survey, while answers to open questions are reported further in the main text.
Fig. 1.
Overview of COVID-19 diffusion in Italy at the beginning of the survey on 12th March 2020 (1a) and at the end of the survey on 15th March 2020 (1b). COVID-19, novel coronavirus disease.
Table 2.
Survey section 1: general (i.e. non-COVID-19) preventive measures for reducing the risk of infections in oncologic patients.
| All, n (%) n = 122 | Red Zoneb, n (%) n = 39 (32) | North, n (%) n = 26 (21) | Centre, n (%) n = 18 (15) | South and islands, n (%) n = 25 (20) | ||
|---|---|---|---|---|---|---|
| Vaccination of oncologic pts in view of a systemic therapy | No | 8 (7) | 2 (5) | 2 (8) | 2 (11) | 0 |
| Yes | 114 (93) | 37 (95) | 24 (92) | 16 (89) | 25 (100) | |
| Which kind of oncologic treatment will the vaccinated pts receivea | CT | 28 (25) | 8 (20) | 7 (27) | 4 (22) | 6 (24) |
| ICI | 12 (11) | 4 (10) | 4 (15) | 1 (5) | 1 (4) | |
| HT, TT | 16 (14) | 6 (15) | 4 (15) | 2 (11) | 3 (12) | |
| None, follow-up | 8 (7) | 3 (8) | 1 (4) | 0 | 2 (8) | |
| All pts | 64 (57) | 22 (56) | 16 (61) | 5 (28) | 16 (64) | |
| Pts with risk factorsc | 42 (37) | 14 (36) | 7 (27) | 8 (44) | 7 (28) | |
| Which kind of vaccination is/are adviseda | Seasonal flu | 72 (64) | 27 (69) | 17 (65) | 11 (61) | 12 (48) |
| Pneumococcal | 8 (7) | 3 (8) | 2 (8) | 0 | 0 | |
| Both | 42 (37) | 11 (28) | 8 (31) | 4 (22) | 13 (52) | |
| Other (tetanus, VZV) | 1 (<1) | 1 (<1) | 0 | 0 | 0 | |
| Report of seasonal flu cases (e.g. national registry) | No | 94 (80) | 28 (72) | 21 (81) | 16 (89) | 23 (92) |
| Yes | 15 (13) | 8 (20) | 3 (11) | 1 (5) | 2 (8) | |
| UNK | 9 (7) | 3 (8) | 2 (8) | 1 (5) | 0 |
BMI, body mass index; CT, chemotherapy; HT, hormonal therapy; ICI, immune-checkpoint inhibitors; pts, patients; TT, targeted therapy; UNK, unknown; VZV, varicella zoster virus; COVID-19, novel coronavirus disease.
Questions with more than one possible answer.
Red Zone at the time of the survey includes the following Italian countries: Lombardia, Emilia Romagna, Veneto.
Age ≥75 years, cardiovascular and/or respiratory disease, chronic infections, diabetes, obesity (BMI ≥ 30), immune-suppressive therapies.
Table 3.
Survey section 2: COVID-19 preventive measures.
| Survey questions | Answers | All, n (%) n = 122 | Red Zoneb, n (%) n = 39 (32) | North, n (%) n = 26 (21) | Centre, n (%) n = 18 (15) | South and islands, n (%) n = 25 (20) |
|---|---|---|---|---|---|---|
| Triage processd for pts accessing oncologic services | No | 6 (5) | 2 (5) | 1 (4) | 1 (6) | 2 (4) |
| Yes | 112 (95) | 37 (95) | 25 (96) | 17 (94) | 23 (96) | |
| Which kind of pts are triageda | All | 79 (70) | 24 (61) | 24 (92) | 10 (56) | 14 (56) |
| Pts with fever | 20 (19) | 7 (18) | 1 (4) | 5 (28) | 6 (24) | |
| Pts with RSe | 14 (12) | 5 (13) | 1 (4) | 4 (22) | 4 (16) | |
| Pts with feverf + RS | 8 (7) | 8 (20) | 0 | 4 (22) | 5 (20) | |
| Pts are questioned about feverf, RS and/or contact with high-risk subjects | No | 5 (4) | 1 (2) | 1 (4) | 2 (11) | 1 (4) |
| Yes | 113 (96) | 38 (97) | 25 (96) | 16 (89) | 24 (96) | |
| Diagnostic work-up for pts with suspicious symptoms | No | 39 (33) | 9 (23) | 6 (23) | 9 (50) | 13 (52) |
| Yes | 79 (67) | 30 (77) | 20 (77) | 9 (50) | 12 (48) | |
| Measures for reducing pts accesses from first cases of COVID-19 | No | 11 (9) | 5 (13) | 2 (8) | 1 (6) | 1 (4) |
| Yes | 107 (91) | 34 (87) | 24 (92) | 17 (94) | 24 (96) | |
| Which kind of pts are these measures addressed toa | All follow-up visits (non-urgent) | 98 (92) | 30 (77) | 24 (92) | 15 (83) | 22 (88) |
| Follow-up visits of high-risk ptsc | 33 (31) | 9 (23) | 7 (27) | 7 (39) | 6 (25) | |
| pts receiving adjuvant therapy | 4 (4) | 0 | 1 (4) | 1 (6) | 2 (8) | |
| Alternative modalities to get in touch with pts (e.g. telephonic interview) | No | 23 (20) | 10 (26) | 3 (11) | 4 (22) | 4 (16) |
| Yes | 88 (80) | 25 (64) | 21 (81) | 14 (78) | 22 (88) | |
| Reduced access for pts coming from Red Zone, and/or reporting feverf and/or RS | No | 21 (18) | 9 (23) | 3 (11) | 6 (33) | 2 (8) |
| No, Red Zone out of catchment area | 18 (15) | 2 (5) | 4 (15) | 4 (22) | 6 (24) | |
| Yes | 77 (66) | 28 (72) | 19 (73) | 8 (45) | 17 (68) | |
| Reduced access for visitors and/or caregivers of pts in hospital ward, day hospital, outpatient visits | No | 0 | 1 (3) | 0 | 0 | 0 |
| Yes, limited access for one visitor per patient | 59 (51) | 23 (59) | 10 (38) | 9 (50) | 14 (56) | |
| Yes, denied access for visitors | 50 (43) | 13 (33) | 15 (58) | 9 (50) | 11 (44) | |
| Autonomous management of measures | Yes | 50 (43) | 17 (44) | 11 (42) | 7 (39) | 12 (48) |
| Medical direction measures | 53 (46) | 18 (46) | 13 (50) | 6 (33) | 12 (48) | |
| Regional measures | 13 (11) | 4 (10) | 2 (8) | 5 (28) | 1 (4) | |
| Measures for reducing pts accesses in view of actual legislationga | No, internal measures already activated | 61 (52) | 22 (56) | 12 (46) | 9 (50) | 16 (64) |
| Yes | 59 (51) | 19 (49) | 16 (61) | 9 (50) | 9 (36) | |
| Which kind of pts are these measures addressed toa | All follow-up visits (non-urgent) | 82 (92) | 26 (67) | 21 (81) | 12 (67) | 19 (76) |
| Follow-up visits of high-risk ptsb | 26 (29) | 9 (23) | 4 (15) | 3 (23) | 8 (32) | |
| Pts receiving adjuvant therapy | 3 (3) | 0 | 1 (4) | 1 (8) | 2 (8) | |
| Did your Country provide guidelines for oncologic pts management during COVID-19 emergency? | No | 33 (28) | 11 (28) | 7 (27) | 6 (33) | 7 (28) |
| Yes | 73 (63) | 26 (67) | 17 (65) | 8 (45) | 16 (64) | |
| Only for hospital pts | 10 (9) | 2 (5) | 2 (8) | 4 (22) | 2 (8) | |
| How is your activity changing in view of actual legislationg? | Significant decreased | 28 (24) | 9 (23) | 6 (23) | 7 (39) | 5 (20) |
| Negligible decreased | 70 (60) | 23 (59) | 18 (69) | 9 (50) | 15 (60) | |
| Unchanged | 10 (9) | 5 (13) | 1 (4) | 1 (6) | 2 (8) | |
| Increased | 0 | 0 | 0 | 0 | 0 | |
| UNK | 8 (7) | 2 (5) | 1 (4) | 1 (6) | 3 (12) |
BMI, body mass index; pts, patients; RS, respiratory symptom; UNK, unknown; COVID-19, novel coronavirus disease.
Questions with more than one possible answer.
Red Zone at the time of the survey includes the following Italian countries: Lombardia, Emilia Romagna and Veneto.
Age ≥75 years, cardiovascular and/or respiratory disease, chronic infections, diabetes, obesity (BMI ≥ 30), immune-suppressive therapies.
Patients triage includes: vital signs, and respiratory signs/symptoms evaluation.
Definition of fever: TC ≥ 37.5 °C.
Definition of respiratory symptoms: dyspnea, cough, rhinitis.
Administrative order issued on 11th March (refer text for complete details).
Table 4.
Survey section 3: overview of COVID-19 diffusion.
| Survey questions | Answers | All, n (%) n = 122 | Red Zoneb, n (%) n = 39 (32) | North, n (%) n = 26 (21) | Centre, n (%) n = 18 (15) | South and islands, n (%) n = 25 (20) |
|---|---|---|---|---|---|---|
| Have your oncologists been requested for guard duties in Internal Medicine and/or Emergency wards? | No | 75 (61) | 19 (49) | 15 (58) | 15 (83) | 24 (96) |
| Yes | 39 (32) | 20 (51) | 11 (42) | 3 (17) | 1 (4) | |
| Are guard duties including COVID wards? | No | 29 (24) | 9 (23) | 5 (19) | 6 (33) | 7 (28) |
| Yes | 28 (23) | 15 (38) | 9 (35) | 1 (5) | 1 (4) | |
| Has any of your patients been diagnosed with COVID? | No | 86 (70) | 21 (54) | 20 (77) | 14 (78) | 25 (100) |
| Yes | 29 (24) | 18 (46) | 6 (23) | 4 (22) | 0 | |
| How was COVID diagnosis performed?a | Contact with high-risk subject(s)c | 8 (6) | 7 (18) | 0 | 1 (5) | – |
| Symptoms at triage | 11 (9) | 7 (18) | 3 (8) | 1 (5) | – | |
| Hospitalised patients and/or emergency room access | 15 (12) | 9 (23) | 3 (8) | 2 (11) | – | |
| Do you reckon that actual measures will reduce the risk of COVID diffusion in oncologic wards? | No | 1 (<1) | 1 (3) | 0 | 0 | 0 |
| Yes, negligible | 47 (38) | 18 (46) | 10 (38) | 5 (28) | 10 (40) | |
| Yes, significant | 65 (53) | 20 (52) | 16 (62) | 13 (72) | 15 (60) |
COVID-19, novel coronavirus disease.
Questions with more than one possible answer.
Red Zone at the time of the survey includes the following Italian countries: Lombardia, Emilia Romagna and Veneto.
High-risk subjects: people with known COVID infection and/or coming from the Red Zone.
Results of Section 1 show that the overall tendency throughout Italy is to perform preventive vaccination in oncologic patients (Table 2). Most vaccinated patients are either receiving active systemic treatment (chemotherapy, immune therapy and hormonal or targeted therapy) and/or present one or more predisposing risk factors (i.e. age ≥75 years, cardiovascular and/or respiratory disease, chronic infections, diabetes, obesity, immune-suppressive therapies). The most widely adopted vaccination is for seasonal flu; however more than 30% of oncologists suggests also performing pneumococcal vaccination in those patients. Seasonal flu cases are not usually reported by medical oncologists to the dedicated national registry, rather this is commonly a duty of family doctors.
Answers to the questions in Section 2 clearly show that, even if by the time of the survey COVID-19 represented an emergency mainly in the north of Italy, diagnostic measures for all patients accessing oncologic services were immediately activated in the whole country (Table 3). Triage of patients included vital signs monitoring before entering the hospital (body temperature, SpO2, respiratory rate) but also questioning patients on the presence of symptoms during the 15 days before the visit and possible contacts with subjects affected by COVID-19 or coming from high-risk areas. In more than 65% of cases, the triage procedure was followed by preventive isolation and diagnostic work up of symptomatic patients, consisting in chest X-ray and rhino-pharyngeal swab to rule out the presence of SARS-CoV-2.
After the very first reports of COVID-19 in Italy, measures to reduce hospital access for oncologic patients were taken almost throughout the country. Such measures consisted mainly in delaying visits not considered to be urgent (i.e. patients in follow-up after surgery and/or radiotherapy and/or patients with breast cancer receiving adjuvant hormonal treatment after surgery), even more so if the patients presented risk factors (i.e. age >85 years, presence of comorbidities). Alternative ways to get in touch with patients have been widely used: most patients underwent telephonic interviews with interpretation of laboratory and radiologic examination reports, while in other cases, family doctors were delegated to inspect the results of follow-up examinations. Access to oncologic structures was similarly limited and/or denied for visitors and caregivers, either for outpatient visits, day hospital and ward admissions.
With the enactment of the decree on 9th March and subsequent decree on 11th March, containment preventive measures became effective in the Red Zone before and on the whole Italian territory thereafter. However, by that time, most oncologic units had already activated measures to contain access, under regional or internal (hospital medical direction) orders. As so, more than 50% of oncologic structures did not have to modify the measures they implemented to reduce the risk of infections, in view of the actual legislation. Owing to such measures, more than 20% of structures had reported a significant reduction in their routine activity, while 60% had only a negligible reduction and 9% had not substantially changed their activity.
Answers to the questions in Section 3 show that almost one third of oncologic structures had to employ their oncologists for guard duties in the internal medicine ward and/or emergency department; in 23% of cases, guard duties in the COVID ward were included (Table 4). This percentage was understandably higher in the north of the country, reaching 51% and 38% of oncologists employed for internal medicine/emergency department and COVID ward guard duties, respectively, in the Red Zone. Twenty-four percent of Italian oncology departments had at least one patient diagnosed with COVID-19, with a higher rate in the Red Zone (46%) and no diagnosis at all in the south of Italy and in islands. On examining reports from the Red Zone, it emerges that most patients accessed the emergency room presenting with fever and/or respiratory symptoms (23%), while a significant proportion of patients was diagnosed after a triage procedure (18%) and/or a medical interview regarding possible contacts with subjects at risk (18%).
When questioned about the impact of containment measures in oncologic structures, most physicians found that measures could have a significant impact on reducing the risk of COVID-19 diffusion (53%), while 38% found they could have only a negligible effect. Answers to an open question asking whether other useful measures were applied (i.e. other than those indicated by decrees) raised the following issues: re-distribution of patients’ treatment sessions homogeneously throughout the week, reduction of hospital access by relying on family doctors for home visits (e.g. medications, patients on treatment with oral metronomic chemotherapy), creation of a dedicated telephone line for emergencies, careful evaluation of risk-to-benefit ratio in heavily pre-treated patients and possibly postponing the start of further lines of palliative therapies. Regarding working activity, multidisciplinary boards have been converted in telematic meetings and counselling of patients in other hospital wards have been managed by phone, when feasible. In some cases, physicians on duty in COVID wards have been consequently waived from oncologic activities to reduce the risk of infection for both patients and colleagues.
2. Discussion
Results of this survey deserve several considerations. Some effective points emerge from this survey, which partly have been also raised in the comment recently released by the European Society for Medical Oncology [7]. First, oncologists face the need to preserve the continuum of care for most of their patients, as the benefit of ensuring a well-delivered anti-cancer treatment plan outweighs the risk of COVID-19 infection. However, the risk from COVID-19 exposure varies significantly from patient to patient, making treatment tailoring important now more than ever. Second, physicians have to get used to a new working activity, which implies the use of tele-consultation services when feasible and reducing the number of visits by means of customising treatment delivery (three or two-weekly as opposed to weekly, oral or subcutaneous alternatives as opposed to intravenous administration). In addition, in view of a visit a telephonic ‘previous day’ triage could help to avoid the access of symptomatic patients to oncologic wards. Third, protection of patients and physicians is paramount to keep providing the best service in a safe way.
This last issue raises the question on how to optimise oncologic resources for COVID-19 emergency. Owing to both clinical characteristics of oncologic patients, which are frail and at high risk for infections, and features of oncologic services, which often cannot be postponed, how can oncologist reasonably help in this emergency without compromising patients’ continuum of care? To date, no clear indications have been provided to healthcare providers in oncology, making it difficult to create a common line of action.
3. Conclusions
In conclusion, results of our survey suggest that Italian oncology departments have promptly set a proactive approach to the actual emergency. Together with indications provided by national decrees and internal dispositions, several individual initiatives have contributed to reorganise working activity in the actual condition. The medical community worldwide is facing a difficult situation, and oncologists in particular require several extra precautions to protect the patients first and their activity thereafter. International cooperation is an important starting point, as heavily affected nations can serve as an example to find out ways to safely preserve health activity during the pandemic.
Fundings
No funding was obtained for the present investigation.
Conflict of interest statement
The authors they have no conflicts of interest to declare for the present article.
Acknowledgements
The authors thank all the CIPOMO members for participating in the present survey, thereby making this work possible to be shared in the oncologists' community.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ejca.2020.03.024.
Appendix A. Supplementary data
The following is/are the Supplementary data to this article:
References
- 1.The World Health Organization (WHO) https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at: Accessed March 22nd 2020.
- 2.Lazzerini M., Putoto G. COVID-19 in Italy: momentous decisions and many uncertainties. Lancet Glob Health. 2020 Mar 18 doi: 10.1016/S2214-109X(20)30110-8. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The World Health Organization (WHO) Health emergency dashboard. https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd Available at: Accessed March 19th 2020.
- 4.El Ramahi R., Freifeld A. Epidemiology, diagnosis, treatment, and prevention of influenza infection in oncology patients. J Oncol Pract. 2019;15(4):177–184. doi: 10.1200/JOP.18.00567. [DOI] [PubMed] [Google Scholar]
- 5.Liang W., Guan W., Chen R., Wang W., Li J., Xu K. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu J., Ouyang W., Chua M.L.K., Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. March 25th 2020 doi: 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Society for Medical Oncology (ESMO) Newsroom. https://www.esmo.org/newsroom/covid-19-and-cancer/supporting-oncology-professionals Available at: Accessed March 22nd 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.