Highlights
-
•
The recent outbreak of SARS‐CoV‐2 has assumed worldwide proportion.
-
•
Tracheostomy in intubated COVID-19 patients requires adjunctive safeguards.
-
•
A step-by-step approach named CORONA is proposed in order to recall essential recommendations during the surgical procedure.
-
•
The CORONA-method would allow a secure space in which health workers can guarantee their activity, safely.
Introduction
The recent outbreak of SARS-CoV-2 has reached worldwide proportions since it began in late 2019 [1]. Due to the high virulence via aerosol transmissions, to date COVID-19 has infected more than 575,444 people all over the world, causing 26,654 confirmed deaths [2]. Italy is the leading nation in the world for infections, counting about 86,498 (15.0%) confirmed positive people, as for number of Sars-CoV-2 associated deaths, reached 8460 people on march 28th, 2020. The high rate of hospital and intensive care unit (ICU) admission provoked a serious congestion across hospitals and extreme measures have been taken to avoid a health-service collapse.
According to official online data, roughly 10% of Italians that are infected are health-care workers, which account for 7763 people [3]. Indeed, health workers incur a higher risk of infection and among these, anesthetists and surgeons are most prone to exposure.
Sedated ICU patients who require prolonged intubation, often require a safer management of the airway, biasing for tracheostomy. A recent systematic review revealed how early tracheostomy, performed in the first 7 days after orotracheal intubation, is associated with a reduction of mechanical ventilation duration, mortality rate and length of stay in ICU [4]. Despite surgical tracheostomies being routinely performed in the surgeon’s daily practice, the surgeon’s risk of exposure to COVID-19 during this procedure is consistent. Due to the direct access to the airway and the mechanical ventilation, which generates a huge amount of droplets in case of air-leakage from the cuff, tracheostomies place surgeons to be the highest risk category, together with ICU nurses and doctors. Surgical tracheostomy on sedated and intubated patient is, by far, preferable than awake patient tracheostomy or percutaneous cricothyrotomy for which air-flow cessation cannot be obtained and droplets emission is inevitably higher.
Due to the expected rise of tracheostomy procedures in such scenario, we propose a step-by-step approach in order to minimize the operator infection risk and avoid health worker shortage.
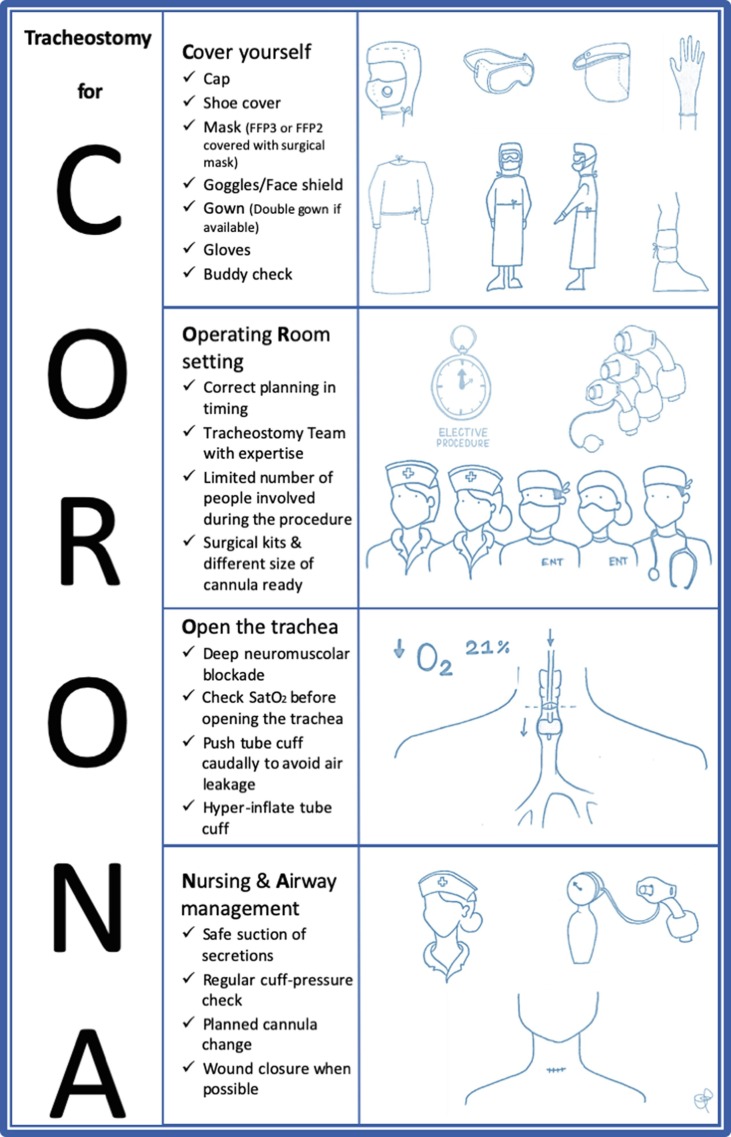
The CORONA-steps acronym aims to create easy to remember steps that the tracheostomy must be accompanied by: Covering yourself (C), Operating Room setting (OR), Opening the trachea (O) and Nursing and Airway management (NA). For this purpose, an illustrative and intuitive memorandum has been created (Fig. 1 ).
Fig. 1.
Illustration of the CORONA-steps for a safe tracheostomy in COVID-19 positive patient.
The CORONA method step-by-step
C for covering
Up to date there is no evidence-based guidelines on the use of personal protection equipment (PPE). Furthermore, in the worst-case scenario, PPE shortage or improper use could threaten health workers beyond the already high risk of infection. Few guidelines were recently released for tracheostomy procedures in COVID-19 positive patients [5], [6], [7], [8]. The rationale of covering should be a multilayer donning and doffing in order to minimize the possibility of contamination and regenerate reusable PPE (i.e. goggles, surgical wears and theater clogs) [9].
Before dressing, bracelets and other jewelry must be removed for surgical scrubbing.
-
–
Cap and shoe covers: are considered necessary for safely dressing;
-
–
Mask: FFP3 (Europe) or N99 (US) masks must be preferred than any other option. In case of FFP3 mask shortage, FFP2 or N95 masks can be used, covered by surgical mask. FFP mask covering with surgical mask seems reasonable to facilitate multi-layer doffing;
-
–
Goggles: eyes protection can be reached by surgical goggles, preferably, or a face shield;
-
–
Gown: use of double gown is preferable, where available;
-
–
Gloves: use of double nitrile gloves is suggested;
Consider additional coverage such as surgical hoods. Alternatively, face shield can be worn on top of goggles.
Once dressing is completed, full “buddy check” is recommended to prevent incorrect or incomplete covering.
OR for operating room setting
Where available, tracheostomy should be performed in the operating room. Alternatively, and probably more frequently, a provisional operating room can be set up in the ICU, ideally employing a negative pressure room. If any of these circumstances is not available, tracheostomy should be performed in an aerial-isolated room (i.e. doors and windows closed).
The procedure requires precise planning in timing and it should be performed on an already intubated and sedated patient.
Because of the risk-related procedure, the operating room must host only strictly required workers, meaning surgeons, an anesthesist and nurses.
Surgery: within a surgical department, a tracheostomy-team can be settled in order to avoid infection exposure by rotating shifts. For this reason, no more than two surgeons per procedure should be involved. In addition, expert surgeons would guarantee fast and effective tracheostomy comparing to less experienced surgeons or residents. Surgeons are required to check for the disposition of the correct surgical instruments, which can vary according to operator habit.
Anesthesia: if not indicated, a single anesthesist would be sufficient for mechanical ventilation and tube removal after tracheal incision.
Nurse: a scrub nurse and an assistant nurse should cope with surgical table and anesthesist assistance. Most of ORs and ICUs are equipped with disposable surgical kits while surgical instruments for tracheostomy should be stored in dedicated kits. These arrangements can help in avoiding extra and unnecessary surgical instruments. This setting allows an appropriate and rapid instrument dismissing and reconditioning. Along with instruments, the non-fenestrated cuffed tracheostomy tube with expected diameter-size should be prepared on the surgical table. A handy and close storage for different-size cannulas must be rapidly accessible to the assistant nurse.
O for open the trachea
This chapter will not discuss the surgical steps for tracheostomy, but rather it will outline some crucial hints which can be helpful to downplay passages at risk.
The patient in supine position, with hyper-extended head and face covered by drapes, requires a deep neuromuscular blockade in order to avoid swallowing and cough reflexes. Oxygenation must be achieved with positive end-expiratory pressure (PEEP). Once the anterior wall of the trachea is exposed, the anesthetist:
-
–
reduces the oxygen-percentage of the inflated air to 21%;
-
–
pushes the tube as caudally as possible, so as to avoid cuff breach;
-
–
hyper-inflates the tube cuff to ensure lower airway isolation.
Rapidly, the surgeon incises the trachea avoiding cuff damage and creates a window according to the most common technique. Tracheal incision must be performed as much cranially as possible (e.g. 1° or 2° inter-tracheal space). The anterior tracheal wall can be sutured to the skin to facilitate insertion and post-operative management.
Tracheal tube removal and tracheal cannula insertion represents the most hazardous step for infection spread. At this stage ventilation is stopped entirely, the tracheal tube is lifted, without extubating the patient, until its bottom side passes the tracheal window, then cannula is inserted in the tracheal lumen. Promptly, the cannula cuff is inflated at the appropriate pressure level and a non-fenestrated inner tube along with the heat and moisture exchanger is positioned: only then the ventilation is resumed by close airway circuit attachment. Tracheal cannula should be considered correctly positioned until CO2 value is displayed, avoiding stethoscope contamination by thoracic auscultation. Only at this point endotracheal tube is completely removed together with the sterile drape covering the face and tracheal cannula is secured to the neck with sutures and staples. Dressing should be performed so that no cannula change would be required for 7 days. Even PPE doffing is a crucial moment which should be carried out in a separate area, even then with “buddy check”. OR should be decontaminated according to the local guidelines.
NA for nursing and airway management
Tracheal cannula management must be performed in a BSL-3 setting which is nowadays the standard for regular ward and ICUs hosting COVID-19 positive patients. In the first 7 days tracheal cannula management should be performed by trained nursing staff and includes safe suction with a close airway circuit and regular checks of cuff-pressure. No dressing change should be performed unless evidence of local infection and cannula cuff should not be deflated unsafely. The cannula should be held during any passive movement of the patient to avoid air leakage from the stoma.
Cannula change can be planned 7–10 days later using the same standards (PPE utilization and airflow interruption). Subsequent cannula change can be delayed 30 days after.
Conclusions
Although tracheotomy is a widely described surgical technique, the current literature does not contain guidelines on the safe execution and management of this procedure in COVID-19 positive patients.
In this setting, CORONA-steps aims to promote a safe method for tracheostomy management in COVID-19 positive patients.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO). Coronavirus disease (COVID-19) Pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Published 2020.
- 3.Istituto Superiore di Sanità (ISS). Integrated Surveillance of COVID-19 in Italy; 2020. https://www.epicentro.iss.it/coronavirus/bollettino/Infografica_28marzo ENG.pdf.
- 4.Adly A., Youssef T.A., El-Begermy M.M., Younis H.M. Timing of tracheostomy in patients with prolonged endotracheal intubation: a systematic review. Eur Arch Otorhinolaryngol. 2018;275(3):679–690. doi: 10.1007/s00405-017-4838-7. [DOI] [PubMed] [Google Scholar]
- 5.UK E. Framework for Open Tracheostomy in COVID-19 Patients; 2020. [DOI] [PMC free article] [PubMed]
- 6.Canadian Society of Otolaryngology - Head and Neck Surgery. Recommendations from the CSO-HNS Taskforce on Performance of Tracheotomy During the COVID-19 Pandemic; 2020. [DOI] [PMC free article] [PubMed]
- 7.Cheung JC-H, Ho LT, Cheng JV, Cham EYK, Lam KN. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med February 2020. doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed]
- 8.Società Italiana di Otorinolaringoiatria (SIO). La Tracheostomia in Pazienti Affetti Da COVID-19; 2020.
- 9.Harrod M., Petersen L., Weston L.E. Understanding workflow and personal protective equipment challenges across different healthcare personnel roles. Clin Infect Dis. 2019;69(Supplement_3):S185–S191. doi: 10.1093/cid/ciz527. [DOI] [PubMed] [Google Scholar]