The emergence in 2012 of a new disease-causing coronavirus has generated substantial concern. As of June 26, 2013, Middle East respiratory syndrome coronavirus (MERS-CoV) had caused 77 laboratory-confirmed cases and 40 deaths.1 The virus is related to the severe acute respiratory syndrome coronavirus (SARS-CoV) that emerged in 2002–03. And, as SARS-CoV had during its prepandemic stage, MERS-CoV has probably been transmitted from an unknown animal host to human beings repeatedly in the past year.2, 3 Cases of human-to-human transmission have also been documented in several countries.1 This raises an important question: does MERS-CoV have the potential to cause a pandemic?
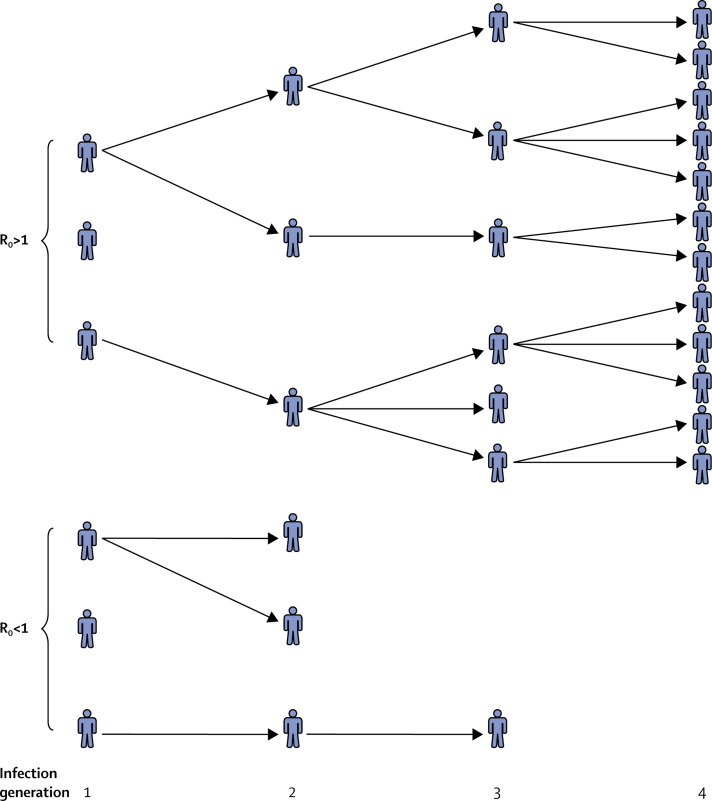
In The Lancet, Romulus Breban and colleagues4 address this question. Mathematical epidemiologists often use a simple but useful measure called the basic reproduction number (R0)—the average number of infections caused by one infected individual in a fully susceptible population.5, 6, 7, 8 If R0 is greater than 1, cases could grow exponentially and cause a full-blown epidemic (figure ). By contrast, if R0 is less than 1, then transmission is guaranteed to fade away, other things being equal. A primary task upon emergence of a new pathogen is estimation of its R0.6, 7, 8
Figure.
Early generations of infection transmission according to whether R0 is greater than or less than 1
R0=basic reproduction number.
Estimation of R0 during the prepandemic stage can be plagued by data uncertainty and variability, however. The number of secondary infections caused by an index case can be highly variable.8, 9, 10 Sometimes, an individual with a highly infectious disease will only cause a few infections. Conversely, individuals with a disease of normally low infectiousness can occasionally cause many infections. This effect is compounded by the small number of confirmed cases during the prepandemic stage, and the difficulty of identifying whether the earliest patients were infected by other human beings or by animals. Additionally, if R0 is not much larger than 1 (ie, between 1 and about 1·5), there is a fair chance that transmission will fade out anyway. Hence we cannot conclude that R0 is less than 1 just because secondary transmission seems to be low, as is the case for MERS-CoV so far. Using intuition to estimate whether R0 is greater than or less than 1 might not be accurate during the prepandemic stage, necessitating investigation using statistical methods.
Breban and colleagues4 apply a specialised statistical method to estimate the R0 of MERS-CoV.11 By carefully constructing different scenarios for who infected whom in recent MERS-CoV clusters, the investigators compute R0 under best-case and worst-case scenarios for MERS-CoV transmission trees. In the worst-case scenario, R0 is only 0·69 (95% CI 0·50–0·92). Despite the small number of confirmed cases so far, the upper 95% CI on the R0 is less than 1, meaning that MERS-CoV is unlikely to cause a pandemic, although a 99·7% CI might also have been useful to estimate pandemic risk, in addition to the standard 95% interval. For comparison, the investigators estimate that R0 was 0·80 (95% CI 0·54–1·13) for prepandemic SARS-CoV in southeast Asia (2002–03).
Breban and colleagues4 also provide calculations that enable the R0 estimates to be updated as more information about new MERS-CoV cases is reported. If the next index patient infects eight or more individuals, the investigators estimate that there is a 5% chance that R0 is actually above 1, under the worst-case scenario.
Breban and colleagues4 do a thorough job accounting for how their conclusions might be impacted by the quality of surveillance systems, the possibility of symptomatic and mild infections, and the network structure of who infected whom within MERS-CoV clusters. Other factors are more difficult to account for because the investigators would have to know how the situation might change in the future. For example, very recent reports document six asymptomatic infections.1 Additionally, R0 might change seasonally according to climate, school calendars, or yearly gatherings such as pilgrimages that put individuals in closer proximity to one another.12 If such gatherings involve greater contact between humans and infected animals, they would also create an opportunity for more disease introductions from animal populations.
Another potential future development is that MERS-CoV might start evolving, as SARS-CoV did. In the case of SARS-CoV, several mutations enabled the spike glycoprotein of the virus to bind with the angiotensin-converting enzyme 2 human receptor, making it much easier for the virus to infect humans and thus probably increasing the R0 of the virus.13 Evolution presents a particularly relevant challenge for estimating R0 from a series of outbreaks distributed through time. The approach used by Breban and colleagues4 implicitly assumes that R0 does not change. Hence, a trend towards increasing cluster sizes would be interpreted by their method as natural variability unrelated to virus adaptation. If cluster sizes were actually growing because the virus was evolving a higher R0, the method would underestimate the actual, more evolved R0. Therefore, the significance of a large, new cluster might be misinterpreted. A method that allows for the estimated R0 to rise or fall over time might capture movement toward the R0=1 threshold caused by viral adaptation or seasonality, although the amount of data available for MERS-CoV probably does not permit this at present.
To maximise our chances of containing MERS-CoV infection, we need continuing research, including updated R0 estimates and methodological refinements. However, the analysis by Breban and colleagues4 concludes that MERS-CoV—in its current guise—is unlikely to cause a pandemic.
Acknowledgments
We declare that we have no conflicts of interest.
References
- 1.WHO Middle East respiratory syndrome coronavirus (MERS-CoV) update. June 26, 2013. http://www.who.int/csr/don/2013_06_26/en/index.html (accessed June 28, 2013). [DOI] [PMC free article] [PubMed]
- 2.Song H-D, Tu C-C, Zhang G-W. Cross-host evolution of severe acute respiratory syndrome coronavirus in palm civet and human. Proc Natl Acad Sci USA. 2005;102:2430–2435. doi: 10.1073/pnas.0409608102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drosten C, Seilmaier M, Corman VM. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis. 2013 doi: 10.1016/S1473-3099(13)70154-3. published online June 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Breban R, Riou J, Fontanet A. Interhuman transmissibility of Middle East respiratory syndrome coronavirus: estimation of pandemic risk. Lancet. 2013 doi: 10.1016/S0140-6736(13)61492-0. published online July 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diekmann O, Heesterbeek JAP. Mathematical epidemiology of infectious diseases. John Wiley & Sons; New York: 2000. [Google Scholar]
- 6.Cauchemez S, Van Kerkhove MD, Riley S. Transmission scenarios for Middle East respiratory syndrome coronavirus (MERS-CoV) and how to tell them apart. Euro Surveill. 2013;18:20503. [PMC free article] [PubMed] [Google Scholar]
- 7.Bauch CT, Lloyd-Smith JO, Coffee MP, Galvani AP. Dynamically modelling SARS and other newly emerging respiratory illnesses: past, present, and future. Epidemiology. 2005;16:791–801. doi: 10.1097/01.ede.0000181633.80269.4c. [DOI] [PubMed] [Google Scholar]
- 8.Meyers LA, Pourbohloul B, Newman MEJ. Network theory and SARS: predicting outbreak diversity. J Theor Biol. 2005;232:71–81. doi: 10.1016/j.jtbi.2004.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lloyd-Smith JO, Schreiber SJ, Kopp PE, Getz WM. Superspreading and the effect of individual variation on disease emergence. Nature. 2005;438:355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galvani AP, May RM. Dimensions of superspreading. Nature. 2005;438:293–295. doi: 10.1038/438293a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blumberg S, Lloyd-Smith JO. Inference of R0 and transmission heterogeneity from the size distribution of stuttering chains. PLoS Comput Biol. 2013;9:e1002993. doi: 10.1371/journal.pcbi.1002993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan K, Memish ZA, Chabbra A. Global public health implications of a mass gathering in Mecca, Saudi Arabia during the midst of an influenza pandemic. J Travel Med. 2010;71:75–81. doi: 10.1111/j.1708-8305.2010.00397.x. [DOI] [PubMed] [Google Scholar]
- 13.Holmes KV. Adaptation of SARS coronavirus to humans. Science. 2005;309:1822–1823. doi: 10.1126/science.1118817. [DOI] [PubMed] [Google Scholar]