The three flu pandemics of the 20th century, in 1918, 1957, and 1968,1 caused millions of deaths, mainly from acute respiratory failure. More recently, outbreaks of the severe acute respiratory syndrome coronavirus, in 2002, and the Middle East respiratory syndrome coronavirus, in 2012, have been characterised by human-to-human transmission and high incidence of acute respiratory failure. The growing alarm for the novel coronavirus (2019-nCoV) spreading from China brings back the spectre of the rapidly diffusing pandemics of the past.2
Non-invasive ventilation is an effective and common treatment for patients with mild to moderate acute respiratory failure.3 It is associated with mortality reduction compared to either spontaneous breathing or mechanical ventilation by endotracheal tube as supported by several randomised trials.4 Emergency departments and intensive care units are increasingly applying non-invasive ventilation.3 When used to treat acute respiratory failure, non-invasive ventilation is applied to the patient mainly by face mask or helmet.3
Since coronavirus diffusion takes place by droplet transmission,2 aerosolisation during hospital procedures like intubation or bronchoscopy might represent a big concern, exposing other patients and health-care staff to an increased risk of infection, as during the flu pandemia.1 Aerosolisation with nosocomial amplification of the infection can also potentially happen around the face mask during non-invasive ventilation, as demonstrated in different simulation studies.5 Accordingly, the efficacy and safety of non-invasive ventilation during viral pandemic infection are still debated. However, during pandemics, the number of intensive care unit beds for mechanical ventilation through tracheal intubation could rapidly become insufficient,1 whereas non-invasive ventilation can be offered also outside the intensive care unit.4
To increase safety during non-invasive ventilation, use of a helmet as a non-invasive ventilation interface can be considered to avoid aerosolisation when the helmet is connected to the ventilator without air dispersion through a spring-valve; unfortunately, a helmet costs more than most face masks. Accordingly, when facing a patient with acute respiratory failure of suspected viral nature (and, above all, during pandemics), we recommend the adoption of helmets and avoidance of face masks as the non-invasive ventilation interface. Moreover, we suggest that manufacturers should develop cheap and safe non-invasive ventilation interfaces to be used during viral pandemics.
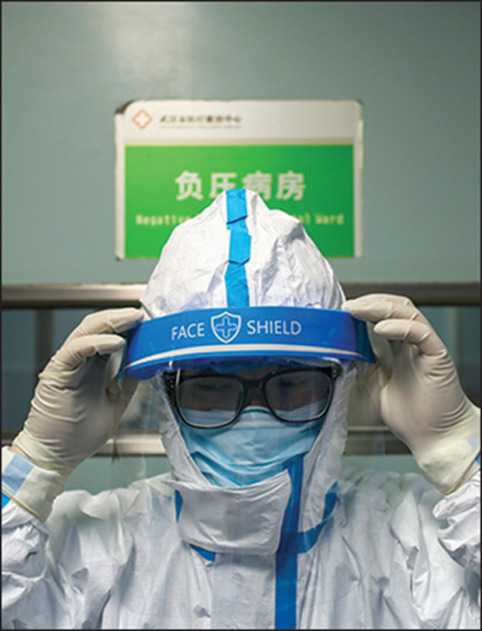
© 2020 Barcroft Media/Contributor/Getty Images
Acknowledgments
We declare no competing interests.
References
- 1.Kain T, Fowler R. Preparing intensive care for the next pandemic influenza. Crit Care. 2019;23:337. doi: 10.1186/s13054-019-2616-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020 doi: 10.1016/S0140-6736(20)30185-9. published online Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–259. doi: 10.1016/S0140-6736(09)60496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cabrini L, Landoni G, Oriani A, et al. Noninvasive ventilation and survival in acute care settings: a comprehensive systematic review and metaanalysis of randomized controlled trials. Crit Care Med. 2015;43:880–888. doi: 10.1097/CCM.0000000000000819. [DOI] [PubMed] [Google Scholar]
- 5.Hui DS, Chow BK, Ng SS, et al. Exhaled air dispersion distances during noninvasive ventilation via different Respironics face masks. Chest. 2009;136:998–1005. doi: 10.1378/chest.09-0434. [DOI] [PMC free article] [PubMed] [Google Scholar]


