A new Director-General of WHO will be selected in May, 2017. Richard Horton and Udani Samarasekera asked the six candidates competing for the position about their candidacy.
The forthcoming election of the next Director-General of WHO comes at a critical moment not only for the world's only multilateral health agency but also for the precarious trajectory of global health itself. WHO is often criticised for failing to live up to the expectations of the health community. Sometimes, as in the case of how the agency managed the early stages of the Ebola virus outbreak, that criticism is justified. But WHO plays a vital and successful, and frequently neglected, part in setting norms and standards for health in countries. It has a powerful convening role. And, should a Director-General choose to do so, the agency has unprecedented authority to offer leadership in health.
As the world enters a new era—that of the Sustainable Development Goals—the Director-General has an essential voice in shaping the meaning of health in an era of human dislocation, pervasive inequality, mass migration, ecological degradation, climate change, war, and humanitarian crisis. Six excellent candidates for Director-General are standing. All have wide experience in health, as one would expect, but each offers a very different platform. Some candidates have formidable international experience in global health. Others have forged their reputations nationally. Some have strong technical credentials. Others offer political skills. Some come from countries that should be WHO's greatest concern. Others are from nations that are traditionally seen as donors. Some have expertise in what might be considered the traditional agenda of global health (infectious diseases and women's and children's health). Others bring experience of newer concerns. This great diversity of candidates is a strength. It allows the Executive Board of WHO in January, 2017, and then the World Health Assembly in May, to select a candidate based on a clear diagnosis of the global predicament for health and the solutions needed. To help clarify their experience, visions, and ideas, we invited each candidate to offer a brief manifesto and to answer a series of ten questions to illuminate their positions on what we see as some priorities for the organisation.
Tedros Adhanom Ghebreyesus
Ethiopia

© 2016 Photo courtesy of Dr. Tedros Adhanom
WHO has helped improve the health of people across the globe. More children live to celebrate their fifth birthdays, more women survive childbirth and have access to family planning, and significant progress has been made against infectious diseases.
Yet despite progress, daunting challenges lie ahead. Globalisation has made it easier for infectious pathogens to spark global pandemics that threaten lives and economic security. Antimicrobial resistance is rendering previously treatable diseases deadly. Ageing and unhealthy lifestyles are leading to non-communicable diseases, while injuries and health impacts of climate and environment change present a danger. Mass population movements also lead to global health challenges.
I envision a world in which everyone can lead healthy and productive lives, regardless of who they are or where they live. Achieving this vision and the Sustainable Development Goals requires a strong, revitalised WHO that is effectively managed, adequately resourced, results driven, and led with political acumen. We need a WHO that belongs to all of us equally, puts people first, and ensures health is at the centre of sustainable development efforts.
As Director-General of WHO, I would focus on five priorities:
-
(1)
Transforming WHO into a more effective, transparent, and accountable agency that is independent, science and innovation based, responsive and harmonised, with a shared vision at the headquarters, regional, and country levels. WHO has to strike a balance between bold reform and organisational stability to deliver results;
-
(2)
Advancing universal health coverage and ensuring all people can access the services they need without risk of impoverishment. This includes driving domestic resources for health, strengthening primary health care, and continuing to expand access to preventive services, diagnostics, and high-quality medicines for diseases like HIV, tuberculosis, malaria, diabetes, heart and chronic respiratory diseases, cancer, and mental health conditions;
-
(3)
Strengthening the capacity of national authorities and local communities to detect, prevent, and manage health emergencies, including antimicrobial resistance, and promote global health security;
-
(4)
Putting the wellbeing of women, children, and adolescents at the centre of the global health and development agenda and positioning health on the gender equality agenda;
-
(5)
Supporting national health authorities to better understand and address the health effects of climate and environmental change.
As Ethiopia's former Minister of Health and through my leadership at various global health initiatives, I have learned what it takes to create real and sustainable change. I led the revitalisation of weak health systems at Ethiopia's national and community levels; mobilised unprecedented human and financial resources; and catalysed large-scale responses to health emergencies. As Minister of Foreign Affairs, I have gained experience and skills in high-level political engagement, including with Heads of State, and played key roles in resolving conflicts and advancing regional integration. Last year, I helped find common ground between parties with polarised positions to forge the Addis Ababa Action Agenda for financing sustainable development.
My vision for WHO and for global health is ambitious, but achievable—and I am confident that I have the political and public health leadership skills, experience, and determination to deliver results.
(1) What would be your priorities as Director-General of WHO?
Tackling the biggest health challenges of the 21st century will require innovative solutions that defy “business as usual.” WHO will need to broaden and intensify its engagement with a wider range of stakeholders across the public, private, and civil society sectors. The agency should attract and retain global talent to make it more diverse and inclusive—and to ensure it has the expertise to lead from the front and the centre.
WHO must work with governments to build their national capacity for universal health coverage. Strong, resilient health systems—including infrastructure, workforce, and information systems—are essential to driving good health for all. It is through these systems that children are vaccinated, pregnant women receive antenatal care, and patients with HIV, tuberculosis, malaria, and other communicable diseases receive their treatments. It is also through these systems that diseases like heart and chronic respiratory diseases, diabetes, cancer, and mental health conditions can be prevented, detected early, and managed. WHO must also place women, children, and adolescents—alongside other vulnerable populations—at the centre of its work.
Finally, we must strengthen WHO's response to emerging threats, including disease outbreaks like Ebola, Middle East respiratory syndrome, and Zika, as well as the health effects of climate and environmental change. WHO must work to harmonise emergency responses across partners while bolstering front-line defences at the national and local levels.
(2) WHO cannot do everything. What should WHO not do?
WHO should not consider other global health players as competitors and should not do what others can do better. There are many players working to improve public health globally across government, private sector, civil society, and academia—what I like to call the extended WHO family. The health issues of today—such as non-communicable diseases, antimicrobial resistance, and health security—must be addressed across all sectors, not just the health sector. All partners have a role to play. For its part, WHO should act as a leader and a convener, directing collective efforts toward shared goals, ensuring that everyone is playing to their strengths, and preventing duplication of efforts.
(3) What are the three biggest threats to the health of peoples across the world?
In my opinion, the biggest immediate threat to health is inequitable access to basic health coverage around the world. An estimated 400 million people, many of them women and children, lack access to essential health services. Without ensuring this critical, basic level of coverage—including a strong health workforce and access to medicines—we cannot have a healthy and prosperous world.
Secondly, antimicrobial resistance and health emergencies, including infectious disease outbreaks, pose unprecedented threats. The Ebola crisis in west Africa showed us the dangers of being unprepared for such emergencies, and the Zika outbreak further highlights the need to invest in basic research on the human and environmental health nexus, better surveillance, and new vector control tools. Further, as the microbes that cause diseases like tuberculosis, malaria, syphilis, and gonorrhoea become increasingly resistant to current treatments, we move closer to a world in which we are no longer able to effectively treat everyday infections—threatening to set back a century of progress.
Thirdly, health impacts of climate and environmental change pose a long-term threat, including potential rises in communicable, non-communicable, and vector-borne diseases. Climate change and variations also impact many aspects of life that are inextricably linked to health, including food security, economic livelihoods, air safety, and water and sanitation systems.
(4) What would you do to tackle those threats?
Through inclusive, engaging, and decisive leadership of WHO, I plan to address these threats by:
-
(1)
Helping countries expand their health coverage and protect hard-won gains—particularly as they tackle the dual burden of communicable and non-communicable diseases—and bolstering WHO's work to provide technical guidance. As countries identify unique strategies for strengthening their health systems, WHO should continue to provide technical support and guide national governments on building resilient health infrastructure, workforces, and information systems. While increasing our focus on emerging threats, including non-communicable diseases, health emergencies, and health impacts of climate and environmental change, we must also continue to improve maternal and child health and maintain a strong focus on HIV, tuberculosis, malaria, and eradication of polio;
-
(2)
Ensuring strong, coordinated, and rapid global responses to health emergencies, including antimicrobial resistance. This includes working with countries to ensure the implementation of the International Health Regulations and strengthening WHO's capacity to lead and foster multisectoral collaboration. We must bolster our front-line defence against public health threats by supporting the development of robust health systems, particularly at the primary health-care and community levels, that can prevent disease outbreaks or identify them early, when they can most easily be contained. WHO must champion a “One Health” approach and work with partners across the human and animal health and environmental sectors to coordinate a much bolder global response to antimicrobial resistance. This begins with following up on the commitments Member States made at last month's United Nations General Assembly meeting on antimicrobial resistance. We must also ensure developing countries have access to the newest medicines as they are developed;
-
(3)
Promoting evidence-based decision making and awareness for preventing, mitigating, and responding to the health impacts of climate and environmental change. We must develop transformative new policies and innovations, as well as community-based and multisectoral approaches, to meet these emerging challenges. We must also ensure that efforts to better understand and combat the health effects of climate and environment change are well financed.
(5) What does sustainable development mean to you, and how can WHO make the greatest contribution to the Sustainable Development Goals?
Sustainable development is about making investments that help people lead healthy and productive lives and, in the long term, create well-functioning communities and robust economies. It cannot be achieved without good health. When people are healthy, they are productive, and entire families, communities, and nations thrive. I saw the ripple effect of good health first-hand when I was Minister of Health of Ethiopia. Even with limited resources, we invested in critical health infrastructure, expanded the health workforce, and initiated pioneering financing mechanisms. These reforms helped provide tens of millions of Ethiopians with access to health services, setting us on a path to achieve ambitious health—and broader development—targets and sustain and build on our successes for years to come.
I believe the world's commitment to sustainable development—enshrined in the Sustainable Development Goals (SDGs)—offers a unique opportunity to improve the lives of people everywhere. WHO must work alongside governments and regional organisations—in close collaboration with civil society, private sector, other UN agencies, donors, and other key stakeholders—to drive the implementation of the health objectives of the SDGs and help countries achieve their targets by 2030.
(6) WHO lost credibility over its handling of the Ebola virus outbreak. What must WHO do to rebuild the trust of governments and their citizens?
After the Ebola crisis, WHO launched serious reforms aimed at improving its ability to respond more rapidly and effectively to public health emergencies, whenever and wherever they may arise. I will implement those reforms with a sense of urgency to build confidence among governments and their citizens that we are committed to being the world's foremost technical and political leader on public health emergencies. I will focus on building systems that allow WHO to rapidly deploy resources and scale up to the appropriate level of response, as well as on creating flexible and reliable funding mechanisms to ensure that WHO's ability to pay never hinders its ability to respond. I will continue our work with governments to implement the International Health Regulations so health systems are in place to detect disease outbreaks early, when they are easiest to contain. With this focus on quick wins and medium-term and long-term results, I am confident that we can regain trust around the world.
(7) Does WHO need further reform? If so, what reforms would you implement?
To deliver results, we need a strong, effective WHO that works together at all levels—from Geneva to regional offices and national capitals to local communities. Reforming the organisation will require vigilance, adaptability, and continual reflection.
I am committed to reviewing and refining WHO's ongoing governance and managerial reforms. Striking a balance between reform and stability of the organisation, I will specifically focus on the following areas to deliver results: enhancing the predictability and flexibility of WHO's financing; attracting and retaining the best talent from all parts of the world by creating an engaging and motivating environment; fostering innovation; and improving institutional effectiveness, transparency, and accountability. I will seek innovative partnerships with state and non-state actors, as I strongly believe that effectively tackling the health threats of our time requires united forces.
(8) What are the biggest threats facing WHO in the next 5 years? How will you address these threats?
One of the biggest challenges the WHO faces is the lack of flexibility and predictability of its funding. The annual budget of the organisation is smaller than single medical centres in big economies, and much of its funding comes from voluntary, earmarked contributions. We must be more strategic with what has already been committed, with a focus on value for money, while also pursuing innovative financing solutions and dialogues with Member States and key non-state contributors. I will also establish an Inter-Ministerial Advisory Commission—composed of Ministers of Health, Finance and International Development—to solicit advice, innovative solutions, and recommendations on assessed financial contributions from Member States.
Another challenge is the difficulty of predicting health emergencies and public health threats and of ensuring the agency is prepared to mount rapid and appropriate responses to these threats. This is an area where WHO has begun implementing reforms, as evidenced by its new Health Emergencies Programme, which aims to help countries prepare for, prevent, respond to, and recover from emergencies quickly. I will implement and independently monitor this new programme, while engaging with new mechanisms like the recently established Global Health Crisis Taskforce.
In addition, WHO must attract and retain the best talent and determine the appropriate mechanisms for doing so inclusively. I plan to review, nurture, and refine WHO's ongoing governance and managerial reforms to create an engaging and motivating environment for staff. I will also bring my open-door approach to management to encourage transparency, communication, and collaboration across all levels of WHO.
(9) Should WHO be a leader in health or should it only respond to the wishes of Member States?
WHO has to do both. These roles are not mutually exclusive. WHO should respond to the requests of Member States based on their health priorities and needs. In addition, WHO and its Director General should also proactively put forward a vision that mobilises Member States and other stakeholders, including civil society and the private sector, to ensure the health of people everywhere.
(10) What unique skills would you bring to the job of WHO Director-General?
My career has given me a unique mix of political leadership experience and hands-on public health experience. Because I have worked at all levels—from the community to the highest levels of national and global governance—I understand the challenges faced at the local level and the changes that must be made at the national and global levels to address them and deliver results.
As Ethiopia's Minister of Health, I learned first-hand what it takes to revitalise a weak health system with limited resources. We created 3500 health centres and 16 000 health posts to improve access to basic health care across the country. We trained and deployed 38 000 health extension workers at the community level—a model that has been replicated in more than a dozen countries across Africa. We built 30 new medical schools, leading to a 20-fold increase in the number of doctors trained each year. And we tackled stock-outs of essential medicines, transformed weak information systems and poor health data collection, increased country ownership of health programmes, and encouraged more effective donor harmonisation. Together, these successes helped Ethiopia dramatically expand access to health services and meet ambitious health targets. Notably, we reduced child mortality by two-thirds, maternal mortality by 69%, HIV infections by 90%, malaria mortality by 75%, and mortality from tuberculosis by 64%.
Through my engagement with global health initiatives, I have also gained invaluable experience in global health diplomacy. For example, as Chair of the Global Fund's board, I provided oversight on the organisation's comprehensive reform agenda. As Minister of Foreign Affairs, I brought together 193 UN Member States to agree to the Addis Ababa Action Agenda at the Third International Conference on Financing for Development in July, 2015. This was an historic milestone, forging a global partnership to achieve and finance the SDGs, including those related to health. In 2013, as Chair of the Executive Council of the African Union, I spearheaded the drafting of Agenda 2063, a global strategic framework aimed at accelerating Africa's economic, political, and social development through regional cooperation and solidarity. I also played a key role in resolving regional conflicts and overcoming political and cultural tensions that once impeded collaboration.
I am proud that my candidacy for WHO Director-General has been endorsed by the African Union. I am confident in my ability to lead WHO in a new era and serve as a champion for the health of all people, regardless of who they are or where they live.
Flavia Bustreo
Italy

© 2016 University of Essex
The greatest injustice of our time is that millions of adults, adolescents, and children around the world die unnecessarily from preventable causes for which there are evidence-based interventions. Millions more fail to reach their full potential for health and wellbeing, which also constrains their contributions to social and economic development. Many of the millions of refugees and internally displaced people in the world do not have access to basic services. Where is the equity for these people? Where is their human right to the highest attainable standard of health, as enshrined in the WHO Constitution and numerous human rights treaties?
In my life, I have been inspired by the transformative power of science, knowledge, and international partnerships in WHO's work that eradicated smallpox by 1980 and halved preventable maternal and child mortality during the Millennium Development Goals (MDGs). The collaborative efforts of WHO and partners have pushed through life-saving innovations such as the first-generation Ebola vaccine, and established the landmark WHO Framework Convention on Tobacco Control. We now have to channel this power to address critical inequities to realise the central promise of the Sustainable Development Goals (SDGs)—leave no one behind.
I can summarise my vision for WHO's work in five words: Equity, Rights, Responsiveness, Evidence, and Partnership. Five words, but charged with so much meaning and power for global health.
If we are serious about achieving SDG 3 through universal health coverage, we must unite around equity and rights, and use WHO's unparalleled convening power to bring together the scientific evidence and mobilise global partnerships. This will enable WHO to be more responsive to countries' needs related to current and emerging health threats, including non-communicable diseases and antimicrobial resistance. Most importantly, it will drive a sustained response to disease outbreaks and humanitarian emergencies, which deprive the most vulnerable of their health and their dignity. Currently, health has become an issue no national government can address alone, as the Ebola epidemic and increased migration have so acutely demonstrated. Global health security begins with intense surveillance in the most remote corners of the world, able to detect the appearance of new pathogens or the mutation of existing ones, but is only possible if governments collaborate with WHO to share the findings of this surveillance and act together in a WHO-coordinated response.
Fortunately, much of this is already beginning to happen. In my role as Assistant Director-General, Family, Women's and Children's Health at WHO, I worked closely with colleagues at WHO and the Office of the High Commissioner for Human Rights to set up the High-Level Working Group on Health and Human Rights, and will continue to support its work whole heartedly. The WHO Health Equity Monitor team working with global partners have developed resources to help countries assess inequalities and incorporate the results into planning. I was privileged to play a leading role in the collaborative effort to develop the Global Strategy for Women's, Children's and Adolescents' Health (2016–2030) launched by the UN Secretary-General and world leaders as a frontline implementation platform for the SDGs. With its predecessor strategy and accompanying Every Woman Every Child movement, it is one of the most powerful global health initiatives—raising more than US$60 billion since 2010, with multi-stakeholder efforts contributing to the unprecedented progress to end preventable mortality and promote health and wellbeing. And we can all see the huge potential in the landmark climate change agreement in Paris, where WHO's work with partners on the scientific evidence helped mobilise political commitment to explicitly recognise the links between climate change, equity, and the right to health in the agreement.
We need much more of this kind of concerted, high-level collaboration to embed equity and rights, responsiveness, evidence, and partnership at the core of global health and WHO's work. I am very proud that the Government of Italy presented my candidature for WHO Director-General so this can happen under my leadership for the benefit of the health and wellbeing of people in all countries.
(1) What would be your priorities as Director-General of WHO?
We need to drive progress towards achieving the health SDG as a cross-cutting driver of sustainable development, enhancing policies in other sectors that are crucial determinants of health and to which health contributes, for example education, energy, water, sanitation and hygiene, and infrastructure development.
We must expand universal health coverage for proven, evidence-based health interventions, building on the progress in HIV, malaria, tuberculosis, and MDG 4 and 5, with tools for assessing and treating newer global health priorities such as cancers and NCDs.
We must drive the reform of WHO to more effectively support Member States as they respond to health emergencies and outbreaks, such as the devastating Ebola outbreak, Zika, yellow fever, and the new threats of antimicrobial resistance.
We must address the impact of climate change on the health of citizens, mediated through the changing patterns of diseases vectors, disruption in access to food, safe water, and clean air. And make WHO, and the health sector as a whole, carbon neutral.
We need to prioritise the health of women, children, and young people everywhere—especially to reduce the impact of ill health due to migration and crises—improving their nutrition and wellbeing across the life course and addressing remaining gaps such as stillbirths.
We must maximise efforts to achieve equity using a human-rights-based approach in health and sustainable development.
(2) WHO cannot do everything. What should WHO not do?
WHO should not try to duplicate the functions of its Member States that are represented on the organisation's governing bodies by ministries of health. Countries should assess their own health needs and develop and implement their own plans to strengthen health systems and improve the health of citizens; the role of WHO is to support Member States in these efforts. WHO should lead global health and bring together all stakeholders, without duplicating what others can do.
(3) What are the three biggest threats to the health of peoples across the world?
At macro level the three biggest health threats are: (1) epidemics and humanitarian emergencies, which compound poverty and the striking inequities in income and social status across the world; (2) the slowness of the international community, to date, in recognising and addressing the strong links between ill health and climate change; (3) overlooking the demands and contributions of demographic changes in countries, most notably due to population ageing.
(4) What would you do to tackle those threats?
To respond to epidemics and humanitarian emergencies, WHO has currently embarked on significant reforms to become more operational, coordinate centrally in one programme, and strengthen surveillance and adherence to the International Health Regulations by Member States. I will advance the reform aggressively, adjusting to the findings of evaluations and maintaining a constant vigilance on the emergence of new threats and pathogens, such as antimicrobial resistance and the Zika virus.
In 2015, the WHO Executive Board endorsed a new work plan on climate change and health. We need to implement and further develop this work plan to ensure health is properly represented in the climate change agenda and to raise awareness of threats that climate change presents to human health. We also need to coordinate reviews of the scientific evidence on the links between climate change and health, and develop a global research agenda. Member States are working to reduce their health vulnerability to climate change, and to promote health while reducing carbon emissions; WHO must play an important role in supporting this activity.
Comprehensive public health action and investment to address population ageing is urgently needed around the new concept of functional ability (which is a product of a person's intrinsic physical and mental capacities and their interaction with environmental factors). Making these investments will have valuable social and economic returns, both in terms of the health and wellbeing of older people and in enabling their ongoing participation in society.
(5) What does sustainable development mean to you, and how can WHO make the greatest contribution to the Sustainable Development Goals?
The SDGs provide an opportunity for WHO to act on what the recent evidence clearly shows—that health and sustainable development are closely inter-related. Health contributes to social and economic development and other sectors contribute to health. WHO needs to amplify its ongoing work within health and with other sectors to tackle shared challenges and achieve common goals.
Sustainable development is self-perpetuating. In health terms, that means that every health intervention or programme should not only deliver benefits today, but also into the future. In the past, this is where the health community has often failed, saving a child's life with timely intervention during childbirth, but then not doing enough as that same child fell ill from a lack of essential nutrition or vaccines. Assuming the same child survived, they may have developed habits in adolescence that are associated with the burden of non-communicable diseases in adulthood, and may have experienced the lack of universal health coverage to support their healthy ageing. In this way, millions of people irretrievably lose the opportunity to achieve their full potential for health and wellbeing across their life.
A sustainable approach to health requires integrated health care across the life course, with support from sectors outside the health sector—such as water, sanitation, education, and finance—which can help create an enabling environment for health (a key ingredient for sustainability). This will entail a massive amount of cooperation between multiple partners and stakeholders. As WHO is ideally situated to facilitate and improve global cooperation on health, its greatest contribution to the SDGs may be as a facilitator of coordinated multi-stakeholder action.
(6) WHO lost credibility over its handling of the Ebola virus outbreak. What must WHO do to rebuild the trust of governments and their citizens?
The experience from the Ebola outbreak has highlighted the weaknesses of health system capacity in the three countries mostly affected, Guinea, Liberia, and Sierra Leone, but also the slow global response to prevent further spread of the outbreak. As noted earlier in answer 4, WHO has currently embarked on a significant reform to become more operational, coordinate centrally in one programme, and strengthen surveillance and adherence to the International Health Regulations by Member States. I will advance the reform aggressively, adjusting to the findings of evaluations and maintaining a constant vigilance on the emergence of new threats and pathogens, such as antimicrobial resistance and the Zika virus.
(7) Does WHO need further reform? If so, what reforms would you implement?
Further reforms are essential. WHO needs to get better at responding to health issues as they emerge and to the opinions and needs of the people it serves, and to become a more effective, transparent, and accountable organisation, with streamlined decision-making processes. Looking outwards, it needs to drive support for innovation and research—including through its normative standard setting function—in medical science, technology, policy, business, the social sciences, and health financing. It must strive to create an enabling environment for innovation and health by helping to match innovation to global health needs and mitigating the risks of innovation investment through forward-looking partnership models with Member States, the private sector and others, without compromising its integrity.
WHO's function as a knowledge provider and facilitator needs strengthening. The organisation must meet the knowledge needs of countries by facilitating global knowledge sharing and evidence synthesis and response to policy needs. And it needs to expand its own knowledge base, for example by understanding the changing funding landscape for the achievement of the highest attainable mental and physical health for citizens, especially the growing role of in-country financing.
(8) What are the biggest threats facing WHO in the next 5 years? How will you address these threats?
The biggest threat to WHO is that it fails to respond to the changing needs of Member States and their citizens. For example, low-income and middle-income countries are increasingly aiming to develop domestic sources of health funding. WHO needs to understand how this will change the global health landscape. To support WHO Member States in identifying and responding to epidemics and other public health threats, in the most effective and timely way possible, WHO needs to marshal its technical support across departments and set up strategic partnerships with other agencies and partners.
(9) Should WHO be a leader in health or should it only respond to the wishes of Member States?
WHO comprises both Member States and the secretariat. In my experience, Member States want WHO, as a collective, to provide leadership to implement the organisation's mandate in health, and to address health challenges that no single Member State can. This requires collective action, which Jamison et al. define as “an economically rational approach to provision of public goods from which all can benefit…international collective action responds to opportunities of which benefits cover many nations”. However, this is not to say that WHO should dictate to individual Member States. Rather it should use its unique capacity as a global convenor to generate consensus on which to base collective action. WHO should always bear in mind the priorities and wishes of Member States and their citizens, and their sovereign right to decide how national health policy is implemented.
(10) What unique skills would you bring to the job of WHO Director-General?
My unique position as the only WHO internal candidate is one of the key strengths as a candidate for the role of Director-General, and through my extensive work with governments and multi-stakeholder partnerships also clearly perceive global health issues from perspectives outside the organisation too. I believe that these twin perspectives are necessary to effectively lead WHO.
As the only WHO internal candidate, I bring in-depth management experience and extensive knowledge of the organisation—the pitfalls and dynamics and the strengths and weaknesses—and have driven reforms and innovation, mainstreaming of gender, equity, and human rights across the entire organisation. I have supported and collaborated closely with WHO staff, our most precious assets, hired real talents in the leadership of my team, and have demonstrated the ability to raise significant financial resources (my cluster is the best funded in WHO).
In addition, my experience as medical doctor and epidemiologist working in many countries, as well as the close engagement in multi-stakeholder partnerships, gave me the opportunity to learn how to clearly perceive global health issues from the perspective of external partners.
As a medical doctor and epidemiologist, I acquired first-hand experience of public health in numerous settings, including post-war, epidemics and outbreaks, and internal and external migration. I have contributed to setting up surveillance systems to detect pneumonia and diarrhoeal diseases in countries of the former Soviet Union, as well as the first global antimicrobial surveillance for drug resistance tuberculosis in the world, and response to meningitis and cholera outbreaks in Sudan.
Partners have valued my leadership skills to build partnerships, such as the creation and leadership of the Partnership for Maternal, Newborn and Child Health (PMNCH), and achieve consensus in complex, multi-stakeholder and multi-country contexts, and appreciated my political vision that has helped set far-reaching agendas for health, without settling for a minimum common denominator.
I have had the honour to work with the highest level of governments, presidents and prime ministers, ministers of health and finance, parliamentarians, to forge for example the G7 Muskoka initiative in 2010 and the African Union initiative on women's and children's health. My jobs outside of WHO—for example at the World Bank, at Gavi, and as an adviser to the Prime Minister of Norway—have given me a clear understanding of the arguments needed to prioritise investments in health and health systems both domestic and internationally. I have a track record of achieving increased political and financial commitments and setting up systems for accountability and transparency. These accomplishments have also been characterised by advocacy for greater participation of civil society, such as the Citizen Hearings for women's and children's health, and especially greater youth engagement in decision making for health.
I have been closely engaged with the scientific community and media through publishing in the medical, political, and foreign affairs journals, as well as in the mainstream media and social media from The Lancet to the Hindustan Times. In addition to almost 100 peer reviewed articles in leading scientific journals, book chapters, I have a regular blog with Huffington Post and a vibrant Twitter following.
In conclusion, I have proven unique skills and experience to harness the power of evidence and advocacy to mobilise political commitment and resources for health. I am honoured to put these skills and experience at the service of the global health community to take on this new challenge and to ensure that WHO can achieve the international commitment to the right to the highest attainable standard of health for all people.
Philippe Douste-Blazy
France

© 2016 Stephane Cardinale-Corbis/Contributor
As a candidate for Director-General of WHO, I wish to see WHO effectively fulfilling its mandate as the leading organisation in global health and consistently promoting health not only as a human right, but as the right choice for governments in a world of competing demands and interests. As Director General, I will be dedicated to working within the global system to finance and promote pragmatic, long-term solutions to the root causes of poor health and inequality, and to ensuring that action on health is a major driver of progress towards sustainable development as a whole.
My vision for WHO is focused on three goals: reform, responsiveness, and results.
My reform agenda will begin with the development of a comprehensive organisational vision and strategy negotiated with Member States. This will ensure that WHO is focused on the most important challenges in global health today and has coherent plans to address them. Secondly, the organisation must function more cohesively, with continuous dialogue and clear lines of accountability between the Director-General, Regional Directors, and country offices. This cohesiveness can be achieved through strong political leadership and technical proficiency from headquarters, supported by more explicit delivery agreements between different levels of the organisation. Thirdly, WHO must be more proactive and strategic in its fundraising to ensure that it has more predictable and sustainable funding. Drawing upon my experience in innovative financing for development, I will work to develop new sources of revenue that supplement Member State contributions and non-core funding to support the essential, core functions of WHO.
Under my leadership, WHO will demonstrate a strong culture of responsiveness, especially with regard to health emergencies, drawing upon the difficult lessons of Ebola and other recent health crises. The world cannot afford and will not tolerate a WHO failure in this core area of its mandate. The Health Emergencies Programme (HEP) must be quickly scaled up, with clear lines of authority, effective functional links with other parts of the organisation, and a commitment to continuous learning and improvement. While the HEP is a major priority in creating a more responsive WHO, the organisation must exhibit a culture of responsiveness in all its work, including its action on non-communicable diseases and their social and environmental determinants, as well as its efforts to tackle new challenges posed by the HIV, tuberculosis, and malaria epidemics.
WHO must be more consistently focused on results. Its resources must be clearly directed to the global health priorities agreed to by Member States and the organisation needs to more consistently demonstrate that it is achieving impact. This can be done by ensuring a stronger emphasis on value for money, strengthening performance and management data, and linking the budget more closely to results and impact.
Finally, WHO must be focused on its core responsibilities at global and country levels. Its essential roles at the global level are to convene multiple stakeholders (including civil society and the private sector), build strong alliances to improve health outcomes and address the social, economic, and environmental determinants of health—especially for the poorest and most vulnerable—and to develop consensus on health policies, norms, and standards. At the country level, WHO must continue to be the organisation that Member States respect and depend on for the highest standards of evidence-informed guidance and advice, based on country needs and promoting country ownership.
As a physician and an experienced public sector manager and political leader, I believe I am well equipped to provide the leadership that will restore and maintain WHO's essential role in global health.
(1) What would be your priorities as Director-General of WHO?
As Director-General, I would specifically promote WHO leadership and action in the following five priority areas: (1) ensuring that WHO responds effectively to emerging and re-emerging infectious diseases; (2) tackling the unprecedented growth of non-communicable diseases; (3) bolstering health systems to implement universal health coverage; (4) increasing the availability, affordability and access to essential medicines; and (5) tackling the growing challenge of antimicrobial resistance.
Sustained attention to maternal and child health and increased attention to mental health will also feature prominently on my agenda.
(2) WHO cannot do everything. What should WHO not do?
WHO should remain an organisation that coordinates global health actors, develops consensus on health strategies, norms, and policies, and provides support to countries for their implementation. It should not itself act as an implementing or funding agency or engage in project management.
WHO should not impose on countries strategies or programmes that have been elaborated without their full participation, that are not likely to be funded, and/or that impose additional bureaucratic requirements on countries' health governance and systems.
Internally, WHO should avoid duplication of activities at different levels of the organisation and initiatives that are independent of the overall vision and strategy for the organisation that is agreed to by Member States. Clusters/departments should only be structured in such a way as to align with the organisational vision and strategy.
(3) What are the three biggest threats to the health of peoples across the world?
The three biggest threats to people's health globally are: (1) the persistent risk of emerging epidemics; (2) the increasing prevalence of non-communicable diseases, driven by social and environmental factors; and (3) diminishing global solidarity and attention to health and health commodities as global public goods, in the context of a globalisation that is largely market-driven and marked by growing global political tensions.
(4) What would you do to tackle those threats?
-
(1)
Scale up the Health Emergencies Programme and ensure that it has sustainable funding; strengthen surveillance and country and regional preparedness for disease outbreaks; integrate lessons from recent health crises; ensure strong coordination across the UN and effective partnership with non-government actors;
-
(2)
Ensure strong WHO leadership in response to NCDs with a clear recognition that over 90% of premature deaths from NCDs occur in low-income and middle-income countries; develop evidence based normative guidance with a strong focus on prevention and addressing major risk factors, including tobacco use and obesity; and
-
(3)
Provide strong political leadership to promote public health and access to medicines and other health commodities as global public goods within the context of universal health coverage, with a focus on building equitable, people-centred, and responsive health systems.
(5) What does sustainable development mean to you, and how can WHO make the greatest contribution to the Sustainable Development Goals?
Sustainable development is development that strikes an appropriate balance between different—and often competing—needs, while ensuring that all development efforts are as synergistic and mutually reinforcing as possible and that development efforts today do not compromise the choices available to future generations. Effective leadership by WHO within the sustainable development framework should not only focus on fighting diseases, promoting wellbeing, and strengthening health systems (SDG 3), but also link with and contribute to other key development goals such as progress against poverty, inequality, social exclusion, environmental degradation, and related determinants of health.
Key priorities for WHO in the context of the SDGs must include actively reviving mobilisation around global public goods that are key to sustainable development, implementation of universal health coverage, strengthening primary health care, and the effective implementation of the International Health Regulations. The SDGs also present an historic opportunity to further emphasise the importance of health within national development strategies and plans.
(6) WHO lost credibility over its handling of the Ebola virus outbreak. What must WHO do to rebuild the trust of governments and their citizens?
As noted in earlier responses, WHO must increase the effectiveness of its responses to health emergencies through fast and effective implementation of the Health Emergencies Programme. More generally, WHO must develop and promote a more strategic vision on health and serve as a tireless advocate for health in the face of competing interests. The organisation must continue to show leadership as the principal coordinating and convening body in health; support multi-stakeholder dialogue, including by showing increased openness to actors from civil society and the private sector; and remain the world's leading builder of consensus on evidence-based approaches and normative guidance.
(7) Does WHO need further reform? If so, what reforms would you implement?
As described in my overall vision at the beginning of this message, key reforms required are the development of an organisational vision and strategy negotiated with Member States; increased coherence and improved lines of accountability across the three levels of the organisation; more predictable and sustainable funding; and increased accountability through more effective linking of budget with performance, results and impact.
(8) What are the biggest threats facing WHO in the next 5 years? How will you address these threats?
The three biggest threats facing the organisation are: (1) loss of confidence in the organisation as a result of suboptimal performance and consequent decreases in funding; (2) institutional complacency and drift deriving from a lack of strategic vision and focus; and (3) as a result of (1) and (2), further fragmentation of the global health architecture.
As discussed in earlier responses, these threats need to be addressed by implementation of further reforms and development of a strategic vision and focus for the organisation negotiated with Member States.
(9) Should WHO be a leader in health or should it only respond to the wishes of Member States?
As the sole international organisation with universal legitimacy on global health, WHO should lead in developing a global vision to tackle the current and future challenges in global health. Political leadership and multi-stakeholder engagement are needed to build consensus among Member States and their citizens on that vision.
(10) What unique skills would you bring to the job of WHO Director-General?
As a former minister of both Health and of Foreign Affairs, I will bring the strong political and diplomatic leadership skills that are essential to WHO at this key moment in its history and I will consistently make the political case for health as an investment in sustainable development, rather than an expense.
As a former mayor of Toulouse, I have managed an annual budget of US$1·5 billion and 30 000 employees, comparable to the budget and exceeding the workforce of WHO. I will bring strong administrative and management experience to this role.
As the Founder and Chair of UNITAID and the UN Secretary General's Special Envoy on Innovative Financing for Development, I have contributed to creating the first source of innovative finance for health, and I will bring a history and practice of innovation to the leadership of WHO.
David Nabarro
UK

© 2016 Anadolu Agency/Contributor
Our world is challenged by a changing climate, violent conflict, persistent poverty, and mass migration. The benefits of globalisation and new technologies remain unequally shared. As a result, people face an ever-growing avalanche of threats to their health. I have worked on such issues for over 40 years. As I see it, the need for a robust, reliable, and responsive WHO has never been more urgent.
I am honoured to be presented as a candidate for the position of Director-General. All my professional life I have been working in public health—as a community-based practitioner, educator, public servant, director, diplomat, and coordinator. In the past 12 years, successive Secretaries-General of the United Nations have entrusted me to lead collective action on pressing and complex challenges—responding to avian and pandemic influenza, promoting food security, ending malnutrition, combating Ebola, promoting the 2030 Agenda for Sustainable Development, and advancing efforts relating to climate change.
I have the experience and skills needed to serve WHO as Director-General: I will focus on four key priorities:
-
(1)
Alignment with the Sustainable Development Goals (SDGs). The 2030 Agenda offers a clear roadmap for a more peaceful, equitable, and prosperous future within communities and nations. Health is central to the achievement of the SDGs. As a result of my experience in the last year I am ready to ensure that WHO is well positioned for this new era: I will encourage horizontal, cross-disciplinary, intersectoral working that yields measurable results;
-
(2)
Transforming WHO to respond to outbreaks and health emergencies. In times of outbreaks and health emergencies, WHO is expected to exercise leadership by providing unparalleled technical expertise, while empowering others to act. I have led inter-agency efforts to combat disease threats and outbreaks (including malaria, avian influenza, Ebola, Zika, and cholera). In 2015–2016, I chaired the Advisory Group on the Reform of WHO's Work in Outbreaks and Emergencies. I am committed to completing the work needed to solidify WHO's capacity to respond to outbreaks and health emergencies.
-
(3)
Trusted engagement with Member States. National authorities have the primary responsibility to promote the health of their people, but health objectives cannot be achieved without the full engagement of people and civil society, as well as decisive leadership and strong commitment from governments. WHO needs to be a trusted partner of all governments while holding itself to the pledge that world leaders themselves made in the 2030 Agenda to leave no one behind. I have consistently sought to engage with Member States in ways that are respectful and reliable, consistent, transparent, and accountable.
-
(4)
Advancing people-centred health policies. Ever since the Primary Health Care Movement in the 1970s, WHO has advocated people-centred policies for health. Implementation depends on there being spaces in which organisations working for people's health engage openly with other stakeholders. It calls for consistent attention to the capabilities and circumstances of care providers. I continue to champion the interests of all who work to sustain people's health everywhere—including within households, communities, work-places, health-care facilities, and institutions.
(1) What would be your priorities as Director-General of WHO?
As the Director-General of WHO, I would ensure that WHO can deliver in four areas: (1) alignment with the Sustainable Development Goals; (2) transforming WHO to respond to outbreaks and health emergencies; (3) trusted engagement with Member States; and (4) advancing people-centred health policies.
The 2030 Agenda for Sustainable Development—with its focus on equity, inclusiveness, and leaving no one behind—builds on the spirit of Primary Health Care, championed by WHO's Member States for four decades. WHO's contribution to the SDGs should include: enabling all people everywhere to attain the highest possible standard of health; continuing attention to health's economic, social, political, and environmental determinants; completing the unfinished work for the Millennium Development Goals; addressing the growing challenge of non-communicable diseases; and ensuring universal access to effective health services, medicines, technologies, and financial protection. In all my work within the UN system I have encouraged horizontal, cross-disciplinary, intersectoral working and have advocated whole of government and whole of society approaches that will be needed to address the SDG health agenda.
Ensuring capacity to prepare for and respond to disease outbreaks and health emergencies will always be a key priority of WHO. It must do this in ways that are predictable, robust, and reliable, and that reflect the interests of all nations and peoples. This will include developing national capacities in line with the International Health Regulations; encouraging strategic research and innovation; urgent strategic action on antimicrobial resistance; giving special attention to the needs of vulnerable and threatened communities—including those who seek to move and take refuge so as to escape suffering; and reinforcing effective global responses to severe health crises. I intend to complete the work needed to secure WHO's credibility as an organisation with both the normative excellence and the operational agility needed to lead responses to health crises.
When engaging with Member States, WHO should be seen as the strategic leader, innovator, catalyst, and convener for people's health. WHO should do this in ways that reflect both current realities and the needs of coming decades. This requires a culture that constantly heeds the interests and concerns of Member States and their people; that leads through empowerment and example, that engages with all other actors and thought leaders committed to promoting health and health equity, and that encourages all concerned to trust the effectiveness and responsiveness of WHO.
In advancing people-centred health policies, WHO should serve as a champion for the interests, wellbeing, and capabilities of all health-care providers. WHO should intensify efforts to ensure the effectiveness of health caregivers, encouraging skills development and competency testing, and protecting the interests (and physical safety) of all who sustain people's health in households, communities, workplaces, health-care facilities, and institutions.
Community engagement and inclusive partnering will be critical for each and every one of these priorities. I have seen the importance of community ownership and engagement in all my professional work. I have seen how Ebola eventually caused families to change how they buried their dead, and appreciated the heartache caused by this profound change of practice. I see how Zika now challenges women to reconsider when they become pregnant. These decisions on how a person comes into the world, how they leave it, and how they are supported when they are ill are the most intimate decisions people make and often reflect firmly-held belief systems. That is why people and their representatives (civil society, faith leaders, traditional leaders, and women's groups) need to be engaged, and listened to, whenever health policies are being shaped and implemented.
Inclusive partnering means engaging in broad coalitions and nurturing movements for transformative change. It will require transparent handling of multiple interests and encourage guaranteed and inclusive involvement of less powerful but vitally important stakeholders—be they small nations, minority groups, people with special needs, or those who are so often neither seen nor heard, and are often left behind.
(2) WHO cannot do everything. What should WHO not do?
Policy decisions as to what WHO should (or should not) do will be made by Member States. In principle WHO has to be prepared to help countries address any threat to their people's health. Situations will arise when WHO takes the lead on specific issues. But usually WHO provides technical support to national authorities as they address specific health issues: in these situations WHO may also serve as a catalyst, facilitator, or convener. This calls for strategic leadership that is both confident and effective—to define priorities, support those responsible for implementation, and establish the roles of different actors.
Global stewardship is important. It means drawing on the strengths of all of WHO. As Director General, I will encourage each of the levels of WHO to contribute according to their respective strengths, ensuring clear delineation of responsibilities and accountability for the use of resources. I will do this at all times in conjunction with the Regional Directors and their teams.
(3) What are the three biggest threats to the health of peoples across the world?
-
(1)
Poverty, inequality, and weak governance: people's health is undermined if they do not have reliable access to adequate income, nutritious food, water, sanitation, and shelter. These factors are further exacerbated when there is conflict, political instability, fragility, abuse of human rights, and inequitable economic growth. In combination, these factors contribute to the breakdown of basic health systems, a lack of basic needs, inadequate financial protection and—inevitably—a further spiral of ill health and poverty.
-
(2)
Existing and emerging infections: outbreaks of infectious disease undermine economies, society, and stability: hence the need to promote health security, and reduce risks due to HIV/AIDS, malaria, tuberculosis, diarrhoeal diseases, and other existing infections. With hotter temperatures, heavier rainfall, increased urbanisation, and changes in livestock production, patterns of disease incidence alter. This results in increased risks of people being affected by vector-borne and zoonotic diseases with epidemic potential.
-
(3)
Low priority for health and health care: if health not given sufficient attention in global, national, and local governance and policy making, people are more likely to face serious illness and to become poorer as a result. This can be the case when levels of investment in health are low or inequitable; when competing economic interests undermine health; when there is no cross-sectoral action for health or when there is insufficient investment in opportunities for physical activity and nutrition among young people. Such policy deficits can increase risks of illness arising from climate change and undermine efforts to address NCD risk factors. Challenges will be even greater if there is insufficient attention to the growing threat of antimicrobial resistance.
(4) What would you do to tackle those threats?
Three elements are critical—the 2030 Agenda, the One Health Approach, and political advocacy.
The 2030 Agenda offers a framework for establishing positive linkages between health and the other Sustainable Development Goals. It will be important for WHO to ensure that attention is paid to health when policy makers take decisions on how they deal with migrants, how to conduct war, how they regulate the environment. WHO will need to encourage and support an all of government approach, making sure that ministries of health are working alongside ministries of sanitation, social welfare, and security.
Similarly, the One Health approach focuses on the issues that emerge at the interface between animals, humans, and the ecosystems in which they live. This is evolving into the concept of planetary health that seeks to integrate human health within ongoing dialogues on climate-compatible economic growth, resilient livelihoods, sustainable infrastructure, the future of land and oceans, urbanisation, and industrial development. Examination of the connections within different settings quickly exposes immediate or potential opportunities for health improvement through action in sectors and disciplines other than health.
Finally, WHO will always need to be an advocate for health outcomes: elevating and maintaining health as a priority on political agendas at all levels. In recent years, political groupings such as the African Union, Association of Southeast Asian Nations, the European Union, the G7 and the G20, as well as the United Nations, have increasingly focused on health as a priority. It is important that WHO plays its part in such settings to explain, interpret and be ready to advance issues as leaders provide political impetus for health. Antimicrobial resistance was highlighted in this way at the 71st UN General Assembly in New York in September, 2016.
(5) What does sustainable development mean to you, and how can WHO make the greatest contribution to the Sustainable Development Goals?
Sustainable development, as set out in the 2030 Agenda for Sustainable Development adopted by Member States, provides a universal framework to be pursued by all governments, businesses, civil society, and individuals everywhere. It is the plan for our common future—for people, planet, prosperity, and peace through partnership. Implementation of this agenda—in concert with other multilateral agreements on disaster risk, financing for development, climate change, migration, and antimicrobial resistance—can be expected to have a dramatic impact on people's abilities to be healthy and to access care in case of illness. This is a result of the connectedness of the 17 goals, though is explicitly set out in Goal 3 with its emphasis on universal health coverage.
As discussed above, WHO's contribution to the SDGs should include: enabling all people everywhere to attain the highest possible standard of health; continuing attention to health's economic, social, political, and environmental determinants; completing the unfinished work for the Millennium Development Goals; addressing the growing challenge of non-communicable diseases; and ensuring universal access to effective health services, medicines, technologies, and financial protection.
(6) WHO lost credibility over its handling of the Ebola virus outbreak. What must WHO do to rebuild the trust of governments and their citizens?
The cultural, institutional, and organisational changes needed in WHO have been clearly set out in the report of the Advisory Group on Reform of WHO's Work in Outbreaks and Emergencies, a group which I chaired from 2015–2016. The changes suggested in this report have been internalised within WHO—and will be progressively reflected in the performance of country, regional, and headquarters offices. Implementation has started: it needs to be sustained in a continuous and consistent way with the support of the Independent Oversight and Advisory Committee that will provide recommendation on options for improvement. Over time, as new levels of performance are achieved and benchmarked, credibility and confidence will return, additional funds will be mobilised and WHO's contribution to outbreak prevention, preparedness and response, as well as in health emergencies, will reach the standard required by Member States.
(7) Does WHO need further reform? If so, what reforms would you implement?
Looking ahead, I see WHO as a magnet that attracts talented people, builds their skills over time and deploys them in ways in which they can be most effective. This is increasingly being achieved through skilful, empowered, and accountable managers at all levels of the organisation. I see WHO as an organisation that increasingly manages scarce funds creatively, transparently and with clear lines of accountability. I would also like to see these features of the organisation better advanced, appreciated and understood—within and outside WHO.
All multilateral organisations need constant transformation to ensure that their systems, priorities and processes are responsive to the changing political, technological, environmental, social, cultural and economic contexts of people's lives. I expect WHO to remain an active player in the transformation of the wider UN system in line with the 2030 Agenda for Sustainable Development, seeking ways to ensure the relevance of individual agencies as well as coherence of international systems as a whole.
There will be times when substantive transformation is needed to tune up a particular aspect of an organisation's performance. This occurred during the 2014–15 Ebola outbreak. WHO has been affected by the criticisms it received in relation to handling complex disease outbreaks. The flexibility and willingness of professionals inside and outside WHO—adjusting effectively to new ways of working—has shown that WHO can function as an organic and adaptable entity.
Member States will continue to debate ways in which the governance undertaken by the Executive Board and the World Health Assembly enables the Secretariat to be more effective and contributes to the global influence of the WHO as a whole. There will remain the constant challenge of aligning finance to desired outcomes. This will include ensuring that any trade-offs in ways resources are allocated reflect the interests of people who are at risk of ill health and for whom illness has the greatest consequences.
The Director-General is expected to steer the process of transformation, to affirm priorities and to encourage partnering when this can be helpful. When Director General I will encourage WHO personnel to develop the collective capabilities and confidence they need to see their organisation as a technical leader that contributes to better lives for everyone. WHO is now moving in the right direction: the challenge is to help all who are within or associated with it to recognise the contributions they make. They should come to appreciate that although these contributions are never as great as they would wish, they should be confident that they are organising and partnering in ways that have substantial impact for people in many different places. Through their inspiration and example, I expect that WHO senior managers will continue to lead the process of transformation, and be partners with the Director General in achieving even more.
(8) What are the biggest threats facing WHO in the next 5 years? How will you address these threats?
It is likely that WHO will experience five major threats to its effectiveness.
-
(1)
Finance: with significant fixed costs, the effects of inflation and a static budget, it is difficult to increase both efficiency and effectiveness without any reduction in the tasks being undertaken. Dependence on specified voluntary contributions is inevitable, though it is important to ensure that these do not encourage the organisation to pursue activities that might be better carried out by others or that divert resources from higher priority activities that are less well-funded. The financing reforms initiated by the current administration, which focus on alignment, transparency, and impact, are moving in the right direction and should be sustained.
-
(2)
Locating and employing strategic leaders: WHO continues to depend on its human resources—maintaining a diverse pool of highly skilled and experienced experts who have the skills needed to work effectively with Member States. Volatile voluntary funding inevitably leads to widespread use of short-term hiring arrangements: this makes it difficult for managers to maintain these pools. Innovative means for accessing experts from national institutions (with appropriate geographical balance and diversity) should be sustained, with care to ensure they function within the WHO culture, norms, and operating procedures. Being a WHO staff member needs to be synonymous with both technical excellence and the ability to work effectively with national authorities.
-
(3)
Maintaining space for interaction, handling multiple interests, and sustaining integrity: multiple stakeholders are involved in global health. They include civil society networks, individual NGOs at international, national, and community level, professional associations, the media, think tanks, national and transnational corporations. They also now include articulate individuals and informal communities of advocates with strong voices and novel influence thanks to information technology, social media, and organisational skills. While this is a welcome development, this multiplicity of actors engage with WHO because they seek to influence decision making. This can be challenging both for WHO's Member States and for the Secretariat.
-
(4)
Governance: it is important to ensure the primacy of WHO's governors, the Member States, when policy decisions are made. It is also important to ensure that the expertise and independence of the Secretariat are protected when standard setting work is undertaken. And, given the increasing significance of multi-stakeholder working, it is important that safe spaces exist for all parties to interact. These spaces should enable the inclusion of those who might lack the power they need to ensure their voices are heard and presence is felt. I have substantial experience in partnering and fostering movements and appreciate the careful balance that is required to benefit from the work of multiple stakeholders, while maintaining the independence of the technical and normative functions that need to be undertaken from within the UN system.
-
(5)
Novel threats: the global health community has learnt to anticipate unexpected threats—whatever the cause. The transformation of WHO's work in outbreaks and emergencies will lead to a more predictable, agile, and effective capacity for action. This will always involve WHO working with other entities in ways that reflect comparative advantages. When an incident occurs and a response is triggered, pre-planned procedures should engage a broad range of operational entities, strategic partners and international political actors at the highest level. It is now well-recognised that simulations involving critical experts from within government, UN, NGOs, scientists, business, and media are invaluable. Results must be shared with world leaders at regular intervals so that they can appreciate states of readiness and institute necessary system changes to ensure that they are able to contain extreme threats to people's health and global stability.
(9) Should WHO be a leader in health or should it only respond to the wishes of Member States?
As strategic leader for world health, WHO needs to appreciate and be responsive to the needs of Member states and their people. This means that WHO needs to support national governments in the pursuit of health objectives, providing excellent technical advice, identifying gaps in national capacities, and engaging in political advocacy to ensure such gaps are addressed. At the same time, just as world leaders pledged to leave no one behind when they adopted the 2030 Agenda for Sustainable Development, WHO must strive to listen and respond to all stakeholders, ensuring that the most vulnerable and those that are hardest to reach have access to quality health services.
In this context leadership is vital: it must be both strategic and sensitive. WHO's health leaders need to use diplomatic skills to broker constructive agreement and avoid gridlock when national interests diverge. They need to make it clear at the highest levels of government when States fail to honour international regulations in ways that impact on the health of their own or other populations. They need to use the power of evidence to hold up a mirror to states' performance. They should be ready to champion issues that are vital to the right to health while recognising that for some members these may be controversial. They must be able to accept criticism and acknowledge that their judgments will be questioned.
(10) What unique skills would you bring to the job of WHO Director-General?
I have extensive experience from work within communities in southeast Asia, east Africa, the Middle East, and Latin America. I have led a range of health and development initiatives, always analysing them from the perspective of their impact on the wellbeing of people, their households and their territories. I know the major organisations and players in global health, and have worked with many of them since their foundation. I have worked in senior positions within WHO and have experience of transforming work on outbreaks and emergencies. I offer a safe pair of hands in crises and am effective at bringing different actors together so they work in synergy. I have developed the ability to work with world leaders in fostering partnerships and collaborative environments through which diverse interests and actors come together in pursuit of common goals and measure their achievements. I enjoy that aspect of my work very much indeed.
My leadership within WHO has included roles on malaria control, environmental health, health emergencies, and the office of a previous Director-General. I understand the challenges of managing transformation in WHO and know that success calls for working effectively across all levels and elements of the organisation in ways that enable all to contribute effectively. I have senior management experience within a major donor government and understand the world of bilateral development agencies. As an adviser to successive Secretaries-General, I have become familiar with many aspects of the UN system and ways in which it can contribute to advancing personal, community, national, and international health. One of my main responsibilities over the past year has been to work with the heads of all the entities in the UN system as they work together for the Sustainable Development Goals and act on climate change. As Director-General, I will build on these relationships and seek to increase the extent to which the entire UN system focuses on people's health.
Sania Nishtar
Pakistan
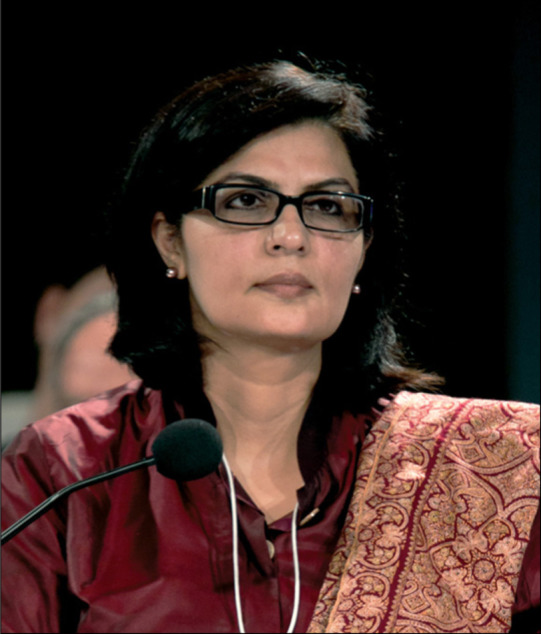
© 2016 Benedikt von Loebell
As WHO nears its 70th anniversary, the mood is not yet celebratory. While some Member States still express support for and confidence in the organisation, others openly debate WHO's merits and consider the case for its continued survival. In a world brimming with unprecedented opportunity for health improvement, WHO faces structural limitations and reputational damage. The new Director-General must usher in an era of renewal.
Against this backdrop, I present my vision, centred on the firm belief that as the world's only universal multilateral agency in health, WHO has critical mandates and that its relevance matters deeply today in the face of several pressing health challenges, and my conviction that the organisation has the potential to re-emerge as the world's most trusted and leading health agency. My vision, therefore, focuses first on the need for WHO to reclaim its primacy and earn the world's trust as its lead health agency. Such renewal will not simply be a matter of reorganisation; it must run deeper and touch every aspect of the life of WHO. I pledge, therefore, to bring reforms to rapid fruition, to embrace meaningful and timely transparency, to institutionalise true accountability, to ensure value for money, and to drive a culture based on results and concrete delivery. These have featured saliently in my 10 Pledges, to achieve a renewed and reinvigorated WHO.
Universal attainment of the highest possible level of health and wellbeing is an undisputed goal. The new vision for WHO reiterates its importance and flags that its achievement is a collaborative effort. WHO exists in a crowded landscape of global health actors, sectors other than health influence health outcomes, and other stakeholders have a role to play. The systemic interlinkages between the economic, social, and environmental determinants of sustainable development require a profound change from the prevailing sectoral view of health. In order to affect change, I pledge to focus WHO on its core and exclusive mandates and to exercise WHO's leadership by establishing a shared vision, through effective coordination, building on comparative advantage and by establishing a partnership-fostering culture. My programmatic Pledges centre on delivering effective operational readiness in outbreaks and emergencies, strengthened action on global public goods, focus on supporting countries to reduce the health risks of climate change capitalising on the health co-benefits of the low carbon economy, and country-relevant support to achieve the Sustainable Development Goals (SDGs), with an emphasis on universal health coverage and multisectoral action.
My mix of civil society, governmental, medical, multilateral, and grassroots experience allows me to relate to a wide variety of partners and participants, and to understand WHO and its challenges from a wide range of perspectives. If elected, I will lead a WHO that leverages each of these stakeholders' contributions and inspires them to increased engagement and accountability.
I bring a track record of finding solutions. I bridge divides, speak truth to power, drive change, deliver results in resource-constrained environments, and have demonstrated commitment to transparency and accountability. I have the resolve, ability, and experience to provide strong and decisive leadership for WHO—while listening carefully to stakeholders and adapting decisions to a rapidly changing global health environment.
I have committed to voluntarily making my electoral campaign financing public to demonstrate that there will be no hidden influence of campaign financing during my term in office. I will focus on fulfilling WHO's mandate and holding it accountable for delivering results ethically. UN agencies should serve as models of transparency and ethical management and decision-making. My leadership would be a humble but committed step toward positioning WHO as a beacon of ethically rigorous service to humanity.
(1) What would be your priorities as Director-General of WHO?
My priorities are signalled in the New Vision for WHO and the 10 Pledges for Action. My vision for WHO is one in which “WHO reclaims its primacy and earns the world's trust as its lead health agency, and has the ability to foster and sustain partnerships to achieve the vision for health—universal attainment of the highest possible level of health and well-being”. I make ten pledges to achieve this vision. Under my leadership, WHO will demonstrate and deliver:
-
(1)
Transparency and accountability in all areas of its work: WHO will adopt an accountability framework that is straightforward to enforce and is guided by independent voices. As a starting point, I will voluntarily make my own electoral campaign financing a matter of public record and scrutiny.
-
(2)
Leadership for action: leadership will not be subject to special interests, but will rather focus on fulfilling the mandate of the organisation, such that it becomes accountable for results and delivers.
-
(3)
Operational readiness in outbreaks and emergencies: WHO will continue to develop the financial, technical, institutional, and technological capacity to detect, lead, manage, and coordinate the response to outbreaks and emergencies with health consequences, including supporting countries to enhance preparedness and resilience.
-
(4)
Country-relevant support to achieve the SDGs: countries will be supported to achieve the Sustainable Development Goals, particularly Goal 3 to “ensure healthy lives and promote well-being for all at all ages”, with the understanding that the goals are interlinked, and with full realisation of the importance of gender equality and poverty reduction as critically important measures for health.
-
(5)
Strengthened action on global public goods: WHO will live up to its core mandate for collective action to produce global public goods in health—as producer of health norms and standards, as steward of the world's health knowledge, and as bulwark against threats such as antimicrobial resistance.
-
(6)
Focus on health-climate interaction: WHO's actions will support adaptation to and mitigation of climate change, capitalising on the co-benefits of action for health.
-
(7)
Accelerated pace of reforms: WHO will evolve to tackle its systemic constraints, and will reform into an effective, well-managed, transparent, accountable, and cohesive organisation, which achieves value for money, and where robust evidence guides decision-making. WHO will exploit to best effect, the synergies between its headquarters, regional offices, and country offices, and will develop the capacity to look beyond the horizon to anticipate global health trends and what is required to respond.
-
(8)
Management for results: a culture of management for results will be fostered throughout the organisation. Amongst other things, this also means creating a performance-enabling environment, and breaking intra-organisational silos.
-
(9)
A culture of partnerships: WHO will develop the institutional capability to work with all appropriate partners in a transparent, accountable, efficient, and effective manner to improve global health while upholding the principles enshrined in WHO's constitution, and with safeguards against undue influences.
-
(10)
New models for financing: WHO will deliver value for money through a combination of efficient and cost-effective working. Through innovative financing measures, WHO will strive for a budget that is proportionate to its scope of responsibility.
These Pledges are grounded in WHO's constitutional parameters, its exclusive mandates, recent global commitments, a universal outlook for health, country systems strengthening, and commitment to build further on the progress currently underway.
© 2016 Harold Cunningham/Contributor
(2) WHO cannot do everything. What should WHO not do?
Achievement of the vision for health is a collaborative effort in which countries and many national and international organisations play an important role. WHO co-exists with many other institutions in a rich and diverse global health institutional landscape. As the world's only universal membership multilateral agency in health, certain critically important global health functions can only be performed by WHO—norm and standard setting, management of outbreaks and emergencies with health consequences, international coordination, and technical leadership in global health. However, WHO cannot and should not attempt to take on every global health function on its own. It must, therefore, focus on its core and exclusive mandates. As the health sector's lead agency, globally, WHO should exercise leadership by establishing a shared vision, forging partnerships and through effective convening and coordination. WHO must recognise that other global health agencies have specific roles and comparative advantage. To cite examples from the areas of financing, the World Bank, Global Fund for AIDS, TB and Malaria, and Gavi have specific competencies. WHO can gain by maximising synergy. If initiatives seek to stimulate research and development of new vaccines, diagnostics, and treatments for neglected diseases of poverty, (particularly those with complete market failures), WHO can become a force multiplier through timely policy and norm setting. Additionally, by leveraging partners' efforts strategically and effectively, WHO can help mobilise resources to further its own mission—as in the case of the Pandemic Emergency Financing Facility and the Global Health Security Agenda in relation to WHO's operational role in emergencies. There are many opportunities to tap the wide constituency of knowledge-related stakeholders in ways that play to the advantaging of their strengths to further WHO's technical mission. Similarly, many other UN agencies have comparative advantage in areas that matter for WHO's work. Throughout the document “a New Vision for WHO: 10 Pledges for Action” I give examples of work that can be done better by other organisations.
The complex but rich institutional environment in global health is an opportunity for WHO to hone its much-needed coordinating role, which is why I have committed to investing in a Coordination-centred Capacity Building Initiative, as one of the several specific commitments in my pledges. This will aim for WHO's excellence in this area, with the understanding that coordination is one of WHO's key mandates. Through clearer collaborative division of labour and better understanding and acceptance of comparative advantage gains in global health can be achieved faster and better.
(3) Which are the three biggest threats to the health of the peoples, worldwide?
Infectious outbreaks and emergencies with health consequences, antimicrobial resistance (AMR) and the silent pandemic of non-communicable diseases (NCDs), are the biggest immediate threats to the collective health of people, worldwide. These, together with the longer term threat of climate change, threaten to wipe out the development gains of the last century. A flu pandemic in today's interconnected world could kill an estimated 80 million, even with the advanced medicines and technologies at hand. Apart from pandemics, infectious outbreaks such as the Zika virus, can be devastating for societies and economies. Extreme climate events threaten the health and wellbeing of people across the world, particularly those in the Small Island Developing States. Conflicts, disasters, and other catastrophes can lead to widespread public health emergencies. Health is one of the top concerns of the 130 million people who are affected by humanitarian crises across the globe, today. The continued expansion of AMR can reverse most of the medical gains of the last century. Similarly, with an annual estimated 38 million death toll and significant premature mortality, NCDs, are not just the leading cause of death worldwide, but also pose a huge burden on societies and economies. They are projected to incur economic losses of US$7 trillion over the next 15 years in case of inaction to address them. All these threats are cross-border in nature. As such, WHO's role as the world's only multilateral agency in health assumes great significance. Notwithstanding WHO's challenges, its relevance has never been more significant than it is today as it has the mandate to intervene, lead the response, and support national action to address these threats.
In addition to the challenge of collective health security, it is also critical to address other more “individual-centric” threats to health, such as widening health inequities, poor coverage, lack of financial risk protection, and poor quality of care. This creates a strong imperative for countries to adopt universal health coverage (UHC) as a policy goal, given its cross-cutting potential to address both sets of challenges.
(4) What would you do to tackle these threats?
In all three above-mentioned areas, global political and technical consensus has been achieved on the way forward. The 69th WHA approved the Health Emergencies Programme, which is now in its initial states of implementation. In September this year, at the high level meeting of the President of UNGA, there was overwhelming political support to combat AMR, building further on the 2015 WHO Global Action Plan on Antimicrobial Resistance and relevant resolutions of Food and Agriculture Organization and WHO. The global political response to NCDs is much further along, evident in the earlier 2011 UNGA-led political declaration on NCDs, existing frameworks such as the WHO-Framework Convention on Tobacco Control (FCTC), and significant normative and technical work, led by WHO, completed. With the global frameworks in place, I will simply focus on action, refining strategies based on knowledge learnings and positioning WHO as a leader, which leverages the strengths of all partners to assist countries to combat these challenges.
Implementation necessitates action at various levels. Some of the changes currently underway at WHO, for example, the Health Emergencies Programme (with its all hazards approach, new accountability mechanisms, and implicit humanitarian system-wide coordination of the response to large-scale health hazards) need to be fully institutionalised and appropriate structures, staffing, and processes need to be aligned with its “One Program” approach. WHO's support to countries for implementing agreed treaties and action plans or developing plans where needed, has to be strengthened. In addition, it is critical for WHO to promote two policy approaches at the country level: UHC and multisectoral governance mechanisms.
UHC can help prevent and manage disease outbreaks, assist in implementing the International Health Regulations, and can build resilience against the health effects of climate change. UHC is also central for achieving coverage and financial risk protection goals. Hence achievement of UHC is one of the central pillars to combat these challenges, and others more broadly to achieve the vision for health.
Similarly, multisectoral governance arrangements are necessary to deliver on the SDGs and build on the Paris Climate Change agreement. For example, policies to address NCDs need all sectors to work together—including health, finance, foreign affairs, education, agriculture, energy, planning, and others. Tackling AMR necessitates action to address crosscutting issues in animal and human health, agriculture, food, and environment. Similarly, dealing with emergencies has a major interplay with broader disaster management systems. Furthermore, UHC is not just a health but also a social policy objective. I have previously outlined the systemic absence of incentives to forge multisectoral collaboration in government systems as one of the key issues plaguing the functioning of governments (Lancet 2014). WHO must lead a strong call for sectoral cooperation both at the level of governments and international partners.
(5) What does sustainable development mean to you and how can WHO make the greatest contribution to the Sustainable Development Goals?
Sustainable development means harmony and alignment between economic, social, and environmental objectives. It refers to the co-existence of inclusive growth and human development, with flourishing natural systems, resources, and ecosystem services upon which the economy and society depends.
Most SDGs deeply impact health and wellbeing through their focus on bridging inequality, and fostering inclusive economic growth and environmental protection. Therefore, as the health sector's lead agency, globally, WHO can make an important contribution to the SDGs by positioning health at the centre of the sustainable development agenda as enabler, determinant, and outcome of development. The systemic inter-linkages between the economic, social, and environmental determinants of sustainable development create an imperative for a profound change from the prevailing sectoral view of health. WHO can contribute by effectively responding to this major institutional, operational, and knowledge challenge. In addition, it must also advocate for effective action where the determinants impacting health are outside the health sector's scope and shape their behaviours in such a way that the political, economic, and commercial objectives of these actors are reconciled with public health goals.
This necessitates a new approach to leadership, new institutional competencies, systemic innovations to break silos, and a partnership-fostering culture. An international coordinated effort is needed to re-energise institutions, broaden intellectual formation, and improve future leadership. I would aim to lead a transformation so that WHO can be ahead of other agencies in responding to the sustainable development agenda.
SDG 3, “Ensure healthy lives and promote well-being for all at all ages”, is directly health-related, with UHC as its central pillar. One of the greatest contributions WHO can make is to advance the SDGs' agenda through its support for UHC. UHC saves lives by promoting healthy life expectancy, reducing poverty, and protecting household incomes. Under my leadership, WHO will promote UHC as a health policy goal for all countries, and will help ministries of health galvanise commitment at the head of state level. Embracing UHC means building on previous commitments to primary health care and including long-term social policy commitment, domestic resource allocation, and a move linking coverage for essential services to financial risk protection. UHC must also be inclusive of prevention, health promotion, and public health, and should focus on achieving equity.
However, the success of UHC hinges on effective health systems. Amongst other things this should also include advocacy and technical support to help countries overcome systemic barriers and greater attention to bridging stewardship deficiencies in countries, especially in mixed health systems. I realise country needs differ substantially. I will, therefore, strive to make WHO's technical assistance country-tailored, taking advantage of its three-tier structure, especially WHO's unique 150-country-strong footprint. At the same time, I will also focus on strengthening WHO's technical assistance to countries in terms of quantum, quality, and relevance. As the global community and countries look at a full (sometimes overwhelming) suite of interventions, WHO must promote the ones that are high “value for money”, and have the potential to maximise synergies across silos, align with a rights-based approach, and impact in terms of gender equality and equity in outcomes.
(6) WHO lost credibility over its handling of the Ebola virus outbreak. What must WHO do to rebuild trust of governments and their citizens?
Transparency and accountability are vital for safeguarding WHO's role and achieving the vision for WHO. Transparency and accountability are mutually reinforcing. Accountability is not only, or even primarily a punitive concept, but rather has a preventive function and is essential to re-establishing trust in WHO. Under my leadership, WHO will deliver transparency in all areas of its work, and will adopt an accountability framework that is straightforward to enforce and is guided by independent voices.
Good management is also key at this juncture in WHO's history. I will establish Priority Metrics for WHO and a Delivery Unit, reporting directly to the office of the Director-General, to drive a culture of management for results throughout the organisation. The new unit will also work to address intra-organisational silos across diseases and areas of work, and build teams across large departments to maximise coherent approaches. Noting that the varied quality of WHO staff is frequently cited as one of the key limitations of the organisation, performance management will be one of the key areas of focus of the Delivery Unit.
WHO must exhibit a performance enabling environment with clear responsibilities, the right incentives to perform, performance reward mechanisms, and effective accountability frameworks. Staff must be supported to give the best possible advice, even when they are under pressure from powerful interests. Transparency in recruitment processes, and merit-based hiring is equally critical. To regain trust, WHO must deliver value for money, in a fiscally-constrained environment. Reforms in the pipeline and others that may be initiated need to be brought to fruition in a timely and effective manner. Programmatic changes must be implemented efficiently and a culture of evidence-based decision making needs to be ingrained. These changes are not mutually exclusive and need to cascade into action in tandem.
(7) Does WHO need further reform? if so, what reforms would you implement?
I will address WHO reforms through four approaches—which are not mutually exclusive. First, before discussing further reform, I will take stock of existing efforts underway, build further on them, and accelerate pace, where needed, as for example, in the case of reform of WHO's emergency's operations and reform concerning the modalities of stakeholder engagement, both of which are in the early stages of implementation. I will plough back learnings to refine operations. Other process-related reforms, such as those centred on agenda management, budget alignment, monitoring, information management, and financing, are at various stages of implementation. Within 30 days of assuming office, I will convene a “stock-taking” meeting to refine a plan for the way forward.
Secondly, I will explore options to fully exploit synergies between headquarters, regional and country offices. As an entry point, I will fully institutionalise the Senior Management Global Policy Group. Thirdly, I will seek Member States' support for an objective and knowledge-driven reform to tackle WHO's structural and managerial problems. Lastly, under my leadership, capacity for forecasting will be institutionalised so that WHO looks beyond the horizon and hones its ability for response to emerging threats.
(8) What are the biggest threats facing WHO in the next 5 years? How will you address these threats?
WHO is under a twofold threat. One of them emanates from the unpredictable nature of infectious outbreaks and emergencies with health consequences. WHO has suffered reputational damage during its handling of the west African Ebola crisis and the reform to overcome the agency's inherent weaknesses is in its initial stages of implementation. Pending the full and effective institutionalisation of capacity and funding, WHO will remain vulnerable to threats emanating from infectious hazards and emergencies with health consequences.
WHO is undergoing reform in an overall context where Agenda 2030 has signalled a fundamental change compared to what was the norm in the era of the MDGs. WHO has to realign itself in this changing context. It must get better at leading through coordination and establish capacity to forge and sustain partnerships with appropriate safeguards. In addition, it must also develop both the culture as well as the capacity to harness the myriad innovations and changing ecosystems, which are either driving change in health directly or have the potential to do so in order to achieve the vision for health. Failure to reform and transform is a threat in its own right. As WHO's work becomes increasingly intersectoral, as it should, WHO must in tandem efficiently and effectively, enforce all procedures of FENSA (WHO Framework of Engagement with Non-State Actors) to build safeguards against undue influences, which can undermine public confidence and create a reputational risk.
(9) Should WHO be a leader in health or should it only respond to the wishes of Member States?
WHO is a Member State governed organisation, and as such Member States have an important policy making role. However, as a multilateral agency with a clear public mandate and mission it has a responsibility towards people as well, which is implicit in the framing section of its constitution, which states: “Informed opinion and active co-operation on the part of the public are of the utmost importance in the improvement of the health of the people.” Therefore, it clearly must be a leader in health.
(10) What unique skills would you bring to the job of WHO Director-General?
I have a unique combination of major institutional leadership from both governmental and non-governmental sectors. I am a medical doctor as well as having a research background. I have worked extensively both in the multilateral system as well as at the grassroots level serving poor communities. I have built institutions from scratch and have taken them to scale. I have been able to find innovative solutions to complex problems, have delivered results in resource-constrained environments, and have an ironclad commitment to transparency and accountability. I have worked with and led people from every region of the world from diverse backgrounds and perspectives, and have been able to convene widely diverse constituencies, build bridges across different cultural, social, economic, and political perspectives. I am a bridge between the Muslim world and the west and have the confidence of both developed and developing countries.
My work with systems reform and experience to navigate change and deliver results are relevant for the WHO reform process currently underway. In my civil society role, I have campaigned to promote accountability and institutionalised it while building institutions. This is a critical strength WHO needs. I have experience in both governance as well as management, both from my experience chairing and serving on boards nationally and internationally and I have deep management experience building institutions and taking them to scale. I have gained experience in strategy formulation, fund mobilisation, partnership building, and use of innovations for systems-building. I have proven resource mobilisation skills and have leveraged transparency, accountability, and value for money to auger donors' trust. Establishing institutions in a resource-constrained environment have made me adept at efficient utilisation of resources and building strong systems for change.
As WHO is committed to the SDGs, I have a natural advantage given my experience in the two major additional areas of focus for the SDGs—NCDs and UHC. My expertise in sectors outside health (social protection, governance, reform, and public-private engagement) allows me to understand the multisectoral nature of health.
I am known for my collaborative approach and ability to engage a wide variety of governmental and non-governmental stakeholders to address complex problems and lead transformations. I have been humbled to be globally decorated as an innovator. It goes without saying that with my developing country background and proven pro-poor record, I am well-placed to represent the views of, and be responsive to, the needs of the underprivileged. As a woman leader and change agent, I am particularly gender-sensitive. With a long track-record and broad acceptability in international civil society, and experience engaging with the private sector through my work on obesity prevention, I can bring diverse voices to the negotiating table. I have been blessed with the knowledge of micro—understanding people's needs—to influence the macro in terms of policy reform and institutional change.
Miklós Szócska
Hungary

© 2016 Thaler
The responsibilities of WHO for global health are relatively straightforward. As the Director-General of WHO, I should work for: making people on this planet healthier and more cautious for their health; universal health coverage should protect the sick, health systems should be resilient, equitable, and ever growing in quality; the mission of health promotion, prevention, cure, and care should be provided by a properly trained, motivated, and innovative health labour force.
I envisage a strong WHO as the indisputable, impartial leader in global health, the world's advocate for value driven health policy for better health and reduced inequities within the 2030 Agenda and Sustainable Development Goals (SDGs). The world needs WHO as a leading international change agent for health, an agile global agency to deal with the extremes and the unexpected. The road to resilience is long: it requires an organisation, which is a knowledge centre of technical and social innovations, and the master of technical and political feasibility.
The next Director-General will have to close the gap that exists between theoretical solutions and failures in implementation. In many cases, we have evidence and proper solutions ready for what should be done. Many times we solve problems of a technical nature, but fail when we have to initiate behavioural change. The consequence is a high failure rate with change or local actions. No technical solution is valid without an implementation and consultative change methodology. Changes should be evidence-based and balanced with behavioural insights. No external solution is valid without local ownership. Working on what should go together with how. Acting as an advocate for change, this approach will be the key methodological element of my work.
We should act in the present, be prepared for the unexpected, and plan and build for the future of health. Traditional answers and official procedures that were useful and sufficient to lay the foundations of global institutions in a steadier world, do not necessarily deliver solutions in the present social, political, and industrial realities. New, globally successful health actors and donors grew out of the rapidly changing environment and successfully started to fill the adaptational vacuum to dominate the institutional world with their actions. WHO has to transform to become an agile global agency and build renewed global partnerships to meet the challenges, relying on already existing initiatives, and the values and exceptional professional power of WHO.
We have to make health a global political economic and financial priority. The international community of health policy makers and experts is united and ready to align their actions with the SDGs, and its health priorities. However, in times of global economic crisis, fiscal austerity, and regional conflicts, this is not enough. We have to break out of the inbreeding of our internal professional wish-lists. The health community has to be able to influence the agendas of global and national political and fiscal decision makers to make them act towards solutions. The SDG agenda offers an unprecedented momentum to renew commitments for health at the highest political level.
(1) What would be your priorities as Director-General of WHO?
-
(1)
The management of pandemics—with utmost agility in preparedness, forecasting, modelling, logistics, and surveillance, in coordinated partnership, with interventions that are culturally tailored, supporting local actions with global rapid response teams complementing weak or missing local capacities.
-
(2)
Sharing the risks could not be managed without stable and sustainable funding; acknowledging the unprecedented efforts of global donors, it is time to recognise the need for institutional resource generation responses to promote universal coverage and pandemic risk sharing; understanding that global funding is of political consideration and should happen in dialogue with governmental and business communities, we should promote innovative economic models for generating resources, such as public health product taxation.
-
(3)
In the fight against antimicrobial resistance (AMR), humanity should be equipped with new antibiotics and ensure access to high priced medicines (vaccines and drugs) globally; with new business models developed in dialogue with a portfolio of stakeholders from donors through research to business communities; the antibiotics strategy should be managed through influencing behaviour of professionals and cross-sectoral interventions.
-
(4)
Health human resources developments and balancing migration globally in coordinated partnership.
-
(5)
WHO should promote innovation and technology in changing the trends regarding accessibility and equity and take advantages of the tools of the 21st century by: utilising big data technologies to improve our warning and surveillance systems and predictive capabilities; mobile and wearable technologies to take diagnostics and therapy to places where they never existed before, this way promoting access very cost-effectively; and point of care technologies to provide health care for those in the flow of migration.
-
(6)
Countries emerging from conflicts without solid public administration systems—by development of public health systems parallel to and integrated in the establishment of new public administration.
-
(7)
The development of primary care and care coordination through cross-country learning and sharing good practices.
-
(8)
Fighting non-communicable diseases (NCDs) globally with social mobilisation and behaviour change in mind.
-
(9)
Partnerships and collaboration should be endorsed. Health problems are larger than what a single organisation could ever bear. I will work to achieve effective collaboration partnerships and coordinated actions within the UN and with Member States, donors, and international stakeholders.
(2) WHO cannot do everything. What should WHO not do?
Though the portfolio of WHO could only be renewed through a thorough thematic and administrative review process, there would be guiding principles for my work.
WHO should not be more clever than the best microbiologists or epidemiologists on the planet, we should mobilise them for partnership supporting our decisions and interventions.
WHO should not be more experienced than the most experienced field workers, rather we should work in partnership with them and support their actions.
WHO should not run duplicate or redundant professional activities and programmes in the organisation to avoid organisational interference and inefficient utilisation of funds.
WHO should not take over the role of development and funding agencies.
While WHO should focus on its normative mandate it should not forget to represent health as human right for all, so it should not give in on its values, impartiality, or neutrality.
(3) What are the three biggest threats to the health of peoples across the world?
Three complex answers represent my view on the biggest threats to the health of people.
-
(1)
The consequences of climate change and the connected world—water shortage and novel and emerging diseases and pandemics.
-
(2)
Irresponsible individual and social behaviour. We should think about consumer behaviour and marketing of food or the utilisation of antibiotics, business models that lead monopoly pricing, decision making, or business models that prefer short-term gains versus long-term values and sustainability. We can see that all these could be derived from human behaviour or social interactions. These represent an utter challenge to health in various ways. They contribute to the formation of NCDs and through the burden of disease they challenge the sustainability of health systems globally. It is also man-made legislative systems that determine social prioritisation between health, education, or industrial interests, not to talk of violence or accidents.
-
(3)
The third threat is of a paradox nature. On the one hand, the emergence of big data in health and genomics offer the hope for new therapies, personalised medicine, and prevention. On the other hand, the emergence of global data collection and data sharing industries also carries the threat that our digital health phenotype and genomic identity become marketing products, outside the domains of medical and health ethics. Genomically targeted medication also assumes the same logic as genomically targeted poisoning, or genocide.
(4) What would you do to tackle those threats?
The threats to health are larger than what a single organisation could ever bear. I will work to achieve effective collaboration partnerships and coordinated actions within the UN and with Member States, donors and international stakeholders, civil society, patients' organisations, and non-state actors.
We need an efficient public health regulatory agenda to support the creation of an enabling environment to offer people the easy choice for health. Prevention and promotion should be well tailored interventions that consider human behaviour.
We should also work for new and sustainable business models for high priced technologies and medicines.
We should meet the challenge of re-prioritising health in political and fiscal decision making.
We should initiate a debate and legislation of the liberalisation and control of the utilisation of health data that takes 21st century technological realities into account.
(5) What does sustainable development mean to you, and how can WHO make the greatest contribution to the Sustainable Development Goals?
SDGs represent a revolutionary momentum. They represent the commitment of Member States and the heads of those Member States, who took accountability for implementing them. They also represent a new chance that investment in health can happen in a complex way.
WHO should work to translate the SDGs into measurable implementation objectives and actions and should assist Member States on the road to implementation.
(6) WHO lost credibility over its handling of the Ebola virus outbreak. What must WHO do to rebuild the trust of governments and their citizens?
The importance of WHO is growing in this era of collective uncertainty. Its independence from partial interests and neutrality is uniquely important, thus to regain the credibility of and trust towards WHO is a top priority.
As I mentioned, the management of pandemics is a top priority for me: utmost agility and innovation in preparedness, forecasting, modelling, logistics, and surveillance. Actions should be carried out in coordinated partnership with other UN agencies and those in the field. The interventions should be culturally tailored instead of medicalised, focus on assisting building local capacities and the support of local actions with global rapid response teams complementing weak or missing local capacities.
We should be active on the field with continuous internal control and feedback from partners that we are on the correct road. We should honestly learn from our own shortcomings and take them into account, when transforming WHO as an organisation and its procedures.
Crisis communication capacities should be improved and the potential of relevant big data analytics in warning systems or modelling should also be explored.
(7) Does WHO need further reform? If so, what reforms would you implement?
Yes, the WHO should transform. In this process we have to build on the achievements of the ongoing WHO reform initiatives of Madame Chan in alignment with the broader UN reform agenda.
With promoting the idea of resilient health systems towards Member States, comes the responsibility of WHO to be resilient. WHO has all the potential and is full of expertise and benevolent staff to accomplish a cultural change. To make this happen I will ensure a team spirit, a culture of open speech and consultation for all staff members, career progression, and recruitment based on merit. The key components of the transformation strategy include: developing change management capacities; redesigning performance and reporting in a global project portfolio management framework focusing on results, problem solving; preventing bureaucracy from strangling action; development of rapid response teams and task forces to support country efforts to cope with local health-related emergencies, building on mobilising WHO's resources globally; further development of risk communication capabilities; empower professional and management information systems by big data technologies and enhance transparency; stabilising funding of WHO and its priority programmes.
As a leading umbrella organisation in its changing institutional system, WHO should engage in renewed partnerships.
We should be good listeners and ensure that no expertise is wasted by ignorance, no partnerships are lost by indolence, no resistance is provoked by arrogance.
(8) What are the biggest threats facing WHO in the next 5 years? How will you address these threats?
The number one threat is the erosion of the WHO “brand”. Though it is still unique and strong, the radically changing institutional environment gave room to new agencies and institutions that compete for legitimacy with less solid normative foundations. The above suggested WHO organisational reforms address this threat.
Antagonistic industry interests play a pro-active role in undermining WHO efforts and WHO policies. In many domains WHO is competing with antagonists that are rich in resources to influence. This is an area, where WHO should act in shrewd agility using its institutional weight and credit to support Member States globally. The focus of persuasion should be turned towards key political and fiscal decision makers.
The internal threat is organisational inertia. The above suggested WHO organisational reforms address this threat with special attention to unexpected outbreaks that will regularly test the resilience of the organisation.
(9) Should WHO be a leader in health or should it only respond to the wishes of Member States?
As I mentioned, WHO has to assume the position of a leading international change agent, an agile global agency, which is a knowledge centre of technical and social innovations, and the master of technical and political feasibility. This transformation is needed to effectively respond to the requests of Member States, based on renewed partnerships. WHO cannot become a global leader in health without a deep understanding of the needs and perspectives of Member States.
© 2016 Harold Cunningham/Contributor
(10) What unique skills would you bring to the job of WHO Director-General?
My health reform and public health regulatory agenda demonstrate a strong understanding of health priorities and an ability to put knowledge into action. I believe that the implementation of these reforms and the management of the EU presidency prepared me to act on a global level.
I habitually do my job working in teams and as public health interventions are collaborative efforts I am ready to mobilise WHO and the best public health experts and institutions to support our decisions and actions with a global network.
The Health Services Management Training Centre of Semmelweis University has been a partner institute of international agencies and universities. As director I gained broad experience with international training programmes focusing on health reforms, financing, AIDS, and tuberculosis in Europe, central Asia, Asia, and Africa. These interactive training programmes focused on skill development for international participants to define their problems, plan relevant interventions, and develop local ownership towards solutions.
My first leadership experience was being elected as student president from the opposition at the dawn of the system change of the late 80s. I have learnt the importance of mobilising people and organisational resources for change. Since then I have developed a systemic approach of consultations with stakeholders and professionals to prevent resistance against change and for developing ownership of the problems and solutions. These capacities helped me to manage the Hungarian health care with a demanding reform agenda through the world economic crisis and stay in office for a full electoral term, while average life expectancy in my position was 20 months in the previous 20 years. During my term, we successfully managed the European Presidency with strong human resources crisis and sustainability of the health services agenda.
The anti-smoking regulation was carried through the full legislative processes in 76 days (!), with 84·1% majority votes, and even 64% of smokers supported it. In the first year of the introduction of HPV vaccination 80% of mothers requested their daughters to be vaccinated. The rapid implementation and public support of the public health regulations demonstrate that I managed to advocate the interest of health and we successfully persuaded stakeholders and the public as well. The decrease of trans-fat content of food, introduction of HPV vaccination for adolescent girls, and the introduction of public health product tax (PHPT) on food and beverages with added salt and sugar content were also on the agenda. PHPT proved to be an innovative tool to influence consumer and industry behaviour simultaneously, and generated invaluable resources during the deepest times of economic crisis. People consumed less added sugar and salt and companies improved their food production formulas. Revenues from PHPT were used to raise the salaries of nurses and doctors to slow down health worker emigration. In 2013 WHO awarded the government for the anti-smoking actions and Hungary jumped to the 11th place from the 27th on the Tobacco Scale Control Index.
Managing the large-scale health system reform laid down the foundations of a new national health service by nationalising hospitals, re-engineering and integrating patient pathways, introducing regionally centralised capacity planning, and tailoring capacities to current needs. Our pharmaceutical policy of innovative payment schemes, taxing, and competitive bidding radically decreased drug expenditure of health insurance and citizens, making therapies more accessible in times of economic crisis. All this required dialogue with various stakeholders. Savings in drug expenditures or re-engineering patient pathways also needed regulatory interventions, but a successful dialogue with patient and professional associations and industry as well, to accept crisis realities. We efficiently managed conflicting interests of non-governmental actors.
The organisational transitions and development projects during my mandate were reinforced by innovative management interventions. We introduced big data and network analysis in supporting decisions and management control and these approaches could also be useful in forecasting and modelling pandemics. The centralised national procurement of utilities and pharmaceuticals yielded radical cost savings and larger volumes of medicines and vaccines. The broad range of reform, development, and organisational interventions were monitored for performance through project portfolio management.
Teaching on international programmes for a diverse audience, that many times brought conflicting war experience to the teaching room, equipped me to touch the problems of health in a way to put it above all particular conflicts and self interests. These experiences prepared me for my work on various WHO and other professional committees and missions to successfully develop agreement, and initiate and implement change in culturally diverse or even divided context.
As minister of state, I participated in my country's global opening initiatives and developed active cross-cultural relationships.
For more on Sania Nishtar's New Vision for WHO and the 10 Pledges for Action see http://www.sanianishtar.info/manifesto/




