Abstract
Background:
Osgood-Schlatter disease (OSD) affects 1 in 10 adolescents. There is a lack of evidence-based interventions, and passive approaches (eg, rest and avoidance of painful activities) are often prescribed.
Purpose:
To investigate an intervention consisting of education on activity modification and knee-strengthening exercises designed for adolescents with OSD.
Study Design:
Case series; Level of evidence, 4.
Methods:
This study included 51 adolescents (51% female; age range, 10-14 years) with OSD. The 12-week intervention consisted of an activity ladder designed to manage patellar tendon loading and pain, knee-strengthening exercises, and a gradual return to sport. The primary outcome was the global reporting of change at 12 weeks, evaluated with a 7-point Likert scale (successful outcome was considered “much improved” or “improved”). Additional endpoints were at 4, 8, 26, and 52 weeks. Secondary outcomes included the Knee injury and Osteoarthritis Outcome Score (KOOS), objective strength, and jump performance.
Results:
Adolescents reported a mean pain duration of 21 months at enrollment. After 12 weeks, 80% reported a successful outcome, which increased to 90% at 12 months. At 12 weeks, 16% returned to playing sport, which increased to 69% at 12 months. The KOOS subscores of Pain, Activities of Daily Living, Sport and Recreation, and Quality of Life improved significantly (7-20 points), and there were improvements in knee extension strength (32%; P < .001), hip abduction strength (24%; P < .001), and jumping for distance (14%; P < .001) and height (19%; P < .001) at 12 weeks.
Conclusion:
An intervention consisting of activity modification, pain monitoring, progressive strengthening, and a return-to-sport paradigm was associated with improved self-reported outcomes, hip and knee muscle strength, and jumping performance. This approach may offer an alternative to passive approaches such as rest or wait-and-see, often prescribed for adolescents with OSD.
Registration:
NCT02799394 (ClinicalTrials.gov identifier)
Keywords: Pediatrics, musculoskeletal, pain, apophysitis
Osgood-Schlatter disease (OSD) is growth-related apophysitis of the knee, affecting 1 in 10 athletic adolescents.4 While the source of pain in OSD is unclear, adolescents with OSD often report pain localized to the tibial tuberosity, which is aggravated during knee-loading activities.3,6 Clinically, OSD is characterized by localized pain and swelling at the tibial tuberosity and pain during palpation of the tibial tuberosity.6 Its prevalence is highest in active adolescents,4 with early sport specialization associated with a 4-fold greater relative risk of developing OSD.8
OSD is commonly reported to resolve within 12 to 18 months, despite the lack of data supporting this.6 Recent evidence challenges this assumption,7 and even after “recovery,” adolescents demonstrate negative ultrasound findings and impaired function.9 Overall, 60% of those diagnosed with OSD at an orthopaedic department within a 6-year period reported OSD-related pain at a median of 4 years’ follow-up. This continued pain was associated with impairments in both knee function and quality of life.7 The large deficits in strength and function18 appear to persist after the resolution of symptoms.12,19 Perhaps because of the previously assumed innocuous nature of the condition, there is a dearth of research evaluating interventions to reduce symptoms, improve function, and speed up recovery.2 Intervention studies are confined to a randomized controlled trial investigating injections and a retrospective cohort investigating surgical management.2,21 No trials or cohort studies have evaluated other management strategies.2 A high degree of sport participation and repetitive overuse are considered critical in the development of OSD,8 and these indications can provide key treatment targets that have never been investigated. The aim of this study was to investigate the effect of an intervention consisting of education on activity modification and knee-strengthening exercises designed for adolescents with OSD.
Methods
Study Design
This prospective cohort study was pre-registered on clinicaltrials.gov (NCT02799394) and approved by the ethics committee of the North Denmark Region (N-2014-0100). Parental informed consent and participant assent were acquired from all participants. Reporting complies with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.5
Recruitment
Participants were recruited between 2015 and 2017 via local schools and social media. All adolescents with knee pain who responded to a questionnaire distributed to schools or to posts on social media were telephoned and subsequently invited for a clinical examination. This process was used to recruit participants for this trial (adolescents with OSD) and another study on adolescents with patellofemoral pain (NCT0240267314). The clinical examination was conducted by 1 of 2 experienced physical therapists (K.K. or L.W.) and did not include radiographs as inclusion or exclusion criteria. The criteria used to diagnose OSD were in line with previous literature6,20 (Table 1).
TABLE 1.
Inclusion and Exclusion Criteria
| Inclusion criteria |
|
| Exclusion criteria |
|
Intervention
The intervention included 4 visits with a physical therapist over a 12-week period. Parents were required to take part in all 4 visits. The intervention was structured into 2 blocks (Table 2). Initial load management (weeks 0-4) consisted of a temporary reduction in sport participation. During this period, participants were instructed to refrain from pain-aggravating activities and sport participation. In addition, participants were instructed to perform knee exercises in the form of static holds and bridges to avoid the loss of muscle strength. This was supported by a load-based activity ladder and pain monitoring (Appendix 1).
TABLE 2.
Building Blocks of the Interventiona
| Block 1 (0-4 wk) | Block 2 (5-12 wk) | |
|---|---|---|
| Educational components |
|
|
| Modalities to gradually increase knee joint loads |
|
|
| Specific tools introduced |
|
|
aOSD, Osgood-Schlatter disease.
During the second block (weeks 5-12), adolescents were instructed to (1) perform a progressive home-based knee-strengthening program and (2) follow the activity ladder and progression model for return to sport. Knee strengthening consisted of 3 exercise progression levels (with increasing levels of difficulty). This also guided adolescents’ progression on the activity ladder; that is, adolescents had to be able to perform the squat (progression level 2) within the “OK zone” before progressing to step 3 on the activity ladder (Appendix 1). During each of the visits, the focus was on helping adolescents and their parents understand and manage training loads and pain. The activity ladder and pain monitoring model enabled participants to progress exercises and activities between visits (the full intervention, including sets and repetitions for the exercises, can be seen in Appendix 1).
A training diary was used to measure adherence to the strength exercises. Participants who did not return the diary were assumed not to have completed any exercises. Adherence to activity modification was determined by ActiGraph monitors.
Baseline Demographics
Weight was measured by a weighing scale (Seca). Height was measured with a measuring tape while participants stood with their back straight against a wall in their bare feet. Pain duration was determined by asking the following: “For how long have you experienced your knee pain?” Participants reported current and previous sport participation (before knee pain) and if they had reduced/stopped sport because of pain.
Outcomes
Self-reported questionnaires were completed by participants at baseline (before the intervention was started) and after 4, 8, 12, 26, and 52 weeks. Ultimately, 12 weeks was considered our primary endpoint. If needed, parents helped participants answer the questions. Before the assessment, all questions were piloted in the same age group to ensure comprehensibility. The primary outcome was self-reported improvement on a 7-point Likert scale ranging from “much improved” to “much worse,” with the midpoint being “no change.” Participants were deemed to have a successful outcome if they reported “improved” or “much improved.” This has previously been used in other studies on adolescents with knee pain.17
In addition to improvement, the self-reported questionnaire included the Knee injury and Osteoarthritis Outcome Score (KOOS),19 highest degree of pain during the past week measured by a numeric rating scale (ranging from 0 to 10, with 0 being “no pain” and 10 being “worst pain imaginable”), if they considered themselves to be completely free of knee pain at each follow-up, and sports participation (times per week). These questions have previously been used in adolescents with knee pain, enabling comparisons.13,17 Health-related quality of life was measured by the youth version of the EuroQol–5 Dimensions with 3 levels (hereafter referred to as EQ-5D-Y).1
Physical Activity
Objective physical activity was measured with an ActiGraph GT3X+.18 This is a commercially available 3-axis accelerometer that has been validated for collecting physical activity data.11 It is a wearable device that measures acceleration, which is filtered and processed to obtain activity counts. These counts are proprietary measures used to classify time spent in activities, with different intensities such as sedentary, moderate, and vigorous physical activity according to predefined count thresholds. The ActiGraph GT3X+ was initialized using ActiLife software (version 5.0; ActiGraph) and set to record at 30 Hz. Participants were instructed to wear the ActiGraph on their wrist for a minimum of 1 week (1) at the time of inclusion, (2) during block 1 of activity modification, and (3) at the 12-week follow-up. Data were analyzed using ActiLife software to extract time spent in sedentary, light, and moderate to vigorous physical activity. For further information on data analysis, see Appendix 2.
Lower Limb Strength
Isometric knee extension and hip abduction strength were assessed at baseline and 4- and 12-week follow-up. Muscle strength was assessed using a Commander PowerTrack handheld dynamometer (JTECH Medical) fixed with a belt to the examination couch. All strength tests were conducted isometrically and can be seen in Appendix 1. The average of 3 consecutive measurements, normalized to body weight and lever length, was used for analysis. The procedure is identical to previous work in adolescents, and it has demonstrated high reliability.13
Lower Limb Jumping Performance
Lower extremity jumping performance was used to assess lower limb function at baseline and 4- and 12-week follow-up. This was done with single-leg vertical and horizontal jumps. To measure single-leg vertical jumps, participants first marked their highest standing reach: While standing with chalk on their fingertips, participants reached as high as they could and made a mark on a blackboard. Participants then performed a single-leg maximal vertical jump (their most painful knee) and marked the highest point, landing on the same leg. Participants had their other hand free and were given a minimum of 1 practice attempt or until they were proficient with the movement. Participants then performed 3 maximal-effort jumps, with the best trial used for analysis. Jump height was calculated as the vertical distance between jump reach and standing reach. The single-leg horizontal jump for distance (broad jump) was measured as the distance from the tip of the shoe at the start position and the heel at the landing position. Each trial was conducted with a 30-second pause between, and pain during testing was recorded. Changes over time are expressed as percentages from baseline for each participant.
Sample Size
This was a pilot study with no previous data available on which to base the sample size. The sample size was therefore based on the following rationales: (1) a sample large enough to explore outcomes and perform sample size calculations for future clinical trials and (2) the ability to capture the heterogeneity of the sample in terms of sex and sport participation.
Statistical Analysis
All data were visually inspected for approximate normality using a Q-Q plot. The mean ± SD is reported when data were normally distributed. Nonnormally distributed data are presented as the median and interquartile range. All calculations were performed using Stata (version 11; StataCorp).
To maximize data availability for the ActiGraph, a general linear mixed model was used. This enabled the inclusion of ActiGraph data from 47 participants over the 3 time points. The model accounted for the within-participant nature by including random effects for participants, with a variance component covariance structure and restricted maximum likelihood estimation. The best-fitting covariance structure for the residuals was a compound symmetry structure evaluated with the –2 restricted log likelihood (1234.99) and Akaike information criterion (1238.99). Time (baseline, 4 weeks, and 12 weeks) was included as a fixed repeated-measures factor, with moderate to vigorous physical activity as the dependent variable. Repeated-measures analysis of variance (ANOVA) was used to evaluate changes in strength over time (baseline, 4 weeks, and 12 weeks) for the dependent variables of knee extension torque and hip abduction torque. Similarly, repeated-measures ANOVA was used to evaluate the effect of time (baseline and 4, 8, 12, 26, and 52 weeks) on the KOOS and EQ-5D-Y. In cases where the assumption of sphericity was violated, the Greenhouse-Geisser correction was used.
Results
Participants
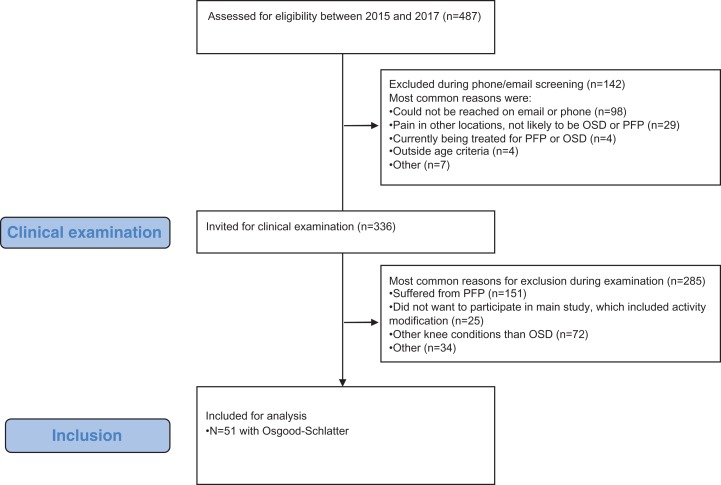
Over the 5-month recruitment period, 51 adolescents with OSD were enrolled in the study (Figure 1). At enrollment, adolescents reported a mean pain duration of 21 ± 12.5 months. There were 18 participants who reported that they had previously received treatment for their OSD, most commonly by a physical therapist (17/18). Baseline demographics are included in Table 3. Response rates were 88% at the primary endpoint, 80% at 12-month follow-up, and 96% at 4-week follow-up.
Figure 1.
Flowchart for recruitment of participants. The participants were recruited in parallel for both a study on Osgood-Schlatter disease (OSD) and patellofemoral pain (PFP).
TABLE 3.
Baseline Demographics (N = 51)a
| Value | |
|---|---|
| Age, y | 12.7 ± 1.1 |
| Female sex, % | 51 |
| Weight, kg | 55.8 ± 10.1 |
| Height, cm | 165.5 ± 8.4 |
| BMI, median (IQR), kg/m2 | 20.2 (17.6-22.0) |
| Previously treated for knee pain, % | 35 |
| Difficulty with kneeling, %b | 58 |
| Use of pain medication for knee pain, % | 12 |
| Physical activity, min, mean (95% CI)c | |
| Sedentary | 344.2 (330.3-358.1) |
| Average light | 333.8 (315.7-351.9) |
| Average moderate | 115.5 (106.4-124.6) |
| Average vigorous | 133.1 (117.5-148.7) |
| Moderate to vigorous | 248.7 (225.1-272.2) |
| Reached WHO minimum physical activity recommendations per day, % | 92 |
aValues are reported as mean ± SD unless otherwise indicated. BMI, body mass index; IQR, interquartile range; KOOS, Knee injury and Osteoarthritis Outcome Score; WHO, World Health Organization.
bBased on participants reporting “moderate” or “severe” difficulties on question 5 of the KOOS Sport and Recreation subscale.
cBased on available ActiGraph data from 47 adolescents with Osgood-Schlatter disease; there were missing data from 4 participants at baseline.
Primary Outcome
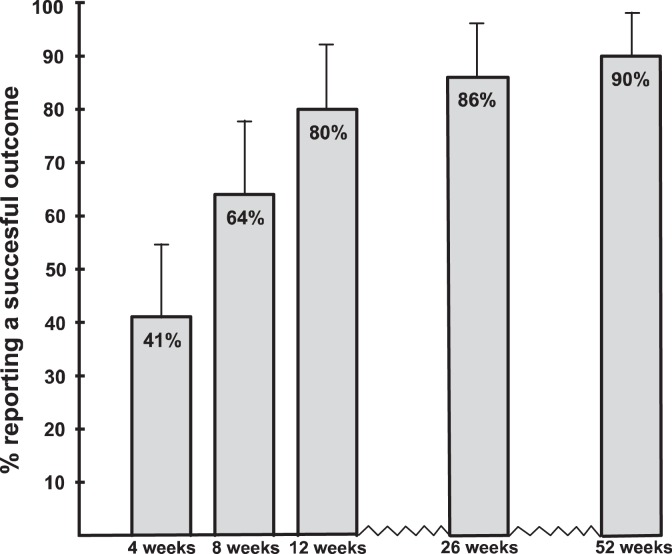
At the primary endpoint (12 weeks), 80% reported a successful outcome (improved or much improved), which increased to 90% at 12 months (Figure 2).
Figure 2.
Proportion reporting a successful outcome (success defined as reporting “much improved” or “improved” on the global rating of change scale). Error bars indicate 95% CIs.
Self-Reported Knee Pain, Disability, and Quality of Life
Highest degree of pain during the past week decreased from a median score of 7 of 10 at baseline to 2 of 10 at 12 weeks (P < .001) (Figure 3). The KOOS Pain subscore improved 14 points during the first 12 weeks, reaching a mean of 91 points after 12 months (P < .001) (Figure 3). A total of 27 of 45 considered themselves free from knee pain at 12 weeks, which was similar at 12 months (24/43). Participants improved 7 to 20 points on the KOOS subscales of Activities of Daily Living, Sport and Recreation, and Quality of Life from baseline to the primary endpoint (P < .001) (Figure 3). This was a 9- to 34-point improvement at 12-month follow-up (P < .001). Moreover, 38.7% reported moderate or severe difficulty in kneeling at 4 weeks (based on responses to question 5 of the KOOS Sport and Recreation subscale), which improved to 9.5% at 12-month follow-up. The EQ-5D-Y index score increased significantly (F 3,105 = 13.6; P < .001) by 0.13 points at 12 weeks and by 0.23 points at 12 months (Figure 3). Significant changes from baseline are presented in Figure 3 for the KOOS and EQ-5D-Y.
Figure 3.
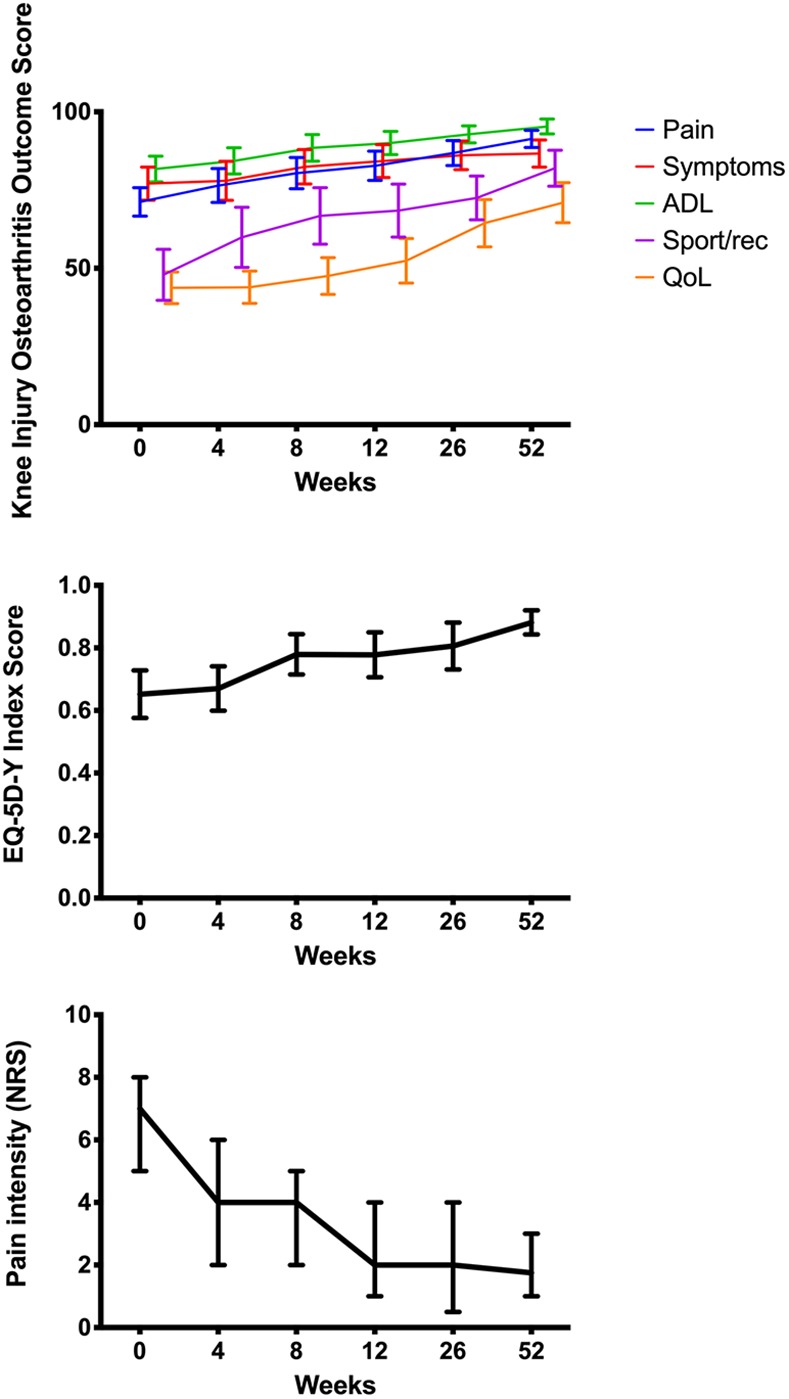
Self-reported outcomes from baseline to 12 months: Knee injury and Osteoarthritis Outcome Score (KOOS), health-related quality of life (QoL) as measured by the youth version of the EuroQol–5 Dimensions (EQ-5D-Y), and highest degree of pain during the past week (numeric rating scale [NRS]). ADL, Activities of Daily Living.
Physical Activity and Sport Participation
At 12 weeks, 16% returned to playing sport, which increased to 67% at 6 months and 69% at 12 months (Table 4).
TABLE 4.
Sport Participation
| Before Intervention | After Intervention | |||||
|---|---|---|---|---|---|---|
| 4 wk | 8 wk | 12 wk | 26 wk | 52 wk | ||
| Participation in sport the previous month, number of positive responses/total responses | 51/51 | 7/49 | 4/44 | 7/43 | 28/42 | 27/39 |
| Current sport participation (training + competition per week), median (interquartile range), h/wk | 4 (3-5) | 1 (1-3) | 1.5 (1.0-2.5) | 1.5 (1.0-2.5) | 2 (1-3) | 3 (2-4) |
Physical Activity and Compliance With Exercises
The general linear mixed model showed a significant effect of time (F 2,72 = 6.7; P = .002). On average, participants decreased moderate to vigorous physical activity by 15 minutes per day (95% CI, –33 to 3; P > .05) during activity modification (corresponding to 1 hour 45 minutes per week) and by 37 minutes per day (95% CI, 27 to 38; P < .001) at 12-week follow-up (ie, >4 hours per week). Participants performed the majority of the exercises as prescribed, with a mean exercise frequency of 3.4 to 4.5 sessions per week (Table 5).
TABLE 5.
Compliance With Knee Exercisesa
| Days to Completion | Exercise Sessions in Total | Exercise Sessions per Week | Notes | |
|---|---|---|---|---|
| Block 1 | 4 wk for all | 18 (13-25) | 4.5 (3.3-6.3) | 13 did not report performing any of the exercises in block 1 |
| Exercise progression 1 | 33.5 (17-53) | 15 (8-24) | 3.4 (2.9-3.8) | 11 did not report performing any of the exercises in progression 1 |
| Exercise progression 2 | 25 (11-34) | 11 (5-15) | 3.5 (3.1-3.9) | 22 did not report performing any of the exercises in progression 2 |
| Exercise progression 3 | 19 (15-27) | 9.5 (7-12) | 3.4 (3.2-3.6) | Only 12/51 reached progression 3 (as documented by their training diary) |
aValues are reported as median (interquartile range). Based on data from 38 training diaries.
Hip and Knee Muscle Strength and Jumping Performance
At the 12-week follow-up, there were significant improvements in knee extension strength (32%; P < .001) and hip abduction strength (24%; P < .001). Similarly, there were significant increases in single-leg horizontal jumps (14%; P < .001) and vertical jumps (19%; P < .001).
Use of Medication and Additional Treatments
No participants reported using painkillers at the 12-week follow-up, compared with 12% at baseline (P < .001). There were 2 participants who reported receiving additional treatments between baseline and 12-week follow-up. Additional treatments, types of treatments, and use of painkillers across all time points can be found in Appendix 3.
Satisfaction With Treatment
At the 12-week follow-up, 71% (32/45) were “very satisfied” with the results of treatment. None were “very unsatisfied.” Overall, 43 of 45 (96%) would recommend the intervention to a friend with the same type of knee pain. Furthermore, 29% said that they would be “very satisfied” to live with their current knee symptoms, while 31% said that they would be “very unsatisfied.”
At 12-month follow-up, 67% were “very satisfied” with the results of treatment. Overall, 43% would be “very satisfied” to live with the current level of symptoms, while 2 (5%) would be “very unsatisfied.” When asked, 38 of 42 (90%) would recommend the intervention to a friend with similar knee pain.
Discussion
This is the first study to use an active management strategy focusing on adolescents’ specific deficits and preferences for returning to sport. There were high rates of self-reported successful outcomes (80% at 12 weeks and 90% after 12 months), and knee extension strength reached values similar to those in adolescents without knee pain.18 However, only 16% returned to sport after 12 weeks, which increased to 67% after 6 months. Only 18 of 45 considered themselves completely free from knee pain at 12 weeks, which was similar at 12 months (19/43). This highlights that despite the majority of adolescents reporting that they were improved, one-third still experienced knee pain and continued to be impeded in their sport participation. This is underscored by the fact that at 12-month follow-up, less than 50% (43%) responded that they would be satisfied to live with current symptoms. Due to the long symptom duration at baseline (nearly 2 years), it may be prudent to consider this a long-standing condition, which may in some cases need ongoing management. However, this study indicates that the addition of targeted strength training can offset some of the previously documented long-term negative impacts that this condition can have on strength and function.9
Targeting Sport Participation and Physical Activity
This study targeted sport participation, which is thought to be associated with the development of OSD.8 The intervention was delivered to adolescents and their parents to take into account the unique social and developmental considerations of adolescents. It was thought that engaging parents may help optimize adherence to the intervention.15 Participants reduced their moderate to vigorous physical activity by 15 minutes per day after 4 weeks and 37 minutes per day at 12 weeks. This could indicate that it takes time before they learn how to modify physical activity levels and how it might help them. Only 16% returned to playing sports at 3 months. This is likely because participants were required to reach progression 3 of the exercises before returning to sport. Based on the training diaries, only 12 participants had reached progression 3 by week 12, which should be taken into consideration in future research.
After 12 months, 69% returned to playing sport, although with lower weekly participation than before inclusion. This is in contrast to common expectations from a narrative review that OSD will disappear within 12 to 18 months,6 but it fits well with clinical experience. This may indicate that OSD is not as short-lived as described in the literature (which is supported by the number of participants who were unsatisfied with living with current symptoms and the duration of symptoms at baseline). While the intervention was designed to help adolescents progressively increase in exercises and activities before returning to sport, the paradigm may have impeded return to sport because of the requirements that we imposed on them.
Importantly, the contradiction of adolescents reporting to be much improved while being unable to fully participate in sport requires further research to disentangle and underlines the need for adolescent-specific patient-reported outcome measures. While the EQ-5D-Y index score improved over 12 months, the mean score of 0.82 points at 12-month follow-up is still lower than that of healthy controls in this age group,13,18 indicating a sustained long-term impact of OSD on quality of life during adolescence. The management of OSD may therefore need to continue for an extended period of time, and perhaps more focus should be on longer term outcomes. As approximately one-third did not return to sport within 1 year, and the KOOS Sport and Recreation subscore was 80 points at 12 months, focus is needed to further optimize the management of this long-standing and sport-disabling condition. It seems relevant to investigate who is at highest risk of a poor prognosis and what features categorize these patients. Previous research on adolescents with patellofemoral pain has shown that characteristics of their pain experience (intensity, duration, and frequency of pain), together with quality of life, were associated with a 2-year prognosis.16 Whether these prognostic factors are also valid for adolescents with OSD is unclear.
Adolescents with OSD have shown approximately 30% lower isometric knee extension strength compared to their pain-free peers,18 and deficits may persist after the resolution of symptoms.9 Therefore, progressive strengthening was included in the current study to help offset the sustained impact into adulthood that has previously been documented.20 The exercises were intended to increase muscle strength and stimulate tissue adaptation around the knee. The exercise levels were guided by the patient’s symptoms and progressed to prepare participants for return to sport-specific activities. The intervention increased strength to the same level as adolescents without knee pain.18 Theoretically, this should help prepare adolescents for the physical demands associated with sport. Improvements in jump for height and distance suggest returning to sport-specific activities. Treatments such as stretching, rest, and other passive modalities that are recommended6 neglect this. The strength training component of this intervention may therefore help to ameliorate these previously documented long-term deficits.
Comparison With Previous Studies
The only randomized trial21 compared an injection of local anaesthetic with dextrose with either usual care or local anaesthetic alone. The dextrose group was also advised to reduce sport participation. That study found that the dextrose injection was associated with higher rates of asymptomatic sport participation (3/22 in usual care group vs 14/21 in dextrose group). Because of the combined injection and recommendations on sport participation, it is impossible to disentangle the effective component of the intervention group. The lack of demographic data makes a comparison with the current population difficult.
The longer term outcomes observed in the current study are in line with those of Kujala et al.10 In that retrospective study at a sports medicine clinic in Finland,10 patients diagnosed with OSD were prescribed 2 months of rest as the initial treatment. On average, they had 3.2 months of complete rest from sport because of knee symptoms, and 70% were forced to limit activities for 10.2 months, on average. Kujala et al highlighted the potential long-standing nature of OSD and indicated that rest may not be adequate for all adolescents suffering from OSD. Overall, 50% of their sample continued to experience mild tenderness at the tibial tuberosity even after complete ossification, and 15 of 50 reported pain at the patellar tendon or at the inferior pole of the patella.10
Limitations
This was a noncontrolled study, and specific treatment effects cannot be disentangled from the natural course of the condition. However, the long-term duration of pain complaints at baseline indicates that a quick natural resolution of symptoms is unlikely. Adolescents were diagnosed with OSD at study commencement. It is unclear if adolescents with continued reports of knee pain at 12-month follow-up still had OSD-related knee pain only or if they reported additional pain complaints (as in 15/50 patients from Kujala et al10). Because of the lack of adolescent-specific patient-reported outcome measures for knee pain, we used outcomes that we believed were meaningful to this population and enabled external comparisons. We included 2 functional tests: jump for height and jump for distance. The reliability of these 2 tests is not known for this population. Knee kinematics was not measured, and it is unclear how knee kinematics might have changed during the course of the intervention.
Conclusion
This study implemented an intervention of activity modification, pain monitoring, progressive strengthening, and a return-to-sport paradigm in 51 adolescents with OSD. The subjective and objective measures of knee function and sporting activity improved over 12 months, and 69% of adolescents returned to playing sport after 12 months. This may offer an alternative to passive approaches, which include rest and avoidance of painful activities, but future studies should aim to improve the management of adolescents with OSD and their return to sport and quality of life.
Supplemental Material
Supplemental Material, DS_10.1177_2325967120911106_Appendix_1 for Activity Modification and Knee Strengthening for Osgood-Schlatter Disease: A Prospective Cohort Study by Michael S. Rathleff, Lukasz Winiarski, Kasper Krommes, Thomas Graven-Nielsen, Per Hölmich, Jens Lykkegard Olesen, Sinéad Holden and Kristian Thorborg in Orthopaedic Journal of Sports Medicine
APPENDIX 1
Patient Education Leaflet Used During the Study (English Translation)
See the Supplemental Material published separately online.
APPENDIX 2
Analysis of ActiGraph Data
The ActiGraph is a commercial 3-axis accelerometer, validated for collecting physical activity.2 Participants wore the ActiGraph on the wrist of their nondominant arm, and data were analyzed using ActiLife. Raw data were converted into files with a 10-second epoch length for subsequent validation of wear time and classification of intensity. Nonwear time was defined as bouts of ≥60 minutes of consecutive zero counts, allowing interruptions of up to 2 consecutive nonzero counts (≤100 counts/min). Adolescents were told to record the type of activity missed by the ActiGraph during nonwear. A valid day was defined as 600 valid wear-time minutes per 24 hours, and 4 valid days was the minimum requirement for analysis. The Evenson et al1 cut points were used for categorizing sedentary (0-100 counts/min), light (101-2295 counts/min), moderate (2296-4011 counts/min), and vigorous (≥4012 counts/min) physical activity, as per previous research in children and adolescents.2 The time spent in consecutive sedentary bouts of ≥10 minutes was used to calculate the average weekly sedentary time. In addition, variables were computed to indicate whether participants met the World Health Organization’s weekly physical activity recommendations (ie, >150 minutes of moderate to vigorous physical activity or >75 minutes of vigorous activity).
References
- 1. Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–1565. [DOI] [PubMed] [Google Scholar]
- 2. Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821–1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
APPENDIX 3
Use of Painkillers and Additional Treatmentsa
| No. of Participants | |
|---|---|
| 4 wk (n = 48) | |
| Physical therapy | 2 |
| Treatment (type not specified) | 2 |
| Pain medication | 3 |
| 8 wk (n = 44) | |
| Physical therapy | 1 |
| Treatment (type not specified) | 3 |
| Pain medication | 1 |
| 12 wk (n = 43) | |
| Treatment (type not specified) | 2 |
| Pain medication | 0 |
| 26 wk (n = 42) | |
| Physical therapy | 3 |
| Treatment (type not specified) | 3 |
| Pain medication | 0 |
| 52 wk (n = 41) | |
| Physical therapy | 2 |
| Body Self Development System | 1 |
| Craniosacral therapy | 1 |
| Pain medication | 0 |
aSample sizes refer to the number of participants who responded at each time point.
Footnotes
Final revision submitted December 19, 2019; accepted December 23, 2019.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by the Danish Council for Independent Research (DFF-4004-00247B) and the TRYG Foundation (grant ID: 118547). Center for Neuroplasticity and Pain is supported by the Danish National Research Foundation (DNRF121). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Scientific Ethical Committee of the North Denmark Region (N-2014-0100).
Supplemental Material: Appendix 1 is available at http://journals.sagepub.com/doi/suppl/10.1177/2325967120911106.
References
- 1. Burström K, Egmar AC, Lugnér A, Eriksson M, Svartengren M. A Swedish child-friendly pilot version of the EQ-5D instrument: the development process. Eur J Pub Health. 2011;21(2):171–177. [DOI] [PubMed] [Google Scholar]
- 2. Cairns G, Owen T, Kluzek S, et al. Therapeutic interventions in children and adolescents with patellar tendon related pain: a systematic review. BMJ Open Sport Exerc Med. 2018;4(1):e000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Circi E, Atalay Y, Beyzadeoglu T. Treatment of Osgood-Schlatter disease: review of the literature. Musculoskelet Surg. 2017;101(3):195–200. [DOI] [PubMed] [Google Scholar]
- 4. de Lucena GL, Santos Gomes dos C, Guerra RO. Prevalence and associated factors of Osgood-Schlatter syndrome in a population-based sample of Brazilian adolescents. Am J Sports Med. 2011;39(2):415–420. [DOI] [PubMed] [Google Scholar]
- 5. Elm von E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. [DOI] [PubMed] [Google Scholar]
- 6. Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW. Osgood Schlatter syndrome. Curr Opin Pediatr. 2007;19(1):44–50. [DOI] [PubMed] [Google Scholar]
- 7. Guldhammer C, Rathleff MS, Jensen HP, Holden S. Long-term prognosis and impact of Osgood Schlatter 4 years after diagnosis: a retrospective study. Orthop J Sports Med. 2019;7(10):2325967119878136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hall R, Barber Foss K, Hewett TE, Myer GD. Sport specialization’s association with an increased risk of developing anterior knee pain in adolescent female athletes. J Sport Rehabil. 2015;24(1):31–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kaya DO, Toprak U, Baltaci G, Yosmaoglu B, Ozer H. Long-term functional and sonographic outcomes in Osgood-Schlatter disease. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1131–1139. [DOI] [PubMed] [Google Scholar]
- 10. Kujala UM, Kvist M, Heinonen O. Osgood-Schlatter’s disease in adolescent athletes: retrospective study of incidence and duration. Am J Sports Med. 1985;13(4):236–241. [DOI] [PubMed] [Google Scholar]
- 11. Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821–1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pihlajamäki HK, Mattila VM, Parviainen M, Kiuru MJ, Visuri TI. Long-term outcome after surgical treatment of unresolved Osgood-Schlatter disease in young men. J Bone Joint Surg Am. 2009;91(10):2350–2358. [DOI] [PubMed] [Google Scholar]
- 13. Rathleff CR, Baird WN, Olesen JL, Roos EM, Rasmussen S, Rathleff MS. Hip and knee strength is not affected in 12-16 year old adolescents with patellofemoral pain: a cross-sectional population-based study. PLoS One. 2013;8(11):e79153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rathleff MS, Graven-Nielsen T, Hölmich P, et al. Activity modification and load management of adolescents with patellofemoral pain: a prospective intervention study including 151 adolescents. Am J Sports Med. 2019;47(7):1629–1637. [DOI] [PubMed] [Google Scholar]
- 15. Rathleff MS, Rathleff CR, Holden S, Thorborg K, Olesen JL. Exercise therapy, patient education, and patellar taping in the treatment of adolescents with patellofemoral pain: a prospective pilot study with 6 months follow-up. Pilot Feasibility Stud. 2018;4:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rathleff MS, Rathleff CR, Olesen JL, Rasmussen S, Roos EM. Is knee pain during adolescence a self-limiting condition? Prognosis of patellofemoral pain and other types of knee pain. Am J Sports Med. 2016;44(5):1165–1171. [DOI] [PubMed] [Google Scholar]
- 17. Rathleff MS, Roos EM, Olesen JL, Rasmussen S. Exercise during school hours when added to patient education improves outcome for 2 years in adolescent patellofemoral pain: a cluster randomised trial. Br J Sports Med. 2015;49(6):406–412. [DOI] [PubMed] [Google Scholar]
- 18. Rathleff MS, Winiarski L, Krommes K, et al. Pain, sports participation, and physical function in 10-14 year olds with patellofemoral pain and Osgood Schlatter: a matched cross-sectional study of 252 adolescents. J Orthop Sports Phys Ther. 2020;50(3):149–157. [DOI] [PubMed] [Google Scholar]
- 19. Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ross MD, Villard D. Disability levels of college-aged men with a history of Osgood-Schlatter disease. J Strength Cond Res. 2003;17(4):659–663. [DOI] [PubMed] [Google Scholar]
- 21. Topol GA, Podesta LA, Reeves KD, Raya MF, Fullerton BD, Yeh H-W. Hyperosmolar dextrose injection for recalcitrant Osgood-Schlatter disease. Pediatrics. 2011;128(5):e1121–e1128. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, DS_10.1177_2325967120911106_Appendix_1 for Activity Modification and Knee Strengthening for Osgood-Schlatter Disease: A Prospective Cohort Study by Michael S. Rathleff, Lukasz Winiarski, Kasper Krommes, Thomas Graven-Nielsen, Per Hölmich, Jens Lykkegard Olesen, Sinéad Holden and Kristian Thorborg in Orthopaedic Journal of Sports Medicine