“I would rather be remembered for my paradoxes than for my prejudices.”
René Dubos
The history of antibiotics is usually told as triumph followed by tragedy. First comes the bold promise of the sulpha drugs, then the dawning of the antibiotic era proper with the discovery of streptomycin and the rediscovery of penicillin; then the sobering realisation that these wonder drugs could have an expiry date. In this story of antibiotic hope and “antibiotic abandon”—to borrow James Whorton's prescient phrase—certain scientists and drugs figure prominently: Selman Waksman and streptomycin, but also Gerhard Domagk and prontosil, Howard Florey and penicillin.
Only rarely do historians mention another miracle drug, gramicidin, and the Rockefeller researcher who discovered it, René Dubos. To some extent this is understandable: despite being hailed in 1939 as a “hundred thousand times” more powerful than the sulpha drugs, gramicidin proved highly toxic when administered intravenously and although it was widely used during World War 2 to treat wounds and other topical infections it was soon eclipsed by streptomycin.
However, gramicidin was the first antibacterial agent to emerge from systematic scientific research and, together with tyrothricin, its less pure form, the first to be produced commercially and used clinically. As such, it arguably has a greater claim than streptomycin to have launched the antibiotic revolution. Yet no sooner had Dubos unveiled gramicidin than he withdrew from research in this field, convinced that such antimicrobial agents would only encourage the growth of bacterial resistance. The result was that by 1943 Dubos was advising premedical students not to follow the example of their elder colleagues who practise “the wasteful and inconsiderate use of antibiotics”, and by the late 1950s he was explicitly warning that “at some unpredictable time and in some unforeseeable manner nature will strike back”. Dubos thus presents a paradox for historians of antibiotics, disrupting the triumphant phase of the narrative and foreshadowing the tragedy that follows.
Yet Dubos's role in this history is worth recalling not only because, as his former student, the bacterial geneticist Joshua Lederberg put it in on the occasion of the 50th anniversary of the discovery of gramicidin, it reminds us of “science's immense diversity”, but because Dubos's ecological insights are increasingly relevant to our own “post-antibiotic” times—a period that has not only seen the resurgence of old bacterial scourges, such as tuberculosis, but also the emergence of new infectious disease threats, such as severe acute respiratory syndrome and avian influenza.
To appreciate the impact of Dubos's discovery it is sufficient to recall that in the 1930s nearly all the available chemotherapeutic agents were based on poisonous principles—arsenic, mercury, complex dyes—that were rendered less toxic to animal tissue by chemical substitution or modification. But until Dubos, no one had thought to look for a purifying agent in the ecology of bacteria themselves. Educated at a French agricultural college, Dubos shared Pasteur's faith that germs can impede other germs. However, it was not until 1924 that a chance meeting with Waksman led Dubos to take up an offer to study for a PhD in soil microbiology at Rutgers University in New Jersey, USA. There he became adept at soil chemistry and bacteriology, so much so that when he arrived at the Rockefeller Institute in 1927 to help Oswald Avery's search for an agent that could decompose the polysaccharide capsule of the virulent type III pneumococcus—the leading cause of lobar pneumonia—he was bold enough to suggest he investigate whether such a principle existed in the soil. Accordingly, Dubos fetched mud from a New Jersey cranberry bog and, using a basic chemistry set and a few gardening techniques, cultivated a microbe that removed the pneumococcus capsule with an enzyme he dubbed S-III. By 1930, he and Avery had shown that S-III was able to completely cure mice infected with pneumonia. But just when it looked as if it might be purified into a therapeutic serum to treat humans, the enzyme was eclipsed by Domagk's discovery of prontosil, plunging Avery into despair. Yet it soon became apparent that prontosil and other sulpha drugs were potentially toxic when given in adequate doses, leading Dubos to seek a gentler alternative, and as before he looked to the soil for an answer.
In his earlier experiment, Dubos had observed that the cranberry bog only produced the S-III enzyme when it was fed the polysaccharide capsule and nothing else—an adaptive response that Dubos later called “one of the most important biological laws I have ever been in contact with”. Now, he actively sought to see whether he could train, or domesticate, the microbes in the soil by repeatedly feeding them suspensions of staphylococci and other Gram-positive bacteria. 2 years and countless soil samples later, Dubos was thrilled to see his soil contained a new bacterium, Bacillus brevis, that disintegrated the staphylococci, and from which he was able to isolate gramicidin and tyrothricin.
His announcement at a conference at New York's Waldorf Astoria in 1939 proved a sensation. Holding up a tiny bottle containing 500 g of his new bactericide, Dubos told his audience that it contained enough grey powder to protect 5 trillion mice against pneumonia and streptococcal infections. Never mind that tyrothricin had yet to be tested on humans, as The New York Times put it, Dubos's research “opens up a vast field in the search for chemical agents for fighting bacterial enemies”.
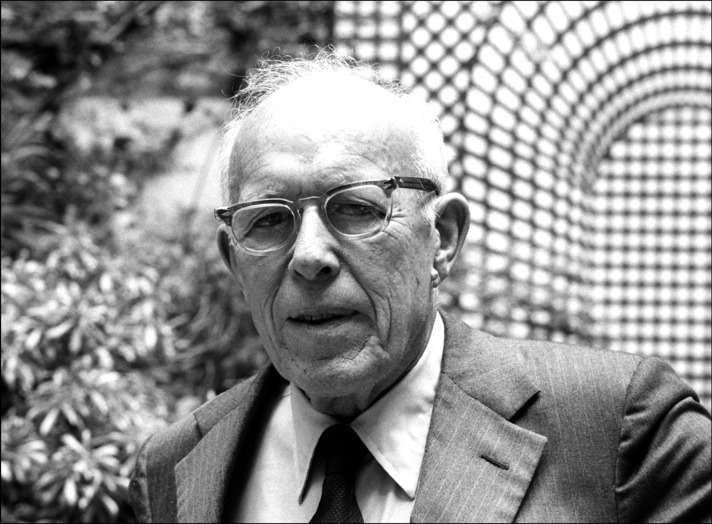
René Dubos (1901–82)
© 2016 Sophie Bassouls/Sygma/Corbis
The fact that Dubos had discovered tyrothricin using “a set of dime-store tumblers” only added to the story's appeal and long after the drug's therapeutic limitations had become apparent, Dubos's discovery was still being billed as “one of the most romantic stories in modern research”. Dubos's announcement also stimulated Florey and Ernst Chain to look further into penicillin and persuaded Waksman to undertake his search using similar soil techniques that led to the eventual isolation of streptomycin. It is no exaggeration to say that no discovery contributed more to the faith in antibiotics and the conviction at mid-20th century that scientific medicine would soon eradicate all infectious diseases than Dubos's. It also established his scientific reputation, earning him the 1948 Lasker Award and election to the US National Academy of Sciences, no small feat for an agriculturally trained Frenchman without a medical degree.
But as Carol Moberg recounts in her biography, Dubos never used the term antibiotic, preferring the term antibacterial, which more accurately reflected his ecological approach and the biological principles he had used in his search for naturally occurring antagonists in the soil, and by 1942 he had abandoned antibiotics research and left the Rockefeller for Harvard. The reasons for Dubos's decision are unclear but seem to be motivated as much by personal reasons as intellectual conviction: while isolating tyrothricin, his wife, Marie Louise, suffered a devastating relapse of tuberculosis, partly, Dubos believed, as a result of the stress of the war and the loss of contact with her family in France, and in 1942 she died. Dubos could not believe that his wife had succumbed to an infection that she had harboured since childhood. Clearly, the tuberculosis bacilli alone could not explain her illness. Instead, Dubos vowed to explore the role of host factors and social and environmental disturbances in the pathogenesis of disease. Marie Louise's death also awakened Dubos's humanistic sensibility. The result is that today Dubos is better remembered for his popular writings linking human health with the environment and his catchphrase, “think globally, act locally”.
It is not only for his pivotal contribution to antibiotics research that Dubos deserves a place in its history. Without his early appreciation of the transformational properties of microbes and the phenomenon of bacterial adaptation, it is unlikely that calls for more rational prescription practices in the face of relentless pharmaceutical marketing in the 20th century would have taken the form they did. Indeed, it was while at Harvard that Dubos drafted The Bacterial Cell, a book that was to have a seminal influence on the next generation of biomedical researchers, including Lederberg. In the book, Dubos challenged the then dominant notion of bacterial fixity and urged bacteriologists to take note of the plasticity of bacteria, warning that the widespread use of chemotherapeutics would favour the production of “unsuspected variants, exhibiting all degrees of drug fastness and of pathogenicity”. However, Dubos's starkest departure from then medical orthodoxy came in his 1959 book, Mirage of Health, in which he compared the faith in antibiotics to “the naïve cowboy philosophy that permeates the wild West thriller” and warned that complete freedom from disease was “almost incompatible with the process of living”.
Antibiotic resistance, particularly to the sulpha drugs, was already widespread by the time Dubos penned these prophetic words. Dubos died in 1982 and therefore did not live to see the widespread community outbreaks of meticillin-resistant Staphylococcus aureus or the resurgence of tuberculosis and pneumonia infections in the wake of AIDS. Fortunately, Lederberg had been paying attention and in the late 1980s he used his position as head of the Rockefeller University to revive Dubos's warnings about the mutability and adaptability of pathogens in the face of shifting disease ecologies and changing social patterns. Although Lederberg's main concern was new viral diseases such as AIDS, in a 1988 address at the Rockefeller he included the evolution of antibiotic resistance within a new category he termed “emergent diseases”. In this way, Lederberg reminded his audience of the relevance of Dubos's ideas to the present and restored him to his place in the history of both antibiotics and disease ecology.
Acknowledgments
Mark Honigsbaum is a Wellcome Trust Research Fellow at Queen Mary University of London. He is currently working on a history of ideas of disease ecology. Research for this article was funded by a grant-in-aid from the Rockefeller Archive Center.
Further reading
- Dubos RJ. Mirage of health. George Allen & Unwin; London: 1959. [Google Scholar]
- Moberg CL. René Dubos, friend of the good earth: microbiologist, medical scientist, environmentalist. ASM Press; Washington, DC: 2005. [Google Scholar]
- Moberg CL, Cohn ZA, editors. Launching the antibiotic era: personal accounts of the discovery and use of the first antibiotics. Rockefeller University Press; New York: 1990. [Google Scholar]
- Podolsky SH. The antibiotic era: reform, resistance, and the pursuit of a rational therapeutics. Johns Hopkins University Press; Baltimore, MD: 2015. [Google Scholar]