Executive summary
The west African Ebola epidemic that began in 2013 exposed deep inadequacies in the national and international institutions responsible for protecting the public from the far-reaching human, social, economic, and political consequences of infectious disease outbreaks. The Ebola epidemic raised a crucial question: what reforms are needed to mend the fragile global system for outbreak prevention and response, rebuild confidence, and prevent future disasters? To address this question, the Harvard Global Health Institute and the London School of Hygiene & Tropical Medicine jointly launched the Independent Panel on the Global Response to Ebola. Panel members from academia, think tanks, and civil society have collectively reviewed the worldwide response to the Ebola outbreak. After difficult and lengthy deliberation, we concluded that major reforms are both warranted and feasible. The Panel's conclusions offer a roadmap of ten interrelated recommendations across four thematic areas:
1. Preventing major disease outbreaks
All countries need a minimum level of core capacity to detect, report, and respond rapidly to outbreaks. The shortage of such capacities in Guinea, Liberia, and Sierra Leone enabled Ebola to develop into a national, and worldwide, crisis.
-
•
Recommendation 1: The global community must agree on a clear strategy to ensure that governments invest domestically in building such capacities and mobilise adequate external support to supplement efforts in poorer countries. This plan must be supported by a transparent central system for tracking and monitoring the results of these resource flows. Additionally, all governments must agree to regular, independent, external assessment of their core capacities.
-
•
Recommendation 2: WHO should promote early reporting of outbreaks by commending countries that rapidly and publicly share information, while publishing lists of countries that delay reporting. Funders should create economic incentives for early reporting by committing to disburse emergency funds rapidly to assist countries when outbreaks strike and compensating for economic losses that might result. Additionally, WHO must confront governments that implement trade and travel restrictions without scientific justification, while developing industry-wide cooperation frameworks to ensure private firms such as airlines and shipping companies continue to provide crucial services during emergencies.
2. Responding to major disease outbreaks
When preventive measures do not succeed, outbreaks can cross borders and surpass national capacities. Ebola exposed WHO as unable to meet its responsibility for responding to such situations and alerting the global community.
-
•
Recommendation 3: A dedicated centre for outbreak response with strong technical capacity, a protected budget, and clear lines of accountability should be created at WHO, governed by a separate Board.
-
•
Recommendation 4: A transparent and politically protected WHO Standing Emergency Committee should be delegated with the responsibility for declaring public health emergencies.
-
•
Recommendation 5: An independent UN Accountability Commission should be created to do system-wide assessments of worldwide responses to major disease outbreaks.
3. Research: production and sharing of data, knowledge, and technology
Rapid knowledge production and dissemination are essential for outbreak prevention and response, but reliable systems for sharing epidemiological, genomic, and clinical data were not established during the Ebola outbreak.
-
•
Recommendation 6: Governments, the scientific research community, industry, and non-governmental organisations must begin to develop a framework of norms and rules operating both during and between outbreaks to enable and accelerate research, govern the conduct of research, and ensure access to the benefits of research.
-
•
Recommendation 7: Additionally, research funders should establish a worldwide research and development financing facility for outbreak-relevant drugs, vaccines, diagnostics, and non-pharmaceutical supplies (such as personal protective equipment) when commercial incentives are not appropriate.
4. Governing the global system for preventing and responding to outbreaks
An effective worldwide response to major outbreaks needs leadership, clarity about roles and responsibilities, and robust measures for accountability, all of which were delayed or absent during the Ebola epidemic.
-
•
Recommendation 8: For a more timely response in the future, we recommend the creation of a Global Health Committee as part of the UN Security Council to expedite high-level leadership and systematically elevate political attention to health issues, recognising health as essential to human security.
-
•
Recommendation 9: Additionally, decisive, time-bound governance reforms will be needed to rebuild trust in WHO in view of its failings during the Ebola epidemic. With respect to outbreak response, WHO should focus on four core functions: supporting national capacity building through technical advice; rapid early response and assessment of outbreaks (including potential emergency declarations); establishing technical norms, standards, and guidance; and convening the global community to set goals, mobilise resources, and negotiate rules. Beyond outbreaks, WHO should maintain its broad definition of health but substantially scale back its expansive range of activities to focus on core functions (to be defined through a process launched by the WHO Executive Board).
-
•
Recommendation 10: The Executive Board should mandate good governance reforms, including establishing a freedom of information policy, an Inspector General's office, and human resource management reform, all to be implemented by an Interim Deputy for Managerial Reform by July 2017. In exchange for successful reforms, governments should finance most of the budget with untied funds in a new deal for a more focused WHO. Finally, member states should insist on a Director-General with the character and capacity to challenge even the most powerful governments when necessary to protect public health.
These ten recommendations are concrete, actionable, and measurable. High-level political leadership is now needed to translate this roadmap into enduring systemic reform so that the catastrophe of the Ebola outbreak will never be repeated.
Introduction
“We do not have the capacity to respond to this crisis on our own. If the international community does not stand up, we will be wiped out. We need your help. We need it now.”
Naimah Jackson, Team Leader, Médecins Sans Frontières Ebola Treatment Center, Monrovia. Address to the UN Security Council, Sept 18, 20141
The west African Ebola epidemic that began in 2013 was a human tragedy that exposed a global community altogether unprepared to help some of the world's poorest countries control a lethal outbreak of infectious disease. The outbreak engendered acts of outstanding courage and solidarity, but also immense human suffering, fear, and chaos, largely unchecked by high-level political leadership or reliable and rapid institutional responses.
The outbreak continues as of November, 2015. It has infected more than 28 000 people and claimed more than 11 000 lives,2 brought national health systems to a halt, rolled back hard-won social and economic gains in a region recovering from civil wars, sparked worldwide panic, and cost several billion dollars in short-term control efforts and economic losses.3, 4 Guinea, Liberia, and Sierra Leone were most badly affected. The Ebola outbreak is a stark reminder of the fragility of health security in an interdependent world, and of the importance of building a more robust global system to protect all people from such risks.5 A more humane, competent, and timely response to future outbreaks needs greater willingness to assist affected populations, and systematic investments to enable the global community to perform four key functions:
-
1.
Strengthen core capacities within and between countries to prevent, detect, and respond to outbreaks when and where they occur.
-
2.
Mobilise faster and more effective external assistance when countries are unable to prevent an outbreak from turning into a crisis.
-
3.
Rapidly produce and widely share relevant knowledge, from community mobilisation strategies to protective measures for health workers, and from epidemiological information to rapid diagnostic tests.
-
4.
Provide stewardship over the whole system, entailing strong leadership, coordination, priority-setting, and robust accountability from all involved.6
The Ebola outbreak emphasised failures in performing all four of these functions. Clarity about roles, responsibilities, and rules—and accountability for adherence to them—is essential in a complex system that must involve local, national, regional, and international actors spanning the public, private, and non-profit sectors. Yet, this clarity and accountability was fundamentally absent. Without addressing these governance issues, we will remain wholly unprepared for the next epidemic, which might very well be more devastating, virulent, and transmissible than Ebola or previous disease outbreaks.7, 8, 9
The Independent Panel on the Global Response to Ebola is a joint initiative of the Harvard Global Health Institute and the London School of Hygiene & Tropical Medicine to review the global community's response to the Ebola outbreak. The 19 members come from academia, think tanks and civil society around the world, with expertise in Ebola, disease outbreaks, public and global health, international law, development and humanitarian assistance, and national and global governance. The Panel took a global, system-wide view with a special focus on rules, roles, and responsibilities to identify changes necessary to prevent and prepare for future outbreaks.
This Panel report outlines the main weaknesses exposed during different phases of the Ebola outbreak, followed by ten concrete, interrelated recommendations across four thematic areas: preventing major disease outbreaks, responding to major disease outbreaks, research—production and sharing of data, knowledge, and technology, and governing the global system, with a focus on WHO.
Our primary goal is to convince high-level political leaders worldwide to make necessary and enduring changes to better prepare for future outbreaks while memories of the human costs of inaction remain vivid and fresh.
Systemic weaknesses exposed by the Ebola outbreak
The Ebola outbreak witnessed many types of failures. For analytical purposes, we divide the epidemic roughly into four phases, underlining the most salient issues that arose.
During the initial phase from December, 2013, to March, 2014, the first infections occurred in a remote rural area of Guinea where no outbreaks of Ebola had previously been identified.10 The lack of capacity in Guinea to detect the virus for several months was a key failure, allowing Ebola eventually to spread to bordering Liberia and Sierra Leone. This phase underscored the problem of inadequate investments in health infrastructure, despite national governments' formal commitments to do so under the International Health Regulations (2005),11 and awareness among donors that many lower income countries would need substantial external support. It also underscored inadequate arrangements between governments and WHO to share, validate, and respond robustly to information on outbreaks.
In March, 2014, a second phase began in which intergovernmental and non-governmental organisations began to respond, starting with Médecins Sans Frontières, which already had teams on the ground. That month, both Guinea and Liberia confirmed Ebola outbreaks to WHO. By March 24, Ebola was confirmed in Conakry, home to more than one in seven Guineans. Two months later Ebola had spread to three capital cities with international airports. Without any approved drugs, vaccines or rapid diagnostic tests, health workers struggled to diagnose patients and provide effective care. Without sufficient protective gear, and initially without widespread understanding of the virus, hundreds of health workers themselves became ill and died. Despite Médecins Sans Frontières' warnings about the unprecedented scope of the outbreak,12 national authorities in Guinea downplayed it for fear of creating panic and disrupting economic activity.12, 13 Internal documents14 suggest similar concerns might have influenced WHO, which publicly characterised the outbreak in March as “relatively small still”.15 WHO's Global Alert and Response Network sent an expert team to support national efforts, as did others such as the US Centers for Disease Control and Prevention. However, those teams withdrew from Guinea and Liberia in May when reported cases decreased, even as viral transmission continued.16 In late May, Sierra Leone became the third country to declare an Ebola outbreak to WHO. For the first time in the known history of Ebola, the virus had spawned sustained outbreaks in three countries. This should have raised substantial alarm, as coordination was weak between the national governments of Liberia, Guinea, and Sierra Leone, the borders extremely porous, and human movement and trade highly fluid. In late June, Médecins Sans Frontières labelled the situation as “out of control” and publicly called for more international attention and resources.17
This second phase witnessed three interrelated failures. First, in a failure of political leadership, some national authorities did not call for greater international assistance despite the humanitarian crisis, and in some cases downplayed the outbreak. Second, WHO's in-country technical capacity was weak, shown by its decision to withdraw its international team too soon and its poor responses in Guinea and Sierra Leone to requests for technical guidance from ministries of health and health-care providers.18, 19 Third, WHO did not mobilise global assistance in countering the epidemic despite ample evidence the outbreak had overwhelmed national and non-governmental capacities—failures in both technical judgment and political leadership.
The third phase began in July as cases, global attention, panic, and responses all grew. Funding increased, with the World Bank committing US$200 million in the first major external financing response.20 Media attention and public interest substantially increased after the evacuation of two infected US aid workers from Liberia.21 Fear and hysteria in response to Ebola infections in the USA later led to quarantines of returning aid workers and other measures counterproductive for controlling the epidemic.22 Dozens of countries, private companies, and universities began implementing travel restrictions, and many airlines ceased flying into the region.23 On Aug 7, WHO convened the International Health Regulations Emergency Committee, and the next day the Director-General officially designated the Ebola outbreak a public health emergency of international concern (“an extraordinary event which is determined...to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response.”11) Detected cases grew exponentially. Ebola treatment centres in all three countries were stretched beyond capacity and forced to turn away patients at their gates.12 A growing lack of trust between population groups and government authorities hindered community mobilisation and public education.24
In the ensuing weeks, the global community mobilised, with new commitments of financing, health personnel, and logistical support from the African Union, China, Cuba, the European Union, the UK, the USA, the World Bank, the International Monetary Fund, and the UN agencies. The UN Security Council passed Resolution 2177 declaring the outbreak a threat to international peace and security, the only time it has done so regarding an outbreak and only the second resolution ever (after HIV/AIDS in 2000) to focus on a disease.25 The UN Secretary General created a new entity to coordinate the international response, the UN Mission for Emergency Ebola Response.26 Additionally, trials for two candidate vaccines were launched in Europe and the USA, and WHO convened an expert group to develop guidance for the ethics of using experimental therapies.27
Despite increased mobilisation of political attention and resources, this third phase witnessed several failures. First, public and private restrictions on trade and travel further harmed an already suffering region and hindered control efforts.16, 28 Second, the operational response commenced slowly, taking months for funding, personnel, and other resources to reach the region.28, 29, 30 Third, the creation of the UN Mission for Emergency Ebola Response bypassed the pre-existing UN body for emergency coordination, the Office for the Coordination of Humanitarian Affairs, further blurring the lines of responsibility for international coordination. Fourth, field staff often reinvented strategies for community mobilisation and contact tracing because relevant lessons from previous Ebola outbreaks in Uganda and the Democratic Republic of Congo were not effectively transferred.31 Fifth, international staff with Ebola sometimes received experimental therapies (albeit, the efficacy and risks of which were unknown) and were evacuated while national staff largely were not, a demoralising and often deadly distinction for many health workers.32, 33 Sixth, there was poor understanding of how to take into account community beliefs, practices, and solutions, properly address rumours, and involve local leaders—with sometimes fatal consequences for health workers and communities.34
A fourth phase began towards the end of 2014 as the epidemic turned a corner. The total number of cases began to decline in the hardest hit countries as community leaders and organisations joined control efforts, even before large-scale global assistance arrived. Ebola had been imported into Nigeria, Mali, and Senegal in the second half of 2014. Nevertheless, rapid information sharing, and mobilisation of health workers for contact tracing and patient care had limited the outbreak in Senegal to one confirmed infection.35 In Nigeria, the Nigerian Center for Disease Control, previous experience with polio eradication efforts and a lead poisoning emergency were all cited as important factors in successful control of the outbreak in Africa's most populous country.36 By the end of January, 2015, more than $5 billion had been committed for the Ebola response (although the proportion of these funds actually spent on Ebola and in the affected countries remains unclear).37 Research and development efforts were quickly operationalised despite uncertainty on processes for regulatory approval, with at least three vaccine candidates, three blood products, and five drug candidates in clinical trials, with WHO playing a coordinating role.38 During this phase, the binding constraints were no longer political attention, funding, or human resources, but operational coordination, accountability for effective use of funds, and maintaining momentum to prevent new infections.
Amidst the crisis, many acts of courage, solidarity, innovation, and leadership prevailed, often at a substantial personal cost. In west Africa more than 800 local health workers contracted Ebola caring for the sick; more than 500 of those caregivers died.39 Community members volunteered to trace contacts, local leaders educated communities, and religious authorities promoted new burial practices to prevent transmission. Several non-governmental organisations vocally advocated for a stronger global response, treated patients, trained health workers, supported community mobilisation and longer-term recovery efforts. Additionally to massive funding from traditional donors, the African Union, the Economic Community of West African States, Cuba, and China made substantial contributions of personnel, funding, logistics, and technology (Huang Y, Council on Foreign Relations, personal communication).40 Private foundations and companies contributed funds, with $245 million from the top five contributors, along with meaningful in-kind assistance, such as air lifts.3 The initiation and conduct of clinical trials were accelerated amidst the challenging conditions of an outbreak, enabled by the cooperative efforts of industry, research funders, regulatory authorities in the USA, Europe, and west Africa, scientists, and directly affected communities.
These positive steps notwithstanding, this Panel's overarching conclusion is that the long-delayed and problematic international response to the outbreak resulted in needless suffering and death, social and economic havoc, and a loss of confidence in national and global institutions. Failures of leadership, solidarity, and systems came to light in each of the four phases (panel 1 ). Recognition of many of these has since spurred proposals for change. We focus on the areas that the Panel identified as needing priority attention and action.
Panel 1. Summary of system weaknesses exposed across four phases of the Ebola outbreak.
Pre-outbreak and Phase 1: December, 2013–March, 2014
-
•
Inadequate national investment and donor support for building national health systems capable of detecting and responding to disease outbreaks
-
•
Inadequate arrangements to monitor country commitments to do so
Phase 2: April, 2014–July, 2014
-
•
Little incentive for countries to report outbreaks early
-
•
Insufficient overall technical capacity among national and international teams
-
•
WHO slow to mobilise global attention or assistance
Phase 3: August, 2014–October, 2014
-
•
Government and private sector disregard for WHO recommendations regarding travel and trade restrictions
-
•
Slow global operational response
-
•
Unclear responsibility for international coordination
-
•
Weak channels for lessons from previous Ebola outbreaks
-
•
Little access to therapies in limited supply, or medical evacuation for national as opposed to international health workers
-
•
Poor understanding of the importance of community engagement
Phase 4: October, 2014–September, 2015
-
•
Weak coordination of global operational response
-
•
Inadequate transparency on resource flows
-
•
Weak accountability for use of funds at all levels
Preventing major disease outbreaks
Preventing small-scale outbreaks from becoming large-scale emergencies needs a minimum level of core capacities in all countries to detect, report, and respond rapidly (panel 2 ). In the wake of the severe acute respiratory syndrome (SARS) outbreak, governments committed to developing such core capacities by 2012 under the revised International Health Regulations (2005), with the 2012 deadline extended for some countries to 2014, then 2019 after Ebola struck. According to self-assessments, as of 2014, two-thirds of countries had not met their core capacity requirements and 48 countries had not responded to WHO queries regarding their readiness.41 The International Health Regulations did not include binding obligations for donors to provide support to poorer countries to meet these obligations, nor to fund WHO to fulfil its mandate to provide technical assistance.42 These shortcomings did not attract serious action or funding until the Ebola outbreak. Despite unprecedented international financing during the past decade to combat particular diseases in developing countries, health systems in many resource-poor settings remain ill-prepared for outbreak response.43 No alternate strategy has been developed to supplement these national-level weaknesses. If countries remain unable to detect outbreaks in a timely way, the rest of the chain of International Health Regulation-stipulated notifications and responses will fail once again.44
Panel 2. Summary of International Health Regulations core capacity requirements for surveillance and response11.
Local community level or primary public health response level
-
•
Detect cases, report cases, and implement immediate control measures
Intermediate public health response levels
-
•
Confirm reported events and support or implement control measures
-
•
Assess reported events and report if appropriate
National level
-
•
Assess all reports of urgent events within 48 h
-
•
Notify WHO immediately
-
•
Determine rapidly the control measures needed to prevent domestic and international spread
-
•
Provide support through specialised staff, laboratory analysis of samples, and logistical assistance
-
•
Provide on-site assistance as needed to supplement local investigations
-
•
Provide a direct operational link with senior health and other officials
-
•
Provide direct liaison with other relevant government ministries
-
•
Provide, by the most efficient means of communication available, information and recommendations received from WHO
-
•
Establish, operate, and maintain a national public health emergency response plan
Additionally, according to the International Health Regulations, countries agreed to report potential health emergencies within 24 h to WHO for joint risk assessment, with the option of doing so confidentially. WHO was also permitted to receive, analyse, and ask for verification of outbreak information received from non-governmental sources. Governments might hesitate to report outbreaks publicly for fear of political and economic repercussions, as occurred in China with SARS in 2003. Yet, history has shown that early reporting is essential to reduce both the health toll of an outbreak and its political and economic consequences. Governments agreed in the International Health Regulations to prompt notification, and in return, were reassured of the curtailment of unwarranted trade or travel restrictions and support from WHO technical assistance. During the Ebola outbreak, however, 40 countries and many private firms implemented restrictions on travel or trade, despite WHO's recommendations against such measures and the Security Council's warnings about the resulting isolation of affected countries.23, 25, 45, 46, 47, 48
We conclude that several concrete steps must be taken to prevent future outbreaks from becoming large-scale catastrophes.
Recommendation 1: Develop a global strategy to invest in, monitor, and sustain national core capacities
WHO should convene governments and other major stakeholders within 6 months to begin developing a clear global strategy to ensure that governments invest domestically in building core capacities and to mobilise adequate external support to supplement efforts in poorer countries.
There is growing momentum in the wake of Ebola for such investments: the US Government has committed $1 billion to build core capacities in at least 30 developing countries, including Guinea, Liberia, and Sierra Leone.49 This work is being coordinated under the Global Health Security Agenda, a US-launched initiative that now consists of nearly 50 countries.50 At its June, 2015, summit, the Group of 7 (G7) announced support for 60 countries, although the G7 did not explicitly commit funds nor agree to a concrete plan.51 Financial commitments for recovery have also been made at various Ebola conferences and summits.52, 53, 54 Other initiatives might also contribute to core capacity building. These include the Gates Foundation's Child Health and Mortality Prevention Surveillance Network,55 the joint Institut Pasteur-China Centers for Disease Control initiative to train west African scientists in outbreak response,56 the Merieux Foundation's laboratory strengthening activities in west Africa,57 and the UK's £195 million Fleming Fund for antimicrobial resistance.58 These welcome signals need to become sustained budget commitments to support national or regional plans, such as the Mano River Union Post-Ebola Socioeconomic Recovery Programme,59 and reviewed systematically beyond this initial phase at forums such as the G7, the G20, and the World Health Assembly. Furthermore, dialogues about health security should not be isolated from broader discussions about development financing, including of the Sustainable Development Goals, as Ebola exposed how substantially an epidemic could roll back hard-won development gains.
A clear, coordinated plan, supported by a transparent central system for tracking and monitoring these resource flows, will be needed to minimise fragmentation and ensure that core capacities are systematically built and sustained. The proposed Accountability Commission for Disease Outbreak Prevention and Response (recommendation 5) should monitor investments and results for core capacity building. Further analysis is needed to estimate the required level of additional funding. Strategic investments for International Health Regulation core capacities can and should also strengthen broader health systems.7, 60 For example, health information systems can support surveillance and monitoring of outbreaks and routine health services; training and payment of community health workers and civil society service providers can help achieve universal health coverage, while providing an essential trained workforce during emergencies.
Additionally, regional and subregional actors should develop capacities to supplement gaps at the national level. For example, in Africa, national governments, the African Development Bank, and other donors should invest in the infrastructural backbone for a network of laboratories, information systems, and training of African national emergency responders based in centres of excellence. The Pan American Health Organization has shown the feasibility of a regional network of centres for disease control, and building such a network could be a central task of the proposed African Centres for Disease Control and Prevention. Although the African Centres for Disease Control and Prevention might be perceived as a competitor to the WHO Regional Office for Africa, a clear delineation of responsibilities for outbreak response versus other health issues should enable close collaboration between the two.
Finally, governments must agree to regular, independent, external assessment of their core capacities. Monitoring requirements should accompany external financing. Assessments will also be needed in self-financing countries. Some governments objected at the 2015 World Health Assembly to independent assessment.61 Nevertheless, a method for peer assessment piloted by five countries through the Global Health Security Agenda could provide a basis for a monitoring process acceptable for all countries.
Recommendation 2: Strengthen incentives for early reporting of outbreaks and science-based justifications for trade and travel restrictions
Political leaders, governments, and international organisations must strengthen the set of incentives and disincentives so that governments report disease outbreaks early. Among these should be stronger disincentives for implementing trade and travel restrictions without a scientific or public health basis.
WHO should promote transparency by publishing lists of countries that delay reporting disease outbreaks, while commending countries that rapidly share public information as Mexico did in 2009 with H1N1. WHO publicly challenged China's Government to be more transparent about SARS, showing the organisation's potential political power. WHO should also publicly disclose lists of countries that implement trade and travel restrictions when WHO Temporary Recommendations advise against them and countries that do not provide a science or public health rationale for such measures (as required by the International Health Regulations). Doing so will require a delicate balancing act between WHO's role as trusted interlocutor with governments on sensitive outbreak-related information, and its role as guardian of the International Health Regulations. Although an individual government might object to such scrutiny in the short term, politically supporting WHO's prerogative to do so serves the long-term interests of global public health.62
Funding bodies such as the World Bank, the Asian Infrastructure Investment Bank, the African Development Bank, and the New Development Bank (previously known as the BRICs Development Bank) should create economic incentives for early reporting by committing to disburse emergency funds rapidly to assist countries when outbreaks strike and compensating for economic losses that might result. The World Bank's proposed Pandemic Emergency Financing Facility or the African Union's African Risk Capacity agency63 offer the possibility of insurance to mitigate the economic costs linked to outbreak reporting. The trigger for disbursement should be a risk assessment done under the aegis of WHO.
Because private firms such as airlines and shipping companies are not directly bound by public international law, alternate governance mechanisms are needed to prevent isolating countries when outbreaks strike. The UN Secretary General should convene relevant industry associations and UN bodies such as the Office for the Coordination of Humanitarian Affairs, WHO, the International Civil Aviation Organization, and the International Maritime Organization to identify crucial services provided by private firms and develop plans to continue such services during emergencies.16 These could include designating a UN focal point for the private sector during outbreaks, designing industry-wide cooperation frameworks, and developing codes of conduct.
Responding to major disease outbreaks
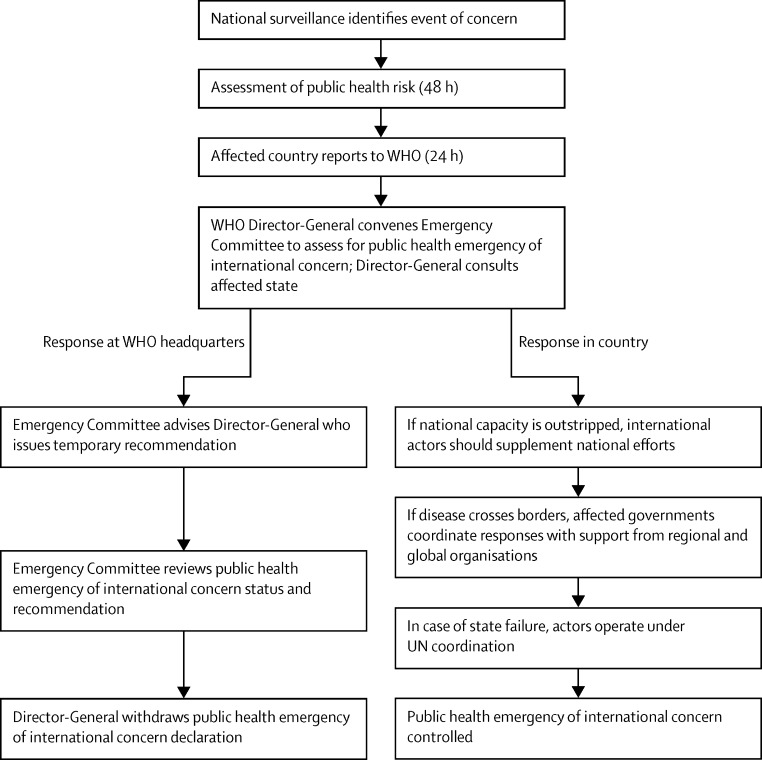
If preventive measures fail and an outbreak escalates into a major crisis, responsibility for taking action and alerting the broader global community must be clearly designated (figure 1 ).
Figure 1.
Current global response system for responding to public health emergencies of international concern11
As noted, countries agreed as part of the International Health Regulations to notify WHO of any potential public health emergency of international concern within 24 h of assessment. WHO rapidly shares information with the Global Alert and Response Network, a loose network coordinated by WHO of academics, government scientists, non-governmental organisations, and health volunteers. The Global Alert and Response Network analyses and assesses reports, deploys investigators, conducts laboratory examination and identification of the outbreak cause, and advises on further measures, including, as a final resort, a potential public health emergency of international concern declaration. However, the Global Alert and Response Network's skeleton staff is too small to deploy in multiple suspected outbreaks, its budget has been severely cut, and it is not authorised by WHO to draw public attention to a crisis.
Responsibility for declaring a public health emergency of international concern belongs to the WHO Director-General, who convenes an Emergency Committee of independent experts for a recommendation. However, the Director-General did not use her International Health Regulation-granted authority to convene the Emergency Committee nor declare a public health emergency of international concern until 5 months after Guinea and Liberia had notified WHO.64 In view of the severity of Ebola virus disease, rapid cross-border spread, weaknesses of the affected national health systems, the post-conflict setting,65 and repeated warnings from non-governmental organisations in the region,12 the Director-General had ample reason to raise international attention by convening the Emergency Committee or declaring a public health emergency of international concern earlier. The committee responsible for reviewing WHO's performance during the Ebola outbreak (the WHO Ebola Interim Assessment Panel) and leaked internal emails suggest several reasons for the delay including concerns about political opposition from west African leaders, economic ramifications, and a culture within WHO discouraging open debate about sensitive issues, such as emergency declarations.14, 64 WHO might also have hesitated because it was sharply criticised for creating panic by declaring a public health emergency of international concern during the relatively mild 2009 H1N1 pandemic.9 Whatever the root causes, the delay emphasised the risks inherent in vesting such consequential decision making power in a single individual. This risk is heightened when there is no institutional mechanism of accountability for leadership failures.
After the public health emergency of international concern declaration, a substantial global response was mobilised. However, this response arrived late, was slow to deliver funds and health workers, was inflexible in adapting to rapidly changing conditions on the ground, was inadequately informed about cultural factors relevant to outbreak control, and was poorly coordinated. The result was, in essence, a $5 billion scramble. An excessive burden fell on national and international non-governmental organisations and local communities to do the highest-risk work such as patient care and burials. The creation of the UN Mission for Emergency Ebola Response as an ad hoc body operating outside established humanitarian response structures reportedly made coordination of the crisis response even more difficult.64, 66 Funding was low until the upsurge of commitments in September, 2014, and, even then, there were long lags between pledges and disbursement. By one account, nearly $3 billion had been pledged by the end of 2014 but only a third of this money was disbursed.69 Furthermore, transparency of financial flows is crucial to minimise duplication, to ensure aid goes to areas of most need rather than those easiest to assist, and to ward against mismanagement. However, transparency was, and remains, wholly inadequate: on the donor side, multiple tracking systems exist but it remains impossible to construct a clear, comprehensive picture of monetary and in-kind pledges and disbursements across the many public and private donors.37 On the recipient side, who received what funds to do which tasks also remains an opaque puzzle—and assessing the effect or efficient use of those funds is more difficult still.
We offer three further recommendations to tackle these issues.
Recommendation 3: Create a unified WHO Centre for Emergency Preparedness and Response with clear responsibility, adequate capacity, and strong lines of accountability
High-level political leaders must clearly designate who is responsible for responding when disease outbreaks outstrip national capacities, invest in the capacity to respond, and ensure accountability for fulfilment of these responsibilities.
Although national governments and non-governmental organisations working on the ground are the first line of defence when outbreaks arise, WHO is crucial for the second line of defence when governments need international support or when an outbreak strikes more than one country. To strengthen WHO's capacity during outbreaks, we welcome the Stocking Panel's recommendation to create a WHO Centre for Emergency Preparedness and Response, and offer several additional recommendations regarding its key functions and attributes.
The centre should merge the outbreak risk assessment and response capacities that reside in the Global Alert and Response Network with WHO's humanitarian teams, which presently respond to natural disasters, refugee crises, and other large catastrophes. Its operational lines of authority from headquarters to regions and countries should be clearly designated. The centre should assess risks on the basis of the information that countries and others provide to WHO, and mobilise necessary laboratory, epidemiological, clinical, communications, and logistical responses. It should have powerful analytical, data processing, and advisory capacity to command respect in both policy and scientific communities. The centre should develop rapid response and strong coordinating capacity, and be able to assemble the world's best expertise to tackle disease threats. Between crises, the centre should develop protocols, build relationships, and negotiate agreements with governments, multilateral organisations, non-governmental organisations, private firms, and other actors to mobilise rapidly during emergencies, including strengthening capacities in developing countries so that they might better respond nationally and participate internationally. In a multicountry outbreak, the centre should ensure government-to-government coordination by establishing channels of direct communication for rapid information sharing. It should be responsible for building a virtual global health workforce from both industrialised and developing countries by setting standards for certifying crisis responders, ranging from communications experts and logisticians to surgeons and managers. These responders would continue working for their home organisations, but provide surge capacity in a crisis. Finally, the centre should provide technical assistance to countries to build and maintain International Health Regulation-mandated core capacities.
The centre should have its own Executive Director who is accountable for performance jointly to a separate Board of Directors and to the Director-General. The multistakeholder Board should include broad representation of governments from each WHO region, scientific expertise including about animal health, operational responders from all sectors, and funders. The Executive Director should inform the Board immediately when the Centre's risk analysis suggests that coordinated international action is needed and mobilise an appropriate response. Similar governing structures have worked effectively for WHO-affiliated entities including the Global Polio Eradication Initiative, the International Agency for Research on Cancer, UNITAID, and the Special Programme for Research and Training in Tropical Diseases.
The centre's budget should be protected and adequately resourced through a dedicated revolving fund. The fund should immediately disburse money for rapid scale-up when a crisis strikes, then be replenished from funds raised for that crisis to be ready for the next one.
The centre and its Board should work closely and routinely with the Director-General so that the highest levels of leadership are constantly aware of evolving disease threats, and can marshal WHO's legal, political, and human resources at regional and country levels when needed. WHO should use its International Health Regulation-granted authority to expedite access to affected sites by technical teams and pressure any state that impedes international responses to, or obscures, disease threats in its territory.
The centre must have access to sensitive outbreak information that countries are required to share with WHO; further analysis is needed as to whether this would require amendment to the International Health Regulations.
A third line of defence will be needed if the initial response does not succeed and an outbreak becomes a humanitarian crisis (eg, a UN level 3 emergency68), threatening not only public health, but also political, economic, and social stability. International coordination of the large-scale effort needed in this case should be done by the Office for the Coordination of Humanitarian Affairs. However, because the Office for the Coordination of Humanitarian Affairs (and most other humanitarian actors) do not specialise in crises precipitated by disease outbreaks, they should develop in-house capacity and a broad coordination framework with the health sector for such emergencies.
Recommendation 4: Broaden responsibility for emergency declarations to a transparent, politically protected Standing Emergency Committee
Member states should amend the International Health Regulations to broaden responsibility for declaring a public health emergency of international concern. The Director-General convenes, and is advised by, an ad hoc Emergency Committee constituted from a list of independent experts; however, authority and responsibility to declare a public health emergency of international concern rests exclusively with the Director-General. We recommend the creation of a Standing Emergency Committee that meets regularly, with the mandate to declare a public health emergency of international concern by a majority vote of its members. The emergency declaration should trigger other actions, such as financial disbursements by development banks, emergency data-sharing and specimen-sharing rules, and emergency regulatory procedures for new drugs, vaccines, and diagnostics (recommendations 6 and 7). The Director-General should chair, communicate, and explain the Standing Emergency Committee's decisions. Following an open call for nominations, the Director-General would appoint the first members; thereafter, the Standing Emergency Committee itself would periodically vote in new members to preserve its independent character. Minutes and votes of Standing Emergency Committee members should be published immediately following each meeting for the sake of transparency, to build external confidence, reduce political interference, and strengthen the committee's hand against resistant states. Similarly to other institutions responsible for technically complex yet politically consequential decisions, such as central banks or drug regulatory authorities, the Standing Emergency Committee must be protected from political pressure that might interfere with its judgment.
The committee should possess high-level public health expertise and base its decisions on scientific principles and evidence, assessing risks for human health, disease spread, and international traffic. The Standing Emergency Committee should have adequate economic expertise to weigh the risks of disrupted trade and travel against those posed by the outbreak and advise on how to ameliorate economic harm.
The Standing Emergency Committee should also issue early warnings of major potential risks on the basis of continuing assessments done by the WHO Centre. The committee should also consider replacing the present binary system, which calls for determining the presence or absence of a public health emergency of international concern, with a graded system of warnings.64 Finally, the Standing Emergency Committee should publish an annual report detailing its activities to ensure public accountability and continued political attention to health threats. The Committee should be financed purely through assessed contributions to protect against undue donor influence.
A committee does not by definition operate more effectively than an individual, and might succumb to risk aversion and dysfunction; nevertheless, the combination of measures described above should provide the Standing Emergency Committee with the autonomy and capacity for credible, authoritative decision making.
Recommendation 5: Institutionalise accountability by creating an independent Accountability Commission for Disease Outbreak Prevention and Response (Accountability Commission)
The UN Secretary General should create an Accountability Commission as an independent body comprised of civil society, academia, and independent experts doing real-time and retrospective system-wide assessment of global responses to major disease outbreaks. The Accountability Commission would track and analyse the contributions and results achieved by national governments, donors, UN agencies, international and national non-governmental organisations, and the private sector. All major actors would be expected to share information promptly with the Accountability Commission about financial, in-kind, or operational contributions; the the Accountability Commission should publish the names of organisations unwilling to share such information. The Accountability Commission would assess aid effectiveness, including funds committed, paid, disbursed, and spent; both short-term and long-term accomplishments achieved with those funds; and the timeliness, effectiveness, cultural appropriateness, and equity of the response for intended beneficiaries. The Accountability Commission should liaise directly with and provide a forum for representatives of communities directly affected by outbreaks. Finally, it should monitor efforts to build and sustain national core capacities.
The Accountability Commission would report to the World Health Assembly and the Security Council's Global Health Committee (recommendation 8), and publish its findings regularly during and after each public health emergency of international concern. After an open call for nominations, the Secretary General would appoint the first members; thereafter, the Accountability Commission itself would periodically vote in new members to preserve its independent character. The Accountability Commission would offer an important multistakeholder platform for various constituencies involved in and affected by disease outbreak responses. This proposal builds on analogous efforts to strengthen system-wide accountability for other global efforts, such as the UN Commission on Information and Accountability for Women's and Children's Health69 and the Independent Monitoring Board of the Global Polio Eradication Initiative, credited with helping to reinvigorate the performance of this effort.70 The Accountability Commission would be a more permanent institution, however, with a broader mandate than these two previous initiatives.
Research: producing and sharing data, knowledge, and technology
Producing and rapidly sharing knowledge during outbreaks is essential. However, reliable systems for rapid transmission of epidemiological, genomic, and clinical data were not established during the Ebola epidemic. Although governments in the three worst affected countries transmitted epidemiological information to WHO, robust channels were not established for direct data exchange and coordination between the three capitals. Although some researchers shared genomic sequencing data early in the outbreak through an open access database, other researchers later withheld such data from the public domain.71 And although care providers and researchers collected thousands of patient samples, now housed in laboratories in west Africa and worldwide, no clear arrangements exist for scientists to access those samples,72 for their safe handling, or to ensure that west African patients benefit from the findings or technology that might result.73
Previous epidemics show that better arrangements are feasible. During the 2003 SARS outbreak, WHO established online systems for data sharing among a worldwide network of scientists, enabling researchers to identify the virus, sequence its genome, and understand its characteristics.74 In 2006, an international consortium of researchers agreed to data sharing norms for influenza, which enabled real-time dissemination and publication of epidemiological and clinical data during H1N1 in 2009.73 The Consortium for the Standardization of Influenza Seroepidemiology helps to coordinate a global community of researchers working on influenza serology. Furthermore, after 4 years of intergovernmental negotiations, the 2011 WHO Pandemic Influenza Preparedness Framework achieved a delicate balance between sharing samples and access to the resulting technology.76, 77 However, no analogous framework exists for other pathogens.
Access to knowledge embodied in the form of technologies has been a particularly difficult issue. As noted, no drugs, vaccines, or rapid diagnostic tests had been approved for Ebola when the outbreak began. Although scientists had identified the virus nearly four decades earlier and basic research had advanced understanding of the disease, Ebola was not an attractive target for industry investment in research and development, nor was it high on the public health research agenda. Somewhat serendipitously, the US and Canadian Governments had years earlier made defence-related investments in Ebola, which meant that university and pharmaceutical industry researchers had developed several experimental drug and vaccine candidates when the outbreak hit.
As noted, clinical trials for vaccines and drugs were launched in record time (with encouraging results for one vaccine candidate reported in July, 2015).78 Nevertheless, the overall research and development effort could have moved faster if there had been investments beforehand to advance candidate products through phase 1 or 2 trials and a system to prioritise the most important technologies. For example, effective rapid point-of-care diagnostics could have enhanced contact tracing, counteracted community resistance and denial, protected health workers, reduced patient loss to follow-up, eased overburdened treatment centres, and supported the continued operation of shipping and airline services. A systematic way of posing and answering operational research questions, such as the relative merits of using intravenous fluids for patient care, would also have strengthened the response. Furthermore, WHO provided valuable technical leadership about the ethics of using unproven therapies, but little guidance on how strictly limited quantities of drugs should be rationed. West African health workers and patients were largely denied access to the stocks sometimes available to international staff.79
In several instances, WHO proved its capacity to lead, convene, coordinate, and establish norms among a broad range of public and private actors on research and development and data sharing. Additionally to its guidance about experimental therapies, WHO convened research and development actors in mid-2014 and late-2014, and again at a global Ebola research and development summit in May, 2015. In July, 2015, WHO also issued guidance about accelerating regulatory approval of technologies in emergencies. WHO also convened a meeting in September, 2015, to build norms for open data sharing as part of an effort to develop a “blueprint” to guide the collective research and development efforts of industry and governments for emergencies. These successful efforts should be institutionalised to better govern knowledge production and sharing in future outbreaks.
Recommendation 6: Develop a framework of rules to enable, govern and ensure access to the benefits of research
Before the 2016 World Health Assembly, WHO should convene governments, the scientific research community, industry and non-governmental organisations to begin developing a framework of norms and rules for research relevant to disease outbreaks. The framework's goal would be to provide guidance on three interrelated issues:
-
1.
Access to data and samples to enable and accelerate research, which would involve rapid sharing of epidemiological surveillance and clinical data to inform outbreak control strategies; incentives and platforms for open sharing and access to genomic sequencing data; access to specimen samples (with appropriate biosafety measures).
-
2.
Appropriate conduct of research, including improved ethical standards for research and development (eg, including involving affected populations in setting research priorities, patient participation and consent); previous agreement about experimental protocols, such as trial design, to speed clinical trials when outbreaks strike;80 access to clinical trial data, such as publication of negative and positive results; clear pathways for approval by stringent regulatory authorities and in countries of use; and building on and investing in research capacities in epidemic-affected countries.
-
3.
Equitable access to the benefits of research, including priority, affordable access to newly developed health technologies for affected populations, including health workers; and ethical guidelines for rationing products with limited availability.
An overarching framework is needed to bring coherence and fill gaps in the fragmented system of international rules shaping outbreak-related research (including the International Health Regulations, Pandemic Influenza Preparedness Framework, Convention on Biological Diversity and its Nagoya Protocol, Agreement on Trade Related Aspects of Intellectual Property Rights, and numerous guidelines and agreements for data ownership and sharing among scientists). The framework would include both non-binding norms such as guidelines or codes of conduct, and binding rules such as contractual obligations or international law. Further analysis is needed to specify the most appropriate instruments for each issue area.
Some norms would apply at all times to prepare for potential outbreaks; others could be limited to and triggered by a public health emergency of international concern declaration. Establishment of such norms in advance would strengthen preparedness and reduce counter-productive competition between researchers or institutions during emergencies.
Ideally, such a normative framework would cover all pathogens with the potential to cause major outbreaks. However, in view of the complexity and political difficulties reaching agreement on these issues, a feasible starting point might be to develop a pilot framework for one or several diseases such as viral haemorrhagic fevers. Lessons from this pilot could subsequently be applied to expanding the framework to other pathogens. The Accountability Commission (recommendation 5) should monitor progress towards developing this framework and subsequently monitor adherence to it.
Recommendation 7: Establish a global facility to finance, accelerate, and prioritise research and development
The UN Secretary General and the WHO Director-General should convene in 2016 a high-level summit of public, private, and not-for-profit research funders to establish a global financing facility for research and development for health technology relevant for major disease outbreaks. The facility would support manufacturing, research, and development for drugs, vaccines, diagnostics, and other non-pharmaceutical supplies (such as personal protective equipment) where the commercial market does not offer appropriate incentives. For known pathogens, the facility could invest in bringing candidate drugs, vaccines, technology platforms, and other relevant products through proof of concept, phase 1, and phase 2 testing in humans, so that they are ready for wider testing, manufacturing, and distribution when an outbreak strikes. During an outbreak the facility would rapidly mobilise finance for priority research and development projects, such as diagnostics for novel pathogens.
The establishment of a similar fund for diseases affecting developing countries was a central recommendation of the 2012 report of the WHO Consultative Expert Working Group on research and development.81 As a result, a pooled international fund was created to support “demonstration projects” that test new research and development business models, such as open knowledge innovation and de-linkage of research and development financing from end product prices. With a management structure already established, the demonstration projects offer an important option for pursuing research and development for Ebola or other diseases.
The global financing facility should be a lean, efficient entity that mobilises and strategically deploys resources. It would not be a monolithic entity nor the sole funder for epidemic-related research and development because some pluralism and competition among funders is desirable. Nevertheless, a global facility would offer the advantage of enabling coordination between different research funders through a common framework, strengthening networks between researchers, establishing processes for priority setting, and reducing transaction costs for both grantees and smaller donors.82, 83 It could also require information sharing between researchers as a condition of funding, thereby giving teeth to the data-sharing framework (recommendation 6). Intellectual property or any other asset resulting from these investments should be managed as a public good to enable follow-on innovation, open knowledge sharing, access to technology, and a fair public return on investment. Support for a global research and development financing mechanism now seems to be growing, as shown in calls for a $2 billion global fund for vaccine development for pandemics,82 a $2 billion global fund for antimicrobial resistance,84 and a $2–3 billion global fund that would cover emerging infectious diseases, neglected diseases, and antimicrobial resistance.85
Governing the global system for preventing and responding to outbreaks
An effective global system for preventing and responding to outbreaks needs well coordinated and appropriately resourced actors to fulfil clearly defined roles and responsibilities and to hold each other accountable for doing so (table ). Many actors have crucial roles in this complex system: national governments have the main responsibility for their populations' health. National governments are also responsible for immediately sharing information with neighbouring countries and the international community in the event of a potential public health emergency of international concern. They also hold responsibility for calling for international assistance if domestic capabilities prove inadequate.
Table.
Roles of WHO and other organisations in disease outbreaks
| Role of WHO | Roles of other organisations | |
|---|---|---|
| Capacity building function | ||
| Strengthen core capacities within and between countries to prevent, detect, and respond to outbreaks | Support governments with technical and scientific knowledge and advice | Financing by major public and private donors; technical assistance by specialised agencies and non-governmental organisations |
| Support function | ||
| Mobilise external assistance when countries unable to prevent an outbreak from becoming a crisis | Raise awareness of major disease events; declare public health emergencies of international concern as appropriate; early-stage rapid response to outbreaks; convening for resource mobilisation | Financing by development banks, Global Fund, and GAVI; financing by other major public and private donors; operations by UN humanitarian aid agencies, NGOs, and foreign medical teams; advocacy by civil society |
| Knowledge function | ||
| Rapidly produce and widely share relevant knowledge (eg, community mobilisation strategies, protective measures for health workers, epidemiological data, and rapid diagnostic tests) | Assess disease threats worldwide; establish technical norms, standards, and guidance; convene to negotiate rules for knowledge sharing | Knowledge production by non-governmental organisations, community leaders, social scientists, research funders, scientific researchers, pharmaceutical industry, and academia |
| Stewardship function | ||
| Leadership | Political, scientific, technical leadership | All leaders |
| Coordination | Coordinate early outbreak response; convening stakeholders to resolve conflicts and negotiate rules | UN coordination if outbreak becomes a humanitarian crisis |
| Priority-setting | Convening stakeholders to set priorities | .. |
| Accountability | Hold governments accountable for adherence to International Health Regulations | Civil society and media |
In turn, international actors are responsible for supporting national governments individually and collectively. WHO should play a central part in monitoring, assessing, and responding to disease outbreaks. National and regional agencies for disease control and academies of science also offer important technical capacities for managing outbreaks. Development banks are responsible for mobilising and disbursing financing to support governments and collective action. The international humanitarian system, including the Office for the Coordination of Humanitarian Affairs, UNICEF, the World Food Programme, the UN High Commissioner for Refugees, other UN bodies, and non-governmental organisations are responsible for mounting an effective operational response if an outbreak escalates into a humanitarian crisis. The research community is responsible for producing relevant knowledge on the outbreak, and developing and producing technologies to intervene. Civil society, including academia and the media, play a crucial part in drawing attention to unmet needs, neglected challenges, and systemic failings, and demanding accountability from responsible actors. Finally, the UN Security Council is responsible for addressing threats to international peace and security.
Ebola developed from a relatively small outbreak into a large-scale emergency because of the failures of multiple actors to fulfil their mandated roles and responsibilities. Our final three recommendations outline the institutional changes needed to prevent such failures from recurring.
Recommendation 8: Sustain high-level political attention through a Global Health Committee of the Security Council
In recognition of health as an essential facet of human and national security, the UN Security Council should establish a Global Health Committee consisting of government representatives. The Committee's main goal would be to expedite and elevate political attention to health issues posing a serious risk to international peace and security and provide a prominent arena to mobilise political leadership. Specifically, the Committee would monitor and publish an annual report on progress in building a strong and effective global health security system, taking into account analyses from the Accountability Commission and WHO. The Committee would also address alleged non-compliance with International Health Regulation provisions on trade and travel measures. The Committee would not declare public health emergencies of international concern. This decision would remain technically driven and under the authority of WHO. The Committee would not be able to veto WHO decisions or reports of the Accountability Commission. Rather, the Committee's main role would be as an arena for high-level attention to health threats and a forum for problems not adequately resolved by the WHO governing bodies.
WHO in the global system
WHO is an essential hub in the global system for health security. However, evidence of confusion and disagreement about its role is ample.86 Since the 19th century, cross-border disease control was the first and most widely accepted rationale for intergovernmental health cooperation.87 Yet, in the wake of the global financial crisis when WHO laid off more than a tenth of its headquarters staff, outbreak response capacity was deeply and disproportionately cut.88 Disease outbreaks are not the only important work for WHO, but they are foundational to the organisation's mandate.
Within a global system for disease outbreak response, what should be WHO's essential role? WHO's near-universal state membership, governance structure, and deep relationships with health ministries situate it uniquely to perform four core functions (table): support governments in building national core capacities for prevention, surveillance, and response through technical and scientific knowledge and advice; assess and provide rapid early response to outbreaks, raise awareness of major disease events, and declare public health emergencies of international concern when appropriate; establish technical norms, standards and guidance; and convene actors to set goals, mobilise resources, resolve conflicts, and negotiate rules. Performance of these functions needs strong political, scientific, and normative leadership with solid backing from member states.
However, WHO's failings on these core functions during the Ebola outbreak have now produced an existential crisis of confidence. Ebola exacerbated a trend since the 1990s of many governments and other organisations working around WHO. Decades of reducing assessed contributions in real terms has starved the organisation of resources. Donors have earmarked voluntary contributions, effectively controlling nearly 80% of WHO's budget by 2015.89 The result is an organisation that seems to have lost its way. Although the budget has more than doubled from US$1·6 billion in 1998–99 to US$4 billion in 2012–13, the organisation itself controlled an ever-shrinking share. One casualty of recent decisions was WHO's reduced ability to control cross-border disease outbreaks, a core task for which it was created in 1948.
In the wake of Ebola, the organisation's traditional claims of legitimacy based on near-universal state membership no longer seem sufficient. A true recovery will need far greater willingness by member states to entrust resources and delegate authority to WHO, but it has rarely been in a weaker position to command such trust and authority. Confidence in the organisation's capacity to lead is at an all-time low. Calling for additional staff or a larger budget will not address this. WHO must find a way to prioritise what it does, and regain its credibility, independence, and legitimacy to perform its core functions (table). Breaking out of this 20-year impasse will demand clear commitment and a different kind of leadership by WHO to implement fundamental reforms under a tight timeline, matched by an equally clear commitment by member states to reward such reform with appropriate authority and resources. WHO performed a key coordinating function in research and development during the Ebola epidemic. It was also central to controlling nine previous Ebola outbreaks, SARS, and other epidemics. These examples are important reminders of what WHO can do under determined leadership. WHO is in a formal reform process that was spurred by a budget crisis in 2011; in some ways, it has been in a perennial process of reform since at least the 1990s. These previous efforts are a reminder that high-level political leadership, such as the engagement of heads of state, will be needed if the outcome is to be different this time. At this point, anything less than fundamental reform will mean continued marginalisation and decline, alongside increasing vulnerability for global public health.
Recommendation 9: A new deal for a more focused, appropriately financed WHO
To rebuild trust, respect, and confidence within the international community, WHO should maintain its broad definition of health, but substantially scale back its expansive range of activities to focus on core functions. The scope of WHO's work would thus continue to embrace the full range of health issues, but its functions should be far more circumscribed. We restrict our analysis to core functions in infectious disease outbreaks. However, there remains the need to define WHO's core functions in other key areas of work, such as non-communicable diseases, injuries, environmental health, health systems, and social determinants of health. For this purpose, the January 2016 Executive Board should launch a fundamental review of the organisation's constitution and mandate to define its core functions. This review should identify and hand over non-core activities to other actors, thereby streamlining WHO's activities. It should also examine which core functions are not being fulfilled or adequately funded.
The financing model for WHO is unstable and politically vulnerable. The January 2016 Executive Board should also begin developing a new financing model for assessed contributions focused on core functions and draft a transparently implemented policy about when to accept or reject voluntary contributions at headquarters, regional, and country offices. If WHO strictly defines its core functions and accelerates other good governance reforms (recommendation 10), member states should shift most of its financing to assessed and non-earmarked voluntary contributions.
Recommendation 10: Good governance of WHO through decisive, timebound reform, and assertive leadership
Restoring credibility demands that WHO institutionalises accountability mechanisms, strengthens and clarifies how it works with other actors, and fosters strong leadership. The January 2016 Executive Board should launch a process to implement four new policies for WHO to meet basic principles of good governance: establish a freedom of information policy, with appropriate safeguards; create a permanent Inspector General's office to monitor overall performance of the organisation and its entities, reporting to the Executive Board; conclude continuing work on the Framework of Engagement with Non-State Actors to better govern the way WHO interacts with civil society, academia, foundations, and the private sector; and revise human resource policies to attract or retain well qualified staff, including for leadership positions, while letting go of chronic underperformers.
The Executive Board should seize the short window of opportunity available for such reforms by giving a strong mandate to an Interim Deputy for Managerial Reform reporting to the Director-General to implement these policies by July, 2017 (before the next Director-General takes office). In line with the reformed approach to human resources, all upcoming leadership selection and election processes at headquarters, regional, and country offices should be based on personal, technical, and leadership merits. The Executive Board, with the participation of civil society, should do an annual appraisal of senior leadership to strengthen accountability.
As the next Director-General election approaches, member states should insist on a dynamic leader with a strong record of focusing on people, able to manage crises, implement reforms, and communicate strategically. A key attribute should be proven high-level political leadership with the character and capacity to challenge even the most powerful governments when necessary to protect public health. It is in the collective interest of member states to have a strong, empowered leader heading the WHO.
Conclusion
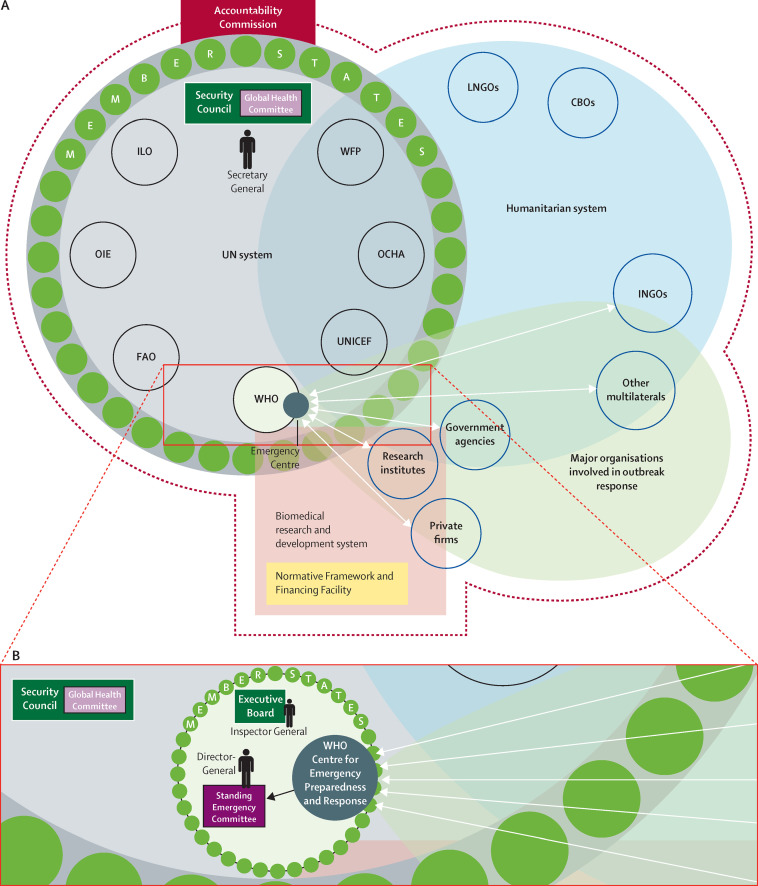
Taken together, the Panel's ten recommendations provide a vision for a more robust, resilient global system able to manage infectious disease outbreaks (panel 3 , figure 2 ). Preventing small outbreaks from becoming large-scale emergencies demands investment in minimum capacities in all countries and encouragement of early international reporting of outbreaks by adhering to agreed international rules. Responding effectively to outbreaks demands much stronger operational capacity within WHO and within the broader aid system if outbreaks escalate into humanitarian emergencies, a politically protected process for WHO's emergency declarations, and strong mechanisms for the accountability of all involved actors, from national governments to non-governmental organisations and from UN agencies to the private sector. Mobilisation of the knowledge needed to combat outbreaks will require an international framework of rules to enable, govern, and ensure access to the benefits of research, and financing to develop technology when commercial incentives are inappropriate. Finally, effective governance of this complex global system demands high-level political leadership and a WHO that is more focused and appropriately financed and whose credibility is restored through the implementation of good governance reforms and assertive leadership.
Panel 3. Summary of recommendations.
Preventing major outbreaks
-
1.
Develop a global strategy to invest in, monitor, and sustain national core capacities
-
2.
Strengthen incentives for early reporting of outbreaks and science-based justifications for trade and travel restrictions
Responding to major outbreaks
-
3.
Create a unified WHO Centre for Emergency Preparedness and Response with clear responsibility, adequate capacity, and strong lines of accountability
-
4.
Broaden responsibility for emergency declarations to a transparent, politically protected Standing Emergency Committee
-
5.
Institutionalise accountability by creating an independent Accountability Commission for Disease Outbreak Prevention and Response
Research: producing and sharing data, knowledge, and technology
-
6.
Develop a framework of rules to enable, govern, and ensure access to the benefits of research
-
7.
Establish a global facility to finance, accelerate, and prioritise research and development
Governing the global system
-
8.
Sustain high-level political attention through a Global Health Committee of the Security Council
-
9.
A new deal for a more focused, appropriately financed WHO
-
10.
Good governance of WHO through decisive, time bound reform and assertive leadership
Figure 2.
Framework of reform proposals
(A) Outbreak response involves several overlapping systems, including the humanitarian system, the UN System, and the biomedical and research development system. The scope of the proposed Accountability Commission would include all of these. Examples of organisations within each system are shown. ILO=International Labour Organisation. OIE=World Organisation for Animal Health. FAO=Food and Agriculture Organisation. OCHA=Office for the Coordination of Humanitarian Affairs. WFP=World Food Programme. LNGOs=local non-governmental organisations. CBO=community-based organisations. INGOs=international non-governmental organisations. (B) Taking a closer look within the WHO, several changes are proposed. The proposed Centre for Emergency Preparedness and Response would sit within WHO, coordinating the many actors involved in global outbreak response and sharing and receiving information with those actors. The Centre's governing Board is to be comprised of member states and non-state actors. The creation of a Standing Emergency Committee would replace the current ad hoc International Health Regulation Emergency Committee. The Standing Emergency Committee will meet and receive information from the Emergency Centre regularly, with the mandate to declare a public health emergency of international concern by a majority vote of its members. The Director-General would chair this committee. A permanent Inspector General's office is proposed, along with other good governance reforms (not depicted in the figure) such as a freedom of information policy.
The human catastrophe of the Ebola epidemic that began in 2013 shocked the world's conscience and created an unprecedented crisis. It exposed deep inadequacies in the national and international institutions responsible for protecting the public from the far-reaching human, social, economic and political consequences of disease outbreaks. The reputation and credibility of WHO has suffered a particularly fierce blow. Ebola brought to the forefront a central question: is major reform of international institutions feasible to restore confidence and prevent future catastrophes? Or should leaders conclude the system is beyond repair and take ad hoc measures when the next major outbreak strikes?
After difficult and lengthy deliberation, our Panel concluded major reforms are warranted and feasible. The Panel refined its recommendations into a roadmap of ten interrelated reforms that in combination can strengthen the global system for outbreak prevention and response.
The roadmap gives greatest weight to clarification of the roles and responsibilities of the many actors involved in outbreak response, investing in capacities to fulfil those roles, and demanding accountability for meeting those responsibilities. These measures are concrete, actionable, and measurable. Success requires one other essential ingredient: high-level political leadership determined to translate this roadmap into enduring systemic reform so that the immense human suffering of the Ebola outbreak will not be repeated.
Acknowledgments
Acknowledgments
We thank Julio Frenk for initial discussions that led to the creation of the Panel, and Robert Marten and the Rockefeller Foundation for supporting the London meeting of the Panel, and research and dissemination efforts. We are grateful to Emily Anne Robinson for research and organisational support for the Boston meeting, and to Zoe Mark Lyon for research support.
Contributors
All authors contributed to study concept, data analysis and interpretation, and provided critical revisions of the manuscript for important intellectual content. PP, AKJ, MAP, and DS chaired and co-chaired the Panel, respectively, providing high level content and directional oversight. SM supervised the study design, data collection, data analysis, and data interpretation; drafted the manuscript; and led all revisions. BH, JAL, and LRW contributed to the data collection, data analysis and data interpretation; creation of figures; and provided administrative, technical, and material support.
Declaration of interests
AKJ, SM, and LRW report a grant from the Rockefeller Foundation supporting the conduct of the study. SM additionally serves on the Board of Directors of Doctors Without Borders/Médecins Sans Frontières (MSF), USA. DS reports serving on the Board of Trustees of Save the Children (UK). CC reports her roles as Vice Chair of the Board, Clinton Foundation and Member of the Board, Clinton Health Access Initiative. LOG is a Commission Member of the Global Health Risk Framework Commission (international, independent, multi-stakeholder expert commission, National Academy of Medicine Secretariat, Director of WHO Collaborating Center on Global Health Law and Human Rights, and an Advisor on the UN High-Level Panel on Global Response to Health Crises. GML is a Commission Member of the Global Health Risk Framework Commission and contributes to the work of the UN High Level Panel on Global Response to Health Crises. MT reports a grant and travel funding from GlaxoSmithKline, the Malaria Vaccine Initiative, the Bill & Melinda Gates Foundation, and is a member of the Board of the Optimus Foundation and the Scientific Advisory Board of the Novartis Institute for Tropical Diseases. SD was former Executive Director of Doctors Without Borders/Médecins Sans Frontières (MSF) USA. PP reports grants from the Bill & Melinda Gates Foundation, UNAIDS, the UK Department for International Development, and the European Commission's Innovative Medicines Initiative, and is a Board member of Biocartis. All other authors declare no competing interests.
References
- 1.Naimah JKP. MSF addresses UN Security Council emergency session on Ebola. 2014. http://www.msf.org/article/msf-addresses-un-security-council-emergency-session-ebola (accessed Aug 19, 2015).
- 2.WHO Ebola situation reports. 2015. http://apps.who.int/ebola/ebola-situation-reports (accessed Oct 7, 2015).
- 3.UN Office of the Special Envoy on Ebola Resources for Results III. 2015. https://ebolaresponse.un.org/sites/default/files/rriii_finalf_updated.pdf (accessed Aug 19, 2015).
- 4.Financial Tracking Service Appeal: Ebola virus outbreak—overview of needs and requirements (inter-agency plan for Guinea, Liberia, Sierra Leone, region). October 2014–June 2015. https://fts.unocha.org/pageloader.aspx?page=emerg-emergencyDetails&emergID=16506 (accessed July 28, 2015).
- 5.Heymann DL, Chen L, Takemi K. Global health security: the wider lessons from the west African Ebola virus disease epidemic. Lancet. 2015;385:1884–1901. doi: 10.1016/S0140-6736(15)60858-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frenk J, Moon S. Governance challenges in global health. N Engl J Med. 2013;368:936–942. doi: 10.1056/NEJMra1109339. [DOI] [PubMed] [Google Scholar]
- 7.Gates B. The next epidemic—lessons from Ebola. N Engl J Med. 2015;372:1381–1384. doi: 10.1056/NEJMp1502918. [DOI] [PubMed] [Google Scholar]
- 8.World Bank Group Preparing for the Next Outbreak. 2015. http://pubdocs.worldbank.org/pubdocs/publicdoc/2015/7/267501437591636421/Preparing-for-the-Next-Outbreak-FINAL-English.pdf (accessed Aug 20, 2015).
- 9.Report of the Review Committee on the functioning of the International Health Regulations (2005) in relation to Pandemic (H1N1) 2009. http://apps.who.int/gb/ebwha/pdf_files/WHA64/A64_10-en.pdf (accessed April 5, 2015).
- 10.WHO Ground zero in Guinea: the outbreak smoulders—undetected—for more than 3 months. 2015. http://www.who.int/csr/disease/ebola/ebola-6-months/guinea/en/ (accessed July 29, 2015).
- 11.WHO . International Health Regulations. World Health Organization; Geneva: 2005. [Google Scholar]
- 12.Médecins Sans Frontières Pushed to the limit and beyond: a year into the largest ever Ebola outbreak. 2015. http://www.msf.org.uk/sites/uk/files/ebola_pushed_to_the_limit_and_beyond.pdf (accessed May 29, 2015).
- 13.Frontline PBS. Outbreak. Inside the troubled early days of Guinea's Ebola response. 2015. http://www.pbs.org/wgbh/pages/frontline/health-science-technology/outbreak/watch-inside-the-troubled-early-days-of-guineas-ebola-response/ (accessed Aug 19, 2015).
- 14.Cheng M, Satter F. Emails: UN health agency resisted declaring Ebola emergency. 2015. http://bigstory.ap.org/article/2489c78bff86463589b41f3faaea5ab2/emails-un-health-agency-resisted-declaring-ebola-emergency (accessed April 29, 2015).
- 15.Samb S. WHO says Guinea Ebola outbreak small as MSF slams international response. 2014. http://www.reuters.com/article/2014/04/01/us-guinea-ebola-idUSBREA301X120140401 (accessed April 29, 2015).
- 16.Garrett L. Ebola's lessons: how the WHO mishandled the crisis. 2015. https://www.foreignaffairs.com/articles/west-africa/2015-08-18/ebola-s-lessons
- 17.Doctors Without Borders Canada/Médecins Sans Frontières (MSF) Canada Ebola in west Africa: “the epidemic is out of control.”. 2014. http://www.msf.ca/en/article/ebola-west-africa-epidemic-out-control (accessed April 29, 2015).
- 18.Cheng M, Satter R, Larson KAP. Investigation: bungling by UN agency hurt Ebola response. 2015. http://bigstory.ap.org/article/3ba4599fdd754cd28b93a31b7345ca8b/ap-investigation-bungling-un-agency-hurt-ebola-response (accessed Sept 20, 2015).
- 19.Reuters AHF: failed global Ebola response demands new leadership. 2015. http://uk.reuters.com/article/2015/02/24/ca-ahf-ebola-response-idUKnBw245381a+100+BSW20150224 (accessed Aug 19, 2015).
- 20.The World Bank Ebola: World Bank Group mobilizes emergency funding to fight epidemic in west Africa. 2014. http://www.worldbank.org/en/news/press-release/2014/08/04/ebola-world-bank-group-mobilizes-emergency-funding-for-guinea-liberia-and-sierra-leone-to-fight-epidemic (accessed April 29, 2015).
- 21.Belluz J, Hoffman S. Why we fail at stopping outbreaks like Ebola. 2014. http://www.vox.com/2014/9/30/6843117/slow-ebola-virus-epidemic-response-WHO-after-brantly-Americans-infected/in/5740388 (accessed April 29, 2015).
- 22.Yale Global Health Justice Partnership and American Civil Liberties Union . Fear, Politics, and Ebola How Quarantines Hurt the Fight Against Ebola and Violate the Constitution. Yale Global Health Justice Partnership; Connecticut: 2015. [Google Scholar]
- 23.WHO Statement on the 1st meeting of the IHR Emergency Committee on the 2014 Ebola outbreak in west Africa. 2014. http://www.who.int/mediacentre/news/statements/2014/ebola-20140808/en/ (accessed April 29, 2015).
- 24.MacDougall C. Liberia's military tries to remedy tension over Ebola quarantine. The New York Times; Monrovia: 2015. [Google Scholar]
- 25.UN Security Council With spread of Ebola outpacing response, Security Council adopts resolution 2177 (2014) urging immediate action, end to isolation of affected states. 2014. http://www.un.org/press/en/2014/sc11566.doc.htm (accessed June 22, 2015).
- 26.Special Representative of the UN Secretary General arrives in Accra to establish the UN Mission for Ebola Emergency Response Headquarters. United Nations; New York: 2014. [Google Scholar]
- 27.WHO . Ethical considerations for use of unregistered interventions for Ebola virus disease. WHO; Geneva: 2014. [Google Scholar]
- 28.Nierle T, Jochum B. Ebola: the failures of the international outbreak response. 2014. http://www.msf.org/article/ebola-failures-international-outbreak-response (accessed Aug 20, 2015).
- 29.Grépin KA. International donations to the Ebola virus outbreak: too little, too late? BMJ. 2015;350:h376. doi: 10.1136/bmj.h376. [DOI] [PubMed] [Google Scholar]
- 30.Gettleman J. As Ebola rages, poor planning thwarts efforts. The New York Times; New York: 2014. [Google Scholar]
- 31.Abramowitz SA, McLean KE, McKune SL. Community-centered responses to Ebola in urban Liberia: the view from below. PLoS Negl Trop Dis. 2015;9:e0003706. doi: 10.1371/journal.pntd.0003706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jambawai M. We are dying of Ebola; where is the world? Africa Review. 2014. http://www.africareview.com/Opinion/No-outside-help-as-Ebola-devastates-Sierra-Leone/-/979188/2464846/-/wvre5nz/-/index.html (accessed Aug 19, 2015).
- 33.Green A. Sheik Humarr Khan. Lancet. 2014;384:740. doi: 10.1016/s0140-6736(14)61428-8. [DOI] [PubMed] [Google Scholar]
- 34.Liu J. Disease outbreak: Finish the fight against Ebola. Nature. 2015;524:27–29. doi: 10.1038/524027a. [DOI] [PubMed] [Google Scholar]
- 35.Mirkovic K, Thwing J, Diack PA, the Centers for Disease Control and Prevention (CDC) Importation and containment of Ebola virus disease—Senegal, August–September 2014. MMWR Morb Mortal Wkly Rep. 2014;63:873–874. [PMC free article] [PubMed] [Google Scholar]
- 36.Shuaib F, Gunnala R, Musa EO, the Centers for Disease Control and Prevention (CDC) Ebola virus disease outbreak—Nigeria, July–September 2014. MMWR Morb Mortal Wkly Rep. 2014;63:867–872. [PMC free article] [PubMed] [Google Scholar]
- 37.Grabowski A, Hohlfelder E. When losing track means losing lives: accountability lessons from the Ebola crisis. 2015. http://one-org.s3.amazonaws.com/us/wp-content/uploads/2015/07/White_Paper_Ebola.pdf (accessed July 25, 2015).
- 38.WHO Ebola R&D effort—vaccines, therapeutics, diagnostics. Jan 30, 2015. http://www.who.int/medicines/ebola-treatment/ebola_r_d_effort/en/ (accessed May 29, 2015).
- 39.WHO Ebola situation report–17 June 2015. 2015. http://apps.who.int/ebola/current-situation/ebola-situation-report-17-june-2015 (accessed Aug 20, 2015).
- 40.Garrett L. How Cuba could stop the next Ebola outbreak. 2015. http://foreignpolicy.com/2015/05/06/cuba-ebola-west-africa-doctors/ (accessed Aug 20, 2015).
- 41.WHO Implementation of the International Health Regulations (2005). Responding to health emergencies. 2015. http://apps.who.int/gb/ebwha/pdf_files/EB136/B136_22-en.pdf (accessed Aug 19, 2015).
- 42.Gostin LO. Ebola: towards an International Health Systems Fund. Lancet. 2014;384:e49–e51. doi: 10.1016/S0140-6736(14)61345-3. [DOI] [PubMed] [Google Scholar]
- 43.Sridhar D, Clinton C. 2014. Overseeing global health. 2014. https://www.imf.org/external/pubs/ft/fandd/2014/12/pdf/sridhar.pdf (accessed Oct 5, 2015).
- 44.WHO . Implementation of the International Health Regulations (2005)—report of the Review Committee on second extensions for establishing national public health capacities on IHR implementation. World Health Organization; Geneva: 2015. [Google Scholar]
- 45.WHO . Statement on the 2nd meeting of the IHR Emergency Committee regarding the 2014 Ebola outbreak in west Africa. World Health Organization; Geneva: 2014. [Google Scholar]
- 46.WHO . Statement on the 3rd meeting of the IHR Emergency Committee regarding the 2014 Ebola outbreak in west Africa. World Health Organization; Geneva: 2014. [Google Scholar]
- 47.WHO . Statement on the 4th meeting of the IHR Emergency Committee regarding the 2014 Ebola outbreak in west Africa. World Health Organization; Geneva: 2015. [Google Scholar]
- 48.WHO . Statement on the 5th meeting of the IHR Emergency Committee regarding the Ebola outbreak in west Africa. World Health Organization; Geneva: 2015. [Google Scholar]
- 49.The White House Office of the Press Secretary Fact sheet: the global health security agenda. 2015. https://www.whitehouse.gov/the-press-office/2015/07/28/fact-sheet-global-health-security-agenda (accessed Sept 14, 2015).
- 50.Pope AE. Uniting in Seoul to extinguish epidemic threats through the global health security agenda. 2015. https://www.whitehouse.gov/blog/2015/09/16/uniting-seoul-extinguish-epidemic-threats-through-global-health-security-agenda (accessed Oct 3, 2015).
- 51.G7 Leaders declaration. 2015. https://www.g7germany.de/Content/EN/_Anlagen/G7/2015-06-08-g7-abschluss-eng_en.pdf (accessed June 20, 2015).
- 52.European Commission Press release database. 2015. http://europa.eu/rapid/press-release_AGENDA-15-4220_en.htm#4 (accessed Aug 19, 2015).
- 53.UN Global Ebola Response . International Ebola recovery conference, July 9–10, 2015. United Nations; New York: 2015. [Google Scholar]
- 54.The World Bank . Ebola: World Bank Group provides new financing to help Guinea, Liberia and Sierra Leone recover from Ebola emergency. The World Bank; Washington, DC: 2015. [Google Scholar]
- 55.Bill & Melinda Gates Foundation The Bill & Melinda Gates Foundation to fund disease surveillance network in Africa and Asia to prevent childhood mortality and help prepare for the next epidemic. 2015. http://www.gatesfoundation.org/Media-Center/Press-Releases/2015/05/Child-Health-and-Mortality-Prevention-Surveillance-Network (accessed July 20, 2015).
- 56.Bréchot C. Train Africa's scientists in crisis response. Nature. 2015;524:7. doi: 10.1038/524007a. [DOI] [PubMed] [Google Scholar]
- 57.Najjar-Pellet J, Machuron JL, Bougoudogo F. Clinical laboratory networks contribute to strengthening disease surveillance: the RESAOLAB Project in west Africa. Emerg Health Threats J. 2013 doi: 10.3402/ehtj.v6i0.19960. published online Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wellcome Trust Fleming Fund launched to tackle global problem of drug-resistant infection. 2015. http://www.wellcome.ac.uk/News/Media-office/Press-releases/2015/WTP058933.htm (accessed Aug 20, 2015).
- 59.Mano River Union Post-Ebola Socio-Economic Recovery Programme. April 2015. http://reliefweb.int/sites/reliefweb.int/files/resources/mru_sub-regional_socioeconomic_strategy_030715.pdf (accessed July 20, 2015).
- 60.Save the Children 2015. A wake up call: lessons from Ebola for the world's health systems. 2015. http://blogs.savethechildren.org.uk/2015/03/a-wake-up-call-lessons-from-ebola-for-the-worlds-health-systems/ (accessed May 29, 2015).
- 61.Garrett L. The Ebola review: parts I and II. 2015. http://foreignpolicy.com/2015/06/06/ebola-review-world-health-organization-g-7-merkel/ (accessed Aug 31, 2015).
- 62.Crampton T. WHO criticizes China over handling of mystery disease. The New York Times; Hong Kong: 2003. [Google Scholar]
- 63.African Risk Capacity African Risk Capacity insurance mechanism. http://www.africanriskcapacity.org/ (accessed Oct 5, 2015).
- 64.WHO . Report of the Ebola interim assessment panel—July 2015. World Health Organization; Geneva: 2015. [Google Scholar]
- 65.Oleribe OO, Salako BL, Ka MM. Ebola virus disease epidemic in West Africa: lessons learned and issues arising from West African countries. Clin Med. 2015;15:54–57. doi: 10.7861/clinmedicine.15-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kamradt-Scott A, Harman S, Wenham C, Smith F. Saving lives: the civil-military response to the 2014 Ebola outbreak in west Africa. University of Sydney; Sydney, Australia: 2015. [Google Scholar]
- 68.Inter-Agency Standing Committee Working Group Humanitarian system-wide emergency activation: definitions and procedures. PR/1204/4078/7. April 2012. http://reliefweb.int/sites/reliefweb.int/files/resources/IASC%20System-Wide%20Activation.pdf (accessed July 25, 2015).
- 69.Commission on Information and Accountability for Women's and Children's Health Keeping promises, measuring results. 2011. http://www.who.int/topics/millennium_development_goals/accountability_commission/Commission_Report_advance_copy.pdf (accessed July 25, 2015).
- 70.Bristol N, Millard C. “The power of straight talk: the Independent Monitoring Board of the Global Polio Eradication Initiative,” Center for Strategic and International Studies. 2015. http://csis.org/publication/power-straight-talk (accessed Oct 2, 2015).
- 71.Yozwiak NL, Schaffner SF, Sabeti PC. Data sharing: make outbreak research open access. Nature. 2015;518:477–479. doi: 10.1038/518477a. [DOI] [PubMed] [Google Scholar]
- 72.Steenhuysen J. Exclusive: U.S. Ebola researchers plead for access to virus samples. 2014. http://www.reuters.com/article/2014/11/05/us-health-ebola-usa-research-exclusive-idUSKBN0IP1DZ20141105 (accessed May 29, 2015).
- 73.Check Hayden E. Proposed Ebola biobank would strengthen African science. Nature. 2015;524:146–147. doi: 10.1038/524146a. [DOI] [PubMed] [Google Scholar]
- 74.Heymann DL, Rodier G. SARS: a global response to an international threat. Brown J World Aff. 2003;10:85–197. [Google Scholar]
- 76.WHO Pandemic Influenza Preparedness Framework Advisory Group Technical Expert Working Group on genetic sequence data. 2014. http://www.who.int/influenza/pip/advisory_group/PIP_AG_Rev_Final_TEWG_Report_10_Oct_2014.pdf?ua=1 (accessed July 29, 2015).
- 77.Fidler DP, Gostin LO. The WHO pandemic influenza preparedness framework: a milestone in global governance for health. JAMA. 2011;306:200–201. doi: 10.1001/jama.2011.960. [DOI] [PubMed] [Google Scholar]
- 78.Henao-Restrepo AM, Longini IM, Egger M. Efficacy and effectiveness of an rVSV-vectored vaccine expressing Ebola surface glycoprotein: interim results from the Guinea ring vaccination cluster-randomised trial. Lancet. 2015;386:857–866. doi: 10.1016/S0140-6736(15)61117-5. [DOI] [PubMed] [Google Scholar]
- 79.Pollack A. Opting against Ebola drug for ill African doctor. The New York Times; New York: 2014. [Google Scholar]
- 80.Borio L, Cox E, Lurie N. Combating emerging threats—accelerating the availability of medical therapies. N Engl J Med. 2015;373:993–995. doi: 10.1056/NEJMp1508708. [DOI] [PubMed] [Google Scholar]
- 81.WHO Consultative Expert Working Group on research and development Research and development to meet health needs in developing countries: Strengthening global financing and coordination. 2012. http://www.who.int/phi/CEWG_Report_5_April_2012.pdf (accessed May 29, 2015).
- 82.Plotkin SA, Mahmoud AA, Farrar J. Establishing a global vaccine-development Fund. N Engl J Med. 2015;373:297–300. doi: 10.1056/NEJMp1506820. [DOI] [PubMed] [Google Scholar]
- 83.Moon S. Demonstration financing: considerations for the new international fund for R&D. 2014. http://www.dndi.org/images/stories/advocacy/pilot-pooled-international-fund_web.pdf (accessed July 25, 2015).
- 84.O'Neill J. Securing new drugs for future generations: the pipeline of antibiotics. 2015. http://amr-review.org/sites/default/files/SECURING%20NEW%20DRUGS%20FOR%20FUTURE%20GENERATIONS%20FINAL%20WEB_0.pdf (accessed May 29, 2015).
- 85.Balasegaram M, Bréchot C, Farrar J. A global biomedical R&D fund and mechanism for innovations of public health importance. PLoS Med. 2015;12:e1001831. doi: 10.1371/journal.pmed.1001831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Clift C. What's the World Health Organization for?: final report from the centre on Global Health Security Working Group on Health Governance. 2014. http://www.chathamhouse.org/sites/files/chathamhouse/field/field_document/20140521WHOHealthGovernanceClift.pdf (accessed May 29, 2015).
- 87.Lee K. The World Health Organization. Routledge; Abingdon: 2008. [Google Scholar]
- 88.Fink S. Cuts at W.H.O. hurt response to Ebola crisis. The New York Times; New York: 2014. [Google Scholar]
- 89.WHO Proposed Programme Budget 2016–2017. 2015. http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_7-en.pdf (accessed June 20, 2015).
Uncited References
- 67.Financial Tracking Service Ebola Virus Outbreak - Overview of Needs and Requirements (inter-agency plan for Guinea, Liberia, Sierra Leone, Region) 2015. https://fts.unocha.org/pageloader.aspx?page=emerg-emergencyDetails&emergID=16506 (accessed June 10, 2015).
- 75.Bogner P, Capua I, Cox NJ, Lipman DJ. A global initiative on sharing avian flu data. Nature. 2006;442:981. [Google Scholar]