Abstract
Since the implementation of the Hospital Readmissions Reduction Program (HRRP), readmissions have declined for Medicare patients with conditions targeted by the policy (acute myocardial infarction, heart failure, and pneumonia). To understand whether HRRP implementation was associated with a readmission decline for patients across all insurance types (Medicare, Medicaid, and private), we conducted a difference-in-differences analysis using information from the Nationwide Readmissions Database. We compared how quarterly readmissions for target conditions changed before (2010–12) and after (2012–14) HRRP implementation, using nontarget conditions as the control. Our results demonstrate that readmissions declined at a significantly faster rate after HRRP implementation not just for Medicare patients but also for those with Medicaid, both in the aggregate and for individual target conditions. However, composite Medicaid readmission rates remained higher than those for Medicare. Throughout the study period privately insured patients had the lowest aggregate readmission rates, which declined at a similar rate compared to nontarget conditions. The HRRP was associated with nationwide readmission reductions beyond the Medicare patients originally targeted by the policy. Further research is needed to understand the specific mechanisms by which hospitals have achieved reductions in readmissions.
Preventable hospital readmissions within thirty days of discharge have drawn the attention of policy makers because they are associated with poor outcomes and high financial costs.1–4 To address this problem, the Hospital Readmissions Reduction Program (HRRP) was implemented as part of the Affordable Care Act (ACA), starting in October 2012. The HRRP targets hospitals with greater-than-expected all-cause, risk-standardized readmission rates for Medicare beneficiaries with specific target conditions.5 To date, over three-quarters of participating hospitals have been penalized by the HRRP, with total Medicare penalties reaching $2 billion.6–8
Observational studies suggest an association between the HRRP and a reduction in Medicare readmissions for the three conditions originally targeted by the policy: acute myocardial infarction (AMI), heart failure, and pneumonia.9–11 However, less is known about readmission trends for these conditions among non-Medicare populations, such as patients with Medicaid or private insurance, who accounted for 18 percent and 20 percent of all readmissions in 2013, respectively.12 Recent data show that target conditions are increasingly common in these younger populations13 and that associated readmission costs are substantial, totaling over $1.5 billion for private insurance and Medicaid readmissions in 2013.12,14 The few studies that examined patients with these two insurance types reported a decline in readmission rates among non-Medicare patients during the time of HRRP implementation, but they did not adjust for the confounding effect of other secular trends.15 Other studies have been limited to single years,16 selected US states,13,17,18 or single conditions.19–21
Given the readmission burden among patients with Medicaid and private insurance, understanding their readmission trends in the context of the HRRP is important for a few reasons. First, a decline in readmissions among these groups in response to the HRRP might suggest that hospitals implemented systemwide initiatives to improve quality or transitions of care10 or, alternatively, that hospitals increasingly treated patients in emergency departments and observation units to avoid inpatient readmissions. Second, if readmissions remained high or un-changed among non-Medicare patients, policy makers might consider developing readmission reduction policies that incentivize improvements in quality and transitions of care for these populations.
To address this gap in knowledge, we used data from the Nationwide Readmissions Database, maintained by the Agency for Healthcare Research and Quality, to determine whether the HRRP was associated with a decline in readmissions among patients with Medicaid and private insurance who have target conditions.
Study Data And Methods
DATA SOURCE
The Nationwide Readmissions Database contains discharge data from twenty-two geographically dispersed states that accounted for 51.2 percent of the US population and 49.3 percent of hospitalizations in 2014, and it is designed to generate national estimates of readmissions when sampling weights are used.22 The database includes data from all payers and the uninsured, which makes it a unique source of information to use in studying the impact of the Hospital Readmissions Reduction Program on nationwide readmissions across all insurance types. It contains data on over 100 variables for each hospital stay, including International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), diagnosis codes; patient demographics; and hospital costs.22
This study was exempted from review by the Institutional Review Board at Beth Israel Deaconess Medical Center.
STUDY POPULATION
Information was obtained about all hospitalizations of adults (people older than age eighteen) between January 1, 2010, and December 31, 2014. Each year of data from the Nationwide Readmissions Database is independently created, using verified patient linkage identification numbers, and patients cannot be tracked across years. Therefore, data from December of each year were excluded, which allowed every patient to have thirty days of follow-up. Hospitalizations with in-hospital death, missing insurance type, and discharges against medical advice were excluded. Patients who were coded as having AMI but discharged on the same day as they were admitted were not included as an index admission, as these patients are unlikely to have had true AMI. Patients ages sixty-five and older whose primary insurance was Medicaid (“dual eligibles”) were included in the Medicare cohort.14,23 Hospitalizations with patient transfers were merged and attributed to the terminal hospitalization in the chain.23 Patients were allowed to contribute more than one readmission to our data as long as the index hospitalization occurred less than thirty days after any previous hospitalization. A second hospitalization that occurred within thirty days of another for the same patient was counted only as a readmission. Only the first readmission was included in the analysis.
PATIENT AND HOSPITAL CHARACTERISTICS
Patients’ demographic characteristics used for risk adjustment included age, sex, and twenty-nine comorbidities collected by the Nationwide Readmissions Database based on the Elixhauser Comorbidity Index.24 Primary discharge ICD-9-CM diagnosis codes—listed in online appendix exhibit 625—were used to identify patients with the conditions originally targeted by the policy (AMI, heart failure, and pneumonia). Admissions with alternative primary discharge diagnosis codes were defined as nontarget. Among these, ICD-9-CM codes for elective total hip or total knee amputations, chronic obstructive pulmonary disease, and coronary artery bypass graft were excluded since these conditions were publicly known to be potential targets for future HRRP penalties. Insurance status collected by the database was designated as the primary insurance payer for each admission. Hospitalization characteristics included length-of-stay and costs of index admission and readmission. Institutional characteristics included hospital size and teaching and ownership status.
OUTCOME
The primary outcome was unplanned all-cause thirty-day readmission, which we calculated using the criteria from the 2014 Centers for Medicare and Medicaid Services (CMS) methodology for hospitalwide readmission measures.23 We defined this outcome as the occurrence of an unplanned hospitalization for any cause occurring one to thirty days after discharge from an index hospitalization (that is, the hospitalization to which the readmission outcome is attributed). Using these criteria, we calculated national risk-adjusted readmission rates for each condition by aggregating all admissions from all hospitals across a given year.
STATISTICAL ANALYSIS
The study objective was to understand whether readmission rates for non-Medicare patients with target conditions declined more than those for patients with nontarget conditions after HRRP implementation. This objective was accomplished through the use of a two-step model. In the first step we estimated quarterly risk-standardized readmission rates for both target and nontarget conditions, within each insurance type. In the second step we used a piecewise linear model to analyze these rates and generate the slopes of the readmission decline before and after HRRP implementation. Finally, we compared the change in slope of the rates for target conditions with that for nontarget conditions (the difference-in-differences), within each insurance type.
ESTIMATION OF RISK-STANDARDIZED READMISSION RATES:
We first estimated quarterly risk-standardized readmission rates. For each condition, insurance type, and quarter of the calendar year, we fitted a logistic regression model using generalized estimating equations, with readmission status as a binary outcome. Covariates included patients’ demographic characteristics, comorbidities, insurance type, and target condition. We accounted for clustering at the hospital level using an exchangeable correlation structure, since hospitalizations within the same hospital tend to have similar outcomes.26 Goodness of fit was examined using the chi-square test of the deviance. We specifically controlled for the change in patients’ comorbidities over time, to isolate the effect that hospital-level characteristics exerted on nationwide readmissions. To do so, we randomly selected the patient population hospitalized in the last quarter of 2014 as the reference group in our model. We then used the covariate distributions from this group, together with the estimated model parameters from each quarter, to calculate the predicted readmission rates for each quarter in our study period standardized for case-mix.
DIFFERENCE-IN-DIFFERENCES ANALYSIS:
For each target condition and insurance type, we then calculated whether there was a change in the decline of the risk-adjusted quarterly readmission rates after HRRP implementation, compared to the period before implementation. To accomplish this, we first analyzed trends in the estimated risk-standardized readmission rates through a piecewise linear model that included quarters (a continuous variable), insurance type, target condition, and the interaction terms among the three variables. This model allowed us to estimate two slopes for the trend of risk-adjusted readmission rates, one before HRRP implementation and one after it. The last quarter of 2012 was used as the intervention point between the two periods, to assess the impact of the HRRP on readmissions after the actual implementation of the policy—which is when CMS began penalizing hospitals with higher-than-expected readmission rates.9,10,27 The difference between the two slopes characterized the change in trend for a given condition. This difference was calculated for the three target conditions (individually and combined) as well as for the control (nontarget conditions) in each insurance type.
Finally, we computed the difference between the change in slopes (that is, the post-HRRP slope minus the pre-HRRP slope) for each target condition and the change in slope for nontarget conditions. This difference-in-differences was computed for each insurance type to determine whether the HRRP was associated with a reduction in readmissions for patients with target conditions who had Medicaid or private insurance. Multiple comparison adjustment was performed by controlling the false discovery rate at 0.05.28 All analyses were performed using SAS, version 9.4.
LIMITATIONS
Our analysis must be considered in the context of the study design. First, its observational nature limited our ability to make causal inferences regarding our findings.
Second, since the Nationwide Readmissions Database does not track patients across years, its risk-adjustment criteria differ from those of CMS, which uses claims data extending twelve months before an index admission.23 We instead used twenty-nine comorbidities coded specifically for this database, consistent with prior studies.14,29,30 Nonetheless, the database remains a unique source of information that allows the evaluation of the HRRP’s impact on nationwide readmission rates across all insurance types.
Third, our results also relied on the validity of the control (nontarget conditions), which has been employed in prior literature.9
Fourth, while 2010 has been employed as the intervention point in prior studies using Medicare claims data,9 readmissions data for the period before 2010 are not available in the database and were not used in the analysis.
Fifth, we chose October 2012 as the intervention point with the goal of assessing the impact of the HRRP after the implementation of financial penalties. The implementation period is a critical time, when hospitals’ behavior could have been influenced by the first consequences of the penalties they started to receive.
Study Results
CHARACTERISTICS OF THE STUDY SAMPLE
During the study period there were index admissions for 3,737,589 people with target conditions (AMI, heart failure, and pneumonia) and for 31,096,617 people with nontarget conditions (appendix exhibit 9).25 Compared to patients with nontarget conditions, those with target conditions were more likely to be older and male across all insurance types except Medicare, whose patients had a similar mean age (exhibit 1). Patients with target conditions often had a larger burden of clinical comorbidities, especially those with non-Medicare insurance (exhibit 1 and appendix exhibit 3),25 and they tended to have longer hospital stays across all insurance types (exhibit 1). Medicare and Medicaid patients with target and nontarget conditions had similar median household incomes by ZIP code and population size of their county of residence, while privately insured patients with target conditions resided in lower-income ZIP codes and areas with larger populations (appendix exhibit 2).25 Lastly, admissions for patients with target and nontarget conditions were similarly distributed across hospitals of different sizes and ownership and teaching statuses (appendix exhibit 4).25
Exhibit 1.
Baseline characteristics of patients at index admission, by insurance and condition type, 2010–14
| Medicare (n = 15,135,169) |
Medicaid (n = 5,960,797) |
Private (n = 9,881,632) |
Other (n = 3,856,608) |
|||||
|---|---|---|---|---|---|---|---|---|
| Target Conditions (n = 2,500,282) | Control conditions (n = 12,634,887) | Target Conditions (n = 297,543) | Control conditions (n = 5,663,254) | Target Conditions (n = 654,399) | Control conditions (n = 9,227,233) | Target conditions (n = 285,365) | Control conditions (n = 3,571,243) | |
| Patient-level demographic characteristics | ||||||||
| Mean age (years) | 79.1 | 78.1 | 49.7 | 37.1 | 57.7 | 55.0 | 54.0 | 43.7 |
| Female (%) | 52.9 | 59.0 | 47.4 | 69.7 | 38.8 | 63.8 | 34.3 | 45.2 |
| Clinical comorbidity with high prevalence in study population (%)a | ||||||||
| Anemias | 29.84 | 24.09 | 23.03 | 14.79 | 17.33 | 11.81 | 16.64 | 11.96 |
| Congestive heart failure | 11.41 | 15.46 | 5.90 | 2.94 | 4.65 | 2.65 | 4.05 | 2.72 |
| Chronic pulmonary disease | 38.63 | 21.84 | 38.77 | 13.56 | 26.38 | 9.95 | 28.31 | 10.81 |
| Depression | 9.99 | 11.31 | 11.24 | 8.74 | 8.84 | 8.57 | 7.27 | 8.73 |
| Diabetes | 38.45 | 31.38 | 38.01 | 13.62 | 32.48 | 13.94 | 30.64 | 14.32 |
| Fluid and electrolyte disorders | 31.71 | 32.88 | 28.67 | 16.09 | 24.57 | 16.65 | 25.41 | 21.46 |
| Hypertension | 72.74 | 70.38 | 59.12 | 25.04 | 59.91 | 31.37 | 58.44 | 32.63 |
| Hypothyroidism | 18.21 | 17.86 | 7.10 | 4.20 | 9.48 | 7.36 | 6.08 | 4.45 |
| Peripheral vascular disease | 12.77 | 9.66 | 5.17 | 1.47 | 6.00 | 2.12 | 4.72 | 1.70 |
| Hospitalization characteristics | ||||||||
| Mean length-of-stay (days) | 5.5 | 5.4 | 5.5 | 4.7 | 4.6 | 3.8 | 4.6 | 4.3 |
| Mean cost of index hospitalization ($) | 12,378.7 | 10,944.4 | 14,167.2 | 8,498.7 | 15,228.8 | 8,783.1 | 13,675.8 | 8,861.7 |
| Mean cost of readmission ($) | 13,607.1 | 12,832.4 | 15,282.3 | 11,253.9 | 17,126.5 | 12,350.6 | 14,919.7 | 10,682.7 |
SOURCE Authors’ analysis of data for 2010–14 from the Nationwide Readmissions Database. NOTES The target conditions were acute myocardial infarction, heart failure, and pneumonia. All patients were discharged alive from the hospital. “Other” includes self-pay and uninsured patients.
Prevalence greater than 10 percent among patients in at least one insurance type.
READMISSION STRATIFICATION BY INSURANCE TYPE
In the period 2010–14, for target conditions, 66.9 percent of all index admissions were for patients with Medicare, 8.0 percent were for those with Medicaid, and 17.5 percent were for those with private insurance, and the percentages for readmissions were similar: 73.5 percent, Medicare; 9.1 percent, Medicaid; and 12.2 percent, private insurance (appendix exhibit 7).25 Average unadjusted readmission rates across all insurance types were 15.4 percent for AMI, 22.5 percent for heart failure, and 16.1 percent for pneumonia (appendix exhibit 4).25 For Medicare, readmission rates were 18.9 percent for AMI, 23.1 percent for heart failure, and 17.5 percent for pneumonia. For Medicaid, readmission rates were 16.8 percent for AMI, 26.7 percent for heart failure, and 17.8 percent for pneumonia. For private insurance, readmission rates were 9.8 percent for AMI, 18.7 percent for heart failure, and 11.9 percent for pneumonia (appendix exhibit 4).25 Over time, unadjusted readmission rates declined across target conditions and insurance types.
ADJUSTED READMISSIONS AND DIFFERENCES IN READMISSION TRENDS
Aggregate risk-adjusted readmission rates declined from 21.3 percent in the first quarter of 2010 to 19.4 percent in the third quarter of 2014 for Medicare, from 20.9 percent to 20.4 percent for Medicaid, and from 13.5 percent to 12.5 percent for private insurance patients (exhibit 2). For all subsequent results, we report the absolute percentage decline in readmission rates per quarter of the study period.
Exhibit 2.
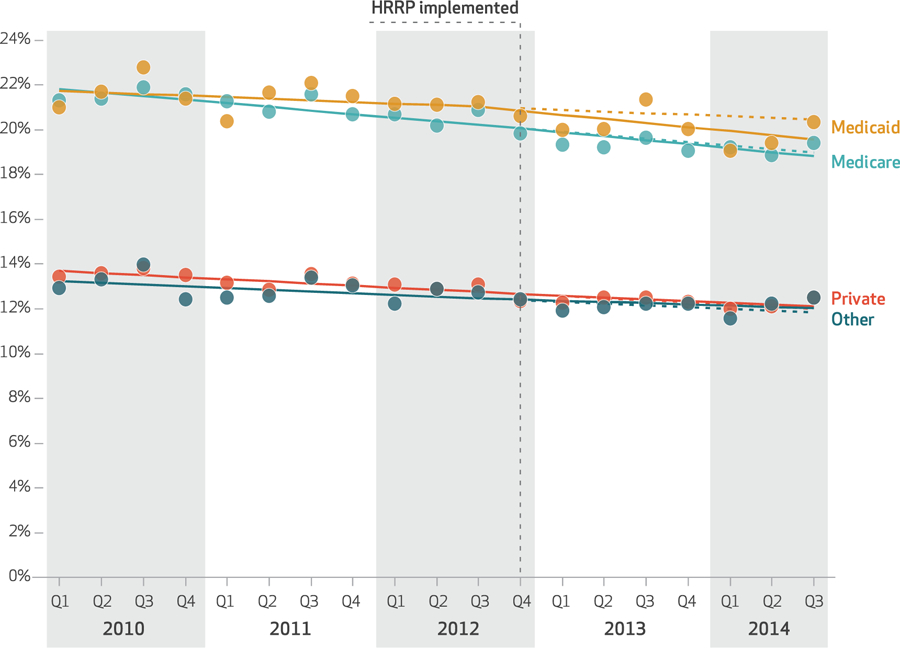
Risk-adjusted readmission rates for three conditions targeted by the Hospital Readmissions Reduction Program (HRRP) from the first quarter of 2010 through the third quarter of 2014, by insurance type
SOURCE Authors’ analysis of data for 2010–14 from the Nationwide Readmissions Database. NOTES The target conditions were acute myocardial infarction, heart failure, and pneumonia. The data shown represent the quarterly risk-adjusted readmission rates, account-ing for the effect of age, sex, and clinical comorbidities and using the fourth quarter of 2014 as the reference group. The dashed lines reflect projected risk-adjusted trends after the HRRP, assuming that pre-HRRP trends had continued. The solid lines represent the observed readmission trends. Solid lines were generated from the data through a piecewise linear model that included quarters, insurance type (“other” includes self-pay and uninsured patients), target condition, and the interaction terms among the three variables.
For Medicaid patients with target conditions, composite readmission rates declined at a faster rate in the post-HRRP period (slope: −0.183; 95% confidence interval: −0.194, −0.173) than in the pre-HRRP period (slope: −0.071; 95% CI: −0.079, −0.064), which yielded a negative change in slope (change: −0.112; 95% CI: −0.128, −0.096) (exhibit 4). Readmission rates for Medicaid patients with nontarget conditions also declined at a faster rate in the post-HRRP period compared to the pre-HRRP period (exhibit 3), although the change in slope was less negative compared to that for the target conditions (change: −0.068; 95% CI: −0.072, −0.064). For composite Medicaid readmissions, therefore, the change in slope between the pre-and post-HRRP periods was significantly greater for target compared to nontarget conditions (difference: −0.044; 95% CI: −0.061, −0.027). Similar results were observed for individual target conditions: Readmission rates for Medicaid patients with AMI (difference: −0.098; 95% CI: −0.132, −0.064), heart failure (difference: −0.030; 95% CI: −0.055, −0.005), or pneumonia (difference: −0.079; 95% CI: −0.107, −0.051) declined significantly after HRRP implementation compared to rates for nontarget conditions (exhibit 4 and appendix exhibit 1).25
Exhibit 4.
Change in readmission rates after implementation of the Hospital Readmissions Reduction Program (HRRP) for target conditions, compared to control conditions
| Change (% per quarter) |
|||
|---|---|---|---|
| Target condition(s) | Control conditions | Difference | |
| ALL THREE TARGET CONDITIONS COMBINED | |||
| Medicare | −0.018 | 0.032 | −0.049**** |
| Medicaid | −0.112 | −0.068 | −0.044**** |
| Private | 0.013 | −0.017 | 0.030**** |
| Other | 0.022 | −0.014 | 0.036**** |
| ACUTE MYOCARDIAL INFARCTION | |||
| Medicare | 0.007 | 0.032 | −0.025**** |
| Medicaid | −0.166 | −0.068 | −0.098**** |
| Private | 0.010 | −0.017 | 0.027**** |
| Other | 0.027 | −0.014 | 0.041**** |
| HEART FAILURE | |||
| Medicare | −0.046 | 0.032 | −0.077**** |
| Medicaid | −0.098 | −0.068 | −0.030** |
| Private | −0.057 | −0.017 | −0.040**** |
| Other | 0.150 | −0.014 | 0.164**** |
| PNEUMONIA | |||
| Medicare | −0.032 | 0.032 | −0.064**** |
| Medicaid | −0.147 | −0.068 | −0.079**** |
| Private | 0.076 | −0.017 | 0.093**** |
| Other | −0.041 | −0.014 | −0.027** |
SOURCE Authors’ analysis of data for 2010–14 from the Nationwide Readmissions Database NOTES “Control conditions” are those other than the three target conditions, as explained in the text. “Other” includes self-pay and uninsured patients.
p < 0:05
p < 0:001
Exhibit 3.
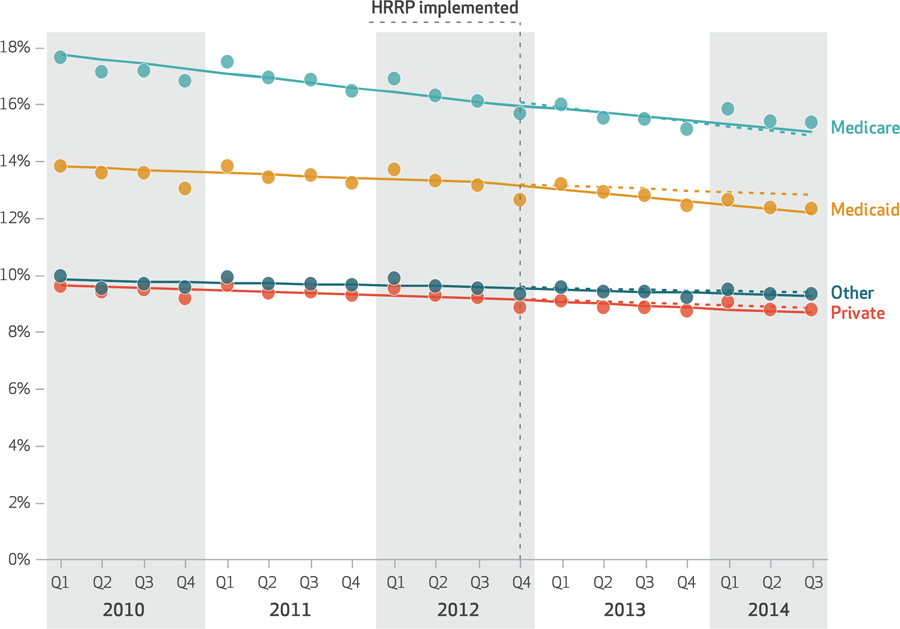
Risk-adjusted readmission rates for conditions not targeted by the Hospital Readmissions Reduction Program (HRRP) from the first quarter of 2010 through the third quarter of 2014, by insurance type
SOURCE Authors’ analysis of data for 2010–14 from the Nationwide Readmissions Database. NOTES “Conditions not targeted” (“control conditions” in exhibits 1 and 4) are all but the three target conditions (acute myocardial infarction, heart failure, and pneumonia), as explained in the text. The data shown represent the quarterly risk-adjusted readmission rates as explained in the notes to exhibit 2. Solid lines were generated as explained in the notes to exhibit 2. “Other” includes self-pay and uninsured patients.
Readmission rates for privately insured patients with target conditions increased significantly in the post-HRRP period compared to the control, both in the aggregate (difference: 0.030; 95% CI: 0.021, 0.039) and individually for AMI (difference: 0.027; 95% CI: 0.013, 0.041) and pneumonia (difference: 0.093; 95% CI: 0.077, 0.109) (exhibit 4 and appendix exhibit 1).25 Readmission rates were found to decline significantly only for privately insured patients with heart failure (difference: −0.040; 95% CI: −0.057, −0.023), which had the highest baseline readmission rate among privately insured patients (appendix exhibit 1).25
Discussion
In this study we evaluated the association between implementation of the Hospital Readmissions Reduction Program and readmission rates across all insurance types. We found that hospital readmissions for three target conditions (acute myocardial infarction, heart failure, and pneumonia) declined significantly not only for Medicare patients but also for Medicaid patients, which is consistent with a spillover effect of the policy beyond the Medicare population. Despite evidence that the HRRP was associated with a reduction in readmissions among Medicaid patients, however, composite readmission rates remained high in this cohort. Privately insured patients had the lowest aggregate readmission rates throughout the study period, with no significant decline at the composite level after HRRP implementation.
We observed a more modest decline in readmissions for target conditions among Medicare beneficiaries during the HRRP announcement period (2010–12) compared to what has been reported in prior studies.9,10,31 This may be because our study was conducted using the Nationwide Readmissions Database, so our analysis was not affected by the change in electronic transaction standards that hospitals use to submit Medicare claims. This change, which occurred in 2011, has allowed hospitals to enter more diagnosis codes per patient (from nine to twenty-five). Recent data suggest that the decline in readmissions observed in some prior studies9,10,31 is likely overstated because of the artificial increase in patient risk scores that resulted from this update. The more modest decline in risk-adjusted Medicare readmissions observed in our study, on the other hand, is consistent with other analyses that accounted for this change in electronic standards.11,32 Though more modest, Medicare readmissions for target conditions did decline at a significantly faster rate compared to nontarget conditions in our study. Importantly, we also found that the HRRP was associated with a reduction in readmissions among Medicaid patients with target conditions, compared with nontarget conditions, both at the composite level and for individual conditions. Collectively, findings from our study suggest that the HRRP provided a strong incentive for hospitals to implement hospitalwide initiatives to reduce readmissions. The extent to which these initiatives reflect true improvements in the quality of care, however, is not clear.
Notably, despite the association of the HRRP with declines in readmissions among Medicaid patients with target conditions, composite Medicaid readmissions in the post-HRRP period remained much higher than Medicare readmissions. Given that approximately one in five US residents are insured with Medicaid, reducing readmissions in a safe manner in this population represents an important way to reduce health care expenditures. In 2013, for example, Medicaid readmissions resulted in $831 million in excess national health expenditures.12,14 Future research should evaluate the extent to which readmissions among the Medicaid population are preventable and identify quality improvement efforts that could reduce preventable readmissions for this high-risk group. Policy makers might consider the merits of designing interventions with incentives for hospitals that specifically target Medicaid readmissions, especially given recent studies that demonstrated reduced Medicare spending as a result of the HRRP.37 Potential efforts to monitor and reduce readmissions among Medicaid patients are aligned with the Data Driven Patient Care Strategy recently announced by CMS, which will soon release Medicaid data to researchers to improve health care for all beneficiaries.38
Among privately insured patients, composite readmission rates for target conditions increased slightly following HRRP implementation, compared to rates for nontarget conditions. Our findings differ from those in prior reports of declining private readmissions at the state level.17 The observed trend may be due to the fact that privately insured patients had the lowest readmission rates throughout the study period. Even after the significant decline in Medicare and Medicaid readmissions following implementation of the HRRP, composite readmission rates for these two cohorts remained much higher than those for privately insured patients. It is therefore possible that composite readmissions for privately insured patients experienced a “flooring effect” following implementation of the HRRP, with less room for additional improvement.9 This may also explain why heart failure, which had the highest baseline readmission rate among privately insured patients, was the only target condition that showed a significant decline in readmission rates in this cohort.
In the years following the announcement of the HRRP, many surveyed hospitals reported launching initiatives to curtail heart failure and AMI readmissions.33 This suggests that the HRRP may have provided an incentive for some hospitals to engage in initiatives that have been shown to reduce readmissions,31 ranging from predischarge interventions such as better medication reconciliation to postdischarge interventions such as ensuring closer follow-up with ambulatory care providers. More recent data, however, suggest that declines in readmissions may also reflect other shifts in patterns of care.34 One study found that the share of Medicare patients returning to a hospital within thirty days of discharge following a hospitalization for target conditions has not changed since the HRRP but that treatment of these patients in emergency departments and observation units has increased.34 This suggests that observed declines in readmissions may, in part, reflect a shift in triage patterns upon return to a hospital, instead of being due solely to improvements in quality of care. Though data on the relationship between the HRRP and postdischarge mortality are mixed, three recent studies demonstrate a significant increase in postdischarge mortality among Medicare beneficiaries hospitalized for heart failure after the HRRP.35–37 One of these studies showed an increase in postdischarge mortality for Medicare patients hospitalized for heart failure and pneumonia, which was concentrated among those who were not readmitted after discharge. These findings raise the possibility that increased use of emergency departments and observation units to reduce readmissions may be detrimental to patients who require higher-level care.37 Further research is needed to increase understanding of the association of the HRRP with mortality trends among Medicaid patients—an analysis we were unable to perform because the Nationwide Readmissions Database does not capture postdischarge deaths—and to clarify the mechanisms by which hospitals have achieved readmission reductions for Medicare and Medicaid patients.
Conclusion
We found that implementation of the Hospital Readmissions Reduction Program was associated with a significant decline in readmissions not just for Medicare patients, but also for Medicaid patients with the target conditions—which suggests that the HRRP may have had a spillover effect on patients who were not directly targeted by the policy. Despite this, composite Medicaid readmissions remained higher than those for Medicare. We were unable to identify strategies used by hospitals to achieve observed reductions in readmissions. Based on recent studies, such interventions could include improvements in quality of care, transitions of care, and efforts to avoid readmissions through greater use of emergency departments and observation units upon return to the hospital. Given recent concerns that the HRRP may have been associated with increased mortality for some target conditions among Medicare patients, further research is needed to clarify how hospitals have achieved systemwide readmission reductions and to understand trends in postdischarge mortality among Medicaid patients since the implementation of the HRRP.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge Joanne Healy and Linda Valsdottir for their technical support through the completion of this work.
Contributor Information
Enrico G. Ferro, Smith Center for Outcomes Research in Cardiology, Beth Israel Deaconess Medical Center, and a resident physician in internal medicine at Brigham and Women’s Hospital, in Boston, Massachusetts..
Eric A. Secemsky, Smith Center for Outcomes Research in Cardiology, Beth Israel Deaconess Medical Center..
Rishi K. Wadhera, Smith Center for Outcomes Research in Cardiology, Beth Israel Deaconess Medical Center, and in the Heart and Vascular Center, Department of Medicine, at Brigham and Women’s Hospital..
Eunhee Choi, Smith Center for Outcomes Research in Cardiology, Beth Israel Deaconess Medical Center..
Jordan B. Strom, Smith Center for Outcomes Research in Cardiology, Beth Israel Deaconess Medical Center..
Jason H. Wasfy, Department of Medicine at Massachusetts General Hospital, in Boston..
Yun Wang, Department of Biostatistics at the Harvard T. H. Chan School of Public Health, in Boston..
Changyu Shen, Smith Center for Outcomes Research in Cardiology, Beth Israel Deaconess Medical Center..
Robert W. Yeh, Smith Center for Outcomes Research in Cardiology, Beth Israel Deaconess Medical Center..
NOTES
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009; 360(14):1418–28. [DOI] [PubMed] [Google Scholar]
- 2.Bueno H, Ross JS, Wang Y, Chen J, Vidán MT, Normand SL, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA 2010;303(21):2141–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ 2011;183(7):E391–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medicare Payment Advisory Commission. Report to the Congress: promoting greater efficiency in Medicare [Internet]. Washington (DC): MedPAC; 2007. June [cited 2018 Dec 28]. Available from: http://www.medpac.gov/docs/default-source/reports/Jun07_EntireReport.pdf [Google Scholar]
- 5.CMS.gov Hospital Readmissions Reduction Program (HRRP) [Internet]. Baltimore (MD): Centers for Medicare and Medicaid Services; [last modified 2018. November 28; cited 2018 Dec 28]. Available from: https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html [Google Scholar]
- 6.Rau J Half of nation’s hospitals fail again to escape Medicare’s readmission penalties. Kaiser Health News [serial on the Internet]. 2015. August 3 [cited 2018 Dec 28]. Available from: https://khn.org/news/half-of-nations-hospitals-fail-again-to-escape-medicares-readmission-penalties/
- 7.Boccuti C, Casillas G. Aiming for fewer hospital U-turns: the Medicare Hospital Readmission Reduction Program [Internet]. San Francisco (CA): Henry J. Kaiser Family Foundation; 2017. March 10 [cited 2018 Dec 28]. Available from: https://www.kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program/ [Google Scholar]
- 8.American Hospital Association. Hospital Readmissions Reduction Program [Internet]. Chicago (IL): AHA; 2016. August [cited 2018 Dec 28]. (Fact Sheet). Available from: https://www.aha.org/system/files/2018-01/fs-readmissions.pdf [Google Scholar]
- 9.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med 2016;374(16):1543–51. [DOI] [PubMed] [Google Scholar]
- 10.Desai NR, Ross JS, Kwon JY, Herrin J, Dharmarajan K, Bernheim SM, et al. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA 2016;316(24):2647–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wasfy JH, Zigler CM, Choirat C, Wang Y, Dominici F, Yeh RW. Readmission rates after passage of the Hospital Readmissions Reduction Program: a pre-post analysis. Ann Intern Med 2017;166(5):324–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fingar K, Washington R. Trends in hospital readmissions for four high-volume conditions, 2009–2013 [Internet]. Rockville (MD): Agency for Healthcare Research and Quality; 2015. November [cited 2018 Dec 28]. (Healthcare Cost and Utilization Project Statistical Brief No. 196). Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb196-Readmissions-Trends-High-Volume-Conditions.jsp [PubMed] [Google Scholar]
- 13.Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, Krumholz HM. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: a retrospective observational cohort study. PLoS Med 2014;11(9):e1001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strom JB, Kramer DB, Wang Y, Shen C, Wasfy JH, Landon BE, et al. Short-term rehospitalization across the spectrum of age and insurance types in the United States. PLoS One 2017;12(7):e0180767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Angraal S, Khera R, Zhou S, Wang Y, Lin Z, Dharmarajan K, et al. Trends in 30-day readmission rates for Medicare and non-Medicare patients in the era of the Affordable Care Act. Am J Med 2018;131(11):1324–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sukul D, Sinha SS, Ryan AM, Sjoding MW, Hummel SL, Nallamothu BK. Patterns of readmissions for three common conditions among younger US adults. Am J Med 2017;130(10):1220.e1–e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carey K, Lin M-Y. Readmissions to New York hospitals fell for three target conditions from 2008 to 2012, consistent with Medicare goals. Health Aff (Millwood). 2015;34(6): 978–85. [DOI] [PubMed] [Google Scholar]
- 18.Chen M, Grabowski DC. Hospital Readmissions Reduction Program: intended and unintended effects. Med Care Res Rev 2017. December 1 [Epub ahead of print]. [DOI] [PubMed]
- 19.Allen LA, Smoyer Tomic KE, Smith DM, Wilson KL, Agodoa I. Rates and predictors of 30-day readmission among commercially insured and Medicaid-enrolled patients hospitalized with systolic heart failure. Circ Heart Fail. 2012;5(6):672–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arora S, Patel P, Lahewala S, Patel N, Patel NJ, Thakore K, et al. Etiologies, trends, and predictors of 30-day readmission in patients with heart failure. Am J Cardiol 2017;119(5): 760–9. [DOI] [PubMed] [Google Scholar]
- 21.Arora S, Lahewala S, Hassan Virk HU, Setareh-Shenas S, Patel P, Kumar V, et al. Etiologies, trends, and predictors of 30-day readmissions in patients with diastolic heart failure. Am J Cardiol 2017;120(4): 616–24. [DOI] [PubMed] [Google Scholar]
- 22.Healthcare Cost and Utilization Project. Overview of the Nationwide Readmissions Database (NRD) [Internet]. Rockville (MD): Agency for Healthcare Research and Quality; [last modified 2018. August 10; cited 2018 Dec 28]. Available from: https://www.hcup-us.ahrq.gov/nrdoverview.jsp [Google Scholar]
- 23.QualityNet. Measures updates and specifications report: hospital-level 30-day risk-standardized readmission measures [Internet]. Baltimore (MD): Centers for Medicare and Medicaid Services; 2014. [cited 2019 Jan 8]. Available for download from: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228774371008 [Google Scholar]
- 24.Healthcare Cost and Utilization Project. Elixhauser Comorbidity Software, version 3.7 [Internet]. Rockville (MD): Agency for Healthcare Research and Quality; 2017. [last modified 2017 Jun 22; cited 2018 Dec 28]. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp [Google Scholar]
- 25. To access the appendix, click on the Details tab of the article online.
- 26.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika 1986; 73(1):13–22. [Google Scholar]
- 27.Dharmarajan K, Wang Y, Lin Z, Normand ST, Ross JS, Horwitz LI, et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA 2017;318(3):270–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57(1):289–300. [Google Scholar]
- 29.Butala NM, Kramer DB, Shen C, Strom JB, Kennedy KF, Wang Y, et al. Applicability of publicly reported hospital readmission measures to unreported conditions and other patient populations: a cross-sectional all-payer study. Ann Intern Med 2018;168(9):631–9. [DOI] [PubMed] [Google Scholar]
- 30.Secemsky EA, Schermerhorn M, Carroll BJ, Kennedy KF, Shen C, Valsdottir LR, et al. Readmissions after revascularization procedures for peripheral arterial disease: a nationwide cohort study. Ann Intern Med 2018;168(2):93–9. [DOI] [PubMed] [Google Scholar]
- 31.Khera R, Dharmarajan K, Wang Y, Lin Z, Bernheim SM, Wang Y, et al. Association of the Hospital Readmissions Reduction Program with mortality during and after hospitalization for acute myocardial infarction, heart failure, and pneumonia. JAMA Network Open. 2018;1(5): e182777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ody C, Msall L, Dafny LS, Grabowski DC, Cutler DM. Decreases in readmissions credited to Medicare’s program to reduce hospital readmissions have been overstated. Health Aff (Millwood). 2019;38(1): 36–43. [DOI] [PubMed] [Google Scholar]
- 33.Bradley EH, Curry L, Horwitz LI, Sipsma H, Thompson JW, Elma M, et al. Contemporary evidence about hospital strategies for reducing 30-day readmissions: a national study. J Am Coll Cardiol 2012;60(7): 607–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Medicare Payment Advisory Commission. Report to the Congress: Medicare and the health care delivery system [Internet]. Washington (DC): MedPAC; 2018. Chapter 1, Mandated report: the effects of the Hospital Readmissions Reduction Program; [cited 2019 Jan 28]. Available from: http://www.medpac.gov/docs/default-source/reports/jun18_ch1_medpacreport_sec.pdf [Google Scholar]
- 35.Gupta A, Allen LA, Bhatt DL, Cox M, DeVore AD, Heidenreich PA, et al. Association of the Hospital Readmissions Reduction Program implementation with readmission and mortality outcomes in heart failure. JAMA Cardiol 2018;3(1):44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huckfeldt P, Escarce J, Wilcock A, Sood N, Rabideau B, Popescu I, et al. HF mortality trends under Medicare readmissions reduction program at penalized and nonpenalized hospitals. J Am Coll Cardiol 2018; 72(20):2539–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the Hospital Readmissions Reduction Program with mortality among Medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA 2018;320(24): 2542–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.CMS.gov [Internet] Baltimore (MD): Centers for Medicare and Medicaid Services. Press release, CMS Administrator Verma unveils new strategy to fuel data-driven patient care, transparency; 2018. April 26 [cited 2018 Dec 28]. Available from: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2018-Press-releases-items/2018-04-26.html [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


