Abstract
Background.
Despite the considerable physical, emotional and social change that occurs during emerging adulthood, there is little research that examines the association between having a chronic health condition and mental disorder during this developmental period. The aims of this study were to examine the sex-specific prevalence of lifetime mental disorder in an epidemiological sample of emerging adults aged 15–30 years with and without chronic health conditions; quantify the association between chronic health conditions and mental disorder, adjusting for sociodemographic and health factors; and, examine potential moderating and mediating effects of sex, level of disability and pain.
Method.
Data come from the Canadian Community Health Survey-Mental Health. Respondents were 15–30 years of age (n = 5947) and self-reported whether they had a chronic health condition. Chronic health conditions were classified as: respiratory, musculoskeletal/connective tissue, cardiovascular, neurological and endocrine/digestive. The World Health Organization Composite International Diagnostic Interview 3.0 was used to assess the presence of mental disorder (major depressive disorder, suicidal behaviour, bipolar disorder and generalised anxiety disorder).
Results.
Lifetime prevalence of mental disorder was significantly higher for individuals with chronic health conditions compared with healthy controls. Substantial heterogeneity in the prevalence of mental disorder was found in males, but not in females. Logistic regression models adjusting for several sociodemographic and health factors showed that the individuals with chronic health conditions were at elevated risk for mental disorder. There was no evidence that the level of disability or pain moderated the associations between chronic health conditions and mental disorder. Sex was found to moderate the association between musculoskeletal/connective tissue conditions and bipolar disorder (β = 1.71, p = 0.002). Exploratory analyses suggest that the levels of disability and pain mediate the association between chronic health conditions and mental disorder.
Conclusions.
Physical and mental comorbidity is prevalent among emerging adults and this relationship is not augmented, but may be mediated, by the level of disability or pain. Findings point to the integration and coordination of public sectors – health, education and social services – to facilitate the prevention and reduction of mental disorder among emerging adults with chronic health conditions.
Key words: Anxiety disorder, bipolar disorder, chronic disease, depression, epidemiological studies, mood disorder, suicidality
Introduction
It is well established that chronic physical health conditions and mental disorder are highly comorbid (Scott et al. 2007) and that the diagnosis of a chronic health condition early in life can have a detrimental impact on mental health later in adulthood (Green et al. 2010, McLaughlin et al. 2010). Although considerable physical, emotional and social change occur during emerging adulthood, the period between 15 and 25 years of age (Arnett, 2000), there is a paucity of research that examines the association between having a chronic health condition and mental disorder during this important developmental period.
Although emerging adults with a chronic health condition and comorbid mental disorder represent a relatively small proportion of the population, there are large public health implications with respect to the use and cost of health services in this understudied population. Due to improvements in the detection and treatment of chronic health conditions, 90% adolescents with a chronic health condition are living into adulthood (Ontario Association of Community Care Access Centres, 2013), placing considerable burden on health systems (Parekh & Barton, 2010) and having a significant individual and public health impact on impairment and premature mortality risk (Kessler et al. 2003, Zhang et al. 2005). Although existing evidence suggests an association between physical health and increased risk for mental disorder in clinical settings (Merikangas et al. 2015), relatively little is known about this relationship in the general population. Addressing this gap in knowledge would produce evidence-based findings that could inform policy and prevention and intervention efforts specifically aimed at reducing mental disorder among emerging adults with and without a chronic health condition.
Epidemiological studies that have included emerging adulthood-specific prevalence of mental disorders are few, and there is even less information available reporting estimates of mental disorder among adolescents and young adults with a chronic health condition. Among the few studies that do exist, they typically do not encompass the full spectrum of emerging adulthood; include relatively small samples; and, are limited to a single chronic health condition, focus on only one or two mental disorders, commonly depression and anxiety, that often do not include diagnostic assessment tools (Davies et al. 2003, Goodwin et al. 2004, Haarasilta et al. 2005, Katon et al. 2007). In addition, the prevalence estimates from these studies are becoming outdated and need to be verified with more contemporary data sources. A recent study of young people aged 9–21 years with chronic health conditions recruited from tertiary paediatric clinics found that approximately 12% have mood or anxiety disorders and there was a direct increase in the prevalence of mental disorders by chronic condition severity (Merikangas et al. 2015). The study by Merikangas et al. (2015) addressed several of the shortcomings of previous studies by including a large sample size, examining a number of physical and mental health conditions, and computing robust models of risk; however, the authors note their study design did not include a comprehensive diagnostic interview and their sampling method targeted young people with moderate or severe chronic health conditions and as a result, was not representative of the population.
In the present study, we used the Canadian Community Health Survey – Mental Health (CCHS-MH) to extend the strengths of previous research to investigate the following objectives: (1) Examine the sex-specific prevalence of lifetime mental disorder (major depressive disorder, suicidal behaviour, bipolar disorder and generalised anxiety disorder) in an epidemiological sample of emerging adults aged 15–30 years with and without chronic health conditions. (2) Quantify the association between chronic health conditions and mental disorder, adjusting for relevant sociodemographic and health factors. (3) Examine the potential moderating effects of sex, levels of disability and pain on risk for mental disorder. (4) Explore the potential mediating effects of levels of disability and pain on the association between chronic health conditions and mental disorder. Informed by previous research (Tunks et al. 2008, Merikangas et al. 2009, Stegmann et al. 2010, Campbell et al. 2015), it was hypothesised that the prevalence and risk for mental disorder would be higher among emerging adults with chronic health conditions; levels of disability and pain, but not sex, would moderate this association; and, levels of disability and pain would mediate the association between chronic health conditions and mental disorder.
Method
Data and sample
Data were obtained from the 2012 CCHS-MH; a national epidemiological study conducted by Statistics Canada (Statistics Canada, 2013). Using a multistage stratified cluster sampling design, a representative sample of respondents ≥15 years of age were included (n = 25 113). Individuals residing in the Canadian territories, Aboriginal settlements, institutions and full-time members of the Canadian Forces were excluded (representing approximately 3% of the target population). Most interviews (87%) were conducted in respondents’ households by an interviewer using computer-assisted personal interviewing. The household-level response rate was 80% and the combined household and person response rate was 69% (Statistics Canada, 2013). For this study, the sample was restricted to participants aged 15–30 years (n = 5947). While emerging adulthood is defined as the ages between 15 and 25 (Arnett, 2000), the age criteria for this study was increased to 30 years to ensure that adequate group sizes for chronic health conditions and mental disorder were available for analysis. All respondents were informed that participation in the CCHS-MH is voluntary with participant confidentiality and privacy guaranteed by Statistics Canada. Analyses were approved by the Hamilton Integrated Research Ethics Board.
Measures
The CCHS-MH used the World Health Organization (WHO) version of the Composite International Diagnostic Interview 3.0 (WHO-CIDI) to classify participants for lifetime axis I disorders according to the criteria defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and WHO International Classification of Disease 10th Revision (ICD-10) (Kessler & Üstün, 2004). The WHO-CIDI begins with a screening and lifetime review module that determines the number of diagnostic sections to be completed. In total, it contains 40 sections, 22 of which are diagnostic that assess mood, anxiety, substance use and other disorders. A considerable amount of methodological research has been carried out which suggests that the WHO-CIDI is valid and reliable (Kessler & Üstün, 2004, Kessler et al. 2004). Primary mental disorders derived in the CCHS-MH were: major depressive episode, suicidal behaviour (thought, plan or attempt; based on the Suicide sub-block of the WHO-CIDI), bipolar disorder and generalised anxiety disorder (Statistics Canada, 2013). The CCHS-MH did not use hierarchical diagnostic criteria for mental disorder; therefore, participants can meet criteria for multiple mental disorders.
Presence of a chronic health condition was assessed using a standard checklist by asking participants if they had been diagnosed by a health professional with a long-term health condition that had lasted or was expected to last at least six months. The conditions included in the CCHS-MH were: asthma, arthritis, back problems (not including fibromyalgia or arthritis), high blood pressure, migraine headache, chronic bronchitis/emphysema/chronic obstructive pulmonary disease, diabetes, epilepsy, heart disease, cancer, effects of a stroke, bowel disease (inflammatory bowel disease, Crohn's disease or ulcerative colitis), Alzheimer's disease/other dementia, chronic fatigue syndrome and multiple chemical sensitivities. As shown in Table 1, chronic conditions were categorised according to the ICD-10 (WHO, 2010): respiratory, musculoskeletal/connective tissue, cardiovascular, neurological and endocrine/digestive. Healthy controls were operationally defined as those participants who did not endorse a diagnosis of any chronic health condition. Based on this case ascertainment strategy, there were n = 1720 participants with a chronic health condition and n = 3527 healthy controls.
Table 1.
Categories of chronic health conditions based on the ICD-10
| Respiratory | Musculoskeletal/connective tissue | Cardiovascular | Neurological | Endocrine/digestive |
|---|---|---|---|---|
| • Asthma | • Arthritis | • Heart disease | • Alzheimer's disease/dementia | • Bowel disease |
| • Chronic bronchitis/emphysema/chronic obstructive pulmonary disease | • Back problems | • High blood pressure | • Chronic fatigue syndrome | • Diabetes |
| • Effects of stroke | ||||
| • Epilepsy | ||||
| • Migraine headaches |
Cancer and multiple chemical sensitivities were not included due to small sample counts and non-specific categorisation.
Disability was measured using the 12-item WHO Disability Assessment Schedule 2.0 (WHODAS 2.0) – generic, self-report measure of global disability severity (Üstün et al. 2010a, b). Domains of functioning assessed by the WHODAS 2.0 are: cognition, mobility, self-care, getting along, life activities and participation. Items on the WHODAS 2.0 are rated using a five-point scale. It asks, ‘In the past 30 days, how much difficulty did you have in…’ Responses range from 0 = none to 4 = extreme/cannot do. Scoring the WHODAS 2.0 in the CCHS-MH was based on the complex scoring method in accordance with published instructions (Üstün et al. 2010b, Statistics Canada, 2013). This method takes into account multiple levels of difficulty for each item. The overall score ranges from 0 to 100, where 0 is no disability and 100 is complete disability. WHODAS 2.0 scores were categorised according to population percentiles to reflect none/mild (<2.8), moderate (2.8–5.5) and severe disability (≥5.6) (Üstün et al. 2010b). The WHODAS 2.0 has good psychometric properties (Andrews et al. 2009, Federici & Meloni, 2010, Üstün et al. 2010b, Kimber et al. 2015). In this sample, the internal consistency reliability was α = 0.84.
Pain was assessed using responses from two items which asked participants whether they are usually free of pain or discomfort (Statistics Canada, 2013). Participants who responded in the affirmative were coded as having no pain. Participants who responded in the negative were then asked to describe the usual intensity of their pain or discomfort as ‘mild’, ‘moderate’, or ‘severe’. Higher scores on the pain measure represent more intense pain or discomfort. Due to low cell counts, participants coded as ‘moderate’ or ‘severe’ were aggregated in the analyses.
Sociodemographic covariates were included in the analyses to provide unbiased estimates of the association between chronic health conditions and mental disorder. These were: participant age and sex, marital status (living with a partner or not), employment (full- or part-time employed or not), immigrant status (born or not born in Canada) and annual household income (from <$20 000 to ≥$100 000 in $20 000 increments).
Analysis
Sex-specific lifetime prevalence of mental disorders was estimated and compared across chronic health conditions using χ2 tests. The Holm–Bonferroni correction was used to adjust for multiple testing to control the family-wise error rate (Holm, 1979). Logistic regression models were computed to quantify the association chronic health conditions and mental disorder, adjusting for participant age, sex, immigrant status, education, household income, level of disability and other physical and mental disorders. Odds ratios (OR) and associated 95% confidence intervals (CI) were computed. Product–term interactions between chronic health conditions and sex, levels of disability and pain, respectively, were included in the logistic regression models to examine the potential moderating effects of these variables on the risk for mental disorder. The product of coefficients method was used to explore whether the level of disability or pain mediated the association between chronic health conditions and mental disorder (MacKinnon, 2008). The Sobel test was used to determine whether the mediating effect was statistically significant (Sobel, 1982). Sampling weights based on the probabilities of selection and participation, developed by Statistics Canada were applied to the analyses to ensure comparability between the CCHS-MH sample and Canadian population. A total of n = 104 (1.7%) of participants had missing data for any lifetime mental disorder. Missing data were associated with lower household income, OR = 0.90 (0.83, 0.98). Analyses were conducted with SAS 9.4 (SAS Institute Inc.).
Results
Sample characteristics
The mean age of participants was 23.5 (SE 0.1) years and 52% were male. Nearly half (45%) had completed postsecondary education, 71% were employed full-time, 25% were living with a partner, and 20% were immigrants. As measured by the WHODAS 2.0, 62% of participants had disability that was classified as none/mild. The group of individuals with chronic health conditions included significantly fewer males (χ2 = 16.5) and immigrants (χ2 = 33.6), had lower income (χ2 = 25.4), and more disability (χ2 = 159.4) and pain (χ2 = 186.5; p < 0.01 for all). There were no significant differences in age, educational attainment, employment or marital status. Detailed sample characteristics and pairwise contrasts among subgroups are shown in Table 2.
Table 2.
Sample characteristice
| Healthy controls (n = 3527) | Respiratory (n = 427) | Musculoskeletal/connective tissue (n = 421) | Cardiovascular (n = 75) | Neurological (n = 633) | Endocrine/digestive (n = 164) | χ2 (p-value) | Pairwise contrasts | |
|---|---|---|---|---|---|---|---|---|
| Age (year) | ||||||||
| 15–19 | 32.6 | 42.7* | 26.0* | 30.5 | 27.7* | 23.0* | 25.4 (0.005) | R < E, N, M |
| 20–24 | 30.3 | 26.9 | 29.3 | 29.5 | 29.6 | 24.7 | ||
| 25–30 | 37.1 | 30.5 | 44.7 | 40.1 | 42.8 | 52.4 | ||
| Male | 55.2 | 52.9 | 47.3* | 61.2 | 40.1* | 32.6* | 33.5 (<0.001) | R, M, C > E, N; M < C |
| Living with partner | 23.8 | 20.4 | 27.0 | 24.6 | 29.9 | 30.9 | 9.8 (0.081) | |
| postsecondary graduate | 45.9 | 32.5* | 48.2 | 36.6 | 41.9 | 50.8 | 27.9 (0.022) | R < M, C, N, E; M > N; C, N < E |
| Full-time employment | 71.0 | 42.1 | 49.6 | 54.9 | 47.8 | 50.6 | 2.8 (0.736) | |
| Immigrant | 23.9 | 13.4* | 12.3* | 15.7 | 9.4* | 2.8* | 44.6 (<0.001) | E < R, M, C, N; N < R |
| Household income, Cad | ||||||||
| <$20 000 | 7.6 | 10.7* | 13.7* | 9.7 | 10.6* | 9.2* | 80.7 (0.004) | R < M, C, N, E |
| $20 000–39 999 | 15.1 | 16.7 | 17.2 | 20.9 | 19.7 | 23.9 | ||
| $40 000–59 999 | 16.8 | 14.2 | 14.9 | 22.3 | 18.1 | 20.9 | ||
| $60 000–79 999 | 16.9 | 24.1 | 14.6 | 12.3 | 12.7 | 9.2 | ||
| $80 000–99 999 | 12.6 | 10.9 | 12.0 | 4.4 | 13.7 | 10.6 | ||
| ≥$100 000 | 30.8 | 23.5 | 27.6 | 30.6 | 25.2 | 26.5 | ||
| Disability, WHODAS 2.0 | ||||||||
| None/mild | 70.5 | 58.1* | 43.2* | 40.4* | 40.8* | 36.4* | 201.9 (<0.001) | R < M, C, N, E |
| Moderate | 12.4 | 12.3 | 10.3 | 13.4 | 13.3 | 15.0 | ||
| Severe | 17.1 | 29.2 | 45.2 | 44.6 | 45.3 | 48.4 | ||
| Pain | ||||||||
| None | 95.5 | 91.0 | 61.7* | 78.8* | 76.3* | 72.2* | 323.4 (<0.001) | R < M, C, N, E; M > C, N, E |
| Mild | 2.8 | 4.0 | 13.8 | 13.1 | 8.1 | 9.5 | ||
| Moderate/severe | 1.7 | 5.0 | 24.5 | 8.2 | 15.7 | 18.4 | ||
Data are percentages. Pairwise contrasts were made among the various chronic health condition categories when the overall χ2 was statistically significant. Chronic health conditions: C, cardiovascular; E, endocrine/digestive; M, musculoskeletal/connective tissue; N, neurological; R, respiratory.
Denotes significantly different from healthy controls at p < 0.05.
Lifetime prevalence of mental disorder
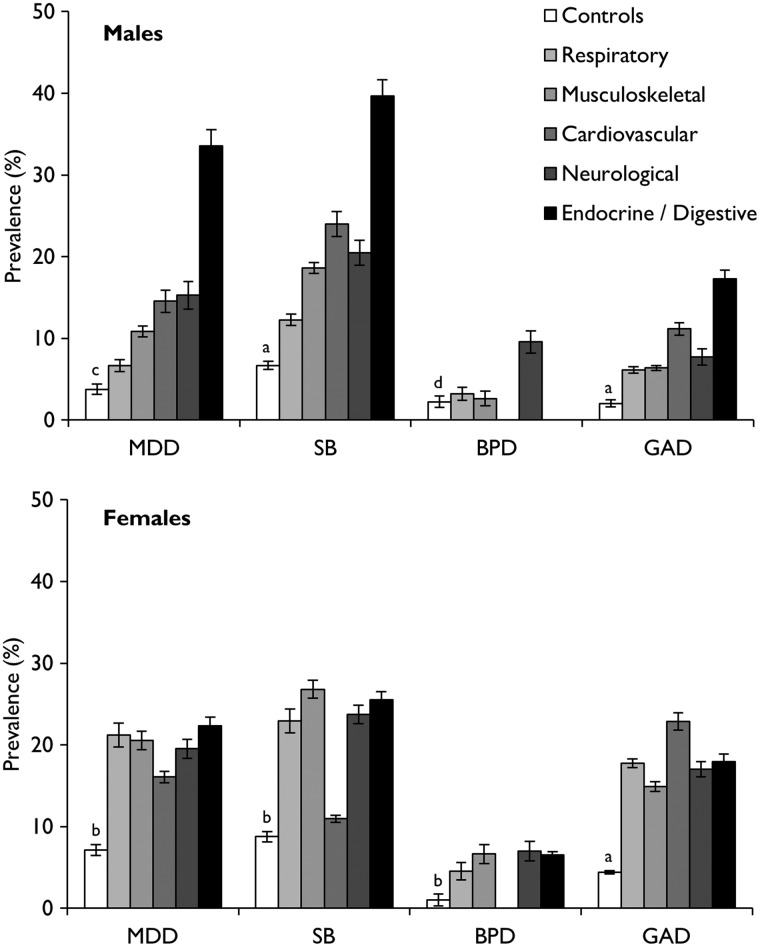
Lifetime prevalence of mental disorders is shown in Fig. 1. Males and females with chronic health conditions typically had higher prevalence of mental disorder compared with healthy controls. As well, substantial heterogeneity of prevalence estimates was found for males with chronic health conditions, but not for females. Males with endocrine/digestive conditions had significantly higher prevalence of major depressive disorder (33.5%) and suicidal behaviour (39.7%) compared with those with respiratory (6.6, 12.3%), musculoskeletal/connective tissue (10.8, 18.6%) or neurological conditions (15.3, 20.5%; p < 0.001 for all). In addition, males with neurological conditions had significantly higher prevalence of major depressive (15.3%) and bipolar disorder (9.6%) compared with those with respiratory conditions (6.6, 3.2%; p = 0.003). Prevalence estimates for bipolar disorder among males with cardiovascular or endocrine/digestive conditions and females with cardiovascular conditions were not released by Statistics Canada.
Fig. 1.
Lifetime prevalence of mental disorders. Due to small cell counts, prevalence of BPD was not released for males and females with a cardiovascular condition and males with an endocrine/digestive condition. Chronic health conditions: C, cardiovascular; E, endocrine/digestive; M, musculoskeletal/connective tissue; N, neurological; R, respiratory. Mental disorders: BPD, bipolar disorder; GAD, generalised anxiety disorder; MDD, major depressive disorder; SB, suicidal behaviour.
aControls < R, M, C, N, E; bControls < R, M, N, E; cControls < M, C, N, E; dControls < N.
Risk for mental disorder
Pooling male and female data, logistic regression models, adjusting for a number of sociodemographic and health variables were computed to examine the association between having a chronic health condition and lifetime mental disorder (Table 3). Participants with respiratory conditions were at increased risk for suicidal behaviour (OR = 1.74, p = 0.013) and generalised anxiety disorder (OR = 1.93, 0.035). Having a musculoskeletal/connective tissue condition increased risk for suicidal behaviour (OR = 1.91, p = 0.002) and cardiovascular conditions increased risk for generalised anxiety disorder (OR = 3.49, 0.021). Participants with neurological conditions had increased risk for suicidal behaviour (OR = 1.56, 0.015) and bipolar disorder (OR = 2.06, 0.025). Participants with endocrine/digestive conditions were at increased risk for major depressive disorder (OR = 2.25, p = 0.013) and suicidal behaviour (OR = 2.04, p = 0.008).
Table 3.
Logistic regression of lifetime mental disorders
| Major depressive disorder | Suicidal behaviour | Bipolar disorder | Generalised anxiety disorder | |
|---|---|---|---|---|
| Respiratory | 1.44 (0.90, 2.30) | 1.74 (1.19, 2.53) | 1.23 (0.59, 2.54) | 1.93 (1.05, 3.57) |
| Musculoskeletal/connective tissue | 1.41 (0.84, 2.38) | 1.91 (1.26, 2.90) | 1.04 (0.50, 2.14) | 1.28 (0.77, 2.15) |
| Cardiovascular | 1.63 (0.56, 4.75) | 1.41 (0.49, 4.00) | 0.65 (0.18, 2.30) | 3.49 (1.20, 10.11) |
| Neurological | 1.52 (0.96, 2.41) | 1.56 (1.09, 2.24) | 2.06 (1.09, 3.87) | 1.65 (0.91, 2.31) |
| Endocrine/digestive | 2.25 (1.19, 4.28) | 2.04 (1.20, 3.46) | 1.32 (0.54, 3.24) | 1.57 (0.78, 3.16) |
Results are reported as adjusted ORs and 95% Cis (significant findings are shown in bold). Healthy controls were the reference category and models controlled for age, sex, immigrant status, education, household income, level of disability, pain, and all other physical and mental disorders shown in the table.
Moderating effects of sex, level of disability and pain
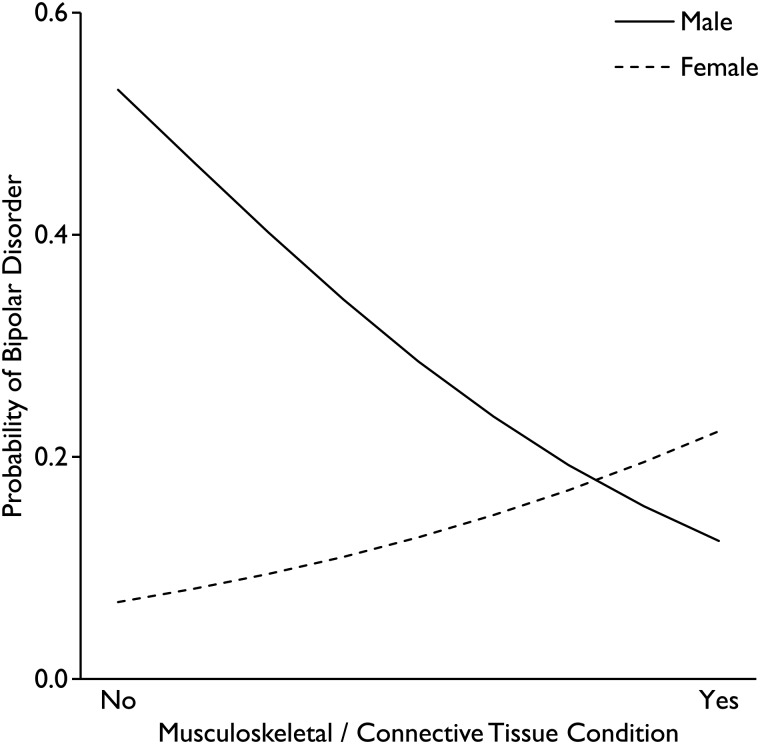
As shown in Table 4, participant sex was found to moderate the association between musculoskeletal/connective tissue conditions and bipolar disorder (OR = 5.54, p = 0.009). Results showed that the risk for bipolar disorder was higher for males without musculoskeletal/connective tissue conditions compared with females; however, among participants with musculoskeletal/connective tissue conditions, risk was higher for females compared with males. An illustration of this qualitative interaction is shown in Fig. 2. None of the models suggested that the level of disability or pain moderated the association between chronic health conditions and mental disorder.
Table 4.
Moderating effects of sex, disability and pain
| Major depressive disorder | Suicidal behaviour | Bipolar disorder | Generalised anxiety disorder | |
|---|---|---|---|---|
| Sex | ||||
| Respiratory | 1.18 (0.46, 3.01) | 1.22 (0.58, 2.57) | 1.93 (0.44, 8.51) | 0.85 (0.24, 2.93) |
| Musculoskeletal/connective tissue | 0.82 (0.32, 2.10) | 0.66 (0.30, 1.44) | 5.54 (1.53, 20.06) | 0.72 (0.28, 1.87) |
| Cardiovascular | 0.64 (0.10, 4.04) | 0.16 (0.02, 1.47) | 1.84 (0.15, 22.75) | 1.57 (0.19, 12.95) |
| Neurological | 0.63 (0.24, 1.65) | 0.82 (0.40, 1.68) | 1.07 (0.34, 3.40) | 1.78 (0.60, 5.29) |
| Endocrine/digestive | 0.34 (0.10, 1.16) | 0.51 (0.17, 1.47) | 3.13 (0.52, 18.97) | 0.76 (0.14, 4.26) |
| Disability | ||||
| Respiratory | 1.18 (0.67, 2.08) | 1.10 (0.73, 1.68) | 1.02 (0.45, 2.35) | 0.67 (0.36, 1.24) |
| Musculoskeletal/connective tissue | 0.68 (0.41, 1.13) | 0.71 (0.47, 1.07) | 1.40 (0.63, 3.11) | 0.79 (0.47, 1.35) |
| Cardiovascular | 0.61 (0.34, 1.11) | 0.64 (0.26, 1.55) | 1.52 (0.75, 4.09) | 0.70 (0.21, 2.32) |
| Neurological | 0.83 (0.53, 1.32) | 0.92 (0.63, 1.34) | 1.07 (0.56, 2.05) | 0.89 (0.55, 1.46) |
| Endocrine/digestive | 0.61 (0.32, 1.17) | 0.72 (0.41, 1.28) | 1.45 (0.47, 4.55) | 1.09 (0.50, 2.41) |
| Pain | ||||
| Respiratory | 1.60 (0.76, 3.35) | 0.83 (0.41, 1.70) | 0.53 (0.14, 1.99) | 0.48 (0.18, 1.33) |
| Musculoskeletal/connective tissue | 0.61 (0.31, 1.20) | 0.78 (0.42, 1.45) | 1.20 (0.38, 3.81) | 0.59 (0.30, 1.18) |
| Cardiovascular | 0.87 (0.26, 2.91) | 0.50 (0.12, 2.08) | 6.61 (0.74, 59.25) | 0.48 (0.14, 1.61) |
| Neurological | 0.74 (0.39, 1.41) | 0.99 (0.52, 1.86) | 1.05 (0.39, 2.80) | 0.72 (0.35, 1.48) |
| Endocrine/digestive | 1.25 (0.56, 2.78) | 0.92 (0.43, 1.95) | 1.18 (0.35, 3.90) | 1.14 (0.40, 3.20) |
Results are reported as adjusted ORs and 95% Cis for the product-term interactions between the moderator (sex, disability and pain) and chronic health condition (significant findings are shown in bold). Healthy controls were the reference category and models controlled for age, sex, immigrant status, education, household income, level of disability, pain, and all other physical and mental disorders shown in the table.
Fig. 2.
Moderating effect of sex on the association between musculoskeletal/connective tissue conditions and bipolar disorder.
Mediating effects of level of disability and pain
Table 5 presents the results of the mediation analyses. Across all models tested, the level of disability was found to significantly mediate the association between chronic health conditions and mental disorder. The proportion of the association between chronic health conditions and mental disorder mediated by the level of disability ranged from a low of 35.2% for respiratory conditions and suicidal behaviour to a high of 94.6% for musculoskeletal/connective tissue conditions and bipolar disorder.
Table 5.
Mediating effects of disability and pain
| Major depressive disorder | Suicidal behaviour | Bipolar disorder | Generalised anxiety disorder | |
|---|---|---|---|---|
| Disability | ||||
| Respiratory | 0.31 (0.13)* | 0.30 (0.12)** | 0.44 (0.19)* | 0.39 (0.16)* |
| Musculoskeletal/connective tissue | 0.45 (0.16)** | 0.44 (0.14)** | 0.64 (0.24)** | 0.57 (0.19)** |
| Cardiovascular | 0.70 (0.28)* | 0.68 (0.25)** | 0.98 (0.41)* | 0.88 (0.33)** |
| Neurological | 0.66 (0.21)* | 0.64 (0.18)*** | 0.93 (0.32)** | 0.83 (0.24)*** |
| Endocrine/digestive | 0.74 (0.26)* | 0.72 (0.22)*** | 1.05 (0.39)** | 0.93 (0.30)** |
| Pain | ||||
| Respiratory | – | 0.40 (0.24) | – | 0.48 (0.29) |
| Musculoskeletal/connective tissue | – | 1.49 (0.49)** | – | 1.79 (0.59)** |
| Cardiovascular | – | 0.84 (0.36)* | – | 1.00 (0.43)* |
| Neurological | – | 1.01 (0.35)** | – | 1.21 (0.42)** |
| Endocrine/digestive | – | 1.12 (0.41)** | – | 1.35 (0.50)** |
Results are reported as adjusted coefficient (standard error). Models controlled for age, sex, immigrant status, education, household income, level of disability, pain, and all other physical and mental disorders shown in the table.
*p < 0.05; **p < 0.01; ***p < 0.001.
Pain was not found to be associated with the major depressive disorder and bipolar disorder, thus tests of mediation were not conducted for these mental disorders. There was no evidence to suggest that pain mediated the association between respiratory conditions and suicidal behaviour or generalised anxiety disorder (Table 5). The proportion of the association between chronic health conditions and mental disorder mediated by pain ranged from a low of 44.5% for respiratory conditions and generalised anxiety disorder to a high of 87.7% for musculoskeletal/connective tissue conditions and generalised anxiety disorder.
Discussion
Summary of findings
Using recent data from a large, representative study of the Canadian population, findings provided evidence to suggest that the lifetime prevalence of major depressive episode, suicidal behaviour, bipolar disorder and generalised anxiety disorder was higher among emerging adults aged 15–30 years with a chronic health condition compared with healthy controls. And, after adjusting for potential confounding sociodemographic and health factors, individuals with a chronic health condition were at increased risk for lifetime mental disorder compared with healthy controls. Hypotheses were supported in that emerging adults with chronic health conditions were at increased risk for at least one mental disorder. Prevalence estimates were comparable, albeit somewhat lower, than those reported previously (Merikangas et al. 2015). These differences are likely attributable to differences in the sampling of participants and assessment of chronic health conditions and mental disorder. In contrast to our study, Merikangas et al. (2015) sampled a younger study population through paediatric outpatient clinics who had more severe chronic health conditions and did not assess mental disorder with a comprehensive interview.
The pronounced heterogeneity in prevalence estimates for mental disorder across chronic health conditions among males compared with females was largely influenced by the high rates of mental disorder in the neurological and endocrine/digestive groups. Largely unpredictable exacerbations in conditions such as epilepsy, migraine headache and inflammatory bowel disease may lead to learned helplessness and a loss of sense of control resulting in declines in mental health (Chaney et al. 1999, Liu et al. 2000, Henkel et al. 2002), particularly among emerging adult males. Likewise, individuals with neurological or endocrine/digestive conditions report high levels of felt and enacted stigma (Jacoby et al. 2005, Saunders, 2014). Evidence suggests that gender differences exist in perceived stigma, whereby males with chronic health conditions report more stigma which negatively affects their mental health and quality of life (Van Brakel, 2006).
As expected, differences in estimates between chronic health conditions and healthy controls were larger than differences among chronic health conditions. Similar findings have been reported in meta-analytic studies of mental health in children and adolescents (Pinquart & Shen, 2011a, b, c, Ferro & Boyle, 2013). A recent longitudinal study of an epidemiological sample of emerging adults showed that while those with asthma or epilepsy were at elevated risk for psychological distress compared with controls, no differences were found between the asthma and epilepsy groups (Ferro, 2014). Although there are differences in the pathophysiology of chronic health conditions, findings from this epidemiological study and previous research suggests a common level of underlying risk for mental disorder among emerging adults with chronic health conditions.
Some notable associations identified in this study warrant discussion. First, the strong association between neurological conditions and bipolar disorder confirms findings from previous epidemiological and small-scale clinical studies of individuals with epilepsy, migraine headache and multiple sclerosis (Ettinger et al. 2005, Sidhom et al. 2014, Wotton & Goldacre, 2014). Biological explanations for this association are unclear; however, several common mechanisms have been identified that can predispose individuals with neurological conditions to bipolar disorder (see Ettinger et al. 2005).
Second, the association between endocrine/digestive conditions and major depressive disorder may in part be attributable to shared neurobiological and psychosocial risk factors (Keethy et al. 2014), as well as symptom manifestations and complications that impair participation and engagement (Szigethy et al. 2014, Morgan et al. 2014). For example, youth with inflammatory bowel disease have increased rates of school absenteeism that result in missed social opportunities and declines in academic achievement, mental health and functioning (Mackner et al. 2012). The high comorbidity between depression/anxiety and suicidal behaviour (Avenevoli et al. 2015) may also contribute to the strong association between respiratory or endocrine/digestive conditions and suicidal behaviour which has been reported in other epidemiological studies of emerging adults (Radobuljac et al. 2009, Bandiera et al. 2013, Chung et al. 2014).
Hypotheses surrounding the moderating effects of sex, level of disability and pain were not supported by the findings. Levels of disability and pain were not found to moderate the association between chronic health conditions and mental disorder. The absence of these moderating effects suggest that individuals with a chronic health condition, regardless of its severity or impact on functioning, are at increased vulnerability for mental disorder. While there is some evidence for an association between musculoskeletal/connective tissue conditions with bipolar disorder (Patten et al. 2006, Evans-Lacko et al. 2009), this is the first study to demonstrate a moderating effect of sex on this association. Future studies are needed to replicate this finding to determine if it is sample-dependent or is evidence of true effect modification.
Levels of disability and pain were found to mediate the association between chronic health conditions and mental disorder, supporting the hypotheses. While these meditational analyses have not been conducted among emerging adults, similar findings have been found in other epidemiological samples of older adults (Ormel et al. 1997, Tunks et al. 2008, Scott et al. 2009, Stegmann et al. 2010). In many instances, chronic health conditions are incurable; as mediators, level of disability and pain represent modifiable targets for intervention that can potential attenuate the negative impact of chronic health conditions on mental disorder.
Implications
Findings from this study have implications for the integration and coordination of services within and across public sectors for individuals with chronic health conditions. Within the health system, the systematic integration of primary care and mental health services are warranted to help mute the observed health declines and failure to achieve developmental milestones associated with having a chronic health condition during emerging adulthood (Reid et al. 2004, Maslow et al. 2011a, b). Evidence suggests that the assessment and subsequent treatment of mental disorder is a cost-effective way to improve the quality-adjusted life years among those with chronic health conditions (Jeeva et al. 2013). Furthermore, the education system is uniquely positioned to deliver broad risk-reduction strategies, as well as targeted interventions (Kratochwill & Shernoff, 2004, National Research Council and Institute of Medicine, 2009) that have sustained effectiveness and reduce the stigma associated with seeking mental health services (Clarke et al. 1995, Lowry-Webster et al. 2001, Weare & Nind, 2011, Cuijpers et al. 2012). Finally, social services can integrate their services with the education system to support participation, social and employment opportunities, and community engagement for emerging adults with chronic health conditions thereby facilitating the prevention or reduction of mental disorder and substance use (Baggio et al. 2015).
Study limitations
These findings should be interpreted in the context of the following limitations. The cross-sectional deign of the study prevented the examination of the temporal relationship between having a chronic health condition and development of a mental disorder among emerging adults. Although mental disorder was contextualised as the outcome in this study, there is some epidemiological evidence suggesting that mental health can contribute to the development of chronic health conditions (Chen et al. 2009, Scott et al. 2011). Chronic health conditions were self-reported and could not be validated with administrative health records. Epidemiological evidence suggests that discordance between self-reported diagnoses and administrative data is relatively large for many chronic conditions, particularly for those with low prevalence (Muggah et al. 2013). This potential information bias may have resulted in non-differential misclassification, likely leading to attenuated associations between chronic health conditions and mental disorder. Due to the relatively small number of participants with cardiovascular or endocrine/digestive conditions, this study may have been underpowered to detect significant associations between these types of conditions and mental disorder (Hsieh, 1989, Hsieh et al. 1998).
Conclusions
Physical and mental comorbidity is an important public health concern. Emerging adults with chronic health conditions are at risk for mental disorder compared their healthy counterparts. There was no evidence of a moderating effect of the level of disability or pain on the association between chronic health conditions and mental disorder; however, they were found to mediate this association. Additional epidemiological research is needed to replicate and expand upon these findings to identify patterns of association, as well as to elucidate other mediating and moderating factors in potential causal pathways between having a chronic health condition and the onset of mental disorder. Health professionals, educators, and those in social services should continue to be mindful of the significant mental health burden among emerging adults with chronic health conditions and strive to integrate services across these sectors to facilitate the optimal mental health outcomes in this vulnerable population.
Acknowledgements
This work was conducted using data collected by Statistics Canada. However, the analyses presented here were conducted by the author and the interpretations presented in this paper do not reflect the interpretations or opinions of Statistics Canada.
Financial Support
Dr. Ferro is supported by the Research Early Career Award from Hamilton Health Sciences.
Conflict of Interest
None.
Ethical Standards
The author asserts that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Andrews G, Kemp A, Sunderland M, Von Korff M, Üstün TB (2009). Normative data for the 12 item WHO disability assessment Schedule 2.0. PLoS ONE 4, e8343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood. A theory of development from the late teens through the twenties. American Psychologist 55, 469–480. [PubMed] [Google Scholar]
- Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR (2015). Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. Journal of the American Academy of Child and Adolesclescent Psychiatry 54, 37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggio S, Iglesias K, Deline S, Studer J, Henchoz Y, Mohler-Kuo M, Gmel G (2015). Not in education, employment, or training status among young Swiss men. Longitudinal associations with mental health and substance use. Journal of Adolescent Health 56, 238–243. [DOI] [PubMed] [Google Scholar]
- Bandiera FC, Ramirez R, Arheart KL, Canino G, Goodwin R.D (2013). Asthma and suicidal ideation and behavior among Puerto Rican older children and adolescents. Journal of Nervous and Mental Disease 201, 587–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell G, Darke S, Bruno R, Degenhardt L (2015). The prevalence and correlates of chronic pain and suicidality in a nationally representative sample. Australian and New Zealand Journal of Psychiatry. doi: 10.1177/0004867415569795. [DOI] [PubMed] [Google Scholar]
- Chaney JM, Mullins LL, Uretsky DL, Pace TM, Werden D, Hartman VL (1999). An experimental examination of learned helplessness in older adolescents and young adults with long-standing asthma. Journal of Pediatric Psychology 24, 259–270. [DOI] [PubMed] [Google Scholar]
- Chen H, Cohen P, Crawford TN, Kasen S, Guan B, Gorden K (2009). Impact of early adolescent psychiatric and personality disorder on long-term physical health: a 20-year longitudinal follow-up study. Psychological Medicine 39, 865–874. [DOI] [PubMed] [Google Scholar]
- Chung JH, Moon K, Kim DH, Min JW, Kim TH, Hwang HJ (2014). Suicidal ideation and suicide attempts among diabetes mellitus: The Korea National Health and Nutrition Examination Survey (KNHANES IV, V) from 2007 to 2012. Journal of Psychosomatic Research 77, 457–461. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR (1995). Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. Journal of the American Academy of Child and Adolescent Psychiatry 34, 312–321. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Beekman AT, Reynolds CF (2012). Preventing depression: a global priority. JAMA 307, 1033–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies S, Heyman I, Goodman R (2003). A population survey of mental health problems in children with epilepsy. Developmental Medicine and Child Neurology 45, 292–295. [DOI] [PubMed] [Google Scholar]
- Ettinger AB, Reed ML, Goldberg JF, Hirschfeld RM (2005). Prevalence of bipolar symptoms in epilepsy vs other chronic health disorders. Neurology 65, 535–540. [DOI] [PubMed] [Google Scholar]
- Evans-Lacko SE, Zeber JE, Gonzalez JM, Olvera RL (2009). Medical comorbidity among youth diagnosed with bipolar disorder in the United States. Journal of Clinical Psychiatry 70, 1461–6. [DOI] [PubMed] [Google Scholar]
- Federici S, Meloni F (2010). WHODAS II: disability self-evaluation in the ICF conceptual frame In International Encyclopedia of Rehabilitation (ed. Stone JH and Blouin M), Center for International Rehabilitation Research Information and Exchange: Buffalo: Retrieved from http://cirrie.buffalo.edu/encyclopedia/en/article/299/ [Google Scholar]
- Ferro MA (2014). Adolescents and young adults with physical illness: a comparative study of psychological distress. Acta Paediatrica 103, e32–e37. [DOI] [PubMed] [Google Scholar]
- Ferro MA, Boyle MH (2013). Self-concept among children and adolescents with a chronic illness: a meta-analytic review. Health Psychology 32, 839–848. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Fergusson DM, Horwood LJ (2004). Asthma and depressive and anxiety disorders among young persons in the community. Psychological Medicine 34, 1465–1474. [DOI] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Archives of General Psychiatry 67, 113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haarasilta L, Marttunen M, Kaprio J, Aro H (2005). Major depressive episode and physical health in adolescents and young adults: results from a population-based interview survey. European Journal of Public Health 15, 489–493. [DOI] [PubMed] [Google Scholar]
- Henkel V, Bussfeld P, Moller HJ, Hegerl U (2002). Cognitive-behavioural theories of helplessness/hopelessness: valid models of depression? European Archives of Psychiatry and Clinical Neuroscience 252, 240–249. [DOI] [PubMed] [Google Scholar]
- Holm S (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics 6, 65–70. [Google Scholar]
- Hsieh FY (1989). Sample size tables for logistic regression. Statistics in Medicine 8, 795–802. [DOI] [PubMed] [Google Scholar]
- Hsieh FY, Bloch DA, Larsen MD (1998). A simple method of sample size calculation for linear and logistic regression. Statistics in Medicine 17, 1623–1634. [DOI] [PubMed] [Google Scholar]
- Jacoby A, Snape D, Baker GA (2005). Epilepsy and social identity: the stigma of a chronic neurological disorder. Lancet Neurology 4, 171–178. [DOI] [PubMed] [Google Scholar]
- Jeeva F, Dickens C, Coventry P, Bundy C, Davies L (2013). Is treatment of depression cost-effective in people with diabetes? A systematic review of the economic evidence. International Journal of Technology Assessment in Health Care 29, 384–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W, Lozano P, Russo J, McCauley E, Richardson L, Bush T (2007). The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. Journal of Adolescent Health 41, 455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keethy D, Mrakotsky C, Szigethy E (2014). Pediatric inflammatory bowel disease and depression: treatment implications. Current Opinion in Pediatrics 26, 561–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Üstün TB (2004). The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research 13, 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Demler O, Stang PE (2003). Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: results from the national comorbidity survey. Journal of Occupational and Environmental Medicine 45, 1257–1266. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, Howes MJ, Jin R, Vega WA, Walters EE, Wang P, Zaslavsky A, Zheng H (2004). Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI). International Journal of Methods in Psychiatric Research 13, 122–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimber M, Rehm J, Ferro MA (2015). Measurement Invariance of the WHODAS 2.0 in a population-based sample of youth. Manuscript Submitted for Publication. [DOI] [PMC free article] [PubMed]
- Kratochwill TR, Shernoff ES (2004). Evidence-based practice: promoting evidence-based interventions in school psychology. School Psychology Quarterly 18, 389–408. [Google Scholar]
- Liu X, Kurita H, Uchiyama M, Okawa M, Liu L, Ma D (2000). Life events, locus of control, and behavioral problems among Chinese adolescents. Journal of Clinical Psychology 56, 1565–1577. [DOI] [PubMed] [Google Scholar]
- Lowry-Webster HM, Barrett PM, Dadds MR (2001). A universal prevention trial of anxiety and depressive symptomatology in childhood: preliminary data from an Australian study. Behaviour Change 18, 36–50. [Google Scholar]
- MacKinnon DP (2008). Introduction to Statistical Mediation Analysis. Erlbaum Psych Press: Hoboken. [Google Scholar]
- Mackner LM, Bickmeier RM, Crandall WV (2012). Academic achievement, attendance, and school-related quality of life in pediatric inflammatory bowel disease. Journal of Developmental and Behavioral Pediatrics 33, 106–111. [DOI] [PubMed] [Google Scholar]
- Maslow GR, Haydon A, McRee AL, Ford CA, Halpern CT (2011a). Growing up with a chronic illness: social success, educational/vocational distress. Journal of Adolescent Health 49, 206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslow GR, Haydon AA, Ford CA, Halpern CT (2011b). Young adult outcomes of children growing up with chronic illness: an analysis of the National longitudinal study of adolescent health. Archives of Pediatrics and Adolescent Medicine 165, 256–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication II: associations with persistence of DSM-IV disorders. Archives of General Psychiatry 67, 124–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Nakamura EF, Kessler RC (2009). Epidemiology of mental disorders in children and adolescents. Dialogues in Clinical Neuroscience 11, 7–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Calkins ME, Burstein M, He JP, Chiavacci R, Lateef T, Ruparel K, Gur RC, Lehner T, Hakonarson H, Gur RE (2015). Comorbidity of physical and mental disorders in the neurodevelopmental genomics cohort study. Pediatrics 135, e927–e938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan E, Patterson CC, Cardwell CR (2014). General practice-recorded depression and antidepressant use in young people with newly diagnosed type 1 diabetes: a cohort study using the clinical practice research datalink. Diabetic Medicine 31, 241–245. [DOI] [PubMed] [Google Scholar]
- Muggah E, Graves E, Bennett C, Manuel DG (2013). Ascertainment of chronic diseases using population health data: a comparison of health administrative data and patient self-report. BMC Public Health 13, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council & Institute of Medicine (2009). Preventing Mental, Emotional, and Behaviorial Disorders among Young People: Progress and Possibilities. Committee on Prevention of Mental Disorders and Substance Abuse among Children, Youth, and Young Adults: Research Advances and Promising Interventions. The National Academies Press: Washington, DC. [PubMed] [Google Scholar]
- Ontario Association of Community Care Access Centres (2013). Health Comes Home: A Conversation About Children With Complex Health Needs Part 3. Ontario Association of Community Care Access Centres: Toronto. [Google Scholar]
- Ormel J, Kempen GI, Penninx BW, Brilman EI, Beekman AT, van Sonderen E (1997). Chronic medical conditions and mental health in older people: disability and psychosocial resources mediate specific mental health effects. Psychological Medicine 27, 1065–77. [DOI] [PubMed] [Google Scholar]
- Parekh AK, Barton MB (2010). The challenge of multiple comorbidity for the US health care system. JAMA 303, 1303–1304. [DOI] [PubMed] [Google Scholar]
- Patten SB, Williams JV, Wang J (2006). Mental disorders in a population sample with musculoskeletal disorders. BMC Musculoskeletal Disorder 7, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, Shen Y (2011a). Anxiety in children and adolescents with chronic physical illnesses: a meta-analysis. Acta Paediatrica 100, 1069–1076. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Shen Y (2011b). Behavior problems in children and adolescents with chronic physical illness: a meta-analysis. Journal of Pediatric Psychology 36, 1003–1016. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Shen Y (2011c). Depressive symptoms in children and adolescents with chronic physical illness: an updated meta-analysis. Journal of Pediatric Psychology 36, 375–384. [DOI] [PubMed] [Google Scholar]
- Radobuljac MD, Bratina NU, Battelino T, Tomori M (2009). Lifetime prevalence of suicidal and self-injurious behaviors in a representative cohort of Slovenian adolescents with type 1 diabetes. Pediatric Diabetes 10, 424–431. [DOI] [PubMed] [Google Scholar]
- Reid GJ, Irvine MJ, McCrindle BW, Sananes R, Ritvo PG, Siu SC, Webb GD (2004). Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics 113, e197–e205. [DOI] [PubMed] [Google Scholar]
- Saunders B (2014). Stigma, deviance and morality in young adults' accounts of inflammatory bowel disease. Sociology of Health and Illness 36, 1020–1036. [DOI] [PubMed] [Google Scholar]
- Scott KM, Bruffaerts R, Tsang A, Ormel J, Alonso J, Angermeyer MC, Benjet C, Bromet E, de Girolamo G, de Graaf R, Gasquet I, Gureje O, Haro JM, He Y, Kessler RC, Levinson D, Mneimneh ZN, Oakley Browne MA, Posada-Villa J, Stein DJ, Takeshima T, Von Korff M (2007). Depression-anxiety relationships with chronic physical conditions: results from the World mental health surveys. Journal of Affective Disorders 103, 113–120. [DOI] [PubMed] [Google Scholar]
- Scott KM, Von Korff M, Alonso J, Angermeyer MC, Bromet E, Fayyad J, de Girolamo G, Demyttenaere K, Gasquet I, Gureje O, Haro JM, He Y, Kessler RC, Levinson D, Medina Mora ME, Oakley Browne M, Ormel J, Posada-Villa J, Watanabe M, Williams D (2009). Mental-physical co-morbidity and its relationship with disability: results from the World mental health surveys. Psychological Medicine 39, 33–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott KM, Von Korff M, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, Haro JM, Lepine JP, Ormel J, Posada-Villa J, Tachimori H, Kessler RC (2011). Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Archives of General Psychiatry 68, 838–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidhom Y, Ben Djebara M, Hizem Y, Abdelkefi I, Kacem I, Gargouri A, Gouider R (2014). Bipolar disorder and multiple sclerosis: a case series. Behavioural Neurology 2014, 536503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobel ME (1982). Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology 13, 290–312. [Google Scholar]
- Statistics Canada (2013). Canadian Community Health Survey (CCHS) – Mental Health. User Guide: Microdata Files. Statistics Canada: Ottawa. [Google Scholar]
- Stegmann ME, Ormel J, de Graaf R, Haro JM, de Girolamo G, Demyttenaere K, Kovess V, Matschinger H, Vilagut G, Alonso J, Burger H, Investigators EM (2010). Functional disability as an explanation of the associations between chronic physical conditions and 12-month major depressive episode. Journal of Affective Disorder 124, 38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szigethy EM, Youk AO, Benhayon D, Fairclough DL, Newara MC, Kirshner MA, Bujoreanu SI, Mrakotsky C, Bousvaros A, Srinath AI, Keljo DJ, Kupfer DJ, DeMaso DR (2014). Depression subtypes in pediatric inflammatory bowel disease. Journal of Pediatric Gastroenterology and Nutrition 58, 574–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tunks ER, Crook J, Weir R (2008). Epidemiology of chronic pain with psychological comorbidity: prevalence, risk, course, and prognosis. Canadian Journal of Psychiatry 53, 224–34. [DOI] [PubMed] [Google Scholar]
- Üstün TB, Chatterrji S, Kostanjsek N, Rehm J, Kennedy C, Epping-Jordan J, Saxena S, von Korff M, Pull C (2010a). Developing the World Health Organization disability assessment Schedule 2.0. Bulletin of the World Health Organization 88, 815–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Üstün TB, Kostanjsek N, Chatterji S, Rehm J (2010b). Measuring Health and Disability: Manual for WHO Disability Assessment Schedule: WHODAS 2.0. World Health Organization: Geneva. [Google Scholar]
- Van Brakel WH (2006). Measuring health-related stigma – a literature review. Psychology, Health and Medicine 11, 307–34. [DOI] [PubMed] [Google Scholar]
- Weare K, Nind M (2011). Mental health promotion and problem prevention in schools: what does the evidence say? Health Promotion Internation 26 (Suppl 1), i29–i69. [DOI] [PubMed] [Google Scholar]
- Word Health Organization (WHO) (2010). International Statisical Classification of Diseases and Related Health Problems. Retrieved 20 April 2015 from http://apps.who.int/classifications/icd10/browse/2010/en
- Wotton CJ, Goldacre MJ (2014). Record-linkage studies of the coexistence of epilepsy and bipolar disorder. Social Psychiatry and Psychiatric Epidemiology 49, 1483–1488. [DOI] [PubMed] [Google Scholar]
- Zhang XP, Norris SL, Gregg EW, Cheng YLJ, Beckles G, Kahn HS (2005). Depressive symptoms and mortality among persons with and without diabetes. American Journal of Epidemiology 161, 652–660. [DOI] [PubMed] [Google Scholar]