Abstract
Aims.
To identify distinct trajectories of depression experienced by a population-based sample of women over a 27-year period and to assess the validity of the derived trajectories.
Method.
The Mater University of Queensland Study of Pregnancy is a birth cohort study which commenced in 1981. Women (N = 6753) were interviewed at their first clinic visit, at 6 months, then 5, 14, 21 and 27 years after the birth of their child, using the Delusions Symptoms – States Inventory. Some 3561 (52.7%) women were followed up at 27 years, with 3337 (49.4%) of the sample completing the Composite International Diagnostic Interview (CIDI). Depression trajectories over a 27-year period were identified using Latent Class Growth Modelling (LCGM). LCGM was used to identify respondents with similar patterns of depression over a 27-year period. At the 27-year follow-up women who completed the CIDI, were stratified according to their trajectory group membership.
Results.
Three trajectory groups, each with different life-course patterns of depression were identified. The low/no symptoms of depression trajectory group comprised 48.4% of women. The mid-depression group (41.7%) had a consistent pattern of occasional symptoms of depression. The high/escalating trajectory group comprised 9.9% of the women in the study. We then examined each trajectory group based on their completion of the CIDI at the 27-year follow-up. Using the CIDI, 27.0% of women in the study had met the DSM-IV criteria for lifetime ever depression by their mean age of 46.5 years. The responses to the CIDI differed greatly for each of the trajectory groups, suggesting that the trajectories validly reflect different life histories of depression. The high/escalating trajectory group had an earlier age of first onset, more frequent episodes, longer duration of each episode of depression and experienced higher levels of impairment for their episodes of depression. For the high symptoms trajectory group, clinically significant depression is estimated to be experienced by women almost one in every 6 days of their life.
Conclusion.
While symptoms of depression are commonly experienced in a large community-based sample of women, a minority of women experience many episodes of depression in their lifetime. It is this group of women who are most impaired and should be of most concern, and who should be the main target of prevention and treatment initiatives.
Key words: Depression, population survey, prospective study, women
Introduction
Population-based studies have stimulated a renewed interest in the natural history of a number of mental illnesses, including depression. Such fundamental questions as the age of first onset of depression, patterns of recovery and recurrence, duration and number of episodes of depression over a lifetime have been described, but only in a few studies and with limited detail. While the available studies are consistent in identifying varying patterns of depression in population-based samples, previous studies have not addressed the question of whether there are different natural histories of depression in subgroups of the population.
Trajectories of depression
A trajectory is broadly equivalent to a life course – that is a pattern of health or behaviour which is exhibited over a lifetime. One approach to studying trajectories involves describing the pattern of health or behaviour for a sample over a defined period of time. This may also involve variations in trajectories by such sociodemographic and other variables as age and exposures to salient events (e.g., having a child, marital breakdown). For example, Beard et al's (2008) review suggests that age of first onset of depression is usually in early adulthood; that episodes of depression after early adulthood are usually recurrences following an earlier onset, and that rates of depression peak in later adulthood (Beard et al. 2008 reinforced by Sutin et al. 2013).
Another way the term trajectory is used (consistent with the intent of this paper) is in the context of subtypes of health and/or behaviour. Only a small number of studies have addressed the possibility that there may be population subgroups with different natural histories of depression (Stoolmiller et al. 2005; Nandi et al. 2009; Luoma et al. 2015). Luoma et al. (2015) have identified six previous studies which have described subgroups or trajectories of depression experienced by women following the birth of a child. These studies all involve longitudinal designs with a single (but across studies, generally, different) measure of depression. They have follow-up periods which vary from 2 to almost 17 years and they identify four, five or six different trajectories of depression (Luoma et al. 2015). These studies tend to have relatively small sample sizes and they use symptom checklists to determine trajectory group membership. We have been unable to locate any previous studies which have sought to validate trajectory group membership using independently derived diagnostic measures of depression.
Natural history of depression
Population and clinic-based studies are consistent in suggesting that depression is a chronic-intermittent condition with both recovery and recurrence being very common (Kessler & Wang, 2009). One ten-country international comparative study (Andrade et al. 2003), using the Composite International Diagnostic Interview (CIDI) to screen population samples, finds a lifetime prevalence of depression which varies from 3% in Japan to almost 17% in the USA. Estimates of the percentage of the population experiencing lifetime ever depression do vary greatly, but generally tend to be in the range of 6–25%, depending upon the sample selected and measures used (Kessler & Wang, 2009). Kessler et al. (2003), using data from the National Comorbidity Survey Replication, find a lifetime prevalence of 16.2% for major depressive disorder, with about half (of previous 12 months cases) rated as severe or very severe.
Up to 90% or more of those with a prior history of major depression have been found to experience recurrences over their life course (Kessler et al. 1994; Kessler & Wang, 2009). In a 15-year study of those in treatment for depression some 85% had a recurrence (Mueller et al. 1999), with a 40% probability of recurrence in the first year (Solomon et al. 2000). Based upon population surveys in Australia and the Netherlands, it has been estimated that males with depression experience 6.8–8.0, and females 7.7–12.8 episodes of major depression over their lifetime (Kruijshaar et al. 2005). A majority of those who have ever experienced depression recover within some months of depression onset, although there is evidence of a highly skewed distribution with a small minority still affected 6–12 months later. Vos et al. (2004), using data from four population surveys, found mean time to recovery of 8–12 weeks with 3–11% of cases still not recovered at the end of the first year (Vos et al. 2004). This indicates that although most persons with depression recover, there exists a smaller subgroup in the population who experience more persistent depression.
While depression may be common, there is less information about subgroups of depression in population samples. The available data suggest that some persons may rarely experience depression while others may frequently experience depressed mood and have many repeated episodes of depression. Little is known about these groups and their characteristics. This paper examines the types of trajectories of depression experienced by a large, population-based sample of women who were recruited early in pregnancy and followed for 27 years after the birth of their child.
Hypotheses
-
1.
Over a 27-year period, respondents will exhibit a stable, consistent and characteristic pattern of symptoms of depression.
-
2.
Most women occasionally experience symptoms of depression, but a majority of women never experience sufficient symptoms of depression to meet the relevant clinical criteria.
-
3.
A small proportion of women experience multiple symptoms of depression over an extended period of their lifetime. These women experience many episodes of depression over their lifetime.
Methods
Sampling
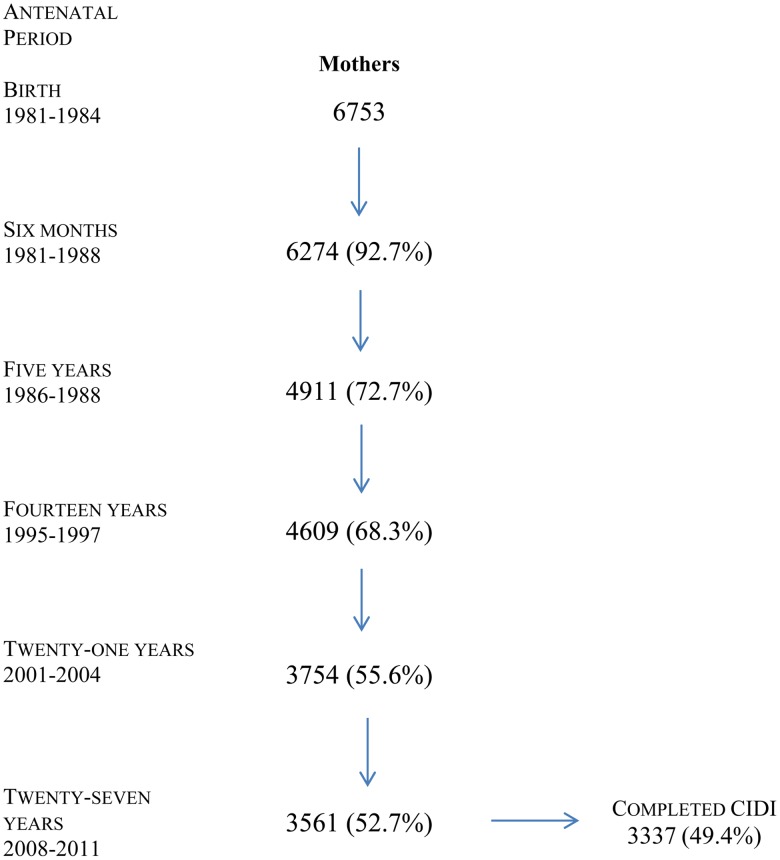
The Mater University Study of Pregnancy (MUSP; wider information about the MUSP study can be found at http://www.socialscience.uq.edu.au/musp) and its outcomes is a prospective birth cohort study which commenced with the recruitment of 6753 women early in their pregnancy. The Mater Hospital, at the time of recruitment, was the main provider of obstetrical services to women living on the south side of the Brisbane River. About half the births in Brisbane occurred at this hospital. Only public patients (about 50% of pregnant women at the hospital) were recruited to the study. Public patients in Australia are generally skewed to the middle to lower income groups. Recruitment was of all consecutive, public patients over the period 1981–1983 with 98.9% of pregnant women who were invited to participate in the study, accepting the invitation (Najman et al. 2005). Further follow-ups were at 6 months, and then 5, 14, 21 and 27 years after the birth (Najman et al. 2014). At the 27-year follow-up 3561 women (52.7% of the original sample) remained in the study. Figure 1 provides the details of sample retention over the 27-year period.
Fig. 1.
Flowchart – % retained in study at each phase of data collection.
Measurement of depression
Two measures of depression were available in this study. The Delusions Symptoms – States Inventory (DSSI) was developed by clinicians, and initially validated on its ability to discriminate between clinical and ‘healthy’ samples (Bedford et al. 1976; Bedford & Foulds, 1977). We administered the seven-item depression subscale at each phase of the study (mean Cronbach alpha = 0.83 over six administrations). We have compared scores on the DSSI depression subscale with the Hospital Anxiety and Depression Scale (HADS) and the Edinburgh Postnatal Depression Scale (EPDS). The mean correlation between the three scales was 0.73 (Najman et al. 2000), roughly equivalent to differences in the clinical assessment of the same patients. For the DSSI depression subscale a symptom was ‘counted’ if the respondent stated she had recently experienced that symptom some of the time, most of the time or all of the time. Respondents could score in the range of 0–7 reflecting the number of symptoms of depression they report experiencing. There is no clear criterion for caseness in this study that corresponds directly to the scoring system used by Bedford et al. (1976). In Appendix A, we have provided a table showing the association between DSSI scores and CIDI diagnoses of depression at the 27-year follow-up. About 50% of those with a DSSI score of 3–4 symptoms meet DSM-IV clinical criteria for depression. The seven depression questions were repeated at each phase of data collection. Trajectories are derived from 6 measures of DSSI depression collected over a 27-year period (first clinical visit at a mean 18 weeks gestation, and 6, 5, 14, 21 and 27 years after the birth of the child).
At the 27-year follow-up, respondents were also administered the CIDI (Kessler & Ustun, 2004). For this paper, we present the results relating to the lifetime ever CIDI (DSM-IV) diagnosis of major depression, as well as details of the number and duration of lifetime episodes of depression meeting the DSM-IV clinical criteria. The CIDI also incorporates a measure of functional impairment associated with depression (Sheehan et al. 1996). The Sheehan Disability Scale (SDS) has very good internal consistency and demonstrates good validity (Arbuckle et al. 2009). The SDS is sensitive to changes in functional impairment over time.
We have also used five measures of the mothers’ sociodemographic characteristics to identify predictors of the depression trajectories. These five are all obtained at the time the mother was recruited to the study; that is the first clinic (obstetrical) visit (FCV). Maternal age is in years at the time of recruitment. Maternal education is the highest level attained. Marital status is self-reported at FCV, as is family income. Parity is taken from the mother's obstetrical history.
Statistical analyses
This paper examines trajectories of maternal depression over the reproductive life course and beyond. Using correlation procedures it is evident that maternal depression scores at one phase of data collection are significantly correlated with depression scores at other phases of data collection. There is persistence in depression scores over the 27 years of follow-up. We have chosen to use the method of Latent Class Growth Modelling to identify typical maternal depression trajectories over the 27 years of follow-up (Nagin, 1999).
Nagin & Tremblay (2005), discussing trajectory analysis note that this is, primarily, a method for reducing complexity when assessing patterns of individual data over time. Individuals do not strictly ‘belong’ to a group; rather groups are created according to the pattern or type of behaviour or mood individuals exhibit over time. In this sense, trajectory analysis is a method of smoothing out individual differences. Thus, the groups are based on an estimate of the probability that the individuals they contain are similar in their scores over the time period involved. It is important to acknowledge that some individuals in a group may exhibit variations from their group in the short term, but over the long term their characteristics are similar to other members of the group.
Data analyses, initially, involved the identification of subgroups of women who have similar depression trajectories over 27 years following the birth of their baby. Developmental trajectories of depression were identified. Semi-parametric mixture models (Lynch et al. 1999; Nagin, 1999) for depression symptoms over a 27-year period were estimated by applying the SAS TRAJ procedure (Nagin, 1999; Jones et al. 2001).
Trajectories of depression symptoms were defined using two types of analysis. Competing models with different numbers of trajectories or trajectories of various shapes/patterns (linear, quadratic, cubic trends, etc.) were computed, and the Bayesian information criterion (BIC) was used to decide which model best fit the data. Depression symptoms can be considered a psychometric scale; consequently, the censored normal model distribution was applied.
The parameter coefficients, estimated by semi-parametric statistical technique, provide direct information concerning group membership probabilities. For every respondent, based on the observed longitudinal pattern of depressed symptoms, the probabilities of belonging to each trajectory group were calculated, and the assigned trajectory group membership using the highest classification probability across groups on a scale of 0–1 was determined. Probabilities of approximately 0.70, 0.80 or higher imply a good fit (Nagin, 2005). As a result, the posterior probabilities and the averaged group membership probabilities for each trajectory were examined to evaluate each model, and used to determine the trajectories of depression to be selected in this study. We have also included, in Appendix B, details of group membership, the BIC and the posterior probabilities for the two, three, four and five group (trajectories) solutions. Once trajectory groups had been identified we use analysis of variance to compare episodes of depression (based upon CIDI DSM-IV criteria); or chi-square tests where we assessed a categorical variable.
Results
Trajectories of depression
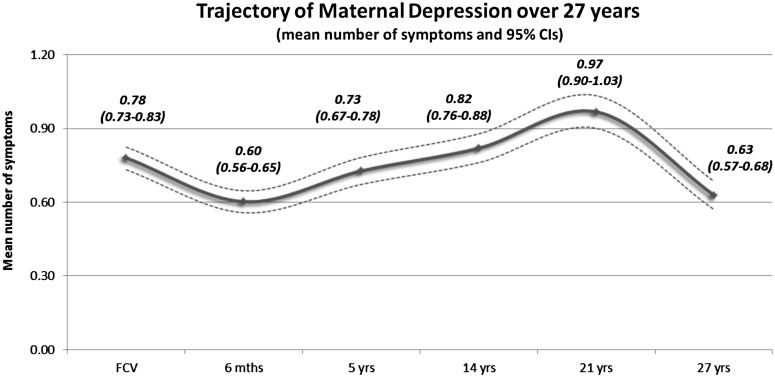
Figure 2 presents details of the mean number of symptoms experienced by respondents at each follow-up. The maternal trajectory of symptoms of depression is that there is a slight decline in symptom burden after the birth of the baby, and then a steady increase until 21 years followed by a decline at the 27-year follow-up.
Fig. 2.
Trajectory of maternal depression over 27 years (mean number of symptoms and 95% CI).
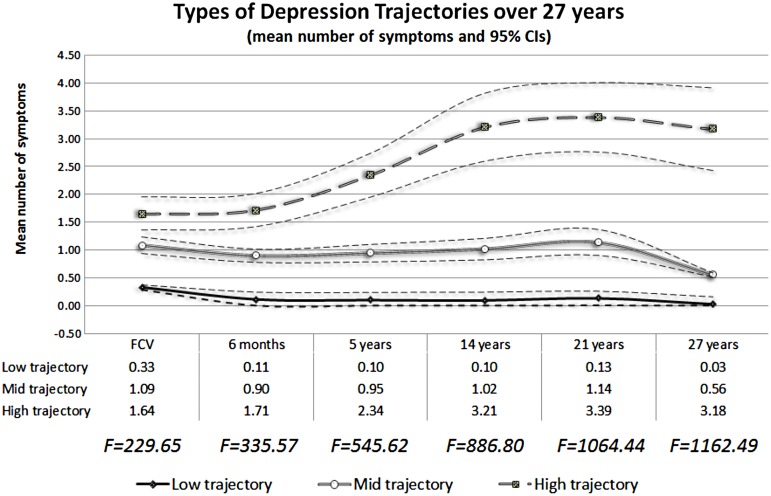
Using trajectory analysis (Nagin, 2005) we have identified three distinct depression trajectories experienced by women over a 27-year period following the birth of their child (Fig. 3). The decision to have three trajectories was based on goodness of fit, parameters of the trajectory modelling and statistically significant results. These were low/no, mid/moderate and high depression trajectories. Figure 3 presents the depression trajectories over the 27-year period from the index pregnancy.
Fig. 3.
Types of depression trajectories over 27 years (mean number of symptoms and 95% CI).
The three trajectory groups differ in their mean number of symptoms at recruitment and these differences in means appear to increase at subsequent follow-up. The low/no depression trajectory group comprise some 48.4% of women in the sample, and characteristically have very few if any symptoms of depression at the time of recruitment (FCV). This remains the case over each data collection and for 27 years. The mid-trajectory group is comprised 41.7% of the sample and these entered the study with a mean of about one symptom. For the mid-depression trajectory group there is little change in the mean number of symptoms of depression over the 27 years following the birth of a child, with the exception of a decline in the average number of symptoms from the 21–27-year follow-ups. The high depression symptoms trajectory group comprised 9.9% of the sample. The high trajectory group has the highest mean number of symptoms prior to the birth and appears to experience an increasing mean number of symptoms of depression from the period shortly after the birth of the study child to the 14-year follow-up, and plateaus thereafter. For the high depression trajectory group average symptoms at the 21-year follow-up are about twice as high as they were at the FCV, with a mean of over three DSSI symptoms experienced by each participant at the 14-year follow-up and thereafter.
Table 1 provides details of predictors of the three depression trajectories. Younger women tended to be disproportionately in the high symptoms trajectory group, as did women who were not married (at FCV). Women in low-income families were also more likely to be in the high symptoms trajectory group, while women with no previous children were less likely to be in the high depression trajectory group (adjusted analysis).
Table 1.
Sociodemographic predictors of trajectory group membership
| OR and CI by trajectory group membership | |||||||
|---|---|---|---|---|---|---|---|
| Unadjusted models | Adjusted models* | ||||||
| Sociodemographics at FCV | Low | Mid | High | Mid | High | ||
| Maternal age | 13–19 | 1 | 2.63 (1.61, 4.30) | 2.89 (1.31, 6.38) | 2.22 (1.30, 3.79) | 2.57 (1.07, 6.15) | |
| 20–35 | 1 | 1.38 (0.89, 2.11) | 1.20 (0.58, 2.46) | 1.44 (0.93, 2.24) | 1.33 (0.63, 2.84) | ||
| 35+ | 1 | 1 | 1 | ||||
| Maternal education | Incomplete high | 1 | 1.22 (0.99,1.50) | 1.37 (0.96, 1.95) | 1.14 (0.93, 1.41) | 1.18 (0.82, 1.69) | |
| Complete high | 1 | 1.13 (0.81, 1.56) | 1.24 (0.71, 2.16) | 1.05 (0.75, 1.46) | 1.16 (0.66, 2.05) | ||
| Post high | 1 | 1 | 1 | ||||
| Marital status | Single/Sep-div-wid | 1 | 2.18 (1.59, 2.99) | 2.83 (1.82, 4.40) | 1.64 (1.16, 2.32) | 1.90 (1.16, 3.11) | |
| Married-liv-together | 1 | 1 | 1 | ||||
| Family income | $10 399 or less | 1 | 1.64 (1.34, 1.99) | 2.66 (1.97, 3.59) | 1.43 (1.17, 1.75) | 2.25 (1.65, 3.06) | |
| $10 400 or more | 1 | 1 | 1 | ||||
| Parity | No children previously | 1 | 1.06 (0.89, 1.25) | 0.93 (0.71, 1.24) | 0.91 (0.76, 1.08) | 0.73 (0.53, 0.99) | |
| One or more kids | 1 | 1 | 1 | ||||
Adjusted for the other sociodemographic variables in the table.
In Table 2, we have examined the CIDI (DSM-IV) diagnostic outcomes for each of the three DSSI 27-year depression trajectories. Diagnostic details involve respondents’ retrospective recall of DSM-IV symptoms of depression based upon the administration of the CIDI to mothers at the 27-year follow-up. Overall, by their mean age of 46.5 years, some 27% of women in this study had met the criteria for a lifetime ever diagnosis of depression.
Table 2.
Association between maternal 27-year DSSI trajectories and CIDI diagnostic assessments at 27-year follow-up (N = 3501)
| CIDI – 27YR diagnostic details | Low trajectory (48%) | Mid trajectory (42%) | High trajectory (10%) | |
|---|---|---|---|---|
| Lifetime ever major depression (N) | 16.7% (1127) | 32.4% (978) | 53.5% (228) |
χ2 = 157.15 p < 0.001 |
| Mean lifetime number episodes (s.d.) | 2.56 (4.79) | 3.74 (6.12) | 8.07 (16.15) |
F = 7.613 p < 0.001 |
| Mean age at first episode years (s.d.) | 30.05 (11.29) | 26.38 (11.94) | 23.91 (11.02) |
F = 4.598 p = 0.011 |
| Mean duration of first episode weeks (s.d.) | 36.29 (72.26) | 36.07 (58.25) | 61.19 (108.71) |
F = 2.463 p = 0.087 |
| Mean time between epi 1 and 2 weeks (s.d.) | 515.52 (566.79) | 398.71 (389.71) | 347.32 (299.17) |
F = 3.443 p = 0.033 |
| Mean number of years of life affected by depression years (s.d.) | 11.87 (12.88) | 9.45 (8.91) | 18.87 (15.34) |
F = 8.811 p < 0.001 |
| Level of impairment (20% most impaired) attributed to depression last 12 months (N) | 0% (10) | 14.3% (84) | 25.7% (70) |
χ2 = 5.72 p = 0.057 |
| Per cent of lifetime meeting DSM-IV criteria for depression (s.d.)* | 3.73 (0.071) | 5.73 (0.098) | 16.62 (0.363) | |
| Significance of difference between trajectory group means | Low v. mid t = 1.45, p = 0.149 |
Mid v. high t = 3.30 p = 0.001 |
High v. low t = 2.74 p = 0.007 |
Per cent of lifetime depressed is calculated by multiplying the number of CIDI (DSM-IV) diagnoses of depression by the duration of the first episode (data on duration of subsequent episodes is not always available) and then dividing by the age (in weeks) of each individual respondent. A small number of outliers (impossible scores) have been removed from the calculations.
The low depression trajectory group is not entirely free of CIDI-based DSM-IV diagnoses of depression, with 16.7% of mothers having a lifetime ever diagnosis. By contrast the majority of mothers (53.5%) in the high DSSI depression trajectory have met the criteria for a lifetime ever DSM-IV diagnosis of depression.
For lifetime ever number of episodes of depression, the high trajectory group averages over eight episodes. Those in the high symptoms trajectory group who met the criteria for major depression had a younger age of first onset of depression, and experienced a much longer duration of first episode of depression, as well as a shorter duration of time between episodes. Using data based upon the mean age of mothers and the mean number and duration of episodes of depression experienced by each of the three DSSI trajectory groups, it is possible to estimate the percentage of the lifetime of a mother during which she had experienced depression. The low trajectory group met the DSM-IV criteria for depression for 3.73% of their lifetime (based upon 2.56 episodes per person and a mean of 36.29 weeks per episode). The mid-DSSI trajectory group experience DSM-IV depression for 5.73% of their lifetime. By contrast the high trajectory group have experienced DSM-IV depression for 16.62% of their lifetime. Using four items to create a composite SDS score, the level of impairment experienced by the high trajectory group for a selected episode of depression is greater than the level of impairment experienced by the other depression trajectory groups.
Discussion
Following the birth of a child we have identified three maternal depression trajectory groups over a 27-year period. While Fig. 1 suggests a 21-year period of increase in symptoms of depression following the birth of a baby; it is notable that none of three trajectory groups present a pattern which is similar to the overall (aggregate) pattern. About half the sample of women (48.4%) manifested few or no symptoms of depression at every stage of follow-up. Another large group (41.7%) had an average of about one symptom of depression at each phase of data collection. Both these trajectories could be argued to reflect persistent and stable characteristics of the mothers in this study, with stability extending over a 27-year period. A third group of women, comprising 9.9% of our sample experience much higher levels of depression, (initially an average of about 1.5 symptoms) with an escalating depression trajectory, with the mean number of symptoms increasing to over three by 14 years after the birth of their child.
Based upon the CIDI DSM-IV diagnostic criteria, 27% of women in this study had ever (lifetime) experienced a depression. This is above the estimates provided by Andrade et al. (2003) and Kessler & Wang (2009), but slightly below the estimate provided by Andrews et al. (2005) and Angst et al. (2015) for population samples. Moffitt et al. (2010) note that prospectively collected data tend to yield lifetime prevalence estimates that are substantially higher than those derived from recall of past episodes using the CIDI or similar measures. If Moffitt is correct then our estimates of lifetime experiences of DSM-IV depression are, at best, conservative. Our finding add to the literature by identifying a small subgroup of women who disproportionately experience many repeated episodes of depression, as well as another subgroup who repeatedly experience occasional symptoms of depression.
Our study provides evidence relevant to concerns about the impact of depression in the postnatal period, and to the vulnerability of a small proportion of women to high levels of depression over their life course. Those with the highest level of depression postnatally, were those with the highest level of antenatal depression. We see no evidence of an increase in depression levels in the period immediately following the birth of a child. We do, however, observe increasing levels of depression for women in the high trajectory group which coincides with the child reaching adolescence. Our data suggest that there exists a substantial minority of mothers who are depressed for long periods of time during which they are engaged in childrearing.
Using lifetime recall data only a small minority of the low/no trajectory group had experienced a DSM-IV depression disorder. By contrast over half the women in the high trajectory group had met criteria for depression. The three trajectory groups differ greatly in their experiences of depression; the mean number of episodes they experience, their age of first episode, the duration of their first episode, the time between episodes, the number of life years affected by depression and the level of impairment associated with their depression.
It is possible to estimate the overall percentage of a lifetime each person in a trajectory group, was depressed. Consistent with the very high burden of disease attributable to depression (Whiteford et al. 2013), one in every 6 days of the life of those in the high trajectory group is estimated to involve living with a depression which meets the DSM-IV clinical criteria.
Data from the CIDI administered at the 27-year follow-up suggest the validity of the long-term trajectories based upon the seven item DSSI. The extent of depression in the high trajectory group must be of concern, particularly as this group comprised about one in ten women in this population sample. From a research perspective the findings are important in suggesting that for a subsample of women in the study, multiple symptoms of depression experienced at any point in time, is associated with experiences of multiple symptoms of depression at other time points.
Our findings also suggest that studies which focus on the consequences of depression experienced either antenatally or postnatally, as a critical period, may be misleading given the chronic recurring nature of depression, particularly for the high depression trajectory group. For example, evidence that postnatal depression leads to adverse child health outcomes might equally be explained by recurrent episodes of depression occurring in early childhood or the adolescent period.
Why is it that 9.9% of women in this study experience such persistently high levels of depression over such a substantial period of their lives? Reviews of gene–environment interaction studies suggest that individuals may exhibit variable levels of vulnerability to external experiences (Belsky & Hartman, 2014). Women in the high trajectory group were more often teenage mothers, not married and of low income. It may be that these women consistently experience higher levels of adversity over their life course. It may also be the case that this study has identified a group of women characterised by a depressive phenotype. There is consistent evidence that mental illnesses (including depression and anxiety) have a substantial genetic basis (Caspi et al. 2003; Heim & Binder, 2012) and genetic and/or epigenetic factors may account for the appearance of a phenotype of women who experience more frequent and longer episodes of depression. While we are only able to speculate about the factors which may precipitate depression, it is clear that this sample of women experience chronic and persistent symptoms and episodes of depressed mood.
Limitations
In interpreting these findings some important limitations are noted. Firstly, the study involves substantial loss to follow-up over a 27-year period. Of 6753 mothers recruited to the study some 3561 (52.7%) were available at the latest follow-up. At this follow-up not all mothers completed the CIDI (N = 2550 available in this cohort). Concerns about bias in loss to follow-up are partly based on the repeated observation (in this study as well as others) that the most economically disadvantaged, those with the worst mental health, and the highest risk lifestyles (smoking, alcohol and illicit substance use) are disproportionally lost to follow-up. In Appendix C, we report loss to follow-up by DSSI depression at the time of recruitment. As a consequence of this biased loss to follow-up it is likely that this study may underestimate the per cent of women who manifest persistent and higher symptom levels over a 27-year period. Biased loss to follow-up would not alter the main findings of the study, namely that almost half the women in this study rarely or never experience depression, while a minority experience much more frequent and more severe symptoms over a much longer component of their life course.
Secondly, it is notable that the number of trajectories identified will be partly determined by the parameters set by the researcher. We have decided to identify broad trajectory groups. It is possible to further subdivide trajectories into a larger number of more homogeneous categories, but this would have little impact on our finding that a large proportion of women rarely experience symptoms of depression while a smaller proportion experience increasing symptoms over an extended period of their reproductive life course.
Thirdly, we have tested the stability of our model by adjusting for age differences at each follow-up. One could suggest that the changes we report reflect the ageing of women in our study rather than their course stage. After adjusting for age we find the three trajectories remain effectively the same, as do the statistical criteria relating to the integrity of the trajectories.
We have estimated the lifetime exposure of different trajectory groups. These estimates are based on the assumption that each episode of depression is of equal duration. As there appears to be a modest decline in the duration of depression for those with many episodes, some ‘discount’ might be applied to the estimates, particularly for the high depression trajectory group. Such an adjustment would marginally reduce the lifetime duration of exposure to depression, particularly for those in the high depression trajectory group.
Conclusion
Women over a 27-year period exhibit a characteristic pattern of depression. Arguably, this pattern reflects a combination of environmental exposures and the level of genetic vulnerability. A great deal more attention should be paid to the social and behavioural consequences of depression for those women in the high symptoms of depression trajectory. For the 9.9% of respondents in the high trajectory group, a substantial proportion of their lives were lived with depression and accompanied by a high level of impairment. If symptoms and diagnoses of depression are common in a population sample, then it may be unrealistic to provide services which address all instances of depression. There may be a need to target the subgroup of the population who exhibit the highest level of impairment and for whom the outcomes of depressed mood are likely to be most severe. There is now some evidence that a range of therapies are able to reduce the duration of depression and the risk of relapse (Vos et al. 2004; Biesheuvel-Leliefeld et al. 2015). This study demonstrates the heterogeneous trajectories of depression in a population sample and suggests the urgent need to target effective interventions for the minority who are most affected by recurrent and persistent episodes of depression.
Acknowledgements
Our thanks to the thousands of parents and children who participated in this study, to Shelby Marrington who has managed the data collection and to Greg Shuttlewood who is responsible for the data management.
Financial support
This study is supported by funding from the National Health and Medical Research Council, Australia and supplementary funding from the Australian Research Council. There has been no commercial or related funding for this project. The funding sources had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of interest
None.
Ethical standards
This study has received approval from the Human Research Ethics Committee and the University of Queensland. The study meets relevant National Health and Medical Research Council ethical requirements.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796015001109.
click here to view supplementary material
References
- Andrade L, Caraveo-Anduaga JJ, Berglund P, Bijl RV, De Graaf R, Vollebergh W, Dragomirecka E, Kohn R, Keller M, Kessler RC, Kawakami N, Kilic C, Offord D, Ustun TB, Vicente B, Wittchen HU (2003). The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. International Journal of Methods in Psychiatric Research 12, 3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G, Poulton R, Skoog I (2005). Lifetime risk of depression: restricted to a minority or waiting for most? British Journal of Psychiatry 187, 495–496. [DOI] [PubMed] [Google Scholar]
- Angst J, Paksarian D, Cui L, Merikangas KR, Hengartner MP, Ajdacic-Gross V, Rössler W (2015). The epidemiology of common mental disorders from age 20 to 50: results from the prospective Zurich cohort Study. Epidemiology and Psychiatric Sciences, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbuckle R, Frye MA, Brecher M, Paulsson B, Rajagopalan K, Palmer S, Degl'Innocenti A (2009). The psychometric validation of the Sheehan Disability Scale (SDS) in patients with bipolar disorder. Psychiatry Research 165, 163–174. [DOI] [PubMed] [Google Scholar]
- Beard JR, Galea S, Vlahov D (2008). Longitudinal population-based studies of affective disorders: where to from here? BMC Psychiatry 8, 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedford A, Foulds GA (1977). Validation of the delusions symptoms states inventory. British Journal of Medical Psychology 50, 163–171. [Google Scholar]
- Bedford A, Foulds GA, Sheffield BF (1976). A new personal disturbance scale (DSSI/sAD). British Journal of Social and Clinical Psychology 15, 387–394. [DOI] [PubMed] [Google Scholar]
- Belsky J, Hartman S (2014). Gene-environment interaction in evolutionary perspective: differential susceptibility to environmental influences. World Psychiatry 13, 87–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biesheuvel-Leliefeld KEM, Hollon SD, van Marwijk HWJ, Cuijpers P, Bockting CLH, Kok GD, Smit F (2015). Effectiveness of phsychological interventions in preventing recurrence of depressive disorder: meta- anlysis and meta-regression. Journal of Affective Disorders 174, 400–410. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R (2003). Influence of life stress on depression: moderation by a polymorphism in the 5-HTT Gene. Science 301, 386–389. [DOI] [PubMed] [Google Scholar]
- Heim C, Binder EB (2012). Current research trends in early life stress and depression: review of human studies on sensitive periods, gene–environment interactions, and epigenetics. Experimental Neurology 233, 102–111. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS, Roeder K (2001). A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods and Research 29, 374–393. [Google Scholar]
- Kessler RC, Ustun TB (2004). The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). International Journal of Methods in Psychiatric Research 13, 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Wang PS (2009). Epidemiology of depression In Handbook of Depression (ed. Gotlib IH and Hammen CL), pp. 5–22. Guilford Press: New York. [Google Scholar]
- Kessler RC, Kendler KS, Wittchen HU, Hughes M, Eshleman S, Zhao S, McGonagle KA, Nelson CB (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51, 8–9. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Walters EE, Rush AJ, Demler O, Merikangas KR, Jin R, Wang PS, Berglund P, Koretz D (2003). The epidemiology of major depressive disorder. Journal of the American Medical Association 289, 3095–3105. [DOI] [PubMed] [Google Scholar]
- Kruijshaar ME, Barendregt J, Vos T, De Graff R, Spijker J, Andrews G (2005). Lifetime prevalence estimates of major depression: an indirect estimation method and a quantification of recall bias. European Journal of Epidemiology 20, 103–111. [DOI] [PubMed] [Google Scholar]
- Luoma I, Korhonen M, Salmelin RK, Helminen M, Tamminen T (2015). Long-term trajectories of maternal depressive symptoms and their antenatal predictors. Journal of Affective Disorders 170, 30–38. [DOI] [PubMed] [Google Scholar]
- Lynch K, Roeder K, Nagin D (1999). Modeling uncertainty in latent class membership: a case study in criminology. Journal of the American Statistical Association 94, 766–776. [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R (2010). How common are the common mental disorders? Psychological Medicine 40, 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller TI, Leon AC, Keller MB, Solomon DA, Endicott J, Coryell W, Warshaw M, Maser JD (1999). Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. American Journal of Psychiatry 156, 1000–1006. [DOI] [PubMed] [Google Scholar]
- Nagin D (1999). Analyzing developmental trajectories: a semiparametric, group-based approach. Psychological Methods 4, 139–157. [DOI] [PubMed] [Google Scholar]
- Nagin D (2005). Group-based Modeling of Development. Harvard University Press: Cambridge. [Google Scholar]
- Nagin D, Tremblay RS (2005). Developmental trajectory groups: fact or a useful statistical fiction? Criminology 43, 873–918. [Google Scholar]
- Najman JM, Anderson MJ, Bor W, O'Callaghan MJ, Williams GM (2000). Postnatal depression – myth and reality: maternal depression before and after the birth of a child. Social Psychiatry and Psychiatric Epidemiology 35, 19–27. [DOI] [PubMed] [Google Scholar]
- Najman JM, Bor W, O'Callaghan M, Williams GM, Aird R, Shuttlewood G (2005). Cohort profile: the Mater-University of Queensland Study of Pregnancy (MUSP). International Journal of Epidemiology 34, 992–997. [DOI] [PubMed] [Google Scholar]
- Najman JM, Khatun M, Mamun A, Clavarino A, Williams GM, Scott J, O'Callaghan M, Hayatbakhsh R, Alati R (2014). Does depression experienced by mothers lead to a decline in marital quality: a 21-year longitudinal study. Social Psychiatry and Psychiatric Epidemiology 49, 121–132. [DOI] [PubMed] [Google Scholar]
- Nandi A, Beard JR, Galea S (2009). Epidemiologic heterogeneity of common mood and anxiety disorders over the lifecourse in the general population: a systematic review. BMC Psychiatry 9, 31–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Harnett-Sheehan K, Raj BA (1996). The measurement of disability. International Clinical Psychopharmacology 11, 89–95. [DOI] [PubMed] [Google Scholar]
- Solomon DA, Keller MB, Leon AC, Mueller TI, Lavori PW, Shea MT, Coryell W, Warshaw M, Turvey C, Maser JD, Endicott J (2000). Multiple recurrences of major depressive disorder. American Journal of Psychiatry 157, 229–233. [DOI] [PubMed] [Google Scholar]
- Stoolmiller M, Kim HK, Capaldi DM (2005). The course of depressive symptoms in men from early adolescence to young adulthood: identifying latent trajectories and early predictors. Journal of Abnormal Psychology 114, 331–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Terracciano A, Milaneschi U, An Y, Ferrucci L, Zonderman AB (2013). The trajectory of depressive symptoms across the adult life span. Journal of the American Medical Association Psychiatry 70, 803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos T, Haby MM, Barendregt JJ, Kruijshaar M, Corry J, Andrews G (2004). The burden of major depression avoidable by longer-term treatment strategies. Archives of General Psychiatry 61, 1097–1103. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Harris MG, McKeon G, Baxter A, Pennell C, Barendregt JJ, Wang J (2013). Estimating remission from untreated major depression: a systematic review and meta-analysis. Psychological Medicine 43, 1569–1585. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796015001109.
click here to view supplementary material