Abstract
AIM
To determine whether ophthalmic photographers (OPs) can conduct virtual clinics (VCs) in medical retina appropriately and whether this increases clinic capacity.
METHODS
Three OPs underwent a training programme to learn how to assess and manage macular edema secondary to diabetes or retinal vein occlusion. The 300 consecutive patients over a 7-month observation period in 2018 were assessed in VCs by both OPs and medical retina consultants. The degree of agreement in treatment decisions between doctors and photographers, as well as adverse events, was recorded. The change in number of patients seen in VCs over two years was also measured.
RESULTS
There was 100% agreement in management decisions between doctors and photographers during the 300-patient observation period. No adverse events were recorded. In 2017, 572 patients were seen in VCs by doctors. After OP clinics were introduced in 2018, this number increased by 24% to 709 patients seen by both photographers and doctors. There was a significant increase in mean number of patients seen per month between 2017 (47.7±11.7) and 2018 (59.1±14.4; P=0.045, 95%CI -22.5 to -0.296).
CONCLUSION
OPs can manage certain medical retina patients in VCs appropriately and can increase clinic capacity significantly for particular conditions.
Keywords: virtual clinics, extended roles, macular edema
INTRODUCTION
Macular edema secondary to diabetes or retinal vein occlusion is a common cause of vision loss[1]–[2]. Diabetic retinopathy is one of the top five causes of sight impairment in the West, accounting for 4.06% of sight impairment in Western Europe[3]. Intravitreal anti-vascular endothelial growth factor agents (anti-VEGF) is an effective treatment for macular edema and have become the primary treatment modality[4]. It is now the most common intraocular procedure worldwide, with increasing numbers performed every year[4]. Patients undergoing treatment for macular edema require multiple hospital visits, putting considerable strain on resources and capacity[5]. Furthermore, the prevalence of this condition is projected to rise[2],[6].
Doctor shortages are set to compound the problem[7]–[8]. In the UK, a clear policy has been set to expand the roles of healthcare professionals, such as nurses, and optometrists to help plug the gap[9]. These new roles, along with virtual clinics (VCs), have been proposed as part of the solution for increasing service capacity and have proved successful[6],[10]–[15]. They may also improve job satisfaction by exposing staff to a wider variety of clinical experiences, including diagnosis and management of common retinal conditions[16].
In the UK, Leicester has a higher prevalence of diabetes compared to national data (8.9% vs 6.4%)[17]. In 2018, the Medical Retina Department at Leicester Royal Infirmary received 2211 new referrals and performed 8511 intravitreal injections. These often generate multiple follow up appointments. To meet rising service demands, we felt it was necessary to investigate extending the roles of our workforce.
OPs are often highly trained technicians who are exposed to a variety of retinal pathology through imaging. The purpose of this Quality Improvement Project was to explore an extended role for OPs in the management of patients under treatment for macular edema secondary to diabetes or retinal vein occlusions. We aimed to formally engage the senior members of the Ophthalmic Imaging Department in the decision making process, increase VC capacity and improve patient care by ensuring timely follow-ups for patients.
SUBJECTS AND METHODS
Ethical Approval
All patients attending VCs were informed that they would be assessed by either doctors or non-medical health care providers and gave informed consent. This project follows the principles outlined in the Declaration of Helsinki.
Our setup for VCs involves the selection of patients who have a stable diagnosis of diabetic retinopathy/retinal vein occlusion or who are undergoing intravitreal treatment for the aforementioned conditions. An initial patient visit is booked for visual acuity testing and optical coherence tomography (OCT) imaging. Subsequently, in the patient's absence, a doctor assesses their condition and makes a decision regarding management. Before 2018, all VCs were completed by medical retina consultants (MRCs).
Two MRCs and three senior OPs first conceptualized the idea of VCs conducted by OPs. A comprehensive policy document was produced by the MRCs detailing the proposal. This was submitted to the relevant heads of departments, and the Trust Audit/Quality Improvement Department. Formal approval as a quality improvement project was obtained before commencement. No patient identifiable data were collected.
A rigorous training regime for the OPs was developed. This included mandatory background reading of medical retina books and a specially developed OCT Interpretation Competency Booklet and participation in local teaching sessions. Weekly sessions discussing OCT findings, the rationale for decisions regarding treatment or monitoring, documentation in notes and clinical outcomes were facilitated. Moreover, treatment pathways were established to assist with decisions regarding treatment or monitoring. The OPs were then assessed by the MRCs according to preset criteria for competency (Table 1).
Table 1. Blank form used to assess criteria for competency.
| Competence category | Positive features | Opportunities for improvement | Performance level/score |
| Communication and working with the patient and/or family | Explanation of procedure to patient. | ||
| Ongoing reassurance of patient. | |||
| Explanation of main aspects of retinal condition and management options. | |||
| Safety | Checking patient identification in notes and computer database. | ||
| Procedural competence | Assess features of OCT. | Read relevant literature (book/online sources) | |
| Decide about appropriate management based on current and previous OCT images, visual acuity results and previous notes. | |||
| Record outcomes in the patients' notes. | |||
| Fill-in appropriate forms for treatment/clinic review. | |||
| Appropriately seek advice when in doubt. |
Once deemed competent, the OPs proceeded to an observation period covering 100 patients each from February 2018 until September 2018. These 100 patients were assessed by both the OPs and the MRCs and decisions regarding diagnosis and management were compared for agreement. The presence of adverse events was also checked. The OPs then proceeded to conduct VCs independently. Since 2018, VCs have been completed by OPs and MRCs. The 300 patients seen by OPs during the observation period were consecutive patients attending the VCs.
OP VCs were initially restricted to follow up patients who have been diagnosed with macular edema secondary to retinal vein occlusion or diabetes. They have since been extended to cover hydroxychloroquine retinopathy screening. Our primary outcomes were the percentage agreement in management decisions between OPs and MRCs during the 300-patient observation period and the number of adverse events observed. Our secondary outcomes were the total number of patients seen in VCs (MRCs and OPs) in 2018 as well as the mean number seen per month. These outcomes were compared with those from 2017 (before OP VCs). The statistical significance of the difference in mean patients/month seen between 2017 and 2018 was calculated using the t-test. Statistics were performed on Microsoft Excel and jamovi [The jamovi project (2019). jamovi (Version 0.9; Computer Software). Retrieved from https://www.jamovi.org]. As a method of ongoing quality control, after the 300-patient observation period, 10% of all patients seen by the OPs are randomly checked by the MRCs for safety and appropriateness of treatment decisions.
RESULTS
Table 2 details the characteristics of patients who were seen during the observation period, including gender, age, number of eyes, laterality and diagnosis. There was 100% agreement in management decisions between OPs and MRCs during this period and there were no adverse events noted.
Table 2. Patient characteristics during the observation period.
| Parameters | Values |
| Total patients (n) | 300 |
| Male | 155 (51.7) |
| Female | 145 (48.3) |
| Mean age (y) | 71 |
| No. of eyes (n) | 403 |
| Right | 204 (50.6) |
| Left | 199 (49.4) |
| Outcome | |
| Observed | 296 (73.4) |
| Treated | 107 (26.6) |
| Diagnosis | |
| BRVO | 129 (42.4) |
| CRVO | 63 (20.7) |
| DMO | 99 (32.6) |
| Other | 13 (4.3) |
BRVO: Branch retinal vein occlusion; CRVO: Central retinal vein occlusion; DMO: Diabetic macular edema.
n (%)
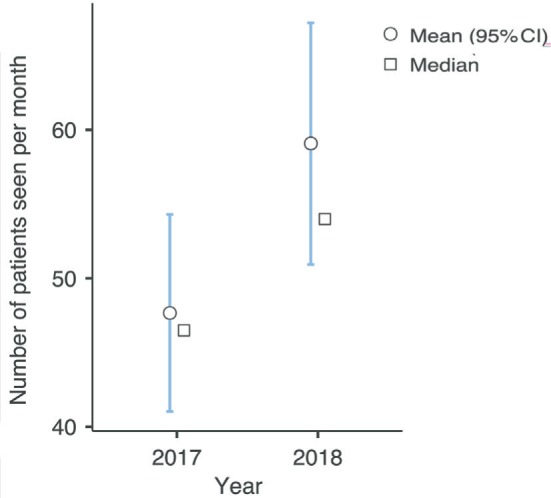
In 2017 (MRCs only) 572 patients were seen in VCs. In the following year (MRCs+OPs) 709 patients were seen in VCs. This represents a rise of 24% in capacity over 1y. Figure 1 details the breakdown per month of numbers of patients seen in 2017 and 2018. The mean number of patients seen per month in 2017 and 2018 were 47.7±11.7 and 59.1±14.4 respectively. The difference between these figures was statistically significant (P=0.045, 95%CI -22.5 to -0.296; Figure 2). Of note, the eventual rise in capacity may be higher than what the current figures suggest. This is due to reduced numbers of patients in the early pilot OP VCs. Furthermore, the OP VCs were not performed at the expense of another service in the department, i.e. there was no consequent reduction in capacity elsewhere or additional employment of staff.
Figure 1. The number of patients seen in VCs before and after the introduction of OPs conducted VCs.
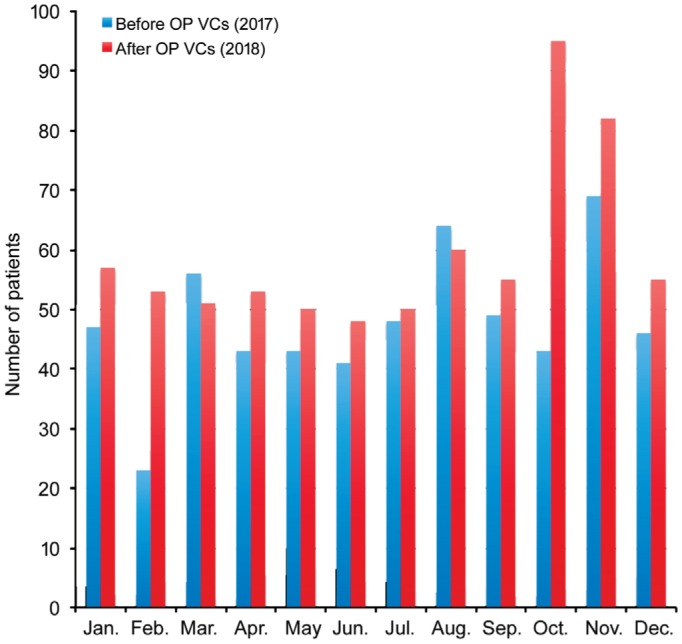
Figure 2. Mean, median and confidence interval of number of patients seen per month before and after the introduction of OP conducted VCs.
DISCUSSION
Within the medical retina service, the prevalence of certain conditions such as diabetic retinopathy and age-related macular degeneration (AMD) is projected to grow substantially over the next decades[6],[18]. Estimates for the projected growth in burden on eye services for diabetic retinopathy and neovascular AMD in the UK are approximately 60% over the next 20y[6]. The rapid adoption of intravitreal pharmacological agents has also increased demand for hospital visits[5]. Furthermore, earlier identification of disease, for example through screening or imaging in optometry practices, may lead to more referrals, and a greater capture of patients that do not necessarily require treatment[10].
The capacity of eye services in the UK is also threatened. The UK has one of the lowest number of ophthalmologists per capita amongst developed countries and an ageing population that is growing at twice the rate of the profession[8].
These factors threaten to overwhelm eye care resources and have lead to efforts to improve efficiency and use of resources. Suggestions for solutions regarding ophthalmologist shortages include devolving all non-consultant dependent tasks to other healthcare professionals[11]. This can be facilitated by VCs. Other benefits of VCs include better access to equipment, such as imaging, outside main clinic times and bottlenecks[11].
The Department of Health, UK, supports extended roles for non-medical healthcare professionals and the investment in their training and development[9]. It is both cost effective and can lead to increased job satisfaction[10],[12],[16],[19]. Shared care between ophthalmologists, optometrists and nurses has been well established and can deliver a safe and effective service[10],[12]–[14],[19]. OPs, however, are not typically involved in patient management decisions. They represent an untapped resource and can potentially help with increasing the capacity and efficiency of eye services, especially as they can combine several roles, such as image acquisition, interpretation and making clinical decisions.
VCs were first described for glaucoma and demonstrated reliability, cost-effectiveness and the ability to increase the capacity of hospital care[12]–[13],[15]. More recently they have been successfully implemented in medical retina departments[10],[14]. Virtual AMD clinics are now run in 63% of eye departments in the UK[6]. Medical retina conditions may be particularly amenable to VCs conducted by non-medical professionals. They are heavily reliant on imaging and visual acuity measurements, which can be recorded in the absence of the healthcare practitioner, and can be protocol driven with pre-determined, objective, thresholds for management[10].
Our results show that VCs by OPs can be conducted appropriately and can lead to an increase in healthcare capacity. These results potentially have important implications. They highlight a new avenue for improving service capacity and efficiency, which is likely to be cost effective and can be extended to several chronic medical retina conditions. Larger studies with longer follow ups are required to determine the safety and long-term outcomes of OP VCs.
Acknowledgments
We would like to acknowledge the senior ophthalmic photographers at Leicester Royal Infirmary who assisted with this project: Andrew Farmer, Kayleigh Parker, Lee Daines.
Conflicts of Interest: El-Khayat AR, None; Anzidei R, None; Konidaris V, None.
REFERENCES
- 1.Klein BE. Overview of epidemiologic studies of diabetic retinopathy. Ophthalmic Epidemiol. 2007;14(4):179–183. doi: 10.1080/09286580701396720. [DOI] [PubMed] [Google Scholar]
- 2.Laouri M, Chen E, Looman M, Gallagher M. The burden of disease of retinal vein occlusion: review of the literature. Eye (Lond) 2011;25(8):981–988. doi: 10.1038/eye.2011.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourne RRA, Jonas JB, Bron AM, et al. Vision Loss Expert Group of the Global Burden of Disease Study Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe in 2015: magnitude, temporal trends and projections. Br J Ophthalmol. 2018;102(5):575–585. doi: 10.1136/bjophthalmol-2017-311258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grzybowski A, Told R, Sacu S, Bandello F, Moisseiev E, Loewenstein A, Schmidt-Erfurth U, Euretina Board 2018 update on intravitreal injections: euretina expert consensus recommendations. Ophthalmologica. 2018;239(4):181–193. doi: 10.1159/000486145. [DOI] [PubMed] [Google Scholar]
- 5.Stewart MW. Treatment of diabetic retinopathy: recent advances and unresolved challenges. World J Diabetes. 2016;7(16):333–341. doi: 10.4239/wjd.v7.i16.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Royal College of Ophthalmologists. The Way Forward Resources – Age-related Macular Degeneration and Diabetic Retinopathy. [Accessed on March 13, 2020]. https://www.rcophth.ac.uk/wp-content/uploads/2015/10/RCOphth-The-Way-Forward-AMD-300117.pdf.
- 7.Fahy N, Hervey T, Greer S, Jarman H, Stuckler D, Galsworthy M, McKee M. How will Brexit affect health services in the UK? An updated evaluation. Lancet. 2019;393(10174):949–958. doi: 10.1016/S0140-6736(19)30425-8. [DOI] [PubMed] [Google Scholar]
- 8.Resnikoff S, Felch W, Gauthier TM, Spivey B. The number of ophthalmologists in practice and training worldwide: a growing gap despite more than 200, 000 practitioners. Br J Ophthalmol. 2012;96(6):783–787. doi: 10.1136/bjophthalmol-2011-301378. [DOI] [PubMed] [Google Scholar]
- 9.Department of Health. The NHS plan: a summary. [Accessed on March 13, 2020]. https://webarchive.nationalarchives.gov.uk/20130123203940/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4010198.
- 10.Kortuem K, Fasler K, Charnley A, Khambati H, Fasolo S, Katz M, Balaskas K, Rajendram R, Hamilton R, Keane PA, Sim DA. Implementation of medical retina virtual clinics in a tertiary eye care referral centre. Br J Ophthalmol. 2018;102(10):1391–1395. doi: 10.1136/bjophthalmol-2017-311494. [DOI] [PubMed] [Google Scholar]
- 11.Amoaku W, Blakeney S, Freeman M, Gale R, Johnston R, Kelly SP, McLaughlan B, Sahu D, Varma D, Action on AMD Group Action on AMD. Optimising patient management: act now to ensure current and continual delivery of best possible patient care. Eye (Lond) 2012;26(Suppl 1):S2–S21. doi: 10.1038/eye.2011.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trikha S, Macgregor C, Jeffery M, Kirwan J. The Portsmouth-based glaucoma refinement scheme: a role for virtual clinics in the future? Eye (Lond) 2012;26(10):1288–1294. doi: 10.1038/eye.2012.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keenan J, Shahid H, Bourne RR, White AJ, Martin KR. Cambridge community optometry glaucoma scheme. Clin Exp Ophthalmol. 2015;43(3):221–227. doi: 10.1111/ceo.12398. [DOI] [PubMed] [Google Scholar]
- 14.Tsaousis KT, Empeslidis T, Konidaris VE, Kapoor B, Deane J. The concept of virtual clinics in monitoring patients with age-related macular degeneration. Acta Ophthalmol. 2016;94(5):e353–e355. doi: 10.1111/aos.12832. [DOI] [PubMed] [Google Scholar]
- 15.Kotecha A, Brookes J, Foster PJ. A technician-delivered ‘virtual clinic’ for triaging low-risk glaucoma referrals. Eye (Lond) 2017;31(6):899–905. doi: 10.1038/eye.2017.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collins K, Jones ML, McDonnell A, Read S, Jones R, Cameron A. Do new roles contribute to job satisfaction and retention of staff in nursing and professions allied to medicine? J Nurs Manag. 2000;8(1):3–12. [PubMed] [Google Scholar]
- 17.Leicester City Council. Diabetes. [Accessed on March 13, 2020]. https://www.leicester.gov.uk/media/181806/diabetes-section-march-2016.pdf.
- 18.Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–149. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 19.DaCosta J, Hamilton R, Nago J, Mapani A, Kennedy E, Luckett T, Pavesio C, Flanagan D. Implementation of a nurse-delivered intravitreal injection service. Eye (Lond) 2014;28(6):734–740. doi: 10.1038/eye.2014.69. [DOI] [PMC free article] [PubMed] [Google Scholar]


