Summary
Almost 2 billion people travel aboard commercial airlines every year. Health-care providers and travellers need to be aware of the potential health risks associated with air travel. Environmental and physiological changes that occur during routine commercial flights lead to mild hypoxia and gas expansion, which can exacerbate chronic medical conditions or incite acute in-flight medical events. The association between venous thromboembolism and long-haul flights, cosmic-radiation exposure, jet lag, and cabin-air quality are growing health-care issues associated with air travel. In-flight medical events are increasingly frequent because a growing number of individuals with pre-existing medical conditions travel by air. Resources including basic and advanced medical kits, automated external defibrillators, and telemedical ground support are available onboard to assist flight crew and volunteering physicians in the management of in-flight medical emergencies.
Introduction
Fitness for air travel is a growing issue because many passengers are unaware of health implications associated with commercial air travel. Almost 2 billion people travel by air every year,1, 2 and physicians are now expected to identify individuals unfit for air travel and give them advice. More than 95% of individuals with health problems who have to travel by air would like to receive more medical advice from their physician.3 Also, the age of travellers is increasing and long-haul aircrafts—such as the Airbus A380 and Boeing 777 LR—are now capable of extending flight times to 18–20 h; therefore, an increasing number of travellers with various underlying medical conditions could face environmental and physiological changes associated with the flight. Here, we review the health issues associated with commercial air travel.
Cabin pressure
Cabin pressure can affect the health and wellbeing of passengers in many ways, including hyobaric hypoxia affecting those with pre-existing respiratory conditions and heart failure, and gas expansion within body cavities and medical devices.
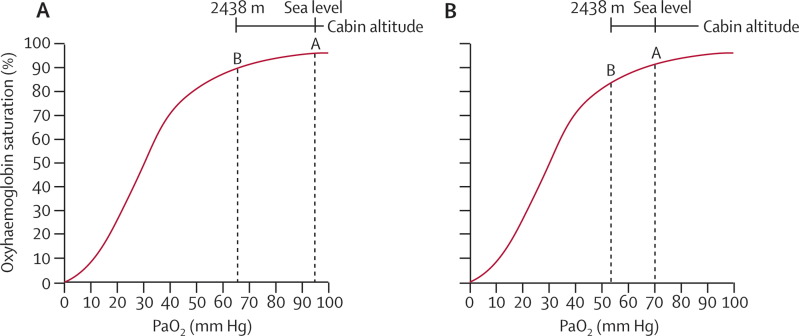
Although commercial flights usually cruise at altitudes of 7010–12 498 m above sea level, the passenger cabin is pressurised to an altitude of 1524–2438 m. Most regulatory governmental agencies require the cabin altitude not to exceed 2438 m.4, 5, 6 Most healthy individuals tolerate this cabin pressure; however, a study of adult volunteers simulating a 20-h flight showed that the frequency of reported complaints associated with acute mountain sickness (fatigue, headache, lightheadedness, and nausea) increased with increasing altitude and peaked at 2438 m, with most symptoms becoming apparent after 3–9 h of exposure.7 Cabin pressurisation to 2438 m reduces the atmospheric pressure of the cabin, resulting in a concomitant decrease of arterial oxygen partial pressure (PaO2) from 95 mm Hg to 60 mm Hg at the maximum cabin altitude of 2438 m.8 In healthy passengers, these pressures lead to a 3–4% decrease in systemic oxyhaemoglobin saturation (the corresponding PaO2 value remains within the flat portion of the oxyhaemoglobin dissociation curve) (figure ).5, 7 However, many passengers with pre-existing cardiac, pulmonary, and haematological conditions have a reduced baseline PaO2, so reduced cabin pressure leads to further reduction of oxygen saturation, which lowers further with increasing flight times (figure).8, 9 The decreased oxygen saturation can exacerbate medical conditions.2, 4, 9, 10 For example, a recent prospective observational study showed that 18% of passengers with chronic obstructive pulmonary disease have at least mild respiratory distress during a flight.11
Figure.
Effect of cabin altitude on oxyhaemoglobin saturation
(A) The aircraft passenger cabin is normally pressurised to an altitude of 1524–2438 m. This reduced pressure within the passenger cabin results in lower systemic PaO2 and decreased oxyhaemoglobin. For most healthy passengers, this results in a decrease in the arterial partial pressure oxygen tension from 95 mm Hg (12·7 kPa) to 65 mm Hg (8·7 kPa) corresponding to an oxyhaemoglobin saturation from 95–100% at sea level (A) to 90% at a cabin altitude of 2438 m (B). (B) Passengers with pre-existing lower sea-level oxyhaemoglobin saturations have greater declines during a flight. In this example, a passenger with mild chronic obstructive pulmonary disease with a sea-level PaO2 of 70 mm Hg (A) and a FEV1 of 1·6 L (50% predicted) will have a corresponding reduction of PaO2 to about 53 mm Hg or oxyhaemoglobin saturation of approximately 84% at a cabin altitude of 2438 m (B). This passenger should be prescribed oxygen for air travel. PaO2=arterial oxygen partial pressure. FEV1=forced expiratory effort in 1 second.
Several methods are available to assess the need for in-flight oxygen (panel 1 ).9, 10, 12, 13 Oxygen supplementation is recommended for passengers with either a resting oxygen saturation of 92% or lower (PaO2 ≤67 mm Hg) or if the expected in-flight PaO2 is less than 50–55 mm Hg.9 Guidelines from the British Thoracic Society (BTS)9 suggest hypoxic-challenge testing in individuals with resting oxygen saturations of 92–95% at sea level who have additional risk factors, such as hypercapnia or abnormal spirometry. The Aerospace Medical Association (AsMa) guidelines suggest sea-level blood gas determination or pulmonary-function testing with hypoxic-challenge testing as the gold standard, and recommend in-flight oxygen for individuals with a sea-level PaO2 of 70 mm Hg or lower, or with an expected in-flight PaO2 of 55 mm Hg or lower.10 However, some evidence suggests that these guidelines might need revision because predictive equations often inaccurately estimate in-flight PaO2.2, 9, 12, 14, 15, 16 Additionally, recent work has shown that initial sea-level oxygen saturation poorly identifies individuals at risk of desaturation below 90% during either hypoxic-challenge testing in the laboratory17, 18 or routine commercial flights.15, 17 No studies that assess individuals with heart failure during commercial air travel exist; however, several small studies have shown that people with chronic heart failure tolerate altitudes up to 2500–3000 m.19, 20 BTS or AsMa guidelines should be followed with patients affected by heart failure who have to travel by air.
Panel 1. Assessment of in-flight PaO2.
Hypoxic-challenge test (hypoxia altitude simulation test):
The maximum cabin altitude of 2438 m can be simulated at sea level with a gas mixture containing 15% oxygen in nitrogen. Individuals breathe the hypoxic gas mixture for 20 min while oxygen saturation is monitored. Arterial blood gases are also measured before and at the end of the test. An individual needs in-flight oxygen if PaO2 falls below 50 mm Hg or if the oxygen saturation measured via pulse oximetry falls below 85%.
Predictive Dillard equations:
PaO2 at altitude can be estimated with several published predictive equations, which use values of ground-level PaO2 and lung-function measurements to predict in-flight PaO2:
-
•
In-flight PaO2=0·453×ground-level PaO2 (mm Hg)+0·386 (FEV1% predicted)+2·44
-
•
In-flight PaO2=0·519×ground-level PaO2 (mm Hg)+11·855×FEV1 (L)−1·760
Several options exist for passengers needing medical oxygen during air travel. Compressed oxygen supplied by the airline is available for individuals with a physician's statement of need and prescription. Since 2005, portable oxygen concentrators, which concentrate oxygen in ambient air by removing nitrogen content, have become available as an alternative to traditional oxygen cylinders. Passengers should possess a signed doctor's statement of medical need and notify the airline of their intention to use portable oxygen concentrators before travelling.21 Because of a modification in the US Government Air Carrier Access Act in May, 2008, all US-based air carriers and foreign air carrier flights that begin or end in the USA have to accommodate passengers who need portable oxygen concentrators.22
Gas in body cavities is also affected by cabin pressure. According to Boyle's law, the volume that a gas occupies is inversely proportional to the surrounding pressure. Thus, at the low cabin pressures associated with cruising altitudes, gas in body cavities expands by 30%.6, 10, 23 For healthy passengers, this expansion can result in minor abdominal cramping and barotrauma to the ears in certain circumstances. However, passengers who have undergone recent surgical procedures are at increased risk of problems related to gas expansion, and many anecdotal reports, including those of bowel perforation24 and wound dehiscence,25 have been published. Guidelines recommend delaying air travel for 14 days after major surgical procedures.10, 23 Individuals with bowel obstructions or diverticulitis are advised to wait 7–10 days before air travel.10, 23
Passengers who scuba dive also have an increased risk of decompression sickness if they fly too soon after diving. The diver's alert network recommends a 12-h interval between diving and air travel for divers who make a dive per day without decompression. Divers participating in several dives per day, or a dive requiring decompression, should wait 24 h before air travel.10, 23
Gas expansion also affects medical devices, such as pneumatic splints, feeding tubes, urinary catheters, and cuffed endotracheal or tracheostomy tubes. Gas-expansion concerns in these devices can be eliminated by instillation of water rather than air during air travel.6, 26
Air travel and venous thromboembolism risk
The relation between long-haul flights (>8 h) and increased risk of venous thromboembolism has generated great interest in both medical publications and the media. Overall, studies show an association between venous thromboembolism and long-haul air travel, with risk up to four-fold, depending on study methods.27, 28, 29, 30, 31, 32, 33
Risk peaks when flight duration is more than 8 h;34, 35, 36 a population-based study showed that risk started to increase when flight duration exceeded 4 h.32 Business-class versus economy-class travel has no effect on venous thromboembolism incidence.37 A systematic review of publications on air-travel venous thromboembolism calculated a pooled odds ratio (OR) of 1·59 (95% CI 1·04–2·43) from case–control studies27, 38, 39, 40, 41 and a relative risk of 2·93 (95% CI 1·5–5·58) from several prospective controlled cohort studies.38, 40 These results are consistent with those of the population-based (MEGA) study (OR 1·7, 95% CI 1·0–3·1).32 Another population-based study of 9000 business travellers followed for 4·4 years showed an absolute risk for venous thromboembolism of one every 4656 flights (incidence rate ratio 3·2, 95% CI 1·8–5·6).33 Risk increased with increasing number of flights during the first 2 weeks after a flight and when other traditional risk factors for venous thromboembolism were present. Several factors—such as immobility, dehydration, hypobaric hypoxia—and individual risk factors (obesity, malignancy, recent surgery, and history of hypercoagulable states) explain why the risk of venous thromboembolism increases with air travel.40, 42
Immobilisation has been linked to 75% of air-travel cases of venous thromboembolism, with the long-flight thrombosis study (LONFLIT) showing the greatest frequency of venous thromboembolism occurring in non-aisle seating where passengers tend to move less.42, 43, 44, 45
Dehydration can increase risk of venous thromboembolism due to haemoconcentration and hyperviscosity, potentially leading to hypercoagulable states.46 Several studies have provided evidence of dehydration or increased lower-limb oedema in healthy people during long-simulated flights.47, 48 Hypobaric-chamber studies have not consistently shown that the mild hypobaric hypoxic changes during a flight lead to increased activation of coagulation in healthy individuals with no thrombophilia compared with that in individuals seated and not moving at ground level.5, 46, 49
Thrombophilia or oral contraceptive use substantially increase the risk of developing venous thromboembolism.29, 32, 50 In the MEGA study,32 factor V Leiden increased this risk by 14 times (OR 13·6, 95% CI 2·9–64·2), and thrombophilia or use of oral contraceptives increased risk 16 times (16·1, 3·6–70·9) and 14 times (13·9, 1·7–117·5), respectively.29
Recommendations to reduce the risk of developing venous thromboembolism during air travel are based more on common sense than on evidence and include: being well hydrated, reducing alcohol and caffeine consumption, changing positions or walking throughout the cabin, and doing periodic calf-muscle exercises to reduce venous stasis. Use of graduated compression stockings with an ankle pressure of 17–30 mm Hg can reduce risk during air travel, as shown by a meta-analysis, in which only two of 1237 individuals who wore compression stockings had venous thrombosis compared with 46 of 1245 individuals who did not wear them.51 Compression stockings therefore are recommended for travellers prone to immobility.51, 52, 53
Anticoagulant thromboprophylaxis in the context of air travel is growing but no formal guidelines exist. One survey done by thrombosis and haemostasis professionals showed major differences in the use of prophylactic measures for air travel.54 Many clinicians seem to recommend aspirin before air travel for individuals at moderate risk of venous thromboembolism. However, because of scarce evidence showing substantial benefit, aspirin is not recommended alone as prophylaxis for any air traveller.41, 43, 52, 55 Although randomised trials have shown benefit of low-molecular-weight heparin as thromboprophylaxis for air travellers who are at moderate risk for venous thromboembolism and do not take routine anticoagulant drugs,43, 56 its routine use in circumstances other than those for air travellers at high risk of venous thromboembolism remains controversial.41, 52
Overall, use of physical and pharmacological thromboprophylaxis should be based on an individual risk assessment. The table summarises evidence-based guidelines updated in 2008 by the American College of Chest Physicians conference on antithrombotic and thrombolytic therapy.52
Table.
Risk of venous thromboembolism prophylaxis in air travellers
| Definition | Recommendations | Quality of evidence* | |
|---|---|---|---|
| Low risk | Flight time less than 8 h or distance less than 5000 km | Avoid constrictive clothing around waist and lower extremities; avoid dehydration; move about cabin several times or do calf-stretching exercises | Grade 1C |
| Moderate risk | Flight time more than 8 h or distance more than 5000 km, and: obesity, large varicose veins, pregnancy, hormone-replacement therapy, tobacco use or oral contraceptives, or relative immobility | Low-risk measures and: wear properly fitted below-knee compression stockings providing 15–30 mm Hg of pressure at the ankle; aisle seating | Grade 1C and grade 2B |
| High risk | Flight time more than 8 h or distance more than 5000 km, and: history of previous venous thromboembolism; hypercoagulable state (eg, factor V Leiden); major surgery 6 weeks before air travel (including hip or knee arthroplasty); known malignancy | Moderate-risk measures and: low-molecular-weight heparin injected before departure in individuals who are not on warfarin | Grade 1C and grade 2B |
Grade 1C is a strong recommendation, but existing evidence is of low quality and benefits clearly outweigh risk or burden. Grade 2B is a weak recommendation derived from moderate quality evidence, and benefits of therapy are balanced with risk and burden.52
Cosmic-radiation exposure
Cosmic radiation comes from outside the solar system and from particles released during solar flares. Intensity of radiation depends on the year (due to solar cycles), altitude, latitude, and length of exposure. Because many types of cancer might be linked to cosmic radiation—especially breast cancer, skin cancer, and melanoma—effects of radiation on flight crews and frequent air-travellers are of concern.58, 59
In 1991, the International Commission on Radiological Protection (ICRP) declared cosmic radiation an occupational risk for flight crews, which led to exposure monitoring and guidelines to reduce crew annual exposure to 20 mSv, which is more than double the exposure of most crews.60, 61, 62 Ground-radiation exposure should be restricted to 1 mSv per year in the population, but air-travel-related cosmic-radiation exposure does not have a specific limit.63 The UK Civil Aviation Authority (CAA) and the European Joint Aviation Authority (JAA) require aircraft capable of flying at altitudes greater than 15 km, to actively monitor radiation levels, so that they can lower flying altitude as needed. However, this regulation is currently not relevant to commercial aviation because no commercial aircraft fly at such altitudes.7
A solar-radiation alert system monitors high-particle intensity from solar radiation, and the US Federal Aviation Administration (FAA) issues a solar-radiation advisory to air carriers via the national oceanic and atmospheric administration (NOAA) weather wire service when solar flares might cause increased radiations at commercial-aircraft altitudes.64
Data for increased cancer risks specifically due to cosmic radiation in crew members are inconclusive.62, 65, 66, 67, 68 No studies have been done to assess the health consequences of cosmic-radiation exposure during air travel in the general population. However, even the most-frequent air travellers are unlikely to be at risk.69 Recommendations need to be in place for pregnant women because the fetus is exposed to the same radiation dose as the mother.70 The ICRP recommends a radiation limit of 1 mSv during the whole pregnancy, whereas the National Council on Radiation Protection and Measurements recommends a monthly limit of 0·5 mSv. These recommendations limit pregnant crew members and frequent air travellers, because flying roughly 15 long-haul round trips, for example, can expose a fetus to more than 1 mSv.61 To avoid risk to the fetus, the FAA recommends pregnant crew members to take short, low-altitude, low-latitude flights, and the CAA requests that employers of a pregnant crew member schedule her flights so that she remains under the 1-mSv limit.7, 59 Pregnant women, and air travellers in general, can access the solar-radiation alert system online before travelling and change flight days accordingly.
Jet lag
Jet lag is a temporary circadian-rhythm disorder associated with long-haul flights, characterised by daytime fatigue, sleep–wake disturbances, decreased appetite, constipation, and reduced psychomotor coordination and cognitive skills.71, 72, 73 Jet lag is due to desynchronisation between the body's internal clock mechanism, residing within the suprachiasmatic nucleus of the hypothalamus,74, 75, 76 and the new light–dark cycle caused by abrupt time-zone changes.72, 73, 77, 78, 79 The degree and severity of jet lag is influenced by both flight direction and number of time zones crossed.72, 80 Westward travel lengthens the traveller's day, thereby causing a phase delay in the circadian rhythm, whereas eastward travel shortens the day and causes a phase advance.72, 73, 80 Travellers have greater difficulty falling asleep after an eastward travel than after a westward travel because of the internal clock's natural tendency to resist shortening the 24-h day cycle.79, 81, 82, 83 Re-entrainment (synchronisation) typically takes one day for every time zone crossed westward or 1·5 days for every time zone crossed eastward.72, 73, 80, 81
Panel 2 lists various therapies available to keep jet lag to a minimum. Exogenous melatonin is the gold standard treatment for jet-lag symptoms.73, 83, 89, 90 When taken in the evening, melatonin phase advances the circadian clock, whereas early morning administration phase delays the circadian rhythm.73, 90 Various treatment regimens have been recommended, but a Cochrane meta-analysis of ten trials concluded that taking 0·5–5 mg of melatonin at the desired destination bedtime is effective for reducing or preventing jet lag.83
Panel 2. Treatments of jet lag.
Agomelatine 73
-
•
New dual melatonin-receptor and serotonin 5-HT2C receptor agonist
-
•
Efficacious for symptoms of depression and sleep–wakefulness disorders
-
•
Not tested for jet lag, but could be more useful for individuals having westward-travel jet lag, who commonly show symptoms of depression
-
•
Some reported efficacy in sleep quality (eg, temazepam)
-
•
Some reported efficacy in other circadian-rhythm or sleep parameters
-
•
Poorly studied
-
•
Might increase night-time awakenings
-
•
Slow-release caffeine showed faster re-entrainment (measured physiologically)
-
•
Phase advances of about 2·5 h
-
•
Usually only needed after arrival but, if travelling across more than 7–8 time zones, pre-treatment for 2–3 days may be needed
-
•
Recommended especially if crossing five or more time zones, travelling eastwardly, or with a history of jet-lag symptoms
-
•
Caution in people with epilepsy or on warfarin (case reports of adverse effects)
-
•
Paediatric use not studied and therefore not recommended
Ramelteon 73
-
•
New melatonin-receptor agonist with no abuse potential
-
•
Indication for treatment of primary insomnia in individuals of 55 years of age or older
-
•
Untested for circadian-rhythm disturbances
-
•
Involves intentional exposure or avoidance to bright light to hasten re-entrainment
-
•
Efficacy is questionable
-
•
Often impractical or inconvenient
Pre-flight sleep hygiene 72, 81, 88
-
•
Westbound: go to sleep 1 h later than usual and be awake 1 h later than usual 3 days before travelling
-
•
Eastbound: go to sleep 1 h earlier than usual and be awake 1 h earlier than usual 3 days before travelling
Use of bright-light exposure to adjust circadian rhythm has shown conflicting results and its benefit depends on combination with other therapies, such as bedtime adjustment or melatonin.91, 92, 93 Simulation studies showed a benefit of gradually advancing the sleep cycle by going to sleep 1 h earlier than usual every day for 3 days before travelling eastward, combined with morning bright-light exposure, in an attempt to phase advance the circadian rhythm.87, 92 For westward travel, one small randomised controlled study of 20 individuals combined bedtime adjustment with timed bright-light versus dim-light exposure after westward travel, and showed larger phase delays in the bright-light group than in the dim-light group (2·59 h vs 1·5 h, p <0·02), but no significant difference in sleep efficiency or self-reported symptoms of jet lag.93
Infectious diseases and air travel
Air travellers spend long periods in enclosed spaces, which facilitates the spread of infectious diseases. Since 1946, several outbreaks of serious infectious diseases have been reported aboard commercial airlines, including influenza,94, 95 measles,96 severe acute respiratory syndrome (SARS),97, 98 tuberculosis,99, 100 food poisoning,101, 102 viral enteritis,103 and small pox.104 Although less-serious outbreaks—such as the common cold or some viral syndromes—have not been reported, they can occur. Lack of reporting is likely to be the result of incubating periods of many infections being longer than the flight. One prospective questionnaire study of air travellers going from San Francisco to Denver during the winter months showed an upper-respiratory tract infection frequency of 3–20% depending on the reporting methods.105 PCR assays to study atypical bacteria and respiratory viruses in 155 air travellers showed that not many travellers had the same viral profile and no association existed between any pathogen and a particular airport, suggesting that travellers acquired their viruses before rather than during the flight.106
Most commercial aircrafts re-circulate up to 50% of the cabin air and use high-efficiency particulate air filters. One study showed no significant difference in self-reported infection rates in aircrafts that use these filters compared with those in aircrafts that use a single-pass cabin ventilation system.105
Risk of onboard transmission of infection is mainly restricted to individuals with either close personal contact or seated within two rows of an index passenger.1, 107 However, on Air China flight 112, 22 passengers and crew member developed probable onboard severe acute respiratory syndrome-associated coronavirus (SARS-CoV) infection.97 The 2002–03 SARS epidemic indicated that commercial air travel has an effect on infectious-disease spread. WHO estimates that 6·5 passengers per million who travelled aboard commercial flights originating from regions of active transmission during the outbreak were symptomatic with probable SARS.108 Overall, 40 flights carried 37 probable SARS-CoV source cases during the outbreak, resulting in 29 probable onboard secondary cases.108
Whether reducing the number of flights during a large-scale epidemic or pandemic would slow the spread of an infectious-disease outbreak remains unclear.109, 110 An observational study, however, showed that the peak date of the US influenza season was delayed 13 days after the terrorist attacks of Sept 11, 2001, consistent with a greatly reduced number of flights during that time.111 This, together with other modelling studies, suggest that flight limitations might slow the spread of pandemic influenza by several weeks, thereby providing time for mass vaccination of the population and contingency plan setup.111
In-flight medical events
Calculation of the exact incidence of in-flight medical events for commercial air travel has always been difficult, mainly because air carriers are not obliged to report in-flight medical events, and no national or international database exists. Scarce data suggest an incidence of 1 in 10 000–40 000 passengers (about 50–100 in-flight medical events per day) aboard US-registered airlines.112 British Airways health services reported 31 200 medical incidents aboard their aircrafts during 2007, with 3000 being deemed serious.113
Many in-flight medical events arise aboard commercial airlines and most are minor.6, 114 Cardiac, neurological, and respiratory complaints are the most serious in-flight medical events, with cardiac and neurological complaints accounting for most diversions.114 Passengers older than 70 years have the highest rates of in-flight medical events,114 but the mean age of passengers with an in-flight medical event is 44 years for men and 49 years for women.6, 112
According to British, Canadian, and US laws, medical professionals are not required to volunteer assistance during an in-flight medical event, unless they have a pre-existing clinical relationship with the passenger. In contrast, physicians in Australia and many Asian, European, and middle east countries are required to provide assistance.6 For international flights, the country where the aircraft is registered has jurisdiction, except when the aircraft is on the ground or in sovereign airspace.6, 112 Medical assistance during an in-flight medical event is protected under Good Samaritan laws, and no physician has ever been held liable for his or her actions while providing medical care. The 1998 US Aviation Medical Assistance Act limits liability for volunteering physicians under the assumption that they act in good faith, receive no monetary compensation, and provide reasonable care. This law pertains to events that occur within US airspace and aircraft registered within the USA.6 Gifts, such as seat upgrades and liquors, are not considered compensation. Furthermore, many airlines indemnify volunteering physicians, and the captain should provide written confirmation on request.112
Commercial aircraft have medical kits (1–4 first-aid kits and at least one enhanced emergency medical kit), as required by aviation regulatory agencies.6, 112 Emergency medical kits vary from carrier to carrier and can be extensively complex (panel 3 ). Most commercial flights also carry an automated external defibrillator, and some models have a screen showing a basic rhythm strip. Most commercial air carriers use on-ground telemedical assistance to medically assess at the gate passengers who seem unfit for travel, and to provide medical advice and support during in-flight medical events. Several companies and academic medical institutions provide 24-h ground-to-air medical support and have ground-based physicians, who also advise the flight deck on the best diversion location and arrange emergency personnel to meet the aircraft.
Panel 3. Typical contents of an enhanced emergency medical kit.
Diagnostic/general
Medications
Allergy
Analgesia
Neurological
Cardiac or resuscitation
Miscellaneous
-
•
Uterine contractant†
Clinicians who offer medical assistance during a flight should know that their role is to assist the flight crew and not to take complete control of the situation. The captain of the aircraft has the ultimate authority (panel 4 ). In case of violent or unruly passengers, volunteering physicians might need to assist in chemical or physical restraint. If chemical restraint is used, physicians should consider that passengers could have ingested alcohol or other substances that might cause oversedation or other effects.116 Panel 5 lists general guidelines for the initial management of common in-flight medical events.
Panel 4. Response to in-flight medical events.
-
•
Be prepared to show medical credential (eg, licence) or answer questions about degree or training
-
•
Act within your abilities
-
•
Obtain consent from the affected passenger. Assume implied consent when passenger is incapacitated or unresponsive
-
•
Do not fear litigation. Although physicians have been deposed, no litigation has ever been brought forward against a responding physician
-
•
Request and establish communication with the airline's ground medical support for advice and consultation regardless of how minor or serious the in-flight medical event is
-
•
Request the enhanced emergency medical kit (many airlines will initially only offer the basic first-aid kit) but do not open it unless needed. Each kit has a placard listing the contents of the kit
-
•
Recommend diversion of the aircraft if you believe it is needed. Recommendation to divert the aircraft should be considered if a passenger has chest pain, shortness of breath, severe abdominal pain that does not improve with initial treatment interventions, cardiac arrest, acute coronary syndrome, severe dyspnoea, stroke, refractory seizure, severe agitation, or if a passenger is persistently unresponsive
-
•
Never officially pronounce a passenger dead, even if you assess that resuscitation is futile and cease treatment, especially on international flights
Panel 5. Guidelines for initial management of in-flight medical events.
Acute abdominal pain
-
•
Administer antiacid if appropriate
-
•
Request cabin altitude reduction to increase cabin pressure, which will increase oxygenation and decrease gas expansion
-
•
Administer paracetamol or ibuprofen to relieve discomfort. Some medical kits contain morphine, which can be used in cases of extreme pain
-
•
A parenteral or oral antiemetic drug if available in the medical kit might help in cases of persistent vomiting
Acute agitation or misconduct
-
•
Attempt to de-escalate the situation. Look for medical causes, such as hypoxia or hypoglycaemia
-
•
Offer or administer benzodiazepine, if available and indicated (be aware for possible oversedative effect, if passenger is already taking other substances)
-
•
If physical restraint is needed, it should be undertaken by 4–5 individuals. The restrained individual should be placed in the left lateral recumbent position
-
•
Appropriately monitor patient if chemical or physical restraints are used. Be aware of high risk of complications (hypoxia, metabolic acidosis, and sudden death) because of fighting against restraints coupled with recent extreme exertion by the agitated passenger
Acute allergic reaction and anaphylaxis
-
•
Administer diphenhydramine 12·5 mg po, im, or iv (paediatric); 25–50 mg po, im, or iv(adult) for both simple allergic reactions and anaphylaxis
-
•
Administer epinephrine 0·01 mL/kg/dose 1 in 1000 solution im or sc every 5–20 min as needed up to three doses (paediatric), or 0·3–0·5 mL 1 in 1000 solution im or sc every 5–20 min as needed up to three doses (adults) in the presence of severe generalised urticaria, angio-oedema, stridor, or bronchospasm
-
•
Establish iv access and administer fluids in presence of anaphylaxis if possible
Chest pain
-
•
If diagnosis is uncertain, an antacid could help to confirm dyspepsia
-
•
For persistent pain or if myocardial infarction is suspected, administer oxygen, aspirin 325 mg po, and nitroglycerin 0·4 mg sublingual every 5 min up to three doses or morphine sulfate 3 mg iv or im, as indicated
-
•
Request cabin altitude reduction to increase cabin pressure
-
•
Some airlines carry automated external defibrillators with a cardiac rhythm display to help assess cardiac rhythm
Asthma or chronic obstructive pulmonary disease
-
•
Administer oxygen and inhaled bronchodilator (two puffs every 15 min) as indicated
-
•
Request cabin altitude reduction to increase cabin pressure
Cardiac arrest
-
•
Place automated external defibrillator on patient. Some defibrillators incorporate a rhythm display that can help making decisions
-
•
Follow basic life support or advanced cardiac life support resuscitation algorithms
-
•
If resuscitation is stopped because of no return of spontaneous circulation, the individual should not be pronounced dead officially on international flights due to medico-legal reasons
Hypoglycemia
-
•
If conscious, administer oral glucose gel
-
•
If not conscious, establish iv access and administer D50 dextrose (1 amp) for adult or 2 mL/kg of D25 dextrose (D50 diluted 1:1 with normal saline solution) for paediatric
Seizure
-
•
Keep passenger away from nearby objects
-
•
Do not place anything in passenger's mouth
-
•
Administer benzodiazepine if available (diazepam 0·1–0·3 mg/kg iv or im for paediatrics, and 5 mg iv or im for adults)
Unresponsive passenger
-
•
Place automated external defibrillator pads on patient
-
•
Establish iv access if possible
-
•
Administer oxygen, D50 dextrose (1 amp) iv for adult or D25 dextrose (2 mL/kg) for paediatric, naloxone 0·1–2 mg iv or im (if available)
-
•
Follow basic life support or advanced cardiac life support resuscitation algorithms
Vasovagal syncope
-
•
Lay patient supine and elevate legs if possible
-
•
Apply cold compress to forehead
Medical fitness for air travel
Airlines have the right to refuse passengers who are unfit to fly for medical reasons.6, 119 Many conditions contraindicate air travel and passengers who cannot tolerate hypoxia or pressure changes should not fly (panel 6 ). Passengers should be able to walk a distance of 50 m and climb one flight of stairs without angina or severe dyspnoea.6 If a passenger needs oxygen, he or she requires physician documentation stating fitness to travel at 2438 m. Passengers bringing needles and syringes into the cabin should possess documentation of need and carry the medication that requires that equipment with pharmacy-labelled identification.124 Some passengers might also need a qualified medical escort, such as passengers whose fitness to travel is in doubt due to possible exacerbation or instability of chronic disease or passengers who have organ failure requiring transplantation.119 Many air carriers have limited transport of passengers on stretchers or those unable to sit upright in a seat.125 Numerous air ambulance services and clinics offer physician-assisted or nurse-assisted escorts for commercial air flights, and physicians or passengers can call airlines for assistance.
Panel 6. Contraindications to commercial air travel.
Cardiac and pulmonary disorders
-
•
Myocardial infarction 7–10 days before air travel
-
•
Unstable angina
-
•
Coronary artery bypass graft 10–14 days before air tarvel
-
•
Decompensated heart failure
-
•
Uncontrolled dysarythmia
-
•
Contagious pulmonary infections
-
•
Baseline sea-level PaO2<67–70 mm Hg without supplemental oxygen
-
•
Obstructive/restrictive lung-disease exacerbation
-
•
Large pleural effusion
-
•
Pneumothorax 3 weeks before air travel (7–14 days with medical escort)
Neurological disorders
-
•
Stroke 5–10 days before air travel
-
•
Uncontrolled seizures or 24–h after grand-mal seizure
Surgical interventions
-
•
Any gastrointestinal, thoracic, ear, nose, and throat, and neurological surgical procedure 10–14 days before air travel
-
•
Uncomplicated appendectomy or laparoscopic surgery 5 days before air travel
Pregnancy
-
•
From 36th week of pregnancy (from 32nd weeks for multiple gestation) up to 7 days after delivery. Doctor certification needed after 28 weeks of pregnancy
-
•
Complicated pregnancy
Paediatrics
-
•
First week of life
Miscellaneous
-
•
Unlikely to survive flight
-
•
Severe contagious illness
-
•
Sickle-cell disease exacerbation 10 days before air travel
-
•
Severe anaemia (haemoglobin <8·5g/dL) unless due to chronic disease
-
•
Aggressive unpredictable behaviour or acute psychosis
-
•
Severe sinusitis
-
•
Decompression syndrome 3–7 days before air travel
Controversies and future directions
Passenger health and wellbeing during commercial air travel continues to evolve. Cabin air quality remains an issue, and it has been linked to passenger and flight crew complaints of dry eyes, stuffy nose, and skin irritation, as well as headaches, lightheadedness, and confusion.126 Peer-reviewed studies on the effect of vaporised organic compounds, such as tricresyl phosphate, that have led to reported cases of crew and passenger incapacitation are needed. These compounds are the result of vaporised jet oils that can mix with air entering the aircraft cabin. Several research groups, such as the cabin air-quality reference group and the Australian civil aviation safety authority, are addressing knowledge gaps on health effects of cabin air, including the role of vaporised organic compounds.
The American society of heating, refrigerating, and air conditioning engineers—an industry leader in developing indoor air-quality standards—set, for the first time, new air-quality standards in commercial aircrafts. The new standards also address chemical, physical, and biological contaminants that affect cabin air quality. How these standards will be adopted by aviation and governmental regulatory agencies remains unclear. At present, no regulations by the CAA, FAA, or JAA exist requiring use, certification, or maintenance of high-efficiency particulate air. New aircrafts, such as the Airbus A380 and Boeing 787, are being designed to operate at cabin altitude of 1829 m compared with the current altitude of 2438 m, in addition to having improved cabin air quality and passenger seating. These changes will improve passenger wellbeing and comfort.
How individuals with compromised cardiac and pulmonary function can endure long air travel needs to be assessed, and current screening guidelines should undergo re-assessment. Furthermore, absence of a globally accepted guideline, and major differences in the use of prophylactic measures by clinicians for air-travel-related thrombosis54 emphasise the need for additional studies on interventions and clear guidelines on prevention of air-travel-related venous thrombosis.
The molecular basis for circadian-rhythm disorders has been recently clarified and future clinical application might lead to new treatments for jet lag.
The risk that commercial aircrafts are vehicles of influenza pandemic spread is real and opportunities exist to keep the risk to a minimum. The international air-transport association, in partnership with WHO and other stakeholders, have established guidelines for aviation-industry operations during pandemic influenza outbreaks to keep commercial air-travel spread to a minimum. These include communication of the risk to the population, establishment of national passenger exit screening from outbreak regions, and increasing airline preparedness (in-flight illness and aircraft cleaning).127, 128
In-flight medical events are projected to increase and AsMa encourages the creation of a database, but many air carriers are reluctant to participate. Commercial space travel is projected to start within the next decade and aerospace medical societies have set up subcommittees to address the unique medical conditions associated with civilian space travel.
In the modern travel era, clear understanding of the medical consequences of commercial flights has become increasingly important. Individuals need to be aware of the possible medical complications of air travel, and physicians should identify people at potential risk from air travel and advise them of any necessary treatments to travel safely.
Search strategy and selection criteria
We searched Medline for peer-reviewed publications over the past 10 years written in English, with the keywords “air travel”, together with “hypoxia”, “surgery”, “cosmic radiation”, “jet lag”, “venous thromboembolism”, “infectious diseases”, “pandemic”, and “in-flight medical emergencies”. Titles, abstracts, or both, of all articles were reviewed to assess relevance. We reviewed governmental reports from the UK Department of Transport Civil Aviation Authority, UK House of Lords, US Federal Aviation Administration, and documents published by the British Thoracic Society, Aerospace Medical Association, WHO, US Institute of Medicine, and the International Commission on Radiological Protection. We also searched the above keywords with the Google search engine.
FEV1=forced expiratory effort in 1 second.
iv=intravenous. po=orally. The list was complied from 6, 112, 115. It does not include all contents but only what is mandated by each regulatory agency. Contents, such as adhesive bandages, gauzes, and elastic bandages, are stocked in basic first-aid kits, which are also carried on aircraft. Both the CAA and the JAA do not require aircraft to carry an automated external defibrillator, although most air carriers have one.
im=intramuscular. iv=intravenously. po=orally. sc=subcutaneously. The list is based on 6, 116, 117, 118.
Conflict of interest statement
We declare that we have no conflict of interest.
Footnotes
Kit specification FAA.
Kit specification JAA.
References
- 1.Mangili A, Gendreau MA. Transmission of infectious diseases during commercial air travel. Lancet. 2005;365:989–996. doi: 10.1016/S0140-6736(05)71089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seccombe LM, Peters MJ. Oxygen supplementation for chronic obstructive pulmonary disease patients during air travel. Curr Opin Pulm Med. 2006;12:140–144. doi: 10.1097/01.mcp.0000208454.03597.bb. [DOI] [PubMed] [Google Scholar]
- 3.Burnett JC. Long- and short-haul travel by air: issues for people with diabetes on insulin. J Travel Med. 2006;13:255–260. doi: 10.1111/j.1708-8305.2006.00057.x. [DOI] [PubMed] [Google Scholar]
- 4.Cabin cruising altitudes for regular transport aircraft. Aviat Space Environ Med. 2008;79:433–439. doi: 10.3357/asem.2272.2008. [DOI] [PubMed] [Google Scholar]
- 5.Toff WD, Jones CI, Ford I. Effect of hypobaric hypoxia, simulating conditions during long-haul air travel, on coagulation, fibrinolysis, platelet function, and endothelial activation. JAMA. 2006;295:2251–2261. doi: 10.1001/jama.295.19.2251. [DOI] [PubMed] [Google Scholar]
- 6.Gendreau MA, DeJohn C. Responding to medical events during commercial airline flights. N Engl J Med. 2002;346:1067–1073. doi: 10.1056/NEJMra012774. [DOI] [PubMed] [Google Scholar]
- 7.Muhm JM, Rock PB, McMullin DL. Effect of aircraft-cabin altitude on passenger discomfort. N Engl J Med. 2007;357:18–27. doi: 10.1056/NEJMoa062770. [DOI] [PubMed] [Google Scholar]
- 8.Humphreys S, Deyermond R, Bali I, Stevenson M, Fee JP. The effect of high altitude commercial air travel on oxygen saturation. Anaesthesia. 2005;60:458–460. doi: 10.1111/j.1365-2044.2005.04124.x. [DOI] [PubMed] [Google Scholar]
- 9.Managing passengers with respiratory disease planning air travel: British Thoracic Society recommendations. Thorax. 2002;57:289–304. doi: 10.1136/thorax.57.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medical Guidelines for Airline Travel, 2nd edn. Aviat Space Environ Med. 2003;74(suppl):A1–A19. [PubMed] [Google Scholar]
- 11.Coker RK, Shiner RJ, Partridge MR. Is air travel safe for those with lung disease? Eur Respir J. 2007;30:1057–1063. doi: 10.1183/09031936.00024707. [DOI] [PubMed] [Google Scholar]
- 12.Dine CJ, Kreider ME. Hypoxia altitude simulation test. Chest. 2008;133:1002–1005. doi: 10.1378/chest.07-1354. [DOI] [PubMed] [Google Scholar]
- 13.Dillard TA, Berg BW, Rajagopal KR, Dooley JW, Mehm WJ. Hypoxemia during air travel in patients with chronic obstructive pulmonary disease. Ann Intern Med. 1989;111:362–367. doi: 10.7326/0003-4819-111-5-362. [DOI] [PubMed] [Google Scholar]
- 14.Dillard TA, Moores LK, Bilello KL, Phillips YY. The preflight evaluation. A comparison of the hypoxia inhalation test with hypobaric exposure. Chest. 1995;107:352–357. doi: 10.1378/chest.107.2.352. [DOI] [PubMed] [Google Scholar]
- 15.Akero A, Christensen CC, Edvardsen A, Skjonsberg OH. Hypoxaemia in chronic obstructive pulmonary disease patients during a commercial flight. Eur Respir J. 2005;25:725–730. doi: 10.1183/09031936.05.00093104. [DOI] [PubMed] [Google Scholar]
- 16.Martin SE, Bradley JM, Buick JB, Bradbury I, Elborn JS. Flight assessment in patients with respiratory disease: hypoxic challenge testing vs predictive equations. QJM. 2007;100:361–367. doi: 10.1093/qjmed/hcm033. [DOI] [PubMed] [Google Scholar]
- 17.Akero A, Christensen CC, Edvardsen A, Ryg M, Skjonsberg OH. Pulse oximetry in the preflight evaluation of patients with chronic obstructive pulmonary disease. Aviat Space Environ Med. 2008;79:518–524. doi: 10.3357/asem.2120.2008. [DOI] [PubMed] [Google Scholar]
- 18.Robson AG, Lenney J, Innes JA. Using laboratory measurements to predict in-flight desaturation in respiratory patients: are current guidelines appropriate? Respir Med. 2008;102:1592–1597. doi: 10.1016/j.rmed.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Agostoni P, Cattadori G, Guazzi M. Effects of simulated altitude-induced hypoxia on exercise capacity in patients with chronic heart failure. Am J Med. 2000;109:450–455. doi: 10.1016/s0002-9343(00)00532-5. [DOI] [PubMed] [Google Scholar]
- 20.Erdmann J, Sun KT, Masar P, Niederhauser H. Effects of exposure to altitude on men with coronary artery disease and impaired left ventricular function. Am J Cardiol. 1998;81:266–270. doi: 10.1016/s0002-9149(97)00901-6. [DOI] [PubMed] [Google Scholar]
- 21.Federal Aviation Administration Use of certain portable oxygen concentrator devices onboard aircraft. FAA-2004-18596; SFAR No 106. 2005. http://rgl.faa.gov/Regulatory_and_Guidance_Library/rgFAR.nsf/0/E567E76F11BCFE55862571F7005AC2B8?OpenDocument&Highlight=oxygen (accessed Oct 12, 2008).
- 22.Nondiscrimination on the basis of disability in air travel Final rule. Fed Regist. 2008;73:27613–27687. [PubMed] [Google Scholar]
- 23.Halloran ME, Ferguson NM, Eubank S. Modeling targeted layered containment of an influenza pandemic in the United States. Proc Natl Acad Sci USA. 2008;105:4639–4644. doi: 10.1073/pnas.0706849105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kenfack R, Debaize S, Sztern B, Joukovsky P. Perforation of a hiatal hernia after a high altitude flight. Rev Med Liege. 2007;62:144–146. [PubMed] [Google Scholar]
- 25.Skjenna OW. Care in the air. CMAJ. 1989;140:1126. [PMC free article] [PubMed] [Google Scholar]
- 26.Bettes TN, McKenas DK. Medical advice for commercial air travelers. Am Fam Physician. 1999;60:801–808. [PubMed] [Google Scholar]
- 27.Ferrari E, Chevallier T, Chapelier A, Baudouy M. Travel as a risk factor for venous thromboembolic disease: a case-control study. Chest. 1999;115:440–444. doi: 10.1378/chest.115.2.440. [DOI] [PubMed] [Google Scholar]
- 28.Arya R, Barnes JA, Hossain U, Patel RK, Cohen AT. Long-haul flights and deep vein thrombosis: a significant risk only when additional factors are also present. Br J Haematol. 2002;116:653–654. doi: 10.1046/j.0007-1048.2001.03330.x. [DOI] [PubMed] [Google Scholar]
- 29.Martinelli I, Taioli E, Battaglioli T. Risk of venous thromboembolism after air travel: interaction with thrombophilia and oral contraceptives. Arch Intern Med. 2003;163:2771–2774. doi: 10.1001/archinte.163.22.2771. [DOI] [PubMed] [Google Scholar]
- 30.Gallus AS. Travel, venous thromboembolism, and thrombophilia. Semin Thromb Hemost. 2005;31:90–96. doi: 10.1055/s-2005-863810. [DOI] [PubMed] [Google Scholar]
- 31.Becker NG, SalIM A, Kelman CW. Air travel and the risk of deep vein thrombosis. Aust NZ J Public Health. 2006;30:5–9. doi: 10.1111/j.1467-842x.2006.tb00077.x. [DOI] [PubMed] [Google Scholar]
- 32.Cannegieter SC, Doggen CJ, van Houwelingen HC, Rosendaal FR. Travel-related venous thrombosis: results from a large population-based case control study (MEGA study) PLoS Med. 2006;3:e307. doi: 10.1371/journal.pmed.0030307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuipers S, Cannegieter SC, Middeldorp S, Robyn L, Buller HR, Rosendaal FR. The absolute risk of venous thrombosis after air travel: a cohort study of 8,755 employees of international organisations. PLoS Med. 2007;4:e290. doi: 10.1371/journal.pmed.0040290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schwarz T, Siegert G, Oettler W. Venous thrombosis after long-haul flights. Arch Intern Med. 2003;163:2759–2764. doi: 10.1001/archinte.163.22.2759. [DOI] [PubMed] [Google Scholar]
- 35.Hughes R, Heuser T, Hill S. Recent air travel and venous thromboembolism resulting in hospital admission. Respirology. 2006;11:75–79. doi: 10.1111/j.1440-1843.2006.00787.x. [DOI] [PubMed] [Google Scholar]
- 36.Hughes RJ, Hopkins RJ, Hill S. Frequency of venous thromboembolism in low to moderate risk long distance air travellers: the New Zealand Air Traveller's Thrombosis (NZATT) study. Lancet. 2003;362:2039–2044. doi: 10.1016/s0140-6736(03)15097-0. [DOI] [PubMed] [Google Scholar]
- 37.Jacobson BF, Munster M, Smith A. The BEST study–a prospective study to compare business class versus economy class air travel as a cause of thrombosis. S Afr Med J. 2003;93:522–528. [PubMed] [Google Scholar]
- 38.Philbrick JT, Shumate R, Siadaty MS, Becker DM. Air travel and venous thromboembolism: a systematic review. J Gen Intern Med. 2007;22:107–114. doi: 10.1007/s11606-006-0016-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Trujillo-Santos AJ, Jimenez-Puente A, Perea-Milla E. Association between long travel and venous thromboembolic disease: a systematic review and meta-analysis of case-control studies. Ann Hematol. 2008;87:79–86. doi: 10.1007/s00277-007-0373-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aryal KR, Al-Khaffaf H. Venous thromboembolic complications following air travel: what's the quantitative risk? A literature review. Eur J Vasc Endovasc Surg. 2006;31:187–199. doi: 10.1016/j.ejvs.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 41.Kuipers S, Schreijer AJ, Cannegieter SC, Buller HR, Rosendaal FR, Middeldorp S. Travel and venous thrombosis: a systematic review. J Intern Med. 2007;262:615–634. doi: 10.1111/j.1365-2796.2007.01867.x. [DOI] [PubMed] [Google Scholar]
- 42.Tasker A, Akinola O, Cohen AT. Review of venous thromboembolism associated with air travel. Travel Med Infect Dis. 2004;2:75–79. doi: 10.1016/j.tmaid.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 43.Cesarone MR, Belcaro G, Nicolaides AN. Venous thrombosis from air travel: the LONFLIT3 study—prevention with aspirin vs low-molecular-weight heparin (LMWH) in high-risk subjects: a randomized trial. Angiology. 2002;53:1–6. doi: 10.1177/000331970205300101. [DOI] [PubMed] [Google Scholar]
- 44.Belcaro G, Cesarone MR, Shah SS. Prevention of edema, flight microangiopathy and venous thrombosis in long flights with elastic stockings. A randomized trial: The LONFLIT 4 Concorde Edema-SSL Study. Angiology. 2002;53:635–645. doi: 10.1177/000331970205300603. [DOI] [PubMed] [Google Scholar]
- 45.Lapostolle F, Surget V, Borron SW. Severe pulmonary embolism associated with air travel. N Engl J Med. 2001;345:779–783. doi: 10.1056/NEJMoa010378. [DOI] [PubMed] [Google Scholar]
- 46.Bendz B, Rostrup M, Sevre K, Andersen TO, Sandset PM. Association between acute hypobaric hypoxia and activation of coagulation in human beings. Lancet. 2000;356:1657–1658. doi: 10.1016/S0140-6736(00)03165-2. [DOI] [PubMed] [Google Scholar]
- 47.Landgraf H, Vanselow B, Schulte-Huermann D, Mulmann MV, Bergau L. Economy class syndrome: rheology, fluid balance, and lower leg edema during a simulated 12-hour long distance flight. Aviat Space Environ Med. 1994;65(10 Pt 1):930–935. [PubMed] [Google Scholar]
- 48.Simons R, Krol J. Jet leg, pulmonary embolism, and hypoxia. Lancet. 1996;348:416. doi: 10.1016/s0140-6736(05)65046-5. [DOI] [PubMed] [Google Scholar]
- 49.Schobersberger W, Fries D, Mittermayr M. Changes of biochemical markers and functional tests for clot formation during long-haul flights. Thromb Res. 2002;108:19–24. doi: 10.1016/s0049-3848(02)00347-x. [DOI] [PubMed] [Google Scholar]
- 50.Schreijer AJ, Cannegieter SC, Meijers JC, Middeldorp S, Buller HR, Rosendaal FR. Activation of coagulation system during air travel: a crossover study. Lancet. 2006;367:832–838. doi: 10.1016/S0140-6736(06)68339-6. [DOI] [PubMed] [Google Scholar]
- 51.Hsieh HF, Lee FP. Graduated compression stockings as prophylaxis for flight-related venous thrombosis: systematic literature review. J Adv Nurs. 2005;51:83–98. doi: 10.1111/j.1365-2648.2005.03463.x. [DOI] [PubMed] [Google Scholar]
- 52.Geerts WH, Bergqvist D, Pineo GF. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edn) Chest. 2008;133(suppl):381S–453S. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 53.Clarke M, Hopewell S, Juszczak E, Eisinga A, Kjeldstrom M. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst Rev. 2006 doi: 10.1002/14651858.CD004002.pub2. CD004002. [DOI] [PubMed] [Google Scholar]
- 54.Kuipers S, Cannegieter SC, Middeldorp S, Rosendaal FR, Buller HR. Use of preventive measures for air travel-related venous thrombosis in professionals who attend medical conferences. J Thromb Haemost. 2006;4:2373–2376. doi: 10.1111/j.1538-7836.2006.02204.x. [DOI] [PubMed] [Google Scholar]
- 55.Watson HG, Chee YL. Aspirin and other antiplatelet drugs in the prevention of venous thromboembolism. Blood Rev. 2008;22:107–116. doi: 10.1016/j.blre.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 56.Chee YL, Watson HG. Air travel and thrombosis. Br J Haematol. 2005;130:671–680. doi: 10.1111/j.1365-2141.2005.05617.x. [DOI] [PubMed] [Google Scholar]
- 57.Possick SE, Barry M. Evaluation and management of the cardiovascular patient embarking on air travel. Ann Intern Med. 2004;141:148–154. doi: 10.7326/0003-4819-141-2-200407200-00014. [DOI] [PubMed] [Google Scholar]
- 58.Aw JJ. Cosmic radiation and commercial air travel. J Travel Med. 2003;10:19–28. doi: 10.2310/7060.2003.30669. [DOI] [PubMed] [Google Scholar]
- 59.Barish RJ. In-flight radiation exposure during pregnancy. Obstet Gynecol. 2004;103:1326–1330. doi: 10.1097/01.AOG.0000126947.90065.90. [DOI] [PubMed] [Google Scholar]
- 60.Friedberg W, Faulkner DN, Snyder L, Darden EB, Jr, O'Brien K. Galactic cosmic radiation exposure and associated health risks for air carrier crewmembers. Aviat Space Environ Med. 1989;60:1104–1108. [PubMed] [Google Scholar]
- 61.Barish RJ. Health physics concerns in commercial aviation. Health Phys. 1990;59:199–204. doi: 10.1097/00004032-199008000-00006. [DOI] [PubMed] [Google Scholar]
- 62.Blettner M, Grosche B, Zeeb H. Occupational cancer risk in pilots and flight attendants: current epidemiological knowledge. Radiat Environ Biophys. 1998;37:75–80. doi: 10.1007/s004110050097. [DOI] [PubMed] [Google Scholar]
- 63.International Commission on Radiological Protection P103: the 2007 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 2007;37:1–332. doi: 10.1016/j.icrp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 64.Copeland K, Sauer H, Friedberg W. Solar radiation alert system. Federal Aviation Administration, US Department of Transportation, 2005, Washington, DC. http://www.faa.gov/library/reports/medical/oamtechreports/2000s/media/0514.pdf (accessed Oct 12, 2008).
- 65.Rafnsson V, Tulinius H, Jonasson JG, Hrafnkelsson J. Risk of breast cancer in female flight attendants: a population-based study (Iceland) Cancer Causes Control. 2001;12:95–101. doi: 10.1023/a:1008983416836. [DOI] [PubMed] [Google Scholar]
- 66.Reynolds P, Cone J, Layefsky M, Goldberg DE, Hurley S. Cancer incidence in California flight attendants (United States) Cancer Causes Control. 2002;13:317–324. doi: 10.1023/a:1015284014563. [DOI] [PubMed] [Google Scholar]
- 67.Rafnsson V, Sulem P, Tulinius H, Hrafnkelsson J. Breast cancer risk in airline cabin attendants: a nested case-control study in Iceland. Occup Environ Med. 2003;60:807–809. doi: 10.1136/oem.60.11.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kojo K, Pukkala E, Auvinen A. Breast cancer risk among Finnish cabin attendants: a nested case-control study. Occup Environ Med. 2005;62:488–493. doi: 10.1136/oem.2004.014738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nicholas JSCK, Duke FE, Friedberg W, O'Brien K., III . Gallactic cosmic radiation exposure of pregnant aircrew members II. US Department of Transportation, Federal Aviation Administration, Office of Aviation Medicine; 2000. [Google Scholar]
- 70.Chen J, Lewis BJ, Bennett LG, Green AR, Tracy BL. Estimated neutron dose to embryo and foetus during commercial flight. Radiat Prot Dosimetry. 2005;114:475–480. doi: 10.1093/rpd/nch493. [DOI] [PubMed] [Google Scholar]
- 71.Morgenthaler TI, Lee-Chiong T, Alessi C. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep. 2007;30:1445–1459. doi: 10.1093/sleep/30.11.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Waterhouse J, Reilly T, Atkinson G, Edwards B. Jet lag: trends and coping strategies. Lancet. 2007;369:1117–1129. doi: 10.1016/S0140-6736(07)60529-7. [DOI] [PubMed] [Google Scholar]
- 73.Srinivasan V, Spence DW, Pandi-Perumal SR, Trakht I, Cardinali DP. Jet lag: therapeutic use of melatonin and possible application of melatonin analogs. Travel Med Infect Dis. 2008;6:17–28. doi: 10.1016/j.tmaid.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 74.Sadun AA, Schaechter JD, Smith LE. A retinohypothalamic pathway in man: light mediation of circadian rhythms. Brain Res. 1984;302:371–377. doi: 10.1016/0006-8993(84)90252-x. [DOI] [PubMed] [Google Scholar]
- 75.Saper CB, Lu J, Chou TC, Gooley J. The hypothalamic integrator for circadian rhythms. Trends Neurosci. 2005;28:152–157. doi: 10.1016/j.tins.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 76.Dubocovich ML. Melatonin receptors: role on sleep and circadian rhythm regulation. Sleep Med. 2007;8(suppl 3):34–42. doi: 10.1016/j.sleep.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 77.Berson DM, Dunn FA, Takao M. Phototransduction by retinal ganglion cells that set the circadian clock. Science. 2002;295:1070–1073. doi: 10.1126/science.1067262. [DOI] [PubMed] [Google Scholar]
- 78.Wright KP, Jr, Hughes RJ, Kronauer RE, Dijk DJ, Czeisler CA. Intrinsic near-24-h pacemaker period determines limits of circadian entrainment to a weak synchronizer in humans. Proc Natl Acad Sci USA. 2001;98:14027–14032. doi: 10.1073/pnas.201530198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gander PH, Kronauer RE, Graeber RC. Phase shifting two coupled circadian pacemakers: implications for jet lag. Am J Physiol. 1985;249:R704–R719. doi: 10.1152/ajpregu.1985.249.6.R704. [DOI] [PubMed] [Google Scholar]
- 80.Deacon S, Arendt J. Adapting to phase shifts I. An experimental model for jet lag and shift work. Physiol Behav. 1996;59:665–673. doi: 10.1016/0031-9384(95)02147-7. [DOI] [PubMed] [Google Scholar]
- 81.Revell VL, Eastman CI. How to trick mother nature into letting you fly around or stay up all night. J Biol Rhythms. 2005;20:353–365. doi: 10.1177/0748730405277233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sack RL, Auckley D, Auger RR. Circadian rhythm sleep disorders: part I, basic principles, shift work and jet lag disorders. An American Academy of Sleep Medicine review. Sleep. 2007;30:1460–1483. doi: 10.1093/sleep/30.11.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Herxheimer A, Petrie KJ. Melatonin for preventing and treating jet lag. Cochrane Database Syst Rev. 2001 doi: 10.1002/14651858.CD001520. CD001520. [DOI] [PubMed] [Google Scholar]
- 84.Donaldson E, Kennaway DJ. Effects of temazepam on sleep, performance, and rhythmic 6-sulphatoxymelatonin and cortisol excretion after transmeridian travel. Aviat Space Environ Med. 1991;62:654–660. [PubMed] [Google Scholar]
- 85.Reilly T, Atkinson G, Budgett R. Effect of low-dose temazepam on physiological variables and performance tests following a westerly flight across five time zones. Int J Sports Med. 2001;22:166–174. doi: 10.1055/s-2001-16379. [DOI] [PubMed] [Google Scholar]
- 86.Lagarde D, Chappuis B, Billaud PF, Ramont L, Chauffard F, French J. Evaluation of pharmacological aids on physical performance after a transmeridian flight. Med Sci Sports Exerc. 2001;33:628–634. doi: 10.1097/00005768-200104000-00018. [DOI] [PubMed] [Google Scholar]
- 87.Revell VL, Burgess HJ, Gazda CJ, Smith MR, Fogg LF, Eastman CI. Advancing human circadian rhythms with afternoon melatonin and morning intermittent bright light. J Clin Endocrinol Metab. 2006;91:54–59. doi: 10.1210/jc.2005-1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tiberge M. Time zone change syndrome. In: Billiard M, editor. Sleep: physiology, investigations and medicine. Springer Publishing; New York, NY: 2003. [Google Scholar]
- 89.Lewy AJ, Ahmed S, Jackson JM, Sack RL. Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int. 1992;9:380–392. doi: 10.3109/07420529209064550. [DOI] [PubMed] [Google Scholar]
- 90.Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9:25–39. doi: 10.1016/j.smrv.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 91.Lahti T, Terttunen J, Leppamaki S, Lonnqvist J, Partonen T. Field trial of timed bright light exposure for jet lag among airline cabin crew. Int J Circumpolar Health. 2007;66:365–369. doi: 10.3402/ijch.v66i4.18280. [DOI] [PubMed] [Google Scholar]
- 92.Burgess HJ, Crowley SJ, Gazda CJ, Fogg LF, Eastman CI. Preflight adjustment to eastward travel: 3 days of advancing sleep with and without morning bright light. J Biol Rhythms. 2003;18:318–328. doi: 10.1177/0748730403253585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Boulos Z, Macchi MM, Sturchler MP. Light visor treatment for jet lag after westward travel across six time zones. Aviat Space Environ Med. 2002;73:953–963. [PubMed] [Google Scholar]
- 94.Moser MR, Bender TR, Margolis HS, Noble GR, Kendal AP, Ritter DG. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol. 1979;110:1–6. doi: 10.1093/oxfordjournals.aje.a112781. [DOI] [PubMed] [Google Scholar]
- 95.Marsden AG. Outbreak of influenza-like illness [corrected] related to air travel. Med J Aust. 2003;179:172–173. doi: 10.5694/j.1326-5377.2007.tb01296.x. [DOI] [PubMed] [Google Scholar]
- 96.Amornkul PN, Takahashi H, Bogard AK, Nakata M, Harpaz R, Effler PV. Low risk of measles transmission after exposure on an international airline flight. J Infect Dis. 2004;189(suppl 1):S81–S85. doi: 10.1086/377698. [DOI] [PubMed] [Google Scholar]
- 97.Olsen SJ, Chang HL, Cheung TY. Transmission of the severe acute respiratory syndrome on aircraft. N Engl J Med. 2003;349:2416–2422. doi: 10.1056/NEJMoa031349. [DOI] [PubMed] [Google Scholar]
- 98.Wilder-Smith A, Leong HN. A case of in-flight transmission of severe acute respiratory syndrome (SARS): SARS serology positive. J Travel Med. 2004;11:130. doi: 10.2310/7060.2004.17091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.McFarland JW, Hickman C, Osterholm M, MacDonald KL. Exposure to Mycobacterium tuberculosis during air travel. Lancet. 1993;342:112–113. [PubMed] [Google Scholar]
- 100.Exposure of passengers and flight crew to Mycobacterium tuberculosis on commercial aircraft, 1992–1995. MMWR Morb Mortal Wkly Rep. 1995;44:137–140. [PubMed] [Google Scholar]
- 101.Tauxe RV, Tormey MP, Mascola L, Hargrett-Bean NT, Blake PA. Salmonellosis outbreak on transatlantic flights; foodborne illness on aircraft: 1947–1984. Am J Epidemiol. 1987;125:150–157. doi: 10.1093/oxfordjournals.aje.a114498. [DOI] [PubMed] [Google Scholar]
- 102.McMullan R, Edwards PJ, Kelly MJ, Millar BC, Rooney PJ, Moore JE. Food-poisoning and commercial air travel. Travel Med Infect Dis. 2007;5:276–286. doi: 10.1016/j.tmaid.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 103.Widdowson MA, Glass R, Monroe S. Probable transmission of norovirus on an airplane. JAMA. 2005;293:1859–1860. doi: 10.1001/jama.293.15.1859. [DOI] [PubMed] [Google Scholar]
- 104.Centers for Disease Control and Prevention International notes-smallpox-Stockholm. MMWR Morb Mortal Wkly Rep. 1963;12:56. [Google Scholar]
- 105.Zitter JN, Mazonson PD, Miller DP, Hulley SB, Balmes JR. Aircraft cabin air recirculation and symptoms of the common cold. JAMA. 2002;288:483–486. doi: 10.1001/jama.288.4.483. [DOI] [PubMed] [Google Scholar]
- 106.Luna LK, Panning M, Grywna K, Pfefferle S, Drosten C. Spectrum of viruses and atypical bacteria in intercontinental air travelers with symptoms of acute respiratory infection. J Infect Dis. 2007;195:675–679. doi: 10.1086/511432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.WHO . Tuberculosis and air travel: guidelines for prevention and control. 2nd edn. World Health Organization; Geneva: 2006. WHO/HTM/TB/2006.363. [PubMed] [Google Scholar]
- 108.WHO . Department of Communicable disease Surveillance and Response. Consensus document on the epidemiology of severe respiratory distress syndrome (SARS). WHO/CDS/CSR/2003.11. World Health Organization; Geneva: 2003. [Google Scholar]
- 109.Germann TC, Kadau K, Longini IM, Jr, Macken CA. Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci USA. 2006;103:5935–5940. doi: 10.1073/pnas.0601266103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cooper BS, Pitman RJ, Edmunds WJ, Gay NJ. Delaying the international spread of pandemic influenza. PLoS Med. 2006;3:e212. doi: 10.1371/journal.pmed.0030212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Brownstein JS, Wolfe CJ, Mandl KD. Empirical evidence for the effect of airline travel on inter-regional influenza spread in the United States. PLoS Med. 2006;3:e401. doi: 10.1371/journal.pmed.0030401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cocks R, Liew M. Commercial aviation in-flight emergencies and the physician. Emerg Med Australas. 2007;19:1–8. doi: 10.1111/j.1742-6723.2006.00928.x. [DOI] [PubMed] [Google Scholar]
- 113.Tonks A. Cabin fever. BMJ. 2008;336:584–586. doi: 10.1136/bmj.39511.444618.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.DeJohn CA, Wolbrink AM, Veronneau SJ, Larcher JG, Smith DW, Garrett JS. An evaluation of in-flight medical care in the U.S. Aviat Space Environ Med. 2002;73:580–586. [PubMed] [Google Scholar]
- 115.Thibeault C, Evans A. Emergency medical kit for commercial airlines: an update. Aviat Space Environ Med. 2007;78:1170–1171. doi: 10.3357/asem.2188.2007. [DOI] [PubMed] [Google Scholar]
- 116.Pierson K, Power Y, Marcus A, Dahlberg A. Airline passenger misconduct: management implications for physicians. Aviat Space Environ Med. 2007;78:361–367. [PubMed] [Google Scholar]
- 117.Dowdall N. “Is there a doctor on the aircraft?” Top 10 in-flight medical emergencies. BMJ. 2000;321:1336–1337. doi: 10.1136/bmj.321.7272.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wyatt J, Illingworth RN, Clancy M, Munro PT, Robertson CE. Oxford Handbook of Accident and Emergency Medicine. 2nd ed. Oxford University Press; Oxford: 2005. [Google Scholar]
- 119.Jorge A, Pombal R, Peixoto H, Lima M. Preflight medical clearance of ill and incapacitated passengers: 3-year retrospective study of experience with a European airline. J Travel Med. 2005;12:306–311. doi: 10.2310/7060.2005.12602. [DOI] [PubMed] [Google Scholar]
- 120.Zahger D, Leibowitz D, Tabb IK, Weiss AT. Long-distance air travel soon after an acute coronary syndrome: a prospective evaluation of a triage protocol. Am Heart J. 2000;140:241–242. doi: 10.1067/mhj.2000.107998. [DOI] [PubMed] [Google Scholar]
- 121.World Health Organization International travel and health. Situation as of 1 January 2005. Geneva, 2005. http://whqlibdoc.who.int/publications/2005/9241580364.pdf (accessed Oct 12, 2008).
- 122.Roby H, Lee A, Hopkins A. Safety of air travel following acute myocardial infarction. Aviat Space Environ Med. 2002;73:91–96. [PubMed] [Google Scholar]
- 123.International Air Transport Association Medical Manual 1st ed. International Air Transport Association, Montreal, Canada. 2004. http://www.iata.org/NR/rdonlyres/F38C6572-2215-411D-BF7E-B1238FC83696/0/medical_manual_june2004_edition_updated_nov07.pdf (accessed Oct 12, 2008).
- 124.Aviation Consumer Protection Division . Fact sheet: steps taken to ensure new security requirements preserve and respect the civil rights of people with disabilities. Department of Transportation; Washington, DC: 2001. http://www.dot.gov/airconsumer/Civil%20Rights%20Fact%20Sheet.htm (accessed Oct 12, 2008). [Google Scholar]
- 125.Teichman PG, Donchin Y, Kot RJ. International aeromedical evacuation. N Engl J Med. 2007;356:262–270. doi: 10.1056/NEJMra063651. [DOI] [PubMed] [Google Scholar]
- 126.Lindgren T, Norback D. Health and perception of cabin air quality among Swedish commercial airline crew. Indoor Air. 2005;15(suppl 10):65–72. doi: 10.1111/j.1600-0668.2005.00353.x. [DOI] [PubMed] [Google Scholar]
- 127.Evans A, Finkelstein S, Singh J, Thibeault C. Pandemic influenza: a note on international planning to reduce the risk from air transport. Aviat Space Environ Med. 2006;77:974–976. [PubMed] [Google Scholar]
- 128.ICAO Guidelines for states concerning the management of communicable disease posing a serious public health risk. International Civil Aviation Orgaization, Montreal Canada. 5 July 2007. http://www.icao.int/icao/en/med/guidelines.htm (accessed Oct 12, 2008).