Abstract
Religious festivals attract a large number of pilgrims from worldwide and are a potential risk for the transmission of infectious diseases between pilgrims, and to the indigenous population. The gathering of a large number of pilgrims could compromise the health system of the host country. The threat to global health security posed by infectious diseases with epidemic potential shows the importance of advanced planning of public health surveillance and response at these religious events. Saudi Arabia has extensive experience of providing health care at mass gatherings acquired through decades of managing millions of pilgrims at the Hajj. In this report, we describe the extensive public health planning, surveillance systems used to monitor public health risks, and health services provided and accessed during Hajj 2012 and Hajj 2013 that together attracted more than 5 million pilgrims from 184 countries. We also describe the recent establishment of the Global Center for Mass Gathering Medicine, a Saudi Government partnership with the WHO Collaborating Centre for Mass Gatherings Medicine, Gulf Co-operation Council states, UK universities, and public health institutions globally.
This is the first in a Series of three papers about mass gatherings medicine
Introduction
Religious events and festivals can be attended by large numbers of pilgrims from within and outside the host country, geographic region, or continent.1, 2, 3, 4, 5 One of the major public health concerns in relation to mass gatherings is the importation or exportation of infectious diseases, and spread between attendees and to the local population.6, 7, 8, 9 The gathering of huge numbers of pilgrims can compromise the health system of the host countries.10, 11, 12, 13 Additionally, the threat to global health security posed by infectious diseases that might be exported to the pilgrims' home country shows the importance of advance planning, global communication, public health surveillance, and response at religious mass gatherings.14, 15, 16, 17, 18
The Hajj or pilgrimage to Makkah, Saudi Arabia, is one of the largest yearly religious mass gatherings worldwide, with more than 2 million people from more than 184 countries.1, 2 Hajj is one of the obligatory five pillars of Islam—a duty that all physically healthy, able-bodied adult Muslims must undertake once in their lifetimes if they can afford it,1, 2 and is undertaken over 5 days during Dhul Hijjah 8–12, the 12th month of the Islamic calendar (figure 1 ). The proximity between pilgrims due to the crowded accommodation, congregation, and prayers creates an ideal environment for transmission of infectious diseases, many of which are preventable if appropriate measures are taken. In this report, we describe the extensive public health planning and surveillance systems that were used to monitor public health risks, and provision of and access to health services during Hajj 2012 and Hajj 2013, which together attracted more than 5 million pilgrims from 184 countries.
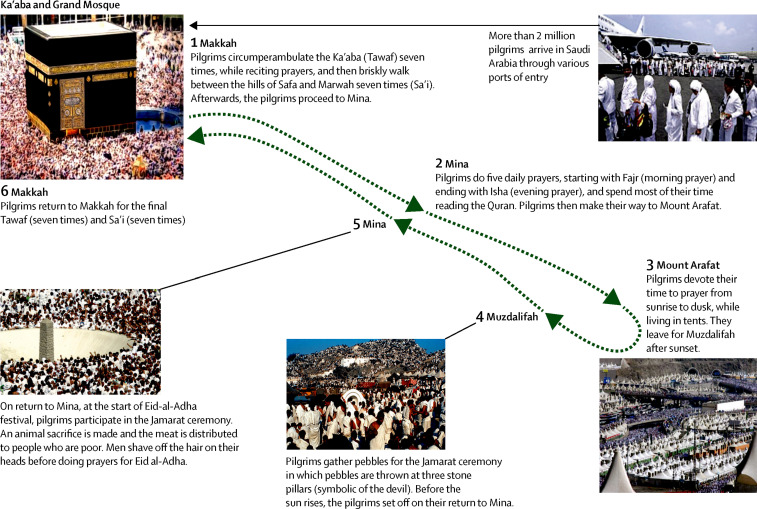
Figure 1.
Stages of the Hajj
For the Hajj, pilgrims wear simple garments (white for male pilgrims), do prayers, and undertake a series of rituals and rites together as an expression of unity, equality, and solidarity irrespective of nationality, ethnic origin, sex, and social class. Pilgrims fulfil each of the required prayer rituals by visiting and doing prayers in a particular order at several of the holy sites in Makkah, commencing at the Ka'aba. Although most pilgrims walk during the Hajj, some may use transport (eg, bus or trains) and those who have a disability or are elderly are pushed along in wheelchairs or carried on the shoulders of other pilgrims.
Hajj and Umrah
Every year more than 10 million pilgrims from 184 countries arrive at Makkah for the Hajj or the Umrah. The Umrah is also a pilgrimage to Makkah, but of shorter duration than the Hajj and can be made at any time of the year. The busiest period for the Umrah is during Ramadan, the month of fasting, which is about 3 months before the Hajj. Although during the Hajj, pilgrims visit the holy cities Makkah and Medina, Saudi Arabia, the strict definition of Hajj only applies to the pilgrimage to Makkah. The lunar calendar is 10 days or 11 days shorter than the Gregorian version used in the west. Thus, the Hajj moves forward by 10 days or 11 days every year according to the Gregorian calendar.
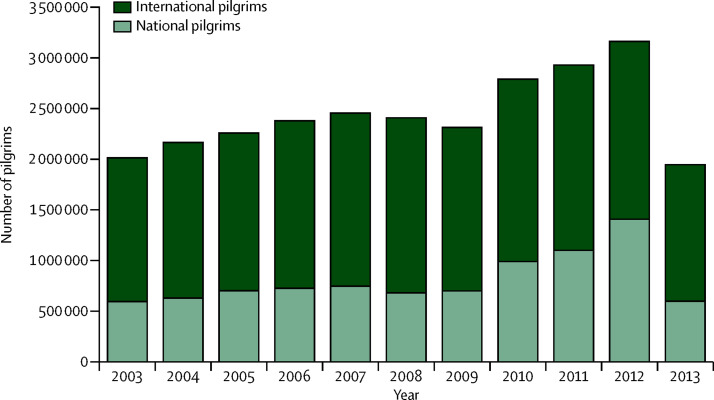
The number of pilgrims undertaking the Hajj has increased from 58 584 in 1920 to 3 161 573 in 2012 (1 752 932 from outside Saudi Arabia). Because of the continued expansion of the Grand Mosque, which surrounds the Ka'aba in Makkah, to accommodate the increasing numbers of pilgrims, the Saudi Government issued permits to pilgrims for Hajj 2013. These permits led to reductions in the number of pilgrims from Saudi Arabia and other countries (figure 2 ). Thus, for Hajj 2013, 1 343 995 international pilgrims visited Saudi Arabia through the 16 ports of entry (94% through the two airports at Jeddah and Medina, 5% through the 11 land ports, and 1% through the three sea ports).
Figure 2.
Number of pilgrims attending the Hajj from 2003 to 2013
Data are from the Saudi Ministry of Hajj19 and Central Department of Statistics and Information.20
Pre-Hajj public health preparedness
The Saudi Government has a well established system for the planning, communication, security, health, safety, and administrative issues in relation to the Hajj. To minimise the health risks to the pilgrims, the Saudi Ministry of Health liaises with governments of all countries from which pilgrims visit Makkah and Medina throughout the year. The public health measures for Hajj are focused on provision of safe water and food supplies, sanitation, vector control, pre-travel health regulations and advice about vaccinations, health checks, and specific immunisation at the port of entry, health education campaigns, and provision of free health care to pilgrims through several clinics and hospitals. A proactive public health programme is initiated before each Hajj, with focus on prevention and surveillance of health hazards, and health-care provision during the pilgrimage. Before each Hajj, the Saudi Ministry of Health disseminates the health requirements for issuance of travel visas, and provides advice about public health guidelines to prevent the spread of respiratory and gastrointestinal infections.21, 22, 23, 24, 25 This advice is re-enforced with widespread health education and prevention campaigns through reading materials, travel agents, pilgrims' group leaders, and media communication during the Hajj.
Infectious disease alert and response
The Hajj poses enormous logistical and planning challenges for the protection of the health of pilgrims21, 22, 23, 24, 25, 26, 27 and Saudi residents and for the maintenance of national and global health security. The Saudi Government's success in alert and response planning for infectious diseases is attributable to a multidisciplinary group of experts from various government sectors who are involved in the advance planning of health services, logistical support, and communications for the Hajj. Continuous monitoring of emerging infectious diseases ensures that, for example, infection with the Middle East respiratory syndrome coronavirus (MERS-CoV) in an individual28 is not transmitted to other pilgrims, thereby avoiding a worldwide epidemic. The Saudi Government coordinates the Hajj activities through a supreme committee and 24 subcommittees for the Hajj.16, 19 For Hajj 2012 and Hajj 2013, the three key planning considerations by the Saudi Government for communicable disease alert and response during the pilgrimage, based on WHO's recommendations for communicable disease alert and response during mass gatherings,29 were risk assessment of what might happen during the Hajj, proactive surveillance for communicable diseases especially because of outbreaks of MERS-CoV and other viral diseases, and response and action. Additionally, input about outbreak management and emerging diseases is provided by WHO, the European Centre for Disease Prevention and Control, UK's Public Health England, and the US Centers for Disease Control and Prevention through the Saudi Public Health Directorate of the Ministry of Health. Thus, a major global effort is needed to maintain the highest level of public health services and increased risk awareness of infectious diseases during the Hajj.
Advance planning
Early preparations for Hajj are undertaken by the Saudi Ministry of Hajj and Ministry of Health.19 Like other years, planning for Hajj 2012 and Hajj 2013 began soon after the end of the previous Hajj with a wide range of feedback in relation to the application of the previous year's public health programme. Additionally, information from monitoring and evaluation of the prevalence and emergence of infectious diseases globally, regionally, and locally is taken into account to develop the public health programme for alert and response for the next Hajj. The planning and management team consists of several multidisciplinary committees (security authorities, civil defence, education authorities, mosques, Saudi Red Crescent Authority, the Custodian of the Two Holy Mosques Institute of the Hajj Research at Umm Al-Qura University, Makkah, and the municipality of Makkah). The response team continuously assesses the global, regional, and local infectious disease patterns and has plans in place for quarantine of any imported threats of infectious diseases.
The Ministry of Health and Ministry of Hajj provide regular updates about Hajj travel advice and health regulations for pilgrims and these are posted on the Ministry of Health's website. They also disseminate this advice through liaising closely with international public health agencies including WHO, Public Health England, the Centers for Disease Control and Prevention, and the European Centre for Disease Prevention and Control, and many religious groups, organisations, and travel agencies that provide Hajj and Umrah services. Regular bulletins also draw attention to any new threats of disease to pilgrims.
Gastrointestinal infections
During any mass gathering, including the Hajj, gastrointestinal infections are a major health hazard. Continuous surveillance of the threat of food poisoning and spread of several viral, bacterial, and protozoal pathogens is done routinely as part of the public health response for the Hajj. Many factors can have a role in causing gastrointestinal infections, including inadequate standards of food preparation, poor personal hygiene, contaminated water supply, the presence of asymptomatic carriers of pathogenic bacteria and parasites, and the large numbers of meals prepared and poorly stored by pilgrims. Public health measures at the Hajj are focused on provision of safe water and food supplies, sanitation, and vector control. A committee for the security control of main water sources in Makkah and the other holy sites does thorough inspections of the quality of drinking water. A daily inspection tour of water treatment plants is done to ensure that the chlorine pumping equipments function properly. Inspections of all main water supply sources and water tanks at various locations including schools, government departments, houses, mosques, hotels, and food stores in Makkah and the other holy sites are done throughout the year.
A committee for the removal of treated sewage water liaises with the Ministry of Health to ensure the safety of produce from irrigated vegetable farms. A thorough survey is done of kitchen workers at hotels and hospitals to identify potential carriers of gut pathogens and to ensure standards of food hygiene are maintained. All kitchens and samples of food and water are inspected to ensure compliance with the health regulations. Additionally, swabs from utensils and throats and nails of the people working in the kitchens are tested for the presence of pathogens. As a precaution, the Ministry of Health strongly enforces the regulation that pilgrims are not allowed to bring fresh food or agricultural products into Saudi Arabia.
Vector-borne diseases
Aedes, Culex, and Anopheles spp mosquitoes are present in Saudi Arabia and are vectors for transmission of arboviruses and malaria,30 thus necessitating a widespread vector control programme that includes a routine and widespread insecticide spraying campaign. For the Hajj, this programme is intensified and the Ministry of Health liaises closely with the Ministry of Public Health and Ministry of Agriculture in Makkah to coordinate and assess pest control, identify the zones and density of mosquitoes, and undertake insecticide spraying campaigns. Specific teams spray housing units earmarked for pilgrims who come from dengue-endemic areas such as India, Pakistan, and Bangladesh with longlasting pesticide before the arrival of the pilgrims. The teams also spray government departments, and all field accommodation used by pilgrims such as tents at the holy sites with a longlasting pesticide. Also, insecticide is sprayed aerially over Arafat and Mina. In accordance with the international health regulations, all aircraft and ship carriers are required to provide an official valid carrier sanitation certificate to verify that insecticide spraying was done before arrival at the port.
Health education and awareness
The diverse cultural, ethnic, and language differences of the pilgrims are taken into consideration in the educational and health awareness campaigns for the prevention of communicable diseases during Hajj. The Ministry of Health liaises with relevant stakeholders (travel agents, Muslim councils, and tour organisers) in the countries where the pilgrims come from to develop appropriate material for education and information including requirements for vaccinations and the precautions to be taken before travel and during the Hajj.22, 23, 24, 25 Various health educational materials (guides, pocket cards, stickers, leaflets, and posters) that are written in English, Arabic, Urdu, and several other languages and include images and sign language are distributed to all sites and to all pilgrims in Makkah and Medina.
Vaccination requirements
To keep the health risks to pilgrims to a minimum and to prevent importation or acquisition of communicable diseases during travel (panel ), the Ministry of Health issues its own health regulations,22, 23, 24, 25 which are updated every year. Before an entry visa for Hajj or Umrah can be issued, pilgrims are required to meet both sets of health regulations. The requirements for Hajj 2012 and Hajj 2013 included vaccinations against yellow fever, meningitis, and polio.
Panel. Major health risks to the pilgrims and the local population at all stages of the Hajj.
Health risks
Infectious diseases
-
•
Influenza viruses
-
•
Coronaviruses
-
•
Pneumococcal sepsis
-
•
Tuberculosis
-
•
Meningococcal sepsis
-
•
Polio
-
•
Yellow fever
-
•
Gasterointestinal infections
-
•
Acute gasteroenteritis (eg, Salmonella spp, Campylobacter spp)
-
•
Food poisoning (eg, Bacillus cereus)
-
•
Cholera, typhoid, and dysentery
-
•
Viral diarrhoea (eg, rotavirus and norovirus)
-
•
Viral hepatitis B, C, D, and E
-
•
Arboviral infections—eg, haemorrhagic fevers and Alkhurma virus
-
•
Parasitic—eg, malaria, scabies, gut parasites, nematodes, trematodes, and cestodes
-
•
Fungal—eg, Tinea spp skin infections
-
•
Blood-borne diseases
-
•
HIV
-
•
Bacterial (other)
-
•
Zoonoses
-
•
Brucellosis
-
•
Leishmaniasis
Heat-related disorders
-
•
Skin milia
-
•
Heat hyperpyrexia
-
•
Heat stroke
Other
-
•
Fires
-
•
Stampedes
-
•
Crush injuries
Prevention
Vaccination (before travelling and at port of entry)
-
•
Influenza
-
•
Meningococcal (ACYW135)
-
•
Polio (mandatory for all pilgrims from countries or areas at risk)
-
•
Pneumococcal
-
•
Rabies
-
•
Hepatitis B
-
•
Cholera
-
•
Typhoid
-
•
Tetanus
-
•
Yellow fever (mandatory for all pilgrims from countries or areas at risk)
Other types
-
•
Ciprofloxacin
-
•
Antimalarial drugs
-
•
Face masks
-
•
Hand and toilet hygiene
Advice
-
•
Health education leaflets and posters
-
•
General education about hygiene, hydration, shelter from direct heat, and seeking and accessing health services
Special precautions
-
•
Sterile shaving blades should be used for the head-shaving ceremony
-
•
Pilgrims with comorbidities (eg, diabetes), or on immunosuppressive agents are more likely to acquire and succumb to infectious diseases
-
•
As new infectious disease threats emerge, recommendations are updated on a regular basis22, 23, 24, 25
All travellers arriving from countries in Africa, South America, and Central America must present a valid vaccination certificate for yellow fever at the border. Individuals without such a certificate will be offered the vaccine and then observed for 10 days. All aircraft, ships, and other vehicles arriving from countries with a prevalence of yellow fever are required to have a valid certificate indicating that disinsection has been done according to WHO's recommendations to eradicate all insect vectors of disease. For Hajj 2013, compliance with vaccination against yellow fever for pilgrims from countries at risk was more than 99%.19
To reduce the risk of invasive meningococcal disease, experts from 11 countries in the Middle East recommended vaccination with the quadrivalent conjugate meningococcal vaccine (ACYW135).31, 32 Adults and children (aged >2 years) are given one dose of the quadrivalent polysaccharide ACYW135 vaccine. Pilgrims arriving from countries in the African meningitis belt—namely, Benin, Burkina Faso, Cameroon, Chad, Central African Republic, Côte d'Ivoire, Eritrea, Ethiopia, The Gambia, Guinea, Guinea-Bissau, Mali, Niger, Nigeria, Senegal, and Sudan—in addition to the vaccination, are given ciprofloxacin tablets at the port of entry to reduce the prevalence of carriers of Neisseria meningitidis. Quadrivalent vaccination is given to pilgrims from within Saudi Arabia, residents of Makkah and Medina and Saudi Government staff who work during the Hajj.
For immunisation against polio, all pilgrims younger than 15 years who travel from countries where polio is reported to be prevalent are expected to be vaccinated against the infection.24, 25 Irrespective of previous immunisation, a single dose of the polio vaccine is administered to pilgrims on arrival to Saudi Arabia from countries where polio has been reported. The number of pilgrims vaccinated against polio at port of entry is about 500 000.5 For Hajj 2013, 430 490 doses of polio vaccine were administered at ports of entry to 99% of eligible pilgrims.19
For seasonal influenza, the Saudi Ministry of Health recommends vaccination, particularly for people at increased risk of severe influenza—ie, pregnant women, children younger than 5 years, elderly people, and individuals who are immunosuppressed or have HIV/AIDS, asthma, or chronic heart or lung diseases. Seasonal influenza vaccination is recommended for pilgrims from within Saudi Arabia, particularly those who have the risk factors described above, and all Saudi health-care workers in Makkah and Medina.
For MERS-CoV, the Saudi Ministry of Health introduced recommendations28 for Hajj 2013 based on the clinical, epidemiological, and scientific data33, 34, 35 that were generated by the Saudi Global Center for Mass Gathering Medicine. According to current recommendations that are reviewed yearly, because of the high mortality rates associated with MERS-CoV infection, people with the following risk factors should postpone Hajj or Umrah for their own safety: individuals who are older than 65 years of age; individuals who have chronic diseases including diabetes, heart disease, kidney disease, respiratory disease, autoimmune disease, or immune deficiency (congenital and acquired); people who are taking immunosuppressive drugs; individuals who have a malignant disease or a terminal illness; pregnant women; and children younger than 12 years. Furthermore, the Saudi Ministry of Health also advises all pilgrims to comply with the common public health guidelines to prevent the spread of respiratory infections.
The Saudi Ministry of Health closely monitors pilgrims' compliance with the international health regulations at all ports of entry—sea, land, and air. The largest numbers of pilgrims arrive through five main ports including King Abdulaziz Airport in Jeddah, Prince Mohammad Airport in Medina, and Hallat Ammar ground crossing in Tabouk. The immunisation status of each pilgrim is checked and, if relevant, appropriate vaccines and antibiotics are administered in clinical examination rooms and holding areas at the main hubs of the international airport terminals for the Hajj.
Information technology and surveillance
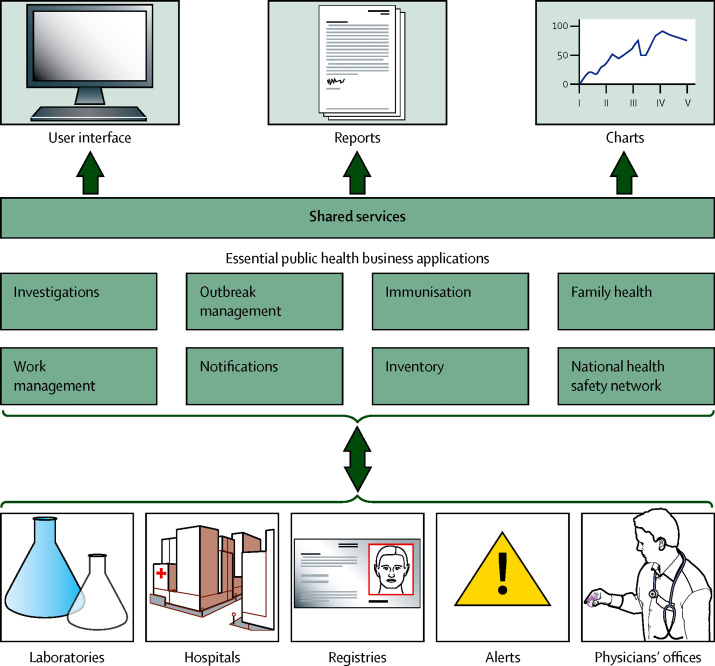
During Hajj, Saudi Arabia provides free medical care to all pilgrims in 25 hospitals with 5000 beds, including 500 beds for critical care. All communicable diseases of importance at mass gatherings are monitored—eg, respiratory tract infections, food poisoning, diarrhoeal diseases, invasive meningococcal disease, viral haemorrhagic fevers (dengue, Alkhurma, Marburg, Crimean Congo, Ebola, and Lassa), yellow fever, polio, and plague. The Command and Control Centre in Makkah uses the latest electronic health surveillance systems for rapid communication, and efficiently initiates appropriate responses during Hajj. The web-based health-care surveillance network (figure 3 ) is used by the Command and Control Centre and is organised into eight main components: investigations, outbreak management, immunisation, family health, notifications, work management, inventory, and national health safety network.
Figure 3.
Web-based health-care surveillance network
Information technology plays an essential part in the gathering of information in a database, from where it can be accessed for statistical analyses and decision making. All end-user surveillance stations gather and send data to the Hajj operation team at the Command and Control Centre through the major local area networks that connect all end-user stations with both wired and wireless connections to the centre. These end-user stations are hospitals, clinics, and medical centres in Mina, Arafat, and Muzdalifah. The information technology system gathers data, does the statistical analysis, and displays and transfers the results to the Command and Control Centre. These results are displayed on the video wall and interactive board. A digital pen was used in 2012 to convert the conventional paper-based system into a digital system for provision of demographic and medical data. Thus, the entire demographic and health data for each case can be captured and relayed rapidly. Information technology is also used by the ambulance information system to record data about medical and administrative procedures done by ambulance staff on patients. The data are transferred swiftly to the hospital emergency departments before the arrival of patients.
Hajj-related outbreaks
Several outbreaks of infectious diseases have been recorded at the Hajj. The first such recorded outbreak was in 632 AD, when malaria was originally called yethrib fever.36 A realisation of the adverse implications of the threat of malaria to public health at the Hajj focused the attention of the Saudi Government on enforcing the regional malaria eradication programme.30
A wide range of viral and bacterial infections of the upper and lower respiratory tract can occur during the Hajj.37, 38, 39, 40, 41, 42, 43, 44, 45, 46 Bacterial and viral pneumonia are common causes of hospital admission in pilgrims.39, 40, 43, 44 Factors that contribute to the spread of these pathogens include proximity between pilgrims, shared accommodation, and dust in the environment. Transmission of tuberculosis during Hajj is difficult to ascertain because of the long incubation.41, 47 The risk of tuberculosis during the Hajj is estimated to be about 10% based on data from before and after screening visits for latent infection with Mycobacterium tuberculosis.48 Most pilgrims come from areas that are highly endemic for tuberculosis49 and many travel to Makkah with active disease or infection that is reactivated by stress. Pulmonary tuberculosis was a leading cause of hospital admission in patients with community-acquired pneumonia. Strategies to reduce the transmission of tuberculosis during the Hajj and development of an evidence base for appropriate intervention measures remains one of the priorities for the Saudi Ministry of Health.
Over the past decade, the emergence of several new coronaviruses and influenza viruses such as influenza A H1N1, severe acute respiratory syndrome (SARS)-CoV, and MERS-CoV have been a concern for the Saudi Ministry of Health. However, no major outbreaks have occurred at the Hajj as shown by the results of a cohort study of French pilgrims in 2012.50 In 2009, fewer than 100 cases of influenza A H1N1 were reported during Hajj at the peak of the pandemic, and only 26 confirmed cases during Umrah.51 In another study, no influenza A H1N1 infection was detected in 559 pilgrims.52 The results of this study, however, showed rapid infection with respiratory viruses and bacteria, particularly rhinovirus and Streptococcus pneumoniae. The Saudi Ministry of Health is assessing vaccines for prevention of pneumococcal infections.53 The ministry is also in the process of defining the exact burden of pneumococcal sepsis (pneumonia, meningitis, or invasive disease) during Hajj.53 Pneumococcal vaccines (polyvalent), specifically for people older than 65 years and those with splenectomy, are available. Additionally, other forms of prevention are widely available and are known to reduce the burden of disease associated with S pneumoniae. Although the effectiveness of pneumococcal vaccination for the prevention of S pneumoniae infections in elderly pilgrims is yet to be ascertained, these individuals might benefit from vaccination with the polyvalent pneumococcal vaccine for the common pneumococcal serotypes that are circulating during Hajj.
MERS-CoV surveillance
In September, 2012, MERS-CoV was first identified as a new virus that causes fatal respiratory disease after identification of a novel β coronavirus from a patient in Jeddah, Saudi Arabia, who died from a severe respiratory illness.54 By the end of March, 2013, 6 months after MERS-CoV was discovered, only 17 cases of MERS-CoV infection were reported globally55—including, nine from Saudi Arabia and four from one family case-cluster.56 Alarmist media reports after the detection of cases of MERS-CoV infection in the UK,57 France,58 Germany,59 and Italy60 resulted in international attention and intense scientific, political, and media activity over the pandemic potential of MERS-CoV because of the next Hajj. Since the first case report of MERS-CoV infection, the Saudi Government and other governments in the Middle East have continued proactive surveillance with immediate reporting of cases of MERS-CoV infection to WHO. Increased surveillance during Hajj 2012 and Hajj 2013 was achieved with a MERS-CoV response team monitoring and gathering data at all clinics and hospitals in Arafat, Makkah, Mina, Muzdalifah, and Medina.
During Hajj 2012 and Hajj 2013, no cases of MERS-CoV infection were detected. Also, no cases were reported after pilgrims returned home. In a cohort study of 154 French pilgrims from whom nasal swabs were obtained before they returned to France, 83% had respiratory symptoms, but none tested positive for MERS-CoV infection.50 58% of the French pilgrims in 2012 and 29% in 2013 had comorbidities that increased their risk of MERS-CoV infection.50 By the end of 2013, no cases of MERS-CoV infection were reported in 5 million pilgrims who undertook the Umrah.
Invasive meningococcal disease
The crowded conditions at the Hajj increase the risk of transmission of N meningitidis and the development of invasive meningococcal disease. Two major outbreaks of Hajj-related meningococcal disease have been reported in Saudi Arabia.61, 62 In 1987, during the outbreak of N meningitidis serogroup A, the incidence of infection was 640 cases per 100 000 pilgrims.61 Three interventions were implemented by the Saudi Ministry of Health after the outbreaks: introduction of compulsory vaccination with bivalent A + C vaccine for all pilgrims (national or international), yearly vaccination campaigns for all people living near the pilgrimage sites, and compulsory administration of oral ciprofloxacin to pilgrims from countries in the sub-Saharan Africa meningitis belt to minimise nasopharyngeal carriage. In 1992, although an increasing number of cases of N meningitidis serogroup A infection were detected, there was no epidemic.62 During Hajj 2000 and Hajj 2001, 400 cases of a hypervirulent strain of W135 N meningitidis infection were reported in returning pilgrims and their contacts.63, 64 The Saudi Ministry of Health responded by recommending the polysaccharide quadrivalent ACYW meningococcal vaccine for children older than 2 years and adults living in Makkah and Medina, children older than 2 years accompanying their parents on Hajj from within and outside of Saudi Arabia, health-care workers in Saudi Arabia, and government personnel serving the pilgrims.
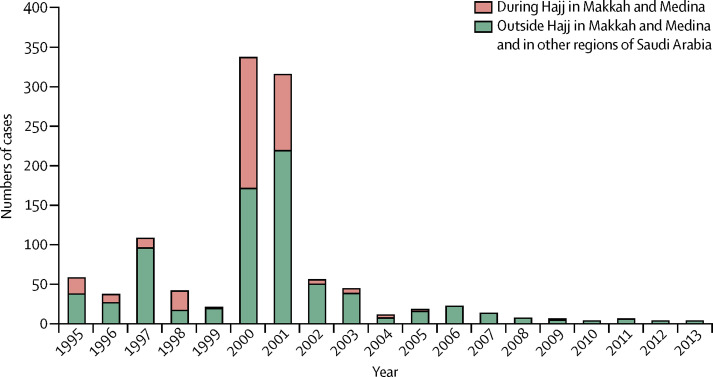
Since 2006, only one case of invasive meningococcal disease has been reported in Medina during Hajj.63 After the introduction of the ACYW vaccine in 2002, the incidence of this disease in Saudi Arabia fell over the years (figure 4 ). Concerns that mass immunisation with vaccines that do not protect against all serogroups could lead to an increase in the incidence of meningococcal disease caused by N meningitidis strains that are not included in the vaccine have not been substantiated. The Saudi surveillance data for invasive meningococcal disease showed a reduction in the number of Hajj-related cases and non-Hajj-related cases after the introduction of the ACYW vaccine in 2002.63 Continued surveillance with yearly analysis of data is necessary to bring about the adaptation of public health measures and avoid future epidemics of invasive meningococcal disease during the Hajj in subsequent years. Data from Hajj 2011 and Hajj 2012 are very encouraging and no further cases have been reported of invasive meningococcal disease.
Figure 4.
Number of cases of invasive meningococcal disease linked to Hajj from 1995 to 2013
Gastrointestinal infections
Outbreaks of gastroenteritis due to food poisoning with Salmonella spp, Staphylococcus aureus, Bacillus cereus, or Clostridium perfringens toxin are common at all religious festivals, including the Hajj.65, 66 Although no major food-borne outbreaks resulting in high mortality rates have been associated with the Hajj, gastroenteritis symptoms were reported in an Iranian group of pilgrims,67 but the cause and source have not been ascertained. There are few reports of the incidence and cause of diarrhoea during the Hajj although diarrhoea is a common cause of hospital admission.40, 44, 68 As the global cholera pandemic continues,68, 69, 70 and outbreaks in countries where pilgrims come from are frequent, cholera is under constant surveillance by the Saudi Command and Control Centre. All cases of diarrhoea and people living in the same camps as the cases are quarantined and their contacts are traced. Because pilgrims on arrival might be incubating the infectious cause of diarrhoea, the focus of public health surveillance is on proactive surveillance, early diagnosis, treatment, and contact tracing and quarantine.
Malaria
A decade ago, cases of malaria reported in pilgrims in Makkah were thought to be a reactivation of the disease in people from malaria-endemic countries or a consequence of Saudi-endemic transmission.30 Saudi Arabia is classified by WHO as a low, geographically restricted malaria transmission area and since 2008 has been listed as being in the elimination stage of the programme. The risk of Plasmodium vivax transmission has been reintroduced and is linked to the increasing number of imported cases. Nearly 75% of all reported cases were from the Indian subcontinent and Ethiopia—19 cases of P vivax malaria were imported in 2011. For Hajj 2012, only 48 cases of malaria were recorded in Makkah and 47 of these were overseas pilgrims (17 from Pakistan, seven Nigeria, five Guinea, five India, four Mauritania, three Afghanistan, one Mali, one Chad, one Somalia, one Ethiopia, one Yemen, and one Ivory Coast). 78 cases of malaria were detected in Medina during the Hajj (35 from Pakistan, 18 Nigeria, 11 India, four Mali, three Guinea, two Mauritania, two Senegal, two Sudan, and one Chad; Memish Z, unpublished).
Best evidence for public health interventions
The Hajj attracts increasing numbers of pilgrims every year. As the events in relation to the recent MERS-CoV outbreak show, the Hajj will continue to pose substantial public health challenges for health authorities in Saudi Arabia, the countries from where pilgrims travel, and worldwide. The introduction and spread of infectious diseases during and after the Hajj or any mass gathering event will remain important topics on the public health agendas for the foreseeable future. Nevertheless, the Hajj offers a great opportunity for creating a health legacy that will enable improvements in health systems and services for mass gatherings. It presents major opportunities to do high-quality cross-sectional, case-control, and longitudinal cohort studies to generate an evidence base for the development of optimum recommendations for prevention, management, and control of infectious diseases and for sustaining global health security for Hajj71 and other mass gatherings.
The Saudi Ministry of Health established the Global Center for Mass Gathering Medicine in 2012 with the headquarters in Riyadh. This centre is a virtual research network of UK academic and public health institutions in partnership with the WHO Collaborating Centre on Mass Gatherings Medicine and WHO Global Capacity Alert and Response. This unique network will undertake longitudinal and cross-sectional cohort studies, review and publish reports, and has brought together a coalition of interested partners to gather and translate an appropriate evidence base into public health policy for use by countries that host mass gatherings. So far, the Global Center for Mass Gathering Medicine has established an overarching board chaired by the Saudi Minister of Health with membership of experts from the University College London, Public Health England, WHO, Saudi Council for Health Specialties, and the Saudi national research funding agency King Abdulaziz City for Science and Technology. The Global Center for Mass Gathering Medicine has held two scientific advisory committee meetings and an international conference. The centre has already embarked on achieving its mandates by undertaking research into the MERS-CoV outbreak, tuberculosis, and HIV in Saudi Arabia.33, 34, 35, 72, 73, 74, 75 The centre's first group of ten Saudi physicians has embarked on a diploma programme for mass gatherings medicine approved by the Saudi Council for Health Specialties. The current focus of research is on MERS-CoV and other respiratory viral infections and best strategies to prevent them. Through provision of a scientific evidence base the Global Center for Mass Gathering Medicine aims to drive the best health promotion, prevention guidelines and practice, and health education for attendees at the Hajj and other mass gatherings.
Conclusions
The spread of infectious diseases at a gathering of large numbers of pilgrims within a short space of time might be expected to compromise the health system of the host country. Additionally, infectious diseases pose a threat to global health security and show the importance of planning, communication, and public health surveillance and response at these religious events. Saudi Arabia has much experience of providing health care during religious mass gatherings through decades of managing millions of pilgrims who undertake Hajj. The formation of the Global Center for Mass Gathering Medicine and its network will serve as a unique platform for providing a research evidence base and for sharing knowledge about the safeguarding and improvement of the health of attendees at mass gatherings.
Search strategy and selection criteria
We searched PubMed and Google Scholar for English-language papers that were published from 1940 to 2014, Cochrane Library from 2001 to 2013, and Embase from 2001 to 2012 with the terms “Hajj” and “mass gatherings” in combination with each of the following: “infectious diseases”, “communicable diseases”, “health services”, “planning”, “mass gatherings”, “vaccination”, and “immunisation”. We also searched for publications by WHO and the US Centres for Disease Control and Prevention for 2001–13. We reviewed studies cited in articles identified in our searches and selected those that we identified as relevant. We also had access to the Saudi Ministry of Health's Hajj reports for 2010–13.
Acknowledgments
Acknowledgments
We thank the staff at the Ministry of Health for their support; Adam Zumla, University College London School of Pharmacy, London, UK, for technical and administrative assistance. AZ acknowledges support from the European and Developing Countries Clinical Trials Partnership TB NEAT, PANACEA, and REMox grants; UBS Optimus Foundation, Switzerland; and National Institute for Health Research Biomedical Research Centre, University College London Hospitals.
Contributors
ZAM, AZ, and DH, AAAR, RFA, BM, and MB initiated the Lancet mass gatherings medicine Series as board members of the Global Center for Mass Gathering Medicine. ZAM and JAA-T wrote the first draft of this manuscript. ZAM, AZ, and JAA-T did the literature search, accessed data from the Saudi Ministry of Health reports about the Hajj, and revised the manuscript. All authors participated in finalising the manuscript.
Declaration of interests
We declare that we have no competing interests.
References
- 1.Gatrad AR, Sheikh A. Hajj: journey of a lifetime. BMJ. 2005;330:133–137. doi: 10.1136/bmj.330.7483.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kraemer JL. The Hajj: the Muslim pilgrimage to Mecca and the holy places. Hist Religions. 2000;40:198–203. [Google Scholar]
- 3.Hymavathi P. Festivals and medical relevance (with special reference to medieval Andhra society) Bull Indian Inst Hist Med Hyderabad. 1993;23:113–123. [PubMed] [Google Scholar]
- 4.Tewari S, Khan S, Hopkins N, Srinivasan N, Reicher S. Participation in mass gatherings can benefit well-being: longitudinal and control data from a North Indian Hindu pilgrimage event. PLoS One. 2012;7:e47291. doi: 10.1371/journal.pone.0047291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Tawfiq JA, Memish ZA. Mass gatherings and infectious diseases: prevention, detection, and control. Infect Dis Clin North Am. 2012;26:725–737. doi: 10.1016/j.idc.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Abubakar I, Gautret P, Brunette GW. Global perspectives for prevention of infectious diseases associated with mass gatherings. Lancet Infect Dis. 2012;12:66–74. doi: 10.1016/S1473-3099(11)70246-8. [DOI] [PubMed] [Google Scholar]
- 7.Al-Tawfiq JA, Zumla A, Memish ZA. Respiratory tract infections during the annual Hajj: potential risks and mitigation strategies. Curr Opin Pulm Med. 2013;19:192–197. doi: 10.1097/MCP.0b013e32835f1ae8. [DOI] [PubMed] [Google Scholar]
- 8.WHO Communicable disease alert and response for mass gatherings: technical workshop. Geneva, Switzerland, April 29–30, 2008. http://www.who.int/csr/resources/publications/WHO_HSE_EPR_2008_8c.pdf (accessed Feb 18, 2014).
- 9.Ahmed QA, Barbeschi M, Memish ZA. The quest for public health security at Hajj: the WHO guidelines on communicable disease alert and response during mass gatherings. Travel Med Infect Dis. 2009;7:226–230. doi: 10.1016/j.tmaid.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 10.D'Alessandro K, Leggio WJ, Jr, Al Mubaireek H. World's largest gathering. Muslim mass pilgrimage poses EMS logistical & planning challenges. JEMS. 2013;38:52–57. [PubMed] [Google Scholar]
- 11.Thackway S, Churches T, Fizzell J, Muscatello D, Armstrong P. Should cities hosting mass gatherings invest in public health surveillance and planning? Reflections from a decade of mass gatherings in Sydney, Australia. BMC Public Health. 2009;9:324. doi: 10.1186/1471-2458-9-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loncarevic G, Payne L, Kon P. Public health preparedness for two mass gathering events in the context of pandemic influenza (H1N1) 2009—Serbia, July 2009. Euro Surveill. 2009;14 doi: 10.2807/ese.14.31.19296-en. pii: 19296. [DOI] [PubMed] [Google Scholar]
- 13.Khan K, Freifeld CC, Wang J. Preparing for infectious disease threats at mass gatherings: the case of the Vancouver 2010 Olympic Winter Games. Can Med Assoc J. 2010;182:579–583. doi: 10.1503/cmaj.100093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Memish ZA, Stephens GM, Steffen R, Ahmed QA. Emergence of medicine for mass gatherings: lessons from the Hajj. Lancet Infect Dis. 2012;12:56–65. doi: 10.1016/S1473-3099(11)70337-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ebrahim SH, Memish ZA, Uyeki TM, Khoja TA, Marano N, McNabb SJ. Public health. Pandemic H1N1 and the 2009 Hajj. Science. 2009;326:938–940. doi: 10.1126/science.1183210. [DOI] [PubMed] [Google Scholar]
- 16.Al-Tawfiq JA, Smallwood CA, Arbuthnott KG, Malik MS, Barbeschi M, Memish ZA. Emerging respiratory and novel coronavirus 2012 infections and mass gatherings. East Mediterr Health J. 2013;19(suppl 1):S48–S54. [PubMed] [Google Scholar]
- 17.Shafi S, Booy R, Haworth E. Hajj: health lessons for mass gatherings. J Infect Public Health. 2008;1:27–32. doi: 10.1016/j.jiph.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Botelho-Nevers E, Gautret P. Outbreaks associated to large open air festivals, including music festivals, 1980 to 2012. Euro Surveill. 2013;18 doi: 10.2807/ese.18.11.20426-en. pii: 20426. [DOI] [PubMed] [Google Scholar]
- 19.Ministry of Hajj. Saudi Arabia Supreme Hajj Committee. http://www.hajinformation.com/main/u1.htm (accessed Jan 21, 2014).
- 20.Central Department of Statistics and Information http://www.cdsi.gov.sa/english/ (accessed April 24, 2014).
- 21.Memish ZA. The Hajj: communicable and non-communicable health hazards and current guidance for pilgrims. Euro Surveill. 2010;15 pii: 19671. [PubMed] [Google Scholar]
- 22.Al-Tawfiq JA, Memish ZA. The Hajj: updated health hazards and current recommendations for 2012. Euro Surveill. 2012;17 pii: 20295. [PubMed] [Google Scholar]
- 23.Memish ZA, Rabeeah AA. Health conditions for travellers to Saudi Arabia for the Umra and Hajj pilgrimage to Mecca: requirements for 2012 (1433) J Infect Public Health. 2012;5:113–115. doi: 10.1016/j.jiph.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Al-Ghamdi AS, Kabbash IA. Awareness of healthcare workers regarding preventive measures of communicable diseases among Hajj pilgrims at the entry point in Western Saudi Arabia. Saudi Med J. 2011;32:1161–1167. [PubMed] [Google Scholar]
- 25.Memish ZA, Al-Rabeeah AA. Health conditions of travellers to Saudi Arabia for the pilgrimage to Mecca (Hajj and Umra) for 1434 (2013) J Epidemiol Glob Health. 2013;3:59–61. doi: 10.1016/j.jegh.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johansson A, Batty M, Hayashi K, Al Bar O, Marcozzi D, Memish ZA. Crowd and environmental management during mass gatherings. Lancet Infect Dis. 2012;12:150–156. doi: 10.1016/S1473-3099(11)70287-0. [DOI] [PubMed] [Google Scholar]
- 27.Khan K, McNabb SJ, Memish ZA. Infectious disease surveillance and modelling across geographic frontiers and scientific specialties. Lancet Infect Dis. 2012;12:222–230. doi: 10.1016/S1473-3099(11)70313-9. [DOI] [PubMed] [Google Scholar]
- 28.WHO MERS-CoV Research Group State of knowledge and data gaps of Middle East respiratory syndrome coronavirus (MERS-CoV) in humans. PLoS Curr. 2013;5:1–30. doi: 10.1371/currents.outbreaks.0bf719e352e7478f8ad85fa30127ddb8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO Communicable diseases alert and response for mass gatherings. Key considerations. 2008. WHO report. http://www.who.int/csr/Mass_gatherings2.pdf (accessed Feb 18, 2014).
- 30.Snow RW, Amratia P, Zamani G. The malaria transition on the Arabian Peninsula: progress toward a malaria-free region between 1960-2010. Adv Parasitol. 2013;82:205–251. doi: 10.1016/B978-0-12-407706-5.00003-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Memish ZA, Shibl AM. Consensus building and recommendations based on the available epidemiology of meningococcal disease in Gulf Cooperation Council States. Travel Med Infect Dis. 2011;9:60–66. doi: 10.1016/j.tmaid.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 32.Shibl A, Tufenkeji H, Khalil M, Memish Z. Consensus recommendation for meningococcal disease prevention for Hajj and Umra pilgrimage/travel medicine. Meningococcal Leadership Forum (MLF) Expert Group. East Mediterr Health J. 2013;19:389–392. [PubMed] [Google Scholar]
- 33.Cotten M, Watson SJ, Kellam P. Transmission and evolution of the Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive genomic study. Lancet. 2013;382:1993–2002. doi: 10.1016/S0140-6736(13)61887-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Memish ZA, Zumla AI, Assiri A. Middle East respiratory syndrome coronavirus infections in health care workers. N Engl J Med. 2013;369:884–886. doi: 10.1056/NEJMc1308698. [DOI] [PubMed] [Google Scholar]
- 35.Assiri A, Al-Tawfiq JA, Al-Rabeeah AA. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13:752–761. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Farid MA. The pilgrimage and its implications in a regional malaria eradication programme. WHO/EMRO inter-regional conference on malaria for the Eastern Mediterranean and European regions. April 1956. World Health Organization report WHO/MAL/168.
- 37.Benkouiten S, Charrel R, Belhouchat K. Circulation of respiratory viruses among pilgrims during the 2012 Hajj pilgrimage. Clin Infect Dis. 2013;57:992–1000. doi: 10.1093/cid/cit446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meysamie A, Ardakani HZ, Ravazi SM, Doroodi T. Comparison of mortality and morbidity rates among Iranian pilgrims in Hajj 2004 and 2005. Saudi Med J. 2006;27:1049–1053. [PubMed] [Google Scholar]
- 39.Madani TA, Ghabrah TM, Albarrak AM. Causes of admission to intensive care units in the Hajj period of the Islamic year 1424 (2004) Ann Saudi Med. 2007;27:101–105. doi: 10.5144/0256-4947.2007.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Madani TA, Ghabrah TM, Al-Hedaithy MA. Causes of hospitalization of pilgrims in the Hajj season of the Islamic year 1423 (2003) Ann Saudi Med. 2006;26:346–351. doi: 10.5144/0256-4947.2006.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alzeer A, Mashlah A, Fakim N. Tuberculosis is the commonest cause of pneumonia requiring hospitalization during Hajj (pilgrimage to Makkah) J Infect. 1998;36:303–306. doi: 10.1016/s0163-4453(98)94315-8. [DOI] [PubMed] [Google Scholar]
- 42.Gautret P, Soula G, Delmont J, Parola P, Brouqui P. Common health hazard in French pilgrims during the Hajj of 2007: a prospective cohort study. J Travel Med. 2009;16:377–381. doi: 10.1111/j.1708-8305.2009.00358.x. [DOI] [PubMed] [Google Scholar]
- 43.Mandourah Y, Al-Radi A, Ocheltree AH, Ocheltree SR, Fowler RA. Clinical and temporal patterns of severe pneumonia causing critical illness during Hajj. BMC Infect Dis. 2012;12:117. doi: 10.1186/1471-2334-12-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Al-Ghamdi SM, Akbar HO, Qari YA, Fathaldin OA, Al-Rashed RS. Pattern of admission to hospitals during Muslim pilgrimage (Hajj) Saudi Med J. 2003;24:1073–1076. [PubMed] [Google Scholar]
- 45.Alherabi AZ. Impact of pH1N1 influenza A infections on the otolaryngology, head and neck clinic during Hajj 2009. Saudi Med J. 2011;32:933–938. [PubMed] [Google Scholar]
- 46.Balkhy HH, Memish ZA, Bafaqeer S, Almuneef MA. Influenza a common viral infection among Hajj pilgrims: time for routine surveillance and vaccination. J Travel Med. 2004;11:82–86. doi: 10.2310/7060.2004.17027. [DOI] [PubMed] [Google Scholar]
- 47.Al-Orainey IO. Tuberculosis infection during Hajj pilgrimage. The risk to pilgrims and their communities. Saudi Med J. 2013;34:676. 668. [PubMed] [Google Scholar]
- 48.Wilder-Smith A, Foo W, Earnest A, Paton NI. High risk of Mycobacterium tuberculosis infection during the Hajj pilgrimage. Trop Med Int Health. 2005;10:336–339. doi: 10.1111/j.1365-3156.2005.01395.x. [DOI] [PubMed] [Google Scholar]
- 49.WHO . Global tuberculosis report 2013. World Health Organization; Geneva: 2013. [Google Scholar]
- 50.Gautret P, Charrel R, Belhouchat K. Lack of nasal carriage of novel corona virus (HCoV-EMC) in French Hajj pilgrims returning from the Hajj 2012, despite a high rate of respiratory symptoms. Clin Microbiol Infect. 2013;19:e315–e317. doi: 10.1111/1469-0691.12174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ziyaeyan M, Alborzi A, Jamalidoust M. Pandemic 2009 influenza A (H1N1) infection among 2009 Hajj pilgrims from Southern Iran: a real-time RT-PCR-based study. Influenza Other Respir Viruses. 2012;6:e80–e84. doi: 10.1111/j.1750-2659.2012.00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kandeel A, Deming M, Elkreem EA. Pandemic (H1N1) 2009 and Hajj pilgrims who received predeparture vaccination. Egypt Emerg Infect Dis. 2011;17:1266–1268. doi: 10.3201/eid1707.101484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rashid H, Abdul Muttalif AR. The potential for pneumococcal vaccination in Hajj pilgrims: expert opinion. Travel Med Infect Dis. 2013;11:288–294. doi: 10.1016/j.tmaid.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 54.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 55.CDC Updated Information on the Epidemiology of Middle East respiratory syndrome coronavirus (MERS-CoV) infection and guidance for the public, clinicians, and public health authorities, 2012–2013. Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2013;62:793–796. [PMC free article] [PubMed] [Google Scholar]
- 56.Memish ZA, Zumla AI, Al-Hakeem RF, Al-Rabeeah AA, Stephens GM. Family cluster of Middle East respiratory syndrome coronavirus infections. N Engl J Med. 2013;368:2487–2494. doi: 10.1056/NEJMoa1303729. [DOI] [PubMed] [Google Scholar]
- 57.Tahir M, Gajraj R, Bardhan M. Evidence of person-to-person transmission within a family cluster of novel coronavirus infections, United Kingdom, February 2013. Euro Surveill. 2013;18 doi: 10.2807/ese.18.11.20427-en. pii: 20. [DOI] [PubMed] [Google Scholar]
- 58.Mailles A, Blanckaert K, Chaud P. First cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infections in France, investigations and implications for the prevention of human-to-human transmission, France, May 2013. Euro Surveill. 2013;18 pii: 20502. [PubMed] [Google Scholar]
- 59.Buchholz U, Muller MA, Nitsche A. Contact investigation of a case of human novel coronavirus infection treated in a German hospital, October–November 2012. Euro Surveill. 2013;18 pii: 20406. [PubMed] [Google Scholar]
- 60.Puzelli S, Azzi A, Santini MG. Investigation of an imported case of middle east respiratory syndrome coronavirus (MERS-CoV) infection in Florence, Italy, May to June 2013. Euro Surveill. 2013;18 doi: 10.2807/1560-7917.es2013.18.34.20564. pii: 20564. [DOI] [PubMed] [Google Scholar]
- 61.Aguilera JF, Perrocheau A, Meffre C. Outbreak of serogroup W135 meningococcal disease after the Hajj pilgrimage, Europe, 2000. Emerg Infect Dis. 2002;8:761–767. doi: 10.3201/eid0808.010422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Al-Gahtani YM, El Bushra HE, Al-Qarawi SM. Epidemiological investigation of an outbreak of meningococcal meningitis in Makkah (Mecca), Saudi Arabia, 1992. Epidemiol Infect. 1995;115:399–409. doi: 10.1017/s0950268800058556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Memish Z, Al Hakeem R, Al Neel O, Danis K, Jasir A, Eibach D. Laboratory-confirmed invasive meningococcal disease: effect of the Hajj vaccination policy, Saudi Arabia, 1995 to 2011. Euro Surveill. 2013;18 doi: 10.2807/1560-7917.es2013.18.37.20581. pii: 20581. [DOI] [PubMed] [Google Scholar]
- 64.Wilder-Smith A, Goh KT, Barkham T, Paton NI. Hajj-associated outbreak strain of Neisseria meningitidis serogroup W135: estimates of the attack rate in a defined population and the risk of invasive disease developing in carriers. Clin Infect Dis. 2003;36:679–683. doi: 10.1086/367858. [DOI] [PubMed] [Google Scholar]
- 65.Al-Mazrou YY. Food poisoning in Saudi Arabia. Potential for prevention? Saudi Med J. 2004;25:11–14. [PubMed] [Google Scholar]
- 66.Al-Joudi AS. An outbreak of foodborne diarrheal illness among soldiers in mina during hajj: the role of consumer food handling behaviors. J Family Community Med. 2007;14:29–33. [PMC free article] [PubMed] [Google Scholar]
- 67.Emamian MH, Mohammad Mohammadi G. An Outbreak of Gastroenteritis Among Iranian Pilgrims of Hajj during 2011. Iran Red Crescent Med J. 2013;15:317–319. doi: 10.5812/ircmj.3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.WHO/UNICEF Sierra Leone Cholera Situation in Sierra Leone, 21 September, 2012. http://www.afro.who.int/index.php?option=com_docman&task=doc_download&gid=7868<emid=259323 (accessed Jan 16, 2014).
- 69.Cholera: situation in the WHO African Region. World Health Organization Regional Office for Africa; Cité du Djoué: 22 August 2012. http://www.who.int/hac/crises/cholera_afro_22august2012.pdf (accessed Oct 4, 2012). [Google Scholar]
- 70.Shibl A, Senok A, Memish Z. Infectious diseases in the Arabian Peninsula and Egypt. Clin Microbiol Infect. 2012;18:1068–1080. doi: 10.1111/1469-0691.12010. [DOI] [PubMed] [Google Scholar]
- 71.Al Rabeeah A, Memish ZA, Zumla A. Mass gatherings medicine and global health security. Lancet. 2012;380:3–4. doi: 10.1016/S0140-6736(12)61073-3. [DOI] [PubMed] [Google Scholar]
- 72.Momattin H, Mohammed K, Zumla A, Memish ZA, Al-Tawfiq JA. Therapeutic options for Middle East respiratory syndrome coronavirus (MERS-CoV)–possible lessons from a systematic review of SARS-CoV therapy. Int J Infect Dis. 2013;17:e792–e798. doi: 10.1016/j.ijid.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Al-Hajoj S, Varghese B, Shoukri MM. Epidemiology of antituberculosis drug resistance in Saudi Arabia: findings of the first national survey. Antimicrob Agents Chemother. 2013;57:2161–2166. doi: 10.1128/AAC.02403-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Abouzeid MS, Zumla AI, Felemban S, Alotaibi B, O'Grady J, Memish ZA. Tuberculosis trends in Saudis and non-Saudis in the Kingdom of Saudi Arabia—a 10 year retrospective study (2000–2009) PLoS One. 2012;7:e39478. doi: 10.1371/journal.pone.0039478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mazroa MA, Kabbash IA, Felemban SM. HIV case notification rates in the Kingdom of Saudi Arabia over the past decade (2000–2009) PLoS One. 2012;7:e45919. doi: 10.1371/journal.pone.0045919. [DOI] [PMC free article] [PubMed] [Google Scholar]