Why is an article about global health included in a special issue on health in the USA? About half the produce that Americans consume is cultivated in other countries, 60 million Americans travel or work outside the USA, and most patients with measles and tuberculosis in the USA acquired their infection elsewhere. Emerging diseases, globalisation of foods and medicines, the rise in antimicrobial resistance, and the ease with which pathogens can be manipulated for good or harm increase each nation's vulnerability and interdependence.
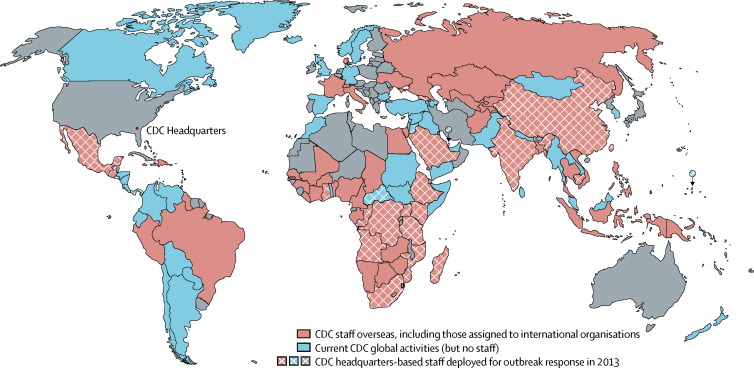
The Centers for Disease Control and Prevention (CDC) has engaged in global health for more than 60 years. Although tackling infectious disease threats has been a constant, the agency has also provided humanitarian assistance in natural disasters, refugee crises, and famines; improved child survival; and strengthened scientific measurement of health metrics. CDC's workforce includes more than 300 internationally deployed public health professionals in addition to around 1330 locally employed staff working in about 60 countries (figure ). CDC's global health strategy aims to: achieve optimum health effects; strengthen global health capacity; improve global health security; and strengthen the organisation's capacity.1 This report describes selected programmes that illustrate these goals.
Figure.
Location of CDC's global programmes and personnel, 2013
CDC=Centers for Disease Control and Prevention.
Leveraging the strengths of the US-implementing agencies for a whole-of-government approach, the US President's Emergency Plan for AIDS Relief (PEPFAR) targets resource-constrained countries that are hardest hit by the HIV epidemic. CDC has played a central role in PEPFAR since its inception, bringing more than 30 years of experience of work in HIV/AIDS. CDC staff work with peers in Ministries of Health and other host country entities to implement effective national programmes in HIV care and treatment, tuberculosis–HIV integration, maternal and child health, HIV prevention, and HIV counselling and testing. Through PEPFAR, CDC is also strengthening public health systems through focused investments in local workforce capacity and health systems that are essential to the scale-up and sustainability of priority PEPFAR programmes and to the strengthening of the broader public health system. For example, growing HIV treatment programmes were shown to be positively correlated with increased rates of facility deliveries by non-HIV infected women.2
In late 2011, President Obama and then-Secretary of State Hillary Clinton advanced the vision of an AIDS-free generation, defined as almost complete elimination of vertical transmission of HIV, greatly reduced incidence of sexual transmission of HIV in adults and adolescents, and universal access to antiretroviral therapy (ART) to people who become infected. President Obama announced in December, 2011, ambitious new targets for priority evidence-based interventions that were to be realised in just 2 years' time: PEPFAR, in 2013, was committed to directly support 6 million patients receiving treatment, an increase of 50% over the previous target; provision of therapy to 1·5 million pregnant women to prevent vertical infection of HIV; and to cumulatively reach 4·7 million men with voluntary medical male circumcisions.3, 4 CDC and its partners worked to make these bold targets a reality. PEPFAR has directly supported 6·7 million patients receiving treatment; provided more than 1·5 million pregnant women with antiretroviral prophylaxis to prevent mother-to-child transmission of HIV during the preceding 2 years; and with cumulative support of 4·2 million medical male circumcisions, was on track to achieve that target by the end of 2013.5
CDC implemented an innovative approach to prevent mother-to-child transmission of HIV in Malawi by working with the Ministry of Health and local partners.6 The new approach, called Option B+, offers all pregnant or breastfeeding women infected with HIV lifelong ART. 1 year after this approach was implemented in 2011, the number of HIV-positive pregnant and breastfeeding women receiving ART increased by more than 700%, from 1257 to 10 663. Option B+ not only reduces mother-to-child transmission to less than 5% but also maintains the mother's health, provides lifelong reduction of HIV transmission to uninfected sexual partners, and prevents mother-to-child transmission in future pregnancies. Other African and Caribbean countries are now initiating this approach. Although each country must weigh the potential effect and costs of Option B+ in reaching the goal of elimination of mother-to-child HIV transmission, this approach could overcome barriers such as inadequate immunological testing capacity, substantial distances between antenatal clinic and ART-initiation sites, and human resource constraints.6
Further, CDC and the US Health Resources and Services Administration initiated the Track 1·0 programme in 2004, to rapidly scale up ART delivery initially through US-based partners.7 In its first phase, PEPFAR was undertaken as an emergency response to provide accelerated access to crucial, lifesaving services and programmes. With PEPFAR's reauthorisation in 2008, CDC worked to further strengthen programme sustainability, country stewardship, and local implementation of core programmes. CDC worked with Ministries of Health to transition service delivery of HIV/AIDS care and treatment to local stewardship in 13 countries. As of February, 2012, these countries had contracts or awards in place with indigenous partners to establish local country ownership of their ART programmes. The transition of treatment programmes to indigenous partners is consistent with CDC's approach across programme areas of working through partner Ministries of Health and other local entities. 61% of CDC's PEPFAR programme funding goes through indigenous entities, and this share should continue to grow as CDC provides the technical support and capacity building to maintain continuity and quality of treatment services.
CDC's influenza programme contributes to strengthened global health security. Influenza viruses spread rapidly without respect to geographical borders. Control of disease caused by these viruses requires accurate laboratory detection, epidemiological response, and development and delivery of appropriately targeted vaccines and other countermeasures. Efforts that focus on seasonal influenza strengthen preparedness for pandemics. Addressing avian influenza has assumed greater priority since emergence of H5N18 and more recently H7N9 influenza viruses.9
The CDC is the National Influenza Center for the USA and one of five WHO International Collaborating Centers for surveillance, epidemiology, and control of influenza. CDC scientists participate in strain selection for seasonal vaccines and prepare candidate vaccine virus strains for vaccine manufacturers. Since the emergence of cases of H5N1 avian influenza in people more than a decade ago, CDC has expanded support to and collaborations on influenza with dozens of countries.
After a local outbreak in 1997 in Hong Kong,10, 11 avian H5N1 influenza resurfaced in 2003, initiating a decade of major epizootics affecting birds in Asia, northern Africa, and Europe, prompting intensified national, regional, and global responses.12 To date, animal-to-human transmission has caused nearly 400 human fatalities, and millions of poultry have been culled in affected areas. The CDC contributed to a comprehensive US Government response to H5N1 avian influenza. It established cooperative agreements with ministries of health in more than 30 countries to strengthen capacity for epidemiological response, laboratory detection, and emergency preparedness; seconded staff to WHO, World Animal Health Organization, and UN Food and Agriculture Organization; collaborated on vaccine and diagnostic studies with the US National Institutes of Health, the Food and Drug Administration, the Biomedical Research and Advanced Development Authority, academic investigators, and industry; and established a strategic national stockpile of antiviral drugs and other emergency supplies.
By April, 2009, when CDC first detected a novel strain of influenza A H1N1, CDC had already enhanced capacity for pandemic response. An Influenza Reagent Repository facilitated the surge in laboratory testing in the USA and other countries. CDC shipped reagents for the detection of novel 2009 H1N1 influenza virus beginning May 1, 2009.13 In addition to 1500 kits shipped to public health laboratories in all 50 states, 1400 diagnostic kits were shipped to laboratries in 153 countries. CDC's investments in strengthening countries' surveillance for severe acute respiratory illness (SARI)14 provided recognition of severe disease in many countries caused by the new influenza strain and helped to monitor changes in clinical severity that might signal viral mutations of concern. In 2013, the SARI surveillance systems monitored the spread of the new Middle East respiratory syndrome (MERS) coronavirus.
On March 31, 2013, Chinese authorities reported to WHO their detection of a novel H7N9 avian influenza virus that caused severe pneumonia in three people in Shanghai and Anhui.9, 15 From Oct 1, 2013, to March 12, 2014, 384 human cases and 123 deaths had been reported by China's National Health and Family Planning Commission, and the novel virus had been isolated from live bird markets.16 The Chinese rapidly completed whole genome sequencing of several viral isolates, posted their sequence data, closed live bird markets in several cities, and initiated targeted culling of birds. The virus is of low pathogenicity in poultry, and subclinical avian infection has complicated animal control efforts. Although no sustained human-to-human transmission has occurred, it is too early to be certain of the full effect that this novel virus will have on human or animal populations. The Chinese authorities responded rapidly and shared information about human disease and genetic sequence data openly.17
The US CDC has collaborated with China's influenza scientists and public health authorities for decades. CDC provided substantial technical assistance, several visiting scientists from China completed training and research projects in Atlanta, and senior scientists from the US CDC provided onsite technical support in China. A major milestone was achieved in 2010, when China was designated as the fifth WHO International Collaborating Center for Reference and Research on Influenza in human beings. China is also the location of one of CDC's Global Disease Detection (GDD) Regional Centers. At GDD sites, US CDC epidemiology, laboratory, and veterinary staff work closely with counterparts from the ministries of health to strengthen early detection and response to public health threats. China also hosts a Field Epidemiology Training Program (FETP), at which a US CDC Resident Advisor works closely with epidemiology trainees in a 2 year programme modelled after the CDC's elite Epidemic Intelligence Service. In recognition of these broad partnerships, China designates national, provincial, and district public health departments as CDCs.
Influenza events highlight the importance of strengthening global health security worldwide. Emerging threats such as avian influenza or severe acute respiratory syndrome can occur anywhere.18 Acceleration of improvements in the capacity for each nation to protect its own citizens and detect and report public health threats of international concern promptly to the global community is urgently needed.19
CDC's experience in Haiti addresses how programmes designed for health effect can strengthen capacity and improve preparedness for health security threats. On Jan 12, 2010, a devastating earthquake struck Port-au-Prince, Haiti, killing an estimated 230 000 people, injuring 300 000 more, displacing more than 20% of the country's 10 million residents, and destroying much of the capital's infrastructure.20 The public health response benefited from CDC's partnership with the Ministry of Public Health and Population (MSPP), and the administrative and non-governmental organisation implementation platforms established under PEPFAR in 2002.20 HIV services recovered to baseline rapidly.21 Yet an urgent need remained to strengthen reportable disease surveillance because of overcrowding and poor living conditions,22, 23 expand capacity to identify reportable pathogens at the national public health laboratory,24 and train a public health workforce. The US Government committed more than US$3 billion in new funds for post-earthquake relief, recovery, and reconstruction; facilitated MSPP's rapid detection of Vibrio cholerae within days of its introduction; and contributed to an effective emergency response20 to the worst national cholera epidemic in the modern era.25 After these back-to-back crises, in early 2011 MSPP, CDC, and other organisations identified seven measurable public health effect goals to transform health services and disease outcomes.26
With the aim to achieve an AIDS-free generation, in 2011, MSPP and PEPFAR-Haiti expanded HIV counselling and testing sites for pregnant women, implemented a case management programme for all HIV-infected women to reduce loss to follow-up, and in 2012 adopted the B+ option that provides all HIV-infected pregnant and breastfeeding women with lifelong ART irrespective of CD4 cell count.6, 27 HIV testing of pregnant women has increased by 74%, from 128 540 in 2010, to 223 626 in 2013.28 The proportion of identified HIV-infected pregnant women who received prophylaxis or ART increased from 61% to 92% during this period.28 Since the earthquake, overall access to ART has nearly doubled;29, 30 in 2013, more than 75% of all eligible HIV-infected Haitians were receiving ART.28
From Oct 20, 2010, to April 28, 2014, Haiti reported 701 961 cases of cholera and 8555 deaths.31 The inadvertent introduction of cholera, which had not been seen in Haiti in more than a century, accounted for 57% of the reported global cholera burden in 2010 and 2011.25 Although the annual case fatality rate has been sustained at the international standard of 1% or less since 2011, elimination will need substantial investment in infrastructure to address inadequate access to improved drinking water (62%) and sanitation (24%).32, 33 MSPP and the National Directorate for Potable Water and Sanitation, with technical support from PAHO, UNICEF, and CDC, developed a 10 year national elimination plan that calls for increased investment in infrastructure and interim measures, such as the scale-up of a new national strategy for household water treatment and storage, the deployment of 264 trained potable water and sanitation technicians to 133 rural communes, and targeted use of oral cholera vaccine.
One of the most important legacy goals for Haiti was to establish a functioning, sustainable, self-correcting public health system. Integration of MSPP's reportable disease surveillance systems,22, 23, 25 expansion of laboratory capacity,20 and the establishment in 2011 of a competency-based, mentor-facilitated FETP have bolstered national public health capacity to detect and monitor disease outbreaks, and use data to drive public health policy. CDC has helped to establish 50 FETPs that have trained nearly 3000 graduates from 69 countries.
The world is more interconnected than ever, and weak links in public health capacity anywhere can have profound effects at distant locations. Governments have responsibilities to their citizens and other nations to detect problems rapidly, communicate promptly, and respond effectively. The CDC focuses on the protection of Americans and improvements in the health and capacity of people worldwide through partnerships with ministries of health, other US Government agencies, non-governmental organisations, and multilateral organisations. The goal of these efforts is to improve health and strengthen capacity while striving for a world more secure from emerging threats.
Acknowledgments
Acknowledgments
We thank Ezra Barzilay, Sally Ezra, Barbara Marston, and Ann Moen for assistance with manuscript and figure preparation; and Harold Jaffe and Tom Frieden for review of the manuscript. The findings and conclusions of this report are those of the authors and do not necessarily reflect the official position of the Centers for Disease Control and Prevention.
Contributors
AS contributed to the overall planning and writing of the manuscript, the literature search, and the development of the figure. JT contributed to the writing of the manuscript, the literature search, and the development of the figure. JB contributed to the writing of the manuscript and the literature search.
Declaration of interests
We declare no competing interests.
References
- 1.Centers for Disease Control and Prevention CDC Global Health Strategy. 2013. http://www.cdc.gov/globalhealth/strategy/pdf/cgh_strategy_overview.pdf (accessed Jan 20, 2014).
- 2.Kruk ME, Jakubowski A, Rabkin M, Elul B, Friedman M, El-Sadr W. PEPFAR programs linked to more deliveries in health facilities by African women who are not infected with HIV. Health Aff (Millwood) 2012;31:1478–1488. doi: 10.1377/hlthaff.2012.0197. [DOI] [PubMed] [Google Scholar]
- 3.Reed JB, Njeuhmeli E, Thomas AG. Voluntary medical male circumcision: an HIV prevention priority for PEPFAR. J Acquir Immune Defic Syndr. 2012;60(suppl 3):88–95. doi: 10.1097/QAI.0b013e31825cac4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Progress in voluntary medical male circumcision service provision—Kenya, 2008–2011. MMWR Morb Mortal Wkly Rep. 2012;61:957–961. [PubMed] [Google Scholar]
- 5.US President's Emergency Plan for AIDS Relief (PEPFAR) Shared responsibility-strengthening results for an AIDS-free generation. 2013 PEPFAR Results. 2013. http://www.pepfar.gov/documents/organization/218406.pdf (accessed Jan 20, 2014).
- 6.Centers for Disease Control and Prevention Impact of an innovative approach to prevent mother-to-child transmission of HIV—Malawi, July 2011-September 2012. MMWR Morb Mortal Wkly Rep. 2013;62:148–151. [PMC free article] [PubMed] [Google Scholar]
- 7.El-Sadr WM, Holmes CB, Mugyenyi P. Scale-up of HIV treatment through PEPFAR: a historic public health achievement. J Acquir Immune Defic Syndr. 2012;60(suppl 3):S96–104. doi: 10.1097/QAI.0b013e31825eb27b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Isolation of avian influenza A(H5N1) viruses from humans—Hong Kong, May–December 1997. MMWR Morb Mortal Wkly Rep. 1997;46:1204–1207. [PubMed] [Google Scholar]
- 9.Gao R, Cao B, Hu Y. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med. 2013;368:1888–1897. doi: 10.1056/NEJMoa1304459. [DOI] [PubMed] [Google Scholar]
- 10.Claas ECJ, Osterhaus ADME, van Beek R. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet. 1998;351:472–477. doi: 10.1016/S0140-6736(97)11212-0. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention Update: isolation of avian influenza A (H5N1) viruses from humans—Hong Kong, 1997–1998. MMWR Morb Mortal Wkly Rep. 1998;46:1245–1247. [PubMed] [Google Scholar]
- 12.Uyeki TM. Human infection with highly pathogenic avian influenza A (H5N1) virus: review of clinical issues. Clin Infect Dis. 2009;49:279–290. doi: 10.1086/600035. [DOI] [PubMed] [Google Scholar]
- 13.Jernigan DB, Lindstrom SL, Johnson JR. Detecting 2009 pandemic influenza A (H1N1) virus infection: availability of diagnostic testing led to rapid pandemic response. Clin Infect Dis. 2011;52(suppl 1):36–43. doi: 10.1093/cid/ciq020. [DOI] [PubMed] [Google Scholar]
- 14.Radin JM, Katz MA, Tempia S. Influenza surveillance in 15 countries in Africa, 2006–2010. J Infect Dis. 2012;206(suppl 1):S14–S21. doi: 10.1093/infdis/jis606. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention Emergence of avian influenza A (H7N9) virus causing severe human illness—China, February-April 2013. MMWR Morb Mortal Wkly Rep. 2013;62:366–371. [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Y, Liang W, Yang S. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet. 2013;381:1916–1925. doi: 10.1016/S0140-6736(13)60903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uyeki TM, Cox NJ. Global concerns regarding novel influenza A (H7N9) virus infections. N Engl J Med. 2013;368:1862–1864. doi: 10.1056/NEJMp1304661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fischer JE, Katz R. Moving forward to 2014: global IHR (2005) implementation. Biosecur Bioterror. 2013;11:153–156. doi: 10.1089/bsp.2013.0030. [DOI] [PubMed] [Google Scholar]
- 19.Ijaz K, Kasowski E, Arthur RR, Angulo FJ, Dowell SF. International Health Regulations—what gets measured gets done. Emerg Infect Dis. 2012;18:1054. doi: 10.3201/eid1807.120487. 1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tappero JW, Tauxe RV. Lessons learned during public health response to cholera epidemic in Haiti and the Dominican Republic. Emerg Infect Dis. 2011;17:2087–2093. doi: 10.3201/eid1711.110827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walldorf JA, Joseph P, Valles JS. Recovery of HIV service provision post-earthquake. AIDS. 2012;26:1431–1436. doi: 10.1097/QAD.0b013e328352d032. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention Launching a National Surveillance System after an earthquake—Haiti, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:933–938. [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention Rapid establishment of an internally displaced persons disease surveillance system after an earthquake—Haiti, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:939–945. [PubMed] [Google Scholar]
- 24.Dowell SF, Tappero JW, Frieden TR. Public health in Haiti—challenges and progress. N Engl J Med. 2011;364:300–301. doi: 10.1056/NEJMp1100118. [DOI] [PubMed] [Google Scholar]
- 25.Barzilay EJ, Schaad N, Magloire R. Cholera surveillance during the Haiti epidemic—the first 2 years. N Engl J Med. 2013;368:599–609. doi: 10.1056/NEJMoa1204927. [DOI] [PubMed] [Google Scholar]
- 26.Vertefeuille JF, Dowell SF, Domercant JW, Tappero JW. Cautious optimism on public health progress in post-earthquake Haiti. Lancet. 2013;381:517–519. doi: 10.1016/S0140-6736(13)60051-3. [DOI] [PubMed] [Google Scholar]
- 27.Schouten EJ, Jahn A, Midiani D. Prevention of mother-to-child transmission of HIV and the health-related Millennium Development Goals: time for a public health approach. Lancet. 2011;378:282–284. doi: 10.1016/S0140-6736(10)62303-3. [DOI] [PubMed] [Google Scholar]
- 28.MESI Monitoring, evaluation and surveillance interface. http://www.mesi.ht (accessed Jan 20, 2014).
- 29.UNAIDS UNAIDS Report on the global AIDS epidemic 2010. http://www.unaids.org/documents/20101123_globalreport_em.pdf (accessed Jan 20, 2014).
- 30.UNAIDS 2013 UNAIDS Report on the global AIDS epidemic. http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf (accessed Jan 20, 2014).
- 31.Ministère de la Santé Publique et de la Population Ministère de la Santé Publique et de la Population daily reports on the cholera epidemic in Haiti [Rapports journaliers du MSPP sur l'évolution du choléra en Haiti] 2014. http://mspp.gouv.ht/site/downloads/Rapport%20Web_28.04_Avec_Courbes_Departementales.pdf (accessed May 3, 2014).
- 32.Waldman RJ, Mintz ED, Papowitz HE. The cure for cholera—improving access to safe water and sanitation. N Engl J Med. 2013;368:592–594. doi: 10.1056/NEJMp1214179. [DOI] [PubMed] [Google Scholar]
- 33.World Health Organization. UNICEF World Health Organization/UNICEF Joint Monitoring Programme (JMP) for Water Supply and Sanitation, 2012. Progress on drinking water and sanitation: 2012 update. http://www.wssinfo.org/data-estimates/tables/ (accessed May 3, 2014).