Abstract
Mass gatherings are regarded as potential risks for transmission of infectious diseases, and might compromise the health system of countries in which they are hosted. The evidence for increased transmission of infectious diseases at international sporting mass gatherings that attract many visitors from all over the world is not clear, and the evidence base for public health surveillance, epidemiology, and response at events such as the Olympics is small. However, infectious diseases are a recognised risk, and public health planning is, and should remain, a crucial part of the overall planning of sporting events. In this Series paper, we set out the planning and the surveillance systems that were used to monitor public health risks during the London 2012 Olympic and Paralympic Games in the summer of 2012, and draw attention to the public health issues—infectious diseases and chemical, radiation, and environmental hazards—that arose. Although the absolute risk of health-protection problems, including infectious diseases, at sporting mass gatherings is small, the need for reassurance of the absence of problems is higher than has previously been considered; this could challenge conventional public health surveillance systems. Recognition of the limitations of health-surveillance systems needs to be part of the planning for future sporting events.
This is the second in a Series of three papers about mass gatherings medicine
Introduction
Mass gatherings are seen as potential risks for transmission of infectious diseases,1 and might be expected to compromise the health system of the city, country, or region in which they are held. This risk and expectation is clearly true for the yearly Hajj in Saudi Arabia, where infectious diseases have been a major problem and where substantial effort is now made by the host country's authorities to mitigate and manage the risk.2 The evidence for the risk of transmission at international sporting mass gatherings—such as the Olympic Games and World Cup—is not clear, but nevertheless public health planning and response are an essential part of the overall planning for these events.
Although reports on the epidemiology of individual mass gatherings have been published, these have been neither comprehensive nor extensive. In this Series paper, we present the planning and surveillance systems used by UK authorities to monitor public health risks—including infectious diseases and chemical, radiation, and environmental hazards—during the London 2012 Olympic and Paralympic Games (known collectively as the 2012 Games), and draw attention to the public health issues that arose and some of the lessons identified from these.
Infectious diseases at Olympic Games
During the 1996 Atlanta and 2000 Sydney Olympic Games, infectious diseases accounted for less than 1% of health-care visits.3 Data for the Attica region in Greece (in which Athens is located) during the Athens 2004 Games showed that, of the health problems for which people visited a primary-care physician, the most common were respiratory infections (6·7%) and gastroenteritis (3·7%). Across all four regions where the Games were located, in areas representing 51% of Greece's population, salmonellosis accounted for about 50% of the mandatory notifications, tuberculosis 17%, hepatitis B 5%, aseptic meningitis 4%, and bacterial meningitis 3%. Recorded morbidity from infectious diseases was very low (2–3%). 14 small clusters (2–4 people) and eight large clusters (6–38 people) of foodborne or waterborne disease were reported in August, 2004. None of these outbreaks was reported from an Olympic venue, highlighting the tendency for all events in an Olympic City during the Games to be labelled as Olympics-related.4
In the Beijing 2008 Olympic Games, the number of cases of communicable diseases (including gastrointestinal infections) paradoxically reduced by 40% compared with the previous year, and no infectious disease outbreaks were reported.5 Enhancement of health-protection measures, particularly food safety and hygiene along the entire food-supply chain, might have caused an absolute decrease in morbidity.6 However, the experience of the Democratic National Convention in Boston, MA, USA, where a reduction in health attendance was also noted during the event, suggests that movement of the resident population out of the mass-gathering environment might also partly explain the reduction in reported cases of communicable diseases.
Changes in normal catering and food-preparation systems during mass gatherings—such as the introduction of temporary or mobile food outlets or catering environments where good standards of hygiene are difficult to maintain—can lead to an increase in the risk of contaminated food and water causing incidents and outbreaks of gastrointestinal diseases. Several gastrointestinal incidents have been reported from mass gatherings such as festivals and sports events.7, 8, 9, 10, 11, 12
Respiratory illnesses have always been major concerns for mass gatherings, as evidenced by the Middle East respiratory syndrome coronavirus. Indeed, airborne spread of microorganisms in the context of a mass gathering could result in not only respiratory tract diseases but also clusters of diseases such as measles, mumps, and meningococcal infection.13 Influenza has frequently been recorded at sporting and music events such as the 2002 Winter Olympics in Salt Lake City, UT, USA,14 and music festivals in 2009 in Belgium,15 Serbia,16 and Hungary,17 and also at the World Youth Day in Sydney, NSW, Australia, in July, 2008.18 However, sustained control measures, including vaccination, during the global pandemic in 2009 averted outbreaks of influenza A H1N1 at the Hajj and the Asian Youth Games, Singapore.19, 20
The extent to which information needs at these mass gatherings are driven by politics and the media rather than by epidemiology or public health risk is not clear from published work. Demand is huge for information about any possible risk to the Games and to the reputation of the host city. Politicians and decision makers often seek reassurance that nothing is happening—this negative finding is not easily and reliably available from traditional surveillance systems. Recognition of the limits of surveillance systems needs to be part of mass-gathering planning.
London 2012 Olympic and Paralympic public health system
Planning and preparation
In the summer of 2012, London hosted the Olympic and Paralympic Games, respectively the largest and second largest international sporting mass gatherings in the world. The Olympics involved 10 500 competitors from 205 nations in 26 sports, and the Paralympics included 4200 competitors from 147 nations in 21 sports. More than 9 million tickets were sold for the Olympic and Paralympic Games, and an estimated 11 million spectators attended across all venues.21, 22
Authorities began public health planning more than 7 years before the Games, following the principles laid out in the WHO Communicable Disease Alert and Response for Mass Gatherings Guidelines, and the experiences of previous host cities.23, 24, 25 Planners recognised that during mass gatherings such as the 2012 Games it is important to address public health issues with the utmost urgency. The systems and capacity need to be in place to rapidly receive and analyse information from surveillance, reporting, and intelligence systems, and to identify and respond to any potential health-protection threat.
The UK Health Protection Agency (HPA, now Public Health England [PHE]), in partnership with other local, national, and international agencies such as WHO, local government authorities, and the UK Food Standards Agency, developed a public health risk assessment for the Games. This assessment informed the UK national cross-government Olympic risk assessment, which formed the basis for the UK Government's Olympic planning.
The approach taken to the public health risk assessment was to follow the principles of risk analysis (what might happen?), surveillance and reporting (how will we know when it happens?), and response (what will we do if it happens?). In response to this risk assessment, systems were enhanced to provide additional surveillance data, improve understanding of the public health effect of the 2012 Games, and raise public awareness and understanding of public health concerns.
Traditional surveillance
The UK, like most developed countries, has well established public health surveillance based on clinician, environmental, and laboratory reporting, augmented in the UK by syndromic reporting systems. These systems are coordinated and managed across England by the PHE as the lead public health agency. Although the systems are very effective, the risk assessment for the Games suggested that they would not be sufficient in terms of speed and comprehensiveness of coverage. Several enhancements to these systems were therefore implemented as part of preparations for the 2012 Games,26, 27 including the addition of data for attendance at Olympics venues to the core reporting requirement of notified cases, and a move from weekly to daily analysis and reports.27 The national Centre for Infectious Disease Surveillance and Control routinely collates reports of incidents, outbreaks, and adverse trends from across the UK; during the Games, in addition to undertaking this daily, they collated the enhanced systems we describe in this Series paper.
Daily analyses of mortality data were also done, and a new system was introduced for sentinel intensive care units to report unexplained illness of probable infectious cause.28 This system involved clinicians in paediatric and adult intensive care units rapidly reporting cases using a customised web-based method. Cases were defined as thought to be due to infections but for which initial laboratory tests did not establish a diagnosis and which did not fit with a recognisable clinical picture, or those in which the patient was not responding to standard therapy.
Syndromic surveillance
Before the Games, the HPA had two well established syndromic surveillance systems that had been used successfully during the Icelandic volcano and pandemic flu incidents.29, 30, 31 These systems were the HPA/NHS Direct Syndromic Surveillance System, which provides so-called pre-primary care data using call information from the health advice telephone service for a range of syndromes, and the HPA/QSurveillance National General Practitioner (GP) Surveillance System, one of the largest GP surveillance systems in Europe, which monitors weekly consultation data from a network of more than 3500 GP practices across the UK. Further GP surveillance was done with the long-term sentinel surveillance scheme coordinated by the Royal College of General Practitioner's Research and Surveillance Centre.
The 2012 Games risk assessment results showed a gap in the surveillance, missing visitors who might attend an out-of-hours provider of primary care (GP services), or attend either a walk-in medical centre or an emergency department. This gap was important, because the NHS directed overseas visitors to these providers to reduce any effect on normal health services. The assessment results also underscored that data from all systems were needed on a daily basis in advance of and throughout the Games.32, 33, 34
The establishment of these two new national syndromic surveillance systems—GP out-of-hours and emergency department—developed specifically for the Games are among the surveillance systems that will continue to operate in England as part of the Games' legacy.35, 36
Event-based surveillance
During the 2012 Games a national event-based surveillance team was the hub for reporting of incidents and outbreaks of an infectious disease from across the UK that might substantially affect the Games, by their effect on venues, Olympic staff, athletes, or visitors, or by the public's perception of the Games.
The team enhanced established systems by reviewing and collating daily incident and response reports submitted by all local health-protection teams. The team also reviewed the national public health case-management system (HPZone) for incidents and diseases of special interest. Information from both these sources was collated, and a Games-specific risk assessment made according to agreed criteria.37 Information about any notable events identified was routinely reported daily to the national coordination centre, or more frequently, if needed.
Polyclinic reporting
For the first time syndromic surveillance reporting was undertaken at the Games polyclinic.38 This polyclinic, in the Athletes' Village in the main Olympic–Paralympic park, was the principal point of access to medical services for athletes and others. Medical facilities39 were also located in every sporting venue, as well as in one of the main hotels housing the Olympic–Paralympic family. Each time a medical service was used, the doctor, first aider, physiotherapist, dentist, or other health-care provider recorded details of the consultation and treatment using a medical encounter form. These forms provided an electronic record of the signs and symptoms of the presenting illness or injury. The London Organising Committee of the Olympic and Paralympic Games (LOCOG) wanted to gain some understanding of the incidence and pattern of infectious disease during the Games time—for the first time an additional section was included on the form to enable this. This section was obligatory for care providers to complete, and asked whether the encounter was fever, rash, diarrhoea or vomiting, respiratory symptoms, jaundice, meningitis or encephalitis, or none of these.
International epidemic intelligence
The HPA worked with international partners—particularly the European Centre for Disease Prevention and Control (ECDC) and WHO—to set up enhanced international surveillance for the 2012 Games.40, 41 This international surveillance monitored and assessed the risk, on a day-to-day basis throughout the surveillance period, of any infectious disease threats abroad that had the potential to affect health in the UK, and, in particular, at the Games. The team undertook joint risk assessments of incidents identified as relevant through an agreed set of criteria designed for the Games, using methods developed for this purpose.
Reporting of hazards
The HPA's Centre for Radiation, Chemical and Environmental Hazards provided a daily environmental hazards situation report based on the gathering and analysis of data for both chemical and radiological incidents, along with any necessary expert public health advice. This report also included a range of environmental quality indicators including air quality, temperature, ultraviolet radiation levels, and pollen levels, as well as information on risks from river and surface-water flooding.42
Enhanced microbiology services
Enhanced clinical, public health, and environmental microbiology laboratory capability and capacity are necessary to meet the increased demands of a mass gathering. As well as additional routine testing requirements, response teams need the ability to rapidly scale up the testing capability as part of the response to an infectious-disease outbreak. The recognised lower threshold for potential public health incidents needs provision of rapid, accurate diagnoses and expert advice, as well as provision of surge capacity. Before the 2012 Games, several innovations in laboratory surveillance, introduced by the HPA's Microbiological Services Division, also began operation.43, 44, 45 The risk assessment for the Games identified likely communicable disease threats, including gastrointestinal, respiratory, waterborne, and vaccine-preventable diseases. As a result, enhanced front-line microbiology services (and, in the case of gastrointestinal pathogens, a more rapid diagnostic assay) were established.
Laboratory testing of water, food, and environmental samples in and around Games venues was an important element of the work. This testing would provide early warnings of exposures to infectious or toxic hazards, ensure satisfactory standards of food and water for consumption were achieved, and guarantee environmental controls (particularly of water in new or vacant buildings and facilities) were properly applied. Additional tests are often requested by event organisers—eg, for the 2012 Games additional tests were done on samples from marinas, hotels, training camps, and ships, as well as on samples from swimming pools, spa pools, water systems, food services, and mobile food vendors. An additional request was to assess the water quality of the architectural water features in the Olympic Park.
Findings
During the Games-time, the HPA Olympics Coordinating Centre (OCC) produced the daily public health situation report, primarily for LOCOG and the Department of Health. Information provided in this report came from across the agency, Devolved Administrations (Scotland, Wales, and Northern Ireland), LOCOG, and organisations such as the Food Standards Agency. A process of assessment for inclusion in the reports submitted to the OCC was agreed, and then a further review to identify what would be included in the situation report. This report was attached to the overarching Department of Health summary of all health activities that went to the national government coordination system that was operational during the Games-time, and its key points were included in the daily Department of Health ministerial briefing.
In the lead-up to the Games (June 2–27, 2012) several reports were received by the HPA of routine infections such as norovirus in several athletic teams (infections occurred before the teams arrived at the Athletes' Village), and of chickenpox among crew on a floating hotel for Games' staff. These outbreaks were managed by following of routine public health measures, such as isolation of people who were ill and provision of information about signs and symptoms of infections. The main risk was that of the athletes with norovirus transferring to the Athletes' Village (a closed community) while infectious—action was therefore taken by LOCOG, on the HPA's advice, to delay and manage the transfer of athletes.
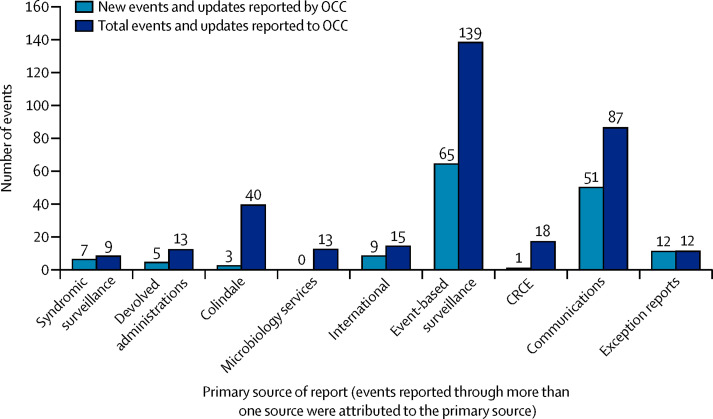
Figure 1 shows the number of events reported in HPA's daily situation report, by primary source of report. Across the 73 days of the HPA's daily Games-time monitoring (July 2–Sept 12), the HPA's situation report included 58 new events (not including the routine daily environment information from the Centre for Radiation, Chemical and Environmental Hazards), and 95 updates on these events. In total, the OCC received reports on 158 events that were assessed by the OCC director and relevant experts to establish relevance to the Games. The table shows the events reported in the daily situation reports.
Figure 1.
Number of events reported in the daily Health Protection Agency situation report, by source
OCC=Olympics Coordinating Centre. CRCE=Centre for Radiation, Chemical and Environmental Hazards.
Table.
HPA's daily situation reports and updates of events
| Events reported | Updates of events | |
|---|---|---|
| Event-based surveillance | 24 | 41 |
| Media or communications | 14 | 37 |
| International | 5 | 4 |
| Centre for Radiation, Chemical and Environmental Hazards | 1 | 0 |
| Devolved Administrations | 3 | 2 |
| National Surveillance Centre | 2 | 1 |
| Microbiology Services Division | 0 | Updates on events reported by evidence-based surveillance |
| Syndromic surveillance | 2 | 5 |
| Exception reports | 7 | 5 |
The events reported were those that met the criteria for inclusion: “any event in the UK or internationally related to either an infectious or non-infectious agent affecting an individual or a group of individuals, which could have put the health of those participating, visiting or working at the Olympics at significant risk; or which was likely to be/had been the subject of media scrutiny which would harm the perception of the Games; or which may have resulted in widespread public concern, which needed to be addressed”.37
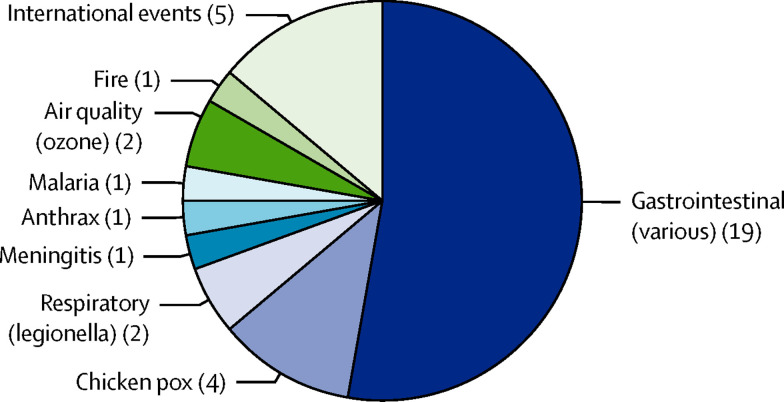
Figure 2 shows the types of events reported in the daily HPA situation report. Most incidents were those routinely seen during summer and, as expected, related mainly to gastroenteritis (possible food poisoning) and vaccine-preventable diseases.46, 47, 48 These incidents posed no risk to the Games and were managed through standard public health measures. However, some events reported were associated with athletes, and the HPA managed these appropriately by the provision of expert advice and close working with LOCOG. As noted, unusual events were reported if they attracted media attention even if they were not directly related to the Games—hence the reporting of a case of anthrax, which was in an intravenous drug user and not connected to the Games.
Figure 2.
Types of event reported in the daily Health Protection Agency situation report
Nothing unusual was reported, but the speed with which the HPA was informed, the response undertaken, and information shared across partners was far quicker than normal, and showed the thirst for information during Games time. Rumour management took up substantial time; rumours were predicted and managed well by provision of accurate, timely information, in addition to the assurance provided to politicians, the media, and the public through the daily reporting.
Sporadic cases of gastrointestinal illness were expected and occurred. Not all gastrointestinal illnesses are food-related, even if people often attribute illness to a recent meal, and identification of a cause or source of infection is not always possible. The numbers and patterns of illnesses recorded during the 2012 Games were not unusual, and were similar to those of other similar mass gatherings. No common food source linked to failures in food-safety management controls was identified; however, despite substantial planning, slight confusion remained around the investigation of food-related incidents and who was responsible for this inside venues. Some of this confusion might have been caused by the involvement of various organisations nationally, and of new organisations such as LOCOG, instead of the standard investigation and response being undertaken by local authorities and health-protection teams. This level of involvement was driven by the political sensitivity of the Games and potential reputational issues.
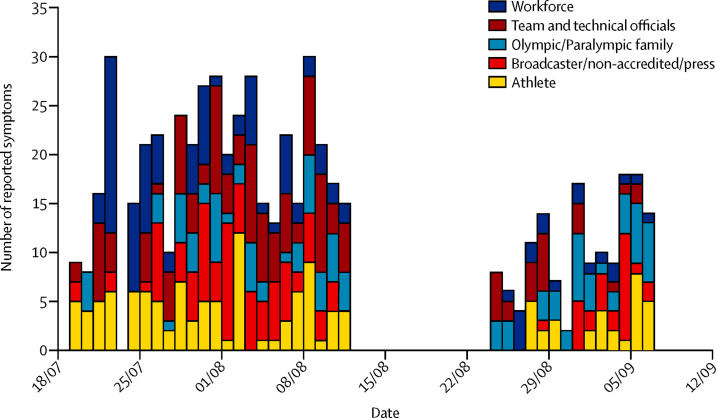
The syndromic surveillance done through the polyclinic did not detect any outbreak that could have been important for the Games. The data received enabled the HPA to feel assured that no outbreak of illness occurred that needed investigation or control measures instigated. The data were reported daily in the OCC situation report. Figure 3 shows an example of reported respiratory symptoms data by category of person.
Figure 3.
Reported respiratory symptoms by category of person, London 2012 Olympic and Paralympic Games
Because the London 2012 Games was the first time this reporting was undertaken, no background data were available for the usual numbers of illness or syndromes expected in the population accessing the polyclinic. If the background data had been available, interpretation of the reported numbers of people with each syndrome, by comparison with expected numbers, would have been easier. Additionally, many teams brought their own doctors from their countries, who saw athletes and officials outside the polyclinic; some cases would therefore not have been reported through the system.
Discussion
No major public health incidents occurred during the London 2012 Olympic and Paralympic Games. Only a few outbreaks of gastrointestinal and respiratory infections were recorded during the period. These outbreaks were not a risk to the Games, and overall infectious disease reports were at rates typical for mass gatherings and unexceptional for an average UK summer. No food-borne illness was directly linked to a Games venue, despite the tendency for those reporting them to label them as such. However, to what extent additional food-safety measures put in place for the Games contributed to the low incidence of illnesses is not possible to say.
To state this confidently, the HPA introduced a number of enhancements to the surveillance and reporting systems, many of which have now been incorporated as routine systems within the UK. Also, close collaboration and robust planning across all relevant stakeholders were key factors in ensuring that all potential issues were identified and that any links to the Games could be reliably ascertained.
Some vaccine-preventable diseases needed more sensitive consideration to balance the competing interests of prevention of spread in a confined community against the desire of elite athletes to not be treated invasively while training and performing. This need shows the importance of real-time information and rapid public health risk assessment that takes into account the context of the incident.
Provision of reassurance to the organising committee (and government and media) that nothing was happening proved to be a very important role of the public health surveillance systems. The importance of this reassurance role is not well described in mass-gathering publications and was not recognised in the initial stages of planning for the 2012 Games. Because the need for this reassurance emerged in the planning discussions, enhancements to surveillance systems and to the coordination and communication of public health activity were necessary to ensure the need could be met. Surveillance systems are not primarily designed to prove that nothing is happening, so they need to be reviewed and enhanced to fulfil this role effectively. Organisers planning mass gatherings in the future should consider this aspect of surveillance requirements as part of their assessment of the existing system's capacity.
To access information from as many sources as possible—eg, through media communications systems—is also important. Information sometimes appeared very quickly in the public domain through social media outlets such as Twitter. These reports were quickly addressed with the enhanced surveillance and reporting systems to assess validity. Robust communication arrangements also ensured rapid dissemination of information to stakeholders, professionals, the media, and the public, and prevented the escalation of rumours. This system of active coordination of information through a single point of contact also allowed us to establish, more accurately than previously, whether events occurring during the Games had a genuine relationship to the Games or were coincidental—something that has not always been possible at mass gatherings.
In conclusion, many of the enhanced surveillance and reporting systems and ways of working have now been embedded, and are a direct legacy of the Games; the public health service in the UK has been enhanced. This enhancement will enable improved national security through better surveillance capacity and cross-sector working, and a coherent approach to public health security issues across national government and globally. It is now important to maintain and build on this enhancement. Our key message is that, although the absolute risk of health-protection problems, including infectious diseases, at sporting mass gatherings is low, the need for reassurance of the absence of problems is higher than has previously been considered, and this could challenge conventional public health surveillance systems. Lessons from this experience of the London 2012 Games are being used by those planning for the Rio 2016 Olympic and Paralympic Games.49, 50
Search strategy and selection criteria
We searched PubMed, Medline, and Embase using the search terms “mass gatherings” or “crowds” in combination with the terms “sporting events” or “Olympics”. We selected publications from the past 5 years, but did not exclude commonly referenced and highly regarded older publications. We also searched the reference lists of articles identified by this search strategy and selected those we deemed relevant. Review articles and websites on mass gatherings and sporting events are cited to provide readers with more details and more references than can be supplied in this paper. We searched only articles published in English.
Contributors
BMcC, DH, MB, ZM, and AZ initiated the series. BMcC, TE, and AZ developed the initial drafts, and all authors contributed to finalising the Series paper.
Declaration of interests
We declare that we have no competing interests.
References
- 1.World Health Organization Communicable disease alert and response for mass gatherings. 2008. http://www.who.int/csr/Mass_gatherings2.pdf (accessed March 19, 2012).
- 2.Abubakar I, Gautret P, Brunette GW. Global perspectives for prevention of infectious diseases associated with mass gatherings. Lancet Infect Dis. 2012;12:66–74. doi: 10.1016/S1473-3099(11)70246-8. [DOI] [PubMed] [Google Scholar]
- 3.Jorm LR, Thackway SV, Churches TR, Hills MW. Watching the Games: public health surveillance for the Sydney 2000 Olympic Games. J Epidemiol Community Health. 2003;57:102–108. doi: 10.1136/jech.57.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsouros A, Efstathiou P, editors. Mass gatherings and public health: the experience of Athens 2004 Olympic Games. WHO/EURO; 2007. http://www.euro.who.int/__data/assets/pdf_file/0009/98415/E90712.pdf (accessed July 27, 2013). [Google Scholar]
- 5.World Health Organization The health legacy of the 2008 Beijing Olympics Games: successes and recommendations. WHO/Western Pacific Region, 2008. http://www.olympic.org/Documents/Commissions_PDFfiles/Medical_commission/The_Health_Legacy_of_the_2008_Beijing_Olympic_Games.pdf (accessed July 27, 2013).
- 6.Moy GG, Han F, Chen J. Ensuring and promoting food safety during the 2008 Beijing Olympics. Foodborne Pathog Dis. 2010;7:981–983. doi: 10.1089/fpd.2009.0473. [DOI] [PubMed] [Google Scholar]
- 7.Lee LA, Ostroff SM, McGee HB. An outbreak of shigellosis at an outdoor music festival. Am J Epidemiol. 1991;133:608–615. doi: 10.1093/oxfordjournals.aje.a115933. [DOI] [PubMed] [Google Scholar]
- 8.Morgan D, Gunneberg C, Gunnell D. An outbreak of Campylobacter infection associated with the consumption of unpasteurised milk at a large festival in England. Eur J Epidemiol. 1994;10:581–585. doi: 10.1007/BF01719576. [DOI] [PubMed] [Google Scholar]
- 9.Crampin M, Willshaw G, Hancock R. Outbreak of Escherichia coli O157 infection associated with a music festival. Eur J Clin Microbiol Infect Dis. 1999;18:286–288. doi: 10.1007/s100960050278. [DOI] [PubMed] [Google Scholar]
- 10.Brockmann S, Piechotowski I, Bock-Hensley O. Outbreak of leptospirosis among triathlon participants in Germany, 2006. BMC Infect Dis. 2010;10:91. doi: 10.1186/1471-2334-10-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgan J, Bornstein SL, Karpati AM, the Leptospirosis Working Group Outbreak of leptospirosis among triathlon participants and community residents in Springfield, Illinois, 1998. Clin Infect Dis. 2002;34:1593–1599. doi: 10.1086/340615. [DOI] [PubMed] [Google Scholar]
- 12.Sejvar J, Bancroft E, Winthrop K, the Eco-Challenge Investigation Team Leptospirosis in “Eco-Challenge” athletes, Malaysian Borneo, 2000. Emerg Infect Dis. 2003;9:702–707. doi: 10.3201/eid0906.020751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmid D, Holzmann H, Alfery C, Wallenko H, Popow-Kraupp TH, Allerberger F. Mumps outbreak in young adults following a festival in Austria, 2006. Euro Surveill. 2008;13:8042. doi: 10.2807/ese.13.07.08042-en. [DOI] [PubMed] [Google Scholar]
- 14.Gundlapalli AV, Rubin MA, Samore MH. Influenza, winter olympiad, 2002. Emerg Infect Dis. 2006;12:144–146. doi: 10.3201/eid1201.050645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gutiérrez I, Litzroth A, Hammadi S. Community transmission of influenza A (H1N1)v virus at a rock festival in Belgium, 2–5 July, 2009. Euro Surveill. 2009;14:19294. doi: 10.2807/ese.14.31.19294-en. [DOI] [PubMed] [Google Scholar]
- 16.Loncarevic G, Payne L, Kon P. Public health preparedness for two mass gathering events in the context of pandemic influenza (H1N1) 2009–Serbia, July 2009. Euro Surveill. 2009;14:19296. doi: 10.2807/ese.14.31.19296-en. [DOI] [PubMed] [Google Scholar]
- 17.Botelho-Nevers E, Gautret P, Benarous L, Charrel R, Felkai P, Parola P. Travel-related influenza A/H1N1 infection at a rock festival in Hungary: one virus may hide another one. J Travel Med. 2010;17:197–198. doi: 10.1111/j.1708-8305.2010.00410.x. [DOI] [PubMed] [Google Scholar]
- 18.Blyth CC, Foo H, van Hal SJ, the World Youth Day 2008 Influenza Study Group Influenza outbreaks during World Youth Day 2008 mass gathering. Emerg Infect Dis. 2010;16:809–815. doi: 10.3201/eid1605.091136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim HC, Cutter J, Lim WK, Ee A, Wong YC, Tay BK. The influenza A (H1N1-2009) experience at the inaugural Asian Youth Games Singapore 2009: mass gathering during a developing pandemic. Br J Sports Med. 2010;44:528–532. doi: 10.1136/bjsm.2009.069831. [DOI] [PubMed] [Google Scholar]
- 20.Memish ZA, Ebrahim SH, Ahmed QA, Deming M, Assiri A. Pandemic H1N1 influenza at the 2009 Hajj: understanding the unexpectedly low H1N1 burden. J R Soc Med. 2010;103:386. doi: 10.1258/jrsm.2010.100263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.London 2012 Everyone's Games. A guide to the London 2012 Olympic Games and Paralympic Games. London: London 2012; 2010. http://www.london2012.com/mm%5CDocument%5CPublications%5CJoinin%5C01%5C24%5C08%5C88%5Ceveryones-games.pdf (accessed June 12, 2012).
- 22.Office for National Statistics (ONS) London 2012 Games attract over half a million overseas visitors in July and August. Newport: ONS; 11 Oct 2012. http://www.ons.gov.uk/ons/dcp29904_282888.pdf (accessed Aug 22, 2013).
- 23.Enock KE, Jacobs J. The Olympic and Paralympic Games 2012: literature review of the logistical planning and operational challenges for public health. Public Health. 2008;122:1229–1238. doi: 10.1016/j.puhe.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 24.Thackway S, Churches T, Fizzell J, Muscatello D, Armstrong P. Should cities hosting mass gatherings invest in public health surveillance and planning? Reflections from a decade of mass gatherings in Sydney, Australia. BMC Public Health. 2009;9:324. doi: 10.1186/1471-2458-9-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization (WHO EURO) Health planning for large public events. Copenhagen: WHO EURO; 9 May 2012. http://www.euro.who.int/en/what-we-do/health-topics/emergencies/disaster-preparedness-and-response/news/news/2012/05/health-planning-for-large-public-events/_recache (accessed Aug 22, 2013).
- 26.Severi E, Heinsbroek E, Watson C, Catchpole M, the HPA Olympics Surveillance Work Group Infectious disease surveillance for the London 2012 Olympic and Paralympic Games. Euro Surveill. 2012;17:20232. doi: 10.2807/ese.17.31.20232-en. [DOI] [PubMed] [Google Scholar]
- 27.The Stationery Office Limited (TSO) Health Protection (Notification) Regulations 2010. The Stationery Office Limited. TSO; London: 2010. http://www.legislation.gov.uk/uksi/2010/659/pdfs/uksi_20100659_en.pdf (accessed Aug 22, 2013). [Google Scholar]
- 28.Heinsbroek E, Said B, Kirkbride H, the HPA USII Steering Group A new surveillance system for undiagnosed serious infectious illness for the London 2012 Olympic and Paralympic Games. Euro Surveill. 2012;17:20237. doi: 10.2807/ese.17.31.20237-en. [DOI] [PubMed] [Google Scholar]
- 29.Smith G, Hippisley-Cox J, Harcourt S. Developing a national primary care-based early warning system for health protection—a surveillance tool for the future? Analysis of routinely collected data. J Public Health (Oxf) 2007;29:75–82. doi: 10.1093/pubmed/fdl078. [DOI] [PubMed] [Google Scholar]
- 30.Smith GE, Cooper DL, Loveridge P, Chinemana F, Gerard E, Verlander N. A national syndromic surveillance system for England and Wales using calls to a telephone helpline. Euro Surveill. 2006;11:220–224. [PubMed] [Google Scholar]
- 31.Health Protection Agency (HPA) Syndromic systems and bulletin archive. HPA; London: 2012. http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/RealtimeSyndromicSurveillance/SyndromicSystemsAndBulletinArchive/ (accessed July 25, 2012). [Google Scholar]
- 32.Health Protection Agency Syndromic Surveillance Report, London 2012 Olympic and Paralympic Games. www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137703688 (accessed Aug 22, 2013).
- 33.Harcourt SE, Fletcher J, Loveridge P. Developing a new syndromic surveillance system for the London 2012 Olympic and Paralympic Games. Epidemiol Infect. 2012;140:2152–2156. doi: 10.1017/S0950268812001781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elliot AJ, Hughes HE, Hughes TC. Establishing an emergency department syndromic surveillance system to support the London 2012 Olympic and Paralympic Games. Emerg Med J. 2012;29:954–960. doi: 10.1136/emermed-2011-200684. [DOI] [PubMed] [Google Scholar]
- 35.Gulland A. Olympics' public health surveillance scheme will be retained after games, agency says. BMJ. 2012;344:e3620. doi: 10.1136/bmj.e3620. [DOI] [PubMed] [Google Scholar]
- 36.Health Protection Agency Press release July 3, 2012. http://www.hpa.org.uk/NewsCentre/NationalPressReleases/2012PressReleases/120603Olympics/ (accessed July 16, 2012).
- 37.Health Protection Agency Significant events reported by the Event Based Surveillance, London 2012 Olympic and Paralympic Games. www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137696661 (accessed Aug 22, 2013).
- 38.Health Protection Agency LOCOG Polyclinic, London 2012 Olympic and Paralympic Games. Available at: www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137703448 (accessed Aug 22, 2013).
- 39.Amiri N, Chami G. Medical services at the Olympics: a monumental challenge. CMAJ. 2010;182:E229–E230. doi: 10.1503/cmaj.109-3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones J, Lawrence J, Payne Hallström L, the international team International infectious disease surveillance during the London Olympic and Paralympic Games 2012: process and outcomes. Euro Surveill. 2013;18:20554. doi: 10.2807/1560-7917.es2013.18.32.20554. [DOI] [PubMed] [Google Scholar]
- 41.Health Protection Agency International Infectious Disease Surveillance, London 2012 Olympic and Paralympic Games. www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137703642 (accessed Aug 22, 2013).
- 42.Health Protection Agency Centre for Radiation, Chemical and Environmental Hazards, Games time planning and delivery – London 2012 Olympic and Paralympic Games. www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137703842 (accessed Aug 22, 2013).
- 43.Health Protection Agency Microbiology Services: preparedness and Response, London 2012 Olympic and Paralympic Games. Available at www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137703754 (accessed Aug 22, 2013).
- 44.Moran-Gilad J, Chand M, Brown C, the HPA Microbiology Services Olympics Planning Group Microbiological aspects of public health planning and preparedness for the 2012 Olympic Games. Epidemiol Infect. 2012;140:2142–2151. doi: 10.1017/S0950268812001835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bishop NC. Overcoming microbial hurdles: keeping the Olympics infection-free. Future Microbiol. 2012;7:913–915. doi: 10.2217/fmb.12.65. [DOI] [PubMed] [Google Scholar]
- 46.Health Protection Agency London Regional Report, London 2012 Olympic and Paralympic Games. www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137703022 (accessed Aug 22, 2013).
- 47.Health Protection Agency South East Regional Report, London 2012 Olympic and Paralympic Games. www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137703361 (accessed Aug 22, 2013).
- 48.Health Protection Agency South West Regional Report, London 2012 Olympic and Paralympic Games. www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137703140 (accessed Aug 22, 2013).
- 49.Health Protection Agency Sharing knowledge and experience from London 2012: HPA summary report. www.hpa.org.uk/Publications/EmergencyPreparationAndResponse/0113London2012report/ (accessed Aug 22, 2013).
- 50.Health Protection Agency Learning from London 2012—a practical guide to public health and mass gatherings. http://www.hpa.org.uk/Publications/EmergencyPreparationAndResponse/1303LearningfromLondon2012/ (accessed Aug 22, 2013).