Summary
Background
The ability to provide medical care during sudden increases in patient volume during a disaster or other high-consequence event is a serious concern for health-care systems. Identification of inpatients for safe early discharge (ie, reverse triage) could create additional hospital surge capacity. We sought to develop a disposition classification system that categorises inpatients according to suitability for immediate discharge on the basis of risk tolerance for a subsequent consequential medical event.
Methods
We did a warfare analysis laboratory exercise using evidence-based techniques, combined with a consensus process of 39 expert panellists. These panellists were asked to define the categories of a disposition classification system, assign risk tolerance of a consequential medical event to each category, identify critical interventions, and rank each (using a scale of 1–10) according to the likelihood of a resultant consequential medical event if a critical intervention is withdrawn or withheld because of discharge.
Findings
The panellists unanimously agreed on a five-category disposition classification system. The upper limit of risk tolerance for a consequential medical event in the lowest risk group if discharged early was less than 4%. The next categories had upper limits of risk tolerance of about 12% (IQR 8–15%), 33% (25–50%), 60% (45–80%) and 100% (95–100%), respectively. The expert panellists identified 28 critical interventions with a likelihood of association with a consequential medical event if withdrawn, ranging from 3 to 10 on the 10-point scale.
Interpretation
The disposition classification system allows conceptual classification of patients for suitable disposition, including those deemed safe for early discharge home during surges in demand. Clinical criteria allowing real-time categorisation of patients are awaited.
Introduction
The ability to provide medical care during sudden increases in patient volume during a disaster or other high-consequence event is a substantial concern for health-care systems. History has shown that during disasters and epidemiological outbreaks, hospitals take the burden of caring for the sick and injured.1, 2, 3, 4, 5, 6 In most major city hospitals, inpatient capacity is constrained on a daily basis.7, 8, 9 Thus, hospitals are concerned about maintenance of inpatient capacity during normal operating conditions, and they are developing methods to improve resource capabilities during surges.10, 11
Several measures have been suggested for the creation of hospital surge capacity.12, 13, 14, 15, 16 These include: cancellation of elective admissions and operations; redesign of current inpatient space to accommodate more beds when needed; opening of unlicensed or unstaffed beds; rapidly outfitting temporary nearby space, such as cafeterias or outpatient facilities; or deployment of temporary portable inpatient units. All these possibilities present unique operational challenges, such as imposition of unpractised routines in the context of rapid incremental demand for inpatient census. Furthermore, most options need hospital staffing to be increased at a time when the case-mix index can also be expected to increase. However, during some public-health emergencies, especially those of a communicable nature, hospitals are likely to have substantial reductions in available staff, as happened during the severe acute respiratory syndrome outbreak.17, 18, 19 Thus, for acute-care hospitals, a means to achieve maximum availability of capacity resources to allow for the care of victims of a disaster is a priority.20
One novel approach to capacity management during disasters is reverse triage, which includes the safe discharge of current inpatients and refocus of hospital resources to those in even greater need. Patients might be discharged home, to facilities set up to care for less acute inpatients (eg, public-health contingency stations21 specifically designed for this purpose), nursing homes, or other acute-care facilities. Thus, a need exists to develop an easy method to categorise hospital patients for safe discharge to suitable venues (including early discharge home), taking into account the existence and competence (or lack thereof) of available external resources.
We report the first phase in the development of inpatient disposition criteria for the creation of hospital surge capacity during catastrophic or high-consequence events. The aim of this phase was to develop a disposition classification system (reverse triage) based on risk tolerance of a consequential medical event as a result of discharge; assuming that critical interventions were withdrawn or withheld. We focus on the main components of the first phase: (1) conceptualisation of the disposition classification system; (2) development of operational definitions of consequential medical events and critical interventions; and (3) derivation of risk estimates related to early discharge from a multidisciplinary panel of experts. Subsequent phases of this project will use clinical data obtained from nearly 4000 hospital patients to examine the validity of the classification system to correctly identify those who can be discharged early.
Methods
Expert panel
We used evidence-based materials combined with an expert panel consensus that was approved by the Institutional Review Board on Human Subjects Research. We hosted a warfare analysis laboratory exercise,22 which was developed by the Johns Hopkins Applied Physics Laboratory in 2004. The exercise uses networked computers that allow anonymous participation through streaming comments entered into individual laptops by panellists.
39 expert panellists (27 clinicians or practitioners, 12 non-clinicians, or non-practising clinicians) took part in the 8-h exercise. Conference organisers determined the composition and the variety of desirable backgrounds of the panel members, who were then identified and specifically invited. All panellists were involved in health care, but represented diverse perspectives, including those of non-clinicians. The composition of the expert panel is shown in panel 1 . 31 of the participants were from various components of the Johns Hopkins Medical Institutions, and eight were from outside agencies and institutions. Almost all the local panellists had experience in other health systems in the USA, and four had experience in other countries. Those from the home institution represented three distinctly different establishments: a major academic health centre, an affiliate teaching centre, and a community hospital. Four of the authors participated in the panel discussions. Individual panellists received a detailed manual of background information on the day's proceedings, goals, objectives, and expectations from the expert panel. Need for written informed consent for participation was waived by the Institutional Review Board on Human Subjects Research because all written comments and risk estimates made by the panellists were anonymous and could not be linked back to an individual.
Panel 1. Composition of expert panel.
Physicians (21)
Emergency medicine (4), internal medicine (6), psychiatry (1), infectious diseases (1), obstetrics/gynaecology (2), oncology (1), paediatrics (2), paediatric emergency medicine (2), general surgery, paediatric surgery (1), critical care/anaesthesiology (2), cardiology (1), nephrology (1), trauma surgery (1), ear nose and throat (1), military surgery (1), military emergency medicine (2), military psychiatry (1)
Nurse practitioners (1) and nurses (9)
Obstetrics and gynaecology (1), psychiatry (1), internal medicine (1), emergency medicine (1), surgery (2), paediatrics (1), military (2), oncology (1)
Experts (39) in
Disaster management (8), disaster and military triage (3), hospital epidemiology (3), research methodology (4), risk management (3), hospital administration (6), home health services (1), social work (1), medical law (1), medical ethics (1), patient safety (6), data analysis (5), military public health (3), city and state public health (3), public health (10), public health preparedness and response (10), homeland security (9), prehospital care (1), international health care (7)
Numbers in each category are shown in parentheses. Some physicians and experts are included in more than one specialist area.
Warfare analysis laboratory exercise
The warfare analysis laboratory is a specialised facility equipped with a network of 53 laptop computers, an integrated audio and visual infrastructure with six large-screen, high-resolution, interactive three-dimensional computer graphics display monitors, a designated data-analysis station, and a 50-seat observation gallery. Plans, definitions, and assumptions can be displayed on large-screen monitors at the front of the room. One or more of the screens can be dedicated to continuous display of anonymous comments from panellists on each networked computer in real time. Items that need opinions or need to be voted on can also be processed and displayed in real-time.
Computer comments are numbered consecutively to help with responses to specific statements. The exercise is a formally defined process and is further described elsewhere.22 The warfare analysis laboratory has a professional team that oversees the process. A trained facilitator guides the process, allowing for discussion of key issues, and maintaining the focus on the day's objectives.
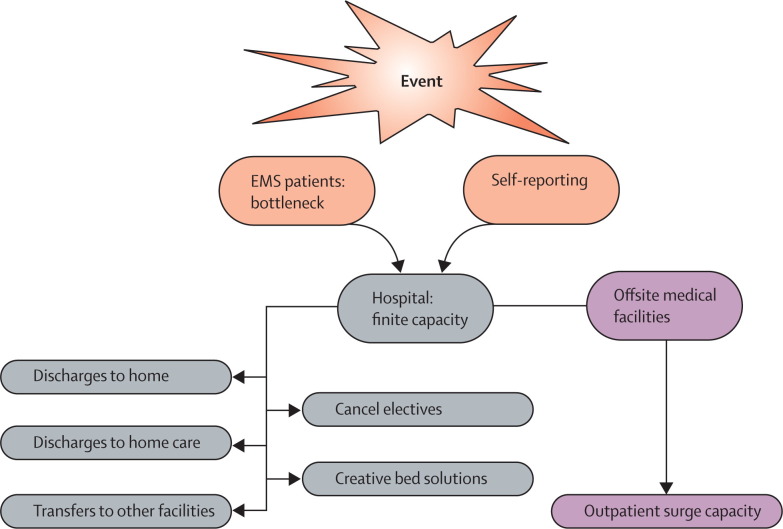
Before the exercise was started, eight consensus panel organisers held two separate full-day rehearsals for the conference, to ensure that presentations, discussion, and voting would go smoothly. On the day of the exercise, panellists were shown how to use the facility and computer data-gathering techniques with presimulations unrelated or indirectly related to the planned session. Panellists were then exposed to short formal presentations on disaster management, surge-capacity concepts (figure ), notions of risk and risk tolerance in health care, an overview of the project, and rationale and specific objectives. Evidence-based information was presented about decision-making devices (eg, Patient Outcomes Research Team [PORT] and Acute Physiology and Chronic Health Evaluation [Apache] III), peer-reviewed publications, and data for adverse events, readmission rate of discharged patients, and iatrogenic events related to being in hospital.
Figure.
Means to create surge capacity
EMS=Emergency medical system.
The tasks of the expert panel during the exercise were to: (1) develop an evidence-based disposition classification system for discharge or transfer based on tolerance for the occurrence of a consequential medical event or the need for a critical intervention during the ensuing 72 h after discharge or transfer; (2) develop consensus definitions of consequential medical event and critical intervention; (3) assign, for each category of the system, the panel's tolerance for a subsequent consequential medical event, or need for an in-hospital critical intervention; and (4) compile a list of critical interventions that would imply the need for continued stay in an acute-care hospital.
The disposition classification system
Discussions were held of assumptions to be used for definition of the disposition classification system. Panellists were presented with proposed assumptions developed by the project leaders and were invited to criticise and include additional assumptions. Final assumptions under which the conference proceeded are shown in panel 2 .
Panel 2. Assumptions held in development of disposition classification system.
-
•
Panellists should think globally and not specifically about their facilities
-
•
The hospital will remain functional (ie, not a target of terrorist threat or disaster)
-
•
Government and other disaster response will occur
-
•
Disaster plans will exist
-
•
Health-care system will recover or be aided within 48–72 h
-
•
Assume ability to smoothly discharge or transfer patients (specific logistical issues will be considered separately).
-
•
A model to compare risk profiles of competing new patients requiring hospital resources exists
-
•
Hospital liability protection exists or is not an issue
-
•
Inpatient beds could be redistributed across various services
-
•
Quality of care will not be compromised
-
•
Only basic (non-professional or family) care will be available to patients discharged into the community (relatives, shelters, or home)
-
•
Hospital patients with dismal prognosis will be considered separately
-
•
Other efforts to improve surge capacity will be continuing
Panellists were shown examples of classification systems used for clinical decision making.23, 24, 25, 26 The notion and number of categories were discussed by panellists both via open comment and anonymous computer input. Discussion focused on dispositions that define severity of illness and likelihood of treatable complications. The process also included a discussion on the language used to define the categories to help with assignment of tolerance of risk for a consequential medical event. Consensus was reached about the number of categories based on tolerance for a consequential medical event.
Consequential medical events and critical interventions
To determine into which category of the disposition classification system a patient falls requires the assessment of risk for a consequential medical event. Assessment of risk took into account the possibility of medical deterioration, a new medical event, or the untoward effect of the withdrawal of a continuing treatment (ie, withdrawal of a critical intervention).
The consensus definition of consequential medical event developed by the panellists was: unexpected death, irreversible impairment, or reduction in function within 72 h of hospital discharge for which an in-hospital critical intervention would be initiated to stabilise or ameliorate the medical disorder or disorders.
Panellists reasoned that medical events were consequential only if acute in-hospital treatment or intervention was needed. Thus, when the probability of a consequential medical event was determined, the panellists agreed that likelihood should be judged on the basis of need for a new or continuing in-hospital treatment, termed critical intervention. Thus, failure to initiate or continue a critical intervention risked a consequential medical event.
To orientate panellists with respect to tolerance of risks taken in daily medical care, panellists were presented data for: 3-day and 15-day readmission rates taken from 26 000 adult discharges during 1 year (2003) for various medical services from one of our hospitals (unpublished data), as well as data of baseline inpatient hospital errors from the Institute of Medicine.27 Risk, consequential medical event, and the definition of critical intervention were then discussed in detail.
After the definitions had been decided on, the panellists voted to define the upper limit of acceptable risk for the occurrence of a consequential medical event (ie, need for critical intervention), for each of the categories of the disposition classification system. Voting was on a scale of 0–100%, with votes given to one decimal point. Results of the first vote were revealed and further discussion ensued. A second (and final) consensus vote was then taken.
After discussion, a consensus definition of critical interventions was formed and became embedded in the definition of consequential medical event, as noted above. Panellists were then presented with a list of critical interventions to consider, and asked to validate or criticise each in view of the consensus definition. A list of possible candidate critical interventions was initially developed by the conference organisers. All panellists were allowed to suggest and add interventions to the list. Panellists with clinical experience or responsibilities were then asked to rank on a Likert scale of 1 to 10 (whole numbers only), how likely, in their opinion, the withholding or withdrawal of each of the listed critical interventions would lead to a consequential medical event. A score of ten was deemed to be synonymous with certainty of a consequential medical event, whereas a score of one implied virtually no associated risk with withholding or withdrawing the specific critical intervention. Panellists without clinical experience or responsibilities participated in discussions, but did not vote. Separate votes were taken for withholding and withdrawing the critical intervention. Data generated by these votes were presented. After further discussion, a final vote was taken.
Data analysis
Data were recorded and stored in a database and were then tabulated. Only the final votes were used for analysis. Data only from clinicians were used for those questions requiring clinical expertise (clinicians could be identified because they logged on as “clinician” rather than “non-clinician”). Because the warfare analysis laboratory exercise requires anonymity in recording participant responses, subgroup analyses by medical specialty were not possible.
Role of the funding source
The study sponsor had no role in the study design, data collection, data analysis, data interpretation, or the writing of the report. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit the paper for publication.
Results
The panellists agreed that a five category disposition classification system was optimum, for the intended task (table 1 ). Consensus was reached on the understanding and wording of the categories. The upper limit of risk tolerance for a consequential medical event for the first category was less than 4%. This category represented patients who the panellists judged to be at low risk of a consequential medical event if discharged early; on the assumption that no skilled medical care was available outside the hospital setting. An example would be a patient admitted for intravenous antibiotics for uncomplicated cellulitis, who could readily be discharged and switched to oral medication.
Table 1.
Consensus disposition classification and tolerance for rate of consequential medical events
| Risk of consequential medical event | Basis | Mean upper limit of tolerance for consequential medical events (IQR) |
|---|---|---|
| 1 (minimim) | Minimum to no anticipated medical events during next 72 h | 3·8% (2–5) |
| 2 (low) | Calculated risk of non-fatal medical event. Transfer to low acuity facility appropriate. Consider early discharge when effects of disaster exceed risks of remaining in hospital—eg, risk of biothreat transmission, effects of resource constraints | 11·7% (8–15) |
| 3 (moderate) | Consequential medical event quite likely without critical intervention | 33·1% (25–50) |
| Discharge to home not advisable | ||
| Transfer to facility of moderate capabilities appropriate | ||
| 4 (high) | Patient care cannot be interrupted without virtually assured morbidity or mortality. Highly skilled care required | 61% (45–80) |
| Transfer to major acute-care facility only | ||
| 5 (very high) | Patient cannot be moved or readily transferred | 92·3% (95–100) |
| Generally unstable for transport | ||
| Consider ICU-capable transport only |
ICU=intensive-care unit.
The next categories had upper limits of risk tolerance of about 12%, 33%, 60%, and 100% respectively. The panellists agreed that category 2 represented those patients who, although at some risk of a consequential medical event, might nonetheless warrant discharge if surge capacity was needed for victims of a disaster; especially if incoming victims are at higher risk of consequential medical event than those patients considered for discharge. Panellists also agreed that this category of patients could warrant discharge in certain biothreat or other contagion situations in which spread of disease in hospitals would present a substantial added risk. An example would be a patient with acute coronary syndrome with no evidence of high risk for adverse events.
Category 3 represented patients who were potentially suitable for transfer to another medical facility. As a group, the risk was judged too high for simple discharge home. An example would be a stable elderly patient who is progressing well 3 days after hip-fracture surgery. Category 4 patients were those at substantial risk and judged likely to need continued acute-hospital resources. Examples of such patients include those in need of emergency surgery, those in need of pressors, and those in active labour. Finally, category 5 patients were those who might be too unstable or critically ill even for transfer to another appropriate facility. Most of these patients would require specialised medical care. Most patients in intensive-care units would be in this category.
Table 2 shows the consensus list of critical interventions that if withdrawn would result in a consequential medical event. Less than half the critical interventions were assessed as 7 or higher (on a scale of 1–10). Only two-thirds were ranked higher than 5. For every situation, panellists' scoring for critical interventions that were withdrawn compared with those that were not available or withheld was much the same as that for critical interventions that were withheld.
Table 2.
Critical interventions and expert panel consensus of likelihood consequential medical event if procedure or treatment modality withdrawn
| Number who voted | Withdraw*(1–10) | |
|---|---|---|
| CPR or defibrillation | 27 | 10 (10–10) |
| Intubation or airway management | 27 | 10 (10–10) |
| Major surgical procedure or operation | 26 | 9 (8–9) |
| Caesarean section | 27 | 9 (9–10) |
| Intravenous drugs; pressors; fluids | 27 | 8 (8–9) |
| Oxygen dependent | 27 | 8 (7–9) |
| Burn care | 27 | 8 (7–9) |
| Cerebral bolt | 27 | 8 (7–10) |
| Dialysis | 27 | 7 (6–9) |
| Thoracostomy | 27 | 7 (6–8) |
| Non-invasive PPV | 27 | 7 (7–9) |
| Thrombolytic therapy | 27 | 7 (6–8) |
| Transfusion | 27 | 6 (5–7) |
| Other invasive procedure | 27 | 6 (5–8) |
| Psychiatric monitoring | 27 | 6 (4–8) |
| Cardiac catheterisation | 27 | 6 (4–7) |
| Thoracentesis | 27 | 5 (4–7) |
| Wound care | 27 | 5 (4–5) |
| Central line | 27 | 5 (3–5) |
| Incision and drainage | 27 | 5 (4–7) |
| Parenteral nutrition | 27 | 5 (3–5) |
| Paracentesis | 27 | 5 (3–6) |
| Vaginal delivery | 27 | 5 (3–8) |
| Arterial line | 27 | 4 (2–3) |
| Lumbar puncture | 27 | 4 (2–5) |
| Cardiac monitoring | 27 | 3 (2–4) |
| Parenteral pain medication | 27 | 3 (3–4) |
| Support for ADLs | 27 | 3 (2–4) |
CPR=cardiopulmonary resuscitation. PPV=positive pulmonary ventilation. ADLs=activities of daily living.
Median (IQR).
Discussion
We have proposed the notion of in-hospital disposition classification scheme (reverse triage) of inpatients to deal with increased hospital demand during high consequence disasters. A system of patient categorisation based on risk tolerance developed by an expert panel provides a context for further work to determine which patients can be safely discharged early at the time of overwhelming need for hospital-based resources.
High consequent events are disasters that overwhelm local or regional infrastructure including the health system. The need to plan for and increase hospital capacity during high consequence disasters is now a standard recommendation.11, 28 Many techniques have been suggested, such as cancellation of elective admissions and surgeries, opening of licensed but unstaffed beds, use of other spaces that can be readily converted for clinical use, and triage and treat offsite as many victims as possible. Most of these techniques need increased staffing at a time when either staff are not available, staffing is degraded because of the disaster itself, or staff are co-opted by the public-health system for other needs. Volunteer staff who are unfamiliar with hospital routine, remain an untested resource, and have yet to be shown as valuable for augmenting hospital capacity in any disaster. Thus, other ideas for increasing or preserving capacity become important.
Much has been written about the appropriate triage of disaster victims. The focus is to concentrate resources on the most severely injured or ill who are likely to survive with definitive medical care.29, 30, 31 One way to create hospital surge capacity—through reverse triage—has received scant attention. In military terms, reverse triage refers to treating those who are not seriously injured first to allow them to return to the battlefield sooner. Here, we expand the notion to the civilian medical model and include consideration of early discharge of the least sick. With present constraints on hospital capacity, making the most of available resources, rather than hoping that plans to augment them can be implemented, becomes an important consideration.
Patients are generally not discharged from hospitals if a consequential medical event is potentially foreseeable. However, a zero risk policy, although desirable, is not feasible. Forster and colleagues32 report that up to 19% of discharged patients have an adverse event in the immediate (3 week) post-discharge period. Despite a strong patient-safety movement today, zero risk for an out of hospital consequential medical event as a condition of discharge is not attainable, and must be balanced against risk tolerance for various medical adverse events, including iatrogenic ones.27, 32, 33, 34, 35, 36
Despite the accepted risks discussed, our experienced panellists were reluctant to ascribe a substantially higher risk to the category 1 patients. Even the risk tolerance assigned for category 2 patients can be regarded as conservative in view of the complex issues faced in major disasters. If a 12% risk of a consequential medical event is accepted, as was the consensus for category 2, the rate is still much less than the adverse event rate reported by Forster.32
The IQR for votes on categories 1, 2, and 5 were fairly narrow, indicating a cohesive consensus. However, the IQR for categories 3 and 4 were quite wide. Categories 3 and 4 would be unlikely to be discharged.
This report represents the first part of a multiphase study. Once the categories are established, the next step will be to derive a system that allows classification of individual hospital patients in real time. To accomplish this, measurable outcomes and prognostic variables are required. The panel initially defined critical interventions as a means to understand the notions of risk. However, the consensus critical interventions will also serve as the outcome measures in subsequent studies. What constitutes a consequential medical event is subjective. Thus, the critical interventions that are the outcome proxy measures were weighted for likely importance. Future analysis will consider the accuracy of such weighting.
The ultimate goal is to produce a disposition classification system that guides clinical decision making during a disaster in a manner similar to the use of the Apache score24, 26 or PORT score23 in everyday clinical practice. In view of the increasing trend toward electronic medical data, prognostic variables of potential interest—eg, vital signs, key laboratory values, diagnostic considerations, co-morbid conditions—could be captured and continuously updated in real-time. Thus, in the event of a disaster, patients would be predesignated for the lowest risk disposition options, through the use of a system such as the one proposed here. If such a system were in place, each patient would have a continuously, updated reliable risk score to assist in disposition making. Starting with those with the lowest risk, discharges would take place in an ascending order of risk. Furthermore, in the future when prognostic scoring of risk for pre-hospital or emergency-department based disaster triage are developed and reliable, the entire demand for inpatient resources from all sources can be simultaneously ascertained and decisions made accordingly. The value of such a device is not only to augment surge capacity, but also to help with rapid decisions when complete or part hospital evacuations are required, such as happened during Hurricanes Katrina and Rita, and the severe acute respiratory syndrome epidemic in Toronto.
A further and potentially important value of the development of a risk-based disposition classification system is that it is also designed for everyday hospital use. Emergency Departments in many parts of the world are often overcrowded, mainly as a result of severely restricted in-patient capacity. Thus, on a small, but real scale, disaster-like settings arise every day. The device being developed here could have a substantial effect on the safe management of hospital capacity on a routine daily basis.
In fact, preliminary data from the next phase of the study, available at this time, show that such a device might prove useful for such dual purpose. Simulating a disaster, we randomly sampled non-intensive-care unit adult patients from 50 medical units in our three-hospital system during 19 weeks.37 Of the 4781 patients sampled, 786 (16%) were discharged routinely on the day of the disaster. Of the remaining patients, 2797 (70%) either had no critical interventions or were discharged in any event during the next 72 h. Although full analysis remains to be completed, these data are consistent with those reported by Davis and colleagues.38 Physicians and nurses in this study opined that about 50% of patients were dischargeable during 72 h. When controlling for patients in intensive-care, the proportion of capacity is similar to ours. Finally, a study from a tertiary-care teaching hospital in the UK, also using opinion survey of nurses showed that more than a third of inpatient beds (including those in intensive-care units) could be made available within 4–12 h of a disaster if increased care were available in the community.39
The fundamental problem with estimation of capacity on the basis of opinion surveys is absence of evidence that the estimates would result in safe practice. Furthermore, as in the case of the UK study, which called for augmentation of community resources, it is unclear whether these resources could reasonably be increased during catastrophic events. Our approach is to establish the scientific basis for a practice that can be modifiable for use both daily and during catastrophic events.
Comments are needed on concerns that might be raised about the work presented here. The expert panellists were from a wide array of professions. Although many of the panellists have varied geographic and institutional experience, we did not attempt to ensure that every hospital structure and size was represented by all disciplines. Thus, inherent geographic or regional bias in the established ranges of risk tolerance could have occurred. However, as noted, about 25% of the panel were not from our system, and most of the panellists had other national and international experience. Even so, the model described is sufficiently robust that risk tolerance notions can be scaled to an individual hospital and even an individual service. If adopted for daily routine use, risk tolerances for categories 1 and 2 might change or be subject to local customs. We did not consider patient or lay perspectives, but again, the variables of the proposed device can be modified in those settings that wish to consider such views. Also, simulations used here might not represent reality, but most disaster planning is based on simulated exercises due to an absence of empirical data. Furthermore, other systems have been developed on the basis of clinical judgment, in the absence of empirical data. One example is the Abbreviated Injury Scale,40, 41 which was originally based on clinical-judgment ratings, and has subsequently been shown to be both valid and reliable in measuring injury severity. More recently, Hick and O'Laughlin,42 using a less structured consensus format, developed an ethical framework for the distribution of scarce intensive-care-unit resources during disasters.
The 48–72 h period of concern is not arbitrary. Generally local resources are highly stressed for this duration in the aftermath of a severe and sudden disaster.43, 44 In fact, the US Joint Commission on Accreditation of Healthcare Organizations position on hospital preparedness states that hospitals should “ensure a 48–72 hour stand-alone capability through the appropriate stockpiling of necessary medications and supplies.”11 Other systems for augmenting surge capacity resources, including those defined by the National Incident Management System,45 are activated within our period of concern.
Thus, external validation of our approach by the general community is needed, and this report serves as an appropriate foundation for such discussions. The next step is to derive a real-time decision rule or scoring system based on clinical variables that allows accurate categorisation of individual patients, followed by prospective validation.
Acknowledgments
Acknowledgments
This study was sponsored by funding from the Agency for Healthcare Research and Quality (U01 HS14353-01). Data in this manuscript were presented, in part, at the 14th World Congress of Disaster and Emergency Medicine, May 14, 2005, Edinburgh, Scotland.
Contributors
All authors participated in the study concept and design, data collection, statistical analysis, interpretation of data, and writing of the manuscript. G D Kelen was the main investigator and had full access to all the data. All authors have seen and approved the final version.
Conflict of interest statement
We declare that we have no conflict of interest.
References
- 1.Kirschenbaum L, Keen A, O'Neill P. The experience of St Vincent's Hospital, Manhattan, on September 11, 2001: preparedness, response, and lessons learned. Crit Care Med. 2005;33(suppl):S48–S52. doi: 10.1097/01.ccm.0000151067.76074.21. [DOI] [PubMed] [Google Scholar]
- 2.Cushman JG, Pachter HL, Beaton HL. Two New York City hospitals' surgical response to the September 11, 2001, terrorist attack in New York City. J Trauma. 2003;54:147–155. doi: 10.1097/00005373-200301000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Hogan DE, Waeckerle JF, Dire DJ, Lillibridge SR. Emergency department impact of the Oklahoma City terrorist bombing. Ann Emerg Med. 1999;34:160–167. doi: 10.1016/s0196-0644(99)70224-6. [DOI] [PubMed] [Google Scholar]
- 4.Booth CM, Stewart TE. Severe acute respiratory syndrome and critical medicine: the Toronto experience. Crit Care Med. 2005;33(suppl):S53–S60. doi: 10.1097/01.ccm.0000150954.88817.6. [DOI] [PubMed] [Google Scholar]
- 5.May AK, McGwin G, Lancaster LJ. The April 8, 1998 tornado: assessment of the trauma system response and the resulting injuries. J Trauma. 2000;48:666–672. doi: 10.1097/00005373-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Greenwald PW, Rutherford AF, Green RA, Giglio J. Emergency department visits for home medical device failure during the 2003 North America blackout. Acad Emerg Med. 2004;11:786–789. doi: 10.1197/j.aem.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 7.Anderson RJ, Boumbulian PJ, Picken SS. The role of public hospitals in urban health. Acad Med. 2004;79:1162–1168. doi: 10.1097/00001888-200412000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Schafermeyer RW, Asplin BR. Hospital and emergency department crowding in the United States. Emerg Med. 2003;15:22–27. doi: 10.1046/j.1442-2026.2003.00403.x. [DOI] [PubMed] [Google Scholar]
- 9.Schull MJ, Szalai JP, Schwartz B, Redelmeier DA. Emergency department overcrowding following systematic hospital restructuring: trends at twenty hospitals over ten years. Acad Emerg Med. 2001;8:1037–1043. doi: 10.1111/j.1553-2712.2001.tb01112.x. [DOI] [PubMed] [Google Scholar]
- 10.US Government Accountability Office . Hospital preparedness: most urban hospitals have emergency plans but lack certain capacities for bioterrorism response. Government Accountability Office; Washington DC: 2003. [Google Scholar]
- 11.Joint Commission on Accreditation of Healthcare Organizations Health care at the crossroads: strategies for creating and sustaining community-wide emergency preparedness systems, 2003. http://www.ncsl.org/programs/health/ep3-12-03.pdf (accessed May 31, 2005)
- 12.Hick JL, Hanfling D, Burstein JL. Health care facility and community strategies for patient care surge capacity. Ann Emerg Med. 2004;44:253–261. doi: 10.1016/j.annemergmed.2004.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schultz CH, Mothershead JL, Field M. Bioterrorism preparedness I: the emergency department and hospital. Emerg Med Clin North Am. 2002;20:437–455. doi: 10.1016/s0733-8627(02)00003-2. [DOI] [PubMed] [Google Scholar]
- 14.Cocanour CS, Allen SJ, Mazabob J. Lessons learned from the evacuation of an urban teaching hospital. Arch Surg. 2002;137:1141–1145. doi: 10.1001/archsurg.137.10.1141. [DOI] [PubMed] [Google Scholar]
- 15.Norcross ED, Elliott BM, Adams DB, Crawford FA. Impact of a major hurricane on surgical services in a university hospital. Am Surg. 1993;59:28–33. [PubMed] [Google Scholar]
- 16.Mahoney EJ, Harrington DT, Biffl WL. Lessons learned from a nightclub fire: institutional disaster preparedness. J Trauma. 2005;58:487–491. doi: 10.1097/01.ta.0000153939.17932.e7. [DOI] [PubMed] [Google Scholar]
- 17.Avendano M, Derkach P, Swan S. Clinical course and management of SARS in health care workers in Toronto: a case series. CMAJ. 2003;168:1649–1660. [PMC free article] [PubMed] [Google Scholar]
- 18.Ho AS, Sung JJY, Chan-Yeung M. An outbreak of severe acute respiratory syndrome among hospital workers in a community hospital in Hong Kong. Ann Intern Med. 2003;139:564–567. doi: 10.7326/0003-4819-139-7-200310070-00008. [DOI] [PubMed] [Google Scholar]
- 19.Lau JT, Yang X, Leung PC. SARS in three categories of hospital workers, Hong Kong. Emerg Infect Dis. 2004;10:1399–1404. doi: 10.3201/eid1008.040041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schultz CH, Koenig KL, Lewis RJ. Implications of hospital evacuation after the Northridge, California, earthquake. N Engl J Med. 2003;348:1349–1355. doi: 10.1056/NEJMsa021807. [DOI] [PubMed] [Google Scholar]
- 21.US Centers for Disease Control and Prevention Fiscal year 2006 justification of estimates for appropriations committee. Available at: http://www.cdc.gov/fmo/FY2006cdccj.pdf (accessed July 12, 2005)
- 22.Nolen JM. The WALEX process. Johns Hopkins APL Technical Digest 2000; 21: 225–230. www.jhuapl.edu/techdigest/td2102/nolen.pdf (accessed July 12, 2006)
- 23.Fine MJ, Auble TE, Yealy DM. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 24.Lemeshow S, Le Gall JR. Modeling the severity of illness of ICU patients: a systems update. JAMA. 1994;272:1049–1055. [PubMed] [Google Scholar]
- 25.Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–2963. doi: 10.1001/jama.270.24.2957. [DOI] [PubMed] [Google Scholar]
- 26.Knaus WA, Wagner DP, Draper EA. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100:1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine Committee on Quality of Health Care in America . To err is human: building a safer health system. National Academies Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- 28.ACEP Policy Statement Health care system surge capacity recognition, preparedness, and response. Ann Emerg Med. 2005;45:239. doi: 10.1016/j.annemergmed.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 29.Gutierrez de Ceballos JP, Turegano Fuentes F, Perez Diaz D. Casualties treated at the closest hospital in the Madrid, March 11, terrorist bombings. Crit Care Med. 2005;33(suppl):S107–S112. doi: 10.1097/01.ccm.0000151072.17826.72. [DOI] [PubMed] [Google Scholar]
- 30.Rodoplu U, Arnold JL, Tokyay R. Mass-casualty terrorist bombings in Istanbul, Turkey, November 2003: report of the events and the prehospital emergency response. Prehospital Disaster Med. 2004;19:133–145. doi: 10.1017/s1049023x00001643. [DOI] [PubMed] [Google Scholar]
- 31.Almogy G, Luria T, Richter E. Can external signs of trauma guide management? Lessons from suicide bombing attacks in Israel. Arch Surg. 2005;140:390–393. doi: 10.1001/archsurg.140.4.390. [DOI] [PubMed] [Google Scholar]
- 32.Forster AJ, Murff HJ, Peterson JF. The incidence and severity of adverse event affecting patients after discharge form the hospital. Ann Intern Med. 2003;138:161–167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 33.Brennan TA, Leape LL, Laird NM. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324:370–376. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 34.Leape LL, Brennan TA, Laird N. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324:377–384. doi: 10.1056/NEJM199102073240605. [DOI] [PubMed] [Google Scholar]
- 35.Leape LL. Institute of Medicine medical error figures are not exaggerated. JAMA. 2000;284:95–97. doi: 10.1001/jama.284.1.95. [DOI] [PubMed] [Google Scholar]
- 36.McDonald CJ, Weiner M, Hui SL. Deaths due to medical errors are exaggerated in the Institute of Medicine report. JAMA. 2000;284:93–95. doi: 10.1001/jama.284.1.93. [DOI] [PubMed] [Google Scholar]
- 37.Kelen GD, Kraus C, and the CEPAR Research Group Creation of health system surge capacity by the immediate discharge of inpatients. Acad Emerg Med. 2005;12(suppl 1):23. [Google Scholar]
- 38.Davis DP, Poste JC, Hicks T, Polk D, Rymer TE, Jacoby I. Hospital bed surge capacity in the event of a mass-casualty incident. Prehospital Disaster Med. 2005;20:169–176. doi: 10.1017/s1049023x00002405. [DOI] [PubMed] [Google Scholar]
- 39.Challen K, Walter D. Accelerated discharge of patients in the event of a major incident: observational study of a teaching hospital. BMC Public Health. 2006;6:108. doi: 10.1186/1471-2458-6-108. dio10.1186/1471–2458–6–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Committee on Medical Aspects of Automotive Safety Rating the severity of tissue damage: I. The Abbreviated Scale. JAMA. 1971;215:277–280. doi: 10.1001/jama.1971.03180150059012. [DOI] [PubMed] [Google Scholar]
- 41.Committee on Medical Aspects of Automotive Safety Rating the severity of tissue damage: II. The Comprehensive Scale. JAMA. 1972;220:717–720. doi: 10.1001/jama.1972.03200050055013. [DOI] [PubMed] [Google Scholar]
- 42.Hick JL, O'Laughlin DT. Concept of operations for triage of mechanical ventilation in an epidemic. Acad Emerg Med. 2006;13:223–229. doi: 10.1197/j.aem.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 43.Rhodes JD, Carafano JJ. State and regional responses to disasters: solving the 72-hour problem. August 21, 2006. http://www.heritage.org/Research/HomelandDefense/bg1962.cfm (accessed Oct 28, 2006)
- 44.Carafano JJ, Weitz R. Learning from disaster: the role of federalism and the importance of grassroots response. http://www.heritage.org/Research/HomelandDefense/bg1923.cfm March 21, 2006. (accessed Oct 28, 2006)
- 45.Department of Homeland Security National Incident Management System. http://www.nimsonline.com/docs/NIMS-90-web.pdf March 1, 2004. (accessed Oct 28, 2006)