Summary
Background
After a massive syphilis epidemic in the first half of the 20th century, China was able to eliminate this infection for 20 years (1960–80). However, substantial changes in Chinese society have been followed by a resurgent epidemic of sexually transmitted diseases. Sporadic reports have provided clues to the magnitude of the spread of syphilis, but a national surveillance effort is needed to provide data for planning and intervention.
Methods
We collected and assessed case report data from China's national sexually transmitted disease surveillance system and sentinel site network.
Findings
In 1993, the reported total rate of cases of syphilis in China was 0·2 cases per 100 000, whereas primary and secondary syphilis alone represented 5·7 cases per 100 000 persons in 2005. The rate of congenital syphilis increased greatly with an average yearly rise of 71·9%, from 0·01 cases per 100 000 livebirths in 1991 to 19·68 cases per 100 000 livebirths in 2005.
Interpretation
The results suggest that a range of unique biological and social forces are driving the spread of syphilis in China. A national campaign for detection and treatment of syphilis, and a credible prevention strategy, are urgently needed.
Introduction
Syphilis is a very serious infection that causes acute cutaneous manifestations including genital ulcers, chronic severe and debilitating compromise of the cardiovascular and nervous systems, and serious effects on reproductive and neonatal health.1 During pregnancy, syphilis infection can lead to spontaneous abortion, congenital deformities, and severe neonatal disease.
Syphilis was first recognised in mainland China in 1505.2 By the time the Communist party assumed power in 1949, the Chinese people were suffering one of the biggest syphilis epidemics in human history. Surveillance studies in the 1950s showed that the infection was present in as many as 84% of prostitutes and 5% of the general population in some large cities, and 2–3% of rural residents.3, 4
Mao Zedong and his government prioritised health care, and the control of syphilis and other sexually transmitted diseases (STD) was one of their key aims.4 In 1952, China developed an unprecedented and unique campaign to eliminate STD. The government instituted mass screening, provided free treatment to infected individuals, and closed brothels.5, 6 This programme seemed to be highly effective, and studies by Chinese and international teams verified the virtual eradication of STDs by the 1960s.7, 8, 9, 10
However, long-term control of STD in China has proved elusive. Economic and social reforms designed to open China to the world have been successful, but also appear to have laid the foundation for the re-emergence of STD. Increased personal wealth, greater geographical mobility, and more relaxed government control11 set the stage for the spread of STD. The first cases of syphilis in China after the death of Mao were reported in 1979.12
These changes led to the establishment of the Chinese National Center for STD Control in 1986, followed by the launch of a national STD surveillance system by the Ministry of Health in 1987. The purpose of this report is to describe the growth and magnitude of the Chinese syphilis epidemic on the basis of Chinese governmental surveillance data.
Methods
Surveillance of STD is done through mandatory case-reporting from government facilities including STD clinics, designated provincial dermatovenereology centres, gynaecology and genitourinary clinics, maternity and children's hospitals, and other health providers in all 31 provinces, municipalities, and autonomous regions of the country. Beginning in 2005, syphilis case-reporting moved from paper reports to electronic online submission.
For each syphilis case, doctors or their assistants filled out a standardised STD reporting card with demographic (age in 10 year intervals, sex, home location, marital status, occupation, and education), clinical (diagnostic evidence, onset of symptoms, stage of syphilis, presence of other STD), and epidemiological information (route of acquisition). According to national guidelines,13 primary syphilis was defined as a clinically compatible case characterised by one or more chancres and inguinal lymphadenopathy, and laboratory confirmation of Treponema pallidum in clinical specimens by dark-field microscopy or reactive non-treponemal rapid plasma reagin, or toluidine red unheated serum test and treponemal T pallidum haemagglutination, or particle agglutination assay for antibody to T pallidum; secondary syphilis was defined as a clinically compatible case characterised by maculopapular rash and, in many cases, lymphadenopathy, and laboratory test confirmation as for primary syphilis; latent syphilis was defined as an asymptomatic case with a possible history of infection supported by two consecutive reactive non-treponemal tests (rapid plasma reagin), a reactive treponemal test (particle agglutination assay), and normal cerebrospinal fluid; and tertiary syphilis was defined as a case with a history of primary, secondary, or latent syphilis with clinical manifestations involving the cardiovascular or central nervous system and laboratory confirmation with reactive non-treponemal tests, or cerebrospinal fluid abnormalities characterised by higher than normal amounts of white blood cells or protein. A case of congenital syphilis was defined as a neonate or child younger than 2 years affected by associated signs and symptoms such as rash, hepatosplenomegaly, and lymphadenopathy, with an infected mother, supported by detection of T pallidum in lesions by dark-field microscopy or reactive serological test.14
To increase the accuracy with which STD incidence could be assessed, a network of 16 sentinel surveillance sites was established in 1987 in areas with high rates of STD. This network was subsequently expanded in 1993 to 26 sites in various cities throughout China. A map of these sentinel sites is shown in figure 1 . Each site has a designated organisational centre from either the dermatovenereology institute or Center for Disease Control hospital networks that coordinates mandated STD reporting from all STD service providers in their jurisdiction, which is in most places a city district or in some an entire city. These sites have strengthened management, standardised diagnosis and treatment protocols, and established laboratory quality assurance measures, for STD surveillance. By comparing the number of STD diagnoses recorded in clinic and laboratory registries at sentinel sites with case reports in the surveillance system, twice-yearly quality control studies indicate that sentinel sites report all but less than 5% of newly diagnosed STD cases.
Figure 1.
Map of 26 national STD sentinel sites in China
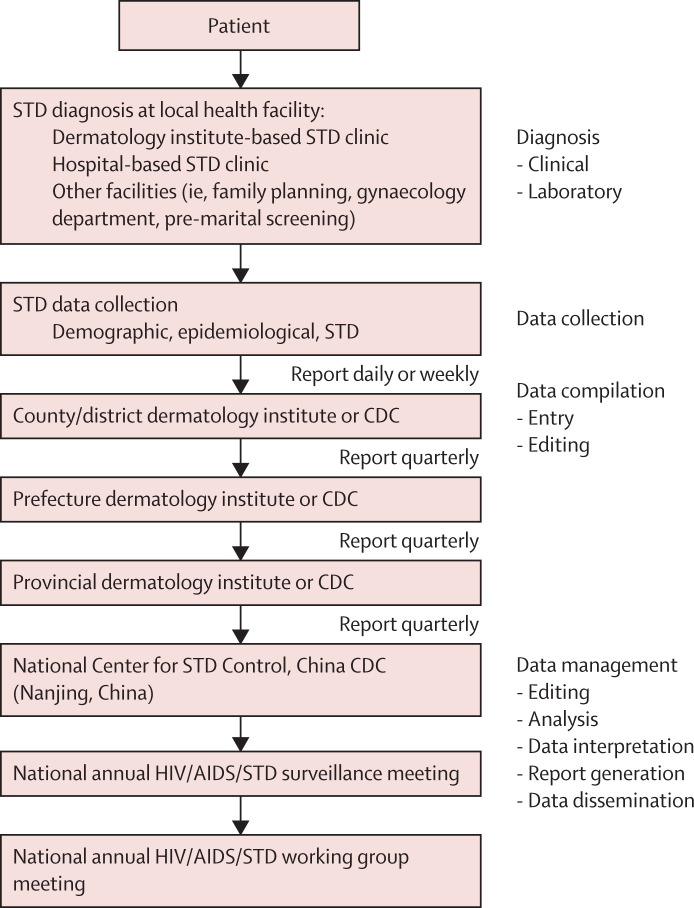
Information from sentinel and non-sentinel sites is collected at the county level and reported quarterly to the next administrative levels until it reaches the National Center for STD Control, where all compiled surveillance data are stored in an electronic database (figure 2 ).
Figure 2.
Reporting structure of China's nationwide STD surveillance system
EpiInfo (Version 1.1, Centers for Disease Control and Prevention, Atlanta, GA, USA) was used to analyse the results in this study.
Total syphilis incidence refers to the number of new syphilis cases at any stage per 100 000 people per year. Because reports based on classification of syphilis into primary, secondary, latent, and tertiary syphilis were not introduced into surveillance reports until 1996, incidence data before this year refer to total syphilis incidence.
The reported incidence of congenital syphilis was calculated by dividing the number of new congenital syphilis cases by the number of livebirths in a specified year. National population and livebirth data were obtained from the National Bureau of Statistics of China.15 The average yearly rate of increase in incidence was calculated as a geometric mean by use of the formula: (incidence at time n divided by incidence at time 1)^(1/[n–1])–1, where n is defined by the interval number of years.
Role of the funding source
The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and the team of co-authors had final responsibility for the decision to submit for publication.
Results
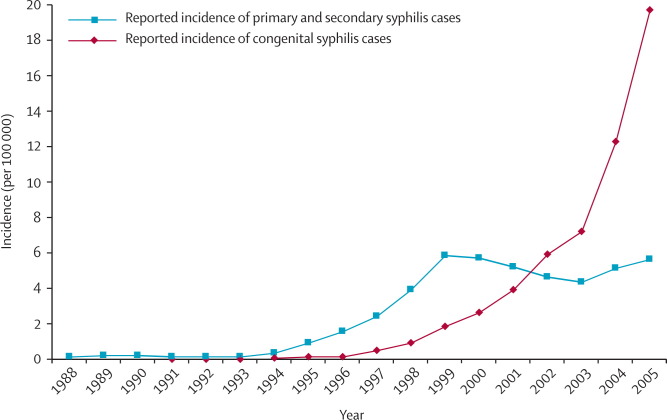
Nationwide surveillance data indicated that after remaining just below 0·2 cases per 100 000 people from 1989 to 1993, the total incidence of syphilis increased from 0·17 cases per 100 000 in 1993 to 6·5 cases per 100 000 in 1999, with incidence of primary and secondary syphilis accounting for 5·85 cases per 100 000 (figure 3 ). After decreasing slightly between 2000 and 2003 (perhaps more a result of administrative changes during that time than a real decline), the incidence of primary and secondary syphilis has increased in the past 2 years to 5·67 cases per 100 000 people. The average incidence of primary and secondary syphilis for the years 2000 to 2005 was 5·13 cases per 100 000 people per year. Incidence of congenital syphilis had grown at a very rapid rate with an average yearly increase of 71·9%, from 0·01 cases per 100 000 livebirths in 1991 to 19·68 cases per 100 000 live–births in 2005 (figure 3). The actual numbers of cases of syphilis classified by the stage of disease are shown in table 1 .
Figure 3.
Reported incidence of congenital syphilis and cumulative primary and secondary syphilis in China from 1988 to 2005, nationwide STD surveillance system
*Aside from congenital syphilis, classification into different stages of syphilis was introduced in 1996. Thus, before 1996, data points for primary and secondary syphilis show incidence for total syphilis. However, an ad hoc survey of syphilis reports in 38 cities from 1990 to 1994 suggested that reported cases of primary, secondary, early latent, tertiary, and congenital syphilis accounted for 20·2%, 46·5%, 28·1%, 2·1%, and 0·7% of total cases, respectively.
Table 1.
Yearly case reports of syphilis classified by stage, nationwide STD surveillance system
| Primary | Secondary | Tertiary | Congenital | Latent | Primary and secondary | Total | |
|---|---|---|---|---|---|---|---|
| 1985 | .. | .. | .. | .. | .. | .. | 184 |
| 1986 | .. | .. | .. | .. | .. | .. | 337 |
| 1987 | .. | .. | .. | .. | .. | .. | 819 |
| 1988 | .. | .. | .. | .. | .. | .. | 1387 |
| 1989 | .. | .. | .. | .. | .. | .. | 1976 |
| 1990 | .. | .. | .. | .. | .. | .. | 2574 |
| 1991 | .. | .. | .. | .. | .. | .. | 1870 |
| 1992 | .. | .. | .. | .. | .. | .. | 1997 |
| 1993 | .. | .. | .. | .. | .. | .. | 2016 |
| 1994 | .. | .. | .. | .. | .. | .. | 4591 |
| 1995 | .. | .. | .. | .. | .. | .. | 11 336 |
| 1996 | 9036 | 9058 | 80 | 35 | 2548 | 18 094 | 20 757 |
| 1997 | 14 134 | 16 085 | 72 | 109 | 3268 | 30 219 | 33 668 |
| 1998 | 23 249 | 25 428 | 143 | 185 | 4760 | 48 677 | 53 765 |
| 1999 | 35 805 | 36 615 | 285 | 359 | 7342 | 72 420 | 80 406 |
| 2000 | 36 075 | 35 424 | 268 | 468 | 7946 | 71 499 | 80 181 |
| 2001 | 32 304 | 33 768 | 199 | 677 | 10 297 | 66 072 | 77 245 |
| 2002 | 29 978 | 29 675 | 277 | 971 | 13 428 | 59 653 | 74 329 |
| 2003 | 30 080 | 26 415 | 327 | 1155 | 14 576 | 56 495 | 72 553 |
| 2004 | 36 420 | 30 058 | 501 | 2035 | 19 297 | 66 478 | 88 311 |
| 2005 | 40 962 | 33 055 | 933 | 3182 | 35 556 | 74 017 | 113 688 |
More than 70% of reported cases of syphilis in the past 10 years were in people aged 20–49 years. The mean ages were slightly higher in northern and central China than in other regions of the country (table 2 ). The ratio of male to female individuals with syphilis decreased from 2·0 to 1·0 between 1988 and 2000, and has held steady for the past 5 years.
Table 2.
Age of people with syphilis in 2005 by region
| Mean age (SD), years | |
|---|---|
| North China (Beijing, Tianjin, Hebei, Shanxi, Inner Mongolia) | 39·2 (15·6) |
| Central China (Henan, Hubei, Hunan) | 39·6 (15·5) |
| Northeast China (Liaoning, Heilongjiang, Jilin) | 37·5 (13·6) |
| East China (Shanghai, Zhejiang, Jiangsu, Anhui, Shandong, Jiangxi, Fujian) | 37·9 (13·5) |
| Northwest China (Shaanxi, Gansu, Ningxia, Qinghai, Xinjiang) | 36·6 (15·2) |
| Southwest China (Yunnan, Guizhou, Sichuan, Chongqing, Xizang) | 37·3 (13·9) |
| South China (Guangdong, Guangxi, Hainan) | 36·6 (14·4) |
| Total | 37·6 (14·1) |
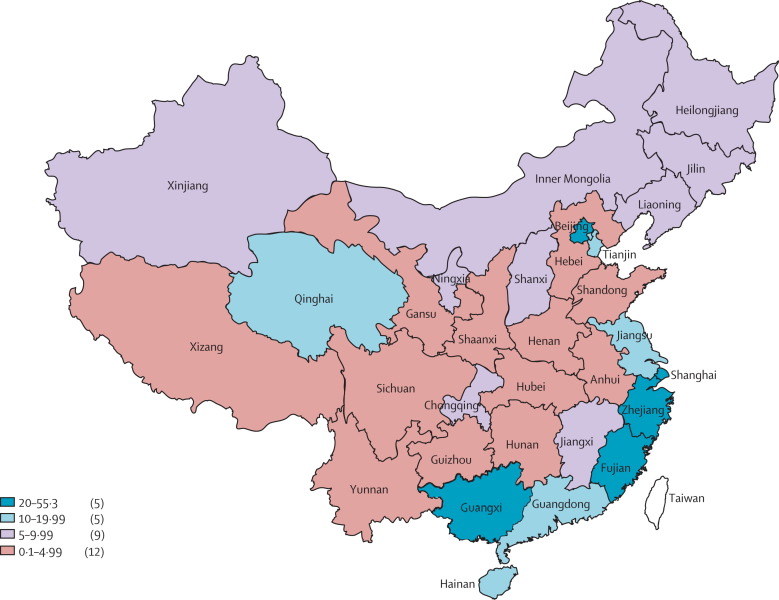
All China's 2882 counties reported cases of syphilis during the past 5 years. In 2005, the highest rates of total syphilis cases were reported in Shanghai (55·3 cases per 100 000 individuals), Zhejiang (35·9 per 100 000), and Fujian (26·8 per 100 000), which together with Jiangsu (13·0 per 100 000) form China's prosperous southeastern seaboard. Beijing municipality had the next highest rate (24·9 per 100 000), followed by the southern Zhujiang River Delta (Guangxi, Guangdong, and Hainan provinces), which reported rates of about 14–21 cases per 100 000 individuals. The northeast provinces (Jilin, Liaoning, and Heilongjiang) and the far western provinces of Qinghai and Xinjiang reported rates of 5–12 cases per 100 000 individuals (figure 4 ).
Figure 4.
Incidence of total syphilis in 2005 by province, nationwide STD surveillance system
Numbers in parentheses show number of provinces in band.
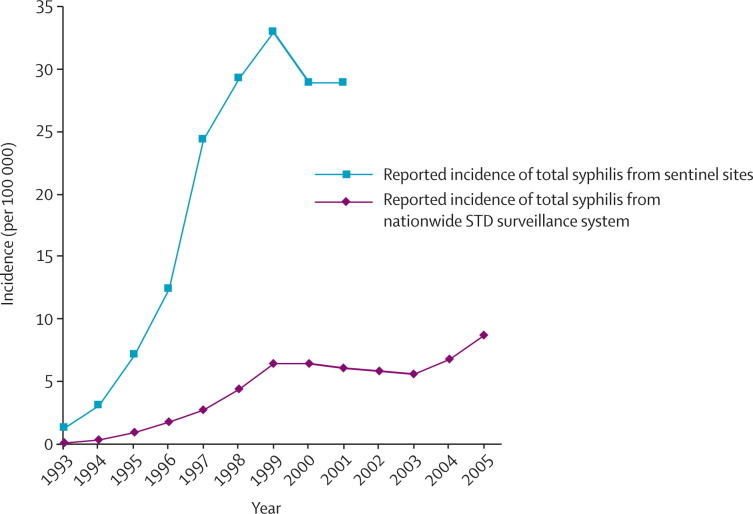
The 26 sentinel STD sites established in 1993 consistently reported a much higher number of cases than did non-sentinel sites. Incidence of total syphilis cases reported by the enhanced surveillance network rose continuously from 1·4 cases per 100 000 individuals in 1993 to 32·9 per 100 000 in 1999 (figure 5 ). Incidence fell slightly in 2000 (28·9 cases per 100 000 individuals) was similar in 2001, paralleling the trend reported by the nationwide surveillance system (figure 5). Despite covering a population of only 35–40 million (about 3% of China's population), the 26 sentinel sites reported about 18% of total syphilis cases from 1995 to 2001.
Figure 5.
Comparison of incidence of syphilis reported by 26 sentinel sites and nationwide STD surveillance system
Discussion
Our report provides a comprehensive view of the re-emergence of syphilis in China. These findings are consistent with reports of the exceptional prevalence of syphilis in high-risk groups in China16, 17, 18 and of the spread of other STD in China,19 including a nationwide cross-sectional survey that showed a high prevalence of chlamydial infection, especially in urban coastal areas.20 Worldwide, resurgence of syphilis in China corresponds to epidemics reported in several cities in the UK,21 Ireland,22 the Russian Federation states,23 and the USA.24
The incidence of primary and secondary syphilis in 2005 (5·67 cases per 100 000) was substantially higher than that in most developed countries; for example, the USA reported 2·7 cases of primary and secondary syphilis per 100 000 individuals in 2004.24 Furthermore, the number of cases cited might not accurately reflect the true extent of the epidemic. STDs treated at hospitals, family planning centres, gynaecological clinics, pharmacies, and private practitioners go largely unreported,25, 26 although these venues represent important access points for patients with STDs. A study in Shenzhen and Guangzhou27 showed that 27% of patients with STDs sought initial care at a site other than a government dermatovenereology centre; in Chengdu28 and Hang–zhou,29 18–40% of patients sought care from private doctors and pharmacists. In an internal, unpublished quality-control study done in 1999, STD surveillance officials found that in one province, more than 75% of STD cases were not reported. Private practitioners were the least reliable, reporting only 0·2% of cases, followed by district-level hospitals (7·9%), provincial-level hospitals (15·4%), and city-level hospitals (35·5%).
Surveillance reporting might also be limited by the availability of governmental resources. The 26 sentinel sites reported about 18% of the nation's aggregate syphilis cases, although these sites cover only 3% of the population. Such results suggest that non-sentinel sites are probably not reporting the actual scale of the epidemic, and that improved surveillance would yield a higher overall incidence than reported here.
As an alternative approach we did a systematic review of published work,17 which suggested the following prevalences of syphilis in specified populations: antenatal women 0·45%; premarital testing 0·66%; voluntary blood donors 0·37%; migrant workers 1·4%; remunerated blood donors 2·86%; possible female sex workers 0·83%; incarcerated female sex workers 12·49%; drug users 6·81%; and men who have sex with men 14·6%.17 In the past 5–10 years, syphilis rates seem to have increased in all these groups, with the greatest increase in drug users (0·96% per year), incarcerated female sex workers (1·41% per year), and men who have sex with men (4·50% per year).17 Surveillance data and focused reports from throughout China provide compelling evidence of a substantial and worsening syphilis epidemic in individuals at high risk, and in the general population.
Syphilis can have devastating health consequences, especially if untreated.1 The increasing privatisation of health care in China has left many people without resources to seek care, particularly for problems like syphilis that on the surface appear to be self-limiting. In a 2004 survey, half the respondents from three provinces reported foregoing health care in the previous year because of its prohibitive cost.30 This proportion is probably much higher in rural areas, as shown by results from one study done in a rural county outside Beijing where 80% of women with symptoms of STD did not seek health care because of its high cost and their own lack of knowledge about STD.31
Obviously, any defects caused by congenital syphilis would be devastating. Additionally, syphilis can contribute to the spread of HIV infection by raising the viral burden in HIV-infected individuals32 and by increasing susceptibility to infection.33 Cotransmission of syphilis and HIV has been reported in Pune, India,34 and syphilis infection in pregnant women might facilitate the vertical transmission of HIV.35 Although the gravity of syphilis during pregnancy cannot be overstated, detection and treatment of the disease could be overshadowed by focus on the prevention of vertical HIV transmission.36
The rapid spread of syphilis in China is probably attributable to a combination of biological and social forces. Grassly and co-workers37 have argued that the extent of syphilis observed in a population most closely indicates the degree of herd immunity. In their analysis of changes in syphilis incidence in the USA over the past 50 years, they concluded that 10-year cycles of disease resurgence could result from depletion of individuals with immunity resulting from natural infection.37 In view of the virtual absence of syphilis in China for 20 years, the general population of young, sexually active individuals would be completely susceptible to this infection.
Social forces could be of even greater importance. Although prostitution in China has an extensive history,38 strict governmental intervention restricted such practices for nearly 40 years.6, 38 However, economic reforms (so obvious in China's growth and globalisation) have led to income gaps and a cultural climate that favours re-emergence of sex work.11 A substantial majority of men and a huge migrant population of male workers have created an increasing demand for sex work.39 It is not a surprise that a high prevalence of syphilis in sex workers has been well documented.16
Sexual practices are also changing. Young Chinese people are increasingly likely to experiment with sex at earlier ages and before marriage.40 Additionally, reduced governmental emphasis on public-health services, increasing costs of individual health care, and reduced availability of health insurance41 might have contributed to reduced recognition and treatment of syphilis.
Clearly, China must attack the spread of STD and especially syphilis. One key component of this intervention is affordable syphilis screening, the tool that proved so powerful in the earliest days of Mao's government.6 The southern city of Shenzhen has pioneered free syphilis screening for all pregnant women, a programme that has been shown to be cost effective and sustainable.42 Further efforts should also be directed at groups in which high syphilis prevalence has been documented, such as men who have sex with men43 and female sex workers.44 Thousands of health centres in China already offer free voluntary counselling and testing for HIV, and additional testing for syphilis in these centres would expand coverage of syphilis screening and help to integrate STD and HIV prevention efforts. However, these strategies will need much support from local and national leaders, as part of the overall urban and rural health reforms.45
STD prevention programmes need to be scaled-up for a mass audience. Preliminary results from the 100% condom use programmes for sex workers promoted in Jiangsu, Hubei, Hunan, Guangxi, and Hainan provinces are favourable, with sharp drops in the prevalence of syphilis in female sex workers.46 These targeted interventions have been complemented by mass education campaigns directed at younger people.
China has recently shown a great interest in the control of infectious diseases. Although the country was perhaps slow to recognise the threat of HIV, this infection is now a key governmental focus for which many active programmes are being developed, including needle exchange and methadone schemes for intravenous drug users, and free medical care for those who are infected with HIV. The resources put into place to control severe acute respiratory syndrome (SARS)47 and avian influenza48 are also impressive.
The spread of syphilis in China has been insidious, and has only recently attracted the attention it deserves. Initial efforts to respond to this epidemic include the pilot screening and prevention programmes and national consultative meetings in 2005 and 2006 that have generated a response strategy and helped to place syphilis on the national agenda. China has shown once before that the control of syphilis is possible,9 and we expect that a new national campaign, although challenging, will show benefit.
Acknowledgments
Acknowledgments
We thank the NIH Fogarty-Ellison Fellowship for providing support for Charles Lin. This work was also funded by the UNC Center for AIDS Research and the UNC STI Clinical Research Center.
Contributors
This project was designed and planned by X-S Chen and M S Cohen. Z-Q Chen and G-C Zhang coordinated data collection and manuscript preparation. Data were collected by X-D Gong, C Lin, X Gao, G-J Liang, and X-L Yue, and analysed by X-D Gong, C Lin, X Gao, X-S Chen, and M S Cohen. C Lin, X Gao, X-S Chen, and M S Cohen drafted and edited the manuscript.
Conflict of interest statement
We declare that we have no conflict of interest.
References
- 1.Golden MR, Marra CM, Holmes KK. Update on syphilis: resurgence of an old problem. JAMA. 2003;290:1510–1514. doi: 10.1001/jama.290.11.1510. [DOI] [PubMed] [Google Scholar]
- 2.Wang JM. Origin of syphilis in China. Chung Hua I Hsueh Tsa Chih. 1923;9:17–20. [Google Scholar]
- 3.Liu MY, Chen YS, Liu HY. Venereal disease screening in Hezuo City of Gannan Tibet Autonomous Prefecture. Chin J Dermatol. 1958;6:76–77. [Google Scholar]
- 4.Horn J. Away with all pests: an English surgeon in the People's Republic of China. Monthly Review Press; New York: 1974. [Google Scholar]
- 5.Cohen MS, Ping G, Fox K, Henderson GE. Sexually transmitted diseases in the People's Republic of China in Y2K: back to the future. Sex Transm Dis. 2000;27:143–145. doi: 10.1097/00007435-200003000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Cohen MS, Henderson GE, Aiello P, Zheng H. Successful eradication of sexually transmitted diseases in the People's Republic of China: implications for the 21st century. J Infect Dis. 1996;174(suppl 2):S223–S229. doi: 10.1093/infdis/174.supplement_2.s223. [DOI] [PubMed] [Google Scholar]
- 7.Cohen MS, Henderson GE. The Chinese hospital: a Socialist work unit. Yale University Press; New Haven: 1984. [Google Scholar]
- 8.Sidel VW. The barefoot doctors of the People's Republic of China. N Engl J Med. 1972;286:1292–1300. doi: 10.1056/NEJM197206152862404. [DOI] [PubMed] [Google Scholar]
- 9.Hu CK, Ge Y, Chen ST. Control and eradication of syphilis in China. Beijing Sci Conference 1964: 167–77.
- 10.Hu CK, Ye GY, Wang GC, Yun GL. Ten years of accomplishments in dermatology and venereology. Chin J Dermatol. 1959;7:290–294. [Google Scholar]
- 11.Gil VE, Wang MS, Anderson AF, Lin GM, Wu ZO. Prostitutes, prostitution and STD/HIV transmission in mainland China. Soc Sci Med. 1996;42:141–152. doi: 10.1016/0277-9536(95)00064-x. [DOI] [PubMed] [Google Scholar]
- 12.Gong XD, Zhang GC, Ye SZ. Epidemiological analysis of syphilis in China from 1985 to 2000. Chin J Sex Transm Infect. 2001;1:1–6. [Google Scholar]
- 13.SBTS/MOH . National standard of the People's Republic of China: diagnostic criteria and management of syphilis (GB 15974-1995) Standards Press of China; Beijing: 1996. [Google Scholar]
- 14.Chang ZQ, Wang QQ, editors. Handbook of sexually transmitted diseases. Shanghai Science and Technology Publishing House; Shanghai: 2004. [Google Scholar]
- 15.National Bureau of Statistics of China National yearly statistical data. http://www.stats.gov.cn/tjgb (accessed July 20, 2006).
- 16.van den Hoek A, Yuliang F, Dukers NH. High prevalence of syphilis and other sexually transmitted diseases among sex workers in China: potential for fast spread of HIV. AIDS. 2001;15:753–759. doi: 10.1097/00002030-200104130-00011. [DOI] [PubMed] [Google Scholar]
- 17.Lin CC, Gao X, Chen XS, Chen Q, Cohen MS. China's syphilis epidemic: a systematic review of seroprevalence studies. Sex Transm Dis. 2006;33:726. doi: 10.1097/01.olq.0000222703.12018.58. 360. [DOI] [PubMed] [Google Scholar]
- 18.Hesketh T, Tang F, Wang ZB. HIV and syphilis in young Chinese adults: implications for spread. Int J STD AIDS. 2005;16:262–266. doi: 10.1258/0956462053420257. [DOI] [PubMed] [Google Scholar]
- 19.Chen XS, Gong XD, Liang GJ, Zhang GC. Epidemiologic trends of sexually transmitted diseases in China. Sex Transm Dis. 2000;27:138–142. doi: 10.1097/00007435-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Parish WL, Laumann EO, Cohen MS. Population-based study of chlamydial infection in China: a hidden epidemic. JAMA. 2003;289:1265–1273. doi: 10.1001/jama.289.10.1265. [DOI] [PubMed] [Google Scholar]
- 21.Brown AE, Sadler KE, Tomkins SE. Recent trends in HIV and other STIs in the United Kingdom: data to the end of 2002. Sex Transm Infect. 2004;80:159–166. doi: 10.1136/sti.2004.009571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hopkins S, Lyons F, Mulcahy F, Bergin C. The great pretender returns to Dublin, Ireland. Sex Transm Infect. 2001;77:316–318. doi: 10.1136/sti.77.5.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Borisenko KK, Tichonova LI, Renton AM. Syphilis and other sexually transmitted infections in the Russian Federation. Int J STD AIDS. 1999;10:665–668. doi: 10.1258/0956462991913240. [DOI] [PubMed] [Google Scholar]
- 24.CDC Primary and secondary syphilis—United States, 2003–2004. MMWR Morb Mortal Wkly Rep. 2002;55:269–273. [PubMed] [Google Scholar]
- 25.Yu AL, Xu CM, Wang J. Survey on under-reporting of STD cases in the first half of 1999 in Gansu Province. Chin J AIDS STD. 1999;6:33–34. [Google Scholar]
- 26.Zhao RL, Zhang ZC, Wang JP. Survey on under-reporting of STD cases in various medical facilities in Yining City in 2001. Chin J AIDS STD. 2003;(suppl):98. [Google Scholar]
- 27.Choi KH, Zheng X, Zhou H, Chen W, Mandel J. Treatment delay and reliance on private physicians among patients with sexually transmitted diseases in China. Int J STD AIDS. 1999;10:309–315. doi: 10.1258/0956462991914177. [DOI] [PubMed] [Google Scholar]
- 28.Lin ZC, Ou ZY, Ma YG. A study of health seeking behavior of 489 STD patients detected by active surveillance. Chin J STD/AIDS Prev Cont. 2001;7:273–277. [Google Scholar]
- 29.Chen YL, Zhou XM, Chen JQ. Research into health care seeking behaviors in STD clinics. Chin J STD/AIDS Prev Cont. 2001;8:237–238. [Google Scholar]
- 30.Lim MK, Yang H, Zhang T, Feng W, Zhou Z. Public perceptions of private health care in socialist China. Health Aff (Millwood) 2004;23:222–234. doi: 10.1377/hlthaff.23.6.222. [DOI] [PubMed] [Google Scholar]
- 31.Zhang HJ, Gao SY, Li FL, Qin Y, Zeng G. Analysis on the situation of RTI prevalence and behavior of health care-seeking in married women in Miyun County. Chin J Family Plan. 2002;5:273–276. [Google Scholar]
- 32.Buchacz K, Patel P, Taylor M. Syphilis increases HIV viral load and decreases CD4 cell counts in HIV-infected patients with new syphilis infections. AIDS. 2004;18:2075–2079. doi: 10.1097/00002030-200410210-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nat Rev Microbiol. 2004;2:33–42. doi: 10.1038/nrmicro794. [DOI] [PubMed] [Google Scholar]
- 34.Reynolds SJ, Risbud AR, Shepherd ME. High rates of syphilis among STI patients are contributing to the spread of HIV-1 in India. Sex Transm Infect. 2006;82:121–126. doi: 10.1136/sti.2005.015040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mwapasa V, Rogerson SJ, Kwiek JJ. Maternal syphilis infection is associated with increased risk of mother-to-child transmission of HIV in Malawi. AIDS. 2002;20:1869–1877. doi: 10.1097/01.aids.0000244206.41500.27. [DOI] [PubMed] [Google Scholar]
- 36.Peeling RW, Mabey D, Fitzgerald DW, Watson-Jones D. Avoiding HIV and dying of syphilis. Lancet. 2004;364:1561–1563. doi: 10.1016/S0140-6736(04)17327-3. [DOI] [PubMed] [Google Scholar]
- 37.Grassly NC, Fraser C, Garnett GP. Host immunity and synchronized epidemics of syphilis across the United States. Nature. 2005;433:417–421. doi: 10.1038/nature03072. [DOI] [PubMed] [Google Scholar]
- 38.Hershatter G. Dangerous pleasures: prostitution and modernity in twentieth-century Shanghai. University of California Press; Berkeley: 1997. [Google Scholar]
- 39.Tucker JD, Henderson GE, Wang TF. Surplus men, sex work, and the spread of HIV in China. AIDS. 2005;19:539–547. doi: 10.1097/01.aids.0000163929.84154.87. [DOI] [PubMed] [Google Scholar]
- 40.Zhang K, Li D, Li H, Beck EJ. Changing sexual attitudes and behaviour in China: implications for the spread of HIV and other sexually transmitted diseases. AIDS Care. 1999;11:581–589. doi: 10.1080/09540129947730. [DOI] [PubMed] [Google Scholar]
- 41.Blumenthal D, Hsiao W. Privatization and its discontents—the evolving Chinese health care system. N Engl J Med. 2005;353:1165–1170. doi: 10.1056/NEJMhpr051133. [DOI] [PubMed] [Google Scholar]
- 42.Cheng JQ. Efficacy of syphilis antenatal screening for 300 000 women in Shenzhen. Sexually transmitted diseases—prevention and control. Shenzhen: Proceedings of the third National STD Congress in the 21st century, 2006: 206.
- 43.Jiang J, Cao N, Zhang J. High prevalence of sexually transmitted diseases among men who have sex with men in Jiangsu Province, China. Sex Transm Dis. 2006;33:118–123. doi: 10.1097/01.olq.0000199763.14766.2b. [DOI] [PubMed] [Google Scholar]
- 44.Ding Y, Detels R, Zhao Z. HIV infection and sexually transmitted diseases in female commercial sex workers in China. J Acquir Immune Defic Syndr. 2005;38:314–319. [PubMed] [Google Scholar]
- 45.Jing F. Health sector reform and reproductive health services in poor rural China. Health Policy Plan. 2004;19(suppl 1):i40–i49. doi: 10.1093/heapol/czh044. [DOI] [PubMed] [Google Scholar]
- 46.WHO . Experiences of the 100% condom use programme in selected countries of Asia. World Health Organization; Geneva: 2004. [Google Scholar]
- 47.Ho D. Is China prepared for microbial threats? Nature. 2005;435:421–422. doi: 10.1038/435421a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Prevention and control of avian influenza in humans in China: achieving the national objectives of the WHO Global influenza Preparedness Plan. Wkly Epidemiol Rec. 2006;81:108–113. [PubMed] [Google Scholar]