Summary
To halt the global tuberculosis epidemic, transmission must be stopped to prevent new infections and new cases. Identification of individuals with tuberculosis and prompt initiation of effective treatment to rapidly render them non-infectious is crucial to this task. However, in settings of high tuberculosis burden, active case-finding is often not implemented, resulting in long delays in diagnosis and treatment. A range of strategies to find cases and ensure prompt and correct treatment have been shown to be effective in high tuberculosis-burden settings. The population-level effect of targeted active case-finding on reducing tuberculosis incidence has been shown by studies and projected by mathematical modelling. The inclusion of targeted active case-finding in a comprehensive epidemic-control strategy for tuberculosis should contribute substantially to a decrease in tuberculosis incidence.
This is the second in a Series of four papers about how to eliminate tuberculosis
Present situation and rationale for change
Tuberculosis is a global epidemic with an estimated 9 million new cases and 1·5 million deaths in 2013.1 Although tuberculosis has been curable for almost 70 years—and despite the fact that millions of individuals are treated every year—the annual rate of decline of tuberculosis incidence globally has averaged only 1·5% for more than a decade.1, 2 Part of the reason for this sluggish progress is that a substantial proportion of people who fall sick with tuberculosis are never diagnosed and treated. WHO estimates that 3 million people with tuberculosis are “missed” each year by health systems, leading to the persistence of infectious cases and the airborne disease's transmission within families and communities.1
Transmission of tuberculosis leads to new infections and new cases of disease. If the global tuberculosis epidemic is to be stopped, not only must existing cases be treated, but the transmission that is constantly producing new infections and cases must also be halted. Trying to eliminate tuberculosis without stopping transmission would be like trying to empty a basin full of water without first turning off the tap that fills it.
Crucial steps to stopping transmission are finding people who have the disease and ensuring that they are immediately put on effective treatment so that they can be rapidly rendered non-infectious. In low-incidence, high-resource settings such as the USA, Canada, and the European Union, policies of targeted active case-finding are in place to limit transmission of tuberculosis in households, communities, and congregate settings.3, 4, 5 Targeted active case-finding means actively seeking out and screening individuals at increased risk of having the disease so that they can be diagnosed early, and, through correct treatment, rendered non-infectious. Targeted active case-finding is a fundamental strategy for disease control that has been used to stop epidemics ranging from smallpox to severe acute respiratory syndrome to Ebola virus disease, and has been recognised as a crucial component of the epidemic-control response to tuberculosis since the 1930s.6, 7, 8
By contrast, most tuberculosis programmes in low-income and middle-income countries with high burdens of tuberculosis have adopted policies that rely on passive case-finding—waiting for the sick to seek care if they are able. Driven in large part by concerns over cost, this strategy prioritises treatment success among passively detected cases and considers case detection to be of secondary importance.9, 10, 11 However, by the time sick individuals seek treatment for their symptoms, they have been infectious for some time, and transmission in the family and community has already occurred.12, 13 The reliance on passive case-finding for tuberculosis has contributed to the present failure to prevent transmission at the level required to turn the tide of the tuberculosis epidemic.12
Key messages.
-
•
Stopping transmission is an essential component of halting the global tuberculosis epidemic; this requires finding individuals with tuberculosis and promptly initiating the correct treatment
-
•
Actively searching for tuberculosis cases in high-risk groups is an efficient and effective way to improve tuberculosis case detection
-
•
Initiation of effective treatment rapidly renders patients non-infectious
-
•
The efficacy of strategies to actively find cases and ensure prompt effective treatment has been shown in high tuberculosis-burden settings
-
•
The ability of targeted active case-finding and prompt treatment to reduce tuberculosis incidence in the population has been suggested by both empirical evaluations and mathematical modelling
-
•
By applying existing knowledge comprehensively and exhaustively to stop the production of new infections and new cases, we can make a substantial impact on the tuberculosis epidemic
Improvement of case detection by actively searching for sick individuals is only the first step in stopping transmission. The second step is to ensure that individuals with tuberculosis are rapidly diagnosed and put on an effective treatment regimen. Delays in diagnosis and treatment contribute to persisting transmission of tuberculosis.12, 13 Diagnostic and treatment policies in high tuberculosis-burden countries have largely relied on conventional sputum smear microscopy as the main diagnostic technique and on a standard empirical treatment regimen of four first-line anti-tuberculosis drugs.14 However, sputum smear microscopy has severe limitations: it fails to detect about half of all tuberculosis cases;15 its sensitivity in children sick with tuberculosis is about 10%;15 its sensitivity in people living with HIV who are sick with tuberculosis is less than 30%;16, 17 it cannot diagnose patients with extrapulmonary tuberculosis, who represented 15% of notified cases in 2013;1 and it cannot detect drug resistance. Furthermore, although cases that are detectable by sputum smear microscopy are generally more infectious than those that are not, the non-detectable cases have been shown to cause 13–17% of transmission in low-incidence settings.18, 19 Reliance on smear microscopy rather than more sensitive procedures for diagnosis thus allows infectious cases to remain undetected in the community for longer. In addition, policies that rely on both sputum smear microscopy and empirical treatment with a standard first-line anti-tuberculosis regimen can result in long periods of ineffective treatment for patients with drug-resistant tuberculosis.
The tuberculosis epidemic cannot be successfully and rapidly curbed without use of recognised control measures for communicable diseases, including targeted active case-finding and prompt initiation of the correct treatment. These activities are both feasible and effective in high tuberculosis-burden settings at present, despite the challenges facing health systems in many of these countries. Thus, with adequate resource investment and political will, substantial decreases in tuberculosis incidence are possible.
Data and successes
Since the 1930s, a range of approaches to targeted active case-finding, tailored to local epidemiology, have been shown to improve tuberculosis case detection.6, 20, 21 By focusing on populations at high risk for tuberculosis, targeted active case-finding strategies detect substantially more cases per number of people assessed than would be detected by screening in the general population. The expected yields of a few common approaches are described in table 1 .
Table 1.
Expected yields for different active case-finding strategies
| Expected prevalence of newly diagnosed tuberculosis in people assessed | |
|---|---|
| Household contact investigation in low-income and middle-income countries22, 23, 24 | 1–5% |
| Screening of outpatients in general health-care facilities in high tuberculosis-burden settings for tuberculosis symptoms and assessment of symptomatic individuals25, 26, 27, 28, 29, 30 | 5–10% |
| Screening of people receiving HIV-associated health care in low-income and middle-income countries with HIV prevalence of more than 5%31 | 1–25% |
| Untargeted screening in general population in 22 high tuberculosis-burden countries1 | 0·1–0·7% |
Once a tuberculosis case is identified, further transmission from that individual can be stopped almost immediately by initiation of effective treatment. A seminal prospective, randomised, controlled study32 done at the Tuberculosis Chemotherapy Center, Madras (now Chennai), India, in the 1950s reported that household members of patients with tuberculosis who were treated at home had no greater risk of tuberculosis disease or infection after 5 years than household members of patients who were treated in sanatoria and thus restricted from contact with their families. Furthermore, since the 1950s, independent studies have measured the infectiousness of patients with tuberculosis who were being treated in hospital using an experimental model in which highly susceptible guineapigs were exposed to the air from a ward of patients with tuberculosis, and then tested for tuberculosis infection. These experiments repeatedly showed a rapid reduction in the patients' infectiousness after initiation of effective therapy, even while they might remain sputum smear positive.33, 34, 35 In the earliest experiments, patients began treatment on the day of admission to the hospital; guineapigs exposed to patients who started effective treatment for drug-susceptible tuberculosis were only 2% as likely to be infected as guineapigs exposed to untreated patients, suggesting that the patients were rendered non-infectious almost immediately after initiation of multidrug therapy.33 In later studies using a similar experimental set-up, rapid attenuation of infectiousness was reported for patients with drug-resistant tuberculosis who were treated effectively with regimens that contained sufficient drugs to which the infecting strains were susceptible.34 By contrast, these guineapig exposure studies have repeatedly reported most infections to be associated with patients who have undiagnosed or ineffectively treated drug-resistant tuberculosis, underscoring the importance of rapid initiation of the correct regimen and the danger of protracted infectiousness in these patients.33, 34, 35, 36 Epidemiologically, the continuing transmission of drug-resistant strains that results from diagnostic failure or an absence of effective treatment is suggested by the prevalence of drug resistance in patients who have never been treated for tuberculosis; across the WHO European Region in 2013, 14% of patients without previous treatment had multidrug-resistant tuberculosis.1
The combination of active case-finding and prompt initiation of effective treatment reduces transmission by removing infectious cases from the population before additional transmission occurs. Although the effect of these activities at a population level is difficult to measure over a short timeframe, evidence suggests that they have a role in reducing tuberculosis incidence. In a community-randomised trial in Brazil, eight communities matched according to socioeconomic indicators were assigned to either an intervention or control condition. In the intervention communities, outreach workers actively sought out household contacts of tuberculosis cases for prompt screening, and treatment was given for both tuberculosis disease and infection.37 The control communities received the local standard of care, which relied on contacts to present to health facilities for assessment, and did not routinely provide preventive therapy. At baseline, the two sets of communities had nearly identical annual tuberculosis case notification rates (340 cases per 100 000 individuals in communities receiving the intervention and 339 per 100 000 in the controls). After 5 years, the intervention communities had a statistically significant 15% lower annual tuberculosis case notification rate than the control communities (p=0·04). A community-randomised trial in Zambia and South Africa allocated 24 communities to four intervention conditions involving different combinations of case-finding interventions such that each group was similar with respect to baseline prevalence of tuberculosis and HIV infection, and demographic characteristics.38 After 3 years, communities in which household contacts of patients with tuberculosis were systematically assessed had an 18% lower prevalence of tuberculosis in adults (p=0·095) and a 55% lower rate of tuberculosis infection in children (p=0·063) than communities in which household contacts were not assessed.
Translation of knowledge into strategy and action
Key strategies to consider
Targeted active case-finding and prompt initiation of effective treatment are crucial components of epidemic control for infectious diseases. Although optimum methods for both can vary across settings, general strategies that have proven effective in a range of settings can provide a starting point for implementation. Table 2 presents key activities and strategies to be considered for stopping tuberculosis transmission in the context of a comprehensive approach to stopping the tuberculosis epidemic.
Table 2.
Key activities and strategies to be considered for prevention of tuberculosis transmission
| Strategies | |
|---|---|
| Targeted active case-finding | Perform contact investigations of patients with tuberculosis Screen clients attending health facilities Use programme data to identify groups of people that account for a disproportionate share of the tuberculosis burden; groups can be defined by individual risk factors or geography Consider, pilot, and assess different targeted active case-finding strategies to find out what works best in a given setting Increase uptake of screening through awareness campaigns, community engagement, initiatives to mitigate stigma, and incentives |
| Prevention of transmission in health facilities | Provide paper masks to individuals suspected of having tuberculosis until they are receiving effective treatment Reduce contact between individuals suspected of having tuberculosis and other people seeking care, particularly susceptible individuals such as young children and people with HIV; contact can be reduced by having patients wait in different areas on the basis of risk and symptoms, or by scheduling clinics for different types of patients at different times Expedite diagnosis for individuals suspected of having tuberculosis Open windows in waiting areas or use outdoor waiting areas where feasible |
| Prompt initiation of effective therapy | Develop protocols and strengthen health systems to ensure that results of diagnostic procedures are received and acted on promptly Use chest radiography and clinical algorithms in addition to bacteriological testing for diagnosis, especially for young children and people with HIV Use rapid molecular tests that can detect both tuberculosis and drug resistance Initiate presumptive treatment for drug-resistant tuberculosis when a contact of a patient with drug-resistant tuberculosis is diagnosed with tuberculosis |
| Formation of partnerships | Integrate tuberculosis care with other health-care services such as HIV care and maternal-child health programmes Engage community members who advocate for best practices, encourage health-care-seeking behaviours, and support patients through treatment Partner with private sector providers to ensure that patients with tuberculosis receive timely diagnoses and appropriate treatment, and that they are reported to the national tuberculosis programme even if they receive care in the private sector |
Active case-finding in high-risk groups
In view of the inability of passive case-finding alone to halt tuberculosis transmission, targeted active case-finding is important in all settings. However, different characteristics are associated with increased tuberculosis risk in different places, and the efficacy of any single approach to active case-finding can vary widely across settings.20 Thus, each tuberculosis programme has to identify what combination of targeted active case-finding activities is the most effective in the local context.
One high-risk group that is present in all settings is contacts of patients with tuberculosis. Contact investigation refers to the process of systematically identifying and screening contacts of patients with tuberculosis.39 Since the risk of transmission increases with the intensity and duration of contact, contact investigation in the household and other places where patients with tuberculosis live (eg, workers' dormitories, prisons) is a logical case-finding strategy to consider in all countries. Common components of contact investigations include patient interviews in the clinic, asking patients to bring household members and other close contacts (particularly children) to the clinic for assessment, and home visits by a health-care worker to identify and screen household members. Although programmes generally prioritise the most infectious cases for contact investigation, investigations of children, who generally have non-infectious forms of tuberculosis, can lead to detection of infectious adult cases; this is sometimes called a source case investigation since transmission is assumed to have occurred from the adult to the child. At a children's hospital in Texas, USA, 17–24% of children diagnosed with tuberculosis were accompanied to the hospital by an adult with previously undiagnosed pulmonary tuberculosis.40, 41
Another generally applicable strategy for targeted active case-finding is regular screening of social or demographic risk groups that contribute a disproportionate number of cases to the local tuberculosis burden (panel ). This strategy is important in both low-burden settings and high-burden settings. Analysis of routinely collected programme data can help identify high-risk groups in a particular location. Furthermore, in some high-burden settings, analysis of programme data can identify geographical hotspots where community-level interventions such as door-to-door screening and deployment of mobile diagnostic units could be a high-yield activity (see Theron and colleagues,46 paper 1 in this Series). In countries where genotyping is practised, such as China, the combination of genotype and geographical data might allow even more specific identification of transmission hotspots.
Panel. Examples of targeted active case-finding policies in risk groups that contribute disproportionately to local tuberculosis burden.
Across the WHO African Region in 2013, the prevalence of HIV in adults aged 15–49 years was 4·5%,42 but an estimated 34% of tuberculosis cases were associated with HIV.1 Screening people with HIV for tuberculosis is therefore a crucial strategy for tuberculosis case detection.
In Russia, about 0·5% of the population is incarcerated. However, prisoners accounted for 27% of tuberculosis cases in 1995.43 Since then, Russia has focused on addressing tuberculosis in prisons, enforcing both mandatory screening and directly observed treatment.43 These policies have been credited with reducing the proportion of tuberculosis cases that were detected in prisons to 12% in 2004.
In the USA, tuberculosis incidence among homeless people is roughly 10 times the incidence in the general population.44 National guidelines recommend that staff in homeless shelters monitor clients for persistent cough and ensure prompt assessment either at the shelter or by providing transportation to a health-care facility.45
One practical consideration for the implementation of targeted active case-finding activities is how to convince individuals to undergo screening for a stigmatised disease, especially if screening requires time and effort on the part of the individual. Strategies that have proven successful at encouraging uptake of services for other stigmatised health issues (eg, HIV, leprosy) have included coupling services for a stigmatised health issue with services for a non-stigmatised one, and community-based awareness campaigns to reduce stigma.47 Several successful active case-finding initiatives for tuberculosis have incorporated advocacy and community mobilisation activities into their strategies.20 Material incentives can also be useful in encouraging people to undergo screening; two randomised controlled trials in the USA reported that small monetary incentives doubled the proportion of homeless people who returned to the clinic to have their tuberculin skin tests read.48
Another practical consideration is what screening and diagnostic algorithm to use. Strategies for targeted active case-finding typically use screening algorithms that progressively reduce the number of individuals at each step of assessment to ensure that time-intensive and resource-intensive procedures such as sputum culture and full clinical assessment by a physician are done for individuals who are likely to have tuberculosis. A common first step is to ask individuals about symptoms and risk factors, and move only those who are symptomatic or high risk to the next step of assessment. However, the choice of symptoms included in the initial interview can greatly affect the performance of the symptom screen, with trade-offs between sensitivity and specificity. In a prevalence survey in western Kenya,49 where the prevalence of bacteriologically confirmed pulmonary tuberculosis was 0·6%, the presence of cough for 2 weeks or longer had 52% sensitivity and 89% specificity in predicting tuberculosis, whereas the presence of any tuberculosis symptom (cough, haemoptysis, weight loss, fever, or night sweats) had 90% sensitivity and 32% specificity. Furthermore, for children, additional symptoms such as reduced playfulness and failure to reach an age-appropriate weight are important components of a symptom screen. Finally, the comparatively high sensitivity (94%) and specificity (73%) of an abnormal chest radiograph for predicting tuberculosis in the western Kenya survey49 (with similar results reported from other prevalence surveys) strongly supports inclusion of chest radiography into screening algorithms.
The decision to implement targeted active case-finding activities has practical implications for the tuberculosis programme and the health system as a whole. Active case-finding activities require staff and diagnostic resources in addition to those already in place to support passive case-finding. Additionally, if active case-finding activities are successful, the number of patients requiring treatment will increase in the short term, even though subsequent reduction in transmission should reduce the number of cases in the long term. Therefore, anticipation of increased diagnostic and treatment capacity should be part of the planning process for any active case-finding activity. Furthermore, monitoring and assessment should be planned to ensure that the people screened by an active case-finding initiative are those at the highest risk rather than those who are easiest to reach, and that increases in diagnoses represent true case detection and not overdiagnosis. Finally, while active case-finding activities have as their main goal the prompt diagnosis and treatment of tuberculosis disease, they can also provide a platform for the diagnosis and treatment of tuberculosis infection and exposure to prevent development of future cases (see Rangaka and colleagues,50 paper 3 in this Series). Therefore, the coordination of case-finding and prevention efforts should be considered.
Prevention of transmission in health-care facilities
Health facilities are a unique setting in which targeted active case-finding can be combined with administrative and environmental infection control measures to prevent nosocomial tuberculosis transmission. Facilities where individuals who are sick spend hours waiting for health care in crowded and poorly ventilated waiting areas can promote transmission within the facility. Detection of these cases as soon as possible is thus crucial to prevent transmission. One strategy to identify cases and prevent nosocomial transmission is to screen individuals in waiting areas for tuberculosis symptoms and quickly separate symptomatic individuals from the general population. This type of rapid triage was instrumental in halting nosocomial transmission during the 2003 outbreak of severe acute respiratory syndrome in Asia.7
For tuberculosis, the strategy “Finding TB cases Actively, Separating safely, and Treating effectively” (FAST) has helped facilities introduce procedures that reduce the risk and duration of exposure to tuberculosis for both patients and health-care workers.51 The FAST strategy includes cough monitoring in waiting rooms and admission wards to identify individuals who might have tuberculosis, rapid diagnosis for those with tuberculosis symptoms, prompt separation of patients with suspected drug-resistant tuberculosis, and rapid initiation of effective treatment for all forms of tuberculosis. Although designed for health-care facilities, the FAST strategy could be adapted to other congregate settings as well.52 Additionally, a range of administrative and environmental interventions can further augment efforts to prevent transmission within facilities, without substantial additional resource investment (table 3 ).
Table 3.
Administrative and environmental strategies for airborne infection control
| Example of implementation | |
|---|---|
| Requesting that patients with tuberculosis wear surgical masks | When admitted to hospital, patients receiving multidrug-resistant tuberculosis treatment at the Airborne Infections Research Facility in Emalahleni, South Africa, were asked to wear surgical masks during the day, excluding mealtimes; infectiousness of air from the ward was reduced after the intervention53 |
| Manipulation of clinic schedules to reduce risk of transmission to susceptible individuals in waiting rooms | At the Indus Hospital in Karachi, Pakistan, before the establishment of a separate tuberculosis clinic, clinic schedules were arranged so that no paediatric clinics were run on days during which patients with tuberculosis were seen (personal experience of FA). |
| Opening windows or doors, or both | In various hospital spaces in Lima, Peru, the amount of ventilation was nearly 20 times higher when windows and doors were opened than when they were closed. With open windows and doors, these spaces were better ventilated than spaces with mechanical ventilation systems (eg, fan-based systems)54 |
Implementation of the FAST strategy in hospitals has reduced both unsuspected tuberculosis and delays in the initiation of effective treatment. After implementing FAST, the National Institute of Diseases of the Chest Hospital in Dhaka, Bangladesh, reported that 9% of patients admitted as so-called non-tuberculosis patients in fact had tuberculosis.51 In a tuberculosis hospital in Voronezh, Russia, implementation of FAST using a molecular diagnostic test reduced the time from admission to initiation of multidrug-resistant tuberculosis treatment to less than 5 days, compared with the weeks that patients would wait to receive results from mycobacterial culture and conventional drug susceptibility testing.51
Diagnosis and prompt initiation of effective treatment
The FAST strategy provides an integrated and streamlined approach that combines active case-finding, diagnosis, and treatment into a single facility-based protocol. When active case-finding is focused outside a health-care facility, strategies are needed to ensure that individuals identified as being at risk for tuberculosis are linked to appropriate diagnosis and treatment, since searching for cases will not have any effect unless these cases are promptly diagnosed and effectively treated.
In view of the limitations of sputum smear microscopy, the goal to diagnose all tuberculosis cases can only be accomplished through the use of other modalities such as radiography, molecular diagnostic tests, bacteriological culture, and clinical algorithms.21 Because children and people with HIV are less likely than others to have bacteriological confirmation of tuberculosis, use of clinical algorithms for these two groups is essential.55, 56, 57 In the future, rapid biomarker-based tests that do not rely on detection of bacteria in sputum could improve the speed and accuracy of diagnosis, particularly in children and people with HIV. Technologies under development at present include antigen detection tests and tests to analyse volatile organic compounds in breath or urine.58
Failure to suspect or identify drug resistance at the time of tuberculosis diagnosis can result in patients receiving inadequate treatment regimens, which prolongs both illness and infectiousness and potentially causes amplification of drug resistance.59, 60 Patients can deteriorate and remain infectious for months in places where policies allow treatment for drug-resistant tuberculosis to be considered only after a patient has been unsuccessfully treated with a first-line regimen. Therefore, use of new molecular diagnostic tests to rapidly diagnose drug resistance and presumptive treatment for drug-resistant tuberculosis are both integral to stopping transmission of drug-resistant strains. Molecular diagnostic tests can detect drug resistance in hours or days rather than the weeks needed for conventional culture-based drug susceptibility testing. In settings with high prevalence of drug resistance, such as Russia, Peru, and various southern African settings, universal drug susceptibility testing using molecular tests has been shown to be feasible, reducing the time to diagnosis of drug resistance and initiation of second-line treatment.51, 61, 62 In settings with low rates of drug resistance in the general tuberculosis patient population, rapid molecular testing of people suspected of having tuberculosis or patients meeting certain criteria for being at an increased risk of drug resistance (eg, contacts of an individual with drug-resistant tuberculosis, individuals with a history of tuberculosis treatment, patients not responding to treatment, and refugees) has proven to be a feasible intermediate step toward universal drug susceptibility testing.
Standardised risk criteria can also be used to identify individuals who should receive treatment for drug-resistant disease, even in the absence of a drug susceptibility test result. For example, high concordance of drug susceptibility test pattern has generally been reported between the index case and secondary cases within households of patients with drug-resistant tuberculosis.63 Therefore, presumptive treatment for drug-resistant disease is warranted for household members of patients with drug-resistant tuberculosis who are themselves diagnosed with tuberculosis, especially young children who are most likely to not have bacteriological confirmation and be infected with the same strain as the index patient.
Even a perfect diagnostic technology or algorithm cannot have an effect on transmission if patients are not rapidly started on treatment. Thus, not only is the method of diagnosis important to consider, but also the timeliness and ease with which patients receive diagnostic results and are linked to care. High rates of failure to initiate treatment after diagnosis have been reported in a range of settings.64 Sometimes, gaps in the health-care delivery system can lead to a failure to communicate test results or an absence of action based on these results.65, 66 In KwaZulu-Natal, South Africa, only 20% of patients with rifampicin-resistant tuberculosis had started tuberculosis treatment within 2 weeks of testing using the Xpert MTB/RIF assay, which yields results within hours.67 In other situations, patients themselves might decline treatment despite receiving a diagnosis of tuberculosis, particularly if they have no or mild symptoms or if treatment interferes with their ability to work. Nearly a quarter of patients diagnosed with sputum smear-positive tuberculosis during a community survey in India did not initiate treatment, with the two most common reasons being lack of interest in treatment and having symptoms too mild to warrant treatment.68 Therefore, strategies are needed to ensure that all individuals diagnosed with tuberculosis are informed of their diagnoses, counselled appropriately, and promptly treated. Strategies could include the collection of accurate contact information during the initial diagnostic encounter, optimisation of diagnostic procedures and communication systems to reduce time to diagnosis and treatment, active follow-up of people who do not initiate treatment, incentives for initiation of treatment, and oversight and support for individuals requiring it during treatment. In some countries, regulations exist that allow a tuberculosis programme to compel a patient to accept treatment despite his or her refusal; the decision about how to balance the rights of a patient with the public health system's mandate to protect the public is complex and warrants careful consideration.69
Partnerships to extend case-finding and care
A health-care system that requires patients to seek or receive tuberculosis care within specific tuberculosis-focused settings or programmes might result in patients spending substantial time and effort accessing tuberculosis care, in addition to their other health-care needs. This burden can discourage patients from either seeking or remaining in care. Thus, a system that makes it easier for patients to access tuberculosis services in conjunction with other health-care services would probably improve both case detection and the probability of treatment initiation and completion.
Many logical points of integration between tuberculosis services and other health-care services exist. The FAST strategy offers one example of a way to integrate tuberculosis screening into primary care settings. Additionally, integration of tuberculosis and HIV services by use of a range of approaches is widely advocated, and is an obvious area for improvement in many countries with high burdens of both diseases. Maternal-child health programmes (including Integrated Management of Childhood Illness screening programmes and malnutrition clinics) provide a platform to offer tuberculosis treatment or preventive therapy to young children.70 Other important points of contact include clinics treating patients with diabetes, chronic obstructive pulmonary disease, or lung disorders associated with smoking, all of which are associated with an increased risk of tuberculosis.71, 72, 73, 74 Achievement of this sort of coordination of care will require tuberculosis programmes to partner with other stakeholders in the general health services rather than working in isolation.
Partnerships outside the public health-care sector can also improve the effectiveness of many of the strategies discussed thus far. For example, engagement of community members who advocate for best practices, encourage health-care-seeking behaviours, and support patients through treatment can help ensure that interventions initiated by the tuberculosis programme have wide-reaching and sustained effect. Additionally, partnerships with other government sectors, such as those in charge of prisons or social welfare programmes, can ease access to vulnerable or hard-to-reach populations. Finally, partnerships with the private sector are necessary in settings such as south Asia, where 80% of patients seek care from private providers.75 In view of the large number and the heterogeneity of private providers, it is an immense undertaking for national tuberculosis programmes to effectively engage these providers to ensure that patients with tuberculosis receive timely diagnoses and appropriate treatment, and that all tuberculosis cases are reported to the national tuberculosis programme even if they are diagnosed and treated in the private sector. Although strategies will vary across settings, some approaches that have proven successful include use of large private hospitals with associated clinic networks as reporting centres for the national tuberculosis programme; use of mobile phone-based platforms to help report screening or diagnostic results from private facilities; and mass media campaigns that give publicity to private facilities that have partnered with the national programme to offer testing and treatment.29, 75
Projection of impact
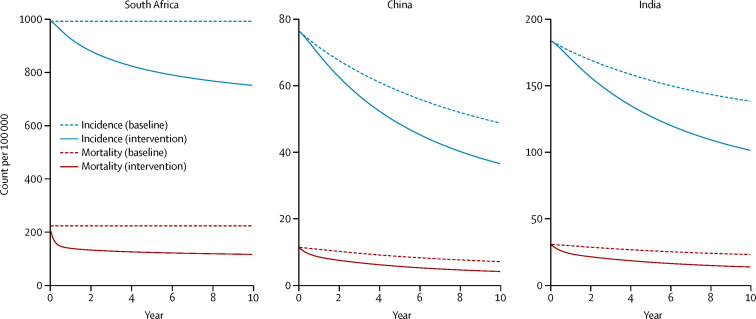
What impact would be expected from a commitment to identify and treat more people with tuberculosis than is achieved at present? Models consistent with the present tuberculosis epidemics in China, India, and South Africa predict that an increase in case detection by 25% can achieve a 40–44% reduction in tuberculosis-associated mortality, a 22–27% reduction in incidence, and a 30–33% reduction in prevalence in 10 years (figure ).76 Furthermore, these interventions were deemed to be highly cost effective, even if the costs of the interventions were as high as US$2500 per case detected in India, and $5000 per case detected in China and South Africa. Importantly, these projections show that the population-level benefits of active case-finding accumulate with time since removal of infectious cases from the population prevents the development of additional cases in both the near-term and long-term future; thus an assessment at the end of 1 year is unlikely to show a substantial effect, even though the 10 year projected benefit is substantial. These projections assume that detection is synonymous with prompt and effective treatment, so all case-finding has to be directly linked to the immediate delivery of care.
Figure.
Projected impact of sustained active case-finding after 10 years in China, India, and South Africa76
Impact represents reduction after 10 years compared with baseline, assuming an active case-finding programme that detects and treats 25% more cases than would otherwise be detected and treated in view of present epidemiological trends in each country. The additional cases detected are assumed to come from a homogeneous population, with detection occurring at a random point of disease progression. Figure courtesy of David Dowdy.
Achievement of a 25% increase in case detection is feasible in view of the strategies already discussed. Of 19 active case-finding initiatives, each lasting 1 year, undertaken in 11 countries, the median increase in notification rates of sputum smear-positive tuberculosis cases was 35%, after controlling for historical trends in case notification rates and changes in case notification rates in control populations that did not receive the interventions.20 In one of these initiatives, undertaken in Karachi, Pakistan, a combination of screening outpatients in clinics and a mass communication campaign encouraging people with prolonged cough to seek care more than doubled the case notification rate in the intervention area compared with the control area.29 A model consistent with local tuberculosis epidemiological data projected that if the level of case detection achieved during the intervention year were maintained, 24% of the tuberculosis cases and 52% of the tuberculosis deaths that would have occurred in the absence of the intervention would be averted in 5 years; even if the level of case detection were to fall back to baseline immediately after the intervention year, 13% of cases and 25% of deaths would be averted.77
Conclusion
Stopping an epidemic requires stopping transmission. For an airborne disease without an effective vaccine, stopping transmission requires finding all cases promptly and rendering them non-infectious through treatment. The only way to accomplish this is to search actively for cases, use effective diagnostic methods and algorithms, initiate patients promptly on the correct therapy, and support them through to cure. The knowledge necessary to do these activities exists and successes have been documented across a range of settings.
While major changes to existing policies and care delivery systems will take time, action in the near future is possible. Some administrative and environmental interventions, such as providing individuals suspected of having tuberculosis with surgical masks until treatment begins and, where practical, opening windows in health facilities, can be implemented immediately without changes to existing systems or large investment of resources. Others, such as performing basic household contact investigations, implementation of the FAST strategy, and expansion of the use of molecular diagnostics, will require some additional human resources, training, and capacity building, but can be rapidly accomplished within the context of existing health-care delivery systems. Still others, such as integration of health-care services, have a slightly longer timeframe because they require the development of partnerships and the reorganisation of existing systems. The development and deployment of new point-of-care diagnostic technologies could accelerate these efforts by making diagnosis easier in the future.
By applying existing knowledge comprehensively and exhaustively, we can stop the production of new tuberculosis infections and cases and make a substantial impact on the epidemic. These efforts would certainly be aided and enhanced by the development of new diagnostic tests, vaccines, and treatments. However, with sufficient commitment of resources, engagement with stakeholders outside national tuberculosis programmes, and careful planning to ensure that all the components of a new comprehensive strategy are coordinated, tuberculosis rates can be substantially reduced.
Acknowledgments
Acknowledgments
This work was supported by a grant from Janssen Global to Harvard Medical School (CMY, SK, MCB); the Global Fund (FA); TBREACH (FA); and the US National Institutes of Health (award K23 AI084548 to AD). The funders had no role in the conception, preparation, review, approval, or submission of this manuscript. The content is solely the responsibility of the authors and does not necessarily represent the views of the US National Institutes of Health or any other funding body. We thank Carole Mitnick for her review and the important comments she contributed during drafting, and Carly Rodriguez for coordination and research assistance in the preparation of this Series paper.
Contributors
CMY, SK, and MCB conceived the idea for this Series paper. CMY wrote the first draft, and all other authors revised it for important intellectual content. All authors approved the final version of the manuscript as submitted for publication.
Declaration of interests
We declare no competing interests.
References
- 1.WHO . Global tuberculosis report 2014. World Health Organization; Geneva, Switzerland: 2014. [Google Scholar]
- 2.Ortblad KF, Lozano R, Murray CJL. An alternative estimation of tuberculosis incidence from 1980 to 2010: methods from the Global Burden of Disease 2010. Lancet. 2013;381:S104. [Google Scholar]
- 3.Taylor Z, Nolan CM, Blumberg HM, the American Thoracic Society. the Centers for Disease Control and Prevention. the Infectious Diseases Society of America Controlling tuberculosis in the United States. Recommendations from the American Thoracic Society, CDC, and the Infectious Diseases Society of America. MMWR Recomm Rep. 2005;54:1–81. [PubMed] [Google Scholar]
- 4.Public Health Agency of Canada. Canadian Lung Association. Canadian Thoracic Society Canadian tuberculosis standards, 7th edn. 2013. http://www.respiratoryguidelines.ca/sites/all/files/Canadian_TB_Standards_7th_Edition_ENG.pdf (accessed July 16, 2015).
- 5.Migliori GB, Zellweger JP, Abubakar I. European union standards for tuberculosis care. Eur Respir J. 2012;39:807–819. doi: 10.1183/09031936.00203811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Golub JE, Mohan CI, Comstock GW, Chaisson RE. Active case finding of tuberculosis: historical perspective and future prospects. Int J Tuberc Lung Dis. 2005;9:1183–1203. [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng VC, Chan JF, To KK, Yuen KY. Clinical management and infection control of SARS: lessons learned. Antiviral Res. 2013;100:407–419. doi: 10.1016/j.antiviral.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tom-Aba D, Olaleye A, Olayinka AT. Innovative Technological Approach to Ebola Virus Disease Outbreak Response in Nigeria Using the Open Data Kit and Form Hub Technology. PLoS One. 2015;10:e0131000. doi: 10.1371/journal.pone.0131000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toman K. Tuberculosis case-finding and chemotherapy questions and answers. World Health Organization; Geneva, Switzerland: 1979. [Google Scholar]
- 10.McMillan CW. Discovering tuberculosis: a global history 1900 to the present. Yale University Press; New Haven and London: 2015. [Google Scholar]
- 11.Keshavjee S, Farmer PE. Tuberculosis, drug resistance, and the history of modern medicine. N Engl J Med. 2012;367:931–936. doi: 10.1056/NEJMra1205429. [DOI] [PubMed] [Google Scholar]
- 12.Golub JE, Bur S, Cronin WA. Delayed tuberculosis diagnosis and tuberculosis transmission. Int J Tuberc Lung Dis. 2006;10:24–30. [PubMed] [Google Scholar]
- 13.Lin X, Chongsuvivatwong V, Lin L, Geater A, Lijuan R. Dose-response relationship between treatment delay of smear-positive tuberculosis patients and intra-household transmission: a cross-sectional study. Trans R Soc Trop Med Hyg. 2008;102:797–804. doi: 10.1016/j.trstmh.2008.04.027. [DOI] [PubMed] [Google Scholar]
- 14.Maher D, Chaulet P, Spinaci S, Harries A. Treatment of tuberculosis: guidelines for national programmes. 2nd edn. World Health Organization; Geneva, Switzerland: 1997. [Google Scholar]
- 15.Murray CJ, Styblo K, Rouillon A. Tuberculosis in developing countries: burden, intervention and cost. Bull Int Union Tuberc Lung Dis. 1990;65:6–24. [PubMed] [Google Scholar]
- 16.Lawn SD, Brooks SV, Kranzer K. Screening for HIV-associated tuberculosis and rifampicin resistance before antiretroviral therapy using the Xpert MTB/RIF assay: a prospective study. PLoS Med. 2011;8:e1001067. doi: 10.1371/journal.pmed.1001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balcha TT, Sturegärd E, Winqvist N. Intensified tuberculosis case-finding in HIV-positive adults managed at Ethiopian health centers: diagnostic yield of Xpert MTB/RIF compared with smear microscopy and liquid culture. PLoS One. 2014;9:e85478. doi: 10.1371/journal.pone.0085478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Behr MA, Warren SA, Salamon H. Transmission of Mycobacterium tuberculosis from patients smear-negative for acid-fast bacilli. Lancet. 1999;353:444–449. doi: 10.1016/s0140-6736(98)03406-0. [DOI] [PubMed] [Google Scholar]
- 19.Tostmann A, Kik SV, Kalisvaart NA. Tuberculosis transmission by patients with smear-negative pulmonary tuberculosis in a large cohort in the Netherlands. Clin Infect Dis. 2008;47:1135–1142. doi: 10.1086/591974. [DOI] [PubMed] [Google Scholar]
- 20.Creswell J, Sahu S, Blok L, Bakker MI, Stevens R, Ditiu L. A multi-site evaluation of innovative approaches to increase tuberculosis case notification: summary results. PLoS One. 2014;9:e94465. doi: 10.1371/journal.pone.0094465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO . Systematic screening for active tuberculosis: principles and recommendations. World Health Organization; Geneva: 2013. [PubMed] [Google Scholar]
- 22.Morrison J, Pai M, Hopewell PC. Tuberculosis and latent tuberculosis infection in close contacts of people with pulmonary tuberculosis in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2008;8:359–368. doi: 10.1016/S1473-3099(08)70071-9. [DOI] [PubMed] [Google Scholar]
- 23.Fox GJ, Barry SE, Britton WJ, Marks GB. Contact investigation for tuberculosis: a systematic review and meta-analysis. Eur Respir J. 2013;41:140–156. doi: 10.1183/09031936.00070812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blok L, Sahu S, Creswell J, Alba S, Stevens R, Bakker MI. Comparative meta-analysis of tuberculosis contact investigation interventions in eleven high burden countries. PLoS One. 2015;10:e0119822. doi: 10.1371/journal.pone.0119822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baily GV, Savic D, Gothi GD, Naidu VB, Nair SS. Potential yield of pulmonary tuberculosis cases by direct microscopy of sputum in a district of South India. Bull World Health Organ. 1967;37:875–892. [PMC free article] [PubMed] [Google Scholar]
- 26.Aluoch JA, Swai OB, Edwards EA. Study of case-finding for pulmonary tuberculosis in outpatients complaining of a chronic cough at a district hospital in Kenya. Am Rev Respir Dis. 1984;129:915–920. doi: 10.1164/arrd.1984.129.6.915. [DOI] [PubMed] [Google Scholar]
- 27.Aluoch JA, Swai OB, Edwards EA. Studies of case-finding for pulmonary tuberculosis in outpatients at 4 district hospitals in Kenya. Tubercle. 1985;66:237–249. doi: 10.1016/0041-3879(85)90061-3. [DOI] [PubMed] [Google Scholar]
- 28.Sánchez-Pérez HJ, Hernán MA, Hernández-Díaz S, Jansá JM, Halperin D, Ascherio A. Detection of pulmonary tuberculosis in Chiapas, Mexico. Ann Epidemiol. 2002;12:166–172. doi: 10.1016/s1047-2797(01)00308-8. [DOI] [PubMed] [Google Scholar]
- 29.Khan AJ, Khowaja S, Khan FS. Engaging the private sector to increase tuberculosis case detection: an impact evaluation study. Lancet Infect Dis. 2012;12:608–616. doi: 10.1016/S1473-3099(12)70116-0. [DOI] [PubMed] [Google Scholar]
- 30.Claassens MM, Jacobs E, Cyster E. Tuberculosis cases missed in primary health care facilities: should we redefine case finding? Int J Tuberc Lung Dis. 2013;17:608–614. doi: 10.5588/ijtld.12.0506. [DOI] [PubMed] [Google Scholar]
- 31.Kranzer K, Houben RM, Glynn JR, Bekker LG, Wood R, Lawn SD. Yield of HIV-associated tuberculosis during intensified case finding in resource-limited settings: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:93–102. doi: 10.1016/S1473-3099(09)70326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kamat SR, Dawson JJ, Devadatta S. A controlled study of the influence of segregation of tuberculous patients for one year on the attack rate of tuberculosis in a 5-year period in close family contacts in South India. Bull World Health Organ. 1966;34:517–532. [PMC free article] [PubMed] [Google Scholar]
- 33.Riley RL, Mills CC, O'Grady F, Sultan LU, Wittstadt F, Shivpuri DN. Infectiousness of air from a tuberculosis ward. Ultraviolet irradiation of infected air: comparative infectiousness of different patients. Am Rev Respir Dis. 1962;85:511–525. doi: 10.1164/arrd.1962.85.4.511. [DOI] [PubMed] [Google Scholar]
- 34.Escombe AR, Moore DA, Gilman RH. The infectiousness of tuberculosis patients coinfected with HIV. PLoS Med. 2008;5:e188. doi: 10.1371/journal.pmed.0050188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dharmadhikari AS, Mphahlele M, Venter K. Rapid impact of effective treatment on transmission of multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2014;18:1019–1025. doi: 10.5588/ijtld.13.0834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Riley RL, Mills CC, Nyka W. Aerial dissemination of pulmonary tuberculosis. A two-year study of contagion in a tuberculosis ward. 1959. Am J Epidemiol. 1995;142:3–14. doi: 10.1093/oxfordjournals.aje.a117542. [DOI] [PubMed] [Google Scholar]
- 37.Cavalcante SC, Durovni B, Barnes GL. Community-randomized trial of enhanced DOTS for tuberculosis control in Rio de Janeiro, Brazil. Int J Tuberc Lung Dis. 2010;14:203–209. [PMC free article] [PubMed] [Google Scholar]
- 38.Ayles H, Muyoyeta M, Du Toit E, the ZAMSTAR team Effect of household and community interventions on the burden of tuberculosis in southern Africa: the ZAMSTAR community-randomised trial. Lancet. 2013;382:1183–1194. doi: 10.1016/S0140-6736(13)61131-9. [DOI] [PubMed] [Google Scholar]
- 39.WHO . Recommendations for investigating contacts of persons with infectious tuberculosis in low- and middle-income countries. World Health Organization; Geneva, Switzerland: 2013. [PubMed] [Google Scholar]
- 40.Muñoz FM, Ong LT, Seavy D, Medina D, Correa A, Starke JR. Tuberculosis among adult visitors of children with suspected tuberculosis and employees at a children's hospital. Infect Control Hosp Epidemiol. 2002;23:568–572. doi: 10.1086/501972. [DOI] [PubMed] [Google Scholar]
- 41.Cruz AT, Medina D, Whaley EM, Ware KM, Koy TH, Starke JR. Tuberculosis among families of children with suspected tuberculosis and employees at a children's hospital. Infect Control Hosp Epidemiol. 2011;32:188–190. doi: 10.1086/657940. [DOI] [PubMed] [Google Scholar]
- 42.WHO Global health observatory data repository, adult HIV prevalence (15–49 years), 2013, by WHO region. 2014. http://www.who.int/gho/hiv/hiv_013.jpg?ua=1 (accessed July 16, 2015).
- 43.Shukshin A. Tough measures in Russian prisons slow spread of TB. Bull World Health Organ. 2006;84:265–266. [PMC free article] [PubMed] [Google Scholar]
- 44.Bamrah S, Yelk Woodruff RS, Powell K, Ghosh S, Kammerer JS, Haddad MB. Tuberculosis among the homeless, United States, 1994–2010. Int J Tuberc Lung Dis. 2013;17:1414–1419. doi: 10.5588/ijtld.13.0270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention Prevention and control of tuberculosis among homeless persons. Recommendations of the Advisory Council for the Elimination of Tuberculosis. MMWR Recomm Rep. 1992;41:13–23. [PubMed] [Google Scholar]
- 46.Theron G, Jenkins HE, Cobelens F. Data for action: collection and use of local data to end tuberculosis. Lancet. 2015 doi: 10.1016/S0140-6736(15)00321-9. published online Oct 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hadley M, Maher D. Community involvement in tuberculosis control: lessons from other health care programmes. Int J Tuberc Lung Dis. 2000;4:401–408. [PubMed] [Google Scholar]
- 48.Lutge EE, Wiysonge CS, Knight SE, Volmink J. Material incentives and enablers in the management of tuberculosis. Cochrane Database Syst Rev. 2012;1 doi: 10.1002/14651858.CD007952.pub2. CD007952. [DOI] [PubMed] [Google Scholar]
- 49.van't Hoog AH, Meme HK, Laserson KF. Screening strategies for tuberculosis prevalence surveys: the value of chest radiography and symptoms. PLoS One. 2012;7:e38691. doi: 10.1371/journal.pone.0038691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rangaka MX, Cavalcante SC, Marais BJ. Controlling the seedbeds of tuberculosis: diagnosis and treatment of tuberculosis infection. Lancet. 2015 doi: 10.1016/S0140-6736(15)00323-2. published online Oct 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barrera E, Livchits V, Nardell E. F-A-S-T: a refocused, intensified, administrative tuberculosis transmission control strategy. Int J Tuberc Lung Dis. 2015;19:381–384. doi: 10.5588/ijtld.14.0680. [DOI] [PubMed] [Google Scholar]
- 52.Dharmadhikari A, Smith J, Nardell E, Churchyard G, Keshavjee S. Aspiring to zero tuberculosis deaths among southern Africa's miners: is there a way forward? Int J Health Serv. 2013;43:651–664. doi: 10.2190/HS.43.4.d. [DOI] [PubMed] [Google Scholar]
- 53.Dharmadhikari AS, Mphahlele M, Stoltz A. Surgical face masks worn by patients with multidrug-resistant tuberculosis: impact on infectivity of air on a hospital ward. Am J Respir Crit Care Med. 2012;185:1104–1109. doi: 10.1164/rccm.201107-1190OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Escombe AR, Oeser CC, Gilman RH. Natural ventilation for the prevention of airborne contagion. PLoS Med. 2007;4:e68. doi: 10.1371/journal.pmed.0040068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.WHO . Guidance for national tuberculosis programmes on the management of tuberculosis in children. 2nd edn. World Health Organization; Geneva, Switzerland: 2014. [PubMed] [Google Scholar]
- 56.WHO . Improving the diagnosis and treatment of smear-negative pulmonary and extrapulmonary tuberculosis among adults and adolescents: Recommendations for HIV-prevalent and resource-constrained settings. World Health Organization; Geneva, Switzerland: 2007. [Google Scholar]
- 57.Getahun H, Kittikraisak W, Heilig CM. Development of a standardized screening rule for tuberculosis in people living with HIV in resource-constrained settings: individual participant data meta-analysis of observational studies. PLoS Med. 2011;8:e1000391. doi: 10.1371/journal.pmed.1000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pai M, Schito M. Tuberculosis diagnostics in 2015: landscape, priorities, needs, and prospects. J Infect Dis. 2015;211(suppl 2):S21–S28. doi: 10.1093/infdis/jiu803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lew W, Pai M, Oxlade O, Martin D, Menzies D. Initial drug resistance and tuberculosis treatment outcomes: systematic review and meta-analysis. Ann Intern Med. 2008;149:123–134. doi: 10.7326/0003-4819-149-2-200807150-00008. [DOI] [PubMed] [Google Scholar]
- 60.van der Werf MJ, Langendam MW, Huitric E, Manissero D. Multidrug resistance after inappropriate tuberculosis treatment: a meta-analysis. Eur Respir J. 2012;39:1511–1519. doi: 10.1183/09031936.00125711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mendoza-Ticona A, Alarcón E, Alarcón V. Effect of universal MODS access on pulmonary tuberculosis treatment outcomes in new patients in Peru. Public Health Action. 2012;2:162–167. doi: 10.5588/pha.12.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Theron G, Zijenah L, Chanda D, the TB-NEAT team Feasibility, accuracy, and clinical effect of point-of-care Xpert MTB/RIF testing for tuberculosis in primary-care settings in Africa: a multicentre, randomised, controlled trial. Lancet. 2014;383:424–435. doi: 10.1016/S0140-6736(13)62073-5. [DOI] [PubMed] [Google Scholar]
- 63.Shah NS, Yuen CM, Heo M, Tolman AW, Becerra MC. Yield of contact investigations in households of patients with drug-resistant tuberculosis: systematic review and meta-analysis. Clin Infect Dis. 2014;58:381–391. doi: 10.1093/cid/cit643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Harries AD, Rusen ID, Chiang CY, Hinderaker SG, Enarson DA. Registering initial defaulters and reporting on their treatment outcomes. Int J Tuberc Lung Dis. 2009;13:801–803. [PubMed] [Google Scholar]
- 65.Botha E, Den Boon S, Verver S. Initial default from tuberculosis treatment: how often does it happen and what are the reasons? Int J Tuberc Lung Dis. 2008;12:820–823. [PubMed] [Google Scholar]
- 66.Buu TN, Lönnroth K, Quy HT. Initial defaulting in the National Tuberculosis Programme in Ho Chi Minh City, Vietnam: a survey of extent, reasons and alternative actions taken following default. Int J Tuberc Lung Dis. 2003;7:735–741. [PubMed] [Google Scholar]
- 67.Naidoo P, du Toit E, Dunbar R. A comparison of multidrug-resistant tuberculosis treatment commencement times in MDRTBPlus line probe assay and Xpert® MTB/RIF-based algorithms in a routine operational setting in Cape Town. PLoS One. 2014;9:e103328. doi: 10.1371/journal.pone.0103328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gopi PG, Chandrasekaran V, Subramani R, Narayanan PR. Failure to initiate treatment for tuberculosis patients diagnosed in a community survey and at health facilities under a DOTS programme in a district of South India. Indian J Tuberc. 2005;52:153–156. [Google Scholar]
- 69.Amon JJ, Girard F, Keshavjee S. Limitations on human rights in the context of drug-resistant tuberculosis: a reply to Boggio et al. Health Hum Rights. 2009 http://www.hhrjournal.org/2009/10/07/limitations-on-human-rights-in-the-context-of-drug-resistant-tuberculosis-a-reply-to-boggio-et-al/ (accessed July 16, 2015). [Google Scholar]
- 70.Detjen A, Gnanashanmugam D, Talens A. A framework for integrating childhood tuberculosis into community-based child health care. CORE Group; Washington, DC: 2013. [Google Scholar]
- 71.Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Med. 2008;5:e152. doi: 10.1371/journal.pmed.0050152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stevenson CR, Forouhi NG, Roglic G. Diabetes and tuberculosis: the impact of the diabetes epidemic on tuberculosis incidence. BMC Public Health. 2007;7:234. doi: 10.1186/1471-2458-7-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Inghammar M, Ekbom A, Engström G. COPD and the risk of tuberculosis–a population-based cohort study. PLoS One. 2010;5:e10138. doi: 10.1371/journal.pone.0010138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ferrara G, Murray M, Winthrop K. Risk factors associated with pulmonary tuberculosis: smoking, diabetes and anti-TNFα drugs. Curr Opin Pulm Med. 2012;18:233–240. doi: 10.1097/MCP.0b013e328351f9d6. [DOI] [PubMed] [Google Scholar]
- 75.Khan MS, Salve S, Porter JD. Engaging for-profit providers in TB control: lessons learnt from initiatives in south Asia. Health Policy Plan. 2015 doi: 10.1093/heapol/czu137. published online Jan 20. [DOI] [PubMed] [Google Scholar]
- 76.Azman AS, Golub JE, Dowdy DW. How much is tuberculosis screening worth? Estimating the value of active case finding for tuberculosis in South Africa, China, and India. BMC Med. 2014;12:216. doi: 10.1186/s12916-014-0216-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dowdy DW, Lotia I, Azman AS, Creswell J, Sahu S, Khan AJ. Population-level impact of active tuberculosis case finding in an Asian megacity. PLoS One. 2013;8:e77517. doi: 10.1371/journal.pone.0077517. [DOI] [PMC free article] [PubMed] [Google Scholar]