Abstract
Background
Retention is the phase of orthodontic treatment that attempts to keep teeth in the corrected positions after treatment with orthodontic braces. Without a phase of retention, there is a tendency for teeth to return to their initial position (relapse). To prevent relapse, almost every person who has orthodontic treatment will require some type of retention.
Objectives
To evaluate the effects of different retention strategies used to stabilise tooth position after orthodontic braces.
Search methods
We searched the following databases: the Cochrane Oral Health Group's Trials Register (to 26 January 2016), the Cochrane Central Register of Controlled Trials (CENTRAL) (2015, Issue 12), MEDLINE via Ovid (1946 to 26 January 2016) and EMBASE via Ovid (1980 to 26 January 2016). We searched for ongoing trials in the US National Institutes of Health Trials Register (ClinicalTrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform. We applied no language or date restrictions in the searches of the electronic databases. We contacted authors of randomised controlled trials (RCTs) to help identify any unpublished trials.
Selection criteria
RCTs involving children and adults who had had retainers fitted or adjunctive procedures undertaken to prevent relapse following orthodontic treatment with braces.
Data collection and analysis
Two review authors independently screened eligible studies, assessed the risk of bias in the trials and extracted data. The outcomes of interest were: how well the teeth were stabilised, failure of retainers, adverse effects on oral health and participant satisfaction. We calculated mean differences (MD) with 95% confidence intervals (CI) for continuous data and risk ratios (RR) with 95% CI for dichotomous outcomes. We conducted meta‐analyses when studies with similar methodology reported the same outcome. We prioritised reporting of Little's Irregularity Index to measure relapse.
Main results
We included 15 studies (1722 participants) in the review. There are also four ongoing studies and four studies await classification. The 15 included studies evaluated four comparisons: removable retainers versus fixed retainers (three studies); different types of fixed retainers (four studies); different types of removable retainers (eight studies); and one study compared a combination of upper thermoplastic and lower bonded versus upper thermoplastic with lower adjunctive procedures versus positioner. Four studies had a low risk of bias, four studies had an unclear risk of bias and seven studies had a high risk of bias.
Removable versus fixed retainers
Thermoplastic removable retainers provided slightly poorer stability in the lower arch than multistrand fixed retainers: MD (Little's Irregularity Index, 0 mm is stable) 0.6 mm (95% CI 0.17 to 1.03). This was based on one trial with 84 participants that was at high risk of bias; it was low quality evidence. Results on retainer failure were inconsistent. There was evidence of less gingival bleeding with removable retainers: RR 0.53 (95% CI 0.31 to 0.88; one trial, 84 participants, high risk of bias, low quality evidence), but participants found fixed retainers more acceptable to wear, with a mean difference on a visual analogue scale (VAS; 0 to 100; 100 being very satisfied) of ‐12.84 (95% CI ‐7.09 to ‐18.60).
Fixed versus fixed retainers
The studies did not report stability, adverse effects or participant satisfaction. It was possible to pool the data on retention failure from three trials that compared polyethylene ribbon bonded retainer versus multistrand retainer in the lower arch with an RR of 1.10 (95% CI 0.77 to 1.57; moderate heterogeneity; three trials, 228 participants, low quality evidence). There was no evidence of a difference in failure rates. It was also possible to pool the data from two trials that compared the same types of upper fixed retainers, with a similar finding: RR 1.25 (95% CI 0.87 to 1.78; low heterogeneity; two trials, 174 participants, low quality evidence).
Removable versus removable retainers
One study at low risk of bias comparing upper and lower part‐time thermoplastic versus full‐time thermoplastic retainer showed no evidence of a difference in relapse (graded moderate quality evidence). Another study, comparing part‐time and full‐time wear of lower Hawley retainers, found no evidence of any difference in relapse (low quality evidence). Two studies at high risk of bias suggested that stability was better in the lower arch for thermoplastic retainers versus Hawley, and for thermoplastic full‐time versus Begg (full‐time) (both low quality evidence).
In one study, participants wearing Hawley retainers reported more embarrassment more often than participants wearing thermoplastic retainers: RR 2.42 (95% CI 1.30 to 4.49; one trial, 348 participants, high risk of bias, low quality evidence). They also found Hawley retainers harder to wear. There was conflicting evidence about survival rates of Hawley and thermoplastic retainers.
Other retainer comparisons
Another study with a low risk of bias looked at three different approaches to retention for people with crowding, but normal jaw relationships. The study found that there was no evidence of a difference in relapse between the combination of an upper thermoplastic and lower canine to canine bonded retainer and the combination of an upper thermoplastic retainer and lower interproximal stripping, without a lower retainer. Both these approaches are better than using a positioner as a retainer.
Authors' conclusions
We did not find any evidence that wearing thermoplastic retainers full‐time provides greater stability than wearing them part‐time, but this was assessed in only a small number of participants.
Overall, there is insufficient high quality evidence to make recommendations on retention procedures for stabilising tooth position after treatment with orthodontic braces. Further high quality RCTs are needed.
Plain language summary
What is the best method for maintaining the correct position of teeth after orthodontic treatment?
Review question
Which approach is most effective at maintaining teeth in their new position after the end of treatment with orthodontic braces?
Background
Once people finish having their teeth straightened with orthodontic braces, the teeth will tend to get crooked again. Orthodontists try to prevent this by using different retention procedures. Retention procedures can include either wearing retainers, which fit over or around teeth, or stick onto the back of teeth, or by using something called 'adjunctive procedures'. Adjunctive procedures either change the shape of the contacts between teeth, or involve a very small procedure to cut the connection between the gum and the neck of the tooth.
Study characteristics
We searched scientific databases to find all the new evidence up to 26 January 2016. This review updates a previous one published in 2006. We included 15 studies that compared different types of fixed and removable retainers and different durations of wear. There were 1722 participants including adults and children. Nine studies took place in a hospital or university setting, five studies in specialist practice and one in a National Health Service Clinic.
The studies evaluated four comparisons: removable retainers versus fixed retainers (three studies); different types of fixed retainers (four studies); different types of removable retainers (eight studies); and one study compared a combination of removable and fixed retainers, use of an adjunctive procedure and a positioner.
We also found four ongoing studies and four studies await classification.
Key results
Most of the evidence was of low quality. One small but well conducted study that compared full‐time and part‐time wear of thermoplastic retainers did not find evidence of a difference in stability (moderate quality evidence).
Quality of the evidence
There is not enough high quality evidence to recommend any one approach to retention over another. Further high‐quality studies are needed.
Summary of findings
Background
Description of the condition
Retention is the phase of orthodontic treatment that attempts to keep teeth in the corrected positions after correction with orthodontic (dental) braces. Without retention there is a tendency for the teeth to return to their initial position. This unfavourable change from the corrected position is known as relapse. The causes of relapse are not fully understood, but are felt to relate to recoil of the fibres that hold the teeth in the jaw bone; pressures from the lips, cheeks and tongue; further growth and the way the teeth meet together (Melrose 1998). To minimise relapse almost every person who has orthodontic treatment will require some type of retention.
Description of the intervention
Retention can be achieved by placing appliances, called retainers, on the teeth, or by undertaking additional or 'adjunctive' procedures to the teeth or the surrounding structures.
The retainers can either be removable, so that the person can take them out to clean, or they can be fixed to the teeth (Atack 2007). Bonded retainers are usually glued or 'bonded' on the back (inside) of the front teeth. These bonded retainers are sometimes referred to as 'fixed retainers'. Some clinicians use an appliance called a positioner after treatment is completed: this helps to 'fine‐tune' the result and can then be worn part‐time to help reduce relapse. Appendix 1 contains a glossary of terms to help describe some of the common type of retainers and adjunctive procedures that are described in this review.
There is no recognised duration for the time that retainers need to be worn. It has been shown that if people stop wearing retainers after one to two years there is a risk of long‐term relapse of the teeth (Little 1981; Little 1988). Therefore, some clinicians prefer to retain for longer periods, sometimes indefinitely. It is also not clear how many hours a day removable retainers need to be worn: some people are asked to wear their retainer full‐time (24 hours a day), while other people are only asked to wear them part‐time (less than 24 hours a day).
Clinicians may also try to reduce relapse by using 'adjunctive' procedures to the teeth (hard tissues) or the surrounding gum (soft tissues). This can involve reshaping of the contact points between teeth known as interproximal reduction (Aasen 2005), or cutting the fibres around the neck of the tooth, that hold the tooth in the jaw bone, known as pericision (Edwards 1988). The glossary of terms in Appendix 1 provides more information on this.
How the intervention might work
Retainers or adjunctive procedures aim to maintain the teeth in the position they were in at the end of orthodontic treatment. Retainers fit over or around the teeth, and prevent them moving away from their final position. Adjunctive procedures may work by improving the contacts between teeth (interproximal reduction) or by cutting fibres that connect the teeth to the gum around the neck of the teeth. These fibres may pull the teeth back towards their original position.
In order for retainers to work, they must keep the teeth in position without doing any harm and be comfortable and acceptable for people to wear. Potentially they could cause damage to the teeth by collecting plaque and calculus, and by making it difficult for people to keep their teeth clean. This build‐up of plaque may cause decay (caries) or inflammation and damage to the surrounding gum. This damage to the gum can cause gingivitis (inflammation of the gums) or periodontal disease (loss of attachment of the tooth to its surrounding gum and bony socket).
Why it is important to do this review
The Cochrane Oral Health Group undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were the most clinically important ones to maintain on The Cochrane Library (Worthington 2015). Consequently, the orthodontic expert panel identified this review as a priority title (Cochrane OHG priority review portfolio).
Retention is a key part of orthodontic treatment. Unless we can maintain the teeth in position after orthodontic treatment, the beneficial effects of the treatment can disappear. There are currently many different types of removable and fixed retainers and it is unclear which retainers are the best, and how long they should be used for. There is also little known about the possible benefits and risks of adjunctive procedures aimed at reducing relapse.
This review investigated the effectiveness of different retention strategies used to stabilise tooth position after treatment with orthodontic braces. It did not attempt to identify the causes of relapse. This review looked at the effects of retainers while in place, not the long‐term effects after they are no longer in use.
Objectives
To evaluate the effects of different retention strategies used to stabilise tooth position after orthodontic braces.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials.
Types of participants
Children and adults who have had retainers fitted or adjunctive procedures undertaken following treatment with orthodontic braces. There was no restriction for the presenting malocclusion or type of active orthodontic treatment undertaken. The participants had to be followed up at least three months after completing their orthodontic treatment.
We excluded:
people who had surgical correction of the jaws;
people with a cleft lip or palate, or both, or other craniofacial syndrome;
people who had orthodontic treatment based on extractions alone or the fitting of a passive space maintainer, or both.
Types of interventions
Retainers or adjunctive techniques, or both, after treatment with orthodontic braces. We included only studies where the full course of definitive orthodontic treatment was completed ‐ therefore, we excluded data on retention strategies at the end of an initial phase of removable or functional appliance treatment.
Types of outcome measures
Primary outcome
Stability.
This could be assessed by an index of tooth irregularity, for example, Little's Irregularity Index (Little 1981), which measures how crooked anterior teeth are or by crowding (see glossary of terms in Appendix 1). It can also be assessed by a change in the shape or size of each arch: this can be measured by intercanine width, intermolar width or arch length. The way the teeth meet together (occlusion) can also be assessed using measurements such as overjet, overbite and assessing the quality of the final results using an index such as the Peer Assessment Rating (PAR index) (Richmond 1992) (see glossary of terms in Appendix 1).
The assessment of stability had to be made at least three months after the fitting of the retainer or after the adjunctive procedure was carried out, or after both.
Secondary outcomes
Failure of the retainers.
This assessed how long retainers lasted without breaking (in months) or how many times they needed to be replaced or repaired during wear. If retainers were lost, we reported this as a failure, since the retainers could not fulfil their role. It is usually recorded how many retainers fail over the observation period.
Adverse effects on the oral health of the:
teeth (in terms of decay) ‐ assessed using indices of demineralisation or identifying the presence of caries;
surrounding structures (gums and other supporting structures) ‐ assessed using periodontal indices or other markers of periodontal disease.
Patient satisfaction.
This often takes the form of a questionnaire.
Search methods for identification of studies
We developed detailed search strategies for for each database searched for the identification of studies for this review. These were based on the search strategy developed for MEDLINE but revised appropriately for each database to take account of differences in controlled vocabulary and syntax rules. The MEDLINE search strategy combined the subject search with the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2009 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of The Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
The MEDLINE subject search used a combination of controlled vocabulary and free‐text terms and is published in Appendix 2.
Electronic searches
We searched the following databases:
Cochrane Oral Health Group's Trials Register (to 26 January 2016) (see Appendix 3);
Cochrane Central Register of Controlled Trials (CENTRAL) (2015, Issue 12) (see Appendix 4);
MEDLINE via Ovid (1946 to 26 January 2016) (see Appendix 2);
EMBASE via Ovid (1980 to 26 January 2016) (see Appendix 5).
There were no restrictions on language or date of publication in the searches of the electronic databases.
Searching other resources
Ongoing trials
We searched the following databases for ongoing trials (see Appendix 6 for details of the search):
US National Institutes of Health Trials Registry (clinicaltrials.gov) (to 26 January 2016);
The World Health Organization (WHO) Clinical Trials Registry Platform (apps.who.int/trialsearch/default.aspx) (to 26 January 2016).
Handsearching
We handsearched conference proceedings and abstracts from the British Orthodontic Conference, the European Orthodontic Conference and the International Association for Dental Research (IADR) from 2011 to 2015.
Checking reference lists
We checked the bibliographies of papers and review articles that we identified.
Personal communication
We contacted the first named authors of randomised trials identified where we required additional information. We requested further information relevant to the review that was not apparent in the published work. We also asked if they knew of any other published or unpublished studies relevant to the review that were not included in the list. In addition, the authors of this review act as referees for many orthodontic publications. If any study submitted for review appeared to fulfil the criteria, then we contacted the authors for further details.
Data collection and analysis
Selection of studies
Two review authors independently carried out the selection of papers, decision about eligibility, quality assessment, risk of bias, and data extraction. We resolved any disagreements by discussion with one of the other two review authors in the team. If additional information was required, we contacted the author directly and categorised the study as 'awaiting assessment'.
Data extraction and management
We extracted data and entered them on a customised data collection form. We recorded the following:
citation details of publication, if appropriate;
summary of the study design;
participants (sample size, age, inclusion and exclusion criteria, setting of study, costs involved to participants);
interventions:
type of retainer;
type of adjunctive procedure;
prescribed and actual duration of retention;
quality assessment of paper (see Assessment of risk of bias in included studies);
outcomes:
primary outcome ‐ assessment of stability;
secondary outcomes ‐ failure of retainers, adverse effects on health, patient satisfaction assessment;
Any additional information that may affect the assessment of the study.
Assessment of risk of bias in included studies
We used the Cochrane 'Risk of bias' tool to assess the risk of bias in the studies (see Section 8.5, Higgins 2011). We assessed the following domains:
random sequence generation;
allocation concealment;
blinding of outcome assessors;
incomplete outcome data reporting;
any selective outcome reporting;
any other sources of bias.
We assessed a study as low risk of bias overall if all the domains were low, unclear if at least one domain was unclear and high if at least one domain was high risk.
Measures of treatment effect
For studies considered eligible for this review, we used the following analyses in line with Cochrane guidance. For dichotomous outcomes, we expressed the estimate of effect of an intervention as risk ratios (RR) together with 95% confidence intervals (CIs). When analysing data for stability, we used the change in irregularity from end of active treatment to final position. If change data were not available, then we used the final irregularity score. For continuous outcomes, we used mean differences (MD) and standard deviations to summarise the data for each group using MD and 95% CIs.
Unit of analysis issues
These were parallel group studies and the statistical unit was the participant.
Dealing with missing data
We contacted trial authors to obtain missing data. We did not exclude a study from the review because of missing summary data; however, we would have discussed the potential implications of its absence from any meta‐analysis if applicable.
Assessment of heterogeneity
We assessed the significance of any discrepancies in the estimates of the treatment effects from the different trials by means of Cochrane's test for heterogeneity and considered heterogeneity significant if P value < 0.10. We used the I2 statistic, which describes the percentage total variation across studies that is due to heterogeneity rather than chance, to quantify heterogeneity with I2 over 50% being considered moderate to high heterogeneity.
Assessment of reporting biases
Only a proportion of research projects are ultimately published in an indexed journal and become easily identifiable for inclusion in a systematic review. We investigated and attempted to minimise potential reporting biases including publication bias, duplicate publication bias and language bias in this review.
If there had been sufficient numbers of trials (more than 10) in any meta‐analysis, we would have assessed publication bias according to the recommendations on testing for funnel plot asymmetry described in Higgins 2011. If we had identified asymmetry, we would have examined possible causes.
Data synthesis
If there were studies of similar comparisons reporting the same outcome measures, we combined them in a meta‐analysis. We combined RRs for dichotomous data, and would have used MDs for continuous data. We used the fixed‐effect model where there were two or three studies combined and would have used random‐effects models where there were more than three studies in the meta‐analysis.
Subgroup analysis and investigation of heterogeneity
We assessed clinical heterogeneity by examining the types of participants and interventions for all outcomes in each study. We did not formulate any hypotheses to be investigated for subgroup analyses.
Sensitivity analysis
We planned to undertake sensitivity analyses to examine the effect of the risk of bias on the overall estimates of effect, by removing studies that were unclear or high risk of bias from the analysis. In addition, we also planned to examine the effect of including unpublished literature on the review's findings. However, there were too few trials to undertake these analyses.
Presentation of main results
We produced a 'Summary of findings' table for each comparison using GRADEpro software. We assessed the quality of the body of evidence with reference to the overall risk of bias of the included studies, the directness of the evidence, the inconsistency of the results, the precision of the estimates, the risk of publication bias and the magnitude of the effect. We categorised the quality of the body of the evidence for each of the outcomes as high, moderate, low or very low and produced 'Summary of findings' tables for the main outcomes in this review. Where there were studies reporting different types of retainer under different comparison headings, we chose to report the findings of the study with the lowest risk of bias in the 'Summary of findings' table, and then included a narrative summary of the other studies in the comments box.
Results
Description of studies
Results of the search
See table of Characteristics of included studies and Characteristics of excluded studies.
The database search in January 2015 identified 441 articles and four additional articles were identified from additional sources (authors of this review). Of these, 11 were duplicates. Of the remaining 434, screening the titles and abstracts discarded 385. Of the remaining 49 articles, for which the full text was examined, we excluded 29. The remaining 20 articles reported on 15 studies. See Figure 1.
1.
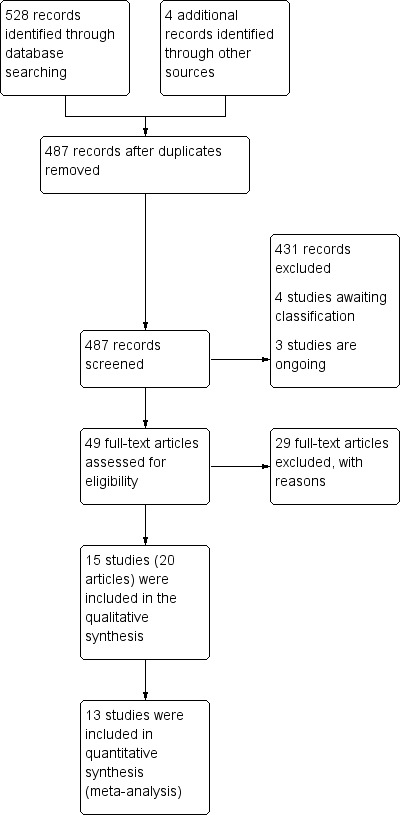
Study flow diagram
On 26 January 2016, we re‐ran the searches and identified seven potentially relevant trials from 53 records. Three of these are ongoing and are described in Characteristics of ongoing studies. Of the four completed and published studies, only one assessed our primary outcome 'stability' but the full text was not available and further information is being sought from the authors. The remaining three studies only assessed secondary outcomes; two of them require translation into English. See the Characteristics of studies awaiting classification section.
Included studies
Types of included studies
We included 15 studies (1722 participants) in this review (Årtun 1997; Aslan 2013; Bolla 2012; Edman Tynelius 2015; Gill 2007; Kumar 2011; Millett 2007; O'Rourke [pers comm]; Rohaya 2006; Rose 2002; Rowland 2007; Salehi 2013; Shawesh 2010; Sun 2011; Thickett 2010). All studies were parallel randomised controlled trials. Thirteen studies were two‐arm trials, one was a three‐arm trial (Edman Tynelius 2015), and one was a four‐arm trial (Årtun 1997).
Data from one study were collected from two articles, publishing different outcomes from the same study (Rowland 2007). Data from Millett 2007 were gathered from three published research abstracts and data from Edman Tynelius 2015 were collected from three articles reporting outcomes at different time intervals. Data and participants from a previous smaller trial were reported in the primary reference for Årtun 1997.
This version of the review did not include three studies that had been included in previous reviews (Edwards 1988; Sauget 1997; Taner 2000). This is because we decided to remove quasi‐randomised trials from the protocol, due to the high risk of bias.
Characteristics of the trial settings and investigators
Nine studies were undertaken in a hospital or university setting (Aslan 2013; Gill 2007; Kumar 2011; Millett 2007; O'Rourke [pers comm]; Rohaya 2006; Rose 2002; Sun 2011; Thickett 2010), five in a specialist practice (Årtun 1997; Bolla 2012; Rowland 2007; Salehi 2013; Shawesh 2010), and one in a National Health Service clinic (Edman Tynelius 2015).
There were six trials from the UK (Gill 2007; O'Rourke [pers comm]; Rohaya 2006; Rowland 2007; Shawesh 2010; Thickett 2010), one from the USA (Årtun 1997), one from Turkey (Aslan 2013), one from Italy (Bolla 2012), one from Sweden (Edman Tynelius 2015), one from India (Kumar 2011), one from the Republic of Ireland (Millett 2007), one from Germany (Rose 2002), one from Iran (Salehi 2013), and one from China (Sun 2011).
Orthodontists provided the care for all the participants in the trials. Four studies stated there was one operator (Bolla 2012; Edman Tynelius 2015; Millett 2007; Rowland 2007), one study stated they had two operators (Årtun 1997), and the remainder did not disclose the number of operators.
Three studies declared external funding sources (Edman Tynelius 2015; Gill 2007; Sun 2011).
Characteristics of the participants
The studies were undertaken on both children and adults. In eight studies, the mean age of participants was under 18 years (Aslan 2013; Edman Tynelius 2015; Gill 2007; O'Rourke [pers comm]; Rowland 2007; Shawesh 2010; Sun 2011; Thickett 2010), in three studies the mean age was over 18 years (Bolla 2012; Rose 2002; Salehi 2013), and four studies did not state the mean age (Årtun 1997; Kumar 2011; Millett 2007; Rohaya 2006).
There were between 20 (Rose 2002) and 397 (Rowland 2007) participants in the 15 studies.
In 10 studies, there were more females than males (Aslan 2013; Bolla 2012; Edman Tynelius 2015; Gill 2007; Millett 2007; O'Rourke [pers comm]; Rowland 2007; Salehi 2013; Shawesh 2010; Thickett 2010), one study had more males than females (Rose 2002), one study had equal numbers of males and females (Sun 2011), and three studies did not report this (Årtun 1997; Kumar 2011; Rohaya 2006).
Characteristics of the interventions
Eight studies compared different types of removable retainers (Aslan 2013; Gill 2007; Kumar 2011; Rohaya 2006; Rowland 2007; Shawesh 2010; Sun 2011; Thickett 2010).
Four studies compared different types of fixed retainers (Årtun 1997; Bolla 2012; Rose 2002; Salehi 2013).
Three studies compared removable retainers with fixed retainers (Årtun 1997; Millett 2007; O'Rourke [pers comm]).
One study compared a combination of removable and fixed retainers, use of an adjunctive procedure and a positioner (Edman Tynelius 2015).
Of the studies comparing removable retainers, the following comparisons were made:
modified thermoplastic retainer versus full coverage thermoplastic retainer (Aslan 2013);
part‐time versus full‐time wear of thermoplastic retainers (Gill 2007; Thickett 2010);
Begg retainers versus thermoplastic retainers, with bonded retainer in lower arch in both groups (Kumar 2011);
Hawley retainers versus thermoplastic retainers (Rohaya 2006; Rowland 2007; Sun 2011);
part‐time versus full‐time wear of Hawley retainers (Shawesh 2010).
Of the studies comparing fixed retainers, the following comparisons were made:
polyethylene ribbon retainer versus multistrand stainless steel;
thick plane stainless steel versus thick spiral stainless steel versus thin flexible stainless steel (Årtun 1997).
Of the studies comparing removable retainers and fixed retainers, the following comparisons were made:
lower multistrand stainless steel versus lower thermoplastic (Millett 2007; O'Rourke [pers comm]);
thick plane stainless steel, thick spiral stainless steel and thin flexible stainless steel versus removable retainer (Årtun 1997).
Characteristics of the outcomes
With the data available, it was possible to analyse the following outcomes:
assessment of stability (Aslan 2013; Gill 2007; Kumar 2011; Millett 2007; O'Rourke [pers comm]; Rohaya 2006; Rowland 2007; Salehi 2013; Shawesh 2010; Thickett 2010);
survival of retainers (Årtun 1997; Bolla 2012; Millett 2007; Rose 2002; Sun 2011);
participant satisfaction (Millett 2007; Rowland 2007);
adverse effects on oral health (Millett 2007).
Assessment of stability was assessed using different measurements:
Little's Irregularity Index (Edman Tynelius 2015; Gill 2007; Millett 2007; O'Rourke [pers comm]; Rowland 2007; Shawesh 2010; Thickett 2010);
Crowding (Shawesh 2010);
Intercanine and intermolar width (Edman Tynelius 2015; Gill 2007; O'Rourke [pers comm]; Rowland 2007; Thickett 2010);
Arch length (Edman Tynelius 2015; O'Rourke [pers comm]; Thickett 2010);
Overjet and overbite (Edman Tynelius 2015; Gill 2007; Thickett 2010);
PAR (Kumar 2011; Thickett 2010);
Settling of the occlusion (Aslan 2013).
This review gave priority to reporting the Little's Irregularity Index (in the 'Summary of findings' tables and conclusions). There is no agreed Core Outcome Measures in Effectiveness Trials (COMET) for stability trials in orthodontics at the present time, so the review authors decided to use Little's Irregularity Index for the preferred outcome measure in this review.
Assessment of survival of retainers were assessed by measuring the number of retainers that failed:
bonded retainer partially or completely detached from the teeth (Årtun 1997; Bolla 2012; Millett 2007; Rose 2002; Salehi 2013; Sun 2011);
bonded retainer fractured (Årtun 1997; Bolla 2012; Millett 2007; Rose 2002; Salehi 2013; Sun 2011);
removable retainer was lost (Årtun 1997; Millett 2007; Sun 2011);
removable retainer no longer fitted (Sun 2011);
removable retainer showed excessive wear (Sun 2011).
Assessment of patient satisfaction was assessed using questionnaires. The following questions were asked:
Was retainer acceptable to wear? Was retainer easy to keep clean? Were you happy with the appearance? (Millett 2007);
Able to wear retainer as instructed? Able to wear retainer away from home? Embarrassed to wear retainer? Discomfort wearing retainer? How did it compare to wearing fixed appliances? (Rowland 2007).
Outcomes were reported at the following intervals:
three months (Kumar 2011);
six months (Aslan 2013; Gill 2007; Kumar 2011; Rowland 2007);
nine months (Aslan 2013);
one year (Edman Tynelius 2015; Millett 2007; Rohaya 2006; Shawesh 2010; Sun 2011; Thickett 2010);
18 months (O'Rourke [pers comm]; Salehi 2013);
two years (Edman Tynelius 2015; Rose 2002);
three years (Årtun 1997);
five years (Edman Tynelius 2015);
six years (Bolla 2012).
Some of the results were provided without standard deviations, or with data that were not amenable to meta‐analysis.
Excluded studies
Of the 29 excluded studies:
16 were not RCTs (Al‐Nimri 2009; Arora 2014; Atack 2007; Axelsson 1993; Barlin 2011; Basciftici 2007; Bauer 2010; Bock 2008; Edwards 1988; Jäderberg 2012; Lindauer 1998; Pandis 2007; Sauget 1997; Tacken 2010; Taner 2000; Vecere 1983);
four investigated methods of placing or supervising retainers rather than comparing different retainers (Bazargani 2012; Conway 2011; ISRCTN56295329; Pandis 2013);
three recruited insufficient participants to complete study (ACTRN12612000670875; ISRCTN22535947; ISRCTN26364810);
three had less than three months' follow‐up (Ahrens 1981; Carvalho 2006; Horton 2009);
three had insufficient data to analyse (Haydar 1992; Larsson 1983; Stormann 2002).
Risk of bias in included studies
See table of Characteristics of included studies and Figure 2 and Figure 3.
2.
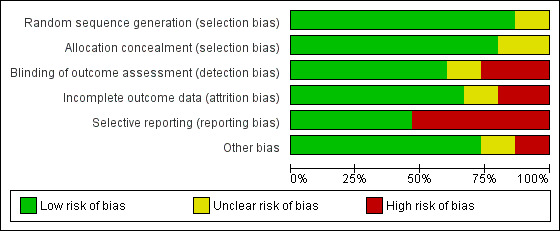
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.
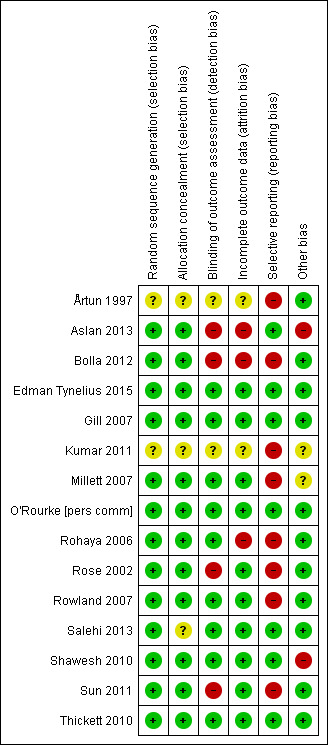
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Sequence generation
Twelve studies had adequate sequence generation (Bolla 2012; Edman Tynelius 2015; Gill 2007; Millett 2007; O'Rourke [pers comm]; Rohaya 2006; Rose 2002; Rowland 2007; Salehi 2013; Shawesh 2010; Sun 2011; Thickett 2010). One study used an approach with a high risk of bias sequence (Aslan 2013). For two studies, it is unclear how the sequence generation was performed (Årtun 1997; Kumar 2011).
Allocation concealment
Allocation concealment was adequate for 11 studies (Bolla 2012; Edman Tynelius 2015; Gill 2007; Millett 2007; O'Rourke [pers comm]; Rohaya 2006; Rose 2002; Rowland 2007; Shawesh 2010; Sun 2011; Thickett 2010). There was a high risk of bias in one study (Aslan 2013), and it was unclear in three studies (Årtun 1997; Kumar 2011; Salehi 2013).
Blinding
Blinding of participants and clinicians is usually not possible in retention research, due to the nature of the intervention. This is because it is not possible to hide either the retainer type or adjunctive procedure. Therefore, the blinding of participants and clinicians was not included in the 'Risk of bias' tables for each study. The lack of ability to blind the participants and clinicians could potentially bias this type of research and should be noted when interpreting the findings.
However, blinding of the assessors is often possible, particularly when assessing stability on study models (except where bonded retainers are still in place). Blinding of the assessors is also possible when assessing the results of participant satisfaction questionnaires. Nine studies used blinding of outcome assessors where possible (Edman Tynelius 2015; Gill 2007; Millett 2007; O'Rourke [pers comm]; Rohaya 2006; Rowland 2007; Salehi 2013; Shawesh 2010; Thickett 2010). For three studies, it was not possible to provide blinding (Bolla 2012; Rose 2002; Sun 2011), and in one study, the outcome assessor was not blinded (Aslan 2013). In two of the studies, it was unclear if blinding of assessors was used (Årtun 1997; Kumar 2011).
Incomplete outcome data
Ten studies reported and explained drop‐outs and withdrawals (Edman Tynelius 2015; Gill 2007; Millett 2007; O'Rourke [pers comm]; Rose 2002; Rowland 2007; Salehi 2013; Shawesh 2010; Sun 2011; Thickett 2010). In three studies, the drop‐outs were not fully reported on (Aslan 2013; Bolla 2012; Rohaya 2006), and in two studies, it was unclear (Årtun 1997; Kumar 2011).
Selective reporting
Seven studies showed no evidence of selective reporting (Aslan 2013; Edman Tynelius 2015; Gill 2007; O'Rourke [pers comm]; Salehi 2013; Shawesh 2010; Thickett 2010). Five studies had a high risk of bias due to reporting bias. The Rowland 2007 study measured, but did not report, overjet and overbite changes, and also selectively reported the participant satisfaction data. One study mentioned use of the PAR index as a measure of stability in the methodology, but the outcome was not reported (Millett 2007), and one study described some aspects of participant satisfaction, without giving data to support this (Rose 2002). In another study, there were missing stability and adverse effects data (Årtun 1997). The author of one study reported that there were more outcomes to be reported (Rohaya 2006). In one study, the lower irregularity was reported, but not the upper (Kumar 2011). We contacted the author of one trial and they confirmed they started collecting data for periodontal health, but abandoned this part way through the study due to time constraints (Bolla 2012). For one study, there were outcomes mentioned on a clinical trial register that have not yet been reported (Sun 2011).
Other potential sources of bias
Eleven studies appeared to be free of other bias (Årtun 1997; Aslan 2013; Bolla 2012; Edman Tynelius 2015; Gill 2007; O'Rourke [pers comm]; Rohaya 2006; Rose 2002; Rowland 2007; Salehi 2013; Thickett 2010).
Two studies showed a high risk of other bias. In one study, the authors tried to qualify the quality of their occlusal result by comparing it to a so‐called "ideal" group, but this group may not have been ideal (Aslan 2013). One study identified that despite adequate randomisation, there was not pre‐treatment equivalence between the two intervention groups (Shawesh 2010). As a result, the authors warned that the results should be interpreted with caution.
For two studies, it was not possible to make a decision as to whether there was other risk of bias due to inadequate information in the articles (Kumar 2011; Millett 2007).
Overall risk of bias
Four studies showed overall low risk of bias (Edman Tynelius 2015; Gill 2007; O'Rourke [pers comm]; Thickett 2010).
Ten studies had a high risk of bias (Årtun 1997; Aslan 2013; Bolla 2012; Kumar 2011; Millett 2007; Rohaya 2006; Rose 2002; Rowland 2007; Shawesh 2010; Sun 2011).
One study was at unclear risk of bias (Salehi 2013).
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings for the main comparison. Removable retainer versus fixed retainer to stabilise tooth position.
| Removable retainer versus fixed retainer to stabilise tooth position | ||||||
| Patient or population: people who had received fixed appliance treatment Setting: specialist orthodontic practice and hospital orthodontic department Intervention: removable retainers Comparison: fixed retainers | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with fixed retainers | Risk with removable retainers | |||||
|
Stability ‐ Little's Irregularity Index in lower arch Ideally 0 mm 12 months |
Mean = 0.43 mm | 0.6 mm more (0.17 more to 1.03 more) | ‐ | 841 (1 RCT) | ⊕⊕⊝⊝ low2 | 1 study with low risk of bias suggested that there is a statistically significant reduction in relapse with the fixed retainer, but this is unlikely to be clinically significant |
| Failure of retainers (lower) | See comment | ‐ | 133 (2 RCTs) | ⊕⊝⊝⊝ very low3 | 2 studies at high risk of bias making multiple comparisons of different types of fixed and removable retainers showed inconsistent results | |
|
Adverse effects on health Evidence of gingival bleeding 12 months |
6174 per 1000 | 327 per 1000 (191 to 543) | RR 0.53 (0.31 to 0.88) | 841 (1 RCT) | ⊕⊕⊝⊝ low2 | 1 study also looked at adverse effects on dental health: caries and periodontal pocketing. There was low quality evidence to suggest that there was additional periodontal pocketing with the fixed retainer |
|
Patient satisfaction How acceptable was the retainer to wear? 0 to 100 VAS (100 is very satisfied) 12 months |
Mean = 91.62 | 12.84 lower (18.6 lower to 7.09 lower) | ‐ | 81 (1 RCT) | ⊕⊕⊝⊝ low2 | 1 RCT found that the participants thought the fixed retainer was easier to keep clean but found no difference in the appearance of their teeth after 1 year of retention |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio; VAS: visual analogue scale | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 Removable thermoplastic versus fixed multistrand 2 Downgraded twice: once for high risk of bias and once for imprecision (only one study) 3 Downgraded three times: once for high risk of bias, once for imprecision and once for inconsistency 4 From control group (fixed) of study
Summary of findings 2. Fixed retainer versus fixed retainer to stabilise tooth position.
| Fixed retainer versus fixed retainer to stabilise tooth position | ||||||
| Patient or population: people who have received fixed appliance treatment Setting: specialist practice or university orthodontic clinic Intervention: one type of fixed retainer Comparison: another type of fixed retainer | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with fixed retainers | Risk with fixed retainers | |||||
| Stability ‐ Little's Irregularity Index | ‐ | ‐ | ‐ | 0 (0) | ‐ | Not reported |
|
Failure of retainers (lower arch) 18 months to 6 years |
3361 per 1000 | 370 per 1000 (259 to 528) | RR 1.10 (0.77 to 1.57) | 228 (3 RCTs)2 | ⊕⊕⊝⊝ low3 | 2 of these RCTs also compared failure rates in the upper arch and found no statistical difference in failure rate (RR 1.25, 95% CI 0.87 to 1.78). 1 study with a high risk of bias showed no evidence of a difference in failure rates between 3 types of metal fixed retainers |
| Adverse effects on health | ‐ | ‐ | ‐ | 0 (0) | ‐ | Not reported |
| Patient satisfaction | ‐ | ‐ | ‐ | 0 (0) | ‐ | Not reported |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 From control group 2 Mandibular polyethylene ribbon bonded retainer versus mandibular multistrand retainer 3 Downgraded twice: once for high risk of bias and once for imprecision
Summary of findings 3. Removable retainer versus removable retainer to stabilise tooth position.
| Removable retainer versus removable retainer to stabilise tooth position | ||||||
| Patient or population: people who have received fixed appliance treatment Setting: specialist practice, university or hospital orthodontic department Intervention: one type of removable retainer or wear time Comparison: another type of removable retainer or wear time | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with Removable Retainers | Risk with Removable | |||||
|
Stability ‐ Little's Irregularity Index in upper arch Ideally 0 mm 12 months |
‐ | ‐ | ‐ | 419 (3 RCT) | ⊕⊕⊝⊝ low to ⊕⊕⊕⊝ moderate |
Data used from 3 studies comparing different removable retainers used for different time periods 1 study at low risk of bias comparing part‐time thermoplastic vs. full‐time thermoplastic retainer showed no evidence to suggest a difference (graded moderate quality evidence: downgraded once due to imprecision). There was also data from additional study with a low risk of bias that could not be analysed using Review Manager 5 that suggested no evidence of difference in relapse when thermoplastic retainers were worn full‐time or part‐time 1 study comparing part‐time and full‐time Hawley retainers showed no evidence of a difference (graded low quality of evidence: downgraded twice due to high risk of bias and imprecision) 1 study at high risk of bias comparing upper Hawley retainers and upper thermoplastic retainers suggested there was statistical, but not clinically significant, reductions in relapse with thermoplastic retainers (graded low quality: downgraded twice due to high risk of bias and imprecision) |
|
Stability ‐ Little's Irregularity Index in lower arch Ideally 0 mm 6‐12 months |
‐ | ‐ | ‐ | 643 (4 RCT) | ⊕⊕⊝⊝ low to ⊕⊕⊕⊝ moderate |
Data used from 4 studies comparing different removable retainers used for different time periods. 1 study at low risk of bias comparing part‐time thermoplastic vs. full‐time thermoplastic retainer showed no evidence to suggest a difference (graded moderate quality evidence, downgraded once due to imprecision) 2 studies at high risk of bias suggested that stability was better for thermoplastic retainers vs. Hawley retainers, and for thermoplastic full‐time retainers vs. Begg (full‐time) retainers (both low quality evidence; downgraded twice due to high risk of bias and imprecision) 1 study with a high risk of bias comparing part‐time and full‐time wear of lower Hawley retainers found no evidence of any difference in relapse (low quality evidence: downgraded twice due to high risk of bias and imprecision). Data from an additional study with a low risk of bias that could not be analysed using Review Manager to support this evidence |
|
Failure of retainers How many broke in total? 12 months |
‐ | ‐ | ‐ | 457 (2 RCTs) | ⊕⊕⊝⊝ low | 2 studies provided data 1 study comparing Hawley retainers vs. part‐time thermoplastic retainers showed no difference in the number of retainers that were lost (low quality evidence, downgraded twice due to high risk of bias) 1 study with a high risk of bias comparing full‐time wear of Hawley retainers vs. full‐time thermoplastic retainers found greater failure rates in the lower thermoplastic retainers (low quality evidence, downgraded twice due to high risk of bias, and imprecision) |
| Adverse effects on health | ‐ | ‐ | ‐ | 0 (0) | ‐ | Not reported |
|
Patient satisfactionEmbarrassed to wear retainer? 12 months |
721 per 1000 | 174 per 1000 (93 to 322) | RR 2.42 (1.30 to 4.49) | 348 (1 RCT)2 | ⊕⊕⊝⊝ low | 1 study comparing Hawley and thermoplastic retainers found participants who wore the Hawley retainers found them harder to wear as instructed, and judged them more negatively when comparing them to the fixed appliances they had worn. There was no evidence of a difference between the Hawley and thermoplastic retainer groups in terms of discomfort or ability to wear them away from home (low quality evidence, downgraded twice as one study with high risk of bias and imprecision) |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 From study control group 2 Hawley versus thermoplastic retainers
Comparison 1: removable retainers versus fixed retainers
There were three trials that investigated removable retainers versus fixed retainers (Årtun 1997; Millett 2007; O'Rourke [pers comm]). In all three studies, the comparison was in the lower arch only.
The Årtun 1997 study compared a removable acrylic and wire retainer with types of fixed retainers.
The Millett 2007 study compared a lower thermoplastic (vacuum‐formed) retainer with a multistrand stainless steel wire bonded to the canines and incisors.
The O'Rourke [pers comm] study compared a lower thermoplastic (vacuum‐formed) retainer with a multistrand stainless steel wire bonded to the canines and incisors. The data from this study were non‐parametric and, therefore, reported in medians, so could not be entered into Review Manager 5 (RevMan 2014). Table 4 shows the data and analysis from the original study.
1. O'Rourke study results: changes in stability measurements at 6, 12 and 18 months.
| Measure | Stability assessments at 6, 12 and 18 months |
Bonded retainer 42 participants (interquartiles) |
Vacuum‐formed retainer 40 participants (interquartiles) |
Mann Whitney P value |
| Little's Irregularity Index | Change between T0 and T1 Change between T1 and T2 Change between T2 and T3 |
0.03 (0.00‐0.82) 0.04 (0.02‐0.18) 0.05 (0.02‐0.20) |
0.08 (0.01‐0.40) 0.10 (0.06‐0.32) 0.07 (0.00‐0.64) |
0.003 (P value < 0.05) 0.03 (P value < 0.05) 0.04 (P value < 0.05) |
| Intercanine width | Change between T0 and T1 Change between T1 and T2 Change between T2 and T3 |
0.11 (0.05‐0.39) 0.22 (0.11‐0.60) 0.29 (0.12‐0.57) |
0.25 (0.10‐0.50) 0.25 (0.09‐0.58) 0.28 ( 0.12‐0.57) |
0.56 0.43 0.32 |
| Intermolar width | Change between T0 and T1 Change between T1 and T2 Change between T2 and T3 |
0.29 (0.11‐0.67) 0.47 (0.15‐1.04) 0.38 (0.12‐0.98) |
0.18 (0.66‐0.52) 0.38 (0.14‐0.90) 0.50 (0.22‐1.05) |
0.92 0.36 0.24 |
| Arch length | Change between T0 and T1 Change between T1 and T2 Change between T2 and T3 |
0.24 (0.08‐0.55) 0.39 (0.13‐0.68) 0.49 (0.09‐0.95) |
0.31 (0.07‐1.18) 0.26 (0.17‐2.01) 0.22 (0.12‐1.79) |
0.17 0.20 0.44 |
| Extraction site space | Change between T0 and T1 Change between T1 and T2 Change between T2 and T3 |
0.00 (0.00‐0.01) 0.00 (0.00‐0.17) 0.03 (0.00‐0.10) |
0.00 (0.00‐0.03) 0.00 (0.00‐0.11) 0.14 (0.00‐0.17) |
0.37 0.47 0.01 (P value < 0.05) |
Stability
Two trials reported stability using Little's Irregularity Index, both comparing lower removable thermoplastic retainers with lower bonded retainers (Millett 2007; O'Rourke [pers comm]).
Lower removable thermoplastic versus lower bonded retainer
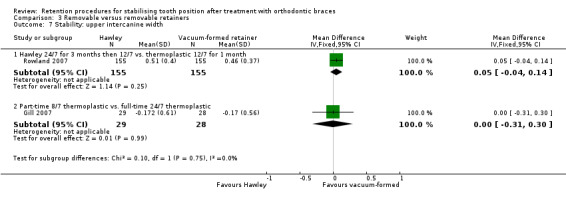
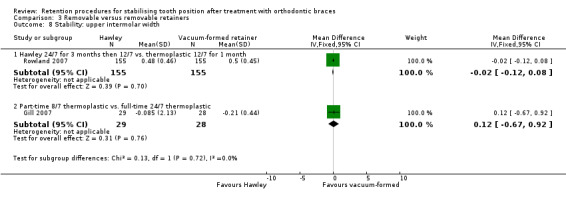
Millett 2007 found a statistically significant difference of 0.6 mm more relapse with a lower removable thermoplastic retainer compared with a lower bonded multistrand retainer (95% CI 0.17 to 1.03; P value = 0.0061). While this was statistically significant, a difference of 0.6 mm would only be clinically significant if restricted to the area of one tooth contact point (Analysis 1.1).
1.1. Analysis.
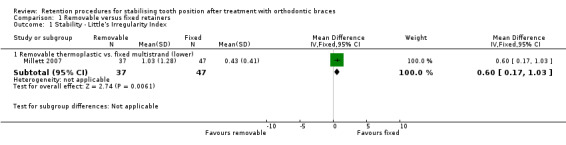
Comparison 1 Removable versus fixed retainers, Outcome 1 Stability ‐ Little's Irregularity Index.
O'Rourke [pers comm] found a statistically significant difference of 0.05 mm more relapse with a lower removable thermoplastic retainer compared with a lower bonded multistrand retainer after six months (P value = 0.003). There was a similar small, but statistically significant, increase in relapse in the removable retainer group at 12 and 18 months. Once again, while these differences were statistically significant, they were not clinically significant. There was no difference reported in intercanine width, intermolar width, arch length and extraction site space opening.
It was not possible to pool the results as the O'Rourke [pers comm] data could not be put into Review Manager 5 (RevMan 2014); they are presented in Table 4.
Failure of retainers
Two studies reported failure of retainers (Årtun 1997; Millett 2007). One study compared three types of bonded retainers and a removable retainer (Årtun 1997), while the other study compared lower thermoplastic retainer with lower bonded retainer.
Comparing three types of lower bonded retainers and removable retainer
In the Årtun 1997 study, there was no difference between the three types of fixed retainers and the removable retainer used (Analysis 1.2).
1.2. Analysis.
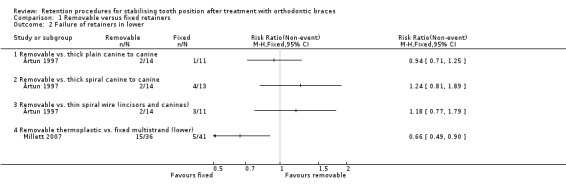
Comparison 1 Removable versus fixed retainers, Outcome 2 Failure of retainers in lower.
Lower removable thermoplastic versus lower bonded retainer
In Millett 2007, there was a statistically significant difference of more failures in the removable retainer group than the bonded retainer group (RR 0.66, 95% CI 0.49 to 0.90; P value = 0.007). This was due to 10 retainers being fractured and five being lost in the removable retainer group, compared with two with some composite loss and five completely debonding in the fixed retainer group. This increase of eight more removable retainer failures was clinically significant (Analysis 1.2).
We did not pool the results due to comparison of markedly different types of retainers. This may explain the different findings between the two studies.
Adverse effects on health
One study investigated adverse effects on health, when comparing lower thermoplastic retainers with lower bonded retainers (Millett 2007).
Lower removable thermoplastic versus lower bonded retainer
The Millett 2007 study reported adverse effects on dental health in terms of evidence of caries, gingival bleeding and periodontal pocketing. There was no evidence of caries in either group (Analysis 1.3). However, there was significantly more gingival bleeding in the bonded retainer group than the removable retainer group (RR 0.53, 95% CI 0.31 to 0.88; P value = 0.0015), which is clinically significant (Analysis 1.4). There was more periodontal pocketing in the bonded retainer group (RR 0.32, 95% CI 0.12 to 0.87; P value = 0.026). However, this periodontal pocketing result should be viewed with caution as the two groups were not equal at debond, with four times as many participants with pocketing in the bonded retainer group (Analysis 1.5).
1.3. Analysis.
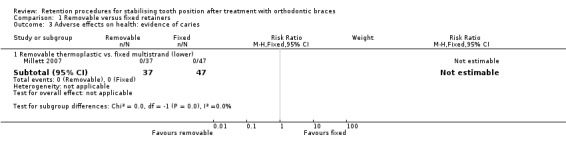
Comparison 1 Removable versus fixed retainers, Outcome 3 Adverse effects on health: evidence of caries.
1.4. Analysis.
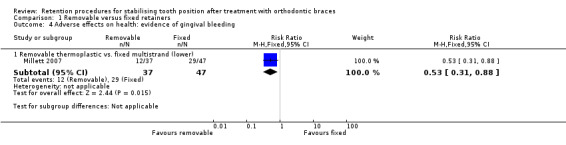
Comparison 1 Removable versus fixed retainers, Outcome 4 Adverse effects on health: evidence of gingival bleeding.
1.5. Analysis.
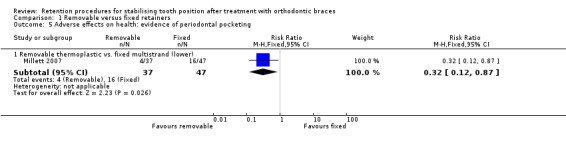
Comparison 1 Removable versus fixed retainers, Outcome 5 Adverse effects on health: evidence of periodontal pocketing.
Patient satisfaction
One study investigated patient satisfaction when comparing lower thermoplastic retainers with lower bonded retainers.
Lower removable thermoplastic versus lower bonded retainer
The Millett 2007 study assessed patient satisfaction using the response to three questions.
There was a statistically significant difference in two questions related to patient satisfaction, with the participants finding the fixed retainer more acceptable to wear (MD ‐12.84, 95% CI ‐18.10 to ‐7.09; P value = 0.000012) (Analysis 1.6) and they also perceived it easier to clean (MD ‐10.31, 95% CI ‐20.05 to ‐0.58; P value = 0.038), although the results for ease of cleaning were unlikely to be clinically significant (Analysis 1.7). The participants were equally happy with the appearance of their teeth with both retainers after one year of retention (Analysis 1.8).
1.6. Analysis.
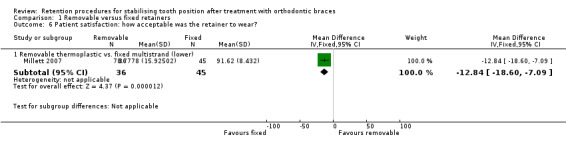
Comparison 1 Removable versus fixed retainers, Outcome 6 Patient satisfaction: how acceptable was the retainer to wear?.
1.7. Analysis.
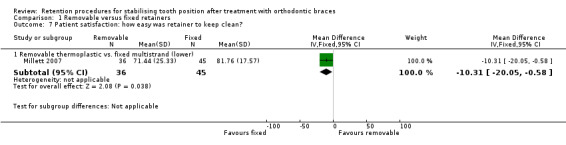
Comparison 1 Removable versus fixed retainers, Outcome 7 Patient satisfaction: how easy was retainer to keep clean?.
1.8. Analysis.
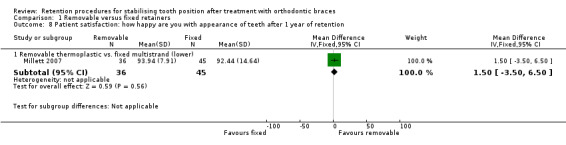
Comparison 1 Removable versus fixed retainers, Outcome 8 Patient satisfaction: how happy are you with appearance of teeth after 1 year of retention.
Comparison 2: fixed retainers versus fixed retainers
Four trials compared different types of fixed retainers (Årtun 1997; Bolla 2012; Rose 2002; Salehi 2013).
The Årtun 1997 study compared three types of fixed retainers: thick (0.032" (0.08 cm)) plain stainless steel wire bonded only to the canines, thick (0.032") spiral stainless steel wire bonded only to the canines and a thin (0.0205") spiral wire bonded to the canines and incisors.
Three other studies compared polyethylene ribbon bonded retainers with multistrand bonded retainers (Bolla 2012; Rose 2002; Salehi 2013). Two of these studies compared upper and lower retainers (Bolla 2012; Salehi 2013), and one study compared lower retainers only (Rose 2002).
Stability
Stability was not reported.
Failure of retainers
Four studies comparing bonded retainers reported failure of retainers. One studies comparing three types of bonded metal bonded retainers, and three studies comparing polyethylene ribbon bonded retainers with multistrand retainers (Analysis 2.1).
2.1. Analysis.
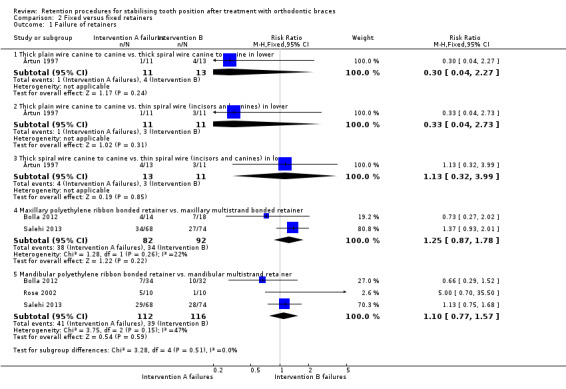
Comparison 2 Fixed versus fixed retainers, Outcome 1 Failure of retainers.
Three types of metal bonded retainers
There was no difference between the failure rates of the three types of bonded retainers in the Årtun 1997 study (Analysis 2.1).
Polyethylene ribbon bonded versus multistrand bonded retainers
Two studies compared failure rates of polyethylene ribbon bonded retainers with multistrand bonded retainers in the maxilla (Bolla 2012; Salehi 2013), and it was possible to undertake a meta‐analysis of these data. The pooled estimate showed an RR of 1.25 (95% CI 0.87 to 1.78; P value = 0.22) indicating no difference in the failure rates. There was low heterogeneity between the studies (P value = 0.26; I2 = 22), with very similar methodology and materials used in both trials (Analysis 2.1).
Three studies compared failure rates of polyethylene ribbon bonded retainers with multistrand bonded retainers in the mandible (Bolla 2012; Rose 2002; Salehi 2013), and it was possible to undertake a meta‐analysis of these data. The pooled estimate showed an RR of 1.10 (95% CI 0.77 to 1.57; P value = 0.59) indicating no difference in the failure rates. There was moderate heterogeneity between the studies (P value = 0.15; I2 = 47%), with similar methodology and materials used in both trials (Analysis 2.1).
Adverse effects on health
Adverse effects on health were not reported.
Patient satisfaction
Patient satisfaction was not reported.
Comparison 3: removable retainers versus removable retainers
Eight studies compared different types of removable retainers (Aslan 2013; Gill 2007; Kumar 2011; Rohaya 2006; Rowland 2007; Shawesh 2010; Sun 2011; Thickett 2010).
Three studies compared Hawley retainers with thermoplastic retainers, but they were worn for different lengths time per day (Rohaya 2006; Rowland 2007; Sun 2011):
upper Hawley retainers full‐time for three months then six months nights only versus upper and lower thermoplastic retainers worn full‐time for one week then part‐time (nights only) (Rohaya 2006);
upper and lower Hawley retainers worn full‐time for three months then nights only (12 hours per day) versus upper and lower thermoplastic retainers worn full‐time for one week then part‐time (12 hours per day) (Rowland 2007);
upper and lower Hawley retainers versus upper and lower thermoplastic retainers worn full‐time (Sun 2011).
One study compared Begg retainers with thermoplastic retainers (Kumar 2011). The participants were instructed to wear their retainers full‐time for six months then part‐time for six months (12 hours per day).
One study compared modified thermoplastic retainers and full‐coverage thermoplastic retainers (Aslan 2013). Participants were asked to wear their retainers full‐time for six months then nights only for three months.
Two studies compared part‐time wear of thermoplastic retainers with full‐time wear of thermoplastic retainers (Gill 2007; Thickett 2010). Gill 2007 defined part‐time as eight hours per day, and Thickett 2010 defined part‐time as 10 hours per day.
One study compared part‐time wear of Hawley retainers (nights only) with full‐time wear of Hawley retainers (Shawesh 2010).
All eight studies reported stability but they assessed it in a variety of ways:
Little's Irregularity Index for each arch (Gill 2007; Rowland 2007; Shawesh 2010; Thickett 2010);
mean Little's Irregularity Index for both arches (Kumar 2011);
crowding (Shawesh 2010);
intercanine and intermolar width (Gill 2007; Rowland 2007);
overjet and overbite (Gill 2007);
settling assessed by increase in occlusal contacts (Aslan 2013);
stability of corrected rotations (Rohaya 2006);
quality of finish measured by PAR index (Kumar 2011).
Two studies investigated failure of retainers (Rowland 2007; Sun 2011).
One study investigated participant satisfaction (Rowland 2007).
Although there were eight studies comparing removable retainers with other removable retainers, only two studies compared similar interventions and similar outcomes (Gill 2007; Thickett 2010). However, it was not possible to pool the results in a meta‐analysis, as the data from the Thickett 2010 study were presented as medians and interquartile ranges, so could not be put into Review Manager 5 (RevMan 2014), but are presented in Table 5.
2. Thickett table of results: medians for full‐time (group 1) and part‐time (group 2) at debond and after one year.
| Outcome | Full‐time at debond | Part‐time at debond | P value at debond | Full‐time after 1 year | Part‐time after 1 year | P value after 1 year |
| LII | 0.04 | 0.14 | 0.46 | 0.71 | 0.89 | 0.5 |
| UII | 0.21 | 0.14 | 0.14 | 1.08 | 1.09 | 0.8 |
| Lower intercanine width | 27.24 | 27.07 | 0.22 | 27.07 | 26.47 | 0.65 |
| Lower intermolar width | 34.09 | 33.32 | 0.52 | 34.35 | 33.6 | 0.61 |
| Lower arch length | 21.1 | 21.02 | 0.44 | 21.28 | 20.14 | 0.06 |
| Upper intercanine width | 35.49 | 34.79 | 0.08 | 34.93 | 34.56 | 0.52 |
| Upper intermolar width | 40.23 | 39.57 | 0.35 | 40.34 | 39.39 | 0.68 |
| Upper arch length | 24.98 | 24.19 | 0.22 | 25.07 | 25.15 | 0.97 |
| Overjet | 2.54 | 2.36 | 0.6 | 2.76 | 2.39 | 0.37 |
| Overbite | 2.86 | 3.31 | 0.14 | 3.14 | 3.74 | 0.05 (P value < 0.05) |
LII: lower Little's Irregularity Index in mm; UII: upper Little's Irregularity Index in mm.
Stability
Seven studies investigated stability when comparing removable retainers.
Modified versus full coverage thermoplastic retainers
Aslan 2013 assessed stability by reporting "settling". This describes the favourable changes in occlusion that happens after treatment is completed, and may be affected by the nature and duration of wear of retainers (see glossary of terms in Appendix 1). There was no difference in the number of total occlusal contacts after six months of full‐time wear. After three further months of nights‐only wear, there was a statistically significant increase in posterior occlusal contacts in the modified thermoplastic group compared with the full coverage thermoplastic retainers (MD 0.95, 95% CI 0.05 to 1.85; P value = 0.038) (Analysis 3.11). However, it is doubtful that an increase in total occlusal contacts from 23 to 35 is clinically significant. There was a statistically significant increase in total anterior occlusal contacts in the full coverage thermoplastic retainers; however, once again the difference of one extra occlusal contact would not be regarded as clinically significant (Analysis 3.12).
3.11. Analysis.
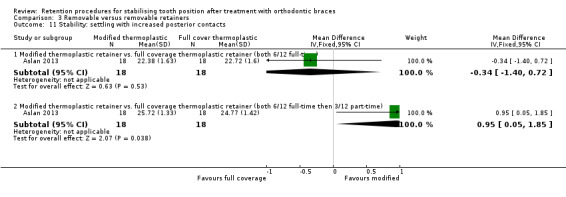
Comparison 3 Removable versus removable retainers, Outcome 11 Stability: settling with increased posterior contacts.
3.12. Analysis.
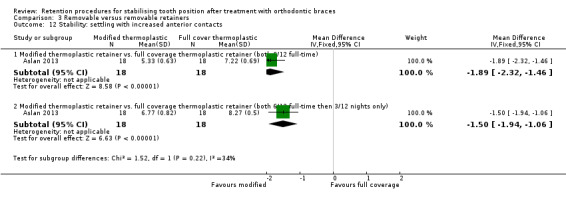
Comparison 3 Removable versus removable retainers, Outcome 12 Stability: settling with increased anterior contacts.
Full‐time versus part‐time wear of thermoplastic retainers
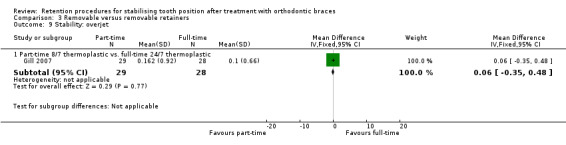
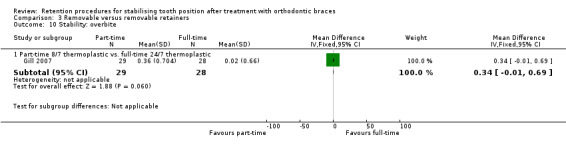
Gill 2007 and Thickett 2010 both compared full‐time wear of thermoplastic retainers versus part‐time wear of thermoplastic retainers. The results from the Gill 2007 study showed no statistical difference in terms of Little's Irregularity Index, intercanine width and intermolar width in both upper and lower arches, and no difference in overjet or overbite (Analysis 3.5; Analysis 3.6; Analysis 3.7; Analysis 3.8; Analysis 3.9; Analysis 3.10). Table 5 presents the results from Thickett 2010. They found no statistical difference in Little's Irregularity Index, arch length, intercanine width and intermolar width in both upper and lower arches, and no difference in overjet. They did find a statistical difference in overbite, but as the difference was 0.6 mm it is unlikely to be clinically significant. While the results could not be combined in a meta‐analysis, the finding of both studies was that there was no evidence of a difference in stability when thermoplastic retainers were worn full‐time or part‐time.
3.5. Analysis.
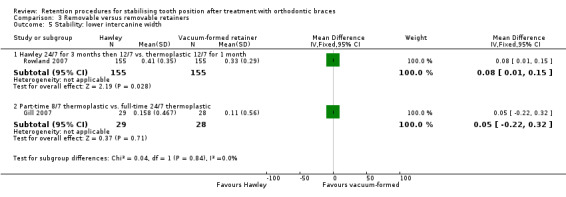
Comparison 3 Removable versus removable retainers, Outcome 5 Stability: lower intercanine width.
3.6. Analysis.
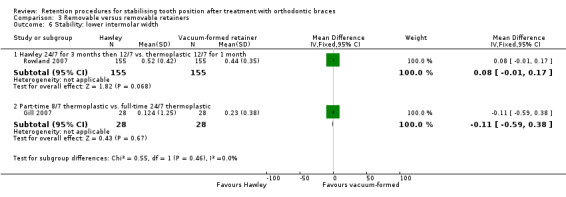
Comparison 3 Removable versus removable retainers, Outcome 6 Stability: lower intermolar width.
3.7. Analysis.
Comparison 3 Removable versus removable retainers, Outcome 7 Stability: upper intercanine width.
3.8. Analysis.
Comparison 3 Removable versus removable retainers, Outcome 8 Stability: upper intermolar width.
3.9. Analysis.
Comparison 3 Removable versus removable retainers, Outcome 9 Stability: overjet.
3.10. Analysis.
Comparison 3 Removable versus removable retainers, Outcome 10 Stability: overbite.
Full‐time versus part‐time wear of Hawley retainers
Shawesh 2010 compared full‐time wear of Hawley retainers with part‐time wear of Hawley retainers. They showed no statistical difference in Little's Irregularity Index or crowding in both arches between the two wear regimens (Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.4).
3.1. Analysis.
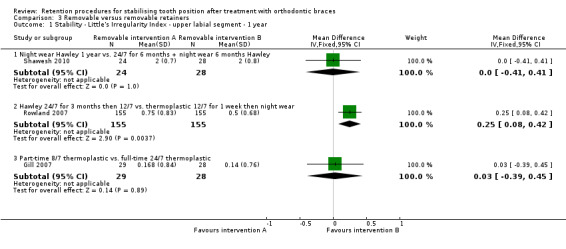
Comparison 3 Removable versus removable retainers, Outcome 1 Stability ‐ Little's Irregularity Index ‐ upper labial segment ‐ 1 year.
3.2. Analysis.
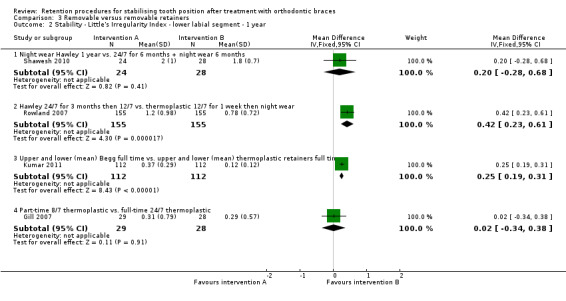
Comparison 3 Removable versus removable retainers, Outcome 2 Stability ‐ Little's Irregularity Index ‐ lower labial segment ‐ 1 year.
3.3. Analysis.
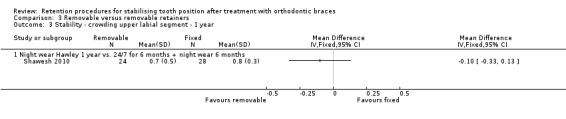
Comparison 3 Removable versus removable retainers, Outcome 3 Stability ‐ crowding upper labial segment ‐ 1 year.
3.4. Analysis.
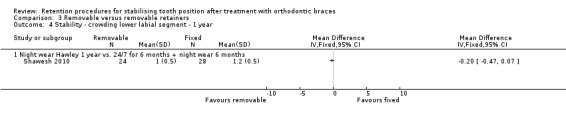
Comparison 3 Removable versus removable retainers, Outcome 4 Stability ‐ crowding lower labial segment ‐ 1 year.
Hawley retainers versus thermoplastic retainers
Rowland 2007 compared Hawley retainers with thermoplastic retainers. They found no statistically significant difference in intercanine and intermolar widths in both arches (Analysis 3.5; Analysis 3.6; Analysis 3.7; Analysis 3.8). However, they did find a statistically significant difference in Little's Irregularity Index in the upper arch, with 0.25 mm (95% CI 0.08 to 0.42; P value = 0.004) more relapse in Hawley retainer group (Analysis 3.1), and in the lower arch of 0.42 mm (95% CI 0.23 to 0.61; P value < 0.0001) more relapse in the thermoplastic retainer group (Analysis 3.2). These differences were very small. Certainly in the upper arch this difference would not be clinically significant. The difference in the lower arch may be clinically significant if the irregularity was restricted to one tooth contact.
The Rohaya 2006 study investigated the ability to maintain previously rotated teeth in a stable position, comparing Hawley retainers and thermoplastic retainers. They found that people wearing thermoplastic retainers were 4.88 times more likely to hold derotated teeth stable than people who wore Hawley retainers (95% CI 1.13 to 21.07; P value = 0.03) (Analysis 3.13). This is likely to be clinically significant.
3.13. Analysis.
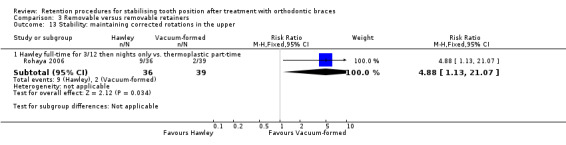
Comparison 3 Removable versus removable retainers, Outcome 13 Stability: maintaining corrected rotations in the upper.
Begg retainers versus thermoplastic retainers
Kumar 2011 compared Begg retainers with thermoplastic retainers (both groups had a bonded retainer in addition in the lower arch). There was a statistically significant difference of 0.25 mm (95% CI 0.19 to 0.31; P value < 0.000001) more irregularity in the lower arch with the Begg retainers. This is unlikely to be clinically significant. There was also a statistically significant reduction in the quality of the result of 1.71 points (95% CI 1.44 to 1.98; P value < 0.0001) on the PAR index in the Begg retainer group, indicating more relapse in this group (Analysis 3.14). Although small, this may be clinically significant.
3.14. Analysis.
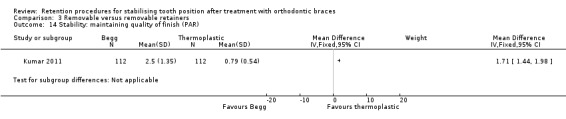
Comparison 3 Removable versus removable retainers, Outcome 14 Stability: maintaining quality of finish (PAR).
Failure of retainers
Hawley retainers versus thermoplastic retainers
Rowland 2007 compared failure rates of Hawley retainers with thermoplastic retainers. They assessed failure rates by recording how many retainers broke and how many were lost. Hawley retainers were more likely to break (32 Hawley retainers broke compared with 12 thermoplastic retainers) giving an RR of 2.96 (95% CI 1.58 to 5.55; P value = 0.000072), which is clinically significant (Analysis 3.15). There was no difference in the number of retainers that were lost (Analysis 3.16).
3.15. Analysis.

Comparison 3 Removable versus removable retainers, Outcome 15 Survival of retainers: how many broke in total.
3.16. Analysis.
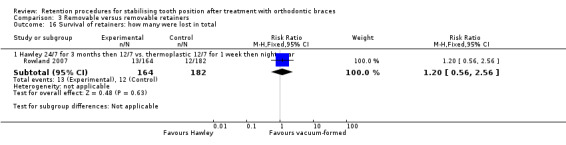
Comparison 3 Removable versus removable retainers, Outcome 16 Survival of retainers: how many were lost in total.
Sun 2011 also compared the failure rate of Hawley retainers and thermoplastic retainers. A retainer was assessed as failed if it fractured, no longer fit, showed local serious abrasion causing holes in the retainer, or loss of retainers. Failure rate was assessed separately for upper and lower retainers. Sun 2011 showed no difference in failure rates in the upper arch (Analysis 3.17). However, in the lower arch there was a statistically significant chance of thermoplastic retainers failing compared with Hawley retainers (25 Hawley compared with 41 thermoplastic). The RR was 0.60 (95% CI 0.43 to 0.83; P value = 0.0023), which is clinically significant (Analysis 3.18).
3.17. Analysis.
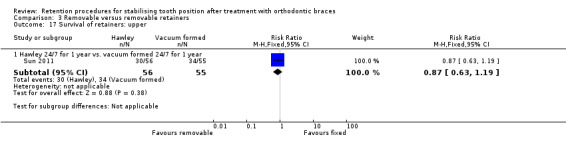
Comparison 3 Removable versus removable retainers, Outcome 17 Survival of retainers: upper.
3.18. Analysis.
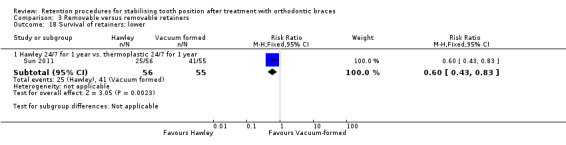
Comparison 3 Removable versus removable retainers, Outcome 18 Survival of retainers: lower.
Since failure was measured in different ways, and one study measured failure rates in total while the other measured them per arch, we could not pool the results of Rowland 2007 and Sun 2011.
Adverse effects on health
Adverse effects on health were not reported.
Patient satisfaction
Hawley retainers versus thermoplastic retainers
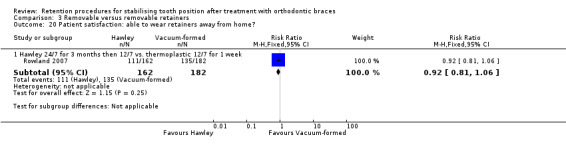
One study assessed patient satisfaction by measuring response to five questions (Rowland 2007). There was a statistically significant response in three of the questions: the participants in the thermoplastic group were more likely to report being able to wear the retainer than participants in the Hawley group, with an RR of 0.89 (95% CI 0.83 to 0.96; P value = 0.0023) (Analysis 3.19); the participants wearing the thermoplastic retainers were less likely to report feeling embarrassed by the retainers, with an RR of 2.42 (95% CI 1.30 to 4.49; P value = 0.0052) (Analysis 3.21); more participants reported that it was more difficult wear Hawley retainers than thermoplastic retainers, when compared with fixed appliances, with an RR of 9.37 (95% CI 3.80 to 23.10; P value < 0.00001) (Analysis 3.23). All of these findings were clinically significant. There was no difference between the two retainers in the amount of discomfort experienced (Analysis 3.22), or whether people were able to wear the retainers away from home (Analysis 3.20).
3.19. Analysis.
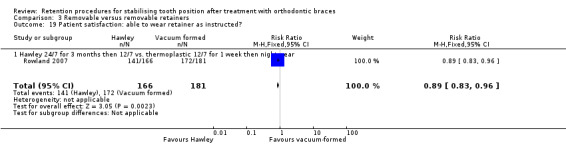
Comparison 3 Removable versus removable retainers, Outcome 19 Patient satisfaction: able to wear retainer as instructed?.
3.21. Analysis.
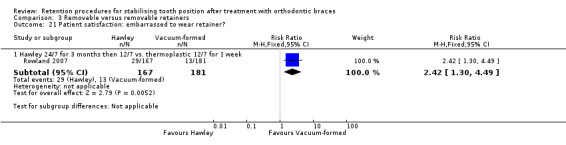
Comparison 3 Removable versus removable retainers, Outcome 21 Patient satisfaction: embarrassed to wear retainer?.
3.23. Analysis.
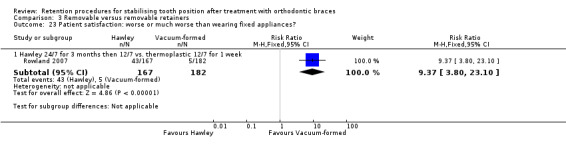
Comparison 3 Removable versus removable retainers, Outcome 23 Patient satisfaction: worse or much worse than wearing fixed appliances?.
3.22. Analysis.
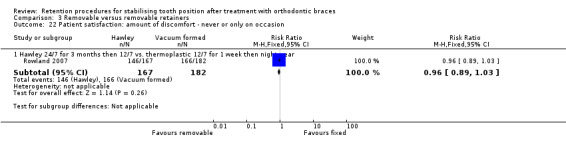
Comparison 3 Removable versus removable retainers, Outcome 22 Patient satisfaction: amount of discomfort ‐ never or only on occasion.
3.20. Analysis.
Comparison 3 Removable versus removable retainers, Outcome 20 Patient satisfaction: able to wear retainers away from home?.
Comparison 4: upper removable and lower fixed retainer versus upper removable retainer and lower adjunctive procedure
Upper removable and lower fixed retainer versus upper removable retainer and lower adjunctive procedure
The Edman Tynelius 2015 study compared an upper thermoplastic retainer and lower rigid stainless steel retainer from lower canine to canine with an upper thermoplastic retainer and the adjunctive procedure of interproximal reduction in the lower arch, with no lower retainer. They measured stability at one, two and five years. Change data were reported for Little's Irregularity Index in both arches, upper and lower intercanine and intermolar width, arch length, overjet and overbite at one and two years. The final Little's Irregularity Index (change data were not available) was reported for both arches at five years.
After one year, there was a statistically significant reduction of 1 mm in the lower intercanine width in the interproximal stripping without lower retainer group (95% CI ‐1.22 to ‐0.78; P value < 0.00001), which may be clinically significant (Analysis 4.6). There was also a statistically significant increase of 0.7 mm in the lower arch length in the lower fixed retainer group (95% CI 0.2 to 1.2; P value = 0.0063), which we would not perceive as clinically significant (Analysis 4.8). There was no difference in the Little's Irregularity Index in either arch, intercanine width in the upper arch, intermolar width in either arch, arch length in the upper arch, overjet or overbite (Analysis 4.1; Analysis 4.2; Analysis 4.3; Analysis 4.4; Analysis 4.5; Analysis 4.7; Analysis 4.9; Analysis 4.10).
4.6. Analysis.
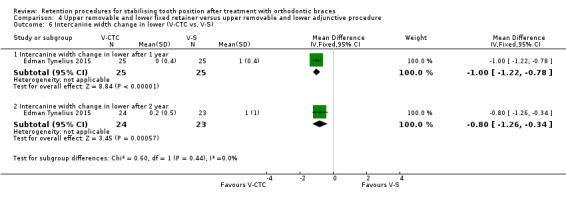
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 6 Intercanine width change in lower (V‐CTC vs. V‐S).
4.8. Analysis.
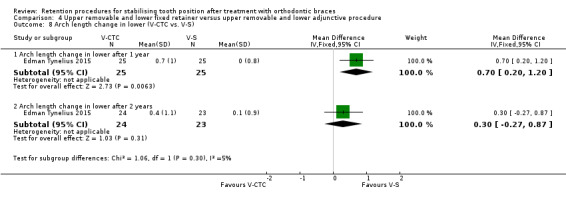
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 8 Arch length change in lower (V‐CTC vs. V‐S).
4.1. Analysis.
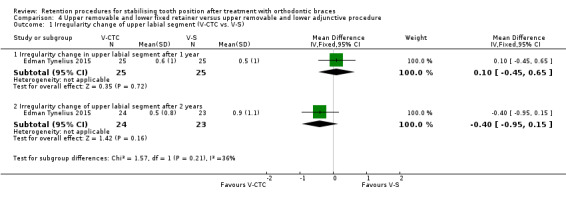
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 1 Irregularity change of upper labial segment (V‐CTC vs. V‐S).
4.2. Analysis.
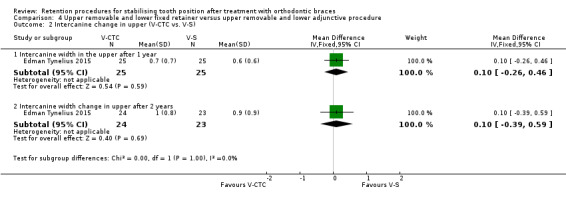
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 2 Intercanine change in upper (V‐CTC vs. V‐S).
4.3. Analysis.
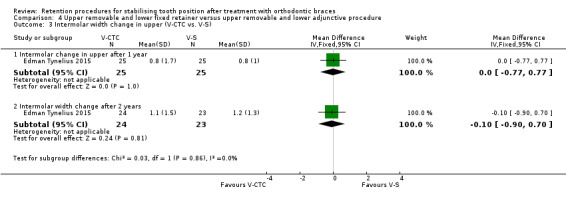
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 3 Intermolar width change in upper (V‐CTC vs. V‐S).
4.4. Analysis.
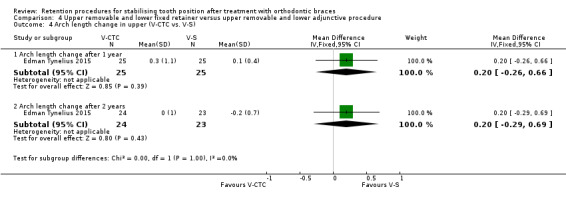
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 4 Arch length change in upper (V‐CTC vs. V‐S).
4.5. Analysis.
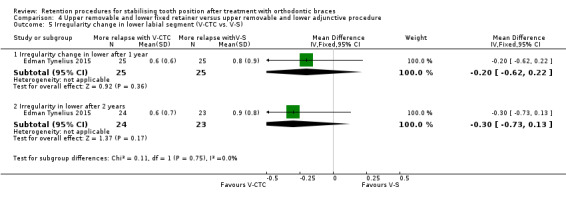
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 5 Irregularity change in lower labial segment (V‐CTC vs. V‐S).
4.7. Analysis.
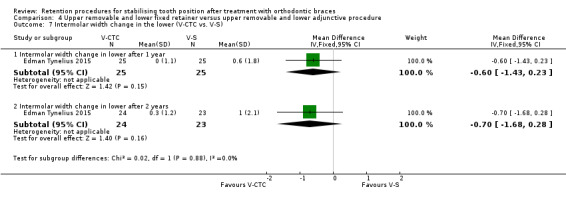
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 7 Intermolar width change in the lower (V‐CTC vs. V‐S).
4.9. Analysis.
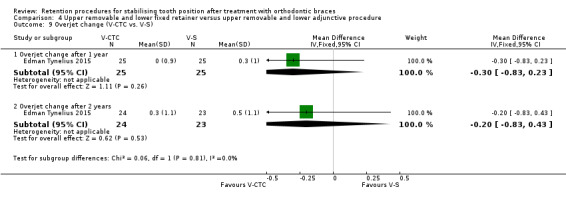
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 9 Overjet change (V‐CTC vs. V‐S).
4.10. Analysis.
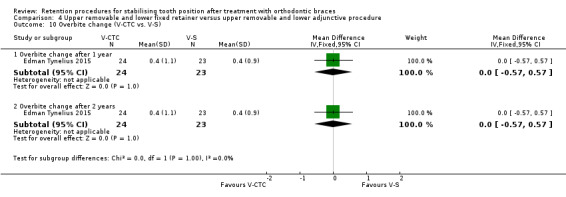
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 10 Overbite change (V‐CTC vs. V‐S).
After two years, there was a statistically significant reduction of 0.8 mm in the lower intercanine width in the interproximal stripping without lower retainer group (95% CI ‐1.26 to ‐0.34; P value = 0.0057), which is unlikely to be clinically significant (Analysis 4.6). There was no difference in the Little's Irregularity Index in either arch, intercanine width in the upper arch, intermolar width in either arch, arch length in either arch, overjet or overbite (Analysis 4.1; Analysis 4.2; Analysis 4.3; Analysis 4.4; Analysis 4.5; Analysis 4.7; Analysis 4.8; Analysis 4.9; Analysis 4.10).
After five years, there was no difference in the final Little's Irregularity Index in either the upper arch or the lower arch (Analysis 4.11; Analysis 4.12).
4.11. Analysis.
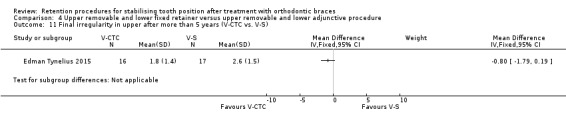
Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 11 Final irregularity in upper after more than 5 years (V‐CTC vs. V‐S).
4.12. Analysis.

Comparison 4 Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure, Outcome 12 Final irregularity in lower after more than 5 years (V‐CTC vs. V‐S).
Comparison 5: upper removable and lower fixed retainer versus positioner
Upper removable and lower fixed retainer versus positioner
The Edman Tynelius 2015 study compared an upper thermoplastic retainer and lower rigid stainless steel retainer from lower canine to canine with a positioner. They measured stability at one, two and five years. Change data were reported for Little's Irregularity Index in both arches, upper and lower intercanine and intermolar width, arch length, overjet and overbite at one and two years. The final Little's Irregularity Index (change data were not available) was reported for both arches at five years.
After one year, there was a statistically significant reduction of 0.7 mm in the lower intercanine width in the interproximal stripping without lower retainer group (95% CI ‐1.14 to ‐0.26; P value = 0.0017), but we would not perceive this to be clinically significant (Analysis 5.6). There was no difference in the Little's Irregularity Index in either arch, intercanine width in the upper arch, intermolar width in either arch, arch length in either arch, overjet or overbite (Analysis 5.1; Analysis 5.2; Analysis 5.3; Analysis 5.4; Analysis 5.5; Analysis 5.7; Analysis 5.8; Analysis 5.9; Analysis 5.10).
5.6. Analysis.

Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 6 Intercanine width change in lower (V‐CTC vs. P).
5.1. Analysis.
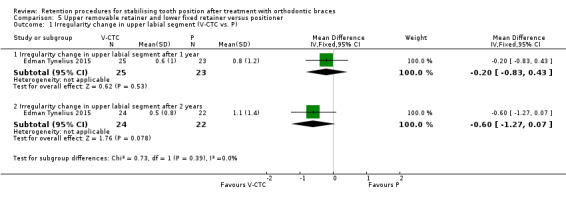
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 1 Irregularity change in upper labial segment (V‐CTC vs. P).
5.2. Analysis.
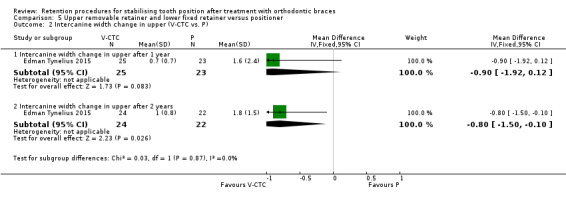
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 2 Intercanine width change in upper (V‐CTC vs. P).
5.3. Analysis.
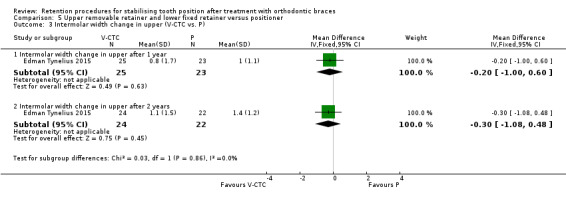
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 3 Intermolar width change in upper (V‐CTC vs. P).
5.4. Analysis.
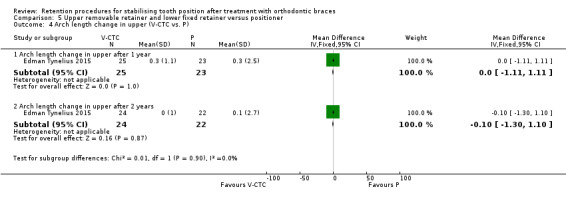
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 4 Arch length change in upper (V‐CTC vs. P).
5.5. Analysis.
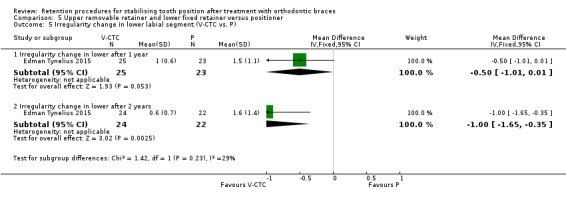
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 5 Irregularity change in lower labial segment (V‐CTC vs. P).
5.7. Analysis.
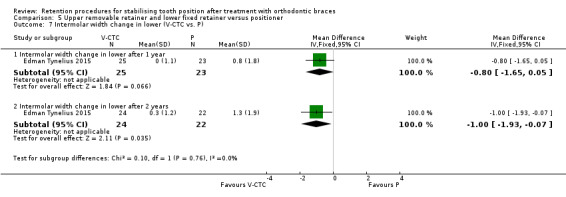
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 7 Intermolar width change in lower (V‐CTC vs. P).
5.8. Analysis.
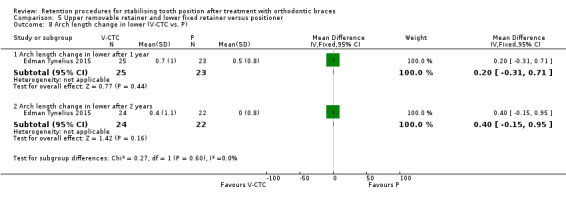
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 8 Arch length change in lower (V‐CTC vs. P).
5.9. Analysis.
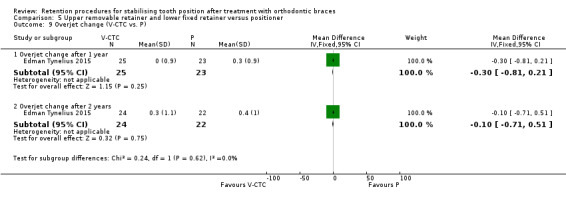
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 9 Overjet change (V‐CTC vs. P).
5.10. Analysis.
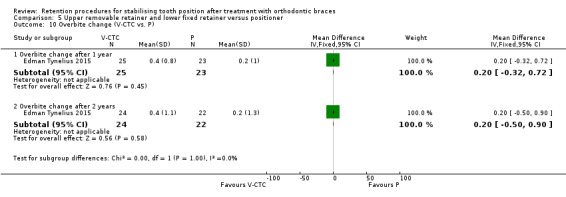
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 10 Overbite change (V‐CTC vs. P).
After two years, there was a statistically significant difference in the upper intercanine width, lower Little's Irregularity Index, lower intercanine width and lower intermolar width. The upper intercanine width reduced more in the positioner group by 0.8 mm (95% CI ‐1.50 to ‐0.10; P value = 0.026), but this is unlikely to be clinically significant (Analysis 5.2). The Little's Irregularity Index in the lower arch increased by 1 mm in the positioner group (95% CI ‐1.65 to ‐0.35; P value = 0.0025), and this is clinically significant (Analysis 5.5). The lower intercanine width decreased by 0.8 mm in the positioner group (95% ‐1.34 to ‐0.26; P value = 0.0037), which we would not regard as clinically significant (Analysis 5.6). The intermolar width decreased by 1 mm in the positioner group (95% CI ‐1.93 to ‐0.07; P value = 0.035), which may be clinically significant (Analysis 5.7). There was no difference in the Little's Irregularity Index in the upper arch, upper intermolar width, upper arch length, lower arch length, overjet and overbite (Analysis 5.1; Analysis 5.3; Analysis 5.4; Analysis 5.7; Analysis 5.8; Analysis 5.9; Analysis 5.10).
After five years, there was significantly more relapse of 1.30 mm change in Little's Irregularity Index in the lower arch with the positioner (95% CI ‐2.42 to ‐0.18; P value = 0.023), which is clinically significant (Analysis 5.12). There was no difference in the upper arch Little's Irregularity Index (Analysis 5.11).
5.12. Analysis.
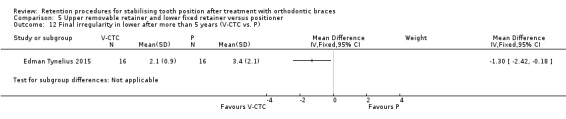
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 12 Final irregularity in lower after more than 5 years (V‐CTC vs. P).
5.11. Analysis.
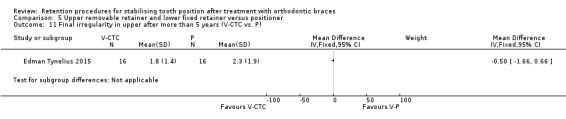
Comparison 5 Upper removable retainer and lower fixed retainer versus positioner, Outcome 11 Final irregularity in upper after more than 5 years (V‐CTC vs. P).
Comparison 6: upper removable retainer and lower adjunctive procedure versus positioner
Upper removable retainer and lower adjunctive procedure versus positioner
The Edman Tynelius 2015 study compared an upper thermoplastic retainer and lower adjunctive procedure of interproximal stripping with a positioner. They measured stability at one, two and five years. Change data were reported for Little's Irregularity Index in both arches, upper and lower intercanine and intermolar width, arch length, overjet and overbite at one and two years. The final Little's Irregularity Index (change data were not available) was reported for both arches at five years.
After one year, there was a statistically significant increase of 0.5 mm in the lower arch length with the positioner (95% CI ‐0.95 to ‐0.05; P value = 0.031), which was not clinically significant (Analysis 6.8). There was no difference in the Little's Irregularity Index in both arches, intercanine or intermolar widths in both arches, upper arch length, overjet and overbite (Analysis 6.1; Analysis 6.2; Analysis 6.3; Analysis 6.4; Analysis 6.5; Analysis 6.6; Analysis 6.7; Analysis 6.9; Analysis 6.10).
6.8. Analysis.

Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 8 Arch length change in lower (V‐S vs. P).
6.1. Analysis.
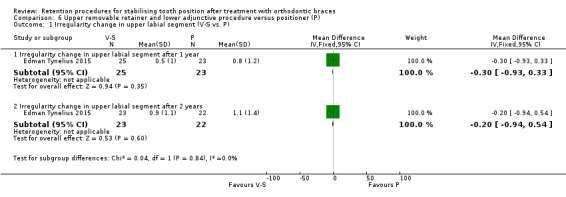
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 1 Irregularity change in upper labial segment (V‐S vs. P).
6.2. Analysis.
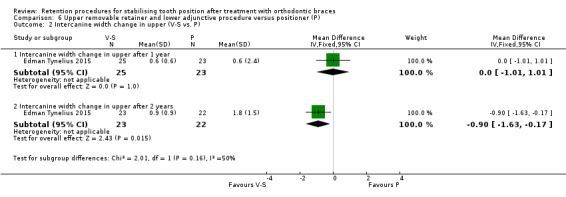
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 2 Intercanine width change in upper (V‐S vs. P).
6.3. Analysis.
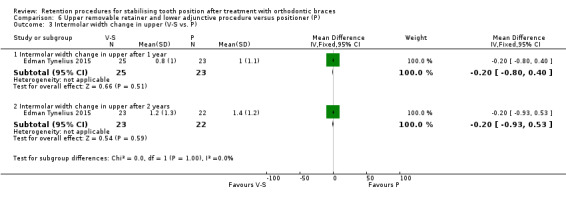
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 3 Intermolar width change in upper (V‐S vs. P).
6.4. Analysis.
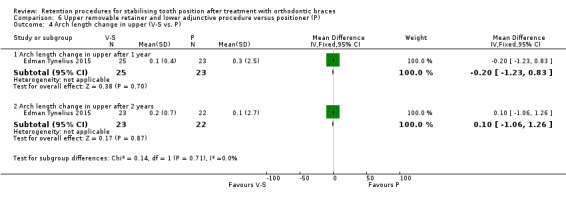
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 4 Arch length change in upper (V‐S vs. P).
6.5. Analysis.
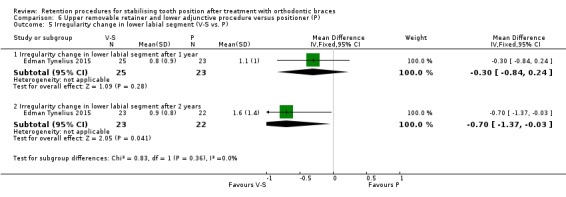
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 5 Irregularity change in lower labial segment (V‐S vs. P).
6.6. Analysis.
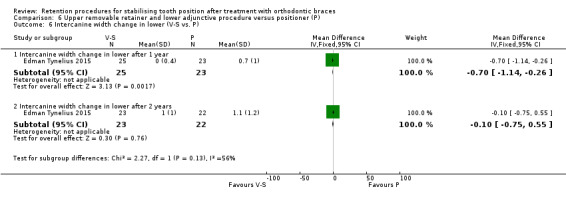
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 6 Intercanine width change in lower (V‐S vs. P).
6.7. Analysis.
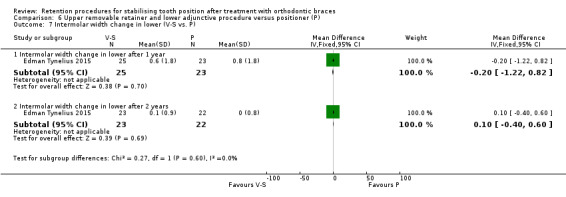
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 7 Intermolar width change in lower (V‐S vs. P).
6.9. Analysis.
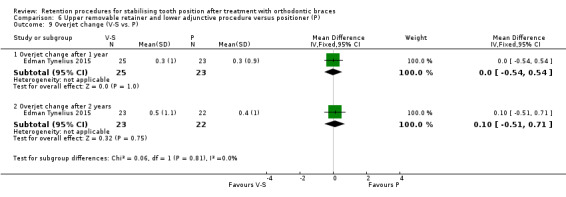
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 9 Overjet change (V‐S vs. P).
6.10. Analysis.
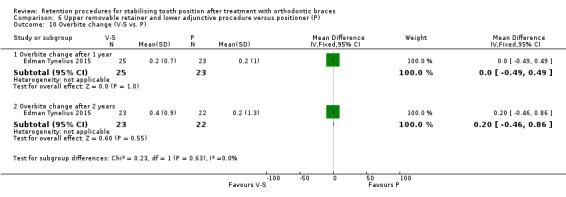
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 10 Overbite change (V‐S vs. P).
After two years, there was a statistically significant difference reduction of 0.90 mm in upper intercanine width with the positioner (95% CI ‐1.63 to ‐0.17; P value = 0.0015), which is not clinically significant (Analysis 6.2). There was also an increase of 0.70 mm in the lower Little's Irregularity Index (95% CI ‐1.37 to ‐0.03; P value = 0.0041), which was also not clinically significant (Analysis 6.5). There was no difference in Little's Irregularity Index in the upper arch, intercanine width in the lower arch, intermolar width in both arches, arch length in both arches, overjet and overbite (Analysis 6.1; Analysis 6.3; Analysis 6.4; Analysis 6.6; Analysis 6.7; Analysis 6.8; Analysis 6.9; Analysis 6.10).
After five years, there was a statistically significant 1.40 mm more relapse in the positioner group in the final lower arch Little's Irregularity Index (95% CI ‐2.77 to ‐0.03; P value = 0.045), which was clinically significant (Analysis 6.12). There was no difference in the final upper Little's Irregularity Index (Analysis 6.11).
6.12. Analysis.
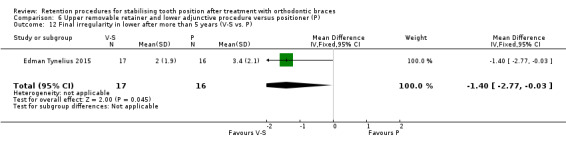
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 12 Final irregularity in lower after more than 5 years (V‐S vs. P).
6.11. Analysis.
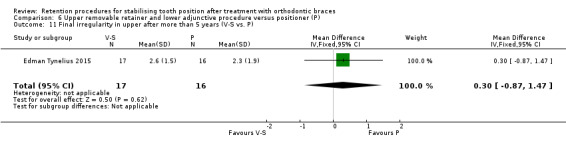
Comparison 6 Upper removable retainer and lower adjunctive procedure versus positioner (P), Outcome 11 Final irregularity in upper after more than 5 years (V‐S vs. P).
Discussion
Summary of main results
Removable retainers versus fixed retainers
Lower multistrand retainer versus lower thermoplastic retainer
We found limited evidence to suggest that multistrand bonded retainers were slightly better at reducing relapse in the lower arch than thermoplastic retainers (Millett 2007; O'Rourke [pers comm]). The bonded retainers were better at reducing irregularity, but there was no difference in maintaining intercanine width, intermolar width and arch length of extraction space opening. There was conflicting evidence about failure rates of these types of retainers (Millett 2007; O'Rourke [pers comm]). There was limited evidence to suggest that bonded retainers lead to increased gingival bleeding compared with thermoplastic retainers, but neither retainer appeared to predispose to caries (Millett 2007). There was some evidence to show that patient satisfaction was higher with bonded retainers, with participants reporting that they were more acceptable to wear than thermoplastic retainers (Millett 2007).
Fixed retainers versus fixed retainers
Polyethylene ribbon fixed retainer versus multistrand fixed retainer
We found weak evidence to suggest that there is no difference in failure rates of polyethylene ribbon fixed retainers and multistrand fixed retainers (Bolla 2012; Rose 2002; Salehi 2013). We were able to pool the data for these studies as the materials and methodology were similar.
Removable retainers versus removable retainers
Part‐time wear versus full‐time wear of thermoplastic retainers
Two studies failed to find a difference in stability between part‐time and full‐time wear (Gill 2007; Thickett 2010). The data from the studies could not be pooled, as the data from Thickett 2010 could not be entered into Review Manager 5 (RevMan 2014); however, both studies reached the same conclusions and we assessed this evidence as of moderate quality.
Hawley retainers versus thermoplastic retainers
There was limited evidence to suggest that thermoplastic retainers offer better retention in the lower arch than Hawley retainers. Rowland 2007 showed a small increase in irregularity in the lower arch with Hawley retainers, although this was unlikely to be significant unless the irregularity was restricted to one tooth contact. One study showed that thermoplastic retainers prevented relapse of previously rotated teeth in the upper arch better than Hawley retainers (Rohaya 2006).
We found limited evidence from two studies looking at failure rates of these two types of retainers (Rowland 2007; Sun 2011). The studies could not be combined due to the marked difference in materials and methodology, in particular that in one study the retainers were worn for long periods on a part‐time basis (Rowland 2007), and in the other study they were worn full‐time except at meal times (Sun 2011). When Hawley retainers were worn three months full‐time, then nine months part‐time, and the vacuum‐formed retainers were worn part‐time, there were more breakages in the Hawley retainers (Rowland 2007). When both sets of retainers were worn full‐time except at meal times, there were more failures in the thermoplastic retainer group (Sun 2011).
There was limited evidence of a greater level of patient satisfaction with thermoplastic retainers than Hawley retainers (Rowland 2007). Participants wearing thermoplastic retainers reported less embarrassment at wearing them than reported by participants wearing Hawley retainers. The participants who wore thermoplastic retainers also found them easier to wear than participants with Hawley retainers, when comparing the retainers to their experience with fixed appliances.
Begg retainers versus thermoplastic retainers
There was limited evidence that thermoplastic retainers may retain the quality of the result better than Begg retainers (Kumar 2011).
Part‐time wear versus full‐time wear of Hawley retainers
There was limited evidence that part‐time wear of Hawley retainers was as effective for preventing relapse of irregular and crowded teeth as full‐time wear (Shawesh 2010).
Full‐coverage versus modified thermoplastic retainers
There was limited evidence that there was no difference in the amount of settling between full‐coverage retainers and modified thermoplastic retainers after six months of full‐time wear (Aslan 2013). However, after moving to a period of part‐time wear, there was more settling (increased occlusal contacts) with the modified thermoplastic retainers.
Upper removable and fixed retainer versus upper removable and lower adjunctive procedure versus positioner
Based on the results of one study, all three approaches maintained the teeth in a reasonably stable position for the first year (Edman Tynelius 2015). However, after two years, there was greater irregularity in the lower arch with the positioner, which could be clinically significant. The fact that adequate stability was maintained in the group with adjunctive procedure but no lower retainer is interesting, because in recent decades it has been presumed that all participants had to wear some sort of retainer to maintain stability. It is important to emphasise that the participants initially presented with normal jaw relationships in all three dimensions (anteroposterior, vertical and transverse proportions), and so were essentially Class I crowding cases. Typically, teeth do not need to be moved as far in these cases. When trying to straighten teeth and obtain a good bite when the jaws do not meet together well, teeth need to be moved further to compensate for this. As a result, it may not be possible to extrapolate these results to most people requiring orthodontic treatment.
Overall completeness and applicability of evidence
Overall, we included 15 studies investigating different approaches to retention and with multiple outcomes in this review. Three studies compared different removable retainers with fixed retainers. Four studies compared different types of fixed retainers. Eight studies compared different types of removable retainers.
One further study, compared a combination of upper thermoplastic and lower bonded versus upper thermoplastic with lower adjunctive procedures versus positioner (Edman Tynelius 2015). It is important to note that there were very strict inclusion criteria for this study and, while the study was well conducted with a low risk of bias, it is important to recognise that the findings may only be applicable to people with similar malocclusions (crowded cases with normal positions of the jaws in all three dimensions).
Only three of the 15 studies reported outcomes beyond two years. This is important as it is felt that retainers may be needed indefinitely to reduce the chances of relapse, so the findings of this review predominantly will inform clinicians of the effects of different approaches to retention in the short term.
When interpreting the results of this review, it is important to remember that the results of the studies may be affected by the age of the participants, initial malocclusions, treatment procedure, amount and type of tooth movement, along with other possible factors that may affect relapse. The impact of these areas is still not fully understood, and is beyond the scope of this review. However, the broader context should always be considered when interpreting studies reporting the stabilising effects of retainers and adjunctive techniques.
There is no agreed Core Outcome Measure in Effectiveness Trials (COMET) for relapse studies in orthodontics at the present time. Therefore, the review authors have prioritised reporting Little's Irregularity Index as the preferred outcome for this review.
We identified four ongoing studies and four studies that are currently awaiting classification and may be included in the next update of this review (see Characteristics of studies awaiting classification and Characteristics of ongoing studies).
Quality of the evidence
The overall quality of evidence is reported in the 'Summary of findings' tables (Table 1; Table 2; Table 3).
Removable retainer versus fixed retainer
There was low quality evidence to assess stability, in the lower arch, adverse effects on health and patient satisfaction. We downgraded the evidence due to high risk of bias and imprecision. There was very low evidence for failure of retainers, with the quality of evidence downgraded three times due to high risk of bias, imprecision and inconsistency. This low quality, or very low quality, of evidence means that future research is very likely to have an impact on our confidence in the estimate of effect and likely to change the estimate.
Fixed retainer versus fixed retainer
There was low quality evidence on failure of retainers, downgraded twice due to high risk of bias and imprecision. This low quality evidence means that future research is very likely to have an impact on our confidence in the estimate of effect and likely to change the estimate.
Removable retainer versus removable retainer
There was moderate quality evidence comparing full‐time wear with part‐time wear of thermoplastic retainers. The results were based on only one study and we downgraded this evidence once due to imprecision. Moderate quality evidence means that further research in this area is likely to have an important impact on our confidence in the estimate of effect, and may change the estimate.
There was low quality evidence in further studies comparing different types of removable retainers: part‐time versus full‐time wear of Hawley retainers; Hawley versus thermoplastic retainers and Begg versus thermoplastic retainers. We downgraded all these low quality studies twice due to high risk of bias and imprecision. Low quality evidence means that future research in these areas is very likely to have an impact on our confidence in the estimate of effect and likely to change the estimate.
Potential biases in the review process
We have used a broad sensitive search strategy of multiple databases, and also searched for unpublished studies and data, without language restrictions. Therefore, we hope that potential bias in the review process has been minimised. We could not analyse two of the studies in Review Manager 5 (RevMan 2014), as the data were reported as medians (O'Rourke [pers comm]; Thickett 2010). Therefore, we can only report the findings of the authors and so we have not included their findings in our final conclusions.
Agreements and disagreements with other studies or reviews
Mai 2014 is a systematic review that investigated Hawley retainers compared to thermoplastic retainers. They identified seven studies to include, but this was because, in addition to randomised controlled clinical trials, they included quasi‐randomised and controlled clinical trials. They reported that there was some evidence to suggest "that there are no differences with respect to changes in intercanine and intermolar widths between Hawley retainers and vacuum‐formed retainers after orthodontic retention". This finding is different to our conclusions, but this was due to different inclusion criteria to our review.
Authors' conclusions
Implications for practice.
We did not find any evidence that wearing thermoplastic retainers full‐time provides greater stability than wearing them part‐time, but this was assessed in only a small number of participants.
Overall, there is insufficient high quality evidence to make recommendations on retention procedures for stabilising tooth position after treatment with orthodontic braces. Further high quality RCTs are needed.
Implications for research.
Retention studies are not easy to undertake, but several randomised controlled clinical trials have now been completed showing that this research is feasible. Relapse is a long‐term problem and long‐term follow‐up of participants is practically difficult and financially demanding. However, given that the vast majority of people requiring orthodontic treatment undergo a phase of retention, this vital area of orthodontic research should continue to be given priority. To minimise the risk of bias, future studies in this field should address the following features:
adequate allocation concealment and appropriate generation of randomisation;
blinding of outcome assessors;
adequate reporting and analysis of withdrawals and drop‐outs;
reporting of all data that are collected;
a priori sample size calculations;
clear inclusion and exclusion criteria;
ideally follow‐up for a number of years, given the long‐term nature of the problem of relapse.
Although some RCTs have addressed aspects of retention given below, further high quality studies in these areas are needed to increase the evidence base:
to compare different types of retainers (fixed and removable);
to investigate the effects of different adjunctive techniques, such as pericision and interproximal reduction;
to further investigate whether adjunctive techniques, for example interproximal reduction, may be sufficient without retainers to provide adequate retention;
to investigate levels of patient satisfaction to different retention regimens, including no retention.
Appropriate outcomes to investigate include:
stability;
survival of retainers;
adverse effects on oral health;
patient satisfaction assessment.
In particular, it would be useful to assess these outcomes over the long term.
What's new
| Date | Event | Description |
|---|---|---|
| 26 January 2016 | New citation required but conclusions have not changed | Search re‐run. Review now includes 13 new studies, making a total of 15 included studies. There are 4 ongoing studies and 4 studies awaiting classification. |
| 26 January 2016 | New search has been performed | Search updated. It was decided to only include randomised controlled trials. Quasi‐randomised controlled trials that had been included in previous reviews were no longer included, to reduce risk of bias and to increase confidence in the results. As a result, three studies that were previously included have now been excluded. |
History
Protocol first published: Issue 3, 2000 Review first published: Issue 1, 2004
| Date | Event | Description |
|---|---|---|
| 19 August 2008 | Amended | Converted to new review format. |
| 11 November 2005 | New search has been performed | This update of the review includes one more study bringing the total number up to five. The search (May 2005) was conducted 28 months after the initial search (January 2003). The results of the review remain unchanged. |
Acknowledgements
We would like to thank Sue Furness, Anne Littlewood, Philip Riley, Sylvia Bickley, Emma Tavender, Luisa Fernandez, Laura MacDonald, Anne‐Marie Glenny and the rest of the Cochrane Oral Health Group for their kind assistance in completing the original review and this update. We would like to thank those who acted as referees for this update: Susan Cunningham, Hend Elsayed and John Fricker.
Appendices
Appendix 1. Glossary of terms
A. Removable retainers in this review
Hawley retainer
This is the oldest reported removable retainer, first described in 1919. It consists of an acrylic baseplate that covers the palate or lies behind the lower teeth, and is usually held in place by attachments known as Adam's clasps that clip onto the first molar tooth that is present in each quadrant. There is typically a labial bow that crosses the labial surfaces of the anterior teeth, which acts to hold the retainer in place, and maintain the stability of the front teeth.
Thermoplastic retainer
This is a clear plastic retainer that typically cover all the teeth. It is formed by heating up a sheet of plastic and moulding this around a model of the patient’s teeth after the treatment is complete. This moulding can be by 'vacuum‐forming' (when the retainers are often referred to as vacuum‐formed retainers), or by pressure. It can be modified to change the amount of occlusal coverage they have.
Begg retainer
This is a removable retainer that is similar to a Hawley retainer. It also has an acrylic baseplate that covers the palate, or lies behind the lower teeth, but does not have clasps covering the occlusal (biting) surfaces. It is retained principally by the labial bow wire, which runs on the outside of all the teeth. The aim is to allow more occlusal settling, but retention of the appliance may not be as good as Hawley retainers due to the lack of specific clasps attached to teeth.
B. Fixed retainers in this review
Multistrand wire fixed retainer
Multistrand wire is a flexible wire made up of smaller diameter stainless steel wires wound together like a piece of rope. It is typically bonded to every tooth in the labial segment. It is usually bonded with composite resin adhesive.
Thick canine to canine retainer
This fixed retainer is made of stainless steel, but is of a thicker diameter than the multistrand and, therefore, more rigid. It is typically bonded only to the canines (hence the name). It is used to allow easier cleaning of the incisors. The other potential advantage that is claimed is that if either attachment fails, the person will know about it (this may not be the case if one of the attachments on the multistrand fails). However, it does not bond to the incisors, so some operators feel there may be the potential for relapse of these teeth.
Polyethylene ribbon retainer
This is a plasma‐treated polyethylene woven ribbon that can be adapted to the lingual surfaces of the teeth, and then bonded using composite resin. Once composite resin adhesive is added, the retainer becomes more rigid and helps to splint the teeth together. It has the potential advantages of being easily adapted to the lingual surfaces of the teeth, biocompatible and aesthetic. Some operators worry that the increased rigidity of this type of retainer may make it more prone to failure as teeth move differentially in normal function.
C. Positioner
A positioner is an appliance that is used to improve the interdigitation of the teeth at the end of treatment. It is typically a single piece of plastic that has been created in the laboratory to guide a person's upper and lower teeth into the ideal position. Although it is really used to 'position' the teeth, it has been used to hold the teeth in position after it has completed its positioning role. The person usually wears it only at night for a defined period.
D. Adjunctive procedures to reduce relapse
Interproximal reduction
Also known as interproximal stripping, this is a process of reshaping the contacts between adjacent teeth to make them broader and flatter. It is hoped that this will make the teeth more stable and less likely to relapse. The reshaping can be undertaken with small abrasive strips that are placed between the teeth, either by hand or on a dental handpiece. It is usually not painful and no anaesthetic is required before, during or after. A minimal amount of enamel is removed.
Pericision
Also known as circumferential supracrestal fiberotomy, this is a process where the fibres around the neck of the teeth are cut to reduce the chances of relapse. These can be cut with a sharp blade under local anaesthetic.
E. Additional terms used in this retention review
Little's Irregularity Index (LII)
This is an index described by a UK orthodontist called Bob Little (Little 1981). It is used to describe the irregularity of the anterior six teeth. The index measures the distance, in millimetres, between the contact points of crooked teeth, and then adds them together. Therefore, the Irregularity Index is the sum of all the displaced contacts between the anterior teeth (canine to canine).
Peer Assessment Rating (PAR)
This is an index used to provide an objective measurement of orthodontic treatment outcome. Described by Richmond 1992, it provides a score measuring any abnormalities in the occlusion ‐ the smaller the score, the better the quality of the result.
Settling
Sometimes referred to as 'occlusal settling', this is a process where the quality of the person's bite improves after orthodontic treatment, with more and better quality contacts between opposing teeth. Retainers are sometimes designed or prescribed to try and improve settling after treatment. This means that they encourage a subtle change (rather than holding teeth exactly still) to improve the result at the end of treatment. It is really a controlled way of allowing teeth to move together after treatment, and in fact involves a deliberate reduction in stability to improve the final result.
Appendix 2. MEDLINE (Ovid) search strategy
1. exp ORTHODONTICS/ 2. orthodontic$.mp. 3. or/1‐2 4. (retention or retain$).mp. 5. (stabilise$ or stabilize$).mp. 6. (fraenectom$ or frenectom$).mp. 7. (fiberotom$ or fibreotom$).mp. 8. "interproximal stripping".mp. 9. pericision.mp. 10. reproximat$.mp. 11. ((gingiv$ or periodont$) adj4 surg$).mp. 12. (retain or retention).mp. 13. 11 and 12 14. or/4‐10 15. 13 or 14 16. 3 and 15
The above subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of The Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 3. The Cochrane Oral Health Group Trials Register search strategy
From January 2013, searches of the Cochrane Oral Health Group Trials Register used the Cochrane Register of Studies and the search strategy below:
#1 (orthodontic*) AND (INREGISTER) #2 ((retention or retain* or relaps* or fraenectom* or frenectom* or fiberotom* or fibreotom* or "interproximal stripping" or pericision or reproximation)) AND (INREGISTER) #3 (#1 AND #2) AND (INREGISTER)
We undertook a previous search of the Oral Health Group Trials Register in February 2012 using the Procite software and the search strategy below:
(orthodontic* and (retention or retainer* or relapse* or "duration of retention" OR (retention and ((gingiv* or periodont*) and surg*)) or fraenectom* or frenectom* or fiberotom* or fibreotom* or "interproximal stripping" or pericision or reproximation)
Appendix 4. The Cochrane Central Register of Controlled Clinical Trials (CENTRAL) search strategy
#1 ORTHODONTICS explode all trees #2 orthodontic* #3 (#1 or #2) #4 (retention or retain*) #5 (stabilis* or stabiliz*) #6 (fraenectom* or frenectom*) #7 (fiberotom* or fibreotom*) #8 (interproximal next strip*) #9 pericision #10 reproximat* #11((gingiv* near surg*) or (periodont* near surg*)) #12 (retain* or retention) #13 (#11 and #12) #14 (#4 or #5 or #6 or #7 or #8 or #9 or #10) #15 (#13 or #14) #16 (#3 and #15)
Appendix 5. EMBASE (Ovid) search strategy
1. exp ORTHODONTICS/ 2. orthodontic$.mp. 3. or/1‐2 4. (retention or retain$).mp. 5. (stabilise$ or stabilize$).mp. 6. (fraenectom$ or frenectom$).mp. 7. (fiberotom$ or fibreotom$).mp. 8. "interproximal stripping".mp. 9. pericision.mp. 10. reproximat$.mp. 11. ((gingiv$ or periodont$) adj4 surg$).mp. 12. (retain or retention).mp. 13. 11 and 12 14. or/4‐10 15. 13 or 14 16. 3 and 15
The above subject search was linked to the Cochrane Oral Health Group filter for identifying randomised controlled trials in EMBASE via Ovid:
1. random$.ti,ab. 2. factorial$.ti,ab. 3. (crossover$ or cross over$ or cross‐over$).ti,ab. 4. placebo$.ti,ab. 5. (doubl$ adj blind$).ti,ab. 6. (singl$ adj blind$).ti,ab. 7. assign$.ti,ab. 8. allocat$.ti,ab. 9. volunteer$.ti,ab. 10. CROSSOVER PROCEDURE.sh. 11. DOUBLE‐BLIND PROCEDURE.sh. 12. RANDOMIZED CONTROLLED TRIAL.sh. 13. SINGLE BLIND PROCEDURE.sh. 14. or/1‐13 15. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 16. 14 NOT 15
Appendix 6. The US National Institutes of Health Trials Register (ClinicalTrials.gov) and the WHO International Clinical Trials Registry Platform search strategy
orthodontic and retain orthodontic and retention
Data and analyses
Comparison 1. Removable versus fixed retainers.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Stability ‐ Little's Irregularity Index | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Removable thermoplastic vs. fixed multistrand (lower) | 1 | 84 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.17, 1.03] |
| 2 Failure of retainers in lower | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Removable vs. thick plain canine to canine | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Removable vs. thick spiral canine to canine | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Removable vs. thin spiral wire (incisors and canines) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Removable thermoplastic vs. fixed multistrand (lower) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Adverse effects on health: evidence of caries | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Removable thermoplastic vs. fixed multistrand (lower) | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Adverse effects on health: evidence of gingival bleeding | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Removable thermoplastic vs. fixed multistrand (lower) | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.31, 0.88] |
| 5 Adverse effects on health: evidence of periodontal pocketing | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Removable thermoplastic vs. fixed multistrand (lower) | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.12, 0.87] |
| 6 Patient satisfaction: how acceptable was the retainer to wear? | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Removable thermoplastic vs. fixed multistrand (lower) | 1 | 81 | Mean Difference (IV, Fixed, 95% CI) | ‐12.84 [‐18.60, ‐7.09] |
| 7 Patient satisfaction: how easy was retainer to keep clean? | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Removable thermoplastic vs. fixed multistrand (lower) | 1 | 81 | Mean Difference (IV, Fixed, 95% CI) | ‐10.31 [‐20.05, ‐0.58] |
| 8 Patient satisfaction: how happy are you with appearance of teeth after 1 year of retention | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Removable thermoplastic vs. fixed multistrand (lower) | 1 | 81 | Mean Difference (IV, Fixed, 95% CI) | 1.5 [‐3.50, 6.50] |
Comparison 2. Fixed versus fixed retainers.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Failure of retainers | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Thick plain wire canine to canine vs. thick spiral wire canine to canine in lower | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.04, 2.27] |
| 1.2 Thick plain wire canine to canine vs. thin spiral wire (incisors and canines) in lower | 1 | 22 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 2.73] |
| 1.3 Thick spiral wire canine to canine vs. thin spiral wire (incisors and canines) in lower | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.32, 3.99] |
| 1.4 Maxillary polyethylene ribbon bonded retainer vs. maxillary multistrand bonded retainer | 2 | 174 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.87, 1.78] |
| 1.5 Mandibular polyethylene ribbon bonded retainer vs. mandibular multistrand retainer | 3 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.77, 1.57] |
Comparison 3. Removable versus removable retainers.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Stability ‐ Little's Irregularity Index ‐ upper labial segment ‐ 1 year | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Night wear Hawley 1 year vs. 24/7 for 6 months + night wear 6 months Hawley | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.41, 0.41] |
| 1.2 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 week then night wear | 1 | 310 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [0.08, 0.42] |
| 1.3 Part‐time 8/7 thermoplastic vs. full‐time 24/7 thermoplastic | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.39, 0.45] |
| 2 Stability ‐ Little's Irregularity Index ‐ lower labial segment ‐ 1 year | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Night wear Hawley 1 year vs. 24/7 for 6 months + night wear 6 months | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.28, 0.68] |
| 2.2 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 week then night wear | 1 | 310 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [0.23, 0.61] |
| 2.3 Upper and lower (mean) Begg full time vs. upper and lower (mean) thermoplastic retainers full time | 1 | 224 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [0.19, 0.31] |
| 2.4 Part‐time 8/7 thermoplastic vs. full‐time 24/7 thermoplastic | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.34, 0.38] |
| 3 Stability ‐ crowding upper labial segment ‐ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Night wear Hawley 1 year vs. 24/7 for 6 months + night wear 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Stability ‐ crowding lower labial segment ‐ 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Night wear Hawley 1 year vs. 24/7 for 6 months + night wear 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Stability: lower intercanine width | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 month | 1 | 310 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [0.01, 0.15] |
| 5.2 Part‐time 8/7 thermoplastic vs. full‐time 24/7 thermoplastic | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.22, 0.32] |
| 6 Stability: lower intermolar width | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 month | 1 | 310 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.01, 0.17] |
| 6.2 Part‐time 8/7 thermoplastic vs. full‐time 24/7 thermoplastic | 1 | 56 | Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.59, 0.38] |
| 7 Stability: upper intercanine width | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 month | 1 | 310 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.04, 0.14] |
| 7.2 Part‐time 8/7 thermoplastic vs. full‐time 24/7 thermoplastic | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | ‐0.00 [‐0.31, 0.30] |
| 8 Stability: upper intermolar width | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 month | 1 | 310 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.12, 0.08] |
| 8.2 Part‐time 8/7 thermoplastic vs. full‐time 24/7 thermoplastic | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.67, 0.92] |
| 9 Stability: overjet | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Part‐time 8/7 thermoplastic vs. full‐time 24/7 thermoplastic | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.06 [‐0.35, 0.48] |
| 10 Stability: overbite | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Part‐time 8/7 thermoplastic vs. full‐time 24/7 thermoplastic | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.34 [‐0.01, 0.69] |
| 11 Stability: settling with increased posterior contacts | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Modified thermoplastic retainer vs. full coverage thermoplastic retainer (both 6/12 full‐time) | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐0.34 [‐1.40, 0.72] |
| 11.2 Modified thermoplastic retainer vs. full coverage thermoplastic retainer (both 6/12 full‐time then 3/12 part‐time) | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 0.95 [0.05, 1.85] |
| 12 Stability: settling with increased anterior contacts | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Modified thermoplastic retainer vs. full coverage thermoplastic retainer (both 6/12 full‐time) | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐1.89 [‐2.32, ‐1.46] |
| 12.2 Modified thermoplastic retainer vs. full coverage thermoplastic retainer (both 6/12 full‐time then 3/12 nights only) | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐1.94, ‐1.06] |
| 13 Stability: maintaining corrected rotations in the upper | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Hawley full‐time for 3/12 then nights only vs. thermoplastic part‐time | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.88 [1.13, 21.07] |
| 14 Stability: maintaining quality of finish (PAR) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 15 Survival of retainers: how many broke in total | 1 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.96 [1.58, 5.55] |
| 15.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 week then night wear | 1 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.96 [1.58, 5.55] |
| 16 Survival of retainers: how many were lost in total | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 week then night wear | 1 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.56, 2.56] |
| 17 Survival of retainers: upper | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 Hawley 24/7 for 1 year vs. vacuum formed 24/7 for 1 year | 1 | 111 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.63, 1.19] |
| 18 Survival of retainers: lower | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 Hawley 24/7 for 1 year vs. thermoplastic 24/7 for 1 year | 1 | 111 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.43, 0.83] |
| 19 Patient satisfaction: able to wear retainer as instructed? | 1 | 347 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.83, 0.96] |
| 19.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 week then night wear | 1 | 347 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.83, 0.96] |
| 20 Patient satisfaction: able to wear retainers away from home? | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 week | 1 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.81, 1.06] |
| 21 Patient satisfaction: embarrassed to wear retainer? | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 21.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 week | 1 | 348 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.42 [1.30, 4.49] |
| 22 Patient satisfaction: amount of discomfort ‐ never or only on occasion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 22.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 week then night wear | 1 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.89, 1.03] |
| 23 Patient satisfaction: worse or much worse than wearing fixed appliances? | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 23.1 Hawley 24/7 for 3 months then 12/7 vs. thermoplastic 12/7 for 1 week | 1 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.37 [3.80, 23.10] |
Comparison 4. Upper removable and lower fixed retainer versus upper removable and lower adjunctive procedure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Irregularity change of upper labial segment (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Irregularity change in upper labial segment after 1 year | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.45, 0.65] |
| 1.2 Irregularity change of upper labial segment after 2 years | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.4 [‐0.95, 0.15] |
| 2 Intercanine change in upper (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Intercanine width in the upper after 1 year | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.26, 0.46] |
| 2.2 Intercanine width change in upper after 2 years | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.39, 0.59] |
| 3 Intermolar width change in upper (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Intermolar change in upper after 1 year | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.77, 0.77] |
| 3.2 Intermolar width change after 2 years | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.90, 0.70] |
| 4 Arch length change in upper (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Arch length change after 1 year | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.26, 0.66] |
| 4.2 Arch length change after 2 years | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.2 [‐0.29, 0.69] |
| 5 Irregularity change in lower labial segment (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Irregularity change in lower after 1 year | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.62, 0.22] |
| 5.2 Irregularity in lower after 2 years | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.73, 0.13] |
| 6 Intercanine width change in lower (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Intercanine width change in lower after 1 year | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐1.0 [‐1.22, ‐0.78] |
| 6.2 Intercanine width change in lower after 2 year | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.8 [‐1.26, ‐0.34] |
| 7 Intermolar width change in the lower (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Intermolar width change in lower after 1 year | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐0.6 [‐1.43, 0.23] |
| 7.2 Intermolar width change in lower after 2 years | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.7 [‐1.68, 0.28] |
| 8 Arch length change in lower (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Arch length change in lower after 1 year | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.7 [0.20, 1.20] |
| 8.2 Arch length change in lower after 2 years | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.27, 0.87] |
| 9 Overjet change (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Overjet change after 1 year | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐0.3 [‐0.83, 0.23] |
| 9.2 Overjet change after 2 years | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.2 [‐0.83, 0.43] |
| 10 Overbite change (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Overbite change after 1 year | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.57, 0.57] |
| 10.2 Overbite change after 2 years | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.57, 0.57] |
| 11 Final irregularity in upper after more than 5 years (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12 Final irregularity in lower after more than 5 years (V‐CTC vs. V‐S) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
Comparison 5. Upper removable retainer and lower fixed retainer versus positioner.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Irregularity change in upper labial segment (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Irregularity change in upper labial segment after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.83, 0.43] |
| 1.2 Irregularity change in upper labial segment after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐1.27, 0.07] |
| 2 Intercanine width change in upper (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Intercanine width change in upper after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.92, 0.12] |
| 2.2 Intercanine width change in upper after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐0.8 [‐1.50, ‐0.10] |
| 3 Intermolar width change in upper (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Intermolar width change in upper after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.00, 0.60] |
| 3.2 Intermolar width change in upper after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐1.08, 0.48] |
| 4 Arch length change in upper (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Arch length change in upper after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐1.11, 1.11] |
| 4.2 Arch length change in upper after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐0.1 [‐1.30, 1.10] |
| 5 Irregularity change in lower labial segment (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Irregularity change in lower after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.5 [‐1.01, 0.01] |
| 5.2 Irregularity change in lower after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐1.0 [‐1.65, ‐0.35] |
| 6 Intercanine width change in lower (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Intercanine width change in lower after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.7 [‐1.14, ‐0.26] |
| 6.2 Intercanine width change in lower after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐0.8 [‐1.34, ‐0.26] |
| 7 Intermolar width change in lower (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Intermolar width change in lower after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.8 [‐1.65, 0.05] |
| 7.2 Intermolar width change in lower after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐1.0 [‐1.93, ‐0.07] |
| 8 Arch length change in lower (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Arch length change in lower after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.31, 0.71] |
| 8.2 Arch length change in lower after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 0.4 [‐0.15, 0.95] |
| 9 Overjet change (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Overjet change after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.3 [‐0.81, 0.21] |
| 9.2 Overjet change after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.71, 0.51] |
| 10 Overbite change (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Overbite change after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.2 [‐0.32, 0.72] |
| 10.2 Overbite change after 2 years | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 0.2 [‐0.50, 0.90] |
| 11 Final irregularity in upper after more than 5 years (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12 Final irregularity in lower after more than 5 years (V‐CTC vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
Comparison 6. Upper removable retainer and lower adjunctive procedure versus positioner (P).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Irregularity change in upper labial segment (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Irregularity change in upper labial segment after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.93, 0.33] |
| 1.2 Irregularity change in upper labial segment after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.94, 0.54] |
| 2 Intercanine width change in upper (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Intercanine width change in upper after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐1.01, 1.01] |
| 2.2 Intercanine width change in upper after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐0.9 [‐1.63, ‐0.17] |
| 3 Intermolar width change in upper (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Intermolar width change in upper after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.80, 0.40] |
| 3.2 Intermolar width change in upper after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.93, 0.53] |
| 4 Arch length change in upper (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Arch length change in upper after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.23, 0.83] |
| 4.2 Arch length change in upper after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 0.1 [‐1.06, 1.26] |
| 5 Irregularity change in lower labial segment (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Irregularity change in lower labial segment after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.84, 0.24] |
| 5.2 Irregularity change in lower labial segment after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐1.37, ‐0.03] |
| 6 Intercanine width change in lower (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Intercanine width change in lower after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.7 [‐1.14, ‐0.26] |
| 6.2 Intercanine width change in lower after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.75, 0.55] |
| 7 Intermolar width change in lower (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Intermolar width change in lower after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.22, 0.82] |
| 7.2 Intermolar width change in lower after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 0.1 [‐0.40, 0.60] |
| 8 Arch length change in lower (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Arch length change in lower after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.5 [‐0.95, ‐0.05] |
| 8.2 Arch length change in lower after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 0.1 [‐0.40, 0.60] |
| 9 Overjet change (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Overjet change after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.54, 0.54] |
| 9.2 Overjet change after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.51, 0.71] |
| 10 Overbite change (V‐S vs. P) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Overbite change after 1 year | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.49, 0.49] |
| 10.2 Overbite change after 2 years | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 0.2 [‐0.46, 0.86] |
| 11 Final irregularity in upper after more than 5 years (V‐S vs. P) | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.87, 1.47] |
| 12 Final irregularity in lower after more than 5 years (V‐S vs. P) | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | ‐1.4 [‐2.77, ‐0.03] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aslan 2013.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 36 (29 females and 7 males) Mean (± SD) age: 16.9 ± 1.70 years in modified thermoplastic retainer group and 17.30 ± 1.5 years in full‐coverage Essix group Inclusion criteria: people who had completed full fixed appliance treatment lasting at least 15 months, with Class I molar and canine relationships in a university clinic. Exclusion criteria:
Setting: university clinic in Department of Orthodontics, Gazi University, Turkey |
|
| Interventions |
Comparison: modified thermoplastic ("Essix") retainers vs. full coverage thermoplastic ("Essix") retainer Group 1: the modified thermoplastic retainers were 0.060 inches thick had full coverage on the anterior teeth, but were cut away over the premolars and molars to open up the occlusal and half of the lingual and buccal surfaces of the posterior teeth. These retainers were strengthened by a 0.7 mm stainless steel round wire passing distal to the second molars and extending on the lingual surface of the appliance. Small amounts of cold cure acrylic were also added on the anterior and posterior lingual regions of the retainers if required Group 2: the full coverage thermoplastic retainers were 0.030 inches thick and covered all the teeth They also compared these 2 groups to a "normal group", but these were not randomised and will not be considered further here Both groups wore their retainers full time for 6 months then nights only for 3 months |
|
| Outcomes |
Outcome relevant to review: stability Stability assessed by the degree of "settling" of the occlusion. This referred to the vertical movement of teeth after treatment was complete to increase the number of contacts between the opposing teeth Occlusal records taken to record the number and quality of occlusal contacts at 3 time points: within 2 hours of removal of orthodontic appliances, after 6 months and after 9 months |
|
| Notes | No declarations of interest or funding sources declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Selected by picking interventions from a hat (confirmed by personal email correspondence) |
| Allocation concealment (selection bias) | Low risk | Selected by picking interventions from a hat (confirmed by personal email correspondence) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Assessment undertaken at the time of taking the bite record, at which point the operator would be aware of intervention group |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Large drop‐out (28%) not accounted for |
| Selective reporting (reporting bias) | Low risk | No registration on clinical trials registers so not possible to confirm whether other outcomes were recorded and not reported here, but authors confirmed no other outcomes to be reported |
| Other bias | High risk | As well as trying to compare the total number of occlusal contacts, the authors tried to identify the quality of occlusal contacts. However, they did this by comparing to a group of 18 participants with "Class I normal occlusion" who had not had orthodontic treatment. This group may not represent the ideal |
Bolla 2012.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 85 (56 females and 29 males) Mean age: 21.9 years Inclusion criteria: people who had been treated with fixed appliances, with:
Exclusion criteria:
Setting: university clinic in Italy and participants had to pay for treatment (information provided by authors) |
|
| Interventions |
Comparison: polyethylene ribbon retainer vs. multistrand retainer Group 1: polyethylene ribbon retainer were silanised, 14 µm, unidirectional, glass fibre devices embedded in a resin matrix Group 2: multistrand retainer were 0.0175" dead‐soft passive multistrand wire Both types were bonded lateral incisor to lateral incisor in upper, and canine to canine in the lower All were placed under rubber dam using a standardised bonding process |
|
| Outcomes |
Outcome relevant to review: survival of retainers Number of detachments or bond failures recorded after 6 years |
|
| Notes | No measures of patient satisfaction, effect on health or stability were recorded | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Contacted authors who confirmed, "the operator tossed a coin for every patient" after agreeing to be in the study |
| Allocation concealment (selection bias) | Low risk | Contacted authors who confirmed, "the operator tossed a coin for every patient" after agreeing to be in the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not feasible as the outcome assessor could not be blinded to the presence or absence of the wire |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Paper recorded no drop‐outs, but on contacting the authors reported that, "we described only the patients that completed the trial, we estimate, now, we had a drop out of 15‐20 per group" |
| Selective reporting (reporting bias) | High risk | Contacted authors who reported, "we started to check the periodontium, but it was making the visit too long for the administration therefore we had to terminate that evaluation" They also started "evaluating the bacterial flora taking a sample every 3 months, unfortunately we ran out of funds" |
| Other bias | Low risk | No other areas of risk of bias identified |
Edman Tynelius 2015.
| Methods | 3‐arm parallel randomised controlled clinical trial | |
| Participants |
Numbers recruited: 75, 25 in each group (45 females and 30 males) Mean (± SD) age: Group 1 14.1 ± 1.3 years, Group 2 14.7 ± 1.8 years and Group 3 14.3 ± 1.5 years Inclusion criteria: People who had completed upper and lower fixed appliances, with:
Exclusion criteria: no additional criteria specified Setting: NHS clinic in Sweden |
|
| Interventions |
Comparison: upper thermoplastic retainer and a lower bonded retainer vs. upper thermoplastic retainer and lower interproximal stripping and no lower retainer vs. prefabricated positioner Group 1: upper thermoplastic (vacuum‐formed) retainer and a 0.7 mm stainless steel‐bonded retainer bonded to the lower canines only (V‐CTC). Vacuum‐formed retainers were worn 22‐24 hours for the first 2 days and then nights only after this. The bonded retainer was 0.7 mm stainless steel and bonded to the lingual of the canines only Group 2: upper thermoplastic (vacuum‐formed) retainer with interproximal stripping of the lower anterior teeth, but no mandibular retainer (V‐S). Vacuum‐formed retainers were worn 22‐24 hours for the first 2 days and then nights only after this. Interproximal stripping was undertaken 5‐6 weeks before debond and at debond Group 3: prefabricated positioner covering all the maxillary and mandibular teeth (P). Positioner was worn 30 minutes during the day (and participant was encouraged to bite into it) and also during sleep. It was a soft plastic device covering all teeth In the second year of retention, participants wore their removable retainers every other night After 2 years, all retainers were stopped and bonded retainers removed |
|
| Outcomes |
Outcome relevant to review: stability Stability data collected after 1 year Based on Little's Irregularity Index in the upper and lower labial segments, intercanine width, intermolar width, arch length, overjet and overbite Outcomes reported at 1, 2 and 5 years post debond. Change data available for years 1 and 2. Final Little's Irregularity data only in both arches were available for 5 years post‐debond |
|
| Notes | No measurement of survival of retainers, adverse effects on health or patient satisfaction However, it was reported that 2 participants did not comply with the positioner. On contact with the author, the failure rates for the bonded retainers after 1 years were: 18 participants had no failures, 5 had 1 failure, 1 had 2 failures and 1 had 4 failures Also reported the cost‐effectiveness of the outcomes, but they were not relevant to this review |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The generation of randomisation sequence was performed in blocks of five to ensure that equal numbers of patients were allocated to each of the three retention groups". The author confirmed appropriate random number generation |
| Allocation concealment (selection bias) | Low risk | Direct communication with the author confirmed that they used adequate concealment, and neither the participant nor clinician could have known of the intervention to be used in advance. This was done by placing ballots in a hat by an independent observer, so that the clinician could not know what intervention was going to be drawn out |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Paper reported that the outcome assessor was blinded to the retention protocol |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Drop‐outs clearly reported and not included in the final analysis |
| Selective reporting (reporting bias) | Low risk | All the data were reported over the 5‐year study period |
| Other bias | Low risk | No other areas of bias identified |
Gill 2007.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 60 (authors reported gender of participants who completed the study: 32 females and 25 males) Mean (± SD) age: Group 1: 13.72 ± 2.5 years, Group 2: 13.37 ± 1.42 years Inclusion criteria:
Exclusion criteria:
Setting: hospital department in the UK, participants treated free of charge |
|
| Interventions |
Comparison: part‐time wear of upper and lower thermoplastic (vacuum‐formed) retainer vs. upper and lower full‐time wear of thermoplastic (vacuum‐formed) retainer Group 1: part‐time wear of vacuum‐formed retainers (sleeping hours with minimum of 8 hours of wear) Group 2: full‐time wear of vacuum‐formed retainers The vacuum‐formed retainers were full‐arch coverage and made from 1 mm thick polycarbonate sheets |
|
| Outcomes |
Outcome relevant to review: stability Stability assessed using Little's Irregularity Index, intercanine width and intermolar width in both arches, and overjet and overbite. PAR index reported in a graph, but data not sufficiently clear for further analysis Outcomes were measured after 6 months |
|
| Notes | Authors reported the type of initial malocclusion, whether the participants were treated by extraction or non‐extraction and the time in treatment. Despite randomisation, there were more Class II participants in the part‐time group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The authors confirmed the randomisation was generated by rolling a die and allocating the group according to odd or even numbers |
| Allocation concealment (selection bias) | Low risk | "Identical opaque sealed envelopes containing a slip for group allocations were used for the purpose of random allocation" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor was blind to the treatment group |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss of follow‐up data were reported in Consort diagram. Effect was not analysed, but as drop‐out was low, it is unlikely to have a significant effect |
| Selective reporting (reporting bias) | Low risk | Authors confirmed they did not collect any other outcomes and there was no selective reporting |
| Other bias | Low risk | No areas of risk of bias were identified |
Kumar 2011.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 224 (gender split not reported) Mean age: not reported Inclusion criteria: people who had pre‐adjusted edgewise appliance in each arch and:
Exclusion criteria: none reported Setting: university clinic in Department of Orthodontics & Dentofacial Orthopedics, College of Dental Science, Davangere, Karnataka, India |
|
| Interventions |
Comparison: upper and lower Begg retainers vs. upper and lower thermoplastic retainers Group 1: upper and lower Begg retainers. Acrylic baseplates with labial bow of 0.9 mm stainless steel wire. Labial bow had U‐loops opposite the premolars and extended past the last erupted molars Group 2: upper and lower thermoplastic (vacuum‐formed) ‐ Essix A+, (Raintree Essix, New Orleans, USA) retainers All participants had bonded wire placed in the lower as well The participants were instructed to wear them 24 hours per day for 6 months (and then 12 hours per day for the following 6 months ‐ although the 1‐year data were not reported). They were instructed to eat with the retainers in place and remove after eating for cleaning |
|
| Outcomes |
Outcomes relevant to review: stability and patient satisfaction Stability assessed using PAR and Little's Irregularity Index. The results for the lower irregularity were reported, but not the upper Participant satisfaction data included the mean, but no standard deviations, so the data could not be analysed using the Review Manager 5 software (RevMan 2014). We contacted the authors to see if they could provide the raw data to allow analysis, but received no reply. Relapse was assessed at 2 time points after debond: 3 and 6 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported ‐ authors contacted about this but no reply received |
| Allocation concealment (selection bias) | Unclear risk | Not reported ‐ authors contacted about this but no reply received |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported ‐ authors contacted about this but no reply received |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported ‐ authors contacted about this but no reply received |
| Selective reporting (reporting bias) | High risk | Results of irregularity reported in the lower, but not the upper arch |
| Other bias | Unclear risk | Insufficient data in the paper to determine this. Authors contacted but no reply received |
Millett 2007.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 85 (46 females and 39 males) Mean age: not reported Inclusion criteria: all participants had undergone fixed appliance treatment in at least the lower arch with satisfactory alignment and:
Exclusion criteria:
Setting: hospital department in Cork, Republic of Ireland |
|
| Interventions | Comparison: lower bonded retainer vs. lower vacuum‐formed retainer Group 1: bonded retainer was 0.018" stainless steel multistrand wire bonded to lingual of all lower incisors and canines Group 2: vacuum‐formed retainer was full‐occlusal coverage worn on a nights only basis from the day it was fitted In the upper arch, the clinician chose the upper retainer (Hawley or vacuum‐formed) |
|
| Outcomes |
Outcomes relevant to review: stability, survival of retainers, adverse effects on health and participant satisfaction Stability assessed by Little's Irregularity Index. The initial protocol discussed the use of PAR index, but these data were not collected Survival of retainers ‐ vacuum‐formed retainers were assessed as failed if they fractured or were lost (but not worn); bonded retainers were assessed as failed if debonded (clarified this with the authors) Adverse effects on health ‐ caries (evidence of decalcification) and periodontal health (gingival bleeding and periodontal probing > 3 mm) was assessed for lower anterior teeth Participant satisfaction ‐ participant questionnaire assessing retainer wear and acceptability recorded. Data for both retainers available for the following questions:
Outcomes collected 1 year after debond |
|
| Notes | Additional outcome was operator perception of each retainer type ‐ this will not be reported here, as this is not part of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Authors confirmed computer‐generated random sequence |
| Allocation concealment (selection bias) | Low risk | Sealed consecutive opaque envelopes in a separate co‐ordinating centre |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Contact with the author confirmed the assessor was blinded for the intervention type |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Drop‐outs were reported. Authors confirmed the data was analysed on an intention‐to‐treat basis |
| Selective reporting (reporting bias) | High risk | Not all outcomes were reported in the abstracts that had been described in the protocol (PAR index for occlusal change was not collected). Further data will be reported after 2 years of wear |
| Other bias | Unclear risk | As this study was only available as research abstracts, it is unclear as to whether other bias exists |
O'Rourke [pers comm].
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 82 (59 females and 23 males) Mean (± SD) age: 17.73 ± 3.52 years Inclusion criteria: people who had completed treatment with 0.022 x 0.028" pre‐adjusted Edgewise fixed appliances with:
Exclusion criteria:
Setting: NHS hospital orthodontic department in London, UK |
|
| Interventions |
Comparison: thermoplastic retainer vs. bonded retainer in lower arch Group 1: vacuum‐formed retainer (Essix ACE 0.030") in lower arch fitted within 7 days of debond. To wear full‐time for 6 months then nights only every night, then for 6 months of alternate nights Group 2: bonded retainer canine to canine 0.0175" co‐axial stainless steel bonded to every tooth passively with Transbond LR |
|
| Outcomes |
Outcome relevant to review: stability Stability assessed after 18 months by measuring: Little's Irregularity Index, intercanine width, intermolar width, arch length, extraction site space opening |
|
| Notes | Data were non‐parametric so could not be entered into Review Manager 5 to be included in a future meta‐analysis. Results presented as a Table 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used electronic randomisation programme generating a random allocation sequence |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed in blackout envelopes that were identical, tamper evident and prepared in advance |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Models measured in random order and blinded for data analysis |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Operators used an intention‐to‐treat analysis. The authors reported that any participants who failed to attend their appointments were analysed in their original group. Imputation values were used in case of missing data, calculated as the mean of the outcome being measured. The authors acknowledged that due to a higher number of drop‐outs at 18 months, the use of imputation may give increased uncertainty to the results |
| Selective reporting (reporting bias) | Low risk | No registration on clinical trials registers, but authors confirmed there were no other data to report (apart from cost‐effectiveness data, which is not relevant to this review) |
| Other bias | Low risk | No other potential areas of bias identified |
Rohaya 2006.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 218 (gender split not reported) These figures differed from the published paper and were provided by the author Mean age: not reported Inclusion criteria: participants received upper fixed appliance treatment (and sometimes lower fixed in addition). They may have also had an initial stage of functional appliance and possibly extractions. In addition, the participants were prepared to wear either a Hawley or a vacuum‐formed retainer Exclusion criteria:
Setting: District General Hospital in the UK, treatment free of charge |
|
| Interventions |
Comparison: upper Hawley retainer vs. upper thermoplastic (vacuum‐formed) retainer Group 1: upper Hawley retainer full‐time for 3 months then 6 months of nights only (9 months in total) Group 2: upper vacuum‐formed retainer (Essix C, Raintree Essix) full‐time for 1 week then evenings and nights for 3 months, then nights only for 6 months (9 months in total) |
|
| Outcomes |
Outcome relevant to review: stability Stability assessed only in relation to previously rotated upper teeth (upper incisors, canines and premolars) Only participants with ≥ 1 rotated teeth included in the analysis Outcome assessed after 1 year |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Authors contacted and confirmed that this was undertaken appropriately. Computer programme used to produce randomisation and then placed in numbered sealed envelopes prepared in advance by someone else |
| Allocation concealment (selection bias) | Low risk | Authors contacted and confirmed that this was undertaken appropriately. Computer programme used to produce randomisation and then placed in numbered sealed envelopes prepared in advance by someone else |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Authors contacted and reported about participant blinding, "A separate person assessed the models without knowing which retainer had been worn. The models were randomised and only identifiable by a number, the code was broken only after all models had been measured and the results were then linked to the retainer groups for statistical analysis" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The number of drop‐outs was very high (32% in Hawley group and 39% in vacuum‐formed retainer group) and these were not analysed or taken into account |
| Selective reporting (reporting bias) | High risk | Other outcomes collected but not reported. Authors contacted to request this information ‐ they reported that they are planning to publish this in the future |
| Other bias | Low risk | No other biases identified |
Rose 2002.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Number recruited: 20 (8 females and 12 males)
Mean (± SD) age: 22.4 ± 9.7 Inclusion criteria: people were previously identified as needing a lower bonded retainer by the orthodontist in charge of the clinic and the participants had:
Exclusion criteria: none reported Setting: university clinic, Department of Orthodontics, Freiburg University, Germany |
|
| Interventions |
Comparison: polyethylene ribbon retainer versus multistrand retainer Group 1: polyethylene ribbon retainer ('Ribbond') was cut to the correct length, pre‐treated with adhesive bis‐GMA sealant and the bonded with 'Heliosite' orthodontic composite resin Group 2: multistrand retainer was 0.0175" passive multistrand wire Both types were bonded to all teeth, canine to canine in the lower arch. The multistrand retainers were bonded under rubber dam |
|
| Outcomes |
Outcome relevant to review: survival of retainers Failure rates recorded over 2 years |
|
| Notes | Paper describes patient satisfaction with the retainer types, but no data presented on this | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Appropriate randomisation (confirmed with author ‐ used random number generation) |
| Allocation concealment (selection bias) | Low risk | Confirmed as appropriate after contact with author (randomisation was prepared independent to clinician so could not be aware of allocation) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Impossible to blind the assessor to outcomes in this study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no drop‐outs (confirmed with author) |
| Selective reporting (reporting bias) | High risk | Single outcome reported. Description of patient's satisfaction of retainer type, but no data reported |
| Other bias | Low risk | No other areas of bias identified |
Rowland 2007.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 397 (241 females and 156 males) Mean (± SD) age: Group 1: 14.8 years ± 1 year 8 months, and Group 2: 15 years ± 1 year 5 months Inclusion criteria: all participants had pre‐adjusted edgewise fixed appliances and:
Exclusion criteria:
Setting: NHS specialist practice in Bristol, UK, treatment free of charge by 1 operator |
|
| Interventions |
Comparison: upper and lower Hawley retainer vs. upper and lower vacuum‐formed retainers Group 1: upper and lower Hawley retainers, worn 3 months full‐time then 12 hours a day for 3 months Group 2: upper and lower vacuum‐formed retainers ‐ worn full‐time for 1 week then 12 hours a day. Full coverage design made from 1.5 mm 'Erkodur' blank Data collected after 6 months of retention |
|
| Outcomes |
Outcomes relevant to review: stability, patient satisfaction, survival of retainers Stability measured using: Little's Irregularity Index, intercanine width, intermolar width Authors reported that tooth rotations, overjet and overbite analysis were measured, but no data provided in the paper Patient satisfaction assessed by questionnaire. Results of the most relevant questions provided in the paper Survival of retainers ‐ the number of broken retainers recorded for each type of retainer Cost‐effectiveness reported, but this was not 1 of the outcomes for this review |
|
| Notes | Assessment of stability data provided as medians and interquartile ranges. This could not be analysed using Review Manager 5 statistical software, so we requested the raw data, which the authors provided. Helen Worthington (author of this review) then converted these into data that could be input into Review Manager 5 Patient satisfaction data were dichotomised for full analysis as follows:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used block randomisation (taken from "www.randomisation.com") |
| Allocation concealment (selection bias) | Low risk | Concealment done by ensuring randomisation was performed after consent was obtained, using the computer program www.randomisation.com, so the clinician and participant could not know what intervention would be generated |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor blinded to the type of retainer used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Number of drop‐outs clearly reported and described |
| Selective reporting (reporting bias) | High risk | Tooth rotations, overjet and overbite data measured but not reported. The authors also only reported the "most relevant" questions on the patient satisfaction questionnaire |
| Other bias | Low risk | Pre‐treatment equivalence shown for both groups and no other apparent bias present |
Salehi 2013.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 142 (83 females and 59 males) Mean (± SD) age: Group 1: 18.1 ± 5.23 years and Group 2: 18.2 ± 4.81 years Inclusion criteria: people treated with standard edgewise fixed appliances and:
Exclusion criteria:
Setting: clinic of 1 operator in Iran, participants paid for treatment |
|
| Interventions |
Comparison: polyethylene ribbon retainer vs. multistrand retainer Group 1: polyethylene ribbon retainer ('Ribbond') was cut to the correct length, pre‐treated with adhesive bis‐GMA sealant and the bonded with 'Heliosite' orthodontic composite resin Group 2: multistrand retainer was 0.0175" passive multistrand wire Both types were bonded to all teeth, canine to canine in the lower arch Both retainers bonded under rubber dam with Heliosite composite resin using Fluoro Bond adhesive bis‐GMA sealant |
|
| Outcomes |
Outcome relevant to review: survival of retainers Retainer assessed as failed if it debonded from tooth or fractured Survival reported using failure rates of retainers over 18 months |
|
| Notes | No assessment of stability, adverse effects on health or patient satisfaction | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random table number table used |
| Allocation concealment (selection bias) | Unclear risk | No concealment described. Authors contacted to clarify this, but no reply received |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Authors noted that the statistician analysing the data was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Drop‐outs clearly reported and not included in final analysis |
| Selective reporting (reporting bias) | Low risk | No evidence or suggestion of selective reporting |
| Other bias | Low risk | No other suggestions of bias noted |
Shawesh 2010.
| Methods | 2 arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 67 (45 females and 22 males) Mean (± SD) age: Group 1: 15.6 ± 1.6 years, and Group 2: 15.8 ± 1.2 years Inclusion criteria:
Exclusion criteria:
Setting: NHS specialist practice in Manchester, UK, treatment was free of charge |
|
| Interventions |
Comparison: part‐time Hawley retainers vs. full‐time Hawley retainers Group 1: part‐time wear of Hawley retainers for 1 year (retainers worn only at night) Group 2: full‐time wear for 6 months then nights only for 6 months |
|
| Outcomes |
Outcome of relevance to review: stability Stability assessed using Little's Irregularity Index and crowding assessment Outcome measured after 1 year |
|
| Notes | No patient satisfaction assessment, survival of retainers or assessment of effect on dental health | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Very clear description of appropriate randomisation process: "The subjects were randomly allocated to one of the two retention regimen groups using a restricted randomisation technique, in blocks of 12, to ensure equal numbers were allocated to each group. The allocation was decided by throwing an unweighted di where throws of 1, 2 or 3 = group 1 and 4, 5, or 6 = group 2. From this random list, the retention regime was recorded along side a patient identification number" |
| Allocation concealment (selection bias) | Low risk | After randomisation the allocation was "sealed in numbered opaque envelopes and held in a central place. Thus, neither the clinician nor the patient knew their group allocation prior to consenting to the study" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor was blinded to the retention regimen used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Drop‐outs clearly reported and not included in the final analysis |
| Selective reporting (reporting bias) | Low risk | No evidence or suggestion of selective reporting |
| Other bias | High risk | Authors warned that despite the appropriate use of randomisation there was not complete equivalence between groups at the start of treatment. The group with full‐time wear for the first 6 months had 1 mm more crowding and nearly 2 mm more irregularity at the start of treatment. The authors warned that the results should therefore be viewed with caution |
Sun 2011.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 120 (60 females and 60 males) Mean age: 14.7 years (range 12‐17 years) Inclusion criteria:
Exclusion criteria:
Setting: university clinic at West China Stomatology Hospital of Sichuan, China |
|
| Interventions |
Comparison: Hawley retainer vs. thermoplastic retainer Group 1: upper and lower Hawley retainers Group 2: upper and lower clear overlay (thermoplastic) retainers (0.75 mm thick Biolon, Dreve Dentamid GmbH, Unna, Germany) Participants were asked to wear both types of retainer full‐time except during meals. Reviewed at 3, 6 and 12 months and participants contacted if the retainer failed |
|
| Outcomes |
Outcome relevant to review: survival of retainers Survival of retainers assessed by how often they failed. Retainers could fail by fracture, "no longer fitting", local serious abrasion causing penetration and loss of retainers (reported by participant or observed at appointment) Final outcome at 1 year |
|
| Notes | Additional outcomes of effect on oral hygiene mentioned on the clinical trials record but not reported here | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random sequence. Researcher managing this did not participate in the enrolment procedure |
| Allocation concealment (selection bias) | Low risk | Both participant and researcher blinded to randomisation until after the participant had agreed to take part in the trial. The method of concealment not described, although authors reported that they concealed allocation to avoid selection bias and it was done by someone not involved in the enrolment procedure |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Impossible to blind the assessor to the type of retainer in this type of trial, as the assessor had to record the type of failure/breakage of the retainer, and would therefore see the different types of removable retainers |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up was small and these were reported and evenly distributed between each group (5 in the Hawley group and 4 in the clear overlay group) |
| Selective reporting (reporting bias) | High risk | The clinical trials record reported that oral hygiene was the primary outcome, not reported here, and that there were 3 groups ‐ we contacted the authors about this, but did not receive a reply |
| Other bias | Low risk | No other biases identified |
Thickett 2010.
| Methods | 2‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 62 (36 females and 26 males) Mean (± SD) age: Group 1: 13.6 ± 1.5 years and Group 2: 13.8 ± 1.5 years Inclusion criteria:
Exclusion criteria:
Setting: NHS hospital department in Bournemouth, UK, treatment was free of charge |
|
| Interventions |
Comparison: full‐time thermoplastic retainer wear vs. part‐time thermoplastic retainer wear Group 1: full‐time wear for 0‐3 months after debond, then 10 hours per day for 3‐6 months, then alternate nights for 6‐9 months after debond, then 1‐2 times a week for 9‐12 months after debond Group 2: part‐time wear (10 hours per day) for 0‐3 months after debond, then 10 hours per day for 3‐6 months, then alternate nights for 6‐9 months after debond, then 1‐2 times a week for 9‐12 months after debond Both groups had vacuum‐formed retainers made from Essix B material (GAC International, Bohemia, New York, USA) |
|
| Outcomes |
Outcome relevant to review: stability Stability assessed using Little's Irregularity Index, intercanine width, intermolar width, arch length, overjet, overbite, PAR (The authors mistakenly interchange the terms irregularity and crowding, when they mean irregularity) Data collected at 1 year |
|
| Notes | Data were non‐parametric so could not be entered into Review Manager 5 to be included in a future meta‐analysis. Results presented in Table 5 PAR results were not presented in a format that allowed analysis. We requested this from the authors, but they were not provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The paper stated that the participants were allocated by "random number generation" ‐ we contacted the authors and they clarified that this was done appropriately using random number generation |
| Allocation concealment (selection bias) | Low risk | Authors contacted, it was explained that an independent researcher randomised the participant to the intervention after consent was obtained |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Authors contacted, it was confirmed that the outcome assessor was blinded to the retainer type |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Number of drop‐outs reported, but no explanation given. Authors contacted and the drop‐outs were not included in the analysis. Authors confirmed that the drop‐outs were due to participants not attending review appointment |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Other bias | Low risk | There was non‐compliance with the retention regimen, but as this was a effectiveness rather than an efficacy study this is acceptable |
Årtun 1997.
| Methods | 4‐arm parallel randomised controlled trial | |
| Participants |
Numbers recruited: 49 (gender split not reported)
Mean age: not reported, age range 12‐55 years Inclusion criteria: treated with edgewise light‐wire fixed appliances by 2 orthodontists in 1 practice, variety of malocclusions Exclusion criteria: none reported Setting: specialist practice in Seattle, USA Stratified according to age (adult/adolescent), gender and gingival condition |
|
| Interventions |
Comparisons: thick plain stainless steel bonded retainer bonded only to lower canines vs. thick spiral wire bonded retainer bonded only to lower canine vs. thin flexible spiral wire bonded retainer bonded to lower anterior 6 teeth vs. lower removable retainer Group 1: thick, plain 0.032" stainless steel bonded retainer bonded to lower canines only Group 2: thick spiral 0.032" stainless steel spiral wire bonded retainer bonded only to lower canines Group 3: thin flexible 0.0205" stainless steel spiral wire bonded to all lower anterior 6 teeth Group 4: removable retainer. Exact design not described, but in a figure appeared to have acrylic covering the lower anterior 6 teeth, except the incisal edges and supported by metal framework both buccally and lingually. The exact extent of retainer not clear. The amount of wear not reported At time of placement of retainer all participants were taught correct oral hygiene procedures with toothbrush and floss. All retainers were in the lower arch only |
|
| Outcomes |
Outcomes relevant to review: stability, survival of retainers and adverse effects on health Stability was reported using Little's Irregularity Index. There was insufficient data to analyse for this review Survival of retainers was assessed by describing the number of bonded retainers that debonded and how many removable retainers were lost Adverse effects on health were reported in terms of effects on periodontal health and caries. However, the full data were not available, so statistical analysis was not possible on this particular outcome Outcomes assessed after 3 years |
|
| Notes | Contact from authors confirmed that no data were available in addition to those in the published paper. There was insufficient data in the paper to allow analysis of stability or adverse effects | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of randomisation given. Author contacted, but when he moved jobs, the data files for this study were deleted |
| Allocation concealment (selection bias) | Unclear risk | No description given of method of concealment. Author contacted, but when he moved jobs, the data files for this study were deleted |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description given of method of concealment. Author contacted, but when he moved jobs, the data files for this study were deleted |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This is not clear from the paper. Author contacted, but when he moved jobs, the data files for this study were deleted |
| Selective reporting (reporting bias) | High risk | There were data missing from a number of the outcomes. Author contacted, but when he moved jobs, the data files for this study were deleted |
| Other bias | Low risk | No other biases identified |
NHS: National Health Service; PAR: Peer Assessment Rating; SD: standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12612000670875 | Contacted author and insufficient participants were recruited, so study was abandoned |
| Ahrens 1981 | Follow‐up too short. Study only followed up changes for 30 days |
| Al‐Nimri 2009 | Allocation was not randomised (treatments were allocated alternately) |
| Arora 2014 | Lead author confirmed by email that the groups were allocated alternately (not by randomisation) |
| Atack 2007 | Retrospective review paper |
| Axelsson 1993 | Contact with authors confirmed study was retrospective |
| Barlin 2011 | Contact with authors confirmed study was retrospective |
| Basciftici 2007 | Allocation was not randomised |
| Bauer 2010 | Not a true randomised controlled trial. Based on a sample from a previous study based on 50 participants. In this study, they claimed to allocate randomly, but there were 28 participants in 1 group and 22 in the other group. This was done deliberately as the authors reported they wanted to "oversample" as they expected problems in the Perfector group |
| Bazargani 2012 | Described different methods of placing fixed retainers, not different types of retainers |
| Bock 2008 | Retrospective study |
| Carvalho 2006 | Participant had individual teeth treated for 8 weeks and then the retention was only for 8 weeks |
| Conway 2011 | Study compared different methods of attaching the same retainer ‐ so did not fit the review criteria |
| Edwards 1988 | Not a randomised controlled trial. Interventions were allocated alternately, so the sequence generation was not random, and there was no allocation concealment. Although the study had been an included study in a previous version of this review, we decided to remove quasi‐randomised trials from the inclusion criteria, to reduce the risk of bias. In addition, the study had substantial drop‐out, and the effects of the drop‐outs were not discussed or analysed. We decided that the lack of adequate sequence generation and allocation concealment produced a large risk of bias, so we excluded this study from the review |
| Haydar 1992 | Insufficient data available in paper to allow statistical analysis |
| Horton 2009 | Retention phase only followed up for 2 months (less than the required 3 months for this review) |
| ISRCTN22535947 | Correspondence with author confirmed insufficient participants attended for recall to allow analysis of data |
| ISRCTN26364810 | Personal correspondence with lead author confirmed the retention part of the study was never completed |
| ISRCTN56295329 | Study was a method of supervision of retainers, not comparison of different retention regimens |
| Jäderberg 2012 | We contacted the authors who explained that treatment groups were allocated "alternately" and not by randomisation |
| Larsson 1983 | Insufficient data to allow analysis according to statistician |
| Lindauer 1998 | Prospective, but non‐randomised study |
| Pandis 2007 | Retrospective study |
| Pandis 2013 | Excluded as study investigating different types of adhesive (not comparing different types of retainers) |
| Sauget 1997 | Not a randomised controlled trial. Interventions were allocated alternately, so the sequence generation was not random, and there was no allocation concealment. Although the study was included study in a previous version of this review, we decided to remove quasi‐randomised trials from the inclusion criteria, to reduce the risk of bias. We decided that the lack of adequate sequence generation and allocation concealment produced a large risk of bias, so we excluded this study from the review |
| Stormann 2002 | Insufficient data in the original publication. Contacted authors, who were unwilling to release any further data |
| Tacken 2010 | Allocation not randomised |
| Taner 2000 | Not a randomised controlled trial. After personal communication with the authors they confirmed that the participants were allocated alternately, not randomly. As the interventions were allocated alternately, the sequence generation was not random, and there was no allocation concealment. Although the study had been an included study in a previous version of this review, we decided to remove quasi‐randomised trials from the inclusion criteria, to reduce the risk of bias. We decided that the lack of adequate sequence generation and allocation concealment produced a large risk of bias, so we excluded this study from the review. |
| Vecere 1983 | Reviewed author's thesis, which confirmed that the study was retrospective |
Characteristics of studies awaiting assessment [ordered by study ID]
Choi 2010.
| Methods | RCT |
| Participants | 66 (23 male, 43 female; mean age of 23.42 +/‐ 10.19 years) |
| Interventions | Conventional wraparound retainer versus circumferential comfortable retainer |
| Outcomes | Distorted speech, gagging sensation and discomfort assessed by participant on VAS scale |
| Notes | Translation of full text needed |
Liu 2010.
| Methods | RCT |
| Participants | 66 |
| Interventions | Fiber‐reinforced composite versus multistrand stainless steel wire as fixed lingual retainer |
| Outcomes | Bleeding index, pocket depth, flexural modulus, maximum shear bond strength |
| Notes | Translation of full text needed |
Torkan 2014.
| Methods | RCT |
| Participants | 30 |
| Interventions | Fiber‐reinforced composite retainer versus a spiral wire retainer extended on the lingual surfaces of both maxillary and mandibular arches from canine to canine |
| Outcomes | Health of the periodontium assessed radiographically |
| Notes |
Xu 2011.
| Methods | RCT |
| Participants | 45 |
| Interventions | Vacuum‐formed retainers versus lingual fixed retainers combined with Hawley retainers |
| Outcomes | Overbite, overjet and calculus index scores; tooth rotation, intercanine and intermolar width, and Little's index of irregularity |
| Notes | Full text requested from author 27 January 2016 |
Characteristics of ongoing studies [ordered by study ID]
ChiCTR‐TRC‐07000055.
| Trial name or title | Hawley's retainer and transparent retainer for the oral cavity hygiene in orthodontic patients |
| Methods | Randomised parallel controlled trial |
| Participants | Males and females up to 25 years of age Inclusion criteria 1. Patients live in Chengdu and won't leave Chengdu in 2 years; 2. When the trial is over, periodontia is healthy by periodontal therapy (normal color and no bleeding with exploration); 3. Age requirement: the second molar erupted and occlused until 25 years old after the treatment is completed Exclusion criteria 1. Systemic factors: A systemic disease: Diabetes, AIDS, Osteoporosis, Leukemia B Hormone: puberty gingivitis, pregnant women C genetic disease: gingival fibromatosis D Drug history: diphenylhydantoin sodium, cyclosporine, nifedipine E Habit disturbance: odontoprisis, habit of biting stiff object, smoking, drinking wine, unilateral mastication, impropriate teeth brushing, buccal respiration; 2. Local factors: A severe periodontal disease B Local faulty restoration C Faulty designed artificial tooth D restoration of corona dentis E agomphiasis |
| Interventions | Group A: Hawley's retainer Group B: transparent retainer Group C: health control group with no intervention |
| Outcomes | Plaque index, gingival bleeding index, adhesion loss, dental calculus index |
| Starting date | Registered 2007 |
| Contact information | Wenli Lai, Yongchun Yu; jinyu198081@163.com |
| Notes | West China Stomatology Hospital, Chengdu |
ChiCTR‐TRC‐07000454.
| Trial name or title | The impact of the Hawley's removable retainer and clear overlay removable retainer on orthodontic patients' oral hygiene |
| Methods | Parallel RCT |
| Participants | Males and females up to 30 years of age Inclusion criteria 1. Patient is resident and impossible to leave in two years; 2. When ended active orthodontic treatment, patient will receive periodontal treatment until the periodontia recovery, the color of the gingival returned normal and the blood of periodontal (BOP) index is negative; 3. The age: the minimum age is a stage that patient's second molars have been erupted and have occlusion when ended active orthodontic treatment. The maximum age is 30 years old Exclusion criteria 1. Whole body factors 1) Systematic diseases: Diabetes, AIDS, Osteoporosis, Leukemia; 2) Sex Hormone: pubertal gingivitis, gestational period gingivitis; 3) Genetic factor: gingival fibromatosis; 4) Medicine: Phenytoin, cyclosporine; 5) Habit disturbance: brygmus, the custom of biting hard‐thing, smoking and being addicted to drink, unilateral mastication, mis‐brushing habit, oral respiration. 2. Local factors 1) Severe periodontal disease; 2) Local in false dental prosthetic restoration; 3) Mis‐designed partial prosthodontics; 4) Fixed prosthodontics; 5) born‐missed teeth or abnormal extraction. |
| Interventions | Group 1: Hawley's removeavble retainer Group 2: transparent retainer Group 3: normal comparison observation group |
| Outcomes | PLI; Bite the number of the comtact point; GBI; ALI; CI (meaing of acronyms not provided) |
| Starting date | Registered 2007 |
| Contact information | Yu Yongchun , sjxj.558@163.com |
| Notes | Department of Orthodontics, the College of Stomatology of West China, Sichuan University |
Forde 2015.
| Trial name or title | Removable versus fixed orthodontic retention: a prospective randomised controlled trial |
| Methods | 30 participants having successfully completed a course of upper and lower fixed appliance therapy invited to participate in the study. Each participant randomly allocated to either upper and lower labial segment bonded retainers (17 participants) or upper and lower vacuum‐formed retainers (13 participants) using standardised clinical procedures, and materials. 2 calibrated operators were responsible for placing each retainer and managing subsequent participant recall |
| Participants | Consecutive orthodontic patients at 3 hospital orthodontic departments in the UK having completed a course of fixed appliance therapy, using clearly defined inclusion and exclusion criteria |
| Interventions | Upper and lower vacuum‐formed retainers or upper and lower bonded retainers |
| Outcomes | Relapse, failure of retainers, periodontal and dental health outcomes, patient satisfaction and cost‐effectiveness |
| Starting date | 2011 |
| Contact information | simonjlittlewood@aol.com |
| Notes | Ongoing trial |
IRCT2013113015598N1.
| Trial name or title | Comparision of the effect of three different approaches of retention on reopening of extraction space of fixed orthodontic patients in three different retention phases |
| Methods | Parallel RCT, single‐blind |
| Participants | 90 males and females, any age Inclusion criteria: the presence of all the permanent teeth irrespective of third molars; the use of a fixed flexible spiral wire retainer or an extended fixed retainer or a fixed flexible spiral wire retainer along with a Hawley plaque Exclusion criteria:missing teeth; the use of other types of retainers |
| Interventions | Group 1: extended fixed retainer
Group 2: flexible spiral wire retainer Group 3: fixed flexible spiral wire retainer along with Hawley plaque |
| Outcomes | Reopening of extraction space |
| Starting date | 2013 |
| Contact information | Farzaneh Rasouli, rasoulifa@tbzmed.ac.ir |
| Notes | Faculty of Dentistry, Tabriz University of Medical Sciences, Iran |
Differences between protocol and review
After careful consideration, we decided to exclude quasi‐randomised studies in updates of our original Cochrane review, to reduce the risk of bias. This has resulted in the exclusion of three previously included studies from this updated 2015 review (Edwards 1988; Sauget 1997; Taner 2000).
In addition, we changed the term 'quality of life' from the original protocol to 'patient satisfaction' in this updated 2015 review. This is because it better reflects the outcome being described.
Contributions of authors
Simon Littlewood (SL), Declan Millett (DM), Bridget Doubleday (BD) and David Bearn (DB) wrote the protocol. All review authors contributed to writing the review. SL co‐ordinated the review and wrote the letters to the authors and wrote the first draft of the review. SL worked with the Cochrane Oral Health Group to undertake the search strategy. SL, DM, BD, DB and Helen V Worthington (HW) independently assessed the eligibility of the trials, extracted data and assessed the risk of bias in the trials. HW assessed the suitability of the data from the trial reports for inclusion, and advised on and helped undertake statistical analysis.
Sources of support
Internal sources
St Luke's Hospital, Bradford, UK.
Glasgow Dental Hospital, Glasgow, UK.
University of Cork, Cork, Ireland.
School of Dentistry, The University of Manchester, UK.
External sources
-
National Institute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Infrastructure funding to the Cochrane Oral Health Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service (NHS), or the Department of Health.
-
Global Alliance, Other.
Through our Global Alliance (ohg.cochrane.org/partnerships‐alliances), the Cochrane Oral Health Group has received support from: British Association for the Study of Community Dentistry, UK; British Association of Oral Surgeons, UK; British Orthodontic Society, UK; British Society of Paediatric Dentistry, UK; British Society of Periodontology, UK; Canadian Dental Hygienists Association, Canada; Mayo Clinic, USA; National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and Royal College of Surgeons of Edinburgh, UK.
Declarations of interest
Simon J Littlewood: I have previously given educational orthodontic lectures for 3M Unitek. This in no way compromises the integrity of his involvement in this review, but is disclosed for complete transparency. Declan T Millett: none known. Bridget Doubleday: none known. David R Bearn: I received fees from Ormco Europe for lectures not directly related to this review topic. Helen V Worthington: none known.
Four of the review authors (SL, DM, BD and DB) have an interest or have been involved in studies investigating retention procedures, but this has in no way influenced the quality or objectivity of this review.
Two of the review authors (DM and BD) are co‐authors of included studies (Millett 2007; Rohaya 2006), so these review authors did not undertake the analysis of these studies during the review process.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Årtun 1997 {published and unpublished data}
- Årtun J, Spadafora AT, Shapiro PA. A 3‐year follow‐up study of various types of orthodontic canine‐to‐canine retainers. European Journal of Orthodontics 1997;19(5):501‐9. [DOI] [PubMed] [Google Scholar]
- Årtun J, Spadafora AT, Shapiro PA, McNeill RW, Chapko MK. Hygiene status associated with different types of bonded, orthodontic canine‐to‐canine retainers. A clinical trial. Journal of Clinical Periodontology 1987;14(2):89‐94. [DOI] [PubMed] [Google Scholar]
Aslan 2013 {published and unpublished data}
- Aslan BI, Dincer M, Salmanli I, Qasem MAM. Comparison of the effects of modified and full‐coverage thermoplastic retainers on occlusal contacts. Orthodontics: the Art and Practice of Dentofacial Enhancement 2013;14:e198‐208. [DOI] [PubMed] [Google Scholar]
Bolla 2012 {published and unpublished data}
- Bolla E, Cozzani M, Doldo T, Fontana M. Failure evaluation after a 6‐year retention period: a comparison between glass fiber‐ reinforced (GFR) and multistranded bonded retainers. International Orthodontics 2012;10:16‐28. [DOI] [PubMed] [Google Scholar]
Edman Tynelius 2015 {published data only (unpublished sought but not used)}
- Edman Tynelius G, Bondemark L. A randomized controlled trial of three orthodontic retention methods in Class I four premolar extraction cases ‐ stability after 2 years in retention. Orthodontics and Craniofacial Research 2013;16:105‐15. [DOI] [PubMed] [Google Scholar]
- Edman Tynelius G, Bondemark L, Lilja‐Karlander E. Evaluation of orthodontic retention capacity after one year of retention ‐ a randomized controlled trial. European Journal of Orthodontics 2010;32(5):542‐7. [DOI] [PubMed] [Google Scholar]
- Edman Tynelius G, Petrén S, Bondemark L, Lilja‐Karlander E. Five‐year postretention outcomes of three retention methods ‐ a randomized controlled trial. European Journal of Orthodontics 2015;37(4):345‐53. [DOI: 10.1093/ejo/cju063] [DOI] [PubMed] [Google Scholar]
Gill 2007 {published and unpublished data}
- Gill DS, Naini FB, Jones A, Tredwin CJ. Part‐time versus full‐time retainer wear following fixed appliance therapy: a randomized prospective controlled trial. World Journal of Orthodontics 2007;8:300‐6. [PubMed] [Google Scholar]
Kumar 2011 {published and unpublished data}
- Kumar AG, Bansal A. Effectiveness and acceptability of Essix and Begg retainers: a prospective study. Australian Orthodontic Journal 2011;27:52‐6. [PubMed] [Google Scholar]
Millett 2007 {published and unpublished data}
- McDermott P, Field D, Erfida I, Millett DT. Operator and patient experiences with fixed or vacuum formed retainers. Irish Division IADR Conference Abstract 0017. Cork, 2007.
- McDermott P, Millett DT, Field D, Heuvel A, Erfid I. Lower incisor retention with fixed or vacuum formed retainers. IADR Conference Abstract 0642. Toronto, 2008.
- Millett DT, McDermott P, Field D, Erfida I, Doubleday B, Vandenheuvel A, et al. Dental and periodontal health with bonded or vacuum‐formed retainer. IADR Conference Abstract 3168. Toronto, 2008.
O'Rourke [pers comm] {unpublished data only}
- O'Rourke N, Albeedh H, Sharma P, Johal A. Comparison of survival time between two types of orthodontic fixed retainer: a prospective randomized clinical trial [Personal communication]. Personal correspondence with authors. This study has been submitted for publication, but has not been published yet. We were aware of the study as the lead author was an orthodontic postgraduate student in the UK and known to the authors of the review.
Rohaya 2006 {published and unpublished data}
- Rohaya MAW, Shahrul Hisham ZA, Doubleday B. Randomised clinical trial: comparing the efficacy of vacuum‐formed and Hawley retainers in retaining corrected tooth rotations. Malaysian Dental Journal 2006;27(1):38‐44. [Google Scholar]
Rose 2002 {published and unpublished data}
- Rose E, Frucht S, Jonas IE. Clinical comparison of a multistranded wire and a direct‐bonded polyethylene ribbon‐reinforced resin composite used for lingual retention. Quintessence International 2002;33(8):579‐83. [PubMed] [Google Scholar]
Rowland 2007 {published and unpublished data}
- Hichens L, Rowland H, Williams A, Hollinghurst S, Ewings P, Clark S, et al. Cost‐effectiveness and patient satisfaction: Hawley and vacuum‐formed retainers. European Journal of Orthodontics 2007;29:372‐8. [DOI] [PubMed] [Google Scholar]
- Rowland H, Hichens L, Williams A, Hills D, Killingback N, Ewings P, et al. The effectiveness of Hawley and vacuum‐formed retainers: a single‐center randomized controlled trial. American Journal of Orthodontics and Dentofacial Orthopedics 2007;132:730‐7. [DOI] [PubMed] [Google Scholar]
Salehi 2013 {published data only}
- Salehi P, Najafi HZ, Roeinpeikar SM. Comparison of survival time between two types of orthodontic fixed retainer: a prospective randomized clinical trial. Progress in Orthodontics 2013;14:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shawesh 2010 {published and unpublished data}
- Shawesh M, Bhatti B, Usmani T, Mandall N. Hawley retainers full or part time? A randomized clinical trial. European Journal of Orthodontics 2010;32:165‐70. [DOI] [PubMed] [Google Scholar]
Sun 2011 {published and unpublished data}
- Sun J, Yu MY, Liu L, Chen L, Li HW, Zhang L, et al. Survival time comparison between Hawley and clear overlay retainers: a randomized trial. Journal of Dental Research 2011;90:1197‐201. [DOI] [PubMed] [Google Scholar]
Thickett 2010 {published and unpublished data}
- Thickett E, Power S. A randomized clinical trial of thermoplastic retainer wear. European Journal of Orthodontics 2010;32:1‐5. [DOI: 10.1093/ejo/cjp061] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
ACTRN12612000670875 {unpublished data only}
- ACTRN12612000670875. A prospective study of orthodontic retention outcomes with different retention strategies, 2012. www.anzctr.org.au/ACTRN12612000670875.aspx (accessed 2 May 2015).
Ahrens 1981 {published and unpublished data}
- Ahrens DG, Shapira Y, Kuftinec MM. An approach to rotational relapse. American Journal of Orthodontics 1981;80(1):83‐91. [DOI] [PubMed] [Google Scholar]
Al‐Nimri 2009 {published data only}
- Al‐Nimri K, Al Habashneh R, Obeidat M. Gingival health and relapse tendency: a prospective study of two types of lower fixed retainers. Australian Orthodontic Journal 2009;25(2):142‐6. [PubMed] [Google Scholar]
Arora 2014 {published and unpublished data}
- Arora S, Naik RD. Comparing relapse after occlusion using Begg and biocryl retainers. Orthodontic Update 2014;7:59‐66. [Google Scholar]
Atack 2007 {published data only}
- Atack N, Harradine N, Sandy JR, Ireland AJ. Which way forward? Fixed or removable lower retainers. Angle Orthodontist 2007;77 (6):954‐9. [DOI] [PubMed] [Google Scholar]
Axelsson 1993 {published and unpublished data}
- Axelsson S, Zachrisson BU. Clinical experience with direct‐bonded labial retainers. European Journal of Orthodontics 1993;4(15):333. [PubMed] [Google Scholar]
Barlin 2011 {published and unpublished data}
- Barlin S, Smith R, Reed R, Sandy J, Ireland AJ. A retrospective randomized double‐blind comparison of the effectiveness of Hawley vs vacuum‐formed retainers. Angle Orthodontist 2011;81(3):404‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Basciftici 2007 {published data only}
- Basciftci FA, Uysal T, Sari Z, Inan O. Occlusal contacts with different retention procedures in 1‐year follow‐up period. American Journal of Orthodontics and Dentofacial Orthopedics 2007;131(3):357‐62. [DOI] [PubMed] [Google Scholar]
Bauer 2010 {published and unpublished data}
- Bauer EM, Behrents R, Oliver DR, Buschang PH. Posterior occlusion changes with a Hawley vs perfector and Hawley retainer. Angle Orthodontist 2010;80:853‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bazargani 2012 {published data only}
- Bazargani F, Jacobsona S, Lennartssonb B. A comparative evaluation of lingual retainer failure bonded with or without liquid resin. Angle Orthodontist 2012;82:84‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bock 2008 {published data only}
- Bock N, Ruf S. Post‐treatment occlusal changes in Class II division 2 subjects treated with the Herbst appliance. European Journal of Orthodontics 2008;30(6):606‐13. [DOI] [PubMed] [Google Scholar]
Carvalho 2006 {published data only}
- Carvalho CV, Bauer FP, Romito GA, Pannuti CM, Micheli G. Orthodontic extrusion with or without circumferential supracrestal fiberotomy and root planing. International Journal of Periodontics & Restorative Dentistry 2006;26(1):87‐93. [PubMed] [Google Scholar]
Conway 2011 {published and unpublished data}
- Conway M, Littlewood SJ, Hodge T, Nelson‐Moon Z. Bonded retainers placed under rubber dam: an exploratory RCT. Journal of Orthodontics 2011;38:299. [Google Scholar]
Edwards 1988 {published and unpublished data}
- Edwards JG. A long‐term prospective evaluation of the circumferential supracrestal fiberotomy in alleviating orthodontic relapse. American Journal of Orthodontics and Dentofacial Orthopedics 1988;93(5):380‐7. [DOI] [PubMed] [Google Scholar]
- Edwards JG. A surgical procedure to eliminate rotational relapse. American Journal of Orthodontics 1970;57(1):35‐46. [DOI] [PubMed] [Google Scholar]
Haydar 1992 {published and unpublished data}
- Haydar B, Ciger S, Saatçi P. Occlusal contact changes after the active phase of orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics 1992;102(1):22‐8. [DOI] [PubMed] [Google Scholar]
Horton 2009 {published data only}
- Horton JK, Bushang PH, Oliver DR, Behrents RG. Comparison of the effects of Hawley and perfector/spring aligner retainers on postorthodontic occlusion. American Journal of Orthodontics and Dentofacial Orthopedics 2009;135(6):729‐36. [DOI] [PubMed] [Google Scholar]
ISRCTN22535947 {unpublished data only}
- ISRCTN22535947. The benefit of prolonged orthodontic retention ‐ a randomised clinical trial. isrctn.org/ISRCTN22535947 (accessed 2 May 2015).
ISRCTN26364810 {unpublished data only}
- ISRCTN26364810. Orthodontic treatment with a Twin Block appliance randomised to fixed or removable orthodontic retention. isrctn.org/ISRCTN26364810 (accessed 2 May 2015).
ISRCTN56295329 {unpublished data only}
- ISRCTN56295329. How should patients be supervised during orthodontic retention? A randomised controlled trial. isrctn.org/ISRCTN56295329 (accessed 2 May 2015).
Jäderberg 2012 {published and unpublished data}
- Jäderberg S, Feldmann I, Engström C. Removable thermoplastic appliances as orthodontic retainers. European Journal of Orthodontics 2012;34:475‐9. [DOI] [PubMed] [Google Scholar]
Larsson 1983 {published and unpublished data}
- Larsson E, Schmidt G. The effect of the supra‐alveolar soft tissue on the relapse of orthodontic treatment. British Journal of Orthodontics 1983;10(1):50‐2. [DOI] [PubMed] [Google Scholar]
Lindauer 1998 {published data only}
- Lindauer SJ, Shoff RC. Comparison of Essix and Hawley retainers. Journal of Clinical Orthodontics 1998;32:95‐7. [PubMed] [Google Scholar]
Pandis 2007 {published data only}
- Pandis N, Vlahopoulos K, Madianos P, Eliades T. Long‐term periodontal status of patients with mandibular lingual fixed retention. European Journal of Orthodontics 2007;29(5):471‐6. [DOI] [PubMed] [Google Scholar]
Pandis 2013 {published data only}
- Pandis N, Fleming PS, Kloukos D, Polychronopoulou A, Katsaros C, Eliades T. Survival of bonded lingual retainers with chemical or photo polymerization over a 2‐year period: a single‐center, randomized controlled clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics 2013;144:169‐75. [DOI] [PubMed] [Google Scholar]
Sauget 1997 {published and unpublished data}
- Sauget E, Covell DA, Boero RP, Lieber WS. Comparison of occlusal contacts with use of Hawley and clear overlay retainers. Angle Orthodontist 1997;67(3):223‐30. [DOI] [PubMed] [Google Scholar]
Stormann 2002 {published data only}
- Stormann I, Ehmer U. A prospective randomized study of different retainer types. Journal of Orofacial Orthopedics 2002;63(1):42‐50. [DOI] [PubMed] [Google Scholar]
Tacken 2010 {published data only}
- Tacken MP, Cosyn J, Wilde P, Aerts J, Govaerts E, Vannet BV. Glass fibre reinforced versus multistranded bonded orthodontic retainers: a 2 year prospective multi‐centre study. European Journal of Orthodontics 2010;32(2):117‐23. [DOI] [PubMed] [Google Scholar]
Taner 2000 {published and unpublished data}
- Taner T, Haydar B, Kavuklu I, Korkmaz A. Short‐term effects of fiberotomy on relapse of anterior crowding. American Journal of Orthodontics and Dentofacial Orthopedics 2000;118(6):617‐23. [DOI] [PubMed] [Google Scholar]
Vecere 1983 {published and unpublished data}
- Vecere JW. Extraction space closure stability following canine retraction and periodontal surgery. American Journal of Orthodontics 1983;84(1):89‐90. [Google Scholar]
References to studies awaiting assessment
Choi 2010 {published data only}
Liu 2010 {published data only}
Torkan 2014 {published data only}
Xu 2011 {published data only}
References to ongoing studies
ChiCTR‐TRC‐07000055 {unpublished data only}
- Hawley's retainer and transparent retainer for the oral cavity hygiene in orthodontic patients. Ongoing study Registered 2007.
ChiCTR‐TRC‐07000454 {unpublished data only}
- The impact of the Hawley's removable retainer and clear overlay removable retainer on orthodontic patients' oral hygiene. Ongoing study Registered 2007.
Forde 2015 {unpublished data only}
- Removable versus fixed orthodontic retention: a prospective randomised controlled trial. Ongoing study 2011.
IRCT2013113015598N1 {unpublished data only}
- Comparision of the effect of three different approaches of retention on reopening of extraction space of fixed orthodontic patients in three different retention phases. Ongoing study 2013.
Additional references
Aasen 2005
- Aasen T, Espeland L. An approach to maintain orthodontic alignment of lower incisors without the use of retainers. European Journal of Orthodontics 2005;27:209‐14. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Little 1981
- Little RM, Wallen TR, Riedel RA. Stability and relapse of mandibular anterior alignment ‐ first premolar extraction cases treated by traditional edgewise orthodontics. American Journal of Orthodontics 1981;80(4):349‐65. [DOI] [PubMed] [Google Scholar]
Little 1988
- Little RM, Riedel RA, Årtun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. American Journal of Orthodontics and Dentofacial Orthopedics 1988;93(5):423‐8. [DOI] [PubMed] [Google Scholar]
Mai 2014
- Mai W, He J, Meng H, Jiang Y, Huang C, Li M, et al. Comparison of vacuum‐formed and Hawley retainers: a systematic review. American Journal of Orthodontics and Dentofacial Orthopedics 2014;145(6):720‐7. [DOI] [PubMed] [Google Scholar]
Melrose 1998
- Melrose C, Millett DT. Toward a perspective on orthodontic retention?. American Journal of Orthodontics and Dentofacial Orthopedics 1998;113(5):507‐14. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Richmond 1992
- Richmond S, Shaw WC, O'Brien KD, Buchanan IB, Jones R, Stephens CD, et al. The development of the PAR Index (Peer Assessment Rating): reliability and validity. European Journal of Orthodontics 1992;14(2):125‐39. [DOI] [PubMed] [Google Scholar]
Worthington 2015
- Worthington H, Clarkson J, Weldon J. Priority oral health research identification for clinical decision‐making. Evidence‐based Dentistry 2015;16(3):69‐71. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Littlewood 2004
- Littlewood SJ, Millett DT, Doubleday B, Bearn DR, Worthington HV. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD002283] [DOI] [PubMed] [Google Scholar]
Littlewood 2006
- Littlewood SJ, Millett DT, Doubleday B, Bearn DR, Worthington HV. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD002283.pub3] [DOI] [PubMed] [Google Scholar]


