Abstract
Objective:
To estimate the prevalence of use and the micronutrient contribution of dietary supplements among pregnant, lactating, and non-pregnant and non-lactating women in the United States.
Methods:
Cross-sectional data from 1,314 pregnant, 297 lactating, and 8,096 non-pregnant and non-lactating women (aged 20-44 years) in the 1999-2014 National Health and Nutrition Examination Surveys were combined to produce statistically reliable, nationally representative estimates. Information about dietary supplements used in the past 30 days was collected through an interviewer-administered questionnaire and in-home inventory. The prevalence of nutrient-specific supplement use, mean daily nutrient intakes from supplements among users, and motivations for supplement use were assessed. Differences by age, income, and trimester within pregnant women were also tested.
Results:
Seventy-seven percent of pregnant and 70% of lactating women used one or more dietary supplements, whereas 45% of non-pregnant and non-lactating women used supplements. In particular, 64% of pregnant and 54% of lactating women used prenatal supplements. Mean intakes of thiamin, riboflavin, niacin, folic acid, vitamins B6, B12, and C, iron, and zinc from supplements alone were at or above their respective Recommended Dietary Allowances among pregnant and lactating supplement users. About half of pregnant and 40% of lactating women took supplements based on the recommendation of a health care provider. Among pregnant women, those in their first trimester, aged 20-34 years, or in a lower-income family were less likely to use supplements compared to their counterparts.
Conclusion:
The majority of pregnant and lactating women used dietary supplements, which contributed many nutrients in doses above the Recommended Dietary Allowances. While inadequate intakes of folate and iron are of concern among pregnant women not using supplements, supplement users often consumed high doses, suggesting a potential need of health care providers to discuss dietary supplement use and the recommended doses of nutrients during pregnancy and lactation.
Précis
The majority of pregnant and lactating women in the United States use dietary supplements, which contribute many nutrients in doses above the Recommended Dietary Allowances.
Introduction
Nutrient requirements increase during pregnancy and lactation, especially for certain micronutrients like folate, iron, iodine, and copper (1). To prevent possible nutrient inadequacies, clinicians and dietitians routinely recommend or prescribe prenatal supplements. The United States (U.S.) Preventive Services Task Force recommends women planning or capable of pregnancy take 400 to 800 μg/d of folic acid (2), and several health organizations recognize the importance of dietary supplements to meet requirements of specific nutrients (3, 4). Accordingly, the prevalence of dietary supplement use among pregnant women is substantially higher than that among the general population (5–7). Yet, a recent report on total usual nutrient intakes (from both foods and supplements) among U.S. pregnant women using data from the National Health and Nutrition Examination Survey (NHANES) 2001-2014 concluded that a significant proportion (>10%) of pregnant women are not consuming enough of some nutrients (e.g., vitamins A, B6, C, D, and E, folate, calcium, iron, magnesium, and zinc) even though 70% reported the use of dietary supplements (8). While almost no pregnant women had intakes above the tolerable upper intake level (UL) from food sources alone, dietary supplement use increased the proportion of those with intakes above the UL (i.e., potentially at risk of adverse effects due to excessive intakes) of some nutrients, especially iron and folic acid (8).
Thus, the use of dietary supplements should be carefully planned to compensate for under-consumed nutrients as well as to avoid exceeding the UL. However, little is known from a national perspective about nutrient-specific supplement use during pregnancy, and even less is known for lactating women. A few previous studies using national data focused only on supplements containing folic acid, iron, or iodine during pregnancy and lactation (5, 7, 9, 10). Furthermore, although differences in any dietary supplement use by age, family income, and trimester were noted among pregnant women in the NHANES 1999–2006 analysis (5), due to small sample sizes, stratified analyses by specific types of supplements were not possible. Lastly, the motivations for supplement use (i.e., whether based on the recommendation of a health care provider or by the woman’s own decision) of pregnant and lactating women have not previously been reported.
The primary aim of the present study was to describe the prevalence of nutrient-specific dietary supplement use and mean daily nutrient intakes from supplements among pregnant and lactating women in the U.S, using the NHANES 1999–2014 data. We also examined dietary supplement use by age, family income, and trimester within pregnant women, and motivation for supplement use.
Methods
NHANES examines a nationally representative, cross-sectional sample of the U.S. civilian, noninstitutionalized population, selected by using a complex, multistage probability design (11). NHANES is conducted by National Center for Health Statistics (NCHS), and its protocol was approved by the Research Ethics Review Board at the NCHS; further review for data analysis was not required. Since 1999, NHANES has operated as a continuous survey and includes an in-home interview where sociodemographic and dietary supplement use information is collected, followed by a health examination conducted in a mobile examination center within 1 to 3 weeks at which pregnancy and lactation information is collected. Survey participants could select English or Spanish as the language of interview or could request a translator. We combined data from the 1999-2014 NHANES for this analysis because the sample size for pregnant and lactating women is very small for each 2-year survey cycle, particularly after 2007; NHANES oversampled pregnant women during 2000-2006 to increase the precision of their estimates (11). The NCHS recommends combining ≥4 years of data to improve the reliability and stability of estimates (12).
During the health examination, pregnancy and lactation status was assessed using the reproductive health questionnaire administered by interview on women 12 years and older in tandem with a urinary pregnancy test on women aged 8-59 years. Current pregnancy status was determined based on both self-report and urine pregnancy test results and lactation status was determined by self-report of currently breastfeeding a child. However, due to risks of violating anonymity, pregnancy and lactation status is only publicly released by NHANES for women 20-44 years of age since 2007; women of other ages were therefore excluded from this analysis. Women aged 20-49 years had a response rate of 69~81% for the health examination across survey cycles (13). Among women who participated in the mobile examination center examination (n=39,755), we excluded those younger than 20 years (n=18,130), those older than 44 years of age (n=11,910), and those missing dietary supplement use information (n= 8). Therefore, the final analytical sample consisted of 9,707 reproductive-aged women categorized as pregnant (n=1,314), lactating (n=297), or non-pregnant and non-lactating women (n=8,096). Women who were concurrently pregnant and lactating (n=26) were included in the lactating group because pregnancy during lactating represents a particularly demanding nutritional condition (14) and nutrient requirements for lactating women are higher for most nutrients than for pregnant women (1).
During the in-home interview, information on age, sex, race and ethnicity, educational attainment, family income, and marital status was collected through a computer-assisted personal interview. Age was used as a continuous variable or as a categorical variable: 20-34y and 35-44y. Self-reported race and ethnicity used in this analysis were as defined in NHANES: non-Hispanic white, non-Hispanic black, Hispanic, and “other race.” Per NCHS analytical guidelines the “other” race category is not presented separately but is included in all other estimates. Educational attainment was categorized as less than high school graduate, high school graduate or equivalent, and some college or higher. The family income-to-poverty ratio (PIR) was calculated by NCHS as the ratio of annual family income to the poverty guideline to represent family income level. The PIR is categorized as PIR≤130%, 131 to ≤350%, and >350%; a PIR of 130% is an income eligibility criterion for several federal nutrition assistance programs (e.g., Supplemental Nutrition Assistance Program). Marital status was classed as married or living with partner, previously married, or never married. In addition, the trimester of pregnancy (first, second, or third trimester) was coded based on the self-reported month of pregnancy on the reproductive health questionnaire but was only available during 1999-2012. Out of 1,314 pregnant women in these survey cycles, 461 women were missing this information, mostly because they did not self-report pregnancy during the questionnaire interview but had positive urinary pregnancy test results.
Dietary supplement data were collected through a 30-day questionnaire in conjunction with a product inventory in the participants’ homes. Participants were asked to show the interviewer the containers and labels of any supplements used over the previous 30 days when available as well as to report type, frequency, duration, and amount taken for each supplement. After data collection, trained nutritionists at NCHS matched the products reported to the NHANES Dietary Supplement Database that contains information on the serving sizes and nutrient contents (per the product label’s supplement facts panel).
We classified dietary supplement products as follows: 1) “multi-vitamin-mineral” as any product containing 3 or more vitamins and 1 or more minerals, 2) “single- or multi-vitamin” as any product containing at least 1 vitamin without mineral nor botanical ingredient, 3) “single- or multi-mineral” as any product containing at least 1 mineral without vitamin or botanical ingredient, 4) “botanical” as any product with at least 1 botanical ingredient without vitamin nor mineral, and 5) “others” such as calcium plus vitamin D and fatty acid products (5, 15). In addition, we identified prenatal products according to the formulation type; products were coded as prenatal when the product name stated prenatal or the label indicated that it is for use by pregnant women. From the NHANES 2007-2008 cycle and beyond, for each supplement reported, participants were asked if they are taking the supplement for their own reasons or because a doctor or health care provider recommended to. Based on this information, we categorized pregnant and lactating women as those who took at least one supplement of any kind or a prenatal supplement based on a health care provider’s recommendation and those who took products on their own.
Specific nutrient-containing supplements were categorized based on their ingredients as recommended (16); for example, if a product contained folic acid or metafolin (L-methylfolate), it was identified as folic acid-containing supplements. Mean daily intake of nutrients from each supplement was calculated based on the nutrient amount per serving as stated on the product label, the number of servings consumed as reported by the participant, and the number of days taken in the past 30 days as reported by the participant. A total average daily nutrient intake from individual supplements consumed was summed for each participant. This analysis did not include sodium, potassium, fiber, protein, fats, and carbohydrates because these nutrients are rarely included in dietary supplements.
The population distributions of supplemental nutrient intakes are often skewed (17), so we presented estimated means and medians of nutrient intake from dietary supplements among users in conjunction with the current Recommended Dietary Allowance (RDA), Adequate Intake (AI), and UL, established by the Food and Nutrition Board of the National Academies of Sciences, Engineering, and Medicine (NASEM) (1). The RDA is the average daily intake level sufficient to meet the nutrient requirement of nearly all healthy individuals in a particular life stage group (i.e., pregnant women, lactating women, women aged 19-30 years, and women aged 31-50 years) and, therefore, serves a goal for dietary intake for healthy individuals (18). When the amount of evidence on a nutrient is not enough to set the RDA, an AI is set based on estimates of nutrient intake by a group (or groups) of people that are assumed to have adequate intakes. The RDA and AI are presented here as reference points but they are not used to estimate the population prevalence of intakes at potential risk for inadequacy. The UL is the highest average daily nutrient intake level that is unlikely to pose risk of adverse health effects to almost all individuals (18). Folate is unique in that the unit for the RDA is μg dietary folate equivalents (DFE) to take account of different bioavailability of different folate sources, whereas the UL only applies to folic acid, a synthetic form of folate from fortified foods and supplements, but not to food folate (19). Because we only examined folic acid consumed as supplements, we presented the RDA in μg folic acid using the conversion factor of 1 μg DFE = 0.6 μg folic acid (19), assuming supplements were consumed with food. This assumption has been made in the most recent Food and Drug Administration guideline for labeling (20).
Statistical analyses were performed using SAS (version 9.3, SAS Institute Inc., Cary, NC) and SAS-callable SUDAAN (version 11.1, RTI, Research Triangle Park, NC) software. All analyses used survey procedures that account for the complex survey design, incorporating the 16-year examination weights constructed for the combined survey period. Weighting takes into account of the differential probabilities of selection (including oversampling), survey nonresponse, and differences in distributions between final sample and the target population; therefore, using the sampling weights produces nationally representative estimates (12). Standard errors (SEs) were estimated using Taylor Series Linearization. Percentages and SEs of the categorical variables (e.g., sociodemographic characteristics and dietary supplement use) and means and SEs of the continuous variables (e.g., age and nutrient intake) were examined for pregnant, lactating, and non-pregnant and non-lactating women. Differences in distributions of sociodemographic characteristics among subgroups were assessed using Satterthwaite-adjusted Wald Chi-square test, and a p<0.05 was considered statistically significant. Differences in the prevalence of dietary supplement use and mean nutrient intakes among subgroups were assessed using pairwise comparisons, and a Bonferroni-adjusted p<0.0167 (i.e., 0.05 / 3 subgroups) was considered statistically significant. Linear trends were tested using orthogonal polynomials; a p<0.05 was considered to be statistically significant.
Results
In 1999-2014, pregnant and lactating women tended to be younger than non-pregnant and non-lactating women (P<0.0167) (Table 1). The majority of pregnant and lactating women were non-Hispanic white, had some college education or higher, and married or living with partner. Seventy-seven percent of pregnant and 70.3% of lactating women used one or more dietary supplements, significantly higher than the 44.8% of non-pregnant and non-lactating women (P<0.0167). In particular, 64.4% of pregnant and 54.2% of lactating women used a prenatal product, primarily multi-vitamin-minerals, defined as having ≥3 vitamins and at least 1 mineral. The prevalence of any supplement use was significantly higher in older pregnant women (88.1%) than in younger pregnant women (75.2%) (P<0.05) (Figure 1). Among pregnant women, both any supplement use and prenatal supplement use increased with increasing income (P<0.001) (Figure 2). During 1999-2012 when trimester information was available, the prevalence of prenatal supplement use was 52.4% among women in the first trimester and increased to 80.0% among those in the second trimester, remaining stable at 80.4% among those in the third trimester (Table 2).
Table 1.
Sociodemographic characteristics of and dietary supplement use by women (20–44y) by pregnancy and lactation status in the United States, NHANES 1999-2014
| Characteristic | Pregnant women (n=1,314) | Lactating women (n=297) | Non-pregnant and non-lactating women (n=8,096) | P* |
|---|---|---|---|---|
| Age (y), mean ± SE | 28.4 ± 0.3 a | 29.9 ± 0.5 b | 32.5 ± 0.1 c | |
| Race and ethnicity† | 0.001 | |||
| Non-Hispanic white | 53.6 ± 2.5 | 63.1 ± 4.2 | 62.7 ±1.3 | |
| Non-Hispanic black | 16.3 ± 1.7 | 8.7 ± 1.8 | 13.6 ± 0.7 | |
| Hispanic | 20.2 ± 1.7 | 20.7 ± 2.8 | 16.8 ± 1.0 | |
| Education‡ | 0.008 | |||
| Less than high school graduate | 19.3 ± 1.6 | 12.4 ± 2.3 | 15.8 ± 0.6 | |
| High school graduate | 18.1 ± 1.6 | 15.2 ± 2.6 | 21.3 ± 0.7 | |
| Some college or higher | 62.6 ± 2.0 | 72.3 ± 3.3 | 62.9 ± 0.9 | |
| Family income‡ | 0.614 | |||
| PIR≤130% | 27.2 ± 1.8 | 30.0 ± 3.2 | 28.4 ± 0.8 | |
| PIR 131–350% | 33.9 ± 2.1 | 35.6 ± 3.4 | 36.4 ± 0.8 | |
| PIR>350% | 38.9 ± 2.7 | 34.4 ± 3.8 | 35.2 ± 1.0 | |
| Marital status‡ | <0.001 | |||
| Married or living with partner | 78.7 ± 1.9 | 91.8 ± 2.1 | 59.2 ± 0.9 | |
| Previously married | 2.9 ± 0.5 | 5.2 ± 1.8 | 12.5 ± 0.5 | |
| Never married | 18.4 ± 1.8 | 3.0 ± 1.1 | 28.4 ± 0.9 | |
| Any supplement use | 77.4 ± 1.6 a | 70.3 ± 3.2 a | 44.8 ± 0.8 b | |
| Multi-vitamin-mineral | 72.9 ± 2.0 a | 64.4 ± 3.5 a | 31.0 ± 0.7 b | |
| Single- or multi-vitamin | 11.1 ± 1.5 a | 10.1 ± 2.5 a | 15.0 ± 0.5 a | |
| Single- or multi-mineral | 10.9 ± 1.4 a | 12.0 ± 2.5 a | 7.8 ± 0.4 a | |
| Botanical | ES§ | ES§ | 5.4 ± 0.3 | |
| Prenatal supplement use | 64.4 ± 1.9 a | 54.2 ± 3.5 b | 3.4 ± 0.3 c | |
NHANES, National Health and Nutrition Examination Survey; PIR, family income-to-poverty ratio
All estimates are percentages ± SEs otherwise noted.
Estimates with different alphabetic characters are significantly different from each other at a Bonferroni-adjusted p<0.0167.
P-values for categorical sociodemographic variables were obtained from Satterthwaite-adjusted Wald Chi-square test.
Race and ethnicity does not sum to 100% because the “other” race category is not presented.
9, 683, and 119 women are missing information on education, family income, and marital status.
Estimate suppressed because of relative standard error is greater than 30%.
Figure 1.
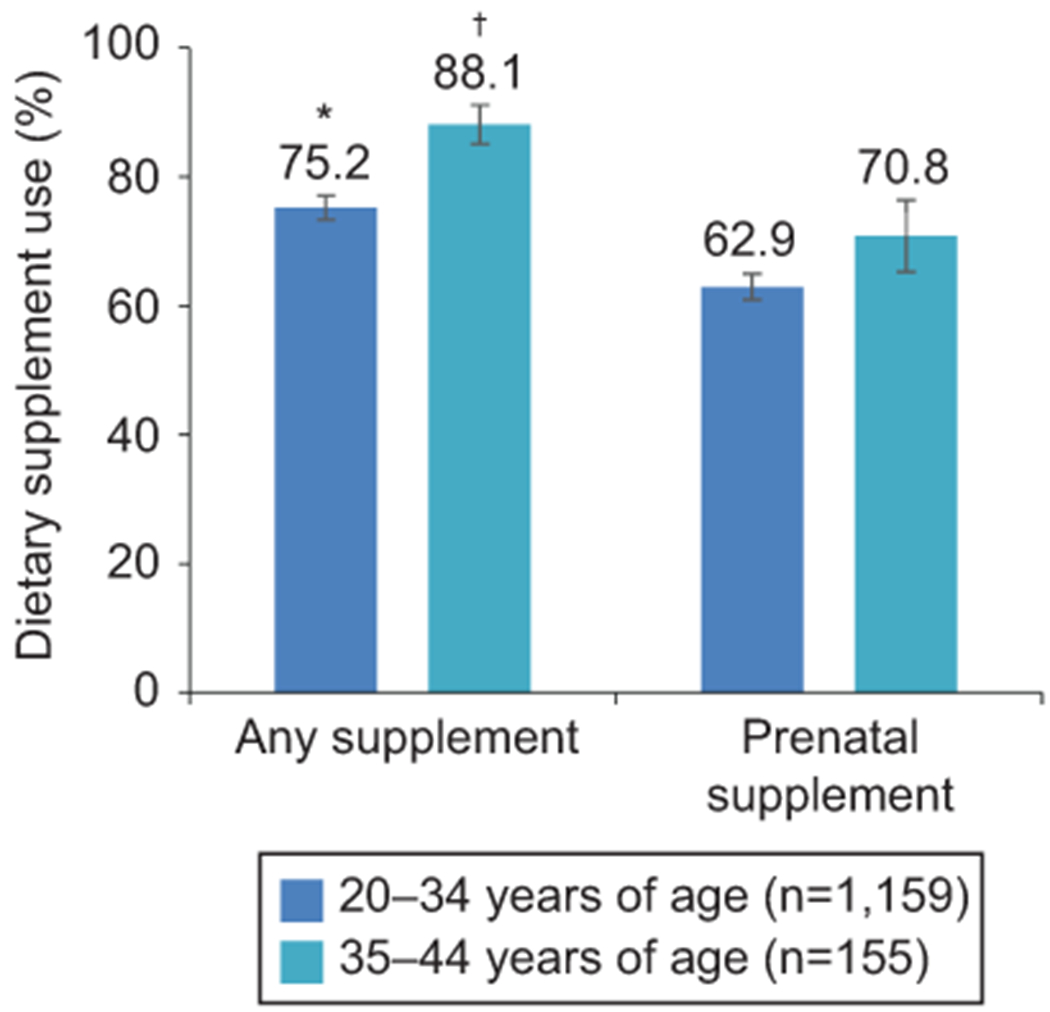
Prevalence of dietary supplement use by younger (20–34 years of age) and older (35–44 years of age) pregnant women in the United States, National Health and Nutrition Examination Survey 1999–2014. *†Estimates are significantly different from each other at P<.05.
Figure 2.
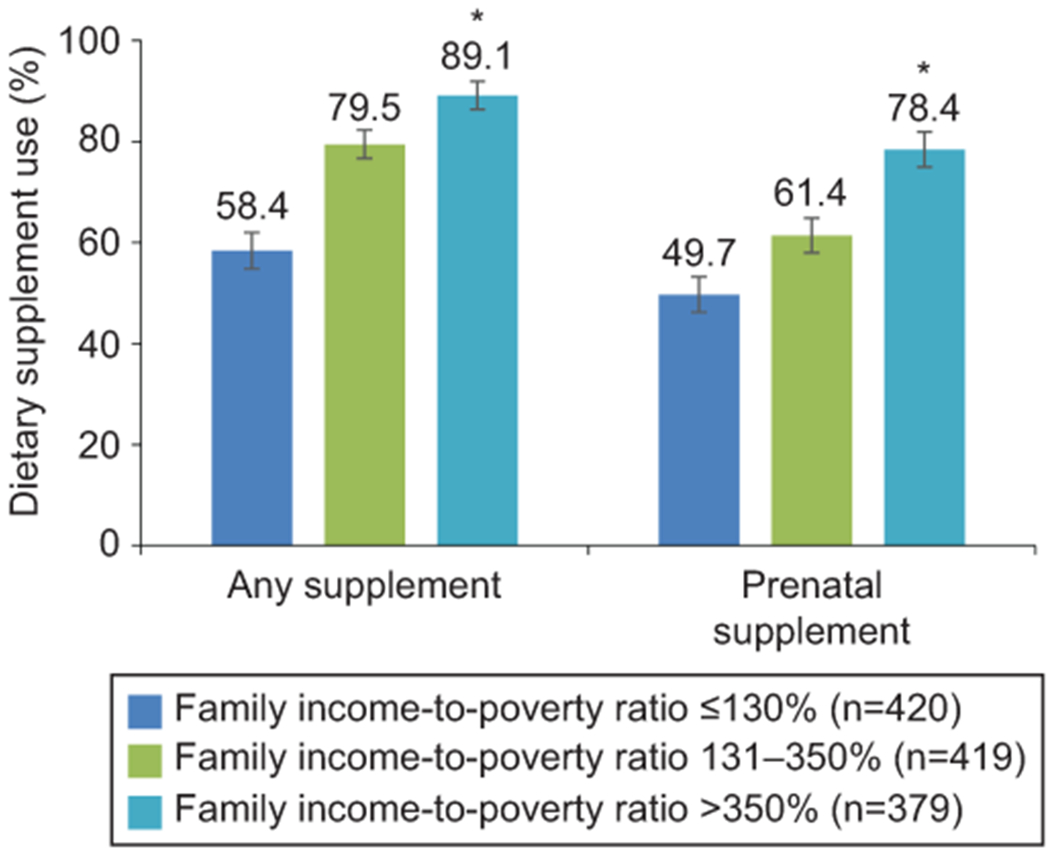
Prevalence of dietary supplement use by family income-to-poverty level among pregnant women (20–44 years of age) in the United States, National Health and Nutrition Examination Survey 1999–2014. *Significant linear trend across family income-to-poverty ratio categories (P<.001).
Table 2.
Prevalence of dietary supplement use by trimester of pregnancy among pregnant women (20-44y) in the United States, NHANES 1999-2012 (n=790)
| Trimester* |
|||
|---|---|---|---|
| First (n=147) | Second (n=332) | Third (n=311) | |
| Any supplement use | 72.0 ± 5.8 a | 86.3 ± 2.5 a,b | 90.8 ± 2.4 b |
| Multi-vitamin-mineral | 69.9 ± 5.8 a | 82.2 ± 3.0 a | 87.0 ± 3.1 a |
| Folic acid-containing | 70.6 ± 5.9 a | 84.3 ± 2.9 a | 87.5 ± 3.0 a |
| Iron-containing | 66.1 ± 6.2 a | 81.9 ± 3.0 a,b | 89.3 ± 2.5 b |
| Iodine-containing | 22.8 ± 5.9 a | 19.8 ± 3.5 a | 22.8 ± 4.2 a |
| Prenatal supplement use | 52.4 ± 6.3 a | 80.0 ± 3.1 b | 80.4 ± 3.4 b |
NHANES, National Health and Nutrition Examination Survey
All estimates are percentages ± SEs.
Estimates with different alphabetic characters are significantly different from each other at P<0.0167.
Information on month of pregnancy was only available in 1999-2012. The 461 women who did not have information on month of pregnancy are not included.
During 2007-2014 when NHANES collected the motivations for supplement use, 47.4% of pregnant women took at least one dietary supplement based on a health care provider’s recommendation, while 16.1% of pregnant women reported the use based on their own decision (Figure 3). Similarly, among lactating women, 39.8% took at least one dietary supplement because of a health care provider’s recommendation, and 22.8% made the decision on their own. Among non-pregnant and non-lactating women, 11.5% took supplements based on a health care provider’s recommendation, 30.6% took on their own.
Figure 3.
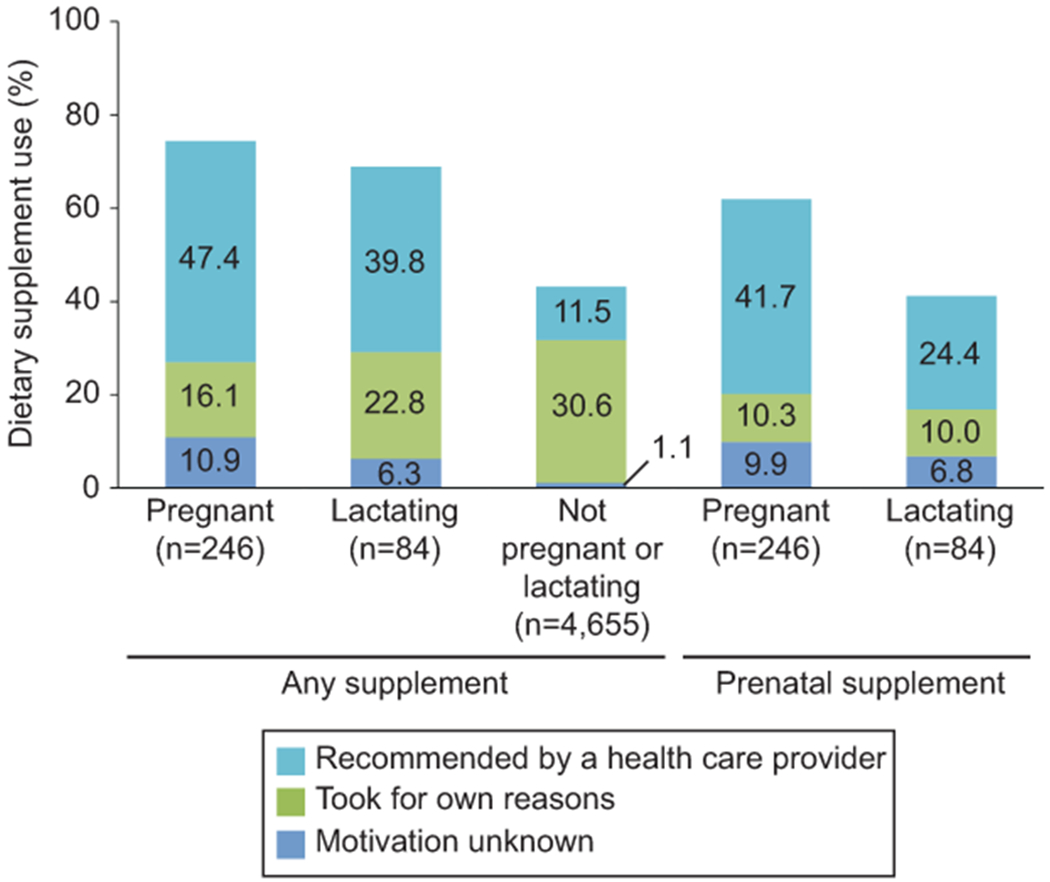
Prevalence of reasons for dietary supplement use among pregnant and lactating women (20–44 years of age) in the United States, National Health and Nutrition Examination Survey 2007–2014 (n=330). Women who used at least one dietary supplement product based on the recommendation of a health care provider were classed as recommended by a health care provider. Information on the reason for dietary supplement use was only available in 2007–2014.
More than 60% of pregnant and lactating women used supplements containing thiamin; riboflavin; niacin; folic acid; vitamins B-6, B-12, C, and D; calcium; iron; selenium; and zinc (Table 3). The prevalence of pregnant and lactating women taking supplements containing the following nutrients was relatively low: choline (5~8%), iodine (18~20%), magnesium (26~28%), phosphorus (5~6%), and selenium (10~12%).
Table 3.
Percentages of women (20-44y) using dietary supplements containing specified micronutrients by pregnancy and lactation status in the United States, NHANES 1999-2014
| Pregnant women (n=1,314) | Lactating women (n=297) | Non-pregnant and non-lactating women (n=8,096) | |
|---|---|---|---|
| Vitamin A | 40.3 ± 2.2 a | 41.6 ± 3.7 a | 22.0 ± 0.6 b |
| Thiamin | 69.4 ± 2.2 a | 63.7 ± 3.4 a | 30.4 ± 0.7 b |
| Riboflavin | 69.4 ± 2.2 a | 63.7 ± 3.4 a | 30.4 ± 0.7 b |
| Niacin | 69.6 ± 2.2 a | 63.9 ± 3.4 a | 31.2 ± 0.7 b |
| Vitamin B6 | 72.8 ± 2.1 a | 65.1 ± 3.4 a | 32.7 ± 0.7 b |
| Folic acid | 73.3 ± 2.1 a | 65.1 ± 3.4 a | 32.9 ± 0.7 b |
| Vitamin B12 | 69.9 ± 2.1 a | 63.9 ± 3.5 a | 32.9 ± 0.7 b |
| Vitamin C | 73.3 ± 2.0 a | 64.6 ± 3.4 a | 35.5 ± 0.8 b |
| Vitamin D | 71.7 ± 2.0 a | 66.8 ± 3.3 a | 33.1 ± 0.7 b |
| Vitamin E | 72.0 ± 2.0 a | 64.0 ± 3.5 a | 32.6 ± 0.7 b |
| Choline | 4.9 ± 1.1 a | 7.6 ± 2.1 a | 5.2 ± 0.3 a |
| Calcium | 68.1 ± 2.2 a | 62.3 ± 3.2 a | 32.2 ± 0.7 b |
| Iodine | 20.4 ± 1.7 a | 17.5 ± 2.5 a | 18.2 ± 0.6 a |
| Iron | 72.3 ± 2.0 a | 65.0 ± 3.3 a | 28.3 ± 0.7 b |
| Magnesium | 28.1 ± 2.1 a | 26.2 ± 3.8 a | 26.0 ± 0.6 a |
| Phosphorous | 5.2 ± 1.0 a | 6.2 ± 2.0 a | 13.3 ± 0.5 b |
| Selenium | 9.9 ± 1.2 a | 11.7 ± 2.7 a | 21.0 ± 0.6 b |
| Zinc | 68.0 ± 2.2 a | 60.6 ± 3.5 a | 29.8 ± 0.7 b |
NHANES, National Health and Nutrition Examination Survey.
All estimates are percentage ± SEs.
Estimates with different alphabetic characters are significantly different from each other at P<0.0167.
The estimated daily mean intakes of micronutrients from dietary supplements among users are presented in Table 4. Mean intakes of thiamin, riboflavin, niacin, folic acid, vitamins B6, B12, and C, iron, and zinc from supplements alone were at or above their respective Recommended Dietary Allowances among pregnant and lactating supplement users. In particular, dietary supplements contributed a mean daily intake of 787 μg/d of folic acid, 9.2 μg/d of vitamin B6, 10 μg/d of vitamin D, 366 mg/d of calcium, 38.4 μg/d of iron, 74.6 μg/d of magnesium and 18.2 μg/d of zinc among pregnant supplement users. Few differences in mean micronutrient intakes among users were observed between pregnant and lactating women. The estimated median intakes from supplements were lower than the means in general, reflecting that the distribution was skewed to the right, but similar patterns by pregnancy and lactation status were observed among median intakes (Appendix 1, available online at http://links.lww.com/AOG/B704).
Table 4.
Mean daily micronutrient intakes from dietary supplements alone among users of dietary supplements containing the specified nutrient, by pregnancy and lactation status in the United States, NHANES 1999–2014
| Pregnant women (n=1,314) | Lactating women (n=297) | Non-pregnant and non-lactating women (n=8,096) | UL | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n* | Mean ± SE | RDA | n | Mean ± SE | RDA | n | Mean ± SE | RDA | ||
| Thiamin (mg)† | 743 | 2.9 ± 0.2 a | 1.4 | 162 | 2.8 ± 0.5 a | 1.4 | 2,065 | 8.1 ± 0.5 b | 1.1 | ND |
| Riboflavin (mg) | 743 | 3.0 ± 0.2 a | 1.4 | 162 | 3.0 ± 0.5 a | 1.6 | 2,066 | 7.3 ± 0.5 b | 1.1 | ND |
| Niacin (mg) | 742 | 19.0 ± 1.6 a,b | 18 | 163 | 17.9 ± 0.9 a | 17 | 2,122 | 22.6 ± 1.0 b | 14 | 35 |
| Vitamin B6 (mg) | 772 | 9.2 ± 0.7 a | 1.9 | 166 | 7.9 ± 1.0 a | 2.0 | 2,219 | 9.6 ± 0.6 a | 1.3 | 100 |
| Folic acid (μg)‡ | 786 | 787 ± 30 a | 360 | 167 | 718 ± 28 a | 300 | 2,196 | 375 ± 7 b | 240 | 1000 |
| Vitamin B12 (μg) | 746 | 16.8 ± 4.6 a | 2.6 | 163 | ES§ | 2.8 | 2,249 | 75.0 ± 10.3 b | 2.4 | ND |
| Vitamin C (mg) | 775 | 126 ± 7 a | 85 | 167 | 136 ± 17 a | 120 | 2,419 | 210 ± 12 b | 75 | 2000 |
| Vitamin D (μg) | 763 | 10.0 ± 0.7 a | 15 | 170 | 12.2 ± 2.3 a | 15 | 2,273 | 15.6 ± 2.6 a | 15 | 100 |
| Choline (mg) | 49 | 15.3 ± 2.8 a | 450‖ | 18 | 13.2 ± 3.5 a | 550‖ | 361 | ES§ | 425‖ | 3500 |
| Calcium (mg) | 756 | 366 ± 69 a | 1,000 | 168 | 269 ± 21 a | 1,000 | 2,475 | 317 ± 9 a | 1000 | 2500 |
| Iodine (μg) | 219 | 116 ± 6 a | 220 | 46 | 104 ± 11 a | 290 | 1,214 | 107 ± 2 a | 150 | 1100 |
| Iron (mg) | 777 | 38.4 ± 1.9 a | 27 | 166 | 34.1 ± 2.6 a | 9 | 1,920 | 17.1 ± 0.4 b | 18 | 45 |
| Magnesium (mg) | 297 | 74.6 ± 9.5 a | 350/360¶ | 67 | 81.4 ± 15.0 a | 310/320¶ | 1,834 | 80.2 ± 2.6 a | 310/320¶ | 350 |
| Phosphorous (mg) | 65 | 130 ± 30 a | 700 | 16 | ES§ | 700 | 864 | 79 ± 3 a | 700 | 4000 |
| Selenium (μg) | 108 | 43.5 ± 6.2 a,b | 60 | 34 | 28.3 ± 4.7 a | 70 | 1,424 | 44.8 ± 1.7 b | 55 | 400 |
| Zinc (mg) | 709 | 18.2 ± 0.5 a | 11 | 160 | 18.5 ± 0.8 a | 12 | 2,023 | 12.2 ± 0.3 b | 8 | 40 |
NHANES, National Health and Nutrition Examination Survey; ND, Not Determined; RDA, Recommended Dietary Allowances; UL, Tolerable Upper Intake Level.
Estimates with different alphabetic characters are significantly different from each other at P<0.0167.
Unweighted sample size of those who consumed dietary supplements containing a specific nutrient.
Nutrient intake from dietary supplements could not be calculated if information on the number of servings consumed or the number of days taken was missing.
In μg folic acid. The RDAs that were presented as μg of dietary folate equivalents were converted to μg of folic acid based on the equation set by the National Academies of Sciences, Engineering, and Medicine, 1 μg of dietary folate equivalents = 0.6 μg of folic acid with meals. The UL only applies to folic acid consumed through fortified food or dietary supplements.
Estimate suppressed because of relative standard error is greater than 30%.
Denotes the Adequate Intakes; unless otherwise noted the RDA is presented.
Magnesium requirement differs based on age; 350 mg for 19–30y and 360 mg for 31–50y.
Between 1999-2002 and 2011-2014, the prevalence of dietary supplement use remained stable among pregnant and lactating women not only in terms of any supplement used but also in specific product categories and specific nutrient-containing supplement used (Appendix 2, available online at http://links.lww.com/AOG/B704). However, among non-pregnant and non-lactating women, the use of supplements containing iodine (23% in 1999-2002 to 15% in 2011-2014; P<0.001) and iron (32% in 1999-2002 to 25% in 2011-2014; P<0.001) decreased over time.
Discussion
Over 70% of pregnant and lactating women aged 20-44 years in the U.S. reported the use of at least one dietary supplement, primarily prenatal supplement. Consistent with previous findings, supplement use was substantially higher among pregnant and lactating women compared to non-pregnant and non-lactating women (5–7). The majority of pregnant women consumed supplements containing a wide range of nutrients, with the daily mean intake of selected vitamins and minerals from supplements reaching or exceeding the RDA. The number and amount of nutrients included in prenatal supplements are not standardized, but almost all products contain one or more nutrients at levels that are as much as the RDA or more (21). Therefore, it is important to examine nutrients from supplements as well as from foods and beverages. Recently, Bailey et al. (8) estimated the total usual nutrient intakes adjusting for within-person variation from the two 24-hour dietary recalls (including supplements) among pregnant women in the NHANES 2001-2014 and compared those to the Dietary Reference Intakes. A significant number of pregnant women had usual intakes below the Estimated Average Requirements (i.e., were at risk of inadequacy) for vitamins A (16%), B6 (11%), C (12%), D (46%), and E (43%), folate (16%), iron (36%), calcium (13%), magnesium (48%), and zinc (11%), and very few met or exceeded the AI for choline (8%). The findings of the present study indicate that some of these under-consumed nutrients, namely, magnesium and choline, are not commonly supplemented during pregnancy and lactation, while other nutrients (i.e., vitamins A, B6, C, D, and E, folate, iron, calcium, and zinc) are consumed from supplements by more than 40% of pregnant and lactating women.
Folate is an especially important nutrient during the periconceptional period as it helps the fetus form the neural tube, but may not be consumed enough from food sources alone (22). Therefore, to help prevent neural tube defects, the U.S. Preventive Services Task Force recommends all women planning or capable of pregnancy to take a supplement containing 400 to 800 μg of folic acid each day, emphasizing a month before conception through 2 to 3 months of pregnancy as the critical period (2). Unfortunately, we found that ~30% of pregnant women in their first trimester did not take any folic acid from supplements. Women in their second and third trimesters were more likely to consume any supplement than those in their first trimester, confirming earlier findings by others (5). It may be possible that women in their early pregnancy may not be aware of their pregnancy or associated recommendations (23) or have difficulties with oral intake due to pregnancy-related nausea and vomiting (24). Nonetheless, mean daily folic acid intake among users was 787 ± 30 μg, which indicates that some users consumed more than recommended amounts; indeed >40% of the pregnant supplement users exceeded the UL in 2001-2014 (8). The UL was set based on the exacerbation of the neurological damage of vitamin B12 deficiency (19). Moreover, the health impacts, if any, of high folic acid intake during pregnancy on fetal development remain largely unknown; some data from animal studies and epidemiological studies raise potential cause for concern, as summarized by Lamers et al. (25)
For iron, the World Health Organization recommends daily supplementation with 30 to 60 mg of iron for pregnant women to prevent maternal anemia, puerperal sepsis, preterm birth, and low birth weight throughout pregnancy (26). Specifically for the U.S. population, the Centers for Disease Control and Prevention recommends 30 mg/day of iron supplementation for all pregnant women (27). We found that 72.3% of pregnant women were using iron-containing supplements, which contributed 38.4 mg/d on average among users. This explains the earlier findings of Bailey et al. (8) that, among pregnant women who took supplements, the prevalence of inadequate iron intake was 80.3% when only food sources were considered, but decreased to 13.9% when dietary supplements were included; at the same time, the prevalence of intakes above the UL increased from 0% to 40.2% when including supplements. The UL for iron was primarily based on gastrointestinal distress as an adverse effect (28). Among pregnant women not using supplements, almost all (95.3%) were at risk of iron inadequacy. Lactating women had a similar pattern of iron-containing supplement use as pregnant women.
Iodine plays a critical role in fetal brain development, especially during early pregnancy (28). Information on iodine intake from food sources is not available in NHANES but an analysis of urinary iodine concentration data from the 2001-2006 NHANES concluded that the iodine status of pregnant women was borderline sufficient; that of lactating women was generally sufficient; and some women, especially those who did not consume dairy products, were at risk for iodine insufficiency based on the WHO criteria (29). To prevent possible insufficiency, the American Thyroid Association recommends that all women who are pregnant, lactating, and planning of pregnancy to supplement 150 μg of iodine a day (30, 31). While most prenatal products contain ~150 μg of iodine (10, 21), iodine-containing supplement use very low among pregnant women (20.4% consuming 116 μg/d from supplements on average) and lactating women (17.5% consuming 104 μg/d from supplements on average) in the U.S. (7, 10, 29).
Motivations for supplement use have been collected in NHANES since 2007. In 2007-2014, about two-thirds of pregnant and 60% of lactating supplement users took at least one product based on a health care provider’s recommendation. These findings were as expected because it is common practice for clinicians and dietitians to recommend or prescribe a prenatal supplement; furthermore, a prescription by a health professional is required for reimbursement by private and public insurance programs. In 1999-2006, 37% and 28% of pregnant women (15-39 years) used prescription and over-the-counter prenatal supplements, respectively (10). Given the wide variety of supplement product formulations available, it is important for health care providers to help individuals review all products they are taking to ensure that safe but not excessive intakes of nutrients are provided (32, 33). Women who are not using prenatal supplements may need encouragement as some barriers to prenatal supplement use have been documented among minority women identified, including adverse effects, forgetting to consume, and perceiving prenatal supplements as unnecessary or ineffective (34). Our results on income differences suggest that limited financial resources may also affect prenatal supplement use among pregnant women (35). Clear and open communication about the benefits of prenatal supplements as well as concerns and alternatives may help improve prenatal supplement use (34).
About 9 out of 10 pregnant women at 35-44 years were using dietary supplements. One possible explanation for the higher prevalence of supplement use in older pregnant women is that they may receive more pre- and perinatal care because pregnancy at 35 years or older is associated with a higher risk of complications (36, 37). In addition, older pregnant women had higher educational attainment and higher family income and were more likely to be married or living with a partner than their younger counterparts (Appendix 3, available online at http://links.lww.com/AOG/B704); all of which have been previously associated with higher supplement use (5, 6).
The strengths of this study include statistically reliable estimates of dietary supplement use among U.S. pregnant and lactating women produced by combining 8 cycles of NHANES data reflecting 16 years. NHANES collects high-quality data on supplement use by using a 30-day questionnaire along with an in-home inventory in which approximately 80% of all supplement products reported were shown to trained interviewers. The prevalence of supplement use has been largely stable among women of reproductive age during 1999-2014, and the NHANES dietary supplement databases were updated for every survey cycle. However, it should be noted that the number of pregnant women was much smaller in 2007-2014 cycles compared to 2000-2006 cycles when pregnant women were oversampled, which may have impacted the precision of the trend analyses. In addition, the number of lactating women was small even after combining multiple cycles, which contributed to the large SEs and imprecision of estimates. There is a need to further examine supplement use during lactation with a larger sample. Another limitation is that the NHANES database relies on manufacturer’s label declarations, which may exceed the label declarations 20% or more (38). Studies supporting the Dietary Supplement Ingredient Database have been chemically analyzing the nutrient contents of dietary supplements, including prenatal supplements. This database should be used to adjust labeled amounts in future research once it’s completely developed (38). Little is known about the reporting bias and measurement error structure of dietary supplements (17). Future studies may also examine biomarkers in relation to supplement use (5, 10). Lastly, NHANES did not collect information about multiple gestational pregnancies or risk factors, such as history of neural tube defects and MTHFR gene polymorphism, which should be considered when assessing individual’s nutritional needs.
In conclusion, the majority of pregnant and lactating women in the U.S. took at least one dietary supplement at some time during their pregnancy, which contributed many nutrients (e.g., thiamin, riboflavin, niacin, folic acid, vitamins B6, B12, and C, iron, and zinc) in doses above the RDA among users. While folic acid and iron supplementation is recommended during pregnancy, some supplement users may consume high doses that lead to excessive intakes. However, some of these high doses may be appropriate because they were recommended by health care providers due to special medical conditions. The use of supplements containing iodine, magnesium, and choline was relatively low among all women of reproductive age, regardless of pregnancy or lactation status. Less than half pregnant and lactating women were taking at least one supplement based on a health care provider’s recommendation. Health care professionals should be aware of and communicate information about nutrition and dietary supplement use, especially for folic acid and iron. The American College of Obstetricians and Gynecologists and the American Society for Reproductive Medicine recommend that women who present for prepregnancy counseling should be screened for their diet and supplements to ensure they are meeting the RDAs for essential nutrients (33). However, the lowest prevalence of dietary supplement use remains among women in the first trimester of pregnancy.
Supplementary Material
Acknowledgement:
This work was supported by National Institutes of Health/National Cancer Institute (U01CA215834). The authors thank Cria Perrine, PhD, at Centers for Disease Control and Prevention for scientific contribution to this work.
Financial Disclosure: Unrelated to this submission, Regan L. Bailey has served as a consultant in the past to the NIH Office of Dietary Supplements, Nestlé, the General Mills Bell Institute, RTI International, and Nutrition Impact; and is a trustee of the International Food Information Council and a board member of International Life Sciences Institute-North America. They have received travel support to present her research on dietary supplements. Johanna T. Dwyer has served an advisory board from McCormick Spice, The Mushroom Council, Bay State Milling, ConAgra Foods (until December 2018), and Nestlé, and editorial fees from Lippincott, Williams, and Wilkins/Wolters Kluwer Publishers, and holds stock in several food and drug companies. The other authors did not report any potential conflicts of interest.
Footnotes
Peer Review History
Peer reviews and author correspondence are available at http://links.lww.com/AOG/B704.
References
- 1.Institute of Medicine. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 2.U.S. Preventive Services Task Force. Folic acid for the prevention of neural tube defects: U.S. Preventive Services Task Force recommendation statement. Annals of internal medicine 2009;150(9):626–31. [DOI] [PubMed] [Google Scholar]
- 3.Procter SB, Campbell CG. Position of the Academy of Nutrition and Dietetics: nutrition and lifestyle for a healthy pregnancy outcome. J Acad Nutr Diet 2014;114(7):1099–103. [DOI] [PubMed] [Google Scholar]
- 4.AAP Committee on Fetus Newborn, ACOG Committee on Obstetric. Guidelines for Perinatal Care, 8th Edition: American Academy of Pediatrics; 2017. [Google Scholar]
- 5.Branum AM, Bailey R, Singer BJ. Dietary supplement use and folate status during pregnancy in the United States. J Nutr 2013;143(4):486–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sullivan KM, Ford ES, Azrak MF, Mokdad AH. Multivitamin use in pregnant and nonpregnant women: results from the Behavioral Risk Factor Surveillance System. Public health reports 2009;124(3):384–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta PM, Gahche JJ, Herrick KA, Ershow AG, Potischman N, Perrine CG. Use of Iodine-Containing Dietary Supplements Remains Low among Women of Reproductive Age in the United States: NHANES 2011-2014. Nutrients 2018;10(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bailey RL, Pac SG, Fulgoni VL 3rd, Reidy KC, Catalano PM. Estimation of Total Usual Dietary Intakes of Pregnant Women in the United States. JAMA network open 2019;2(6):e195967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cogswell ME, Kettel-Khan L, Ramakrishnan U. Iron supplement use among women in the United States: science, policy and practice. J Nutr 2003;133(6):1974s–7s. [DOI] [PubMed] [Google Scholar]
- 10.Gahche JJ, Bailey RL, Mirel LB, Dwyer JT. The prevalence of using iodine-containing supplements is low among reproductive-age women, NHANES 1999–2006. J Nutr 2013;143(6):872–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Center for Health Statistics. National Health and Nutrition Examination Survey: sample design,1999-2006. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2012. [Google Scholar]
- 12.National Center for Health Statistics. National Health and Nutrition Examination Survey: estimation procedures, 2011-2014. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2018. [Google Scholar]
- 13.National Center for Health Statistics. NHANES reponse rates and population totals. Available at: https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx#response-rates. Retrieved July 1, 2019.
- 14.Shaaban OM, Abbas AM, Abdel Hafiz HA, Abdelrahman AS, Rashwan M, Othman ER. Effect of pregnancy-lactation overlap on the current pregnancy outcome in women with substandard nutrition: a prospective cohort study. Facts, views & vision in ObGyn 2015;7(4):213–21. [PMC free article] [PubMed] [Google Scholar]
- 15.Bailey RL, Gahche JJ, Miller PE, Thomas PR, Dwyer JT. Why US adults use dietary supplements. JAMA internal medicine 2013;173(5):355–61. [DOI] [PubMed] [Google Scholar]
- 16.National Center for Health Statistics. National Health and Nutrition Examination Survey 2013-2014 data documentation, codebook, and frequencies: dietary supplement use 30-Day, total dietary supplements. Available at https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/DSQTOT_H.htm. Retrieved July 10, 2019.
- 17.Bailey RL, Dodd KW, Gahche JJ, Dwyer JT, Cowan AE, Jun S, et al. Best Practices for Dietary Supplement Assessment and Estimation of Total Usual Nutrient Intakes in Population-Level Research and Monitoring. J Nutr 2019; 149(2):181–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Institute of Medicine. Dietary Reference Intakes: Applications in Dietary Assessment. Washington, DC: The National Academies Press; 2000. [PubMed] [Google Scholar]
- 19.Institute of Medicine. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington (DC): National Academies Press; 1998. [PubMed] [Google Scholar]
- 20.Saldanha LG, Dwyer JT, Andrews KW, Brown LL, Costello RB, Ershow AG, et al. Is Nutrient Content and Other Label Information for Prescription Prenatal Supplements Different from Nonprescription Products? J Acad Nutr Diet 2017;117(9):1429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U.S. Food and Drug Administration. Converting Units of Measure for Folate, Niacin, and Vitamins A, D, and E on the Nutrition and Supplement Facts Labels: Guidance for Industry. Available at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-converting-units-measure-folate-niacin-and-vitamins-d-and-e-nutrition-and. Retrieved September 2, 2019.
- 22.Bailey RL, Dodd KW, Gahche JJ, Dwyer JT, McDowell MA, Yetley EA, et al. Total folate and folic acid intake from foods and dietary supplements in the United States: 2003-2006. Am J Clin Nutr 2010;91(1):231–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception 2011;84(5):478–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nguyen P, Thomas M, Koren G. Predictors of prenatal multivitamin adherence in pregnant women. J Clin Pharmacol 2009;49(6):735–42. [DOI] [PubMed] [Google Scholar]
- 25.Lamers Y, MacFarlane AJ, O’Connor DL, Fontaine-Bisson B. Periconceptional intake of folic acid among low-risk women in Canada: summary of a workshop aiming to align prenatal folic acid supplement composition with current expert guidelines. Am J Clin Nutr 2018;108(6):1357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. WHO Recommendations on antenatal Care for a Positive Pregnancy Experience. Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- 27.Center for Disease Control and Diseases. Recommendations to prevent and control iron deficiency in the United States. MMWR Morb Mortal Wkly Rep 1998;47(Rr-3):1–29. [PubMed] [Google Scholar]
- 28.Institute of Medicine. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington. DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 29.Perrine CG, Herrick K, Serdula MK, Sullivan KM. Some subgroups of reproductive age women in the United States may be at risk for iodine deficiency. J Nutr 2010;140(8):1489–94. [DOI] [PubMed] [Google Scholar]
- 30.Becker DV, Braverman LE, Delange F, Dunn JT, Franklyn JA, Hollowell JG, et al. Iodine supplementation for pregnancy and lactation-United States and Canada: recommendations of the American Thyroid Association. Thyroid 2006;16(10):949–51. [DOI] [PubMed] [Google Scholar]
- 31.Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, et al. 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 2017;27(3):315–89. [DOI] [PubMed] [Google Scholar]
- 32.Marra MV, Bailey RL. Position of the Academy of Nutrition and Dietetics: Micronutrient Supplementation. J Acad Nutr Diet 2018;118(11):2162–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 762: Prepregnancy Counseling. Obstetrics & Gynecology 2019;133(1):228–30. [DOI] [PubMed] [Google Scholar]
- 34.Tessema J, Jefferds ME, Cogswell M, Carlton E. Motivators and barriers to prenatal supplement use among minority women in the United States. J Am Diet Assoc 2009;109(1):102–8. [DOI] [PubMed] [Google Scholar]
- 35.Shaikh U, Byrd RS, Auinger P. Vitamin and mineral supplement use by children and adolescents in the 1999-2004 National Health and Nutrition Examination Survey: relationship with nutrition, food security, physical activity, and health care access. Arch Pediatr Adolesc Med 2009;163(2):150–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khalil A, Syngelaki A, Maiz N, Zinevich Y, Nicolaides KH. Maternal age and adverse pregnancy outcome: a cohort study. Ultrasound Obstet Gynecol 2013. December;42(6):634–43. [DOI] [PubMed] [Google Scholar]
- 37.Mayo Clinic. Pregnancy after 35: Healthy moms, healthy babies. Available at: https://www.mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/pregnancy/art-20045756. Retrived Aug 12, 2019.
- 38.Andrews KW, Gusev PA, McNeal M, Savarala S, Dang PTV, Oh L, et al. Dietary Supplement Ingredient Database (DSID) and the Application of Analytically Based Estimates of Ingredient Amount to Intake Calculations. J Nutr 2018;148(suppl_2):1413s–21s. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


