ABSTRACT
Background
In light of the publications (2008–2014) linking calcium intake, mainly from supplements, to the elevated risk of cardiovascular events, there is a need to determine if there have been any changes in usual intakes of calcium among Canadians.
Objective
We aimed to examine changes in dietary and total usual intake of calcium among Canadians aged ≥1 y over the period 2004–2015.
Methods
We used nutrition data from 2 nationally representative surveys conducted in 2004 and 2015 (CCHS 2004 Cycle 2.2 and CCHS-Nutrition 2015). This study included all the Canadians across 10 provinces, and the analyses were performed across different age/sex groups. We used the National Cancer Institute (NCI) method to estimate the usual intake of calcium and the prevalence of calcium inadequacy. Multiple logistic regression was performed to assess the relation between supplement uses and sociodemographic variables.
Results
From 2004 to 2015, the usual intake of calcium from food sources significantly decreased in calcium supplement nonusers (from 872 ± 18.2 mg/d to 754 ± 18.0 mg/d), but not in calcium supplement users. The contribution of calcium from the Milk and alternatives food group significantly decreased by 7.5% and 6.1% in calcium supplement users and nonusers, respectively. The prevalence of calcium supplement use significantly decreased from 2004 to 2015 in the Canadian population, from 27.5% to 22.0%. During this time, the percentage contribution of calcium from supplemental sources significantly decreased among Canadians, especially women. The prevalence of calcium inadequacy increased from 58.0% to 68.0% in supplement nonusers; however, among users of calcium supplements, the prevalence of calcium inadequacy remained at ∼31%.
Conclusions
Calcium intake from both food and supplemental sources decreased in the Canadian population over an 11-y period, which must be addressed by policy-makers in their efforts to decrease the high prevalence of calcium inadequacy.
Keywords: calcium, supplement use, usual intake, Canadians, prevalence of inadequacy
Introduction
Calcium is the most abundant mineral in the human body, accounting for almost 40% of total mineral mass (1). Overall, more than 99% of this micronutrient is stored in the skeleton and teeth, as calcium phosphate. The remaining 1% is freely available in the blood, extracellular fluid, and soft tissues, where it plays important roles in a variety of physiological functions (1). Because the human body is not able to synthesize minerals, calcium must be included in the diet at appropriate levels. Based on bone health outcomes, the Institute of Medicine (IOM), in collaboration with the American and Canadian governments, established the most recent DRIs for calcium in 2011 (2, 3). Milk and milk products are the most readily available dietary sources of calcium, whereas major nondairy sources of this mineral are green leafy vegetables, grains, cereals, and legumes (4, 5). In addition, calcium supplements and calcium-fortified foods such as soya milk and orange juice can be excellent sources of this micronutrient (5).
Ensuring adequate intake of calcium throughout the lifespan, through dietary sources, through fortified foods or by supplementation is essential to maximize peak bone mass, to prevent osteoporosis, and to decrease the risk of fractures (6, 7). Calcium appears to have nonskeletal beneficial effects on human health. Some studies have suggested that adequate calcium intake may decrease the risk of gestational hypertension (8), colorectal cancer (9), and premenstrual syndrome (10), with other purported effects being inconclusive (11). Further, in recent years, there has been increasing evidence linking high calcium intake, mainly from supplements, to the elevated risk of cardiovascular disease events (12–15); however, not all studies are in agreement (16, 17).
Through use of data from the NHANES, the dietary (foods and beverages) and supplemental calcium intakes of Americans have been continuously reported over the past several decades (18, 19). In Canada, we previously showed trends in dietary calcium intake of Canadian adults from 1970–1972 to 2004 with use of data from the Nutrition Canada survey and the Canadian Community Health Survey Cycle 2.2 (CCHS 2.2). During this time period, there was a moderate increase in mean calcium intake for men and a large increase for women, especially women aged <51 y (20). Despite improved fortification and supplement use during that time, the mean calcium intake in 2004 remained below recommended amounts in most age and sex groups (20). There are no reports available in the literature determining if there has been a shift in dietary or supplemental intakes of calcium in Canada, in light of recent evidence of adverse effects of calcium intake (12–15).
In the present study, our first objective was to examine changes in dietary and total usual calcium intake in the Canadian population over time with nutrition data from 2 nationally representative surveys conducted in 2004 and 2015. Secondly, we aimed to 1) assess the contribution of each food group to usual dietary calcium intake, 2) report the prevalence of calcium inadequacy among both calcium supplement users and nonusers, and 3) determine factors associated with calcium supplement use in 2004 and 2015.
Methods
Study population
This study is based on nutrition data from the CCHS 2.2 (CCHS 2004) and CCHS Nutrition in 2015. Both data sets are cross-sectional surveys, representing Canadians who reside in the 10 provinces. Data were collected at 2 time points, day 1 and day 2, with a 24-h dietary recall method. The total sample sizes for 2015 day 1 and day 2 were 20,487 and 7623, and the total sample sizes for 2004 day 1 and day 2 were 35,107 and 10,786, respectively. In both sets of survey data, the respondents reported detailed information on their food consumption in terms of time, location, and weight of food consumed. Some additional questions related to sociodemographic status such as age, sex, area of residence, immigration status, BMI, food security status, smoking status, education status, etc., were also asked. Dietary (24-h recall) data were collected with the Automated Multiple Pass Method on the first day and by a telephone interview on the second day. The proxy interview method was used to collect the data for children aged 1–6 y, children aged 6–12 y participated with parental guidance, and individuals aged ≥12 y were interviewed through use of a nonproxy method (21, 22). Permission to access and conduct analyses of CCHS 2004 and 2015 data were obtained from the Research Data Center Program of Statistics Canada (21, 23).
Analytical sample
This study included results from 30,074,236 individuals (weighted frequency) in 2004 and 33,946,610 individuals (weighted frequency) in 2015. We excluded children aged <1 y, pregnant and lactating women, individuals who did not report any food intake in the 24-h recall, and individuals who reported daily caloric intake outside the range of 200–8000 kcal. Individuals with extreme positive high intakes of nutrients were excluded from the study. For the 2004 and 2015 data sets, similar exclusion criteria were applied.
Dietary and supplemental calcium
During the 24-h recall (both 2004 and 2015), the respondents reported the type of food, amount of food, food occasion and location, and dietary supplement intake. In 2015, information was collected for any supplement consumption in the last 24 h. Additional information on supplement intake was obtained, such as frequency of supplement intake, amount of supplement intake, etc. In 2004, no information about supplement intake was available for the last 24 h. Supplement information was available for the 30 d before the day of the interview. Similar to 2015, details concerning supplement use such as dose, frequency of intake over the last 30 d, duration of use, etc., were obtained.
Definitions and covariates
A calcium supplement user was defined as any individual who reported taking any supplements that contain calcium, and calcium supplement nonusers were defined as those who did not report taking any supplements that contain calcium. Categorical variables used were: DRI age groups, food security (yes, no), university degree (yes, no), area of residence (urban, rural), household income (deciles 1–5, deciles 6–10), and chronic conditions (yes, no), unless otherwise specified. The variable chronic condition was categorized as “yes” if any individuals reported having any of the following diseases: diabetes, heart disease, cancer, osteoporosis, hypertension, and as “no” if any individual did not report having any of these diseases. The calcium contributions from 5 food groups and enriched beverages were determined. The 5 food groups included: “Vegetables and fruit,” “Grain products” (whole grain and non-whole grain), “Milk and alternatives” (fluid milk, fortified soy beverages, other milk alternatives), “Meat and alternatives” [beef, game and organ meat, other meats (pork, veal, lamb), legumes, nuts and seeds, eggs, processed meats, poultry, fish, shellfish], and “Other food and beverages.”
Statistical analyses
Analyses were performed with SAS, version 9.4. To produce population-level estimates, weighting and bootstrapping weights were used according to the recommendations of Statistics Canada (22). For comparison of results between 2004 and 2015, the absence of overlapping 95% CI concept was applied (24). α was set at 0.05. Values are presented as percentage ± SE or mean ± SE as appropriate. The association between supplement use and age, sex, income, education, food security, chronic conditions, and area of residence was evaluated with a multiple logistic regression model. To assess the percentages of the population who reported consuming calcium supplements by DRI age groups, descriptive analysis was carried out. In addition, we determined the contribution of 5 main food groups [i.e., “Vegetables and fruit,” “Grain products,” “Milk and alternatives,” “Meat and alternatives,” “Other food and beverages,” and “enriched beverages,” based on Canada's Food Guide (25)] to daily calcium intake.
To obtain the usual intake and prevalence of inadequacy of calcium, the NCI method was used (26). Two models can be used to calculate the usual intake: the amount model and the probability model. The amount model can be used to estimate the usual intake of the nutrients/food that are consumed daily and the probability model can be used to estimate the usual intake of the nutrients/food that are consumed episodically. Because calcium is 1 of the nutrients that is consumed daily, we used the amount model to estimate the usual intake of calcium (27). As supplement information for CCHS 2004 was available based on the last 30 d, we applied the “shrink and add” method for CCHS 2004, and we used “add and shrink” for CCHS 2015 as supplement information was available based on previous days in CCHS 2015 (28). For the NCI analysis, the following covariates were used for both CCHS 2004 and 2015 data:
the sequence of the 24-h recall, categorized as day 1 or day 2;
the day of the week when the 24-h recall data were obtained, categorized as weekdays and weekends;
energy consumption from food during the 24-h recall;
age/sex groups.
SAS macros developed by the NCI (29) were used for the usual intake and prevalence of inadequacy estimation. Further details about the NCI method and SAS macros can be found at the NCI website (26).
Results
Change in dietary and total usual calcium intake
Table 1 reports 11-y changes in dietary and total usual calcium intake and the prevalence of inadequacy among both calcium supplement users and nonusers, by age- and sex-specific groups. The usual dietary intake of calcium significantly decreased (P < 0.05) among children and adolescents in 2015 compared to 2004. The usual intake of calcium from food sources significantly decreased (P < 0.05) from 870 ± 18.2 mg/d (2004) to 755 ± 18.0 mg/d (2015) (all age/sex groups combined) among calcium supplement nonusers. Total usual intake of calcium (food + supplement) significantly decreased (P < 0.05) only in women aged 51–70 y from 1325 ± 35 mg/d in 2004 to 1120 ± 47 mg/d in 2015 among calcium supplement users (Table 1).
TABLE 1.
Intake of calcium and prevalence of calcium inadequacy among Canadian supplement users and nonusers across age/sex groups in 2004 and 20151
| Nonusers – 2004 (n = 21,791,146) | Nonusers – 2015 (n = 26,490,290) | Users – 2004 (n = 8,283,091) | Users – 2015 (n = 7,456,320) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age and sex groups | n (2004)2 | n (2015)2 | Calcium from food, mg/d3 | % below EAR3 | Calcium from food, mg/d | % below EAR3 | Calcium from food, mg/d | Calcium from food and supplement, mg/d | % below EAR3 | Calcium from food, mg/d | Calcium from food and supplement, mg/d | % below EAR3 |
| Children, 1–8 y4 | 2,734,217 | 3,032,727 | 900 ± 19.4 | 29.8 ± 1.9 | 770 ± 6.2* | 42.1 ± 0.8† | 865 ± 31.9 | 1000 ± 32.1 | 22.5 ± 3.0 | 820 ± 46.8 | 935 ± 47.9 | 28.6 ± 4.3 |
| Females | ||||||||||||
| 9–13 y | 986,719 | 884,165 | 930 ± 21.1 | 72.9 ± 1.9 | 840 ± 14.6 | 81.5 ± 0.9† | 960 ± 44.0 | 1100 ± 44.9 | 59.4 ± 3.9 | 865 ± 49.2 | 1030 ± 49.5 | 52.0 ± 5.9 |
| 14–18 y | 1,003,028 | 939,325 | 900 ± 20.1 | 75.9 ± 1.6 | 770 ± 18.1* | 85.7 ± 1.3† | 900 ± 36.4 | 1100 ± 38.8 | 58.5 ± 3.5 | 840 ± 49.0 | 1080 ± 51.4 | 51.2 ± 1.3 |
| 19–30 y | 2,265,199 | 2,001,527 | 790 ± 21.6 | 59.9 ± 2.3 | 680 ± 19.0 | 72.7 ± 2.1 | 820 ± 35.2 | 1180 ± 48.8 | 26.9 ± 3.1 | 810 ± 62.4 | 1120 ± 66.3 | 24.2 ± 4.5 |
| 31–50 y | 4,661,815 | 5,149,851 | 720 ± 19.7 | 67.1 ± 2.3 | 640 ± 30.3 | 77.5 ± 3.6 | 750 ± 30.2 | 1170 ± 42.0 | 28.4 ± 2.9 | 705 ± 34.2 | 1080 ± 43.8 | 27.0 ± 3.3 |
| 51–70 y | 3,261,795 | 4,596,352 | 620 ± 16.2 | 90.9 ± 1.0 | 570 ± 13.9 | 93.8 ± 0.5 | 685 ± 26.2 | 1325 ± 35.1 | 35.0 ± 2.3 | 690 ± 34.2 | 1120 ± 47.0* | 44.0 ± 4.3 |
| ≥71 y | 1,431,158 | 1,847,518 | 540 ± 16.3 | 95.5 ± 0.7 | 500 ± 23.0 | 97.2 ± 0.5 | 600 ± 23.4 | 1160 ± 31.9 | 46.0 ± 2.7 | 600 ± 30.4 | 1090 ± 46.4 | 46.9 ± 4.6 |
| Males | ||||||||||||
| 9–13 y | 1,042,184 | 930,541 | 1130 ± 26.7 | 57.7 ± 2.0 | 930 ± 9.0* | 73.0 ± 0.9† | 1150 ± 63.6 | 1300 ± 63.9 | 43.8 ± 3.9 | 985 ± 66.1 | 1100 ± 61.8 | 46.1 ± 9.3 |
| 14–18 y | 1,050,793 | 999,614 | 1250 ± 32.2 | 50.8 ± 2.0 | 1040 ± 13.5* | 66.0 ± 2.2† | 1310 ± 72.1 | 1514 ± 76.6 | 35.7 ± 4.4 | 1250 ± 111.6 | 1380 ± 98.1 | 30.1 ± 3.2 |
| 19–30 y | 2,579,898 | 2,403,390 | 1130 ± 30.1 | 33.0 ± 2.1 | 965 ± 27.8 | 44.3 ± 1.8 | 1215 ± 75.5 | 1400 ± 75.4 | 20.5 ± 2.9 | 1390 ± 148.7 | 1570 ± 132.5 | 9.2 ± 2.9 |
| 31–50 y | 4,863,071 | 5,205,870 | 970 ± 26.1 | 45.0 ± 2.2 | 875 ± 18.0 | 51.7 ± 2.3 | 1040 ± 49.6 | 1260 ± 53.5 | 25.1 ± 3.3 | 910 ± 46.0 | 1245 ± 52.1 | 17.5 ± 2.7 |
| 51–70 y | 3,141,308 | 4,486,610 | 800 ± 21.1 | 59.6 ± 2.2 | 755 ± 26.5 | 64.1 ± 2.2 | 880 ± 40.7 | 1210 ± 47.7 | 27.4 ± 3.3 | 900 ± 50.7 | 1300 ± 47.0 | 18.4 ± 3.2 |
| ≥71 y | 1,053,052 | 1,469,120 | 650 ± 19.3 | 88.2 ± 1.4 | 615 ± 18.0 | 91.3 ± 1.2 | 740 ± 33.5 | 1170 ± 75.9 | 50.4 ± 3.9 | 750 ± 38.9 | 1230 ± 51.7 | 34.9 ± 4.0 |
| All ages | 30,074,237 | 33,946,610 | 870 ± 18.2 | 58.0 ± 1.6 | 755 ± 18.0* | 68.0 ± 1.7 | 840 ± 29.2 | 1220 ± 31.0 | 31.5 ± 2.2 | 795 ± 40.3 | 1165 ± 45.9 | 31.9 ± 3.3 |
Values are means ± SEs and the NCI analysis were conducted separately for 2004 and 2015 data sets (21, 23, 27). EAR, estimated average requirement; NCI, National Cancer Institute.
The n represents supplement users and nonusers combined for each age group.
The EAR for each age and sex group is in Supplemental Table 1.
Data reported are for collapsed age groups of children 1–3 y and children 4–8 y.
Significant differences (P < 0.05) between usual intakes from 2004 to 2015 were tested with a confidence interval overlapping technique (24).
Prevalence of calcium inadequacy in 2004 and 2015
Among calcium supplement nonusers, from 2004 to 2015, the prevalence of calcium inadequacy significantly increased (P < 0.05) in children and adolescents (Table 1). The prevalence of calcium inadequacy was much less in calcium supplement users than in nonusers. The percentage of individuals with usual calcium intake below the estimated average requirement (EAR) remained relatively unchanged from 2004 (31.5%) to 2015 (31.9%) (all ages).
The percentage of calcium supplement users with total usual calcium intake (food + supplement) above the upper level ranged from 0% to about 13% (women aged 51–70 y) in 2004 and from 0% to about 12% (men aged 19–30 y) in 2015 (data not shown).
Food sources of calcium in 2004 and 2015
The percentage contribution of food groups of Canada's Food Guide (2007) and enriched beverages to dietary calcium intake is reported in Table 2, both for 2004 and 2015. Among calcium supplement nonusers, the proportion of calcium obtained from Milk and alternatives and Grain products significantly decreased (P < 0.05) by 6.1% and 0.6%, respectively, between 2004 and 2015. Conversely, the percentage contribution of “Vegetables and fruit,” “Meat and alternatives,” “enriched beverages,” and “other foods and beverages” significantly increased (P < 0.05) from 2004 to 2015. Similar trends were observed in calcium supplement users; however, there were no significant changes in the percentage contribution of “Grain products” and “Meat and alternatives” (Table 2).
TABLE 2.
Contribution (%) of enriched beverages and food groups of Canada's Food Guide to dietary calcium intake in calcium supplement users and nonusers among Canadians in 2004 and 20151
| 2004 | 2015 | |||
|---|---|---|---|---|
| Food groups | Supplement non-users (n = 21,791,146) | Supplement users (n = 8,283,091) | Supplement non-users (n = 26,490,290) | Supplement users (n = 7,456,320) |
| Vegetables and fruit | 9.6 ± 0.1 | 10.6 ± 0.2 | 10.5 ± 0.2* | 11.6 ± 0.4† |
| Grain products | 13.3 ± 0.1 | 12.0 ± 0.2 | 12.7 ± 0.2* | 11.8 ± 0.4 |
| Milk and alternatives2 | 47.1 ± 0.4 | 45.7 ± 0.5 | 41.0 ± 0.4* | 38.2 ± 0.9† |
| Meat and alternatives3 | 6.3 ± 0.1 | 7.1 ± 0.2 | 6.8 ± 0.2* | 7.5 ± 0.4 |
| Other foods and beverages | 8.0 ± 0.1 | 8.6 ± 0.2 | 9.8 ± 0.2* | 11.6 ± 0.4† |
| Enriched beverages | 0.6 ± 0.1 | 1.3 ± 0.1 | 1.7 ± 0.1* | 2.4 ± 0.3† |
Values are means ± SEs and the analyses were conducted separately for 2004 and 2015 data sets (21, 23).
Milk and alternatives food group includes fluid milk, fortified soy beverages, other milk alternatives.
Meat and alternatives food group includes beef, game and organ meat, other meats (pork, veal, lamb), legumes, nuts and seeds, eggs, processed meats, poultry, fish, shellfish.
Significant differences (P < 0.05) in contribution of calcium from food groups between CCHS 2004 and 2015 among supplement nonusers were tested with use of a confidence interval overlapping technique (24).
Significant differences (P < 0.05) in contribution of calcium from food groups between CCHS 2004 and 2015 among supplement users were tested with use of a confidence interval overlapping technique (24).
Percentages of calcium obtained from supplemental sources in 2004 and 2015
There was a significant decrease (P < 0.05) in the percentage of calcium obtained from supplemental sources not just for the adolescent females, but also for women up to age 70 y and for men aged 19–30 y and 51–70 y (Table 3). The percentage contribution of supplemental sources of calcium to daily intake significantly decreased (P < 0.05) from 29.0% in 2004 to 26.8% in 2015 among calcium supplement users in all age groups (Table 3).
TABLE 3.
Percentages of calcium obtained from supplemental sources among calcium supplement users across age/sex groups of Canadians in 2004 and 20151
| 2004 | 2015 | |||
|---|---|---|---|---|
| Age and sex groups | n | % | n | % |
| Children2 | ||||
| 1–3 y | 693,228 | 13.6 ± 0.8 | 376,484 | 14.1 ± 3.0 |
| 4–8 y | 14.4 ± 0.6 | 11.6 ± 1.3 | ||
| Females | ||||
| 9–13 y | 171,332 | 13.5 ± 0.9 | 100,994 | 11.2 ± 2.3 |
| 14–18 y | 148,385 | 20.9 ± 1.6 | 86,898 | 15.3 ± 2.2* |
| 19–30 y | 140,666 | 28.4 ± 1.9 | 357,322 | 18.8 ± 3.1* |
| 31–50 y | 147,321 | 31.9 ± 1.2 | 1,187,668 | 28.0 ± 1.8* |
| 51–70 y | 473,677 | 42.3 ± 1.0 | 1,911,359 | 34.3 ± 1.5* |
| ≥70 y | 530,612 | 41.5 ± 1.1 | 744,350 | 43.1 ± 1.6 |
| Males | ||||
| 9–13 y | 953,905 | 12.7 ± 0.7 | 92,969 | 9.6 ± 1.7 |
| 14–18 y | 1,557,999 | 15.2 ± 1.1 | 78,315 | 15.9 ± 3.8 |
| 19–30 y | 908,912 | 16.4 ± 1.4 | 325,322 | 7.1 ± 1.7* |
| 31–50 y | 1,612,317 | 19.9 ± 1.3 | 877,011 | 19.3 ± 2.2 |
| 51–70 y | 286,693 | 27.8 ± 1.3 | 998,269 | 23.2 ± 1.5* |
| ≥70 y | 658,044 | 30.4 ± 1.5 | 319,359 | 32.9 ± 1.8 |
| All ages | 8,283,091 | 29.0 ± 0.4 | 7,456,320 | 26.8 ± 0.7* |
Values are means ± SEs and the analyses were conducted separately for 2004 and 2015 data sets (21, 23).
The total n for children aged 1–8 y.
Significant differences (P < 0.05) in % contributions between 2004 and 2015 by age groups were tested with use of a confidence interval overlapping technique (24).
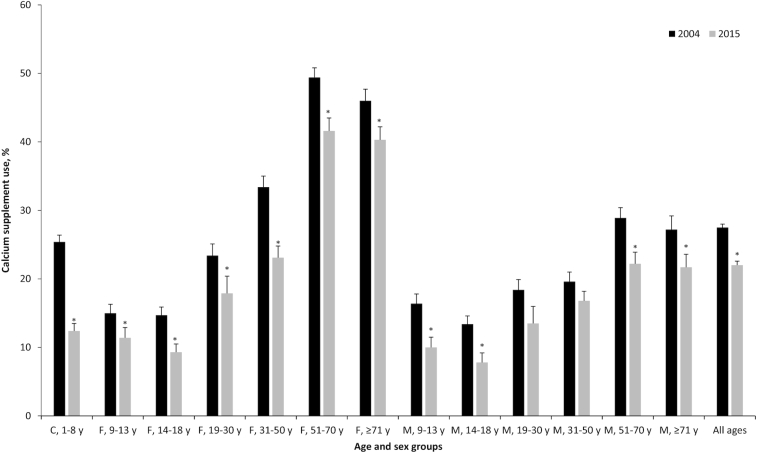
Prevalence of calcium supplement use in 2004 and 2015
From 2004 to 2015, the prevalence of calcium supplement use significantly decreased (P < 0.05) in all age and sex groups, except adult men aged 19–30 and 31–50 y (Figure 1). Overall, the percentage of calcium supplement use in the Canadian population significantly decreased (P < 0.05) from 27.5% in 2004 to 22.0% in 2015.
FIGURE 1.
Prevalence of calcium supplement use in 2004 and 2015 across age-specific and sex-specific groups of Canadians. Values are represented as percentages ± SEs. Data are represented for children in collapsed DRI age groups of children aged 1–3 and 4–8 y. Analyses were conducted separately for 2004 (n = 8,283,091) and 2015 (n = 7,456,320) data sets (21, 23). *Significant differences (P < 0.05) of supplement users between 2004 and 2015 by age groups were tested with use of a confidence interval overlapping technique (24). n of each age/sex group for 2004: C: 1–8 y: 693,228; F: 9–13 y: 171,332, 14–18 y: 148,385, 19–30 y: 140,666, 31–50 y: 147,321, 51–70 y: 473,677, ≥70 y: 530,612; M: 9–13 y: 953,905, 14–18 y: 1,557,999, 19–30 y: 908,912, 31–50 y: 1,612,317, 51–70 y: 286,693, ≥70 y: 658,044; All age: 8,283,091. n of each age/sex group for 2015: C: 1–8 y: 376,484; F: 9–13 y: 100,994, 14–18 y: 86,898, 19–30 y: 357,322, 31–50 y: 1,187,668, 51–70 y: 1,911,359, ≥70 y: 744,350; M: 9–13 y: 92,969, 14–18 y: 78,315, 19–30 y: 325,322, 31–50 y: 877,011, 51–70 y: 998,269, ≥70 y: 319,359; All age: 7,456,320. C, children; M, male; F, female.
Factors associated with calcium supplement use in 2004 and 2015
Table 4 lists the potential factors associated with calcium supplement use in 2004 and 2015. The odds of taking a calcium supplement were 2.3 times greater among children aged 1–8 y than males aged 14–18 y (as the reference group) in 2004. The odds of calcium supplement use were 6.8 times and 2.7 times greater among women and men aged 51–70 y, respectively, than men aged 19–30 y (as the reference group) in 2015. Overall, being female and older age were associated with higher odds of calcium supplement use in both 2004 and 2015. In addition, having a university degree was associated with higher odds of calcium supplement use than those with no university degree in 2004 (OR: 1.3; 95% CI: 1.2, 1.4) and 2015 (OR: 1.2; 95% CI: 1.06, 1.5). Living in urban areas was associated with higher odds of calcium supplement use than living in rural areas (OR: 1.1; 95% CI: 1.01, 1.3 in 2004 and OR: 1.4; 95% CI: 1.1, 1.7 in 2015). Being food secure or having a chronic condition was associated with higher odds of taking a calcium supplement in 2015 but not 2004. Compared with Canadians in lower-income deciles, those in higher-income deciles had 1.4 times (95% CI: 1.2–1.5) higher odds of calcium supplement use in 2004. However, this association no longer existed in 2015 (Table 4).
TABLE 4.
Factors associated with calcium supplement use in 2004 and 2015 among Canadians across age/sex groups1
| 2004 | 20152 | |||
|---|---|---|---|---|
| Sociodemographic variables | n | OR (95% CI) | n | OR (95% CI) |
| Age and sex groups | ||||
| Children | ||||
| 1–8 y3 | 693,228 | 2.3* (1.9, 2.9) | 376,484 | — |
| Female | ||||
| 9–13 y | 148,385 | 1.3 (0.9, 1.7) | 100,994 | — |
| 14–18 y | 147,321 | 1.1 (0.9, 1.5) | 86,898 | — |
| 19–30 y | 530,612 | 2.1* (1.6, 2.7) | 357,322 | 1.4 (0.8, 2.4) |
| 31–50 y | 1,557,999 | 3.4* (2.6, 4.4) | 1,187,668 | 1.8* (1.2, 2.9) |
| 51–70 y | 1,612,317 | 6.8* (5.3, 8.8) | 1,911,359 | 4.2* (2.7, 6.5) |
| ≥71 y | 658,044 | 6.6* (4.9, 8.8) | 744,350 | 4.0* (2.5, 6.5) |
| Male | ||||
| 9–13 y | 171,332 | 1.4* (1.01, 1.8) | 92,969 | — |
| 14–18 y4 | 140,666 | 1 | 78,315 | — |
| 19–30 y5 | 473,677 | 1.5* (1.1, 2.03) | 325,322 | 1 |
| 31–50 y | 953,905 | 1.6* (1.2, 2.2) | 877,011 | 1.2 (0.8, 1.9) |
| 51–70 y | 908,912 | 2.7* (2.1, 3.5) | 998,269 | 1.7* (1.06, 2.7) |
| ≥71 y | 286,693 | 2.7* (2.0, 3.7) | 319,359 | 1.6* (0.9, 2.6) |
| Education6,7 | ||||
| No university degree8 | 5,344,431 | 1 | 4,266,726 | 1 |
| A university degree | 2,811,808 | 1.3* (1.2, 1.4) | 3,188,858 | 1.2* (1.06, 1.5) |
| Food security status7,9 | ||||
| Insecure8 | 878,199 | 1 | 671,351 | 1 |
| Secure | 7,386,314 | 1.03 (0.9, 1.2) | 6,759,038 | 1.3* (1.03, 1.7) |
| Area of residence7,10 | ||||
| Rural8 | 1,361,183 | |||
| 1 | 1,135,711 | 1 | ||
| Urban | 6,921,908 | |||
| 1.1* (1.01, 1.3) | 6,320,609 | 1.4* (1.1, 1.7) | ||
| Income decile7,11 | ||||
| Decile 1–58 | 3,275,598 | 1 | 3,636,975 | 1 |
| Decile 6–10 | 4,245,769 | 1.4* (1.2, 1.5) | 3,819,345 | 1.1 (0.9, 1.3) |
| Chronic condition7,12 | ||||
| No8 | 6,344,515 | 1 | 4,266,452 | 1 |
| Yes | 1,934,803 | 1.03 (0.9, 1.2) | 2,452,416 | 1.3* (1.03, 1.5) |
Values are OR (95% CI) and multivariate logistic regression analyses were conducted separately for 2004 and 2015 data sets (21, 23).
Missing ORs for some DRI age groups in 2015 are a result of missing information on chronic conditions (as covariate for logistic regression) for children and adolescents aged <19 y.
The DRI age groups of children 1–3 and 4–8 y were merged and data presented for an age group of 1–8 y.
Reference group of OR male 14–18 y for 2004.
Reference group of OR male 19–30 y for 2015.
Education: “no university degree” if the individual did not have university degree, and “a university degree” if the individual had a university degree.
The total n of sociodemographic variables may vary because of missing values.
Reference group of OR.
Food security status: “insecure” if the individual was food insecure, and “secure” if the individual was food secure.
Area of residence: “rural” if the individual stayed in a rural area, and “urban” if the individual stayed in an urban area.
Income decile: “decile 1–5” if the individual's income is in decile 1, 2, 3, 4, or 5, and “decile 6–10” if the individual's income is in decile 6, 7, 8, 9, or 10.
Chronic condition is defined as yes/no depending on whether the individual has reported having any of the following diseases: diabetes, heart disease, cancer, osteoporosis, or hypertension.
Significant difference within categories when P < 0.05.
Discussion
This is the first study to report changes in dietary and total usual calcium intake in the Canadian population from 2004 to 2015, through use of nationally representative survey data. Overall, in both calcium supplement users and nonusers, the usual intake of calcium from the diet decreased from 2004 to 2015; however, this decrease was only statistically significant in calcium supplement nonusers. In parallel, the contribution of calcium from the Milk and alternatives food group significantly decreased among both calcium supplement users and nonusers from 2004 to 2015. Overall, the percentage contribution of calcium from supplemental sources significantly decreased from 29.0% to 26.8% among Canadians. This decrease was also statistically significant among females aged 14–18 y, 19–30 y, 31–50 y, and 51–70 y. However, in males, it was only statistically significant in 2 age groups (19–30 y and 51–70 y). The percentage of Canadians taking a calcium supplement significantly decreased from 27.5% in 2004 to 22.0% in 2015. Among calcium supplement nonusers, the prevalence of calcium inadequacy significantly increased in children and adolescents from 2004 to 2015. However, among users of calcium supplements, no significant changes were observed in the prevalence of calcium inadequacy in all age and sex groups in the last decade.
A number of national surveys have investigated the trends in dietary calcium intake in different populations (20, 30, 31). We previously showed that dietary calcium intake of Canadian adults increased from 1970 to 2004, with large increases (up to 215 mg/d) in women and moderate increases (up to 50 mg/d) in men (20). However, the results of the current analysis revealed that from 2004 to 2015, the usual intake of calcium from the diet decreased in both calcium supplement users (−41 mg/d) and nonusers (−118 mg/d). Recent estimates from NHANES also showed that the mean daily intake of dietary calcium decreased from 2009–2010 to 2015–2016 among both American men (−88 mg/d) and women (−57 mg/d) aged ≥2 y (18, 19). Other high-income countries have also shown marked decreases in calcium intake, namely Switzerland (30), Japan (31), and Germany (32).
Milk and milk products are major contributors to calcium intake in most population groups (19, 33–35), especially high-income countries. The observed downward trends in dietary calcium intake were likely a result of a general tendency toward decreasing consumption of dairy products, especially whole milk (36–38). Our data support this observation by showing that from 2004 to 2015, the contribution of calcium from the “Milk and alternatives” food group significantly decreased among Canadians. Although this was accompanied by the increased contribution of other dietary sources of calcium, especially enriched beverages and vegetables and fruit, calcium intake from foods overall fell. A recent report of trends in consumption of dairy products in the United States indicated that between 1970 and 2012, total pounds of dairy products available to eat or drink annually fell from 339.2 pounds/person to 275.9 pounds/person, and Canada is likely similar. This decline in dairy availability mostly stemmed from the decrease in whole milk availability, which dropped from 25.3 gallons/person in 1970 to 5.4 gallons/person in 2012 (36). In parallel, the contribution of milk and dairy to total calcium intake decreased from 50% in 1987–1988 to 37% in 2009–2010, which represents a 13% decrease (19, 39). In a review summarizing trends in dietary behavior and food choices in Finland from 1950 to 2006, it was found that the overall consumption of milk among the Finnish population decreased and shifted from whole milk to low-fat milk (38). This decrease in consumption of milk products and a shift in the type of milk consumed could result from concerns about increased fat intake. In this regard, Cashel et al. showed that eating foods low in fat was the most important health-related food habit among Australian women. Eating foods high in calcium was ranked third for younger women (<50 y), and fourth for older women (≥50 y) (40). Furthermore, elimination of the Milk and alternatives food group in the new 2019 Canada's Food Guide (41) may accelerate the downward trend in the consumption of dairy products and thereby reduce dietary intake of calcium even further.
Our results revealed that the Milk and alternatives food group was the major contributor to daily calcium intake among both supplement users (38.2%) and nonusers (41.0%), followed by Grain products, Vegetables and fruit, Meat and alternatives, and enriched beverages. In the United States, milk and dairy products were the major sources of calcium in the diet (37%). About 17% of total calcium intake was supplied by mixed dishes and 12% by grains. Other sources of calcium were nonalcoholic beverages other than milk (8%), snacks and sweets (7%), protein foods (5%), and vegetables (4%) (19).
We showed that from 2004 to 2015, the percentage contribution of calcium from supplemental sources significantly decreased among Canadians, especially women. A reduction in intake of high doses of supplemental calcium was also observed in the United States, where the prevalence of mean daily supplemental calcium intake at or exceeding the EAR decreased from 9.6% in 2003–2004 to 7.1% in 2013–2014 in women, and from 3.8% to 1.9% in men. Moreover, among calcium-containing supplement users, the mean daily supplemental calcium intake peaked in 2007–2008 at 397 mg/d, thereafter, decreasing to 360 mg/d in 2013–2014 (42). Furthermore, we found that the overall prevalence of calcium supplement use decreased by 5.5% among Canadians. This downward trend was also found in the United States, where the percentage of adults reporting use of calcium supplements decreased from 42% in 2003–2004 to 35% in 2011–2012 (43). The decline in the overall prevalence of calcium supplement use and the parallel decrease in the percentage contribution of supplemental calcium may be attributable to the results of the 2008–2014 publications linking calcium supplement use to increased risk of cardiovascular events (12–15). Moreover, Osteoporosis Canada has recommended getting enough calcium preferably through diet. If diet alone cannot provide the recommended daily intake of calcium, a supplement may assist (44). However, it is important to keep in mind that this downward trend in use/dose of calcium supplements may exacerbate the problem of calcium inadequacy, especially among those who have undergone a transition from being a calcium supplement user to a nonuser. It is well established that women are generally more health-conscious and have more nutrition knowledge than men (45–47), which may partly explain the greater impact of the recent shift in not recommending supplemental calcium on women.
Because of a decline in dietary calcium intake, the prevalence of calcium inadequacy increased from 58.0% in 2004 to 68.0% in 2015 in supplement nonusers. However, among users of calcium supplements, the prevalence of calcium inadequacy remained relatively unchanged (31.5% in 2004 compared with 31.9% in 2015). Our results showed that Canadian children were more likely to meet the EAR for calcium than Canadian adolescents. Moreover, the prevalence of calcium inadequacy tended to increase with age among Canadian adults. A study conducted in a representative sample of Spanish children aged 6–9 y showed that about 26% of the total sample had inadequate calcium intake, with girls presenting a significantly higher percentage than boys (29% compared with 22%) (48). Findings from the Korean National Health and Nutrition Examination Survey (KNHANES) 2007–2010 revealed that 75% of children and adolescents aged 1–18 y (79.1% of girls and 71.6% of boys) had inadequate Ca intake. The prevalence of calcium inadequacy increased significantly from toddlers (45–55%) to adolescents (78–86%) (49). Through use of data from the Australian National Nutrition and Physical Activity Survey 2011–2012, Rouf and colleagues reported that about 83% of adolescent males and 95% of adolescent females failed to meet the EAR for calcium; whereas for young adults 19–25 y, 69% of men and 83% of women did not meet the EAR (50). Although in our study, calcium supplement use was associated with a higher prevalence of meeting recommendations, many individuals (about 32%) failed to meet the EAR for calcium even with the help of supplements. Similarly, in a population-based cohort of Americans aged 45–84 y, nearly half of calcium supplement users did not meet the recommended dietary intake of calcium (51).
This study used nutrition data from 2 nationally representative surveys conducted in Canada with an interval of 11 y: CCHS 2004 (Cycle 2.2) survey and CCHS Nutrition 2015 survey. A major strength of this study was the opportunity to examine the changes in dietary and total calcium intakes, in the light of recent evidence on health-compromising effects of calcium supplementation. Moreover, to our knowledge, this is the first study to monitor the prevalence of inadequacy for calcium among Canadians over time. We also acknowledge some limitations to our study. In 2015, the information regarding calcium supplement use was collected in the previous 24 h, but in 2004 the information was available for the previous 30 d. Secondly, the amount of calcium from calcium-containing antacids was not taken into consideration when assessing the total usual calcium intake. Thirdly, caution should be used when comparing 2004 and 2015 results, because changes to the food booklet resulted in some portion size changes which mostly affected energy, tea, and coffee (52).
In conclusion, we examined changes in dietary and total usual calcium intakes among Canadians through use of 2 nationally representative surveys conducted in 2004 and 2015. Here, we found that dietary calcium intake of Canadians considerably decreased from 2004 to 2015, which may be attributable to the parallel decrease in the contribution of calcium from the Milk and alternatives food group. During these 11 y, the percentage contribution of calcium from supplemental sources significantly decreased among Canadians, especially women. The prevalence of calcium supplement use also significantly decreased among Canadians. This decreasing trend in consumption of dairy products and the use of calcium supplements should be taken into consideration by policy-makers in their efforts to decrease the high prevalence of calcium inadequacy.
Supplementary Material
Acknowledgments
We acknowledge Osteoporosis Canada for their support in knowledge translation activities related to this study. The authors’ responsibilities were as follows—HV and SJW: design of the study; NI and HV: formal analysis; HV, NI, MS, RPP and SJW: original draft preparation; HV and SJW: editing and review of the manuscript; and all authors: read and approved the final manuscript. Osteoporosis Canada is the collaborating partner for knowledge translation initiatives resulting from this study.
Notes
Supported by the Canadian Institutes of Health Research (Grant no. 418774).
Author disclosures: The authors report no conflict of interest.
Supplemental Table 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn.
Abbreviations used: CCHS, Canadian Community Health Survey; EAR, estimated average requirement; NCI, National Cancer Institute.
References
- 1. Sharma S, Sheehy T, Kolahdooz F.. Nutrition at a glance (2 edn). Oxford: Wiley-Blackwell;2015. [Google Scholar]
- 2. Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G et al.. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96(1):53–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. IOM. Dietary Reference Intakes for calcium and vitamin D. Washington (DC): The National Academy Press; 2011. [PubMed] [Google Scholar]
- 4. Preedy VR. Calcium: chemistry, analysis. Function and Effects: Royal Society of Chemistry; 2015. [Google Scholar]
- 5. Weaver CM, Heaney RP. Food sources, supplements, and bioavailability. Calcium in human health. Totowa (NJ): Humana Press; 2006, pp. 129–42. [Google Scholar]
- 6. Cashman K. Calcium intake, calcium bioavailability and bone health. Br J Nutr. 2002;87(S2):S169–77. [DOI] [PubMed] [Google Scholar]
- 7. Weaver CM, Alexander DD, Boushey CJ, Dawson-Hughes B, Lappe JM, LeBoff MS, Liu S, Looker AC, Wallace TC, Wang DD. Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation. Osteoporos Int. 2016;27(1):367–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hofmeyr GJ, Lawrie TA, Atallah AN, Duley L, Torloni MR. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2014(6):Cd001059. [DOI] [PubMed] [Google Scholar]
- 9. Bonovas S, Fiorino G, Lytras T, Malesci A, Danese S. Calcium supplementation for the prevention of colorectal adenomas: a systematic review and meta-analysis of randomized controlled trials. World J Gastroenterol. 2016;22(18):4594–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nevatte T, O'Brien PM, Backstrom T, Brown C, Dennerstein L, Endicott J, Epperson CN, Eriksson E, Freeman EW, Halbreich U et al.. ISPMD consensus on the management of premenstrual disorders. Arch Womens Ment Health. 2013;16(4):279–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Body JJ, Bergmann P, Boonen S, Devogelaer JP, Gielen E, Goemaere S, Kaufman JM, Rozenberg S, Reginster JY. Extraskeletal benefits and risks of calcium, vitamin D and anti-osteoporosis medications. Osteoporos Int. 2012;23(Suppl 1):S1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bolland MJ, Avenell A, Baron JA, Grey A, MacLennan GS, Gamble GD, Reid IR. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Asemi Z, Saneei P, Sabihi SS, Feizi A, Esmaillzadeh A. Total, dietary, and supplemental calcium intake and mortality from all-causes, cardiovascular disease, and cancer: a meta-analysis of observational studies. Nutr Metab Cardiovasc Dis. 2015;25(7):623–34. [DOI] [PubMed] [Google Scholar]
- 14. Xiao Q, Murphy RA, Houston DK, Harris TB, Chow WH, Park Y. Dietary and supplemental calcium intake and cardiovascular disease mortality: the National Institutes of Health-AARP diet and health study. JAMA Intern Med. 2013;173(8):639–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pentti K, Tuppurainen MT, Honkanen R, Sandini L, Kroger H, Alhava E, Saarikoski S. Use of calcium supplements and the risk of coronary heart disease in 52–62-year-old women: the Kuopio Osteoporosis Risk Factor and Prevention Study. Maturitas. 2009;63(1):73–8. [DOI] [PubMed] [Google Scholar]
- 16. Hsia J, Heiss G, Ren H, Allison M, Dolan NC, Greenland P, Heckbert SR, Johnson KC, Manson JE, Sidney S et al.. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115(7):846–54. [DOI] [PubMed] [Google Scholar]
- 17. Paik JM, Curhan GC, Sun Q, Rexrode KM, Manson JE, Rimm EB, Taylor EN. Calcium supplement intake and risk of cardiovascular disease in women. Osteoporos Int. 2014;25(8):2047–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. What We Eat in America. Nutrient intakes from food and beverages: mean amounts consumed per individual, by gender and age, in the United States, 2015–2016; [cited 2019 Apr 10]. [Internet]. Available from: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/1516/Table_1_NIN_GEN_15.pdf. [Google Scholar]
- 19. Hoy MK, Goldman J. Calcium intake of the US population, what we eat in America, NHANES 2009–2010. Food Surveys Research Group: Dietary Data Brief No 13 2014. [Google Scholar]
- 20. Vatanparast H, Dolega-Cieszkowski JH, Whiting SJ. Many adult Canadians are not meeting current calcium recommendations from food and supplement intake. Appl Physiol Nutr Metab. 2009;34(2):191–6. [DOI] [PubMed] [Google Scholar]
- 21. Statistics Canada. Canadian Community Health Survey (CCHS), Cycle 2.2 (2004): nutrition—general health (including vitamin & mineral supplements) & 24-hour dietary recall components; user guide, 2008 2008; [cited 2019 May 21]. [Internet]. Available from: http://www23.statcan.gc.ca:81/imdb-bmdi/pub/document/5049_D24_T9_V1-eng.pdf. [Google Scholar]
- 22. Statistics Canada. The Research Data Centres Information and Technical Bulletin—weighted estimation and bootstrap variance estimation for analyzing survey data: how to implement in selected software 2019; [cited 2019 Oct 1]. [Internet]. Available from: https://www150.statcan.gc.ca/n1/en/catalogue/12-002-X201400111901. [Google Scholar]
- 23. Health Canada. Reference guide to understanding and using the data 2017; [cited 2019 May 21]. [Internet]. Available from: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/reference-guide-understanding-using-data-2015.html. [Google Scholar]
- 24. Knezevic A. Overlapping confidence intervals and statistical significance. StatNews: Cornell University Statistical Consulting Unit. 2008;73(1). [Google Scholar]
- 25. Health Canada. Eating well with Canada's Food Guide 2007; [cited 2019 Jul 30]. [Internet]. Available from: https://www.canada.ca/en/health-canada/services/canada-food-guide/about/history-food-guide/eating-well-with-canada-food-guide-2007.html. [Google Scholar]
- 26. Centers for Disease Control and Prevention. NHANES dietary web data tutorial—advanced dietary analyses 2011; [cited 2019 May 21]. [Internet]. Available from: https://www.cdc.gov/nchs/tutorials/dietary/advanced/. [Google Scholar]
- 27. National Cancer Institute. Usual dietary intakes: details of the method 2018; [cited 2019 Oct 1]. [Internet]. Available from: https://epi.grants.cancer.gov/diet/usualintakes/details.html. [Google Scholar]
- 28. Bailey RL, Dodd KW, Gahche JJ, Dwyer JT, Cowan AE, Jun S, Eicher-Miller HA, Guenther PM, Bhadra A, Thomas PR et al.. Best practices for dietary supplement assessment and estimation of total usual nutrient intakes in population-level research and monitoring. J Nutr. 2019;149(2):181–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. National Cancer Institute. Usual dietary intakes: SAS macros for the NCI method 2018; [cited 2019 May 21]. [Internet]. Available from: https://epi.grants.cancer.gov/diet/usualintakes/macros.html. [Google Scholar]
- 30. Abreu D, Cardoso I, Gaspoz JM, Guessous I, Marques-Vidal P. Trends in dietary intake in Switzerland, 1999 to 2009. Public Health Nutr. 2014;17(3):479–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ohta H, Uenishi K, Shiraki M. Recent nutritional trends of calcium and vitamin D in East Asia. Osteoporos Sarcopenia. 2016;2(4):208–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Trautvetter U, Ditscheid B, Jahreis G, Glei M. Habitual intakes, food sources and excretions of phosphorus and calcium in three German study collectives. Nutrients. 2018;10(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Coudray B. The contribution of dairy products to micronutrient intakes in France. J Am Coll Nutr. 2011;30(5 Suppl 1):410s–4s. [DOI] [PubMed] [Google Scholar]
- 34. Vissers PA, Streppel MT, Feskens EJ, de Groot LC. The contribution of dairy products to micronutrient intake in the Netherlands. J Am Coll Nutr. 2011;30(5 Suppl 1):415s–21s. [DOI] [PubMed] [Google Scholar]
- 35. Mandic-Puljek M, Mandic ML, Perl A, Kenjeric D. Calcium intake, food sources and seasonal variations in eastern Croatia. Coll Antropol. 2005;29(2):503–7. [PubMed] [Google Scholar]
- 36. Bentley J. Trends in US per capita consumption of dairy products, 1970–2012. Amber Waves. U.S. Department of Agriculture, Economic Research Service; 2014; [cited 2019 Jul 18]. [Internet]. Available from: https://www.ers.usda.gov/amber-waves/2014/june/trends-in-us-per-capita-consumption-of-dairy-products-1970-2012/. [Google Scholar]
- 37. Lasater G, Piernas C, Popkin BM. Beverage patterns and trends among school-aged children in the US, 1989–2008. Nutr J. 2011;10:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mannisto S, Laatikainen T, Helakorpi S, Valsta LM. Monitoring diet and diet-related chronic disease risk factors in Finland. Public Health Nutr. 2010;13(6a):907–14. [DOI] [PubMed] [Google Scholar]
- 39. Fleming KH, Heimbach JT. Consumption of calcium in the U.S.: food sources and intake levels. J Nutr. 1994;124(8 Suppl):1426s–30s. [DOI] [PubMed] [Google Scholar]
- 40. Cashel K, Crawford D, Deakin V. Milk choices made by women: what influences them, and does it impact on calcium intake?. Public Health Nutr. 2000;3(4):403–10. [DOI] [PubMed] [Google Scholar]
- 41. Health Canada. Canada's food guide 2019; [cited 2019 Mar 28]. [Internet]. Available from: https://food-guide.canada.ca/en/. [Google Scholar]
- 42. Rooney MR, Michos ED, Hootman KC, Harnack L, Lutsey PL. Trends in calcium supplementation, National Health and Nutrition Examination Survey (NHANES) 1999–2014. Bone. 2018;111:23–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kantor ED, Rehm CD, Du M, White E, Giovannucci EL. Trends in dietary supplement use among US adults from 1999–2012. JAMA. 2016;316(14):1464–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Osteoporosis Canada. Calcium. 2017; [cited 2019 Jul 23] [Internet]. Available from: https://osteoporosis.ca/bone-health-osteoporosis/calcium-and-vitamin-d/calcium/. [Google Scholar]
- 45. Courtenay WH, McCreary DR, Merighi JR. Gender and ethnic differences in health beliefs and behaviors. J Health Psychol. 2002;7(3):219–31. [DOI] [PubMed] [Google Scholar]
- 46. Wardle J, Haase AM, Steptoe A, Nillapun M, Jonwutiwes K, Bellisle F. Gender differences in food choice: the contribution of health beliefs and dieting. Ann Behav Med. 2004;27(2):107–16. [DOI] [PubMed] [Google Scholar]
- 47. Parmenter K, Waller J, Wardle J. Demographic variation in nutrition knowledge in England. Health Educ Res. 2000;15(2):163–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rubio-Lopez N, Llopis-Gonzalez A, Pico Y, Morales-Suarez-Varela M. Dietary calcium intake and adherence to the Mediterranean diet in Spanish children: the ANIVA Study. Int J Environ Res Public Health. 2017;14(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Im JG, Kim SH, Lee GY, Joung H, Park MJ. Inadequate calcium intake is highly prevalent in Korean children and adolescents: the Korea National Health and Nutrition Examination Survey (KNHANES) 2007–2010. Public Health Nutr. 2014;17(11):2489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rouf AS, Sui Z, Rangan A, Grech A, Allman-Farinelli M. Low calcium intakes among Australian adolescents and young adults are associated with higher consumption of discretionary foods and beverages. Nutrition. 2018;55–56:146–53. [DOI] [PubMed] [Google Scholar]
- 51. Burnett-Hartman AN, Fitzpatrick AL, Gao K, Jackson SA, Schreiner PJ. Supplement use contributes to meeting recommended dietary intakes for calcium, magnesium, and vitamin C in four ethnicities of middle-aged and older Americans: the Multi-Ethnic Study of Atherosclerosis. J Am Diet Assoc. 2009;109(3):422–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Statistics Canada. Canadian Community Health Survey—nutrition user guide 2017; [cited 2019 Jul 23]. [Internet]. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=201486. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.