Abstract
Background:
Whether healthcare provider burnout contributes to lower quality of patient care is unclear.
Purpose:
To estimate the overall relationship between burnout and quality of care, and to evaluate if published studies provide exaggerated estimates of this relationship.
Data Sources:
MEDLINE, Embase, and Web of Science, with no language restrictions, from inception through May 28, 2019.
Study Selection:
Peer-reviewed publications published in any language that quantified healthcare provider burnout in relation to patient quality of care.
Data Extraction:
Two reviewers independently selected studies, extracted measures of association of burnout and quality of care, and assessed potential bias using the Ioannidis (excess significance) and Egger (small-study effect) tests.
Data Synthesis:
We screened 11,703 citations, selecting 123 publications with 142 study populations encompassing 241,553 healthcare providers. Relations between burnout and quality of care were highly heterogeneous (I2 93.4%−98.8%). Only 4 studies specified a primary outcome. Of 114 unique burnout and quality combinations, 58 indicated burnout related to poor quality of care, 6 indicated burnout related to high quality of care, and 50 showed no significant effect. Excess significance was apparent (73% observed vs 62% predicted studies with statistically significant results, P = 0.011), with this indicator of potential bias most prominent for the least rigorous quality measures of Best Practices and Quality and Safety.
Limitations:
Primarily observational studies; unable to determine causality or directionality.
Conclusion:
Healthcare professional burnout frequently associates with poor quality of care in the published literature. The true effect size may be smaller than reported. Future studies should pre-specify outcomes to lower the risk of exaggerated effect size estimates.
Funding Sources:
Stanford Maternal and Child Health Research Institute (PI: Tawfik), Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD084679–01, PIs: Profit and Sexton)
INTRODUCTION
Healthcare providers face a rapidly changing landscape of technology, care delivery methods, and regulations that increase risk for professional burnout. Studies suggest that nearly half of healthcare providers may have burnout symptoms at any given time.(1) Burnout has been linked to adverse effects at the provider and organizational levels, including suicidality, broken relationships, decreased productivity, unprofessional behavior, and turnover.(2–6)
Recent attention has focused on the relation between healthcare provider burnout and reduced quality of care, with a growing body of primary literature and systematic reviews reporting associations between burnout and adherence to practice guidelines, communication, medical errors, patient outcomes, and safety metrics.(7–11) Most studies in this field employ retrospective observational designs, and use a wide range of burnout assessments and analytic tools to evaluate myriad outcomes among diverse patient populations.(12) This lack of a standardized approach to measurement and analysis increases the risk of bias of evidence, potentially undermining scientific progress within a rapidly expanding field of research by creating difficulty deciphering which of the apparent clinically significant results represent true effects.(13) The present analysis sought to appraise this body of primary and review literature, developing an understanding of true effects within the field using a detailed evaluation for reporting biases.
Reporting biases take many forms, each contributing to overrepresentation of “positive” findings in the published literature. Study publication bias occurs when studies with negative results are published less frequently or less rapidly than studies with positive results.(14) Selective outcome reporting occurs when multiple outcomes of potential interest are evaluated, but outcomes with positive results are selectively presented or emphasized.(13) Selective analysis reporting occurs when multiple analytic strategies are employed, but those that produce the largest effects are selectively presented. Overall, these biases result in excess statistically significant results in the published literature, threatening reproducibility of findings, promoting misappropriation of resources, and skewing study designs for assessments of interventions to reduce burnout or improve quality.(13)
METHODS
We conducted a systematic literature review and meta-analysis to provide summary estimations of the relation between provider burnout and quality of care, estimate study heterogeneity, and explore the potential of reporting bias in the field. We followed the PRISMA and MOOSE guidelines for methodology and reporting.(15, 16)
Data Sources and Searches
We searched MEDLINE, PsycINFO, Health and Psychosocial Instruments, Mental Measurements Yearbook, Embase, and Web of Science from inception through May 28, 2019, with no language restrictions. We used search terms for burnout and its subdomains (emotional exhaustion, depersonalization, and reduced personal accomplishment), healthcare providers, and markers of quality of care as shown in Appendix Tables 1–3.
Study Selection
We included all peer-reviewed publications reporting original investigations of healthcare provider burnout in relation to an assessment of quality of patient care. Providers included all paid professionals providing outpatient, pre-hospital, emergency, or inpatient care to patients of any age, including medical, surgical, and psychiatric care. We chose an inclusive method of identifying studies of burnout, considering assessments to be related to burnout if the authors defined them as such and used any inventory intended to identify burnout, either in part or in full. We similarly chose an inclusive approach to identifying quality of care metrics, including any assessment of processes or outcomes indicative of care quality. We included objectively measured and subjectively reported quality metrics, originating from the provider, from other sources within the healthcare system, or from patients and their surrogates. We considered medical malpractice allegations a subjective patient-reported quality metric. Although patient satisfaction is an important outcome, it is not consistently indicative of care quality or improved medical outcomes, suggesting that it may be related to factors outside the provider’s immediate control such as facility amenities and access to care.(17–20) Thus, for the purposes of this review we excluded metrics solely indicative of patient satisfaction to reduce bias from these non-provider related factors that may affect satisfaction.
We included peer-reviewed indexed abstracts if they reported a study population not previously or subsequently reported in a full-length manuscript. For study populations described in multiple full-length manuscripts, we included the primary result from the manuscript with the earliest publication date as the primary outcome, with any unique outcomes from subsequent manuscripts as secondary outcomes. We supplemented the database searches with manual bibliography reviews from included studies and related literature reviews.(7–9, 21–24) In line with our reporting bias aim, we did not expand our search beyond peer-reviewed publications and did not contact authors for unpublished data. If insufficient data were presented in a publication to calculate an effect size, we supplemented with data from subsequent peer-reviewed publications when available, yet retained attribution of these effect sizes to the initial report. We excluded any purely qualitative studies.
All investigators contributed to development of study inclusion and exclusion criteria. The literature review and study selection were conducted by two independent reviewers in parallel (authors DT and either AS or KA), with ambiguities and discrepancies resolved by consensus.
Data Extraction and Quality Assessment
We extracted data into a standard template reflecting publication characteristics, burnout and quality metric assessment methods, risk of bias, and strength of reported relationship. Data were extracted by two independent reviewers (DT and AS), with discrepancies resolved by consensus. We estimated effect sizes and precision using Hedges’ g and standard errors (SE), respectively. Hedges’ g estimates effect size similarly to Cohen’s d, but with a bias correction factor for small samples. In general, 0.2 indicates small effect, 0.5 indicates medium effect, and 0.8 indicates large effect.
We classified each assessment of burnout as Overall Burnout, Emotional Exhaustion, Depersonalization, or Low Personal Accomplishment. We also identified burnout assessments as Standard if defined as Emotional Exhaustion score ≥ 27 or Depersonalization score ≥ 10 on the Maslach Burnout Inventory, or as the midpoint and higher on validated single-item scales. We categorized quality metrics within five groups: Best Practices, Communication, Medical Errors, Patient Outcomes, and Quality and Safety, and reverse-coded any “high quality” metrics such that positive effect sizes indicate burnout’s relation to poor quality of care.
For publications with multiple distinct (non-overlapping) study populations reported separately, we considered each population separately for purposes of analysis. For publications with multiple outcomes for the same study population, we decided to perform analyses that use only one outcome per study, ideally the specified primary outcome. Whenever there was no clear primary outcome, we chose the first listed outcome, consistent with reporting conventions of presenting the primary outcome first. We considered other outcomes secondary, excluding them from the primary analyses to avoid bias from intercorrelation but including them in selected descriptive statistics and stratified analyses where appropriate.
Data Synthesis and Analysis
We calculated Hedges’ g from odds ratios (dichotomized data) using the transformation , or from correlation coefficients (unscaled continuous data) using the transformation , both multiplied by a bias correction factor , consistent with published norms.(25, 26) Further details are provided in Appendix Methods.
The majority of studies reported burnout as a dichotomous variable or with unscaled effect size estimates, facilitating transformations as above. We scaled effect sizes accordingly for the 6 studies reporting burnout only as a continuous variable in order to maintain comparability, adapting our methods from published guidelines.(27, 28) Based on known distributions of burnout scores among providers,(29–31) we calculated the difference between the mean scores of providers with and without burnout to average 47.6% of the span of the particular burnout scale used. We thus converted effect sizes from continuous scales to the corresponding effect size reflective of a 47.6% change in scale score when needed to extrapolate to dichotomized burnout. We also performed sensitivity analyses excluding these few scaled effect sizes. More detailed description of this process is in Appendix Methods.
We initially intended to primarily perform a random effects meta-analysis including all primary (or first listed) effect sizes, with secondary meta-analyses stratified by quality metric category and by each unique burnout-quality metric combination. However, due to high heterogeneity in the pooled meta-analyses, we only report summary effects from the unique burnout-quality metric combinations. We also performed sensitivity analyses limited to studies with Standard burnout assessments and those with independently-observed or objectively-measured markers of quality of care. We used the empirical Bayes method with Knapp-Hartung modification to estimate the between-study variance tau2.(32) We evaluated study heterogeneity using I2. Details on this meta-analysis approach are in Appendix Methods.
We performed the Ioannidis test to evaluate for excess significance(33) by identifying the study population with the highest precision (1/SE) among those with the lowest risk of bias (studies using a full validated burnout inventory with an objective quality metric). We then calculated the power of all studies to detect the effect size of this study and compared observed vs. expected number of studies with statistically significant results using paired T-tests. Secondarily, we stratified excess significance testing by outcome category.
Because small studies may carry increased risk for bias, we performed the Egger test to evaluate for small-study effects.(34) We regressed standard normal deviate (Hedges’ g/SE) on precision (1/SE), using robust standard errors due to clustering of effect sizes at the study population level.
We used Stata 15.0 (StataCorp LLC, College Station, TX) for all analyses. All tests were two-sided. For summary effects, we considered two different thresholds of statistical significance, P < 0.05 and the newly proposed P < 0.005.(35, 36) We made no further corrections for multiple testing.
Role of the Funding Source
This study was performed in accordance with the Institutional Review Board requirements of Stanford University, and was classified as research not involving human subjects. This study was funded by the Stanford Maternal and Child Health Research Institute and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The funders of this study had no role in study design, data collection, analysis, interpretation, or writing of the report. The lead author had full access to all data in the study, and affirms that the manuscript is an honest, accurate, and transparent account of the study; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned have been explained.
RESULTS
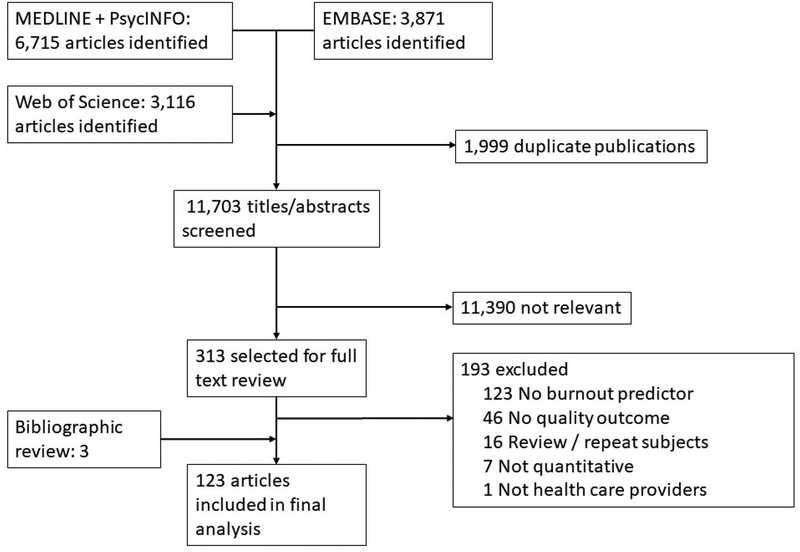
The search identified 11,703 citations, screening produced 313 potentially eligible publications retrieved in full text, and 120 were included, plus 3 additional publications identified by bibliography review (Figure 1). Overall, we included 123 publications from 1994 through 2019,(37–159) encompassing 142 distinct study populations detailed in Appendix Table 4. The median sample size was 376 (interquartile range 129 – 1417). The 142 study populations included physicians (N=71, 50%), nurses (N=84, 59%), and other providers (N=18, 13%), for a total of 241,553 healthcare providers evaluated. Quality metrics covered inpatient (N=122, 86%), outpatient (N=62, 44%), adult (N=134, 94%), pediatric (N=93, 65%), medical (N=135, 95%), and surgical (N=89, 63%) patients. Only 4 studies explicitly specified a primary outcome. Six studies did not provide sufficient data to derive an effect size from the original publication, but provided usable data published in a subsequent review.(39, 66, 69, 107, 115, 117) One research group reported results from a single study population in two publications—the first published effect was considered primary, with results from the later publication date considered secondary effects.(112, 160)
Figure 1.
Study selection process
Overall Burnout, Emotional Exhaustion, and Depersonalization were the primary predictors for 56, 75, and 11 study populations, respectively, from a variety of survey instruments as outlined in Appendix Table 5. The 50 distinct quality metrics included 10 Best Practices, 8 Communication, 10 Medical Errors, 10 Patient Outcomes, and 12 Quality and Safety measures (26 measured provider perception of quality, 15 used independent or objective measures of quality, and 9 included both types of assessments).
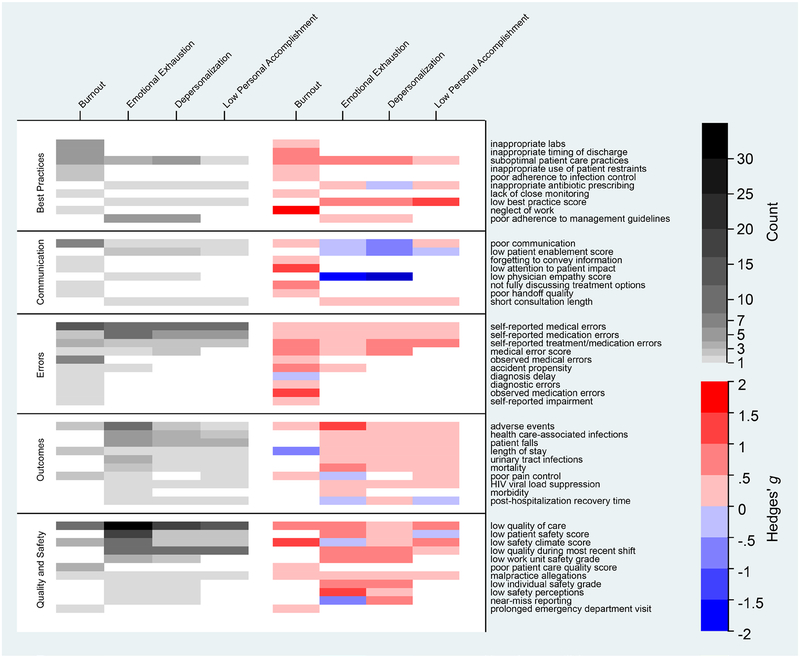
As illustrated in Figure 2, 38 (33%) of the 114 distinct burnout/quality combinations were reported 3 or more times. The most frequently reported effect related Emotional Exhaustion to Low quality of care (N = 41), with the majority of the reported effect sizes in the Quality and Safety and Medical Errors categories. Although all 5 categories of outcomes had estimates more frequently relating burnout in the direction of poor quality of care (denoted in red), 7 of the 16 estimates pointing in the opposite direction were found in the Communication category. Results were similar when limited to primary (or first listed, when primary was not specified) effect sizes only (Appendix Figure 1).
Figure 2.
Summary of all included burnout and quality metric combinations, showing frequency of effect size reporting and value of summary effect size.
Meta-analyses combining burnout and quality metrics within quality categories revealed I2 values of 93.4 to 98.8% indicating extremely high heterogeneity, and therefore summary effects are provided only at the level of the 114 distinct burnout/quality combinations, 46 of which included primary effect sizes. Meta-analyses of these 46 combinations revealed 24 (52%) with statistically significant summary effects > 0 (burnout related to poor quality of care), 1 (2%) with statistically significant summary effects < 0 (burnout related to high quality of care), and 21 (46%) with no difference at the P < 0.05 threshold. When the P < 0.005 threshold was used, the respective numbers were 18 (39%), 1 (2%), and 27 (59%). Results are summarized in Table 1, and primary effect sizes from all included studies are shown in Appendix Figure 2.
Table 1.
Number and direction of summary effect sizes for each combination of burnout and quality metric. Summary effect sizes obtained via empirical Bayes meta-analysis.
| Na | P < 0.05 threshold | P < 0.005 threshold | |||||
|---|---|---|---|---|---|---|---|
| g > 0b | g < 0c | No effectd | g > 0b | g < 0c | No effectd | ||
| Primary effects only | 46 | 24 (52%) | 1 (2%) | 21 (46%) | 18 (39%) | 1 (2%) | 27 (59%) |
| Primary and secondary effects | 114 | 58 (51%) | 6 (5%) | 50 (44%) | 47 (41%) | 6 (5%) | 61 (54%) |
| Standard burnout definitions | 24 | 15 (62%) | 1 (4%) | 8 (33%) | 14 (58%) | 1 (4%) | 9 (38%) |
| Independent/Objective quality metrics | 48 | 14 (29%) | 2 (4%) | 32 (67%) | 9 (19%) | 2 (4%) | 37 (77%) |
Number of distinct burnout/quality combinations represented
Summary effect Hedges’ g > 0 indicates burnout related to poor quality of care
Summary effect Hedges’ g < 0 indicates burnout related to high quality of care
Summary effect Hedges’ g not significantly different from 0 at the specified P-value threshold
Results were similar with inclusion of secondary effect sizes. Of the 114 distinct burnout/quality combinations, 58 (51%) had statistically significant summary effects > 0, 6 (5%) had statistically significant effects < 0, and 50 (44%) showed no difference at the P < 0.05 threshold. When the P < 0.005 threshold was used, the respective numbers were 47 (41%), 6 (5%), and 61 (54%). Results from all burnout and quality metric combinations are shown in Appendix Figure 3. Our findings were similar when limited to studies explicitly using Standard burnout definitions, but the observed relationships were attenuated when limited to independent/objective quality metrics, as shown in Table 1.
The most precise study with low risk of bias(143) reported a small effect size (Hedges’ g=0.26, analogous to an odds ratio of 1.5–1.6). Using this estimate, the Ioannidis test found an excess of observed versus predicted statistically significant studies (73% observed vs 62% predicted at the 0.05 significance threshold, P = 0.011) (Table 2). When stratified by quality metric category, an excess of statistically significant studies was seen in Best Practices and Quality and Safety. Results were similar for the P < 0.005 significance threshold.
Table 2.
Predicted significance vs observed significance for primary (or first listed, when primary was not specified) effect sizes among all included studies, and stratified by quality metric category.
| P < 0.05 threshold | P < 0.005 threshold | ||||||
|---|---|---|---|---|---|---|---|
| Number of studies | Predicted significance | Observed significance | P-value | Predicted significance | Observed significance | P-value | |
| Full cohort | 142 | 62% | 104 (73%) | 0.011 | 46% | 96 (68%) | <0.001 |
| Best Practices | 14 | 12% | 9 (64%) | 0.001 | 2% | 8 (57%) | 0.001 |
| Communication | 5 | 43% | 3 (60%) | 0.67 | 40% | 3 (60%) | 0.63 |
| Medical Errors | 32 | 50% | 20 (62%) | 0.169 | 33% | 15 (47%) | 0.182 |
| Patient Outcomes | 17 | 64% | 9 (53%) | NPa | 54% | 9 (53%) | NPa |
| Quality & Safety | 74 | 65% | 62 (84%) | <0.001 | 50% | 60 (81%) | <0.001 |
NP: not pertinent, observed smaller than predicted
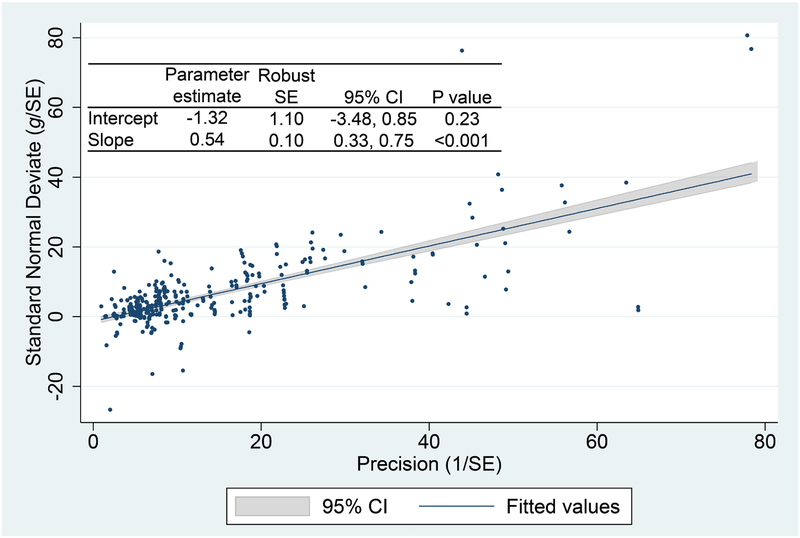
The Egger test did not show small-study effects (Intercept −1.32, 95% CI −3.48 to 0.85) indicating smaller studies did not systematically overestimate effect sizes (Figure 3). Funnel plot relating effect size to standard error is shown in Appendix Figure 4.
Figure 3.
Standard normal deviate (Hedges’ g / standard error) in relation to precision (1 / standard error)
DISCUSSION
This overview extends previous work in the field, by including a comprehensive evaluation for reporting biases in the healthcare provider burnout literature, encompassing 145 published study populations that quantified the relation between burnout and quality of care over a 25-year period for 241,553 healthcare professionals. The majority of evidence suggests a relationship between provider burnout and impaired quality of care, consistent with recent reviews of various dimensions.(7–10, 22) Although the effect sizes in the published literature are modestly strong, our finding of excess significance implies that the true magnitude may be smaller than reported, and the studies which attempted to lower the risk of bias demonstrate fewer significant associations compared to the full evidence base. The fact that only 4 studies specify primary outcomes further supports the possibility of reporting bias causing exaggerated effects.
From a 2015 MEDLINE, Web of Science, and CINAHL search, Salyers et al(9) reported effect sizes of r=−0.26 (Hedges’ g=0.54) and r=−0.23 (Hedges’ g=0.47) for the relationship between burnout and quality and safety outcomes, respectively. These effect sizes are somewhat larger than those observed in the present study. However, the prior meta-analysis also included markers of patient satisfaction, and only included 82 studies through March 2015. More recently, a 2017 all-language search of MEDLINE, Embase, and CINAHL by Panagioti et al.(10) identified 47 physician studies and reported a more similar summary odds ratio of 1.96 for patient safety incidents (approximate Hedges’ g=0.37). However, that review included 42,473 physicians (less than 20% of the number of subjects represented here), and did not include diverse healthcare professionals.
The observed relationships between burnout and quality of care are likely multifactorial. Individuals experiencing burnout may have less time or commitment to optimize the care of their patients, take more unnecessary risks, or lack ability to pay attention to necessary details or recognize the consequences of their actions.(71) Conversely, exposure to adverse patient events or recognition of poor quality of care may result in emotional or other psychological distress to the providers. This phenomenon is often referred to as secondary trauma, particularly in relation to sentinel events or important safety incidents, but it is plausible that it could also arise from repeated minor incidents.(161) The true effect sizes relating burnout and quality of care in both directions are important to understand, in order to make sound decisions on resource allocation and study design of interventions both to improve quality of care and to diminish burnout.
Recent concerns have arisen regarding variability in burnout assessment methods, and this variability was evident among the body of literature compiled here as well.(12) In this regard, the subset of studies in our analysis using the most widely-accepted “Standard” burnout assessment methods demonstrated similar to slightly increased frequency of significant associations when compared to the full evidence base. This finding suggests that the relationship between burnout and quality of care in the published literature is not due to suboptimal measures or variability in the definition of burnout used.
Excess significance in the published literature was specifically noted for adherence to best practice guidelines and for quality and safety metrics. Investigations of burnout in relation to these outcomes are typically retrospective studies of routinely-collected outcome metrics in existing datasets without pre-registered protocols. The relative ease of defining and evaluating many outcomes in many ways with these datasets increases risk for selective outcome reporting and selective analysis reporting, which may have contributed to excess significance. We found slightly lower effect sizes, but without excess significance for the Patient Outcomes subgroup, possibly reflecting the fact that these studies more commonly employed quality metrics with little or no flexibility in their definition and measurement (e.g. mortality or length of stay).
In direct assessment, studies employing independent or objective quality metrics demonstrated less frequent significant effects. This finding is not surprising, as prior research suggests that current methods for objectively measuring quality of care are not able to reliably identify certain events such as errors in judgment, technical procedural mistakes, or near-misses.(10, 162) Objective metrics are also costly to measure and difficult to connect to an individual due to the team-based nature of most clinical care, limiting their application to smaller studies and those in which a quality metric can be connected reliably to a provider. On the other hand, subjective quality metrics may be more sensitive and comprehensive, but more bias-prone (e.g., experiencing burnout may create recall bias). Further research is needed to determine the appropriate balance between the insensitivity of objective quality metrics and the potential for recall bias with subjective quality metrics.
Our analysis found no evidence specifically for small-study effects, in which small (more imprecise) studies report larger effects than large studies. These findings are consistent with those of prior meta-analyses, which traditionally evaluate for small-study effects as a surrogate for all forms of reporting bias.(9, 10) The discrepancy between our findings of overall excess significance without evidence of small-study effects may highlight the insensitivity of the latter test as a marker of all forms of bias. Moreover, smaller studies in this field are more likely to have objective measurements, while larger studies are more likely to have subjective measurements. This would dilute the ability of the small-study effect test to show a typical bias pattern.
Our study should be viewed in light of its design. Although most included studies are cross-sectional, observational and unable to determine the directionality of a causal relationship, longitudinal studies suggest bi-directional causality.(62, 149, 151, 152) We conducted extensive searches by two independent reviewers, but some relevant studies may be missed. Burnout has a number of important outcomes beyond effects on quality of care which were not the focus of our analysis.(2–6) Finally, excess significance may be due to genuine heterogeneity of effects across studies rather than reporting bias.(33) The effects reported here represent the results of heterogeneous studies, and so we do not report a single summary effect size. Rather, we report frequencies of significant summary effect sizes within burnout/quality combinations to provide a quantitative framework for interpretation while acknowledging that a distribution of true effect sizes is expected in this field-wide assessment, in contrast to a traditional meta-analysis.(163)
We avoided scoring quality assessments of the included studies, choosing instead to analyze key aspects of study quality as suggested by the proposed reporting guidelines for meta-analyses of observational studies.(16) Judging the quality of mostly cross-sectional observational studies is notoriously difficult and there are no widely accepted tools. Salyers et al.(9) created a 10-item tool to assess quality aspects in 82 burnout and quality of care studies and they did not identify any relationship between study quality score and effect size.
Our findings carry several important implications for future intervention trials and observational studies. For intervention trials, the potential for exaggerated published effects should be considered in power calculations to lower the risk of false negative results (Type II error). In addition, future studies should attempt to reduce the risk of reporting biases. Standardization and consensus on core outcomes may be useful for future studies if appropriate targets can be identified.(164) Such standardization can improve comparability among studies, facilitating traditional meta-analysis estimates of the relevant effect sizes. Some outcomes such as self-reported medical errors, low quality of care, and low patient safety score were particularly prevalent in the literature, suggesting that researchers already consider these outcomes either important or feasible to measure. However, if core outcomes are to be widely accepted, they must be both important and feasible to measure. Thus, in addition to this “popular vote” approach, expert consensus is needed to curate an appropriate list of core outcomes for this field. Other outcome evaluations could then be discouraged except if a unique justification is present.
Study registration may further reduce the risk of study publication bias and improve transparency surrounding unpublished studies. By registering a study publicly at its outset, researchers can reduce the likelihood that a study is conceived and conducted, but remains unpublished due to undesirable or lackluster results.(165) In a similar manner, protocol pre-specification may reduce the risk of selective outcome reporting and selective analysis reporting within published studies, allowing easier identification of any post-hoc analyses. Published analyses that deviate from the pre-specified protocol would require justification from the authors, and this approach would alert the readers that those results may be more susceptible to bias. These mechanisms are currently used rarely in any field of medicine outside of clinical trials, but could become widely adopted with sufficient advocacy by researchers, publishers, funders, and other stakeholders.
In conclusion, healthcare provider burnout is frequently associated with reduced quality of care in the published literature. However, few rigorous studies exist and the effect size may be smaller than reported, and it may be particularly smaller for objective quality measures. It is not yet known whether curtailing burnout improves quality of care and/or whether improving quality of care reduces burnout, and adequately powered and designed randomized trials (91, 166, 167) will be indispensable to answer these questions.
Supplementary Material
Declaration of interests
JP is supported by the National Institutes of Health. TS is supported by the National Institutes of Health and has received research support from The Physician Foundation; honoraria from multiple healthcare organizations; and royalty fees from the Mayo Clinic as a co-inventor of the Physician Well-being Index, the Medical Student Well-being Index, the Nurse Well-being Index, and the Participatory Management Leadership Index. JBS is supported by the National Institutes of Health. All other authors declare no competing interests.
Footnotes
Publisher's Disclaimer: This is the prepublication, author-produced version of a manuscript accepted for publication in Annals of Internal Medicine. This version does not include post-acceptance editing and formatting. The American College of Physicians, the publisher of Annals of Internal Medicine, is not responsible for the content or presentation of the author-produced accepted version of the manuscript or any version that a third party derives from it. Readers who wish to access the definitive published version of this manuscript and any ancillary material related to this manuscript (e.g., correspondence, corrections, editorials, linked articles) should go to Annals.org or to the print issue in which the article appears. Those who cite this manuscript should cite the published version, as it is the official version of record.
Contributor Information
Daniel S. Tawfik, Division of Pediatric Critical Care Medicine, Department of Pediatrics, Stanford University School of Medicine, Stanford, CA, USA.
Annette Scheid, Department of Pediatric Newborn Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA.
Jochen Profit, Perinatal Epidemiology and Health Outcomes Research Unit, Division of Neonatology, Department of Pediatrics, Stanford University School of Medicine, Stanford, CA, USA;; California Perinatal Quality Care Collaborative, Palo Alto, CA, USA
Tait Shanafelt, Department of Medicine, Stanford University School of Medicine, Stanford, CA, USA.
Mickey Trockel, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Stanford, CA, USA.
Kathryn C. Adair, Department of Psychiatry, Duke University School of Medicine, Duke University Health System, Durham, NC, USA;; Duke Patient Safety Center, Duke University Health System, Durham, NC, USA
J. Bryan Sexton, Department of Psychiatry, Duke University School of Medicine, Duke University Health System, Durham, NC, USA;; Duke Patient Safety Center, Duke University Health System, Durham, NC, USA
John P.A. Ioannidis, Department of Medicine, Department of Health Research and Policy, Department of Biomedical Data Science, Stanford University School of Medicine, Stanford, CA, USA;; Department of Statistics, Stanford University School of Humanities and Sciences, Stanford, CA, USA; Meta-Research Innovation Center at Stanford (METRICS), Stanford University School of Medicine, Stanford, CA, USA
REFERENCES
- 1.Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Satele DV, et al. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2017. Mayo Clin Proc. 2019. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 2.Shanafelt TD, Boone SL, Dyrbye LN, Oreskovich MR, Tan L, West CP, et al. The medical marriage: a national survey of the spouses/partners of US physicians. Mayo Clin Proc. 2013;88(3):216–25. [DOI] [PubMed] [Google Scholar]
- 3.Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, et al. Longitudinal Study Evaluating the Association Between Physician Burnout and Changes in Professional Work Effort. Mayo Clin Proc. 2016;91(4):422–31. [DOI] [PubMed] [Google Scholar]
- 4.Windover AK, Martinez K, Mercer MB, Neuendorf K, Boissy A, Rothberg MB. Correlates and Outcomes of Physician Burnout Within a Large Academic Medical Center. Jama Internal Medicine. 2018;178(6):856–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamidi MS, Bohman B, Sandborg C, Smith-Coggins R, de Vries P, Albert MS, et al. Estimating institutional physician turnover attributable to self-reported burnout and associated financial burden: a case study. BMC Health Serv Res. 2018;18(1):851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van der Heijden F, Dillingh G, Bakker A, Prins J. Suicidal thoughts among medical residents with burnout. Arch Suicide Res. 2008;12(4):344–6. [DOI] [PubMed] [Google Scholar]
- 7.Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ Open. 2017;7(6):e015141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. Plos One. 2016;11(7):e0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salyers MP, Bonfils KA, Luther L, Firmin RL, White DA, Adams EL, et al. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis. Journal of General Internal Medicine. 2017;32(4):475–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis. JAMA Intern Med. 2018;178(10):1317–30. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Rathert C, Williams ES, Linhart H. Evidence for the Quadruple Aim: A Systematic Review of the Literature on Physician Burnout and Patient Outcomes. Med Care. 2018;56(12):976–84. [DOI] [PubMed] [Google Scholar]
- 12.Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA. 2018;320(11):1131–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ioannidis JP, Munafo MR, Fusar-Poli P, Nosek BA, David SP. Publication and other reporting biases in cognitive sciences: detection, prevalence, and prevention. Trends Cogn Sci. 2014;18(5):235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dwan K, Gamble C, Williamson PR, Kirkham JJ, Reporting Bias G. Systematic review of the empirical evidence of study publication bias and outcome reporting bias - an updated review. PLoS One. 2013;8(7):e66844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12. [DOI] [PubMed] [Google Scholar]
- 17.Chang JT, Hays RD, Shekelle PG, MacLean CH, Solomon DH, Reuben DB, et al. Patients’ global ratings of their health care are not associated with the technical quality of their care. Ann Intern Med. 2006;144(9):665–72. [DOI] [PubMed] [Google Scholar]
- 18.Kennedy GD, Tevis SE, Kent KC. Is there a relationship between patient satisfaction and favorable outcomes? Ann Surg. 2014;260(4):592–8; discussion 8–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rao M, Clarke A, Sanderson C, Hammersley R. Patients’ own assessments of quality of primary care compared with objective records based measures of technical quality of care: cross sectional study. BMJ. 2006;333(7557):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schmocker RK, Cherney Stafford LM, Winslow ER. Satisfaction with surgeon care as measured by the Surgery-CAHPS survey is not related to NSQIP outcomes. Surgery. 2019;165(3):510–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chuang CH, Tseng PC, Lin CY, Lin KH, Chen YY. Burnout in the intensive care unit professionals A systematic review. Medicine. 2016;95(50):e5629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dewa CS, Loong D, Bonato S, Trojanowski L, Rea M. The relationship between resident burnout and safety-related and acceptability-related quality of healthcare: a systematic literature review. Bmc Medical Education. 2017;17:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scheepers RA, Boerebach BCM, Arah OA, Heineman MJ, Lombarts K. A Systematic Review of the Impact of Physicians’ Occupational Well-Being on the Quality of Patient Care. International Journal of Behavioral Medicine. 2015;22(6):683–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–81. [DOI] [PubMed] [Google Scholar]
- 25.Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000;19(22):3127–31. [DOI] [PubMed] [Google Scholar]
- 26.Lajeunesse M. Recovering Missing or Partial Data from Studies: A Survey of Conversions and Imputations for Meta-analysis. Princeton, NJ: Princeton University Press; 2013. [Google Scholar]
- 27.Guyatt GH, Thorlund K, Oxman AD, Walter SD, Patrick D, Furukawa TA, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles-continuous outcomes. J Clin Epidemiol. 2013;66(2):173–83. [DOI] [PubMed] [Google Scholar]
- 28.Hasselblad V, Hedges LV. Meta-analysis of screening and diagnostic tests. Psychol Bull. 1995;117(1):167–78. [DOI] [PubMed] [Google Scholar]
- 29.Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–85. [DOI] [PubMed] [Google Scholar]
- 30.Tawfik DS, Phibbs CS, Sexton JB, Kan P, Sharek PJ, Nisbet CC, et al. Factors Associated With Provider Burnout in the NICU. Pediatrics. 2017;139(5):e20164134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952–60. [DOI] [PubMed] [Google Scholar]
- 32.Knapp G, Hartung J. Improved tests for a random effects meta-regression with a single covariate. Stat Med. 2003;22(17):2693–710. [DOI] [PubMed] [Google Scholar]
- 33.Ioannidis JP, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. 2007;4(3):245–53. [DOI] [PubMed] [Google Scholar]
- 34.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
- 35.Benjamin DJ, Berger JO, Johannesson M, Nosek BA, Wagenmakers EJ, Berk R, et al. Redefine statistical significance. Nature Human Behaviour. 2018;2(1):6–10. [DOI] [PubMed] [Google Scholar]
- 36.Ioannidis JPA. The Proposal to Lower P Value Thresholds to .005. JAMA. 2018;319(14):1429–30. [DOI] [PubMed] [Google Scholar]
- 37.Abe K, Ohashi A. Development and Testing of a Staff Questionnaire for Evaluating the Quality of Services at Nursing Homes in Japan. Journal of the American Medical Directors Association. 2009;10(3):189–95. [DOI] [PubMed] [Google Scholar]
- 38.Adzic ZO, Katic M, Kern J, Soler JK, Cerovecki V, Polasek O. Is burnout in family physicians in Croatia related to interpersonal quality of care? Arhiv Za Higijenu Rada I Toksikologiju-Archives of Industrial Hygiene and Toxicology. 2013;64(2):255–64. [DOI] [PubMed] [Google Scholar]
- 39.Aiken LH, Sermeus W, Van Den Heede K, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ (Online). 2012;344(7851):e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Angermeier I, Dunford BB, Boss AD, Boss RW. The impact of participative management perceptions on customer service, medical errors, burnout, and turnover intentions. Journal of Healthcare Management. 2009;54(2):127–40. [PubMed] [Google Scholar]
- 41.Baer TE, Feraco AM, Sagalowsky ST, Williams D, Litman HJ, Vinci RJ. Pediatric resident burnout and attitudes toward patients. Pediatrics. 2017;139(3):e20162163. [DOI] [PubMed] [Google Scholar]
- 42.Baier N, Roth K, Felgner S, Henschke C. Burnout and safety outcomes - a cross-sectional nationwide survey of EMS-workers in Germany. BMC Emergency Medicine. 2018;18(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Balch CM, Oreskovich MR, Dyrbye LN, Colaiano JM, Satele DV, Sloan JA, et al. Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg. 2011;213(5):657–67. [DOI] [PubMed] [Google Scholar]
- 44.Bao Y, Vedina R, Moodie S, Dolan S. The relationship between value incongruence and individual and organizational well-being outcomes: An exploratory study among Catalan nurses. Journal of Advanced Nursing. 2013;69(3):631–41. [DOI] [PubMed] [Google Scholar]
- 45.Basar U, Basim N. A cross-sectional survey on consequences of nurses’ burnout: moderating role of organizational politics. Journal of Advanced Nursing. 2016;72(8):1838–50. [DOI] [PubMed] [Google Scholar]
- 46.Beckman TJ, Reed DA, Shanafelt TD, West CP. Resident physician well-being and assessments of their knowledge and clinical performance. Journal of General Internal Medicine. 2012;27(3):325–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Block L, Wu AW, Feldman L, Yeh HC, Desai SV. Residency schedule, burnout and patient care among first-year residents. Postgraduate Medical Journal. 2013;89(1055):495–500. [DOI] [PubMed] [Google Scholar]
- 48.Boamah SA, Read EA, Laschinger HKS. Factors influencing new graduate nurse burnout development, job satisfaction and patient care quality: a time-lagged study. Journal of Advanced Nursing. 2017;73(5):1182–95. [DOI] [PubMed] [Google Scholar]
- 49.Bronkhorst B, Vermeeren B. Safety climate, worker health and organizational health performance Testing a physical, psychosocial and combined pathway. International Journal of Workplace Health Management. 2016;9(3):270–89. [Google Scholar]
- 50.Brunsberg KA, Landrigan CP, Garcia BM, Petty CR, Sectish TC, Simpkin AL, et al. Association of Pediatric Resident Physician Depression and Burnout With Harmful Medical Errors on Inpatient Services. Academic medicine. 2019;94(8):1150–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chao M, Shih CT, Hsu SF. Nurse occupational burnout and patient-rated quality of care: The boundary conditions of emotional intelligence and demographic profiles. Japan journal of nursing science : JJNS. 2016;13(1):156–65. [DOI] [PubMed] [Google Scholar]
- 52.Chen KY, Yang CM, Lien CH, Chiou HY, Lin MR, Chang HR, et al. Burnout, Job Satisfaction, and Medical Malpractice among Physicians. International Journal of Medical Sciences. 2013;10(11):1471–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cheng C, Bartram T, Karimi L, Leggat SG. The role of team climate in the management of emotional labour: implications for nurse retention. J Adv Nurs. 2013;69(12):2812–25. [DOI] [PubMed] [Google Scholar]
- 54.Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40(6):486–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Colindres CV, Bryce E, Coral-Rosero P, Ramos-Soto RM, Bonilla F, Yassi A. Effect of effort-reward imbalance and burnout on infection control among Ecuadorian nurses. Int Nurs Rev. 2018;65(2):190–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cummings GG, Estabrooks CA, Midodzi WK, Wallin L, Hayduk L. Influence of organizational characteristics and context on research utilization. Nursing Research. 2007;56(4 Suppl):S24–39. [DOI] [PubMed] [Google Scholar]
- 57.Davenport DL, Henderson WG, Mosca CL, Khuri SF, Mentzer RM Jr. Risk-adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions. Journal of the American College of Surgeons. 2007;205(6):778–84. [DOI] [PubMed] [Google Scholar]
- 58.de Oliveira GS Jr., Chang R, Fitzgerald PC, Almeida MD, Castro-Alves LS, Ahmad S, et al. The prevalence of burnout and depression and their association with adherence to safety and practice standards: a survey of United States anesthesiology trainees. Anesth Analg. 2013;117(1):182–93. [DOI] [PubMed] [Google Scholar]
- 59.De Stefano C, Philippon AL, Krastinova E, Hausfater P, Riou B, Adnet F, et al. Effect of emergency physician burnout on patient waiting times. Internal and Emergency Medicine. 2018;13(3):421–8. [DOI] [PubMed] [Google Scholar]
- 60.Deckard G, Meterko M, Field D. Physician burnout: an examination of personal, professional, and organizational relationships. Med Care. 1994;32(7):745–54. [DOI] [PubMed] [Google Scholar]
- 61.Dorigan GH, Guirardello EB. Effect of the practice environment of nurses on job outcomes and safety climate. Revista Latino-Americana De Enfermagem. 2018;26:e3056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336(7642):488–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Faivre G, Kielwasser H, Bourgeois M, Panouilleres M, Loisel F, Obert L. Burnout syndrome in orthopaedic and trauma surgery residents in France: A nationwide survey. Orthopaedics and Traumatology: Surgery and Research. 2018;104(8):1291–5. [DOI] [PubMed] [Google Scholar]
- 64.Galletta M, Portoghese I, D’Aloja E, Mereu A, Contu P, Coppola RC, et al. Relationship between job burnout, psychosocial factors and health care-associated infections in critical care units. Intensive & critical care nursing. 2016;34:51–8. [DOI] [PubMed] [Google Scholar]
- 65.Garrouste-Orgeas M, Perrin M, Soufir L, Vesin A, Blot F, Maxime V, et al. The Iatroref study: medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensive Care Medicine. 2015;41(2):273–84. [DOI] [PubMed] [Google Scholar]
- 66.Gasparino RC, Guirardello Ede B, Aiken LH. Validation of the Brazilian version of the Nursing Work Index-Revised (B-NWI-R). J Clin Nurs. 2011;20(23–24):3494–501. [DOI] [PubMed] [Google Scholar]
- 67.Gopal R, Glasheen JJ, Miyoshi TJ, Prochazka AV. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005;165(22):2595–600. [DOI] [PubMed] [Google Scholar]
- 68.Guirardello EdB. Impact of critical care environment on burnout, perceived quality of care and safety attitude of the nursing team. Revista Latino-Americana de Enfermagem 2017;25:e2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gunnarsdottir S, Clarke SP, Rafferty AM, Nutbeam D. Front-line management, staffing and nurse-doctor relationships as predictors of nurse and patient outcomes. A survey of Icelandic hospital nurses. International Journal of Nursing Studies. 2009;46(7):920–7. [DOI] [PubMed] [Google Scholar]
- 70.Gupta K, Lisker S, Rivadeneira N, Mangurian C, Linos E, Sarkar U. Save Dr Mom: Second adverse event victim experiences: Decisions and repercussions for mothers in medicine. BMJ Quality & Safety. 2019;28:564–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Halbesleben JR, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Management Review. 2008;33(1):29–39. [DOI] [PubMed] [Google Scholar]
- 72.Halbesleben JR, Wakefield BJ, Wakefield DS, Cooper LB. Nurse burnout and patient safety outcomes: Nurse safety perception versus reporting behavior. Western Journal of Nursing Research. 2008;30(5):560–77. [DOI] [PubMed] [Google Scholar]
- 73.Hansen RP, Vedsted P, Sokolowski I, Sondergaard J, Olesen F. General practitioner characteristics and delay in cancer diagnosis. a population-based cohort study. BMC Fam Pract. 2011;12:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hayashino Y, Utsugi-Ozaki M, Feldman MD, Fukuhara S. Hope modified the association between distress and incidence of self-perceived medical errors among practicing physicians: Prospective cohort study. PLoS ONE. 2012;7(4):e35585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Holden RJ, Patel NR, Scanlon MC, Shalaby TM, Arnold JM, Karsh BT. Effects of mental demands during dispensing on perceived medication safety and employee well-being: a study of workload in pediatric hospital pharmacies. Res Social Adm Pharm. 2010;6(4):293–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Holden RJ, Scanlon MC, Patel NR, Kaushal R, Escoto KH, Brown RL, et al. A human factors framework and study of the effect of nursing workload on patient safety and employee quality of working life. Bmj Quality & Safety. 2011;20(1):15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Huang CH, Wu HH, Chou CY, Dai HY, Lee YC. The Perceptions of Physicians and Nurses Regarding the Establishment of Patient Safety in a Regional Teaching Hospital in Taiwan. Iranian Journal of Public Health. 2018;47(6):852–60. [PMC free article] [PubMed] [Google Scholar]
- 78.Huang CH, Wu HH, Lee YC. The perceptions of patient safety culture: A difference between physicians and nurses in Taiwan. Applied Nursing Research. 2018;40:39–44. [DOI] [PubMed] [Google Scholar]
- 79.Huang ECH, Pu C, Huang N, Chou YJ. Resident burnout in Taiwan Hospitals—and its relation to physician felt trust from patients. Journal of the Formosan Medical Association. 2019. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 80.Johnson J, Louch G, Dunning A, Johnson O, Grange A, Reynolds C, et al. Burnout mediates the association between depression and patient safety perceptions: a cross-sectional study in hospital nurses. Journal of Advanced Nursing. 2017;73(7):1667–80. [DOI] [PubMed] [Google Scholar]
- 81.Kang EK, Lihm HS, Kong EH. Association of intern and resident burnout with self-reported medical errors. Korean J Fam Med. 2013;34(1):36–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim MH, Mazenga AC, Simon K, Yu X, Ahmed S, Nyasulu P, et al. Burnout and self-reported suboptimal patient care amongst health care workers providing HIV care in Malawi. PLoS ONE. 2018;13(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kirwan M, Matthews A, Scott P. The impact of the work environment of nurses on patient safety outcomes: A multi-level modelling approach. International Journal of Nursing Studies. 2013;50(2):253–63. [DOI] [PubMed] [Google Scholar]
- 84.Klein J, Frie KG, Blum K, von dem Knesebeck O. Burnout and perceived quality of care among German clinicians in surgery. International Journal for Quality in Health Care. 2010;22(6):525–30. [DOI] [PubMed] [Google Scholar]
- 85.Kwah J, Fallar R, Weintraub JP, Ripp J. The impact of job burnout on measures of professionalism in first-year internal medicine residents at a large urban academic medical center. Journal of General Internal Medicine. 2014;29:S228. [Google Scholar]
- 86.Lafreniere JP, Rios R, Packer H, Ghazarian S, Wright SM, Levine RB. Burned Out at the Bedside: Patient Perceptions of Physician Burnout in an Internal Medicine Resident Continuity Clinic. Journal of General Internal Medicine. 2016;31(2):203–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Laschinger HKS, Leiter MP. The impact of nursing work environments on patient safety outcomes - The mediating role of burnout/engagement. Journal of Nursing Administration. 2006;36(5):259–67. [DOI] [PubMed] [Google Scholar]
- 88.Laschinger HKS, Shamian J, Thomson D. Impact of magnet hospital characteristics on nurses’ perceptions of trust, burnout, quality of care, and work satisfaction. Nursing Economics. 2001;19(5):209–19. [Google Scholar]
- 89.Lewis EJ, Baernholdt MB, Yan G, Guterbock TG. Relationship of adverse events and support to RN burnout. Journal of Nursing Care Quality. 2015;30(2):144–52. [DOI] [PubMed] [Google Scholar]
- 90.Linzer M, Manwell LB, Williams ES, Bobula JA, Brown RL, Varkey AB, et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151(1):28–36, W6–9. [DOI] [PubMed] [Google Scholar]
- 91.Linzer M, Poplau S, Brown R, Grossman E, Varkey A, Yale S, et al. Do Work Condition Interventions Affect Quality and Errors in Primary Care? Results from the Healthy Work Place Study. Journal of General Internal Medicine. 2017;32(1):56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Liu X, Zheng J, Liu K, Baggs JG, Liu JL, Wu Y, et al. Hospital nursing organizational factors, nursing care left undone, and nurse burnout as predictors of patient safety: A structural equation modeling analysis. International Journal of Nursing Studies. 2018;86:82–9. [DOI] [PubMed] [Google Scholar]
- 93.Liu Y, Aungsuroch Y. Factors influencing nurse-assessed quality nursing care: A cross-sectional study in hospitals. Journal of Advanced Nursing. 2018;74(4):935–45. [DOI] [PubMed] [Google Scholar]
- 94.Loerbroks A, Glaser J, Vu-Eickmann P, Angerer P. Physician burnout, work engagement and the quality of patient care. Occupational medicine (Oxford, England). 2017;67(5):356–62. [DOI] [PubMed] [Google Scholar]
- 95.Lorenz VR, Sabino MO, Corrêa Filho HR. Professional exhaustion, quality and intentions among family health nurses. Revista Brasileira De Enfermagem. 2018;71:2295–301. [DOI] [PubMed] [Google Scholar]
- 96.Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of Burnout on Self-Reported Patient Care Among Emergency Physicians. Western Journal of Emergency Medicine. 2015;16(7):996–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.MacPhee M, Dahinten VS, Havaei F. The Impact of Heavy Perceived Nurse Workloads on Patient and Nurse Outcomes. Administrative Sciences. 2017;7(1):7. [Google Scholar]
- 98.Martinussen M, Kaiser S, Adolfsen F, Patras J, Richardsen AM. Reorganisation of healthcare services for children and families: Improving collaboration, service quality, and worker well-being. Journal of interprofessional care. 2017;31(4):487–96. [DOI] [PubMed] [Google Scholar]
- 99.Mazurkiewicz RA, Smith KL, Korenstein D, Ripp J. The impact of resident physician burnout on the quality of care of hospitalized patients. Journal of General Internal Medicine. 2012;27:S323–S4. [Google Scholar]
- 100.Mion G, Libert N, Journois D. [Burnout-associated factors in anesthesia and intensive care medicine. 2009 survey of the French Society of anesthesiology and intensive care]. Annales Francaises D Anesthesie Et De Reanimation. 2013;32(3):175–88. [DOI] [PubMed] [Google Scholar]
- 101.Mohr DC, Eaton JL, Meterko M, Stolzmann KL, Restuccia JD. Factors associated with internal medicine physician job attitudes in the Veterans Health Administration. Bmc Health Services Research. 2018;18(1):244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Molina Siguero A, García Pérez MA, Alonso González M, Cecilia Cermeño P. Prevalence of worker burnout and psychiatric illness in primary care physicians in a health care area in Madrid. Atencion Primaria. 2003;31(9):564–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nantsupawat A, Nantsupawat R, Kunaviktikul W, Turale S, Poghosyan L. Nurse Burnout, Nurse-Reported Quality of Care, and Patient Outcomes in Thai Hospitals. Journal of nursing scholarship : an official publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau. 2016;48(1):83–90. [DOI] [PubMed] [Google Scholar]
- 104.O’Connor P, Lydon S, O’Dea A, Hehir L, Offiah G, Vellinga A, et al. A longitudinal and multicentre study of burnout and error in Irish junior doctors. Postgrad Med J. 2017;93(1105):660–4. [DOI] [PubMed] [Google Scholar]
- 105.Panunto MR, Guirardello ED. Professional nursing practice: environment and emotional exhaustion among intensive care nurses. Revista Latino-Americana De Enfermagem. 2013;21(3):765–72. [DOI] [PubMed] [Google Scholar]
- 106.Passalacqua SA, Segrin C. The Effect of Resident Physician Stress, Burnout, and Empathy on Patient-Centered Communication During the Long-Call Shift. Health Communication. 2012;27(5):449–56. [DOI] [PubMed] [Google Scholar]
- 107.Patrician PA, Shang J, Lake ET. Organizational determinants of work outcomes and quality care ratings among Army Medical Department registered nurses. Res Nurs Health. 2010;33(2):99–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pedersen AF, Carlsen AH, Vedsted P. Association of GPs’ risk attitudes, level of empathy, and burnout status with PSA testing in primary care. [Erratum appears in Br J Gen Pract. 2016 Jan;66(642):15; PMID: 26719464]. British Journal of General Practice. 2015;65(641):e845–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Poghosyan L, Clarke SP, Finlayson M, Aiken LH. Nurse burnout and quality of care: cross-national investigation in six countries. Research in nursing & health. 2010;33(4):288–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pratt M, Kerr M, Wong C. The impact of ERI, burnout, and caring for SARS patients on hospital nurses’ self-reported compliance with infection control. Canadian Journal of Infection Control. 2009;24(3):167–72, 74. [PubMed] [Google Scholar]
- 111.Prins JT, van der Heijden FM, Hoekstra-Weebers JE, Bakker AB, van de Wiel HB, Jacobs B, et al. Burnout, engagement and resident physicians’ self-reported errors. Psychol Health Med. 2009;14(6):654–66. [DOI] [PubMed] [Google Scholar]
- 112.Profit J, Sharek PJ, Amspoker AB, Kowalkowski MA, Nisbet CC, Thomas EJ, et al. Burnout in the NICU setting and its relation to safety culture. Bmj Quality & Safety. 2014;23(10):806–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Qureshi HA, Rawlani R, Mioton LM, Dumanian GA, Kim JY, Rawlani V. Burnout phenomenon in U.S. plastic surgeons: risk factors and impact on quality of life. Plast Reconstr Surg. 2015;135(2):619–26. [DOI] [PubMed] [Google Scholar]
- 114.Rafferty AM, Ball J, Aiken LH. Are teamwork and professional autonomy compatible, and do they result in improved hospital care? Quality in Health Care. 2001;10 Suppl 2:ii32–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ridley J, Wilson B, Harwood L, Laschinger HK. Work environment, health outcomes and magnet hospital traits in the Canadian nephrology nursing scene. CANNT J. 2009;19(1):28–35. [PubMed] [Google Scholar]
- 116.Riquelme I, Chacón JI, Gándara AV, Muro I, Traseira S, Monsalve V, et al. Prevalence of Burnout Among Pain Medicine Physicians and Its Potential Effect upon Clinical Outcomes in Patients with Oncologic Pain or Chronic Pain of Nononcologic Origin. Pain medicine (Malden, Mass.). 2018;19(12):2398–407. [DOI] [PubMed] [Google Scholar]
- 117.Rochefort CM, Clarke SP. Nurses’ work environments, care rationing, job outcomes, and quality of care on neonatal units. J Adv Nurs. 2010;66(10):2213–24. [DOI] [PubMed] [Google Scholar]
- 118.Salyers MP, Fukui S, Rollins AL, Firmin R, Gearhart T, Noll JP, et al. Burnout and self-reported quality of care in community mental health. Adm Policy Ment Health. 2015;42(1):61–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Schmidt SG, Dichter MN, Bartholomeyczik S, Hasselhorn HM. The satisfaction with the quality of dementia care and the health, burnout and work ability of nurses: a longitudinal analysis of 50 German nursing homes. Geriatr Nurs. 2014;35(1):42–6. [DOI] [PubMed] [Google Scholar]
- 120.Schwartz SP, Adair KC, Bae J, Rehder KJ, Shanafelt TD, Profit J, et al. Work-life balance behaviours cluster in work settings and relate to burnout and safety culture: a cross-sectional survey analysis. BMJ Quality & Safety. 2019;28(2):142–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995–1000. [DOI] [PubMed] [Google Scholar]
- 122.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–67. [DOI] [PubMed] [Google Scholar]
- 123.Shields CG, Fuzzell LN, Christ SL, Matthias MS. Patient and provider characteristics associated with communication about opioids: An observational study. Patient Education and Counseling. 2019;102(5):888–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Shirom A, Nirel N. Overload, autonomy, and burnout as predictors of physicians’ quality of care. Journal of Occupational Health Psychology. 2006;11(4):328–42. [DOI] [PubMed] [Google Scholar]
- 125.Sillero-Sillero A, Zabalegui A. Safety and satisfaction of patients with nurse’s care in the perioperative. Revista Latino-Americana De Enfermagem. 2019;27:e3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sokolova O, Pogosova N, Isakova S, Karpova A. Impact of Primary Care Physicians Burnout On Their Adherence to National Guidelines For Common CVD. Global Heart. 2018;13(4):486. [Google Scholar]
- 127.Squires M, Tourangeau A, Spence Laschinger HK, Doran D. The link between leadership and safety outcomes in hospitals. J Nurs Manag. 2010;18(8):914–25. [DOI] [PubMed] [Google Scholar]
- 128.Sturm H, Rieger MA, Martus P, Ueding E, Wagner A, Holderried M, et al. Do perceived working conditions and patient safety culture correlate with objective workload and patient outcomes: A cross-sectional explorative study from a German university hospital. PLoS ONE. 2019;14(1):e0209487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sulaiman CFC, Henn P, Smith S, O’Tuathaigh CMP. Burnout syndrome among non-consultant hospital doctors in Ireland: Relationship with self-reported patient care. International Journal for Quality in Health Care. 2017;29(5):679–84. [DOI] [PubMed] [Google Scholar]
- 130.Sun BZ, Chaitoff A, Hu B, Neuendorf K, Manne M, Rothberg MB. Empathy, burnout, and antibiotic prescribing for acute respiratory infections: a cross-sectional primary care study in the US. British Journal of General Practice. 2017;67(661):e565–e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tawfik DS, Profit J, Morgenthaler TI, Satele DV, Sinsky CA, Dyrbye LN, et al. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin Proc. 2018;93(11):1571–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Teng CI, Shyu YI, Chiou WK, Fan HC, Lam SM. Interactive effects of nurse-experienced time pressure and burnout on patient safety: a cross-sectional survey. International Journal of Nursing Studies. 2010;47(11):1442–50. [DOI] [PubMed] [Google Scholar]
- 133.Toral-Villanueva R, Aguilar-Madrid G, Juárez-Pérez CA. Burnout and patient care in junior doctors in Mexico City. Occupational medicine (Oxford, England). 2009;59(1):8–13. [DOI] [PubMed] [Google Scholar]
- 134.Trockel M, Bohman B, Lesure E, Hamidi MS, Welle D, Roberts L, et al. A Brief Instrument to Assess Both Burnout and Professional Fulfillment in Physicians: Reliability and Validity, Including Correlation with Self-Reported Medical Errors, in a Sample of Resident and Practicing Physicians. Acad Psychiatry. 2018;42(1):11–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tsiga E, Panagopoulou E, Montgomery A. Examining the link between burnout and medical error: A checklist approach. Burnout Research. 2017;6:1–8. [Google Scholar]
- 136.Van Bogaert P, Clarke S, Roelant E, Meulemans H, Van de Heyning P. Impacts of unit-level nurse practice environment and burnout on nurse-reported outcomes: a multilevel modelling approach. Journal of clinical nursing. 2010;19(11–12):1664–74. [DOI] [PubMed] [Google Scholar]
- 137.Van Bogaert P, Clarke S, Wouters K, Franck E, Willems R, Mondelaers M. Impacts of unit-level nurse practice environment, workload and burnout on nurse-reported outcomes in psychiatric hospitals: A multilevel modelling approach. International Journal of Nursing Studies. 2013;50(3):357–65. [DOI] [PubMed] [Google Scholar]
- 138.Van Bogaert P, Dilles T, Wouters K, Van Rompaey B. Practice environment, work characteristics and levels of burnout as predictors of nurse reported job outcomes, quality of care and patient adverse events: A study across residential aged care services. Open Journal of Nursing. 2014;4(5):343–55. [Google Scholar]
- 139.Van Bogaert P, Kowalski C, Weeks SM, Van heusden D, Clarke SP. The relationship between nurse practice environment, nurse work characteristics, burnout and job outcome and quality of nursing care: A cross-sectional survey. International Journal of Nursing Studies. 2013;50(12):1667–77. [DOI] [PubMed] [Google Scholar]
- 140.Van Bogaert P, Meulemans H, Clarke S, Vermeyen K, Van De Heyning P. Hospital nurse practice environment, burnout, job outcomes and quality of care: Test of a structural equation model. Journal of Advanced Nursing. 2009;65(10):2175–85. [DOI] [PubMed] [Google Scholar]
- 141.Van Bogaert P, Timmermans O, Weeks SM, van Heusden D, Wouters K, Franck E. Nursing unit teams matter: Impact of unit-level nurse practice environment, nurse work characteristics, and burnout on nurse reported job outcomes, and quality of care, and patient adverse events--a cross-sectional survey. International journal of nursing studies. 2014;51(8):1123–34. [DOI] [PubMed] [Google Scholar]
- 142.Van Bogaert P, Van Heusden D, Slootmans S, Roosen I, Van Aken P, Hans GH, et al. Staff empowerment and engagement in a magnet (R) recognized and joint commission international accredited academic centre in Belgium: a cross-sectional survey. Bmc Health Services Research. 2018;18(1):756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Van Gerven E, Elst TV, Vandenbroeck S, Dierickx S, Euwema M, Sermeus W, et al. Increased Risk of Burnout for Physicians and Nurses Involved in a Patient Safety Incident. Medical Care. 2016;54(10):937–43. [DOI] [PubMed] [Google Scholar]
- 144.Vifladt A, Simonsen BO, Lydersen S, Farup PG. The association between patient safety culture and burnout and sense of coherence: A cross-sectional study in restructured and not restructured intensive care units. Intensive and Critical Care Nursing. 2016;36:26–34. [DOI] [PubMed] [Google Scholar]
- 145.Vogus TJ, Cooil B, Sitterding M, Everett LQ. Safety organizing, emotional exhaustion, and turnover in hospital nursing units. Med Care. 2014;52(10):870–6. [DOI] [PubMed] [Google Scholar]
- 146.Wawrzyniak AJ, Rodriguez AE. The association between physician burnout and satisfaction on health outcomes in HIV-infected outpatients. Psychosomatic Medicine. 2017;79(4):A102. [Google Scholar]
- 147.Weigl M, Schneider A, Hoffmann F, Angerer P. Work stress, burnout, and perceived quality of care: a cross-sectional study among hospital pediatricians. European Journal of Pediatrics. 2015;174(9):1237–46. [DOI] [PubMed] [Google Scholar]
- 148.Welp A, Meier LL, Manser T. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Frontiers in Psychology. 2015;5:1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Welp A, Meier LL, Manser T. The interplay between teamwork, clinicians’ emotional exhaustion, and clinician-rated patient safety: a longitudinal study. Critical Care. 2016;20(1):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wen J, Cheng Y, Hu X, Yuan P, Hao T, Shi Y. Workload, burnout, and medical mistakes among physicians in China: A cross-sectional study. Bioscience trends. 2016;10(1):27–33. [DOI] [PubMed] [Google Scholar]
- 151.West CP, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, et al. Association of perceived medical errors with resident distress and empathy: A prospective longitudinal study. Journal of the American Medical Association. 2006;296(9):1071–8. [DOI] [PubMed] [Google Scholar]
- 152.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA - Journal of the American Medical Association. 2009;302(12):1294–300. [DOI] [PubMed] [Google Scholar]
- 153.Williams ES, Manwell LB, Konrad TR, Linzer M. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev. 2007;32(3):203–12. [DOI] [PubMed] [Google Scholar]
- 154.Winning AM, Merandi JM, Lewe D, Stepney LMC, Liao NN, Fortney CA, et al. The emotional impact of errors or adverse events on healthcare providers in the NICU: The protective role of coworker support. Journal of Advanced Nursing. 2018;74(1):172–80. [DOI] [PubMed] [Google Scholar]
- 155.Yanos PT, Vayshenker B, DeLuca JS, O’Connor LK. Development and validation of a scale assessing mental health clinicians’ experiences of associative stigma. Psychiatric Services. 2017;68(10):1053–60. [DOI] [PubMed] [Google Scholar]
- 156.Yassi A, Cohen M, Cvitkovich Y, Park IH, Ratner PA, Ostry AS, et al. Columbia, Canada factors associated with staff injuries in intermediate care facilities in British. Nursing Research. 2004;53(2):87–98. [DOI] [PubMed] [Google Scholar]
- 157.You L-m, Aiken LH, Sloane DM, Liu K, He G-p, Hu Y, et al. Hospital nursing, care quality, and patient satisfaction: Cross-sectional surveys of nurses and patients in hospitals in China and Europe. International Journal of Nursing Studies. 2013;50(2):154–61. [DOI] [PubMed] [Google Scholar]
- 158.Yuguero O, Marsal JR, Buti M, Esquerda M, Soler-Gonzalez J. Descriptive study of association between quality of care and empathy and burnout in primary care. Bmc Medical Ethics. 2017;18(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Zarei E, Khakzad N, Reniers G, Akbari R. On the relationship between safety climate and occupational burnout in healthcare organizations. Safety Science. 2016;89:1–10. [Google Scholar]
- 160.Tawfik DS, Sexton JB, Kan P, Sharek PJ, Nisbet CC, Rigdon J, et al. Burnout in the neonatal intensive care unit and its relation to healthcare-Associated infections. Journal of Perinatology. 2017;37(3):315–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Van Gerven E, Vander Elst T, Vandenbroeck S, Dierickx S, Euwema M, Sermeus W, et al. Increased Risk of Burnout for Physicians and Nurses Involved in a Patient Safety Incident. Med Care. 2016;54(10):937–43. [DOI] [PubMed] [Google Scholar]
- 162.Sari AB, Sheldon TA, Cracknell A, Turnbull A. Sensitivity of routine system for reporting patient safety incidents in an NHS hospital: retrospective patient case note review. BMJ. 2007;334(7584):79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ioannidis JP, Patsopoulos NA, Rothstein HR. Reasons or excuses for avoiding meta-analysis in forest plots. BMJ. 2008;336(7658):1413–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Dodd S, Clarke M, Becker L, Mavergames C, Fish R, Williamson PR. A taxonomy has been developed for outcomes in medical research to help improve knowledge discovery. J Clin Epidemiol. 2018;96:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Dal-Re R, Ioannidis JP, Bracken MB, Buffler PA, Chan AW, Franco EL, et al. Making prospective registration of observational research a reality. Sci Transl Med. 2014;6(224):224cm1. [DOI] [PubMed] [Google Scholar]
- 166.Parshuram CS, Amaral AC, Ferguson ND, Baker G, Etchells EE, Flintoft V, et al. Patient safety, resident well-being and continuity of care with different resident duty schedules in the intensive care unit: A randomized trial. Canadian Medical Association Journal. 2015;187(5):321–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.West CP, Dyrbye L, Satele D, Shanafelt T. A Randomized Controlled Trial Evaluating the Effect of Compass (Colleagues Meeting to Promote and Sustain Satisfaction) Small Group Sessions on Physician Well-Being, Meaning, and Job Satisfaction. Journal of General Internal Medicine. 2015;30:S89. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.