Abstract
Objectives:
Genetic counselors (GCs) can frame information in either general terms (i.e., population risks) or individual terms (i.e., tailoring to specific client characteristics). We investigated whether informational framing might reflect GCs’ implicit racial bias.
Methods:
We analyzed previously videotaped genetic counseling sessions with white and minority (Black and Latino) simulated clients (SCs) and modeled the relationship between sixty GCs’ implicit racial bias, as measured by the Implicit Association Test (IAT), and informational framing (general or individual) as characterized by the Roter Interaction Analysis System.
Results:
Higher (more pro-white) IAT scores predicted less informational individuation for minority relative to white SCs. Similarly, higher IAT predicted fewer facilitation and activation statements to minority relative to white SCs. With higher IAT-scoring GCs, minority SCs disclosed less psychosocial and lifestyle information, and asked fewer medical questions (all p<0.05).
Conclusion:
GCs’ racial implicit bias may be associated with less individualized communication style when counseling minority clients.
Practice Implications:
Future research should address whether increasing informational individuation can ameliorate negative consequences of implicit bias and help providers reframe perceptions of minority patients in individual rather than categorical terms.
Keywords: Implicit attitudes, Race/ethnicity, RIAS, Patient-provider communication, Individuation, Genetic counseling
1. Introduction
Here is what I sometimes suspect my face signifies to other Americans: an invisible person, barely distinguishable from a mass of faces that resemble it. A conspicuous person standing apart from the crowd and yet devoid of any individuality. [1]
The opening quote describes the experience of being seen as a member of a group rather than an individual – an experience that is uniquely alienating and may be a particularly harmful dynamic in patient-provider relationships. Racially discordant medical visit interactions have been associated with less patient-centered communication [1], less patient positive affect [1,2], less relationship-building [3], and lower patient satisfaction [2]. While studies suggest that a more patient-centered communication style matters more than racial or ethnic concordance for patient outcomes [4,5], implicit bias may explain racial differences in communication and interpersonal care during medical visits. Implicit bias is the unconscious evaluation of members of a group based on that group’s characteristics. In medical practice, it has been associated with poorer ratings of care [6–8] and less patient-centered communication [7,9] during medical visits.
Both racial discordance and implicit bias are relevant to the care of racially diverse clients seeking genetic counseling services. The genetic counseling profession has historically been and remains racially homogeneous, with 88% of GCs in the U.S. and Canada reporting their race as non-Hispanic white in the 2019 National Society of Genetic Counselors Professional Status Survey [10]. Minority clients are therefore likely to be racially discordant in interactions with GCs. Furthermore, most GCs, like others in the U.S. population, have pro-white implicit bias [9], which has been associated with less client-centered communication in genetic counseling interactions with minority simulated clients [9].
Processes of individuation and categorization may explain how implicit bias affects key processes of genetic counseling communication and medical exchange more generally. Brewer [11] proposed that when people are perceived as being a member of an outgroup, they are more likely to form impressions using a category-based processing mode (categorization), in which the perceiver processes and encodes information about an individual as it relates to a stereotypical category to which that individual belongs. By contrast, one is more likely to form authentic impressions when using an individual-based processing mode (individuation), in which information unique to that individual is recognized as distinguishing him or her from other individuals.
Failure to recognize clients’ individual characteristics may prevent GCs from effectively partnering with clients and could explain the associations between clinician implicit bias and poorer interpersonal care observed in empirical studies [7,9]. Yet, Gaertner and colleagues found that inducing individuals to “re-categorize” themselves by creating a common identity led to more positive evaluations of outgroup members [12]. GCs who are effective at eliciting and responding to clients’ individual characteristics may more effectively create a shared identity and partner around mutual goals.
We wondered whether processes of individuation and categorization may be evident in information exchange and relational dynamics during genetic counseling sessions. The objectives of the present study are 1) to investigate the relationship between implicit racial bias and informational framing of clinical information as individuated or generalized; 2) to explore correlates of implicit bias and patient-centeredness of GCs’ communication; and, 3) to explore effects of GCs’ implicit bias on simulated clients’ (SCs’) communication behavior. We hypothesized that higher pro-white bias would be associated with less individualized communication with minority SCs.
2. Methods
2.1. Procedure
2.1.1. The Genetic Counseling Video Project
This study is a secondary analysis of a subset of videotaped simulated genetic counseling sessions from a previous study of genetic counseling communication, the Genetic Counseling Video Project [13]. Briefly, in 2003 and 2004, GCs practicing in the U.S. and Canada attending national meetings were recruited to participate in the study by consenting to a videotaped simulated counseling session. Six SCs were cross-trained to portray two client scenarios: (1) a pregnant woman of advanced maternal age seeking pre-amniocentesis counseling, and (2) a woman with a family history of breast and ovarian cancer seeking information about BRCA1 and BRCA2 genetic testing. Female SCs included two non-Hispanic Caucasian, two African American, and two Hispanic Latino actors. In approximately 50% of the sessions, an ethnicity-matched male spouse accompanied the female SC. For all scenarios, the SC and spouse were scripted to have a high school education and working-class background with no special prior knowledge of genetics. All SCs were graduate students or acquaintances of graduate students at the Johns Hopkins School of Public Health. The SCs had no special training in genetics. SCs performed with a high degree of accuracy and consistency over time [14].
2.1.2. Implicit Association Test (IAT)
Implicit racial bias scores of study participants were collected in 2010 as part of a study by Schaa and colleagues [9] using the Project Implicit® Black:White Race Implicit Association Test (IAT). The current study uses these scores as an independent variable. The IAT has been widely used to measure implicit bias in other studies of health care professionals [7,15,16]. The IAT methodology is detailed elsewhere [17]. Briefly, the IAT score is based on an algorithm that calculates the mean standardized difference in response time to associate the target concept (black or white race) with an attribute (represented by a descriptive word with a positive or negative connotation). The scores range from +2 (indicating high implicit pro-white bias) to −2 (indicating high implicit pro-black bias), with zero indicating no relative implicit preference.
2.1.3. Roter Interaction Analysis System (RIAS)
The RIAS is a widely used coding system applied to communication in a variety of medical settings including genetic counseling [13,18]. In this study, RIAS codes were applied to produce meaningful categories to analyze GC and SC communication.
2.1.3.1. Informational framing
Information framing was incorporated into the parent study coding as a genetic counseling-specific adaptation of RIAS coding. Coders were trained to distinguish medical and therapeutic information as generalized, referring to the broad patient population or as individualized, referring to the particular medical and family context of the patient. Examples of individualized information are “Based on your age and what you told me about your family history, the chance that you would have a baby with a chromosome problem in one in 103,” or “Amniocentesis can be done as late as 21 weeks and you are right now at 16 weeks, at the window where this is possible.” The more generalized framing of this information would be: “The chance for a baby to be born with any chromosome problem is one in 103” and “Amniocentesis can be done as late as 21 weeks.” Additional examples are provided in Table 1. Practice examples and operational definitions illustrating of these differences were incorporated into the study coding manual. Coders demonstrated high inter-coder reliability overall (≥0.90) on a random sample of 20 videotapes [11].
Table 1.
RIAS codes for simulated client education and counseling in genetic counseling sessions (adapted from Roter et al., 2006)
| Framing of clinical information | Example GC dialogue |
|---|---|
| Individualized | Based on what you told me, there is 20% chance that the genetic mutation would be found. |
| You already had a blood test and now we are talking about a more invasive test for you, amniocentesis. | |
| Generalized | Most women have about a one in nine chance of developing breast cancer. |
| There are several tests available, some are invasive and others are not. |
For the study outcome measure of informational individuation, the sum of GC talk that was RIAS-coded as individually-framed medical and therapeutic information was divided by the sum of generally-framed medical and therapeutic information.
2.1.3.2. Characterizing individuation of interpersonal dynamics
We used RIAS codes that have been previously applied to identify communication behaviors that reflect patient-centeredness or provider-centeredness of the interaction [19–21]. For our outcome variables, we used the following patient-centered behaviors: SC asking psychosocial questions, SC giving psychosocial information, SC emotional talk, SC medical questions, GC asking psychosocial questions, GC giving psychosocial information, GC emotional responsiveness, and GC facilitation and patient activation. The category of GC facilitation and patient activation followed Guan and colleagues’ application of this concept to an observational study of genetic counseling sessions [22]. We also considered as outcome variables the following provider-centered behaviors: SC providing biomedical information, GC asking medical questions, GC procedural talk, and GC biomedical education and counseling.
2.2. Data Analyses
Data were analyzed using R Statistical Software, version 3.5.0 [23]. For all outcome variables, multiple linear regressions were performed with GC’s IAT score, dichotomized SC race (white or minority), and the interaction term between IAT score and dichotomized SC race as the main predictors. Additional covariates considered for the model were scenario (prenatal vs. cancer) and presence of spouse (absent or present). Effects of these covariates are presented as unstandardized coefficients. To explore clustering on the female SC, ICCs were calculated for each model. When the ICC exceeded 0.1, we compared a random effects model to the fixed effects model. However, there were no statistically significant differences between the models or the effects of the covariates. Therefore, we present the fixed effects.
2.2.1. Informational individuation
To approximate a normal distribution of the outcome variable, four outliers were omitted from analysis following sensitivity analyses. These outliers were individual GCs who used an exceptionally high proportion of individualized to generalized information (ratio greater than 1.0). Presence of spouse did not significantly predict variation in informational individuation in this model, so this was omitted as a covariate.
2.2.2. Interpersonal dynamics
Multiple linear regression analyses were performed to explore the relationship between explanatory variables and the outcome variables (each of the RIAS categories for patient- and provider-centered behaviors). When the outcome variable deviated from a normal distribution, outcomes were natural log or square root transformed, or outliers were omitted following a sensitivity analysis. Presence of spouse did not significantly predict variation in the categories “GC facilitation and SC activation” or “SC gives psychosocial and lifestyle information” in these models, so this was omitted as a covariate.
3. Results
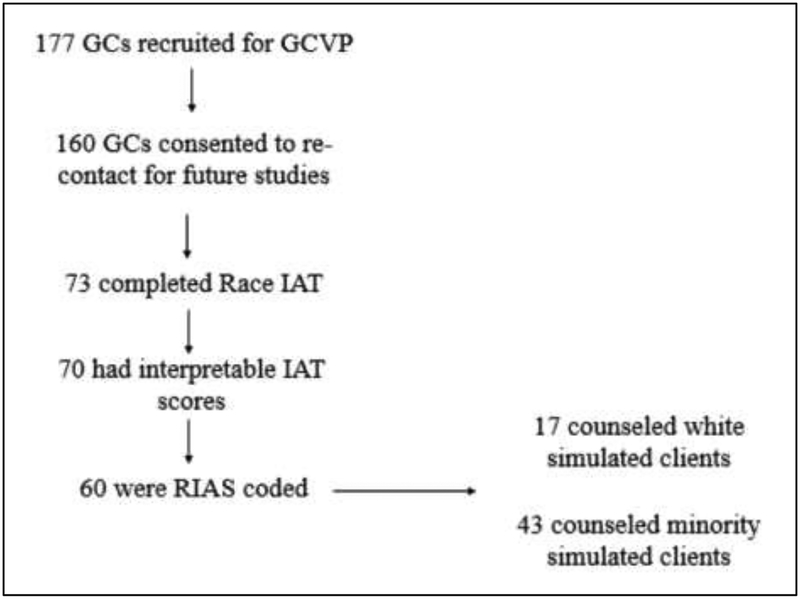
Among 73 GCVP participants who completed the Race IAT, a total of 60 had both interpretable IAT scores and had videotaped a session that was RIAS-coded. Participant flow through the study is summarized in Figure 1 and participant characteristics are shown in Table 2. Genetic counselors were predominantly female (92%) and non-Hispanic/Latino white (90%). Other ethnicities represented in the sample included Asian (7%), multiracial (2%), and Hispanic/Latino white (2%). All NSGC regions were represented in the sample, with region 3 somewhat over-represented in this sample relative to the 2004 Professional Status Survey [24], probably attributable to the 2003 NSGC Annual Conference being held in North Carolina. Similarly, the age distribution was similar to the 2004 Professional Status Survey, with the 31–40 years of age as the most common category, representing 38 percent of the study sample. Overall, GCs had a mean IAT score of 0.42 (s.d. = 0.36), consistent with a moderate degree of implicit pro-white bias. Fifty-eight percent of GCs participated in the prenatal scenario and 42 percent participated in the cancer scenario. In our analyses, there were no substantial differences between GCs who counseled white and minority clients based on scenario, presence of spouse, IAT score, GC race and ethnicity.
Figure 1.
Participant flow through studies
Table 2.
Characteristics of Study Population
| Total | White | Minority | |
|---|---|---|---|
| N | 60 | 17 | 43 |
| Scenario | |||
| Prenatal (%) | 35 (58) | 10 (59) | 25 (58) |
| Cancer (%) | 25 (42) | 7 (41) | 18 (42) |
| Spouse present (%) | 26 (43) | 8 (47) | 18 (42) |
| IAT (mean (sd)) | 0.42 (0.36) | 0.39 (0.35) | 0.43 (0.37) |
| IAT category (%) | |||
| Slight pro-Black | 2 (3) | 0 (0) | 2 (5) |
| Little to no preference | 12 (20) | 4 (24) | 8 (19) |
| Slight pro-White | 13 (22) | 4 (24) | 9 (21) |
| Moderate pro-White | 17 (28) | 5 (29) | 12 (28) |
| Strong pro-White | 16 (27) | 4 (24) | 12 (28) |
| Age in 2003–2004 (%) | |||
| 21–30 | 17 (28) | 9 (53) | 8 (19) |
| 31–40 | 23 (38) | 6 (35) | 17 (40) |
| 41–50 | 14 (23) | 0 (0) | 14 (33) |
| 51+ | 6 (10) | 2 (12) | 4 (9) |
| Gender | |||
| Female | 55 (92) | 15 (88) | 40 (93) |
| Male | 5 (8) | 2 (12) | 3 (7) |
| GC Race and Ethnicity (%) | |||
| White - Not Hispanic or Latino | 54 (90) | 16 (94) | 39 (91) |
| Asian | 4 (7) | 1 (6) | 3 (7) |
| White - Hispanic or Latino | 1 (2) | 1 (6) | 0 (0) |
| Multiracial | 1 (2) | 0 (0) | 1 (2) |
| NSGC Region (%) | |||
| 1: CT, MA, ME, NH, RI, VT, CN Maritime provinces | 3 (5) | 2 (12) | 1 (2) |
| 2: DC, DE, MD, NJ, NY, PA, VA, WV, PR, VI, Quebec | 9 (15) | 4 (24) | 5 (12) |
| 3: AL, FL, GA, KY, LA, MS, NC, SC, TN | 15 (25) | 3 (18) | 12 (28) |
| 4: AR, IA, IL, IN, KS, MI, MN, MO, ND, NE, OH, OK, SD, WI, Ontario | 11 (18) | 3 (18) | 8 (19) |
| 5: AZ, CO, MT, NM, TX, UT, WY, Alberta, Manitoba, Sask. | 8 (13) | 0 (0) | 8 (19) |
| 6: AK, CA, HI, ID, NV, OR, WA, British Columbia | 14 (23) | 5 (29) | 9 (21) |
3.1. Informational individuation
On average, GCs gave individualized clinical information 103 times per session (s.d.=45) and gave generalized clinical information an average of 199 times per session (s.d.=68). The average ratio of individualized to generalized clinical information in this sample was 0.58 (s.d. = 0.42). Descriptive statistics by SC race are presented in Table 3. In the adjusted model (see Table 4), the interaction between SC race and IAT score was statistically significant (β=−0.33, p=0.04), indicating that GCs with higher (more pro-white) IAT scores were less likely to provide individualized medical information to minority SCs. GCs provided a higher ratio of individualized to generalized information in cancer sessions than in prenatal sessions, and scenario was included as a covariate in the regression model (data not shown).
Table 3.
Framing of clinical information provided by genetic counselors - descriptive statistics
| Outcome variable (mean (sd)) | Overall | White | Minority | p-value |
|---|---|---|---|---|
| n | 60 | 17 | 43 | NA |
| Total medical information given by GC | 301.8 | 316.2 | 296.2 | 0.42 |
| (85.3) | (83.4) | (86.4) | ||
| Medical information given by GC: personal frame | 102.5 | 102.0 | 102.6 | 0.96 |
| (44.9) | (44.3) | (45.7) | ||
| Medical information given by GC: general frame | 199.4 | 214.2 | 193.5 | 0.29 |
| (67.8) | (61.1) | (70.1) | ||
| Ratio of personal to general medical information | 0.58 | 0.50 | 0.61 | 0.33 |
| (0.42) | (0.26) | (0.47) |
Table 4.
Results of Multiple Linear Regression Analyses of Genetic Counselor Informational Individuation (adjusted for scenario)
| Outcome variable | GC ratio of individualized to generalized information (RIAS) | |
|---|---|---|
| B (95% CI) |
P value | |
| IAT score | 0.17 | 0.21 |
| (−0.10 to 0.44) | ||
| SC race (White = reference) | 0.19 | 0.03 |
| (0.02 to 0.37) | ||
| IAT*SC race interaction (White = reference) | −0.32 | 0.05 |
| (−0.64 to −0.01) | ||
| Correlation coefficient (adjusted R2) | 0.23 | 0.01 |
| (0.17) | ||
3.2. Other measures of interpersonal dynamics
Descriptive statistics for GC and SC communication are presented in Table 5. GCs were significantly more emotionally responsive and made more facilitation and patient activation statements with minority SCs than with white SCs. Nevertheless, minority SCs asked fewer psychosocial questions and disclosed less psychosocial information relative to white SCs. In adjusted analyses (shown in Table 6.), statistical interaction between IAT score and SC race was significant for three outcomes: GC facilitation and client activation, SC’s provision of psychosocial and lifestyle information, and SC asking medical questions. For GC facilitation and activation, the negative interaction coefficient (β=−0.91, p=0.04) indicates that, when counseling minority SCs, GCs with higher IAT scores were less likely to use facilitation and activation strategies with minority relative to white SCs. There was also an effect of GCs IAT score on SCs communication. When in sessions with more pro-white scoring GCs, minority SCs’ disclosed less psychosocial and lifestyle information and asked fewer medical questions, reflected in negative interactive coefficients (β=−1.26, p<0.05; β=−1.61, p<0.01, respectively).
Table 5.
Client-centered communication – Descriptive statistics
| Outcome variable (mean (sd)) | Overall | White | Minority | p |
|---|---|---|---|---|
| N | 60 | 17 | 43 | NA |
| Client-centered communication categories | ||||
| Psychosocial questions: GC | 17.2 | 17.3 | 17.2 | 0.97 |
| (12.6) | (12.2) | (12.9) | ||
| Gives psychosocial information: GC | 42.4 | 46.9 | 40.7 | 0.28 |
| (20.0) | (13.0) | (22.0) | ||
| Emotional responsiveness: GC | 124.9 | 98.1 | 135.5 | 0.03 |
| (61.9) | (42.2) | (65.6) | ||
| Facilitation and patient activation: GC | 58.9 | 42.7 | 65.4 | 0.03 |
| (36.6) | (22.1) | (39.4) | ||
| Psychosocial questions: SC | 1.2 | 1.8 | 1.0 | 0.004 |
| (1.0) | (1.0) | (1.0) | ||
| Gives psychosocial information: SC | 40.2 | 45.0 | 38.3 | 0.03 |
| (32.4) | (34.3) | (31.8) | ||
| Emotional talk: SC | 16.9 | 14.5 | 17.9 | 0.35 |
| (12.5) | (10.0) | (13.4) | ||
| Medical questions: SC | 3.6 | 4.3 | 3.3 | 0.25 |
| (2.9) | (2.9) | (2.9) | ||
| Provider-centered communication categories | ||||
| Medical questions: GC | 50.2 | 45.9 | 51.9 | 0.39 |
| (24.0) | (25.6) | (23.4) | ||
| Procedural talk: GC | 21.3 | 20.0 | 21.8 | 0.53 |
| (10.1) | (8.4) | (10.7) | ||
| Gives biomedical information and counseling: GC | 355.6 | 369.5 | 350.1 | 0.50 |
| (98.8) | (100.3) | (98.8) | ||
| Gives biomedical information: SC | 67.9 | 63.2 | 69.7 | 0.44 |
| (29.1) | (24.9) | (30.7) |
Table 6.
Results of Multiple Linear Regression Analyses of Client Centeredness RIAS Component Categories
| Outcome variable | GC Facilitation and Client Activation | SC Gives Psychosocial and Lifestyle Information | SC Asks Medical Questions* | |||
|---|---|---|---|---|---|---|
| B (95% CI) |
P value | B (95% CI) |
P value | B (95% CI) |
P value | |
| IAT score | 0.62 | 0.10 | 0.85 | 0.12 | 1.29 | 0.01 |
| (−0.12 to 1.36) | (−0.22 to 1.92) | (0.69 to 1.76) | ||||
| SC race (White = reference) | 0.78 | 0.001 | 0.36 | 0.28 | 0.38 | 0.20 |
| (0.32 to 1.23) | (−0.30 to 1.01) | (−0.21 to 0.96) | ||||
| IAT*SC race interaction (White = reference) | −0.91 | 0.04 | −1.26 | 0.05 | −1.61 | 0.01 |
| (−1.76 to −0.05) | (−2.50 to −0.02) | (−2.71 to −0.51) | ||||
| Correlation coefficient (adjusted R2) | 0.18 | 0.01 | 0.08 | 0.20 | 0.25 | 0.003 |
| (0.17) | (0.03) | (0.19) | ||||
presence of spouse included as a covariate in model; data not shown
4. Discussion and Conclusion
4.1. Discussion
4.1.1. Individuation in communication
Consistent with our hypotheses, higher pro-white implicit bias was associated with less individually-framed information in the counseling of minority relative to white SCs. Our results suggest that implicit bias interferes with GCs’ ability to integrate minority SCs’ individual characteristics and needs on an informational and relational level. Our findings support hypothesized associations between implicit bias and facilitative communication strategies. These include strategies by which counselors cue active listening and elicit clients’ perspectives, thought processes, and reactions by asking for client opinion and checking that they understand clients’ disclosures. From the perspective of intergroup processes, facilitation and activation statements may be important in “re-categorizing” by creating a shared identity around mutual goals, as described by Gaertner and colleagues [12].
The negative relationship between implicit bias and SCs’ verbal behavior is notable. SCs’ disclosure of less lifestyle and psychosocial information may reflect a reciprocal effect through which pro-white bias cues clients to the GC’s lack of interest in psychosocial and lifestyle information, information that tends to be uniquely identifying. The failure to elicit this aspect of a client’s experience would be consistent with categorical processing. Minority clients may also be less willing to disclose personal information if they perceive the GC as showing disinterest or insensitivity. Minority clients may feel that they have less power to raise non-medical matters, which they may perceive as being less relevant to the conversation. Additionally, minority clients may accurately perceive GCs’ implicit bias, which may affect their level of trust and willingness to disclose psychosocial and lifestyle information or ask questions.
We found significant effects of GCs’ IAT scores and the interaction between IAT and SC race on the number of questions asked by SCs: relative to white SCs, minority SCs asked fewer medical questions when GCs had higher pro-white bias. Frequency of SC medical questions in the sample is low, with a mean of 3.6 questions asked per session. However, other studies have found associations between patient race and question-asking. In a study of 109 oncologist-patient interactions, Eggly and colleagues [25] found that black patients asked fewer questions and proportionally fewer direct questions of their oncologist than white patients, even after adjusting for education and income level. The authors suggest that this difference may have been due to patients’ perceptions of relative power in the interaction and patients’ reluctance to challenge the implicit physician-patient hierarchy. Although our study found no significant differences by race in the number of SC medical questions, we did find significant associations with IAT score and IAT-race interaction. Perhaps clinician racial bias contributes to the interactive dynamics of a medical visit, which subsequently influence patients’ question-asking. We also found that GCs were significantly more emotionally responsive and used more facilitation and activation statements with minority rather than white SCs. In a forthcoming manuscript, we discuss the possibility of a compensatory response, in which GCs may react to perceived difficulty in racially discordant communication by being more deliberate in their attempts to partner and communicate [26].
4.1.2. Implications for intervention
Although our intention in exploring informational individuation was to investigate its role in interpersonal processes, individual framing of information has also been associated with improved learning for genetic counseling clients. In an earlier analysis of the role of this variable, Roter and colleagues found that GCs’ use of individualized clinical information facilitated learning among analogue clients with limited literacy [27]. Consistent with those findings, a qualitative study with cancer GCs reported that patients preferred information they interpreted as relevant to their personal context [28]. Given our findings about racial bias, we suggest that failure to individually contextualize information may disproportionately affect clients who are both minorities and have literacy deficits. If genetic counselors provided individually contextualized information more consistently, this could benefit all clients.
We argue that individuation is not only an internal process associated with implicit bias, but also a patient-centered communication strategy that can be enhanced to improve patient education and the patient-provider relationship. Raising awareness about communication differences that are associated with implicit biases (such as GCs’ informational individuation and facilitative communication, as well as differences in clients’ communication patterns) could help clinicians to monitor their behavior and identify opportunities for more individualized communication. Theoretically, consistent individuation could reduce the reinforcing effect of stereotyping and social categorization. In the long term, clinicians who create conditions of equal power and mutual goals through effective communication may become less susceptible to stereotyping through repeated contact with members of other groups and more experience in identifying shared characteristics and values.
4.1.3. Limitations
This is a secondary analysis of a dataset that was intended to generate hypotheses, but which is statistically underpowered to detect associations with small but potentially meaningful clinical implications. Our results suggest a relationship between implicit bias and individualized communication style, which is not generalizable, but which invites replication in a larger and more contemporary sample. Since this sample of GCs was racially homogeneous, we were also unable to assess effects of GC race on communication. Additionally, there were few GCs in the sample with pro-Black or neutral implicit bias on IAT, which limits our ability to identify patterns in communication for these individuals.
We combined Black and Latino SCs in our analysis to maximize statistical power, which limits our ability to detect a difference in relationships between IAT score and cognitive or emotional exchange between the Black and Latino subgroups. However, this approach is consistent with the conceptualization of Black:White implicit bias as reflecting general in-group versus out-group social preferences [29]. Additionally, previous studies have found similar levels of implicit bias against both Blacks and Hispanics using separate IATs to evaluate both Black:White and Hispanic:White preferences among health care providers [6] and community members [6,30].
Using simulated clients presents a standardized task that allows for examining and comparing GCs’ communication behaviors. While possible that individual SCs’ communicative style could be confounded with SC race and ethnicity, we found no evidence that this was the case. Our exploration of ICCs and random effects models did not indicate evidence of clustering on SCs. Furthermore, a previous analysis indicated only small relative differences between individual SCs’ communication style [14].
The delay of 5–6 years between the phases during which communication data and IAT scores were collected is both an advantage and disadvantage to this study’s design. Since the IAT was administered after the simulated session, participants were not aware of a study hypothesis about implicit bias and race when the data were collected. While the dual process model suggests that implicit attitudes are likely to be more stable than explicit attitudes over time, there is empirical evidence from longitudinal studies that individuals’ IAT scores can shift based on positive or negative social or professional contact with members of a social out-group [31–33]. Since individuals’ implicit attitudes may have shifted in the years since they participated in the GCVP, measuring IAT scores several years after conducting the simulated sessions may have introduced random error at the individual level. However, random error would make it more likely that these analyses underestimate rather than overestimate the strength of the relationship between the GCs’ IAT scores and communication behavior.
The data for this study was collected in 2003–2004 and 2010. It is possible that increased awareness to implicit bias and cultural competence – both in clinical training and popular culture – may have changed in recent years. However, there is limited evidence of the effectiveness of cultural competence training in improving clinician behavior and client outcomes [34] and a recent review found limited and sometimes conflicting evidence for the effectiveness of interventions intended to reduce implicit bias and its negative effects [35]. One longitudinal study of 3,547 medical students found that having heard negative comments about African American patients and having unfavorable contact with African American physicians predicted increased pro-white IAT scores, suggesting that over the course of training, environmental factors and clinical experiences may undermine implicit bias interventions even if they are effective in the short term. The empirical literature on reducing implicit bias in clinical settings is relatively recent, with most intervention studies published within the past decade [36–41]. It remains to be seen whether bias-reducing interventions are effective and which practices are most effective.
Although possible that GCs currently practicing have characteristics that differ from those who participated in the original GCVP, there is no evidence of substantial change in racial, ethnic, gender, or regional diversity between the 2004 and 2019 Professional Status Surveys [10,24] and the GCVP participants were broadly representative of practicing GCs in 2003 and 2004 [13].
4.2. Conclusion
Our hypothesis regarding the relationship between implicit bias and individuation was supported in that GCs’ racial attitudes were associated with the use of this specific strategy of informational framing. Categorization, individuation, and the ability to create a shared in-group identity may influence how information is exchanged and the interpersonal dynamics of a genetic counseling interaction. This may have long-term implications for the reduction of implicit biases not only in genetic counseling, but medical practice more broadly. Future descriptive studies and interventions that address implicit racial bias and racial discordance should consider that individuation and categorization may affect communication on multiple levels.
4.3. Practice Implications
Few studies have tested interventions to reduce health care providers’ implicit bias and its negative effects on medical communication and outcomes [23] and we are unaware of any interventions of this kind developed for genetic counselors. Applying concepts from social psychological research on intergroup processes to genetic counseling may help to identify opportunities for intervention, inform clinical supervision practices, and improve educational approaches to cultural competence and communication training. We are intrigued by the potential of a training intervention to indirectly address implicit bias by reducing or ameliorating the negative consequences of bias by targeting clinician communication behaviors such as informational framing. We hope to conduct this type of work in the future. While more research is needed to identify specific communication skills to target through intervention, behavioral intervention strategies could potentially complement existing bias awareness and cultural competence training approaches.
Highlights.
Genetic counselors with more racial bias gave less personally-tailored information
Bias predicted additional correlates of less client-centered communication
Counselors’ biases may have negatively affected clients’ communication
Acknowledgements
We thank Susan Persky, Lori Erby, Julie S. Cohen, Kendra Schaa, and Sara Benjamin-Neelon.
Funding source and disclosure
This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interest
The authors declare they have no conflicts of interest.
REFERENCES
- [1].Johnson RL, Roter D, Powe NR, Cooper LA, Patient Race/Ethnicity and Quality of Patient–Physician Communication During Medical Visits, Am. J. Public Health. 94 (2004) 2084–2090. doi: 10.2105/AJPH.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR, Patient-centered communication, ratings of care, and concordance of patient and physician race, Ann. Intern. Med 139 (2003) 907–915. [DOI] [PubMed] [Google Scholar]
- [3].Siminoff LA, Graham GC, Gordon NH, Cancer communication patterns and the influence of patient characteristics: Disparities in information-giving and affective behaviors, Patient Educ. Couns 62 (2006) 355–360. doi: 10.1016/j.pec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- [4].Adams A, Realpe A, Vail L, Buckingham CD, Erby LH, Roter D, How doctors’ communication style and race concordance influence African-Caribbean patients when disclosing depression, Patient Educ. Couns 98 (2015) 1266–1273. doi: 10.1016/j.pec.2015.08.019. [DOI] [PubMed] [Google Scholar]
- [5].Alegría M, Roter DL, Valentine A, Chen C, Li X, Lin J, Rosen D, Lapatin S, Normand S-L, Larson S, Shrout PE, Patient-Clinician Ethnic Concordance and Communication in Mental Health Intake Visits, Patient Educ. Couns 93 (2013) 188–196. doi: 10.1016/j.pec.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Blair IV, Steiner JF, Fairclough DL, Hanratty R, Price DW, Hirsh HK, Wright LA, Bronsert M, Karimkhani E, Magid DJ, Havranek EP, Clinicians’ implicit ethnic/racial bias and perceptions of care among Black and Latino patients, Ann. Fam. Med 11 (2013) 43–52. doi: 10.1370/afm.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, Inui TS, The Associations of Clinicians’ Implicit Attitudes About Race With Medical Visit Communication and Patient Ratings of Interpersonal Care, Am. J. Public Health. 102 (2012) 979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Penner LA, Dovidio JF, West TV, Gaertner SL, Albrecht TL, Dailey RK, Markova T, Aversive racism and medical interactions with Black patients: A field study, J. Exp. Soc. Psychol 46 (2010) 436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Schaa KL, Roter DL, Biesecker BB, Cooper LA, Erby LH, Genetic counselors’ implicit racial attitudes and their relationship to communication, Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc 34 (2015) 111–119. doi: 10.1037/hea0000155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Professional Status Survey 2019: Demographics & Methodology, National Society of Genetic Counselors, Chicago, IL, 2019. [Google Scholar]
- [11].Brewer MB, Category-based vs. Person-based Perception in Intergroup Contexts, Eur. Rev. Soc. Psychol 9 (1998) 77–106. doi: 10.1080/14792779843000054. [DOI] [Google Scholar]
- [12].Gaertner SL, Dovidio JF, Anastasio PA, Bachman BA, Rust MC, The Common Ingroup Identity Model: Recategorization and the Reduction of Intergroup Bias, Eur. Rev. Soc. Psychol 4 (1993) 1–26. doi: 10.1080/14792779343000004. [DOI] [Google Scholar]
- [13].Roter D, Ellington L, Erby LH, Larson S, Dudley W, The Genetic Counseling Video Project (GCVP): models of practice, Am. J. Med. Genet. C Semin. Med. Genet 142C (2006) 209–220. doi: 10.1002/ajmg.c.30094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Erby LAH, Roter DL, Biesecker BB, Examination of standardized patient performance: accuracy and consistency of six standardized patients over time, Patient Educ. Couns 85 (2011) 194–200. doi: 10.1016/j.pec.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].FitzGerald C, Hurst S, Implicit bias in healthcare professionals: a systematic review, BMC Med. Ethics 18 (2017) 19. doi: 10.1186/s12910-017-0179-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, Eng E, Day SH, Coyne-Beasley T, Implicit Racial/Ethnic Bias Among Health Care Professionals and Its Influence on Health Care Outcomes: A Systematic Review, Am. J. Public Health. 105 (2015) e60–76. doi: 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Greenwald AG, Nosek BA, Banaji MR, Understanding and using the Implicit Association Test: I. An improved scoring algorithm., J. Pers. Soc. Psychol 85 (2003) 197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- [18].Roter D, Larson S, The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions, Patient Educ. Couns 46 (2002) 243–251. doi: 10.1016/S0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- [19].Wissow LS, Brown JD, Krupnick J, Therapeutic alliance in pediatric primary care: preliminary evidence for a relationship with physician communication style and mothers’ satisfaction, J. Dev. Behav. Pediatr. JDBP 31 (2010) 83–91. doi: 10.1097/DBP.0b013e3181cda770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Roter DL, Communication Patterns of Primary Care Physicians, JAMA J. Am. Med. Assoc 277 (1997) 350. doi: 10.1001/jama.1997.03540280088045. [DOI] [PubMed] [Google Scholar]
- [21].Mead N, Bower P, Measuring patient-centredness: a comparison of three observation-based instruments, Patient Educ. Couns 39 (2000) 71–80. doi: 10.1016/S0738-3991(99)00092-0. [DOI] [PubMed] [Google Scholar]
- [22].Guan Y, Roter DL, Wolff JL, Gitlin LN, Christensen KD, Roberts JS, Green RC, Erby LH, The impact of genetic counselors’ use of facilitative strategies on cognitive and emotional processing of genetic risk disclosure for Alzheimer’s disease, Patient Educ. Couns 101 (2018) 817–823. doi: 10.1016/j.pec.2017.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].R Core Team R: A language and environment for statistical computing, R Foundation for Statistical Computing, Vienna, Austria, 2018. https://www.R-project.org/. [Google Scholar]
- [24].Professional Status Survey 2004, National Society of Genetic Counselors, Chicago, IL, 2004. [Google Scholar]
- [25].Eggly S, Harper FWK, Penner LA, Gleason MJ, Foster T, Albrecht TL, Variation in question asking during cancer clinical interactions: A potential source of disparities in access to information, Patient Educ. Couns 82 (2011) 63–68. doi: 10.1016/j.pec.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Lowe C, Beach MC, Roter D, Genetic Counselor Implicit Bias and Its Effects on Cognitive and Affective Exchanges in Racially Discordant Simulations, (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Roter DL, Erby L, Larson S, Ellington L, Oral literacy demand of prenatal genetic counseling dialogue: Predictors of learning, Patient Educ. Couns 75 (2009) 392–397. doi: 10.1016/j.pec.2009.01.005. [DOI] [PubMed] [Google Scholar]
- [28].Joseph G, Pasick RJ, Schillinger D, Luce J, Guerra C, Cheng JKY, Information Mismatch: Cancer Risk Counseling with Diverse Underserved Patients, J. Genet. Couns 26 (2017) 1090–1104. doi: 10.1007/s10897-017-0089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR, Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity, J. Pers. Soc. Psychol 97 (2009) 17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- [30].Blair IV, Judd CM, Havranek EP, Steiner JF, Using Community Data to Test the Discriminate Validity of Ethnic/Racial Group IATs, Z. Psychol 218 (2010). doi: 10.1027/0044-3409/a000006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Anderssen N, Does contact with lesbians and gays lead to friendlier attitudes? a two year longitudinal study, J. Community Appl. Soc. Psychol 12 (2002) 124–136. doi: 10.1002/casp.665. [DOI] [Google Scholar]
- [32].van Ryn M, Hardeman R, Phelan SM, PhD DJB, Dovidio JF, Herrin J, Burke SE, Nelson DB, Perry S, Yeazel M, Przedworski JM, Medical School Experiences Associated with Change in Implicit Racial Bias Among 3547 Students: A Medical Student CHANGES Study Report, J. Gen. Intern. Med 30 (2015) 1748–1756. doi: 10.1007/s11606-015-3447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Phelan SM, Dovidio JF, Puhl RM, Burgess DJ, Nelson DB, Yeazel MW, Hardeman R, Perry S, van Ryn M, Implicit and explicit weight bias in a national sample of 4,732 medical students: The medical student CHANGES study, Obesity. 22 (2014) 1201–1208. doi: 10.1002/oby.20687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Horvat L, Horey D, Romios P, Kis‐ Rigo J, Cultural competence education for health professionals, Cochrane Database Syst. Rev (2014). doi: 10.1002/14651858.CD009405.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Zestcott CA, Blair IV, Stone J, Examining the Presence, Consequences, and Reduction of Implicit Bias in Health Care: A Narrative Review, Group Process. Intergroup Relat. GPIR 19 (2016) 528–542. doi: 10.1177/1368430216642029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Devine PG, Forscher PS, Austin AJ, Cox WTL, Long-term reduction in implicit race bias: A prejudice habit-breaking intervention, J. Exp. Soc. Psychol 48 (2012) 1267–1278. doi: 10.1016/j.jesp.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Teal CR, Gill AC, Green AR, Crandall S, Helping medical learners recognise and manage unconscious bias toward certain patient groups, Med. Educ 46 (2012) 80–88. doi: 10.1111/j.1365-2923.2011.04101.x. [DOI] [PubMed] [Google Scholar]
- [38].Chapman MV, Hall WJ, Lee K, Colby R, Coyne-Beasley T, Day S, Eng E, Lightfoot AF, Merino Y, Simán FM, Thomas T, Thatcher K, Payne K, Making a difference in medical trainees’ attitudes toward Latino patients: A pilot study of an intervention to modify implicit and explicit attitudes, Soc. Sci. Med 199 (2018) 202–208. doi: 10.1016/j.socscimed.2017.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Gonzalez CM, Kim MY, Marantz PR, Implicit Bias and Its Relation to Health Disparities: A Teaching Program and Survey of Medical Students, Teach. Learn. Med 26 (2014) 64–71. doi: 10.1080/10401334.2013.857341. [DOI] [PubMed] [Google Scholar]
- [40].Leslie KF, Sawning S, Shaw MA, Martin LJ, Simpson RC, Stephens JE, Jones VF, Changes in medical student implicit attitudes following a health equity curricular intervention, Med. Teach 40 (2018) 372–378. doi: 10.1080/0142159X.2017.1403014. [DOI] [PubMed] [Google Scholar]
- [41].Wijayatunga NN, Kim Y, Butsch WS, Dhurandhar EJ, The effects of a teaching intervention on weight bias among kinesiology undergraduate students, Int. J. Obes (2019). doi: 10.1038/s41366-019-0325-0. [DOI] [PubMed] [Google Scholar]