Abstract
The antidiabetic, hypoglycemic and oral glucose tolerance test (OGTT) activities of zinc oxide nanoparticles (ZnONPs) were assessed in mice. ZnONPs were prepared by reacting Zn(NO3)2.6H2O and NaOH solution at 70°C with continuous stirring and then characterized by transmission electron microscopy (TEM) and scanning electron microscopy (SEM) techniques. Diabetes was induced by the intraperitoneal injection of streptozotocin (STZ) in mice, and then the blood glucose levels were determined by the glucose oxidase method. The experimental results revealed that ZnONPs suggestively (p<0.001) declined the blood glucose levels (39.79%), while these reductions were 38.78% for the cotreatment of ZnONPs and insulin, and 48.60% for insulin, respectively. In the hypoglycemic study, ZnONPs (8 and 14 mg/kg b.w) reduced approximately 25.13 and 29.15% of blood glucose levels, respectively. A similar reduction was found in the OGTT test, which is also a dose- and time-dependent manner. Overall, ZnONPs possess a potential antidiabetic activity, which could be validated by further mechanistic studies.
Keywords: antidiabetic, insulin, oral glucose tolerance test, streptozotocin, ZnONPs
Introduction
The epidemic metabolic disorder, diabetes mellitus (DM) is characterized by high blood glucose where the patient cannot produce adequate insulin, or body cells do not respond to glucose produced by β-cells in the pancreas. Many people have diabetes all over the world [1–3], and the number is increasing at an alarming rate. According to the World Health Organization, diabetes causes 1.5 million deaths each year worldwide, being one of the most recurrent cause of mortality in developed countries [2]. The high blood sugar of diabetic patients leads to the typical symptoms of polyuria, polydipsia and polyphagia [4]. The development of several medications with multiple modes of actions having glucose-lowering activity is needed to manage diabetes. Many researchers have proved that the role of trace metals with glucose metabolism and their relationship with diabetes. Zinc [5], magnesium [6] and chromium [7] have reported to play a role in blood sugar maintenance and used in diabetes therapy. Over 300 enzymes are activated by zinc in the body, and it plays a crucial role in different metabolic pathways, including glucose metabolism [8]. Zinc is also known to keep the structure of insulin [9] and plays a vital role in insulin biosynthesis, storage and secretion [10]. It has been proved by researches that several zinc transporters in pancreatic β-cells like zinc transporter-8 have a potent role in insulin secretion [11,12]. By following numerous mechanisms, including increased phosphorylation of insulin receptor, enhanced phosphoinositide 3-kinases activity and inhibited glycogen synthase kinase-3, zinc also could improve insulin signaling [13]. Therefore, there is a very complex inter-relationship between zinc, diabetes and diabetic complications and related diabetic symptoms.
Simpler and painless routes for insulin administration are still in demand to manage diabetes as conventional drug delivery systems still have numerous drawbacks, including improper and/or ineffective dosage, low potency, limited specificity for the target, which may result in adverse side effects in other organs/tissues. The use of natural products could be the potential to encounter the limitations of DM treatment [2,14,15]. To overcome the pharmacokinetic limitations of drugs, the novel drug delivery system has considered as an attractive option to deliver the drugs for treating several diseases and disorders [2,16–18]. The loading of insulin, and other sugar-lowering drugs and nutraceuticals, into nanoparticles, has been proposed as a more convenient, non-invasive and safer approach through alternative administration routes [2].
Zinc oxide nanoparticles (ZnONPs), a novel agent to deliver zinc, have great implications in many disease therapies including DM [19]. The development of zinc-based agent would be promising in the treatment of diabetes and its associated complications as zinc supplement have shown ameliorating effect in preclinical studies [19,20]. Alkaladi et al. (2014) [21] studied the antidiabetic role of ZnONPs through induction of insulin, insulin receptors and glucose metabolizing enzymes gene expression. Umrani and Paknikar [22] proved the role of ZnONPs for controlling blood glucose in diabetic rats in the same line. In both studies, they monitored the effect of ZnONPs on diabetic rats only; therefore, in the present study, we tested ZnONPs to validate its effect against diabetes; therefore, we used the mouse models to assess its hypoglycemic and glucose tolerance effects as its effect is already studied in the rat models.
Materials and methods
Materials
Streptozotocin (STZ; Sigma Chemical Co. Ltd., U.K.), NaOH (Loba Chemie, India), ZnO (Loba Chemie, India). ACCU-CHEK active blood glucose meter (Roche Diagnostics Ltd, U.K., serial #GU 02591300). All other chemicals were of analytical grade and obtained from the Laboratory of the Department of Pharmacy, Noakhali Science and Technology University, Bangladesh.
Experimental animals
A total number of 60 mature Swiss albino mice (weight: 22–25 g) were used in the present study. Mice were obtained from the animal house of Jahangirnagar University (JU), Bangladesh. Mice were housed in separate metal cages while maintaining constant environment and nutritional conditions. Fresh and clean drinking water was supplied ad libitum through the specific nipple. The cages of the mice were cleaned regularly, and water and food were supplied twice daily. Acclimatization was done for 7 days before conducting the experiments. All animal experiments were conducted at the Department of Pharmacy, Noakhali Science and Technology University, Bangladesh.
Synthesis of ZnONPs
ZnONPs were prepared by using the method of Gusatti et al. (2011) [23] with slight modification. First, 0.5 M ZnNO3 hexahydrate solution and 1 M NaOH solution were prepared, and the necessary solution was heated up to 70°C and stirred continuously with a magnetic stirrer. Then, ZnNO3 hexahydrate solution was added dropwise into the primary solution slowly with continuous stirring. A white solution of ZnO was observed; in fact, the nanoparticles were dispersed into this white solution. After finishing the addition of ZnNO3 hexahydrate, the mixture was stirred for 2 h more which was followed by cooling. Prepared ZnONPs were filtered and washed by deionized water. Finally, the ZnONPs containing suspension were dried at 65°C for obtaining the white solid residue. These particles were characterized before starting our experiments.
Characterization studies
Transmission electron microscopy (TEM) (JEM 1400 plus, JEOL Ltd., Japan) and scanning electron microscopy (SEM) (JCM 5700, JEOL Ltd., Japan) was employed to determine the size, shape and morphology of ZnONPs. The study was conducted at the Departmental Laboratory of Applied Chemistry and Biochemistry, Kumamoto University, Japan.
Induction of experimental diabetes
Multiple intraperitoneal (i.p.) injection (45 mg/kg body wt.) of STZ was used to induce diabetes in experimental mice. STZ was dissolved in freshly prepared 0.01 M sodium citrate buffer (pH = 4.5) and administered on mice for 5 consecutive days. After STZ injection, the animals could drink glucose solution (5% w/v) overnight to avoid hypoglycemia which might be induced by STZ. Control mice received an equivalent amount of vehicle (citrate buffer) only. When the dosing was completed, STZ-treated mice were kept in normal conditions for 5 days. In fact, after this duration, mice had developed diabetes (blood glucose levels ≥ 11.1 mmol/l) at fasting conditions. The STZ-treated mice were fastened for 12 h, and blood samples were collected from the tail vein for determining the blood glucose levels. Mice in the diabetic group with fasting blood glucose levels higher than 11.1 mmol/l were considered as diabetic, and hence they were selected for further studies.
Animal grouping
For the antidiabetic activity test, the diabetic mice were randomly subdivided into four groups containing five mice in each group. We have followed the experimental procedure of Alkaladi et al. (2014) for this test [21]. Mice were grouped as G-I group for control, where mice were only treated with distilled water. G-II (ZnONPs treated), G-III (ZnONPs and insulin-treated) and G-IV stand for the standard treated group where diabetic mice were injected with insulin 0.4 U/50 mg subcutaneously (s.c.). Each group received their respective doses for consecutive 14 days.
In the hypoglycemic study, 20 mice were taken and grouped into four groups and test was done according to the method of Farag et al. (2014) [24]. Grouping of mice were done as: G-I (control: distilled water, 1 ml/mice, oral), G-II (ZnONPs: 8 mg/kg b.w., oral), G-III (ZnONPs: 14 mg/kg b.w., oral) and G-IV (standard: glibenclamide, 10 mg/kg b.w., oral).
In terms of oral glucose tolerance test (OGTT), we used the method described by Andrikopoulos et al. (2008) [25]. Mice were given 2 g/kg glucose levels orally after 6 h of fasting, and glucose was given orally a few minutes before ZnONPs dosing. Blood glucose was measured at 0, 15, 30, 60, 90 min. Mice were grouped into G-I (control: distilled water, 1 ml/mice, oral), G-II (ZnONPs: 8 mg/kg b.w., oral), G-III (ZnONPs: 14 mg/kg b.w., oral) and G-IV (standard: glibenclamide, 10 mg/kg b.w., oral), where each group contained five mice. Mice were not subjected to killing as tissues were not investigated in the present study.
Biochemical determination
By following the glucose oxidase method using the ‘ACCU-CHEK Active’ kit, the blood glucose levels were determined. The blood glucose levels were measured in all experimental animals before the beginning of the experimental procedures. Fasting blood glucose levels were routinely measured until diabetes was confirmed (mice with fasting blood glucose ≥ 11.1 mmol/l was considered as diabetic).
Sampling protocol
Blood samples (2–3 µl blood) were collected from the tail vein of all experimental mice. The blood glucose levels were monitored by ACCU-CHEK active blood glucose meter.
Statistical analysis
Data were analyzed using one-way ANOVA tests (SPSS software, version-20) followed by Dunnett’s t tests. *p≤0.05 was considered statistically significant, **p≤0.01 moderately significant and ***p≤0.001 highly statistically significant. Values were expressed as mean ± standard error of the mean (S.E.M.) Origin Pro (ver. 8.5, Origin Lab. Corp., U.S.A.) was used for preparing graphical representations.
Results
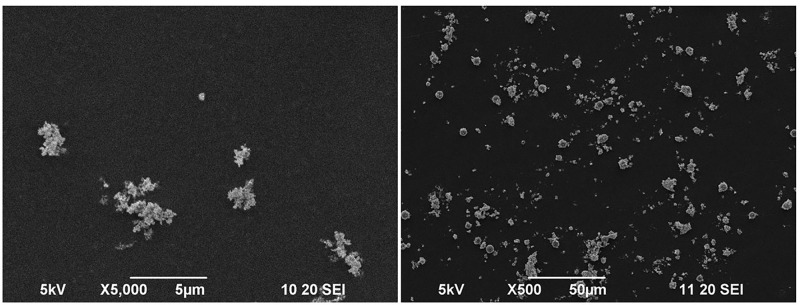
Characterization of ZnONPs using SEM and TEM imaging
High-resolution SEM and TEM imaging were performed for getting the information about structural morphology, size and shape of the synthesized ZnONPs. It was found that most of the ZnONPs were non-spherical; however, some of them were roughly circular (Figures 1 and 2). The size of synthesized nanoparticles was less than 100 nm in most of the cases. However, few particles were more significant than this. The larger ZnONPs found in SEM measurement may be due to the accretion of the smaller ones.
Figure 1. SEM image of ZnONPs. Synthesized nanoparticles were <100 nm in most of the cases; however, few particles are more abundant.
This may happen due to the aggregation of smaller particles after synthesis.
Figure 2. TEM image of ZnONPs.
Most of the nanoparticles were non-spherical; however, some are roughly circular. Most of the synthesized nanoparticles were less than 100 nm in size.
Assessment of antidiabetic activity of ZnONPs
The therapeutic effect of ZnONPs on STZ-induced diabetic mice, as well as their compared effect on insulin treatment, were assessed. The results showed a significant reduction in blood glucose levels in the mice of G-II (ZnONPs treated) and G-III (ZnONPs and insulin-treated) when compared with diabetic non-treated mice, G-I (control) Table 1.
Table 1. Antidiabetic effect of ZnONPs on STZ-induced diabetic mice.
| Groups | Blood glucose levels (mmol/l) | |||
|---|---|---|---|---|
| Dose | Fasting glucose levels | Glucose levels after 2 h | % of inhibition | |
| G-I (Control: Distilled water) | 1 ml/mice (oral) | 18.68 ± 0.34 | 18.54 ± 0.16 | - |
| G-II (ZnONPs) | 14 mg/kg b.w. (oral) | 18.32 ± 0.22 | 11.04 ± 0.22* | 39.74 |
| G-III (ZnONPs + Insulin) | 7 mg/kg b.w. (oral) + 0.2 U/50 g (s.c.) | 18.62 ± 0.27 | 11.40 ± 0.21* | 38.78 |
| G-IV (Standard: Insulin) | 0.4 U/50 g (s.c.) | 18.60 ± 0.19 | 9.56 ± 0.32* | 48.60 |
Mean ± S.E.M. (n=5). Data were analyzed using one-way ANOVA followed by Dunnett’s t test and compared with control.
P<0.005 was considered significant.
Assessment of hypoglycemic activity of ZnONPs
It was found that a sharp and significant decrease in glucose levels were attained when mice were treated with ZnONPs mild dose (G-II: 25.13% inhibition) and ZnONPs moderate dose (G-III: 29.15% inhibition). Standard drug (glibenclamide) can reduce 49.25% reduction in blood glucose levels (G-IV) (Table 2).
Table 2. Hypoglycemic activity of ZnONPs.
| Groups | Blood glucose levels (mmol/l) | |||
|---|---|---|---|---|
| Dose | Fasting glucose levels at 0 h | Glucose levels after 2 h | % of inhibition | |
| G-I (Control: Distilled water) | 1 ml/ mice (oral) | 4.10 ± 0.12 | 3.98 ± 0.06 | - |
| G-II (ZnONPs, mild dose) | 8 mg/kg b.w. (oral) | 3.84 ± 0.19 | 2.98 ± 0.15* | 25.13 |
| G-III (ZnONPs, moderate dose) | 14 mg/kg b.w. (oral) | 4.12 ± 0.13 | 2.82 ± 0.12† | 29.15 |
| G-IV (Standard: Glibenclamide) | 10 mg/kg b.w. (oral) | 4.04 ± 0.10 | 2.02 ± 0.15† | 49.25 |
Mean ± S.E.M. (n=5). Data were analyzed using one-way ANOVA followed by Dunnett’s t test and compared with control.
P<0.01.
P<0.005 was considered significant.
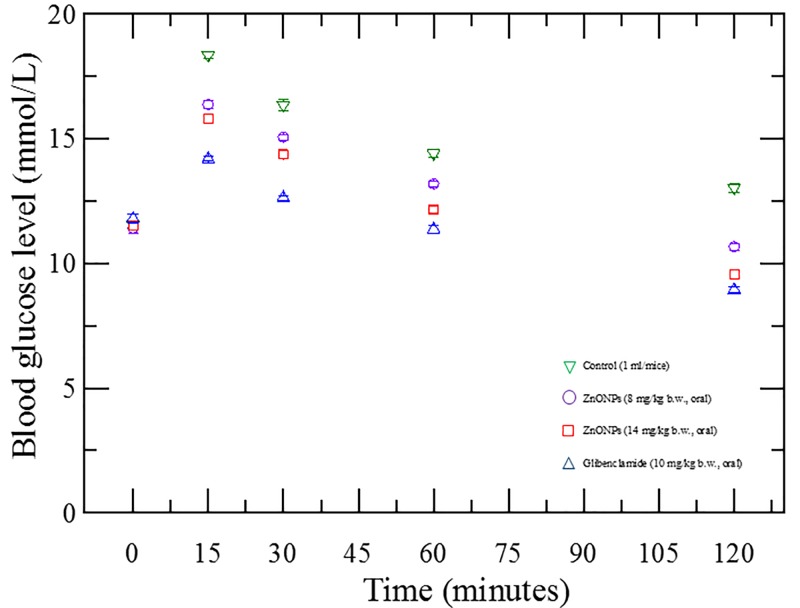
Assessment of OGTT of ZnONPs
ZnONPs (8 mg/kg b.w. for G-II and 14 mg/kg b.w. for G-III mice) significantly reduced the blood glucose levels at 15, 30, 60 and 120 min time interval when compared with control (G-I). Glibenclamide (G-IV) was used as a standard in this experiment. The treatment of ZnONPs resulted in suppression of blood glucose levels of mice is shown in Figure 3.
Figure 3. Oral glucose tolerance effect of ZnONPs.
The figure shows that ZnONPs have a significant blood glucose levels lowering activity and the response follows dose-dependent manner(s).
Discussion
Nanoparticles of many metals such as: zinc, silver, iron and gold oxides have revealed a significant role in medical and biological applications [26]. In this experiment, the administration of ZnONPs to diabetic mice resulted in a considerable reduction in fasted blood glucose levels. The key mechanism of hyperglycemia involves over-production (hepatic glycogenolysis and gluconeogenesis) and decreased utilization of glucose by the tissues [27]. Our result revealed that ZnONPs significantly reduced the glucose levels in STZ-induced diabetic mice. Almost 39.74 and 38.78% reduction in blood glucose levels were found for the groups of mice- ZnONPs, (ZnONPs + insulin), respectively (Table 1) when compared with the control group. STZ may enter the β-cell via a glucose transporter and causes alkylation of DNA [28]. DNA damage induces activation of poly-ADP-ribosylation, a process that is more important for the diabetogenicity of STZ than DNA damage itself. Zinc may provide insulin-like effects in the signal transduction mechanism of insulin and reduce the production of cytokines, which leads to β-cell death due to inflammation in the pancreas during diabetes [13]. According to the study of Alkaladi et al. (2014) [21], ZnONPs can increase serum insulin levels and increase the expression of mRNA of the insulin gene. Other studies found that glucose-stimulated insulin secretion is enhanced by zinc through isolated pancreatic islets of rats [29]. Here ZnONPs may play a role in improving the glucose utilization and metabolism through influencing the improvement of hepatic glycogenesis. ZnONPs may act on the insulin signaling pathway in this aspect [30]. Our study is found to be consistent with the finding of Alkaladi et al. (2014) [21].
The hypoglycemic activity test was done by using two doses of ZnONPs (8 mg/kg and 14 mg/kg b.w. of mice). ZnONPs showed a positive result in hypoglycemia test. It reduced the blood glucose levels significantly (25.13%) for mild dose and (29.15%) for a moderate dose. The standard drug glibenclamide reduced (49.25%) blood glucose levels. It is well established that sulphonylureas (e.g., glibenclamide) cause hypoglycemia by stimulating insulin release from pancreatic β-cell [31]. The comparable effect of the ZnONPs with glibenclamide suggests the possibility of a similar mode of action.
In OGTT, the serum glucose levels of normal mice reached a peak significantly after 15 min nONPs dosing. Mice were given glucose orally (2 g/kg b.w. of mice) just a few minutes before the ZnONPs sampling. We found that blood glucose levels decrease gradually within 2 h. A single administration of ZnONPs dose resulted in prominent glucose suppression during OGTT, which confirm the possibility of antidiabetic effect. The results of our study endorse the finding of Umrani and Paknikar (2014) [22].
Many in vitro and in vivo experiments have verified that zinc has beneficial effects in both type-1 and type-2 diabetes. It is discernible from the findings of the study that zinc plays an essential role in β-cell functioning, glucose homeostasis, the pathogenesis of diabetes and diabetes complications. The purpose of zinc in diabetes has been established by supplementation studies in diabetic rats [32]. Several zinc complexes were synthesized, and they are proven to be very useful in the biological system [33,34]. Many types of research demonstrate that zinc is secreted along with insulin served as an autocrine molecule which enhances the glucose-stimulated insulin secretion from the rat-isolated pancreatic islets [29]. Our experiments revealed that ZnONPs lowered blood glucose levels in diabetic mice significantly. Based on our experimental results, we can suggest that ZnONPs might act as an insulin secretagogue. In the single-dose OGTT study, experimental mice showed an elevated blood glucose levels which reduced after 2 h. Similarly, ZnONPs dose reduced the blood glucose levels just like the antidiabetic action of ZnONPs. As STZ mimic the effect of type-1 diabetes, there is less amount of β-cell mass in the pancreas.
Further, zinc has been reported to regulate glucagon secretion from pancreatic α-cells [35]. Consequently, glucagon-stimulated hepatic pathways (i.e., gluconeogenesis, glycogenesis) would be inhibited in the fasting state of mice which may lead to reduced blood glucose levels after zinc dosing. In the case of hypoglycemic action, the fasting blood glucose levels in healthy mice were in a control state; however, the single-dose administration of ZnONPs significantly reduced the blood glucose levels. Glibenclamide is used in both hypoglycemic and glucose tolerance test as a controlled drug, and it is used in type-2 diabetes. The test groups (G-II, G-III) significantly reduced blood glucose level; that means ZnONP has a significant role in controlling Type-2 diabetes by reducing the production of inflammatory cytokines [13]. Comparing this point of view, ZnONPs may be a potential candidate of agent for controlling Type-2 diabetes. This may be due to the activation of another physiological pathway such as insulin secretion, glucagon regulation and accumulation of glucose in the liver and adipose tissue. Zinc transporters are also recognized in adipose tissues and liver as these organs are the critical regulator of glucose metabolism [36].
Conclusion
Considering the data, ZnONPs showed promising antidiabetic activity, which could be potential in developing an antidiabetic drug. However, this study did not investigate the physiological parameters and molecular mechanisms of ZnONPs; therefore, further mechanistic studies are warranted to supports its antidiabetic action in mice.
Abbreviations
- DM
diabetes mellitus
- OGTT
oral glucose tolerance test
- SEM
scanning electron microscopy
- STZ
streptozotocin
- TEM
transmission electron microscopy
- ZnONP
zinc oxide nanoparticle
Contributor Information
Md. Mamun Or Rashid, Email: mamun.orrashid@nstu.edu.bd.
Md. Jakaria, Email: md.jakaria@florey.edu.au.
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
The authors declare that there are no sources of funding to be acknowledged.
Open Access
Open access for this article was enabled by the participation of University of Melbourne in an all-inclusive Read & Publish pilot with Portland Press and the Biochemical Society under a transformative agreement with CAUL.
Author Contribution
S.A.S. conducted the laboratory works and drafted the manuscript. M.M.O.R. supervised the study progression. M.G.U., F.N.R., M.S.H. and M.A.H. helped in conducting experiments and data analysis. M.J. reviewed, edited and revised the manuscript, and handled the correspondence. All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Ethics Approval
Ethical approval was taken for handling mice (for the present study) from the institutional ethical committee before starting experiment. ‘Principles of the laboratory animal care’ (NIH publication no. 85-23, revised 1985) and ‘national animal care laws’ were strictly followed during handing of these animals for the study.
References
- 1.Lin Y. and Sun Z. (2010) Current views on type 2 diabetes. J. Endocrinol. 204, 1 10.1677/JOE-09-0260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Souto E.B., Souto S.B., Campos J.R. et al. (2019) Nanoparticle delivery systems in the treatment of diabetes complications. Molecules 24, 4209 10.3390/molecules24234209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vieira R., Souto S.B., Sanchez-Lopez E. et al. (2019) Sugar-lowering drugs for type 2 diabetes mellitus and metabolic syndrome-strategies for in vivo administration: part-II. J. Clin. Med. 8, 152 10.3390/jcm8091332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wild S., Roglic G., Green A., Sicree R. and King H. (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27, 1047–1053 10.2337/diacare.27.5.1047 [DOI] [PubMed] [Google Scholar]
- 5.Arthur B. and Chausmer S. (1998) Zinc, insulin and diabetes. J. Am. Coll. Nutr. 17, 109–115 [DOI] [PubMed] [Google Scholar]
- 6.Wells I.C. (2008) Evidence that the etiology of the syndrome containing type 2 diabetes mellitus results from abnormal magnesium metabolism. Canadian J. Physiol. Pharmacol. 86, 16–24 10.1139/Y07-122 [DOI] [PubMed] [Google Scholar]
- 7.Wang Z.Q. and Cefalu W.T. (2010) Current concepts about chromium supplementation in type 2 diabetes and insulin resistance. Curr. Diabetes Rep. 10, 145–151 10.1007/s11892-010-0097-3 [DOI] [PubMed] [Google Scholar]
- 8.Haase H., Overbeck S. and Rink L. (2008) Zinc supplementation for the treatment or prevention of disease: current status and future perspectives. Exp. Gerontol. 43, 394–408 10.1016/j.exger.2007.12.002 [DOI] [PubMed] [Google Scholar]
- 9.Sun Q., Van Dam R.M., Willett W.C. and Hu F.B. (2009) Prospective study of zinc intake and risk of type 2 diabetes in women. Diabetes Care 32, 629–634 10.2337/dc08-1913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edmin S., Dodson G. and Cutfield S. (1980) Role of zinc in insulin biosynthesis: some possible zinc insulin interactions in the pancreatic beta cells. Diabetologia 19, 174–182 [DOI] [PubMed] [Google Scholar]
- 11.Smidt K., Jessen N., Petersen A.B. et al. (2009) SLC30A3 responds to glucose-and zinc variations in ß-cells and Is critical for insulin production and in vivo glucose-metabolism during ß-cell stress. PLoS ONE 4, e5684 10.1371/journal.pone.0005684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rungby J. (2010) Zinc, zinc transporters and diabetes. Diabetologia 53, 1549–1551 10.1007/s00125-010-1793-x [DOI] [PubMed] [Google Scholar]
- 13.Jansen J., Karges W. and Rink L. (2009) Zinc and diabetes—clinical links and molecular mechanisms. J. Nutr. Biochem. 20, 399–417 10.1016/j.jnutbio.2009.01.009 [DOI] [PubMed] [Google Scholar]
- 14.Salehi B., Ata A., Vak N. et al. (2019) Antidiabetic potential of medicinal plants and their active components. Biomolecules 9, 551 10.3390/biom9100551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Daliu P., Annunziata G., Tenore G.C. and Santini A. (2020) Abscisic acid identification in Okra, Abelmoschus esculentus L. (Moench): perspective nutraceutical use for the treatment of diabetes. Nat. Product. Res. 34, 3–9 10.1080/14786419.2019.1637874 [DOI] [PubMed] [Google Scholar]
- 16.Jakaria M., Cho D-Y, Haque E. et al. (2018) Neuropharmacological potential and delivery prospects of thymoquinone for neurological disorders. Oxid. Med. Cell. Long. 2018, 1209801 10.1155/2018/1209801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jakaria M., Azam S., Haque M.E. et al. (2019) Taurine and its analogs in neurological disorders: Focus on therapeutic potential and molecular mechanisms. Redox Biol. 24, 101223 10.1016/j.redox.2019.101223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jakaria M., Haque M.E., Kim J., Cho D.-Y., Kim I.-S. and Choi D.-K. (2018) Active ginseng components in cognitive impairment: therapeutic potential and prospects for delivery and clinical study. Oncotarget 9, 33601–33620 10.18632/oncotarget.26035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang K.S. (2019) The current and future perspectives of zinc oxide nanoparticles in the treatment of diabetes mellitus. Life Sci. 239, 117011 10.1016/j.lfs.2019.117011 [DOI] [PubMed] [Google Scholar]
- 20.Ukperoro J.U., Offiah N., Idris T. and Awogoke D. (2010) Antioxidant effect of zinc, selenium and their combination on the liver and kidney of alloxan-induced diabetes in rats. Mediterrinean J. Nutr. Metab. 3, 25–30 10.3233/s12349-009-0069-9 [DOI] [Google Scholar]
- 21.Alkaladi A., Abdelazim A. and Afifi M. (2014) Antidiabetic activity of zinc oxide and silver nanoparticles on streptozotocin-induced diabetic rats. Int. J. Mol. Sci. 15, 2015–2023 10.3390/ijms15022015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Umrani R.D. and Paknikar K.M. (2014) Zinc oxide nanoparticles show antidiabetic activity in streptozotocin-induced Type 1 and 2 diabetic rats. Nanomedicine 9, 89–104 10.2217/nnm.12.205 [DOI] [PubMed] [Google Scholar]
- 23.Gusatti M., Barroso G.S., Campos C.E.M.d. et al. (2011) Effect of different precursors in the chemical synthesis of ZnO nanocrystals. Mater. Res. 14, 264–267 10.1590/S1516-14392011005000035 [DOI] [Google Scholar]
- 24.Farag M., Al-Rehaily A., Ahmad M.S. and Mothana R.A. (2014) Detection of hypoglycemic and antidiabetic fraction in ethanol extract of Jatropha curcas aerial parts. Pharmacol. Pharmacy 5, 663 10.4236/pp.2014.57076 [DOI] [Google Scholar]
- 25.Andrikopoulos S., Blair A.R., Deluca N., Fam B.C. and Proietto J. (2008) Evaluating the glucose tolerance test in mice. Am. J. Physiol. Endocrinol. Metab. 295, E1323–E1332 10.1152/ajpendo.90617.2008 [DOI] [PubMed] [Google Scholar]
- 26.Hirst S.M., Karakoti A.S., Tyler R.D., Sriranganathan N., Seal S. and Reilly C.M. (2009) Anti‐inflammatory properties of cerium oxide nanoparticles. Small 5, 2848–2856 10.1002/smll.200901048 [DOI] [PubMed] [Google Scholar]
- 27.Lin H.V. and Accili D. (2011) Hormonal regulation of hepatic glucose production in health and disease. Cell Metab. 14, 9–19 10.1016/j.cmet.2011.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goud B., Dwarakanath V. and Chikka B. (2015) Streptozotocin-a diabetogenic agent in animal models. Int. J. Pharmacy Pharma. Res. 3, 253–269 [Google Scholar]
- 29.Richards-Williams C., Contreras J.L., Berecek K.H. and Schwiebert E.M. (2008) Extracellular ATP and zinc are co-secreted with insulin and activate multiple P2X purinergic receptor channels expressed by islet beta-cells to potentiate insulin secretion. Purinergic Signal. 4, 393 10.1007/s11302-008-9126-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quesada I., Tudurí E., Ripoll C. and Nadal A. (2008) Physiology of the pancreatic α-cell and glucagon secretion: role in glucose homeostasis and diabetes. J. Endocrinol. 199, 5–19 10.1677/JOE-08-0290 [DOI] [PubMed] [Google Scholar]
- 31.Sola D., Rossi L., Schianca G.P.C. et al. (2015) Sulfonylureas and their use in clinical practice. Arch. Med. Sci. 11, 840 10.5114/aoms.2015.53304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bolkent S., Yanardag R., Bolkent S. and Mutlu O. (2009) The influence of zinc supplementation on the pancreas of streptozotocin-diabetic rats. Dig. Dis. Sci. 54, 2583 10.1007/s10620-008-0675-2 [DOI] [PubMed] [Google Scholar]
- 33.Karmaker S., Saha T.K., Yoshikawa Y. and Sakurai H. (2009) A zinc (II)/poly (γ‐glutamic acid) complex as an oral therapeutic for the treatment of type‐2 diabetic KKAy mice. Macromol. Biosci. 9, 279–286 10.1002/mabi.200800190 [DOI] [PubMed] [Google Scholar]
- 34.Yoshikawa Y., Adachi Y., Yasui H., Hattori M. and Sakurai H. (2011) Oral administration of bis (aspirinato) zinc (II) complex ameliorates hyperglycemia and metabolic syndrome-like disorders in spontaneously diabetic KK-Ay mice: structure–activity relationship on zinc–salicylate complexes. Chem. Pharma. Bull. 59, 972–977 10.1248/cpb.59.972 [DOI] [PubMed] [Google Scholar]
- 35.Egefjord L., Petersen A.B., Bak A.M. and Rungby J. (2010) Zinc, alpha cells and glucagon secretion. Curr. Diabetes Rev. 6, 52–57 10.2174/157339910790442655 [DOI] [PubMed] [Google Scholar]
- 36.Mahoney B.A., Smith W.A., Lo D.S., Tsoi K., Tonelli M. and Clase C.M. (2005) Emergency interventions for hyperkalaemia. Cochrane Database Syst. Rev. 2, CD003235. [DOI] [PMC free article] [PubMed] [Google Scholar]