Abstract
Hydrogels are polymeric networks having the ability to absorb a large volume of water. Flexibility, versatility, stimuli-responsive, soft structure are the advantages of hydrogels. It is classified based on its source, preparation, ionic charge, response, crosslinking and physical properties. Hydrogels are used in various fields like agriculture, food industry, biosensor, biomedical, etc. Even though hydrogels are used in various industries, more researches are going in the field of biomedical applications because of its resembles to living tissue, biocompatibility, and biodegradability. Here, we are mainly focused on the commercially available hydrogels used for biomedical applications like wound dressings, contact lenses, cosmetic applications, tissue engineering, and drug delivery.
Keywords: Materials science, Biomedical engineering, Nanotechnology, Biotechnology, Hydrogels, Biomedical applications, Commercial products
Materials science; Biomedical engineering; Nanotechnology; Biotechnology; Hydrogels; Biomedical applications; Commercial products
1. Introduction
Hydrogels are hydrophilic polymers, with a three-dimensional network structure that has the ability to absorb a large volume of water due to the presence of hydrophilic moieties (Habib et al., 2015). The term hydrogel was first coined by Van n Bemmelen in 1984 (van Bemmelen, 1894). Later in the year 1960, Wichterle and Lim reported about hydrogels based on poly (2-hydroxyethyl methacrylate), and they suggested hydrogels can be used as filler after enucleation of the eye, manufacturing of contact lenses and arteries (Wichterle and Lim, 1960). Since then many number of researches are going on about hydrogels in the field of agriculture, food industry, drug delivery, tissue engineering and regenerative medicine (Varaprasad et al., 2017). Apart from high water absorption capability, it has other properties like flexibility, porosity, stimuli-responsive, soft structure and its resemblance to living tissue (Bahram et al., 2016). Nowadays, scientists have more interest in using hydrogel for biomedical applications due to its biodegradability, biocompatibility, low immunogenicity and ease of usage. By tuning their physicochemical properties and crosslinking reaction, the hydrogel can be processed as solid, semi-solid and liquid (Varaprasad et al., 2017). As hydrogel has been a field of research for a few decades, there have been commercial products of hydrogels finding most applications in the medical field. In this review, we mainly focus on the various types of hydrogels, applications and commercial products for wound dressings, contact lenses, cosmetic applications, tissue engineering, and drug delivery.
2. Structure of hydrogel
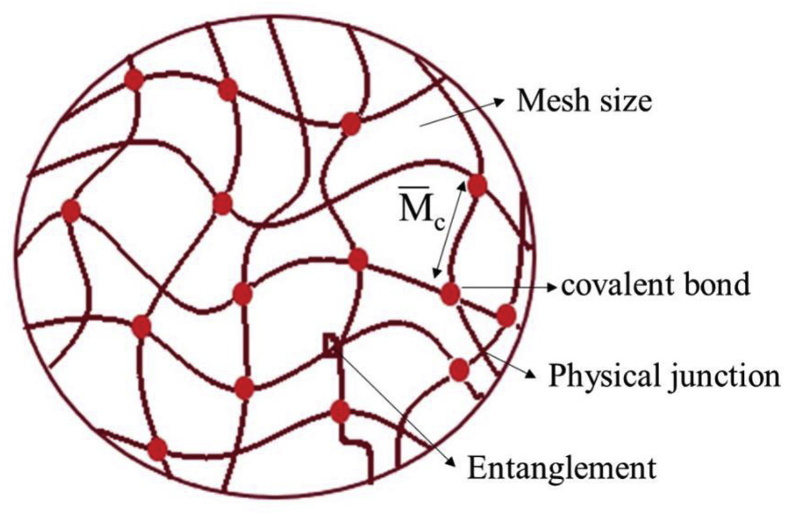
The solid form of a hydrogel is a network structure of crosslinked polymer chains (Ullah et al., 2015). The molecular weight of the hydrogel leads to infinity because of its 3D network structure (Rosiak et al., 1995). At the molecular level, the most important properties to define the hydrogel structure are the mesh size, and the molecular weight of polymer chain between the crosslinks (Figure 1) (Ganji et al., 2010). Crosslinking of hydrogels can be obtained by chemical (covalent) and physical (hydrogen bonding/entanglement) crosslinks. The swelling of a hydrogel is mainly defined by the diffusion of water into the hydrogel (Holback et al., 2011). The hydrogel swelling consist of three stages: 1. primary bound water-where the water molecules attach to the hydrophilic group, 2. secondary boundary water-the interaction of water molecules to the existing hydrophobic groups and 3. free water-at equilibrium swelling, water is filled into the void spaces (Gibas and Janik, 2010). The rate of swelling depends on the concentration of polymer and the crosslinking density (Okay, 2010). The high degree of crosslinking density causes a decrease in swelling ratio and it increases the brittleness of hydrogel.
Figure 1.
Structure of hydrogel at molecular level.
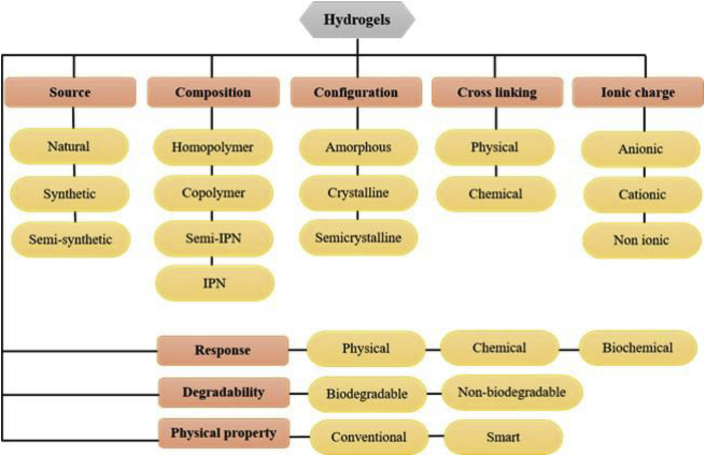
3. Classification of hydrogels
Hydrogels are classified based on its source, preparation, ionic charge, response, crosslinking and physical properties (Ullah et al., 2015) and its further classification is given in a schematic representation in Figure 2.
Figure 2.
Schematic representation of classification of hydrogels.
3.1. Based on source
Based on the source it can be divided into natural, synthetic and hybrid or semi-synthetic (El-sherbiny & Yacoub, 2013). Hydrogels derived from natural sources are a good candidate because of its high biocompatibility but are often limited for its poor mechanical properties and stability (Singh et al., 2016). Collagen, gelatin, alginate, chitosan, etc are examples of natural polymers. Chitosan is a biopolymer composed of N-acetyl D-glucosamine and D-glucosamine units. Chitosan is formed by the deacetylation of chitin, which is found in crustacean shells and it is a polycationic polymer (Croisier and Jérôme, 2013). Youming et al. fabricated an in situ forming hydrogel based on chitosan and hyaluronic acid via Schiff base cross-linking reaction. They showed an improved cellular response of the material and they suggested that this could be a suitable biomaterial for abdominal tissue engineering (Deng et al., 2017). Natural polymers are also used for making bioinks due to their biocompatibility and easy gelation mechanism. A cell encapsulated bioink was fabricated with sodium alginate and collagen or agarose showed good bioactivity and mechanical strength (Yang et al., 2017). These three polymers have a great attraction for making bioink because of its low cytotoxicity and high water content apart from its biocompatibility. Collagen is the natural extracellular matrix protein that provides cell adhesion ligands. Synthetic hydrogels are also a good candidate for biomedical applications because their physicochemical or mechanical properties are tunable and reproducible. Its main disadvantage is the lack of biocompatibility with some of the polymers.
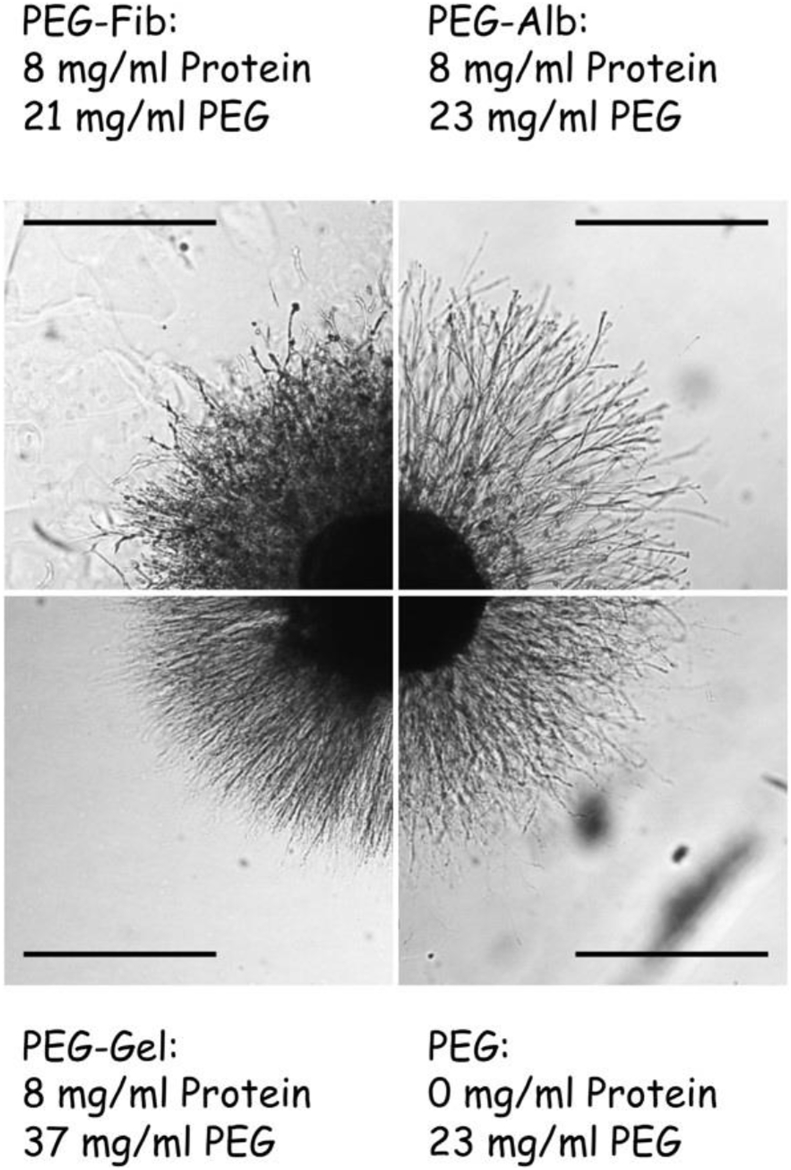
Poly (ethylene glycol), poly (acrylic acid), poly (ethylene oxide), poly (vinyl alcohol), etc. are some of the synthetic synthetic polymers used as hydrogels Ref: (Lee and Mooney, 2001). Physically cross-linked injectable PNIPAAm-polyethylene glycol hydrogel improves cellular response, axonal growth and helps in recovering sensory mortor function. These fabricated hydrogels could be a suitable candidate for the regeneration of axons (Bonnet et al., 2020). Polyethylene glycol is a biodegradable, biocompatible and suitable material for repairing spinal cord injury by nerve repair and inhibits the degeneration of nerve fiber (Kong et al., 2017). Further, a polyvinyl alcohol-polyacrylic acid hydrogel can be a good biomaterial for vascular access with reduced platelet adhesion (Mannarino et al., 2020). The semi-synthetic polymers include gelatin methacrylate, cellulose derivatives, etc (S. Utech and Boccaccini, 2016). Semi-synthetic or hybrid hydrogels are mostly used as they can possess the advantages of both natural and synthetic polymers. The hydrogel with the combination of synthetic polymer material with natural protein gives both mechanical and biological activity. Berkovitch et al. reported that the hydrogel fabricated with polyethylene glycol and proteins used for the encapsulation of dorsal root ganglia cells. This hydrogel as shown in Figure 3 can be used for studying the outgrowth of encapsulated cells by changing the protein and the material rigidity (Berkovitch and Seliktar, 2017).
Figure 3.
Microscopic images of outgrowth of dorsal root ganglia cells on semi synthetic hydrogel of PEG incorporated with diferent proteins. Compared to PEG alone, semi synthetic hydrogels shown better outgrowth of ganglia cells (Adapted from Berkovitch and Seliktar, 2017 with permission).
3.2. Based on composition
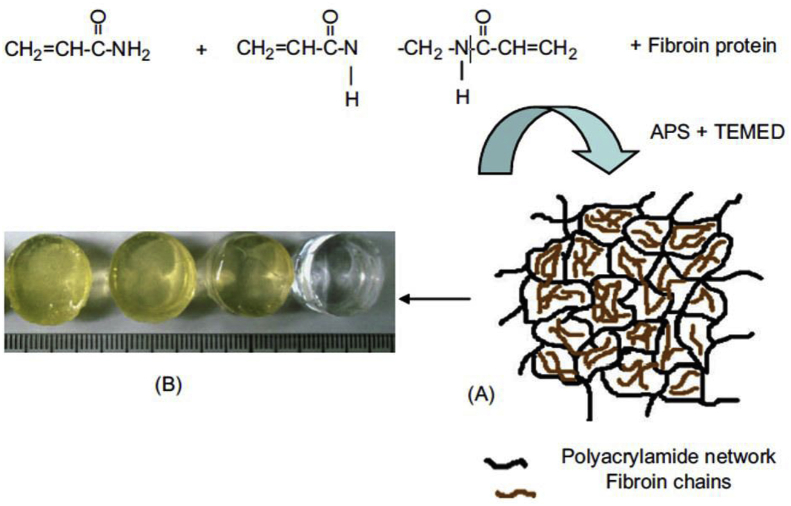
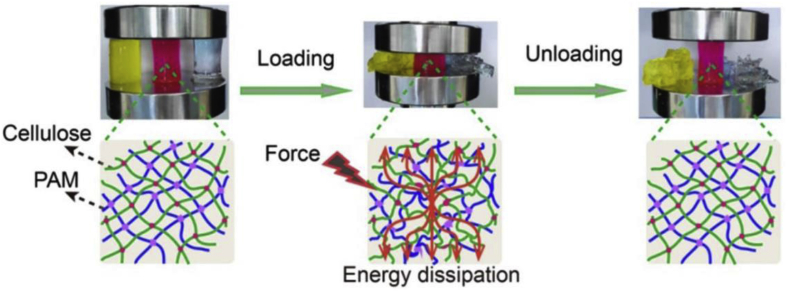
Based on the composition of the polymer, the hydrogel can be divided into homopolymers, copolymer, semi-interpenetrating network, and interpenetrating network. Homo-polymer hydrogels are composed of the same monomer units, where it may have a cross-linked or uncrosslinked network structure based on the basis of monomer nature and polymerization technique. Copolymeric hydrogel composed of two or more different monomer units with a minimum of one hydrophilic component. The copolymer-based hydrogel constructed with PLGA-PEG-PLGA is capable to solubilize the hydrophobic drug, indomethacin. The solubility of the drug is increased when loaded within the copolymer micelles (Qiao et al., 2005). Semi-interpenetrating network hydrogels are formed by the penetration of one linear polymer chain into another crosslinked polymer network without chemical bonds (Garg et al., 2017). Figure 4 shows a semi-interpenetrating network hydrogel of silk fibroin and polyacrylamide was prepared by blending both polymers and used as a matrix for drug release (Mandal et al., 2009). Its properties can be attained by varying the polymer concentrations. The FTIC-inulin and trypan blue dye were used to study in vitro release and it shows a sustained release of these two compounds from the semi-IPN hydrogel. The capability of drug release from the hydrogel proved its use in tissue engineering and other biomedical applications. Interpenetrating network hydrogel (IPN) is the most important one, where it is the combination of crosslinked polymers in network form. In IPN, one polymer is formed or crosslinked in the presence of another polymer network (Dragan, 2017). Researchers are showing greater interest in IPN because of its mechanical properties, mainly the toughness of IPN hydrogel. The mixture of covalently and ionically crosslinked polymer network gives the toughness of hydrogel (Bootsma et al., 2017). However, Lin et al. constructed a dual interpenetrating network hydrogel using cellulose and polyacrylamide polymers without any covalent bond formation. This IPN structure incorporated hydrogel shows significantly improved mechanical strength (Figure 5) (Lin et al., 2018). Puiyan et al. reported that polyethylene glycol diacrylate and modified gelatin interpenetrating network system loaded with gold porphyin (AuP) inhibited tumor growth and reduced angiogenesis in mice bearing human lung cancer xenograft (Lee et al., 2019).
Figure 4.
Semi-interpenetrating network made up of polyacrylamide polymer and silk fibroin chains Incorporation of fibroin improves the elasticity and softness of the hydrogel and helps in sustained release of drug (A) Schematic representation of formation of SF/PAAm semi-IPN network hydrogels (B) Typical appearance of different SF/PAAm semi-IPN hydrogels after removing from moulds (Adapted from Mandal et al., 2009 with permission).
Figure 5.
The compression behaviour of cellulose hydrogel (yellow), Cellulose-polyacrylamide IPN hydrogel (red) and Polyacrlamide hydrogel. Only in IPN hydrogels showed good mechanical integrity after deformation (Adapted from Lin et al., 2018 with permission).
3.3. Based on configuration
Based on the configuration it can be classified as amorphous, semi-crystalline and crystalline hydrogel (Mohite and Adhav, 2017). In 1994, semicrystalline hydrogels were developed by chemical crosslinking method, and it contains both crystalline and amorphous regions. The physically crosslinked semicrystalline hydrogel was prepared by micellar and bulk polymerization techniques. Compared to chemically crosslinked semicrystalline hydrogels, semicrystalline physical hydrogel have the unique property of changing from solid-state to a liquid state and vice versa. Therefore, it can be used as injectable hydrogels andshape-memory hydrogel (Okay, 2018).
3.4. Based on crosslinking
It is generally classified into two types: physical gel and chemical gel based on the type of crosslinking (Hennink; van Nostrum, 2012). Physical cross-linking is the most preferred method for the preparation of hydrogels. It is also known as reversible gel and it is again subdivided as strong physical gel and weak physical gel. Physical cross-linking mainly occurs through molecular entanglement, hydrogen bonding, hydrophobic association or polyelectrolytic interaction (Hu et al., 2019). Loftipour et al. developed a hydrogel by a physical freeze-thaw method using chitosan and polyvinyl alcohol polymers. This kind of physical hydrogel with repeated freeze thaw method provides elastic hydrogel and also increases the crystallinity of hydrogel. This hydrogel could be used for healing skin ulcers by incorporating oxytetracycline, an antibiotic and the hydrogel prepared by three cycles of freeze-thaw containing 5% PVA, 0.75% chitosan, 1000 mg oxytetracycline showed better results of wound healing (Lotfipour et al., 2019). But it lacks adequate mechanical strength and stability. To overcome this drawback, researchers mainly focused on chemical crosslinking. The chemical gel is also called permanent gel and it mainly occurs through chemical agents that cross-link the polymers by covalent interaction (Parhi, 2017). The swelling rate of chemical gel mainly depends on the concentration of the cross-linking agent. An acrylic acid-gelatin polymer hydrogel was constructed by free radical polymerization which is chemically cross-linked with ethylene glycol dimethacrylate with the help of initiator ammonium persulphate. The ability of swelling behaviour depends on the concentration of polymer, monomer and the cross-linking agent. As the concentration of polymer and crosslinker increases, the rate of the swelling ratio is decreased (Majid et al., 2015). Recently, researchers have focused on developing in situ formed hydrogels for biomedical applications such as injectable gels, drug delivery, surgical glue, etc. The chemical process behind the in-situ formation of hydrogel includes enzymatic cross-linking, Schiff base cross-linking, Michael addition, click chemistry and photo-cross-linking (Ko et al., 2013). An in situ forming injectable hydrogel can encapsulate cells and growth factors by simple methods.
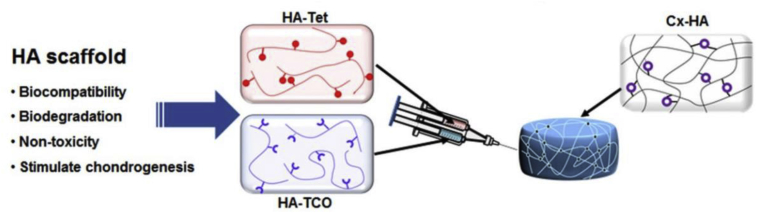
An in situ forming injectable hydrogel fabricated using tyramine conjugated hyaluronic acid via enzymatic cross-linking with horseradish peroxidase (HRP) and galactose oxidase. HRP usually catalyzes the crosslinking reaction with oxidizing agent hydrogen peroxide but it is having fast gelation rate. To avoid this drawback, here they used additional enzyme galactose oxidase to produce hydrogen peroxide (Wang et al., 2020). Rachel et al. studied morphology and functionalities of rat Schwann cells, C2C12 skeletal muscle cells and spinal spheroids from human induced pluripotent stem cells cultured on microbial transglutaminase (mTg) crosslinked gelatin-laminin hydrogel. Enzyme mTg catalyzes the construction of N-e-(gamma-glutamyl) lysine amide bonds (Besser et al., 2019). The cell adhesion and proliferation behaviour of osteoblast and fibroblast cells were studied on in situ forming Michael type addition crosslinked thiolated glycol chitosan hydrogel with oligo (acryloyl carbonate)-b-poly (ethylene glycol)-b-oligo (acryloyl carbonate). The reaction was carried out in PBS of pH 7.4 at 37 °C. The in vitro results showed this hydrogel is not supported for cell adhesion but the hydrogel functionalized with Gly-Arg-Gly-Asp-Cys residues showed better cell adhesion. This modified hydrogel could be a good matrix for tissue engineering applications (Y. Yu et al., 2011). Park et al. developed a chondrogenic differentiation factor (cytomodulin) contained in situ forming click cross-linked hyaluronic acid hydrogel for cartilage repair. After activated the carboxylic group present in hyaluronic acid, it was then modified with tetrazine and transcyclooctene and it was taken in a dual-barrelsyringe, upon injection hydrogel was formed by click-based reaction (Figure 6) (Park et al., 2019).
Figure 6.
Schematic representation of in situ forming click based Hyaluronic acid hydrogel This hydrogel helps in retention of cytomodulin which induces the condrogenic differentiation (Adapted from online open access article Park et al., 2019 with permission).
Apart from conventional hydrogels, there is another unique type of hydrogel is called “smart hydrogels”. It will respond to various stimuli such as light, temperature, pH, ionic strength or electric field, etc. and can cause changes in their swelling behavior, structure and mechanical properties (El-sherbiny & Yacoub, 2013). A smart pH-responsive hydrogel fabricated with acrylic acid, N-isopropylacrylamide and poly (L-lactide)-co-polyethyleneglycol-co-poly (L-lactide) dimethacrylates as a crosslinker can be used for dual drug delivery system. For example, the hydrogel can be loaded with doxorubicin and tetracyclin and release at pH 1.2 and pH 7.4, as the swelling takes place at pH 7.4 and deswelling at pH 1.2 (Xu et al., 2018). The properties of thermosensitive hydrogels are controlled by the equilibrium between hydrophilic and hydrophobic moieties (Chai et al., 2017). PNIPAAm- poly (N-isopropylacrylamide) is the commonly used thermoresponsive hydrogels that can undergo changes in volume due to slight temperature variations. The hydrophilicity or hydrophobicity of PNIPAAm hydrogel considerably changes at their lower critical solution temperature (Matsumoto et al., 2018). Shuo et al. described that the temperature-responsive poly (N-isopropylacrylamide) crosslinked with 4, 4′-dihydroxybiphenyl diacrylate can be used for different applications (Tang et al., 2017). In the field of smart hydrogels, shape memory and self-healing hydrogels are the advanced stimuli-responsive hydrogels (Echeverria et al., 2018).
4. Applications of commercial hydrogel
Due to the flexibility and versatility, hydrogels are used in many fields extending from industrial to biological. Major applications of hydrogel include biomedical, dyes removal, heavy metal ions removal, agriculture, sanitary diapers, pH-sensors, biosensors, and supercapacitors (Bahram et al., 2016). In this review, we only focused on biomedical applications such as wound dressings, cosmetics, contact lenses, drug delivery, and tissue engineering.
4.1. Wound dressings
Wound dressings are materials mainly polymers in the form of gauzes, gels, hydrogels, hydrocolloids etc. Among them, hydrogels are the most promising approach in wound healing. Hydrogels act as an ideal wound dressing as they can provide a moist environment in the wound site, helps in the removal of wound exudates, prevents infection and gives a suitable environment for tissue regeneration (Gupta et al., 2011).
A wound is an injury that happens in body tissues either inside or outside, mainly in skin due to trauma, cut or any other damage (Basu et al., 2017). The wound can cause the disruption of the structure and function of normal tissue. There are two types of wounds; acute and chronic wounds. Acute wound heals completely in a shorter time while the chronic wound takes a longer time to heal. The process of wound healing includes hemostasis, inflammation, proliferation, and remodelling (Whitney, 2005). The wound healing process gets affected by various reasons such as wound infection, depth of the wound, foreign body interaction, stress, pressure, age, diseases, etc (H. Liu et al., 2018). Scarring occurred during normal healing due to the deposition of collagen fibers and it will be there for a long time. With the help of wound dressings, scarless healing occurs. Catanzano et al. developed a composite hydrogel containing alginate and hyaluronan for the wound healing process. Alginate is a polysaccharide having high absorption capacity which helps in minimize wound secretions and promote wound healing by maintaining a moist environment. With the help of hyaluronic acid which helps in keratinocyte migration and proliferation, they successfully prepared alginate-hyaluronan hydrogel through ionic crosslinking (Catanzano et al., 2015). Polysaccharide based hydrogel has greater potential in wound healing application because of its high water absorption ability. A nanocellulose incorporated hemicellulose hydrogels were prepared by Jun et al. This hydrogel helps in adhesion and proliferation of fibroblast cells and it can be a suitable hydrogel material for wound healing (J. Liu et al., 2016).
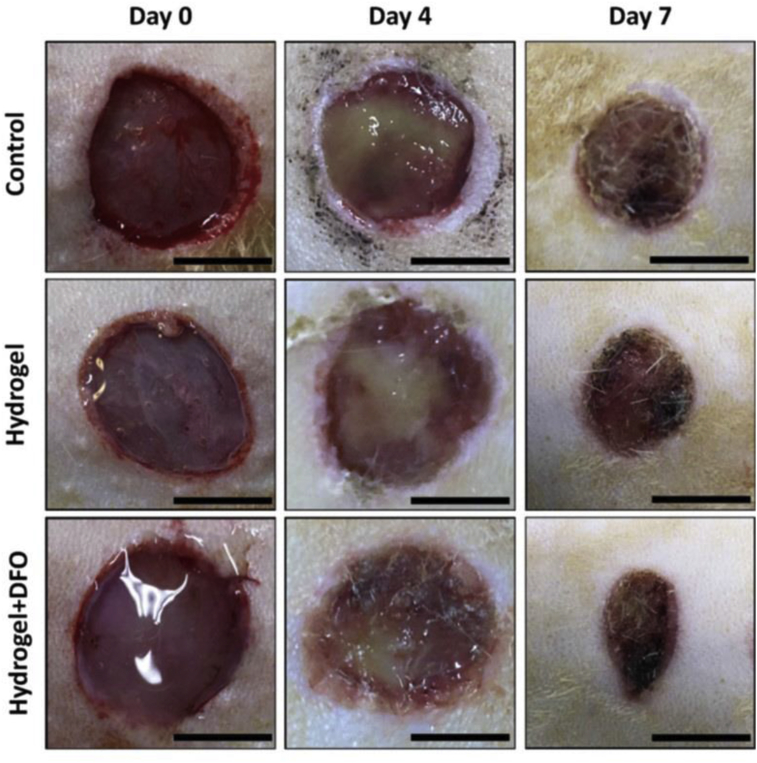
In wound dressing applications, anti-bacterial and anti-inflammatory hydrogels have a good impact. A multifunctional and pH-responsive composite hydrogel made of carboxylated agarose and tannic acid, which is ionically crosslinked with zinc salts for wound healing (Ninan et al., 2016). The pH-responsive property of carboxylated cellulose combined with anti-microbial, anti-inflammatory, anti-oxidant property of tannic acid showed increased compressive strength and anti-bacterial activity. Dextran is another polysaccharide used for synthesizing hydrogel. It helps in situ gelation and controlled release of immobilized growth factor with the help of chitosan microparticles and showed better wound healing in vivo (Ribeiro et al., 2013). Chitosan is an excellent wound healing material because of its haemostatic nature (Ahmed and Ikram, 2016). A physically cross-linked chitosan hydrogel has the ability to reconstruct the skin of third-degree burn, where they tested in pig dorsal area (Viton et al., 2007). An injectable hydrogel constructed via disulphide bond cross-linking of thiolated polyethylene glycol and silver nitrate. This hydrogel is loaded with desferrioxamine, an angiogenic drug and this could repair the diabetic wound with its angiogenic activity (Figure 7) (Chen et al., 2019).
Figure 7.
Improved healing of diabetic skin wound using drug loaded thiolated PEG hydrogel compared to control (Adapted from opne access article Chen et al., 2019 with permission).
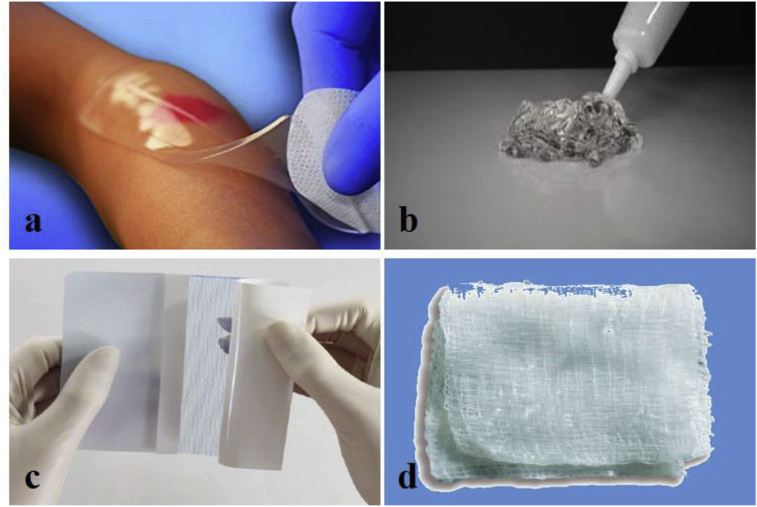
To avoid wound-related diseases and scarring, there is a wide range of hydrogel related wound care products are available in the market. Amorphous gel, hydrogel sheets, hydrogel film, and hydrogel impregnated gauze are the different types of hydrogel wound dressing available in the market (Figure 8). The ActivHeal® hydrogel is one of the wound care dressing available in the market and is used for primary wound dressing (AlTabbaa and Ankrah, 2016). This is an amorphous gel used in the dry wound with low exudate where it slowly increases the moisture content level in the wound environment and promotes moist wound healing through autolytic debridement. And it induces the growth of epithelial cells. This hydrogel is used for various wounds from pressure ulcers, cavity wounds, leg ulcers, diabetic ulcers, post-surgical wounds, and abrasions. Suprasorb® G hydrogel is also used for acute or chronic wounds with low exudate in dry wounds. This gel gently removes necrotic tissue and absorbs it into the gel (“Lohmann-Rauscher website,”). Wound healing by this hydrogel is also by autolytic debridement with moisture donation to the wound environment. The moist environment provides granulation and epithelisation to the wound surface. The main advantages are it reduce wound pain and its ease of usage. It is used with secondary film dressing to secure hydrogel. Acrylic polymers, polyethylene, and phenoxyethanol are the main components of Suprasorb® G hydrogel. AquaDerm™ (“Dermarite website,”a) and DermaSyn® (“Dermarite website,” n.d.-b) are the product of DermaRite, where AquaDerm™ is the hydrogel sheet dressing and DermaSyn® is the hydrogel wound dressing. The functions of both hydrogels are same as that of the previously described hydrogel, where the DermaSyn is the non-oily amorphous gel enriched with vitamin E.
Figure 8.
Different forms hydrogel wound dressing available in market. (a) Neoheal® hydrogel sheet used for wound dressing, (b) Amorphous gel that can be sued for necrotic wounds and burns, (c) - Hydrogel film and (d) Hydrogel impregnated gauze (Image Courtesy: (a) Kikgel, Poland, (b) Avery Dennison Medical, Longford, Ireland-(Finesse Medical Ltd) (c) Lohmann & Rauscher GmbH & Co, Germany and (d) McKesson Medical Supplies).
NU-GEL™ (“Systagenix website,” n.d.) hydrogel is a cost-effective, transparent, and amorphous gel. This hydrogel contains sodium alginate which effectively removes damaged tissue and slough. It also creates the moist in the wound environment for healing. The alginate present in the gel increases the absorptive capacity. The alginate hydrogels have been used as wound dressing material because of its high water content, permeability, and elasticity (W. Yu et al., 2016). It has the potential to reduce bacterial infections and also promote hemostatic properties (Aderibigbe and Blessing Atim, 2018, Ahmed and Ikram, 2016, Al-sabah et al., 2019, Alba-Bueno et al., 2009, Besser et al., 2019). Purilon® gel (“Coloplast website,“) is a hydrogel which contains naturally derived components like calcium alginate and sodium carboxymethyl cellulose. And it does not contains any additives. Apart from leg ulcers, pressure ulcers, etc. it can be used for first and second-degree burns. This gel should be used with secondary wound dressings. The presence of carboxymethyl cellulose in the hydrogels helps in maintaining an optimal moist environment due to high water holding capacity. It also helps in extracellular matrix formation and re-epithelization (Wong and Ramli, 2014).
Neoheal® Hydrogel wound dressings produced by Kikgel manufacturer (“Kikgel website,”). It is a primary hydrogel dressing made up of both natural and synthetic polymers such as agar, polyethylene glycol, and polyvinylpyrrolidone. And this hydrogel is crosslinked via electron beams. This is having enough mechanical strength due to crosslinking. The main advantage is that it contains about 90% of water and it has the capability to absorbing and donating water to the wound environment. It also induces the granulation and epidermisation. Commercially available hydrogel wound dressings like film, sheets and hydrogel incorporated gauze are depicted in Table 1 and gel form in Table 2. From all the products we can understand that all those promote moist wound healing, where it enhanced autolytic debridement. The moist wound healing was first described by George D Winter. From his experiments, he concluded that the epithelization of the superficial wound under moist is twice as compared with the wound exposed to air without scab (George D Winter, 1962).
Table 1.
Commercially available hydrogel wound dressings.
| Product name | Company name | Hydrogel form/Composition | Application | Ref |
|---|---|---|---|---|
| Suprasorb® G | Lohmann & Rauscher Global | Hydrogel film made up of acrylic polymers, polyethylene, and phenoxyethanol with 70% water content. | Dry wounds, Lower leg ulcer, pressure ulcer, first and second-degree burns, scalds | (“Lohmann-rauscher website,”) |
| AquaDerm™ | DermaRite industries | Hydrogel sheet consist of 2-Acrylamido-2 methyl-1 propanesulfonic acid sodium, Propylene Glycol, Poly (ethylene glycol) dimethacrylate, 2-Hydroxy-2-methylpropiophenone with 38–55% water | Pressure ulcers, Minor burns and radiation tissue damage | (“Dermarite website,” a) |
| DermaGauze™ | DermaRite industries | Hydrogel impregnated gauze dressing. Acrylate polymer is the one of the component in DermaGauze. | Acute or chronic partial and full thickness wounds | (“Dermarite website,” c) |
| Neoheal® Hydrogel | Kikgel | Hydrogel sheet consist of PEG, polyvinylopyrrolidone, and agar and it is crosslinked via electron beams. Contains about 90% of water. | Ulcers, abrasions, burns, bed sores and other chronic wounds | (“Kikgel website,”) |
| Simpurity™ Hydrogel | Safe n’Simple | Absorbent sheets containing polyethylene oxide, polyvinyl alcohol, acrylate, polyurethane, and purified water | Dry wounds, skin burns and dry scabs | (“Wound source website,”) |
| Restore Hydrogel | Hollister Incorporated | Hydrogel impregnated gauze pad contains hyaluraonic acid and promote wound healing by autolytic debridement. | Partial and full thickness wound | (“Hollister website,”) |
Table 2.
Commercially available hydrogel wound dressings in gel form.
| Product name | Company name | Composition | Applications | Ref |
|---|---|---|---|---|
| ActivHeal® | Advanced Medical Solutions Ltd. | It is a primary wound dressing contains 85% water. | Pressure ulcers, leg ulcers, diabetic foot ulcers, cavity wounds | (AlTabbaa and Ankrah, 2016) |
| DermaSyn® | DermaRite industries | It's a primary wound dressing contains vitamin E. | Acute or chronic partial and full thickness wounds | (“Dermarite website,”-b) |
| NU-GEL™ | Systagenix | Contains sodium alginate which effectively debrides necrotic tissue and fibrinous slough. | Chronic wound, diabetic foot ulcers, venous leg ulcers and pressure ulcers. | (“Systagenix website,”) |
| Purilon® | Coloplast | Contains calcium alginate and sodium carboxymethyl cellulose with purified water. | Leg ulcers, pressure ulcers, non-infected diabetic foot ulcers and First and second degree burns | (“Coloplast website,“) |
| INTRASITE◊ Gel | Smith and Nephew | Consist of Carboxymethyl cellulose and propylene glycol. | Pressure ulcers, Diabetic foot ulcers Surgical incisions Venous ulcers |
(“Smith and Nephew website,”) |
| SOLOSITE◊ Gel | Smith and Nephew | Contains sodium salt of carboxymethyl cellulose and glycerol with above 60% water. | Minor burns, cuts, abrasions, skin tears, Venous ulcers, Surgical incisions, Diabetic foot ulcers, Pressure ulcers, | (“Smith-Nephew Website,”) |
| Woun'Dres® | Coloplast | It contains the polymers like carbomer and collagen with other ingredients. | Dry wounds | (“Coloplast Website,“) |
4.2. Cosmetic applications
The major function of the skin is to protect the body from environmental factors such as microorganisms and UV radiation. Besides it also helps in maintaining the body temperature and body fluid (Papakonstantinou et al., 2012). Hydration of the skin is important in the maintenance of its appearance and texture (Verdier-Sévrain and Bonté, 2007). Natural aging, due to the genetic factors and photoaging, due to sun exposure serves as major reasons for skin damage apart from climatic conditions and pollution exposure (Baumann, 2007). Cosmetics products are used to enhance skin appearance and texture. Moisturizers, body lotions, skin cleaners are some of the cosmetic items used for maintaining the body. Nowadays, the cosmetics industries showing more interest in hydrogels due to properties like biocompatibility, elasticity, softness and high water content.
The hydrogel can be used for skin issues such as cellulite, wrinkles, pigmentation, skin hydration and aging. Caffeine-containing bioadhesive hydrogel used for cosmetic applications mainly cellulite or gynoid lipodystrophy. The bioadhesive property of hydrogel helps in releasing caffeine gradually into the skin thereby enhancing skin appearance and texture (Parente et al., 2015). Kim et al. developed a liposome in a hydrogel complex system for delaying photoaging, where it enhanced the skin permeation of drugs. The skin permeation of drugs was improved through the hydrogel system, which helps in loosening the skin barrier through skin hydration (Kim et al., 2014). In the market, hydrogel products such as face mask, lip mask, under eye pad, etc. are available for treating skin related issues. Collagen hydrogel (“Bulgaria website,“) by Dr. Derm professional is a hydrogel used as a cosmetic product, which helps in regenerate and to restore the softness, elasticity and hydration of the skin. This hydrogel is made up of hyaluronic acid and collagen. Hyaluronic acid plays an important role in skin moisture by giving hydration to the skin (Papakonstantinou et al., 2012). Table 3 shows the commercially available hydrogels for cosmetic applications.
Table 3.
Different types of hydrogel cosmetic products available in market.
| Product name | Manufacturer | Hydrogel form/Characteristics | Application | Ref |
|---|---|---|---|---|
| Rose soothing hydrogel mask | Moira | Face Mask made with sodium polyacrylate, glycerine, cellulose gum, water etc. with maximum absorption. Soothes and rejuvenate the skin | Face Skin | (“Moira website,”) |
| Collagen Hydrogel | Dr. Derm Professional | Hydrogel contains sea collagen and hyaluronic acid. Nourishes, regenerate the skin of the face | Face Skin | (“Bulgaria website,”) |
| Advanced Génifique Hydrogel Mask | Lancome Paris | Hydrogel face mask made up of glycerine, polyacrylate-13, water etc. enriched with Bifidus extract. Skin will become moisturized, radiant, smoother and looks healthy glow | Face Skin | (“Lancome website,”) |
| Charcoal Hydrogel under eye mask | ELF cosmetics | Under Eyemask contains water, charcoal, seaweed extract, etc. Nourishes and gives a healthy glow to the skin. | Under eye skin | (“Elf cosmetics website,”) |
| Lip patch | Taiki | Hydrogel patch contains sodium hyaluronate and glycerine for moisturizing. Strong adhesion and gives lips elastic and hydrated | Lip | (“Taiki cosmetics website,”) |
| Aloe vera supple skin hydrogel | Images | Sheet mask contains Hyaluronic acid, glycerol, water etc. Moisturizes, nourishes, smooths the skin and also gives elasticity and firmness to the skin. | Face | (“Images website,”) |
| Neutrogena® Hydro Boost® | Johnson and Johnson | Face mask contains hyaluronic acid. Provide instant and long lasting moisture to the skin. | Face | (“Neutrogena website,”) |
4.3. Contact lens
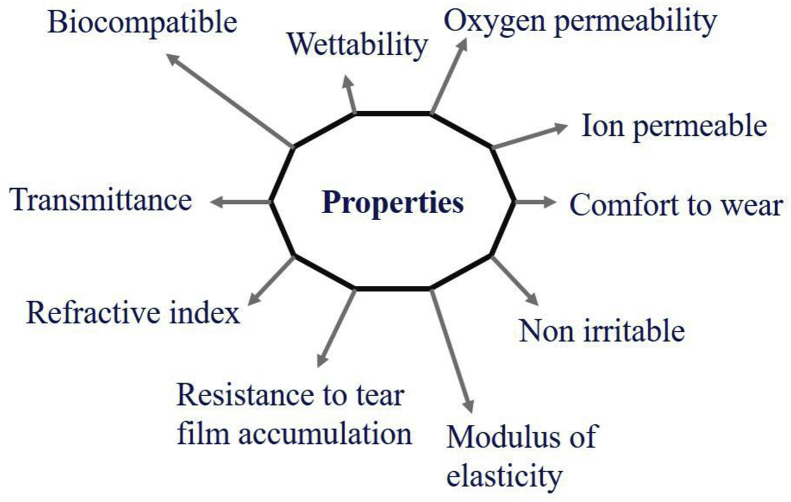
Contact lens gets direct contact with the eye to correct the vision, drug delivery for ophthalmic conditions and cosmetic use (Farandos et al., 2015). There are two major types of contact lens, rigid and soft contact lens. Rigid contact lenses are made with polymer polymethyl methacrylate (PMMA). It has properties like surface wettability, high modulus of elasticity with excellent durability. But it has no oxygen permeability and which also causes eye effects (Geiges, 2001). In 1960, Wichterle and Lim have first described hydrogel for the use of contact lens and other applications (Wichterle and Lim, 1960). A hydrogel system based on Poly (2-hydroxyethyl methacrylate) (pHEMA) was the first hydrogel material used to make a contact lens. Poly (vinyl alcohol), polyacrylonitrile, etc. are the hydrophilic polymers that have been investigated for making hydrogel contact lenses Ref: (Lai et al., 2014). Besides this, silicone and fluorine-based hydrogel contact lens are also investigated. But silicone-based hydrogel contact lenses are one of the most dominant hydrogel material today (Musgrave and Fang, 2019). A soft or hydrogel contact lenses should have properties like high water content, their ability to transfer water and oxygen permeability (Munćan et al., 2016). Oxygen permeability is a very important characteristic of the proper functioning of the cornea. Because cornea uses oxygen from the air to maintain its structure, function, and clarity (Nicolson and Vogt, 2001). The oxygen permeability of hydrogel contact lenses is critically related to the water content and thickness of the contact lens (McMahon and Zadnik, 2000). Apart from this, it should be biocompatible, comfort to wear, continuous tear film for clear vision, permeable to ions for maintaining movement, non-irritable and resistant to tear film accumulation (Figure 9). Luminous transmittance and refractive index are the important requirements for hydrogel for making contact lenses (Caló and Khutoryanskiy, 2015). The extended use of conventional hydrogel contact lenses can cause hypoxia on corneal physiology and corneal integrity and function. The high oxygen permeability capacity of silicone-based soft contact lens can avoid these types of adverse corneal effects. But silicone-based hydrogel contact lens can also have the potential of causing corneal homeostasis with extended use (Stapleton et al., 2006).
Figure 9.
Properties or requirements suitable for hydrogel as contact lenses.
The hydrogel contact lens is available in the market on the basis of daily wear, biweekly wear, monthly contacts, and light adaptive contact. Bausch and Lomb in 1971 launched the first hydrogel contact lens to the market Lai et al., 2014). Today Bausch and Lomb is one of the most popular soft contact lens manufacturers. SofLens Daily disposable, Ultra Contact lens, PureVision2 HD, iconnect and New Biotrue® are the soft contact lens produced by Bausch and Lomb for short and long-sightedness (“Bausch and Lomb website,”-a). They also produced contact lenses such as SofLens Daily Disposable toric, SofLens Toric and PureVision 2 for astigmatism (“Bausch and Lomb website,”-b) and SofLens Multifocal, Bio true ONEday lens and Pure Vision 2 for presbyopia (“Bausch and Lomb website,”-c). Like this, manufacturers such as Johnson & Johnson, CooperVision, Ciba vision, etc. are producing different types of soft contact lenses for different applications. Some of the products are depicted in Table 4. Francisco et al. studied the shape changes in cornea induced by hydrogel contact lenses, specifically first and second-generation hydrogel CLs. They reported that there are changes in topological indices like anterior corneal astigmatism, surface regularity index, and mean keratometry those who are using Soflens 38 and these indices are stable where those who are using Focus Night & Day and Acuvue Oasys hydrogel CLs (Alba-Bueno et al., 2009). Biotrue™ solution manufactured by Bausch and Lomb contains Hyaluronan which can be used for conditioning agent for contact lenses irrespective of its water content (Scheuer et al., 2010).
Table 4.
Commercially available soft contact lenses.
| Product name | Manufacturer | Characteristics | Applications | Ref |
|---|---|---|---|---|
| Airsoft™ | Maxvue vision | Silicone hydrogel material with high water content and oxygen permeability. | Astigmatism | (“Maxvue vision website,”) |
| Gentle 59 | Mark'ennovy | Bioinspired silicone hydrogel lens. | Short sight and long sight | (“Markennovy website,”) |
| Clariti® 1 day | CooperVision® | Silicone hydrogel with high oxygen permeability. Keep eyes moist by attracting water molecules to the lens. | Short sight and long sight | (“Cooper vision Website,“) |
| Miacare™ 1 day | BenQ | Silicone hydrogel with ultra-high oxygen permeability. Contains Hyaluronic acid and sodium alginate as moisturizing agents. | Myopia | (“Miacare Website,”) |
| Soflens daily disposable | Bausch & Lomb | Keep eye comfortable by giving moisture around the lens. | Short and Long sightedness | (“Bausch and Lomb Website,“) |
| Focus® DAILIES® with AquaRelease™ | Ciba Vision | Lubricates the eye for every blink. | Astigmatism | (“Cibavision Website,“) |
| ACUVUE OASYS® | Johnson& Johnson | Maintain moisture, tear film and reduce dryness. | Presbyopia | (“Acuvue Website,“) |
| everclear™ ELITE | Visco Vision | Flexible silicone hydrogel with high oxygen permeability. | Long sightedness | (“Visio direct Website,”) |
4.4. Drug delivery
The process of administering a drug to the human or animal body to achieve a desired therapeutic effect is known as drug delivery (Tiwari et al., 2012). The drug delivery system should deliver the drug in a controlled manner and it should release the drug at an effective rate to the targeted site (Sandeep, SL, & Kanupriya, 2012). There is an increasing interest in using hydrogel as a drug delivery system due to its three-dimensional structural network with high water holding capacity. This property of hydrogel supports in holding drugs and release the drug in a controlled manner. The high amount of water present in hydrogel helps in encapsulate hydrophilic drugs (Li and Mooney, 2016). The sustained release of the drug is achieved by its physical properties such as porosity (Narayanaswamy and Torchilin, 2019). The drug is loaded on the hydrogel by two methods. In the first method, the polymer is mixed with drug followed by polymerization along with crosslinker and the second method is the formed hydrogel is immersed in drug solution (Mishra et al., 2017). The main disadvantages of hydrogel drug delivery system are their low tensile strength and difficulty in loading hydrophobic drugs (Hoare and Kohane, 2008). To increase the loading efficiency of hydrophobic drugs to the hydrogel matrix is by the incorporation of molecules that have the ability to form inclusion complexes and incorporation of hydrophobic moieties (Larrañeta et al., 2018). Molecular imprinting of supermolecular hydrogels increases the drug loading efficiency without affecting the release kinetics (Juric et al., 2019). Diffusion-controlled, swelling controlled, and chemically controlled are the drug release models for the controlled release of drug from hydrogel (Sri and Chatterjee, 2014).
Hydrogel drug delivery system can be used for ophthalmic, vaginal, transdermal, subcutaneous, oral, rectal applications, etc. Anda et al. reported that the nitrosalicyl-imine-chitosan hydrogel system loaded with diclofenac sodium salt provides sustained delivery for local therapy (Craciun et al., 2019). Poloxamer, a block copolymer hydrogel loaded with tetramethylpyrazine (TMP) were studied for the controlled drug delivery. Poloxamer is compatible with both hydrophilic and hydrophobic drugs. In this study they reported that the release rate of the drug was reduced due to TMP is wrapped in micelles and the release rate is increased as the temperature increases (Xia, 2019). Another study reported that paclitaxel-loaded thermo-sensitive in situ forming hydrogel may be used to inhibit local tumor reappearance at tumor resection site (Shive, Bichara, Berrada, & Ruel-garie, 2004).
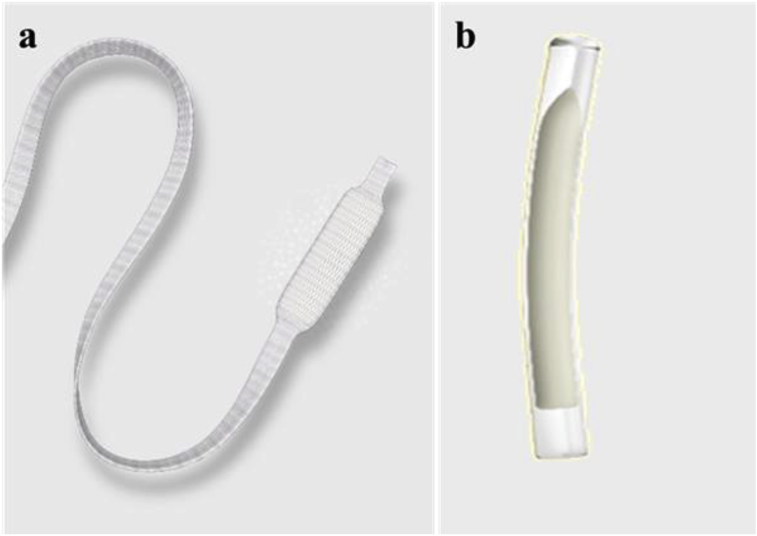
Cervidil® (Ferring Pharmaceuticals Inc.) is a hydrogel vaginal insert used to prepare the cervix for delivery (“Iodine Website,”). It contains dinoprostone also known as prostaglandin E2, it has an important role in cervical ripening. After insertion, the dinoprostone releasing rate is 0.3 mg/h from the total concentration of 10mg. SUPPRELIN® LA (Endo Pharmaceuticals Inc.) (www.fda.gov/medwatch, 2017) is a subcutaneous implant, used for the treatment of central precocious puberty. It is a hydrogel polymer reservoir containing 50 mg histrelin acetate drug in a small flexible tube. It delivers the drug at the rate of 65 mcg per day by diffusion controlled manner over 12 months. Figure 10 showing the commercially available hydrogel implant for drug delivery. There is only a limited number of products are available in the market.
Figure 10.
Commercially available hydrogel implant for drug delivery (a) Cervidil® that contains 10 mg of dinoprostone in a hydrogel and, (b) SUPPRELIN® LA, a subcutaneous implant (Image courtesy: (a) Ferring Pharmaceuticals Inc. USA, (b) Endo Pharmaceuticals, USA.
4.5. Tissue engineering
Tissue engineering is an interdisciplinary field that combines various fields like material science, cell biology, and engineering to repair damaged tissues (O'Brien, 2011). The aim of tissue engineering is to produce scaffolds that can mimic the extracellular matrix for tissue regeneration. A scaffold material should have an interconnected porous structure for the cell ingrowth, nutrients transport, waste removal and it should have mechanical strength that mimics the native tissue. Besides, the scaffolds should also have biocompatibility, biodegradability, sterility and to provide structural support for the cell attachment, proliferation and differentiation (Cascone and Lamberti, 2019). There are different approaches for constructing scaffolds, which include premade porous scaffolds, decellularized extracellular matrix, cell sheets with secreted extracellular matrix and cell encapsulated in self-assembled hydrogel (Chan and Leong, 2008). Hydrogels gained great interest in tissue engineering due to its resemblance to the native extracellular matrix. There are several approaches for hydrogel scaffold fabrication including lyophilization, emulsification, solvent casting – leaching, gas foaming – leaching, photolithography, microfluidic, micro molding and 3D printing (El-sherbiny & Yacoub, 2013).
Hydrogels scaffolds are used in the regeneration of cardiac tissues, cartilage, and bone. Ayesha et al. reported that hydrogel based on nanocellulose and sodium alginate crosslinked with calcium chloride can be used for cartilage tissue engineering (Al-sabah et al., 2019). Another study reported that gelatin-based hydrogel reinforced with eggshell particles, where it helps in the differentiation of pre-mature cells into osteoblast (Wu, Stroll, Lantigua, Suvarnapathaki, & Camci-unal, 2019). Injectable hydrogels are more advantageous than normal hydrogel scaffolds owing to its easy filling of irregular defects and it does not require complex surgical procedures. Xiao et al. described that in situ cross-linkable hyaluronan hydrogel can be used for tissue engineering purposes. Hyaluronan is the extracellular matrix constituent, where it helps in cell adhesion, proliferation, and differentiation (Shu et al., 2004). Polyethylene glycol-modified with RGD motifs which is an in situ photopolymerized injectable hydrogels for bone tissue engineering (Burdick and Anseth, 2002).
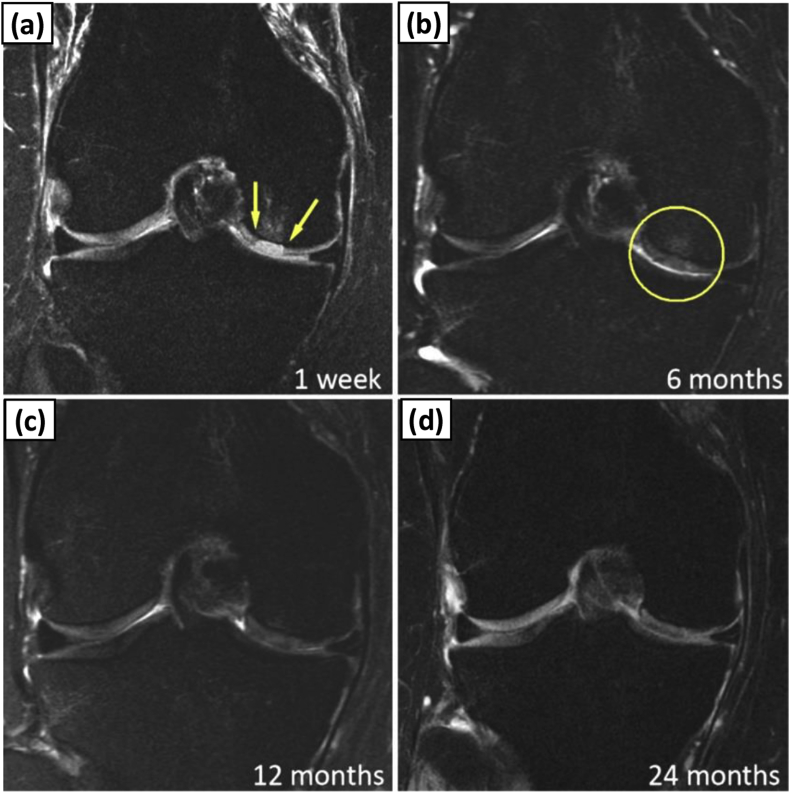
Gelrin C™ (Regentis Biomaterial Ltd.) is a photocrosslinked hydrogel made up of polyethylene glycol and human fibrinogen protein. This is a non-porous injectable hydrogel, which is being evaluated for knee cartilage regeneration (Figure 11) (Trattnig et al., 2015). This product is now under clinical trial. Mebiol® Gel PNIPAAm-PEG 3D Thermo reversible hydrogel (Cosmo Bio co ltd.) is the commercially available hydrogel for stem cell culture, cell implantation, organ or tissue regeneration, drug delivery, and non-cell culture applications (“Cosmobio Website,”). The Mebiol® hydrogels can be only used for research purposes. It is a thermoreversible sol-gel that remains in the gel state at high temperature and transforms into a liquid state at a low temperature. The main features of Mebiol® are easy handling, biocompatible, and highly transparent for cell observation. Qiang Li et al. reported that, by using this thermoreversible three dimensional hydrogel may be used for culturing cells to produce proteins for the therapeutic purpose (Q. Li et al., 2018). HyStem® Hydrogel UV Quick Set Kit (ESI BIO) is the hyaluronic acid UV light-controlled system which supports three-dimensional cell culture for tissue engineering purposes and 3D printing applications (“Esibio Website,”). Corning® Matrigel® matrix (Corning Incorporated Life sciences) is a hydrogel, which mimics the natural extracellular matrix used as a model for 2D and 3D cell culture experiments (“Corning Website,”-a). Corning® PuraMatrix™ peptide hydrogel (Corning Incorporated Life sciences) is another hydrogel used for 3D cell culture. It is mainly composed of water (99%) with 1% of amino acids. It is used for stem cell proliferation, tumor cell migration and invasion, and in vivo analysis of tissue regeneration (“Corning Website,” n.d.-b). Bioglex Ltd. producing various products includes Biogelx™-S, Biogelx™-RGD, Biogelx™-IKVAV, Biogelx™-YIGSR, and Biogelx™-GFOGER (“Biogelx Website,”). These are synthetic peptide powder functionalized with fibronectin, laminin, and collagen except Biogelx™-S. These powders can form hydrogels to mimic the extracellular matrix suitable for 3D cell culture. Except Gelrin C™, all other products are commonly used for the research purpose. In the tissue engineering field, the biomaterials based on hydrogels are still in the research stage and some few products are entered into clinical study.
Figure 11.
Morphological evaluation of GelrinC after implanted in patient. Faster regeneration of cartilage was achieved by using GelrinC implant Series of proton density fat suppressed images in coronal plane show development of cartilage transplant in follow-up examinations after (a) 1 week; (b) 6 months; (c) 12 months; and (d) 24 months. Arrows and circle delineate RT area (Adapted from Trattnig et al., 2015 with permission).
The main limitation of the hydrogel-based scaffold is the hydrogel matrix interaction with cells. The viscoelastic properties of the hydrogel are the important factor which is responsible for cell fate (Lee and Kim, 2018). The economical way to improve the hydrogel stability and cell interactions with the hydrogel matrix will be the most needed research in hydrogels for tissue engineering applications.
5. Future of hydrogels in biomedical applications
Hydrogels are the leading biomaterial candidate in the field of biomedical. It is clear that there is a long way to go in research on hydrogel in biomedical applications especially for tissue engineering and drug delivery. Recently, MIT researchers have developed an ingestible hydrogel device inspired by pufferfish. This high speed and high ratio ingestible hydrogel is made with polyacrylic acid encapsulated in polyvinyl alcohol hydrogel membrane. It can be used for sensing gastric temperature and for sustained release of the drug. The other applications of this ingestible hydrogel are to measure the biosignals, to visualizing the gastrointestinal tract with the help of a micro camera attached to this device or to checking medication patterns (X. Liu et al., 2019). Danyuo et al. reported that the release of prodigiosin, a cancer drug from thermosensitive P(NIPA) based hydrogel for treating breast cancer. The porosity and the crosslinking ratio of hydrogel play an important role in drug release (Danyuo et al., 2019). This kind of study directs a progressive impact on hydrogel-based research for drug delivery. In tissue engineering fabrication technique is very important, nowadays, more researches are based on in situ crosslinked hydrogel. Cathal et al. developed a biopen, which can be used for in situ fabrication of hydrogel scaffold by injecting hydrogel and cells simultaneously (Connell et al., 2016). Although extensive studies have been done on hydrogels in tissue engineering applications, the commercialization of these products are still in progression.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This work was supported by Science and Engineering Research Board (SERB), India (EMR/2017/003504).
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgement
The authors SHA and IM gratefully acknowledge the support from DST project on hydrogels (DST/SERB/EMR/2017/003504).
References
- Acuvue Website. https://www.acuvue.com/contact-lenses/.
- Aderibigbe, Blessing Atim B.B. Alginate in wound dressings. Pharmaceutics. 2018;10(2):42. doi: 10.3390/pharmaceutics10020042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S., Ikram S. Chitosan based scaffolds and their applications in wound healing. ALSConnect. 2016;10(1):27–37. [Google Scholar]
- Al-sabah A., Burnell S.E.A., Simoes I.N., Jessop Z., Blain E., Whitaker I.S. Structural and mechanical characterization of crosslinked and sterilised nanocellulose-based hydrogels for cartilage tissue engineering. Carbohydr. Polym. 2019;212(February):242–251. doi: 10.1016/j.carbpol.2019.02.057. [DOI] [PubMed] [Google Scholar]
- Alba-Bueno F., Beltran-Masgoret À., Sanjuan C., Biarnés M., Marín J. Corneal shape changes induced by first and second generation silicone hydrogel contact lenses in daily wear. Contact Lens Anterior Eye. 2009;32(2):88–92. doi: 10.1016/j.clae.2008.11.002. [DOI] [PubMed] [Google Scholar]
- AlTabbaa O., Ankrah S. Vol. 104. 2016. University of Huddersfield Repository. Technological Forecasting & Social Change; pp. 1–15. [Google Scholar]
- Bahram M., Mohseni N., Moghtader M. An introduction to hydrogels and some recent applications. In Intech Open. 2016 [Google Scholar]
- Basu P., Narendra Kumar U., Manjubala I. Wound healing materials - a perspective for skin tissue engineering. Curr. Sci. 2017;112(12):2392–2404. [Google Scholar]
- Baumann L. Skin ageing and its treatment. J. Pathol. 2007;211(2):241–251. doi: 10.1002/path.2098. [DOI] [PubMed] [Google Scholar]
- Bausch and Lomb website. https://www.bausch.com/our-products/contact-lenses/lenses-for-nearsighted-farsighted.
- Bausch and Lomb website. https://www.bausch.com/our-products/contact-lenses/lenses-for-astigmatism.
- Bausch and Lomb website. https://www.bausch.com/our-products/contact-lenses/lenses-for-presbyopia.
- Bausch and Lomb Website.. http://www.bausch.in/our-products/contact-lenses/lenses-for-short-sighted-long-sighted/soflens-daily-disposable-contact-lenses/.
- Berkovitch Y., Seliktar D. Semi-synthetic hydrogel composition and stiffness regulate neuronal morphogenesis. Int. J. Pharm. 2017;523(2):545–555. doi: 10.1016/j.ijpharm.2016.11.032. [DOI] [PubMed] [Google Scholar]
- Besser R.R., Bowles A.C., Alassaf A., Carbonero D., Claure I., Jones E., Reda J., Wubker L., Batchelor W., Ziebarth N., Silvera R., Khan A., Maciel R., Saporta M., Agarwal A. Enzymatically crosslinked gelatin–laminin hydrogels for applications in neuromuscular tissue engineering. Biomater. Sci. 2020;8(2):591–606. doi: 10.1039/c9bm01430f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biogelx Website. https://www.biogelx.com/peptide-hydrogel-products-2/.
- Bonnet M., Trimaille T., Brezun J., Feron F., Gigmes D., Marqueste T., Plasticité E. Motor and sensitive recovery after injection of a physically cross-linked PNIPAAm- g -PEG hydrogel in rat hemisectioned spinal cord. Materials Science & Engineering C. 2020;107(October 2019):110354. doi: 10.1016/j.msec.2019.110354. [DOI] [PubMed] [Google Scholar]
- Bootsma K., Fitzgerald M.M., Free B., Dimbath E., Conjerti J., Reese G., Sparks J.L. 3D printing of an interpenetrating network hydrogel material with tunable viscoelastic properties. J. Mech Behav. Biomed. Mater. 2017;70:84–94. doi: 10.1016/j.jmbbm.2016.07.020. [DOI] [PubMed] [Google Scholar]
- Bulgaria website, Retrieved August 8, 2019, from, https://www.cosmeticsbulgaria.com/en/product/collagen-hydrogel-for-face-dr-derm-professional/.
- Burdick J.A., Anseth K.S. Photoencapsulation of osteoblasts in injectable RGD-modified PEG hydrogels for bone tissue engineering. Biomaterials. 2002;23:4315–4323. doi: 10.1016/s0142-9612(02)00176-x. [DOI] [PubMed] [Google Scholar]
- Caló E., Khutoryanskiy V.V. Biomedical applications of hydrogels: a review of patents and commercial products. Eur. Polym. J. 2015;65:252–267. [Google Scholar]
- Cascone S., Lamberti G. Hydrogel-based commercial products for biomedical applications: a review. Int. J. Pharm. 2019;118803 doi: 10.1016/j.ijpharm.2019.118803. [DOI] [PubMed] [Google Scholar]
- Catanzano O., D’Esposito V., Acierno S., Ambrosio M.R., De Caro C., Avagliano C., Quaglia F. Alginate-hyaluronan composite hydrogels accelerate wound healing process. Carbohydr. Polym. 2015;131:407–414. doi: 10.1016/j.carbpol.2015.05.081. [DOI] [PubMed] [Google Scholar]
- Chai Q., Jiao Y., Yu X. Hydrogels for biomedical applications: their characteristics and the mechanisms behind them. Gels. 2017 doi: 10.3390/gels3010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan B.P., Leong K.W. Scaffolding in tissue engineering: general approaches and tissue-specific considerations. Eur. Spine J. 2008;17 doi: 10.1007/s00586-008-0745-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Cheng R., Zhao X., Zhang Y., Tam A., Yan Y., Shen H., Zhang Y.S., Qi J., Feng Y., Liu L., Pan G., Cui W., Deng L. An injectable self-healing coordinative hydrogel with antibacterial and angiogenic properties for diabetic skin wound repair. NPG Asia Mater. 2019;11:3. [Google Scholar]
- Cibavision Website. http://www.cibavision.com.my/lenses/focus_ dailies/focus_dailies.shtml.
- Coloplast Website. https://www.coloplast.us/woundres-collagen-hydrogel-1-en-us.aspx.
- Connell C.D.O., Di Bella C., Thompson F., Augustine C., Beirne S. Development of the Biopen: a handheld device for surgical printing of adipose stem cells at a chondral wound site. Biofabrication. 2016;8(1) doi: 10.1088/1758-5090/8/1/015019. [DOI] [PubMed] [Google Scholar]
- Cooper vision Website.. https://coopervision.com/contact-lenses/clariti-1-day.
- Corning Website. (n.d.-a). https://www.corning.com/in/en/products/life-sciences/products/surfaces/matrigel-matrix.html.
- Corning Website. (n.d.-b). https://ecatalog.corning.com/life-sciences/b2b/SE/en/Browse-Products-by-Application/3D-Cell-Culture/3D-Cellular-Models/Other-Corning&-ECMs/p/354250.
- Cosmobio Website. (n.d.). https://www.cosmobio.com/contents/mebiol_gel.html.
- Craciun A.M., Mititelu Tartau L., Pinteala M., Marin L. Nitrosalicyl-imine-chitosan hydrogels based drug delivery systems for long term sustained release in local therapy. J. Colloid Interface Sci. 2019;536:196–207. doi: 10.1016/j.jcis.2018.10.048. [DOI] [PubMed] [Google Scholar]
- Croisier F., Jérôme C. Chitosan-based biomaterials for tissue engineering. Eur. Polym. J. 2013;49(4):780–792. [Google Scholar]
- Danyuo Y., Ani C.J., Salifu A.A., Obayemi J.D., Dozie-Nwachukwu S., Obanawu V.O., Akpan U.M., Odusanya O.S., Abade-Abugre M., McBagonluri F., Soboyejo W.O. Anomalous release kinetics of prodigiosin from poly-N-Isopropyl-Acrylamid based hydrogels for the treatment of triple negative breast cancer. Sci. Rep. 2019;9(1):1–14. doi: 10.1038/s41598-019-39578-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Y., Ren J., Chen G., Li G., Wu X., Wang G., Gu G. chitosan-hyaluronic acid based hydrogels for abdominal tissue regeneration. Scientific Reports. April. 2017:1–13. doi: 10.1038/s41598-017-02962-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dermarite website. (n.d.-a). http://dermarite.com/product/aquaderm/.
- Dermarite website. (n.d.-b). http://dermarite.com/product/dermasyn/.
- Dermarite website. (n.d.-c). http://dermarite.com/product/dermagauze/.
- Dragan E.S. Design and applications of interpenetrating polymer network hydrogels. A review Design and applications of interpenetrating polymer network hydrogels. A review. Chem. Eng. J. 2017;243(May 2014):572–590. [Google Scholar]
- Echeverria C., Fernandes S., Godinho M., Borges J., Soares P. Functional stimuli-responsive gels: hydrogels and microgels. Gels. 2018;4(2):54. doi: 10.3390/gels4020054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-sherbiny I.M., Yacoub M.H. Hydrogel scaffolds for tissue engineering: progress and challenges. Glob cardiol sci pract. 2013;3:316–342. doi: 10.5339/gcsp.2013.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elf cosmetics website. (n.d.). https://www.elfcosmetics.com/charcoal-hydrogel-under-eye-masks/500011.html.
- Endo Pharmaceuticals Inc. (n.d.). https://www.supprelinla.com/patients/what-is-supprelin-la/.
- Esibio Website. (n.d.). https://esibio.com/products/product-category/hydrogels-kits/.
- Farandos N.M., Yetisen A.K., Monteiro M.J., Lowe C.R., Yun S.H. Contact lens sensors in ocular diagnostics. Adv. Healthc. Mater. 2015;4(6):792–810. doi: 10.1002/adhm.201400504. [DOI] [PubMed] [Google Scholar]
- Ferring Pharmaceuticals. (n.d.). https://www.cervidil.com/about-cervidil/.
- Finesse Medical Ltd. (n.d.). https://medical.averydennison.com/en/home/products/wound-care-products/amorphous-hydrogel.html.
- Ganji F., Vasheghani-Farahani S., Vasheghani-Farahani E. Theoretical description of hydrogel swelling: a review. Iran. Polym. J. (Engl. Ed.) 2010;19(5):375–398. [Google Scholar]
- Garg S., Garg A. Hydrogel: classification, properties, preparation and technical features. Asian J. Biomat. Res. 2016;2(6):163–170. [Google Scholar]
- Geiges H. A brief history of contact topology. Expo. Math. 2001;19(June 2011):25–53. [Google Scholar]
- Winter George D. formation of the scab and the rate of epithelization of superficial wounds in the skin of the young domestic pig. Nature. 1962;193:293–294. doi: 10.1038/193293a0. [DOI] [PubMed] [Google Scholar]
- Gibas I., Janik H.Z. Review: synthetic polymer hydrogels for biomedical applications. Chem. Chem. Technol. 2010 [Google Scholar]
- Gupta B., Agarwal R., Alam M.S. Woodhead Publishing Limited; 2011. Hydrogels for Wound Healing Applications. Biomedical Hydrogels: Biochemistry. Manufacture and Medical Applications. [Google Scholar]
- Habib M.A., Akter M.A., Alam M.E., Karim Z., Joarder M.T.A. Hydrogel: a noble approach to healthcare. Int. J. Innovat. Pharmaceut. Sci. Res. 2015;3(72):1372–1388. [Google Scholar]
- Hennink W.E., van Nostrum C.F. Novel crosslinking methods to design hydrogels. Adv. Drug Deliv. Rev. 2012;64:223–236. doi: 10.1016/s0169-409x(01)00240-x. [DOI] [PubMed] [Google Scholar]
- Hoare T.R., Kohane D.S. Hydrogels in drug delivery: progress and challenges. Polymer. 2008;49(8):1993–2007. [Google Scholar]
- Holback H., Yeo Y., Park K. Woodhead Publishing Limited; 2011. Hydrogel Swelling Behavior and its Biomedical Applications. Biomedical Hydrogels. [Google Scholar]
- Hollister website. (n.d.). https://www.hollister.com/en/products/Wound-Care-Products/Wound-Dressings/Hydrogel-Dressings/Restore-Hydrogel.
- Hu W., Wang Z., Xiao Y. Advances in crosslinking strategies of biomedical hydrogels. Biomaterials Sci. 2019 doi: 10.1039/c8bm01246f. [DOI] [PubMed] [Google Scholar]
- Images website. (n.d.). https://www.ladymakeup.com/shop/images aloe.
- Iodine Website. (n.d.). https://www.iodine.com/drug/cervidil/fda-package-insert.
- Juric D., Rohner N.A., von Recum H.A. Molecular imprinting of cyclodextrin supramolecular hydrogels improves drug loading and delivery. Macromol. Biosci. 2019;19(1):1–9. doi: 10.1002/mabi.201800246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikgel website. (n.d.). https://kikgel.com.pl/produkty/neoheal/.
- Kim S.J., Kwon S.S., Jeon S.H., Yu E.R., Park S.N. Enhanced skin delivery of liquiritigenin and liquiritin-loaded liposome-in-hydrogel complex system. Int. J. Cosmet. Sci. 2014;36(6):553–560. doi: 10.1111/ics.12156. [DOI] [PubMed] [Google Scholar]
- Ko D.Y., Shinde U.P., Yeon B., Jeong B. Recent progress of in situ formed gels for biomedical applications. Prog. Polym. Sci. 2013;38(3–4):672–701. [Google Scholar]
- Kong X.B., Tang Q.Y., Chen X.Y., Tu Y., Sun S.Z., Sun Z.L. Polyethylene glycol as a promising synthetic material for repair of spinal cord injury. Neural. Regen. Res. 2017;12(6):1003–1008. doi: 10.4103/1673-5374.208597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Y.-C., Wilson A.C., Zantos S.G. 5th. Wiley Online Library; 2014. Contact Lenses. Kirk-Othmer Encyclopedia of Chemical Technology. [Google Scholar]
- Lancome website. (n.d.). https://www.lancome-usa.com/skin-care/masks/advanced-genifique-hydrogel-melting-sheet-mask/LAN192.html.
- Larrañeta E., Stewart S., Ervine M., Al-Kasasbeh R., Donnelly R.F. Hydrogels for hydrophobic drug delivery. Classification, synthesis and applications. J. Funct. Biomater. 2018;9(1) doi: 10.3390/jfb9010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.H., Kim H.W. Emerging properties of hydrogels in tissue engineering. J. Tissue Eng. 2018;9 doi: 10.1177/2041731418768285. 0–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K.Y., Mooney D.J. Hydrogels for tissue engineering. Chem. Rev. 2001;101(7) doi: 10.1021/cr000108x. [DOI] [PubMed] [Google Scholar]
- Lee P., Lok C., Che C., Kao W.J. 2019. A multifunctional hydrogel delivers gold compound and inhibits human lung cancer xenograft. [DOI] [PubMed] [Google Scholar]
- Li J., Mooney David J. Designing hydrogels for controlled drug delivery. Nat. Rev. Mater. 2016;12(1) doi: 10.1038/natrevmats.2016.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Wang Q., Wang O., Shao K., Lin H., Lei Y. A simple and scalable hydrogel-based system for culturing protein-producing cells. PloS One. 2018;13:1–14. doi: 10.1371/journal.pone.0190364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin F., Lu X., Wang Z., Lu Q., Lin G., Lu B. In situ polymerization approach to cellulose – polyacrylamide interpenetrating network hydrogel with high strength and pH-responsive properties. Cellulose. 2018 [Google Scholar]
- Liu H., Wang C., Li C., Qin Y., Wang Z., Yang F., Li Z., Wang J. A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing. RSC Adv. 2018;8(14):7533–7549. doi: 10.1039/c7ra13510f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Chinga-Carrasco G., Cheng F., Xu W., Willför S., Syverud K., Xu C. Hemicellulose-reinforced nanocellulose hydrogels for wound healing application. Cellulose. 2016;23(5):3129–3143. [Google Scholar]
- Liu X., Steiger C., Lin S., Parada G.A., Liu J., Chan H.F., Yuk H., Phan N.V., Collins J., Tamang S., Traverso G., Zhao X. Ingestible hydrogel device. Nat. Commun. 2019;10(1):493. doi: 10.1038/s41467-019-08355-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohmann-rauscher website. (n.d.). https://www.lohmann-rauscher.com/en/products/wound-care/modern-wound-care/suprasorb-g-gel-dressing/.
- Lotfipour F., Alami-Milani M., Salatin S., Hadavi A., Jelvehgari M. Freeze-thaw-induced cross-linked PVA chitosan for oxytetracyclineloaded wound dressing the experimental design and optimization.pdf. Res. Pharmaceut. Sci. 2019:175–189. doi: 10.4103/1735-5362.253365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majid S., Bukhari H., Khan S., Rehanullah M., Ranjha N.M. Synthesis and characterization of chemically cross-linked acrylic acid/gelatin hydrogels: effect of pH and composition on swelling and drug release. Int. J. Polit. 2015;2015 [Google Scholar]
- Mandal B.B., Kapoor S., Kundu S.C. Silk fibroin/polyacrylamide semi-interpenetrating network hydrogels for controlled drug release. Biomaterials. 2009;30(14):2826–2836. doi: 10.1016/j.biomaterials.2009.01.040. [DOI] [PubMed] [Google Scholar]
- Mannarino M.M., Bassett M., Donahue D.T., James F., Biggins J.F., Bassett M., Donahue D.T. Novel high-strength thromboresistant poly ( vinyl alcohol ) -based hydrogel for vascular access applications alcohol ) -based hydrogel for vascular access applications. Journal of Biomaterials Science. Polym. Ed. 2020:1–21. doi: 10.1080/09205063.2019.1706148. [DOI] [PubMed] [Google Scholar]
- Markennovy website. (n.d.). https://markennovy.com/our_products/gentle-59/.
- Matsumoto K., Sakikawa N., Miyata T. Thermo-responsive gels that absorb moisture and ooze water. Nat. Commun. 2018:1–7. doi: 10.1038/s41467-018-04810-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxvue vision website. https://www.maxvuevision.com/index.php/products/clear-lens/airsoft.
- McKesson. (n.d.). https://mms.mckesson.com/product/488936/McKesson-Brand-61-53044.
- McMahon T.T., Zadnik K. Twenty-five years of contact lenses. Cornea. 2000;19(5):730–740. doi: 10.1097/00003226-200009000-00018. [DOI] [PubMed] [Google Scholar]
- Miacare Website. (n.d.). http://www.miacare.com/weben/html/product/show.aspx?num=27.
- Mishra B., Upadhyay M., Reddy Adena S., Vasant B., Muthu M. Hydrogels: an introduction to a controlled drug delivery device, synthesis and application in drug delivery and tissue engineering. Austin J. Biomed. Eng. 2017;4(4) 1037–1. [Google Scholar]
- Mohite P.B., Adhav S.S. A hydrogels: Methods of preparation and applications. Int. J. Adv. Pharm. 2017;6(3):79–85. [Google Scholar]
- Moira website. (n.d.). https://www.moirabeauty.com/products/rose-soothing-hydrogel-mask.
- Munćan J., Mileusnić I., Šakota Rosić J., Vasić-Milovanović A., Matija L. Water properties of soft contact lenses: a comparative near-infrared study of two hydrogel materials. International Journal of Polymer Science. 2016;2016:1–8. [Google Scholar]
- Musgrave C.S.A., Fang F. Contact lens materials: a materials science perspective. Materials. 2019;12(2):261. doi: 10.3390/ma12020261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayanaswamy R., Torchilin V.P. Hydrogels and their applications in targeted drug delivery. Molecules. 2019;24(3):603. doi: 10.3390/molecules24030603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neutrogena website. (n.d.). https://www.neutrogena.com/skin/skin-moisturizers/neutrogena-hydro-boost-water-gel-with-hyaluronic-acid-for-dry-skin/6811047.html.
- Nicolson P.C., Vogt J. Soft contact lens polymers: an evolution. Biomaterials. 2001;22(24):3273–3283. doi: 10.1016/s0142-9612(01)00165-x. [DOI] [PubMed] [Google Scholar]
- Ninan N., Forget A., Shastri V.P., Voelcker N.H., Blencowe A. Antibacterial and anti-inflammatory pH-responsive tannic acid-carboxylated agarose composite hydrogels for wound healing. ACS Appl. Mater. Interfaces. 2016;8(42):28511–28521. doi: 10.1021/acsami.6b10491. [DOI] [PubMed] [Google Scholar]
- O’Brien F.J. Biomaterials & scaffolds for tissue engineering. Mater. Today. 2011;14(3):88–95. [Google Scholar]
- Okay O. General properties of hydrogels. Hydrogel Sensors Actuators. 2010;6:1–15. [Google Scholar]
- Okay Oguz. 2018. Semicrystalline physical hydrogels with shape-memory and self-healing properties. [DOI] [PubMed] [Google Scholar]
- Papakonstantinou E., Roth M., Karakiulakis G. A key molecule in skin aging Hyaluronic acid. Dermato-Endocrinology. December. 2012:253–258. doi: 10.4161/derm.21923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parente M.E., Ochoa Andrade A., Ares G., Russo F., Jiménez-Kairuz A. Bioadhesive hydrogels for cosmetic applications. Int. J. Cosmet. Sci. 2015;37(5):511–518. doi: 10.1111/ics.12227. [DOI] [PubMed] [Google Scholar]
- Parhi R. Cross-linked hydrogel for pharmaceutical applications: a review. Adv. Pharmaceut. Bull. 2017;7(4):515–530. doi: 10.15171/apb.2017.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S.H., Seo J.Y., Park J.Y., Ji Y.B., Kim K., Choi H.S., Choi S., Kim J.H., Min B.H., Kim M.S. An injectable, click-crosslinked, cytomodulin-modified hyaluronic acid hydrogel for cartilage tissue engineering. NPG Asia Mater. 2019;11:30. [Google Scholar]
- Qiao M., Chen D., Ma X., Liu Y. Injectable biodegradable temperature-responsive PLGA – PEG – PLGA copolymers: synthesis and effect of copolymer composition on the drug release from the copolymer-based hydrogels. Int. J. Pharm. 2005;294:103–112. doi: 10.1016/j.ijpharm.2005.01.017. [DOI] [PubMed] [Google Scholar]
- Ribeiro M.P., Morgado P.I., Miguel S.P., Coutinho P., Correia I.J. Dextran-based hydrogel containing chitosan microparticles loaded with growth factors to be used in wound healing. Mate. Sci. Eng. C. 2013;33(5):2958–2966. doi: 10.1016/j.msec.2013.03.025. [DOI] [PubMed] [Google Scholar]
- Rosiak J.M., Ulański P., Rzeźnicki A. Hydrogels for biomedical purposes. Nuclear Inst. Methods Phys. Res. B. 1995;105(1–4):335–339. [Google Scholar]
- Sandeep C., Harikumar S.L., Kanupriya Hydrogels: a smart drug delivery system. Int. J. Res. Pharm. Chem. 2012;2(3):603–614. [Google Scholar]
- Scheuer C.A., Fridman K.M., Barniak V.L., Burke S.E., Venkatesh S. Contact Lens & Anterior Eye Retention of conditioning agent hyaluronan on hydrogel contact lenses. Contact Lens Anterior Eye. 2010;33:S2–S6. doi: 10.1016/j.clae.2010.10.003. [DOI] [PubMed] [Google Scholar]
- Shive M., Bichara A., Berrada M., Ruel-garie E. A thermosensitive chitosan-based hydrogel for the local delivery of paclitaxel. Eur. J. Pharm. Biopharm. 2004;57:53–63. doi: 10.1016/s0939-6411(03)00095-x. [DOI] [PubMed] [Google Scholar]
- Shu X.Z., Liu Y., Palumbo F.S., Luo Y., Prestwich G.D. In situ crosslinkable hyaluronan hydrogels for tissue engineering. Biomaterials. 2004;25:1339–1348. doi: 10.1016/j.biomaterials.2003.08.014. [DOI] [PubMed] [Google Scholar]
- Singh M.R., Patel S., Singh D. Elsevier Inc; 2016. Natural Polymer-Based Hydrogels as Scaffolds for Tissue Engineering. Nanobiomaterials in Soft Tissue Engineering. Chapter 9. [Google Scholar]
- Smith-Nephew Website. (n.d.)., http://www.smith-nephew.com/professional/products/advanced-wound-management/other-wound-care-products/solosite-gel/.
- Smith and Nephew website. (n.d.)., fromhttp://www.smith-nephew.com/professional/products/advanced-wound-management/intrasite-gel/.
- Sri B., Chatterjee A. As A review on hydrogels as drug delivery in the pharmaceutical field. Int. J. Chem. Pharmaceut. Sci. 2014 [Google Scholar]
- Stapleton F., Stretton S., Papas E., Skotnitsky C., Sweeney D.F. Silicone hydrogel contact lenses and the ocular surface. Ocul. Surf. 2006;4(1):24–43. doi: 10.1016/s1542-0124(12)70262-8. [DOI] [PubMed] [Google Scholar]
- Systagenix website. (n.d.). http://www.systagenix.co.za/our-products/hydration/nu-gelandtrade-hydrogel-298.
- Taiki cosmetics website. (n.d.). https://www.taikicosmetics.com/en/masks-patches-wipes/31-lip-patch.html.
- Tang S., Floy M., Bhandari R., Sunkara M., Morris A.J., Dziubla T.D., Hilt J.Z. Synthesis and characterization of thermoresponsive hydrogels based on N – isopropylacrylamide crosslinked with 4, 4 ′ – dihydroxybiphenyl diacrylate. ACS Omega. 2017;2:8723–8729. doi: 10.1021/acsomega.7b01247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari G., Tiwari R., Sriwastawa B., Bhati L., Pandey S., Pandey P., Bannerjee S.K. Drug delivery systems: an updated review. Int. J. Pharmaceut. Invest. 2012;2(1):2–11. doi: 10.4103/2230-973X.96920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trattnig S., Ohel K., Mlynarik V., Juras V., Zbyn S., Korner A. Morphological and compositional monitoring of a new cell-free cartilage repair hydrogel technology - GelrinC by MR using semi-quantitative MOCART scoring and quantitative T2 index and new zonal T2 index calculation. Osteoarthritis Cartilage. 2015;23(12):2224–2232. doi: 10.1016/j.joca.2015.07.007. [DOI] [PubMed] [Google Scholar]
- Ullah F., Bisyrul M., Javed F., Akil H. Classi fi cation, processing and application of hydrogels: a review. Mater. Sci. Eng. C. 2015;57:414–433. doi: 10.1016/j.msec.2015.07.053. [DOI] [PubMed] [Google Scholar]
- Utech S., Boccaccini A.R. A review of hydrogel-based composites for biomedical applications: enhancement of hydrogel properties by addition of rigid inorganic fillers. J. Mater. Sci. 2016;51(1):271–310. [Google Scholar]
- van Bemmelen J.M. The hydrogel and the crystalline hydrate of copper oxide. Z. Anorg. Chem. 1894;5(1):466–483. [Google Scholar]
- Varaprasad K., Malegowd G., Jayaramudu T., Mohan M., Sadiku R. A mini review on hydrogels classi fi cation and recent developments in miscellaneous applications. Mater. Sci. Eng. C. 2017;79:958–971. doi: 10.1016/j.msec.2017.05.096. [DOI] [PubMed] [Google Scholar]
- Verdier-Sévrain S., Bonté F. Skin hydration: a review on its molecular mechanisms. J. Cosmet. Dermatol. 2007;6(2):75–82. doi: 10.1111/j.1473-2165.2007.00300.x. [DOI] [PubMed] [Google Scholar]
- Visio direct Website. (n.d.). https://www.visiondirect.co.uk/everclear-elite.
- Viton C., Agay D., Mari E., Roger T., Chancerelle Y., Domard A. The use of physical hydrogels of chitosan for skin regeneration following third-degree burns. Biomaterials. 2007;28:3478–3488. doi: 10.1016/j.biomaterials.2007.04.021. [DOI] [PubMed] [Google Scholar]
- Wang L., Li J., Zhang D. Dual-enzymatically crosslinked and injectable hyaluronic acid hydrogels for potential application in tissue engineering. RSC Adv. 2020:2870–2876. doi: 10.1039/c9ra09531d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitney J.D. Overview: acute and chronic wounds. Nurs. Clin. 2005;40(2):191–205. doi: 10.1016/j.cnur.2004.09.002. [DOI] [PubMed] [Google Scholar]
- Wichterle O., Lim D. Hydrophilic gels for biological use. Nature. 1960;185:117–118. [Google Scholar]
- Wong T.W., Ramli N.A. Carboxymethylcellulose film for bacterial wound infection control and healing. Carbohydr. Polym. 2014;112:367–375. doi: 10.1016/j.carbpol.2014.06.002. [DOI] [PubMed] [Google Scholar]
- Wound source website. (n.d.). https://www.woundsource.com/product/simpurity-hydrogel-absorbent-sheets.
- Wu X., Stroll S.I., Lantigua D., Suvarnapathaki S., Camci-unal G. Eggshell particle-reinforced hydrogels for bone tissue engineering: an biomaterials science. April. 2019 doi: 10.1039/c9bm00230h. [DOI] [PubMed] [Google Scholar]
- www.fda.gov/medwatch. (2017).
- Xia H. The controlled release and anti-inflammatory activity of a tetramethylpy r azine-loaded thermosensitive poloxamer hydrogel. Pharmaceut. Res. 2019 doi: 10.1007/s11095-019-2580-0. [DOI] [PubMed] [Google Scholar]
- Xu L., Qiu L., Sheng Y., Sun Y., Deng L., Li X., Bradley M., Zhang R. Biodegradable pH-responsive hydrogels for controlled dual-drug release. J. Mater. Chem. B. 2018;6(3):510–517. doi: 10.1039/c7tb01851g. [DOI] [PubMed] [Google Scholar]
- Yang X., Lu Z., Wu H., Li W., Zheng L., Zhao J. Materials Science & Engineering C Collagen-alginate as bioink for three-dimensional ( 3D ) cell printing based cartilage tissue engineering. Materials Science & Engineering C. September. 2017 doi: 10.1016/j.msec.2017.09.002. 0–1. [DOI] [PubMed] [Google Scholar]
- Yu W., Jiang Y.Y., Sun T.W., Qi C., Zhao H., Chen F., Shi Z., Zhu Y.J., Chen D., He Y. Design of a novel wound dressing consisting of alginate hydrogel and simvastatin-incorporated mesoporous hydroxyapatite microspheres for cutaneous wound healing. RSC Adv. 2016;6(106):104375–104387. [Google Scholar]
- Yu Y., Deng C., Meng F., Shi Q., Feijen J., Zhong Z. Novel injectable biodegradable glycol chitosan-based hydrogels crosslinked by Michael-type addition reaction with oligo ( acryloyl carbonate ) – b -poly ( ethylene glycol ) – b -oligo ( acryloyl carbonate ) copolymers. J. Biomed. Mater. Res. 2011:316–326. doi: 10.1002/jbm.a.33199. [DOI] [PubMed] [Google Scholar]