Abstract
Subchondral insufficiency fractures of the knee are commonly misdiagnosed fractures that are both very painful and difficult to treat. A conservative treatment modality to control symptoms during rehabilitation has not previously been described. This case report presents the alternate use of cooled radiofrequency ablation technique of the genicular nerves for pain relief and bisphosphonate infusion to address the underlying poor bone mineralization/density with imaging follow-up before and after instituted treatments. A middle-aged female patient presenting with atraumatic pain in the medial aspect of the left knee diagnosed on an original magnetic resonance imaging as an insufficiency fracture and debilitating pain. Multiple-surgeon opinions of total knee arthroplasty were not a consideration the patient wanted or could consider given her lifestyle. Cooled radiofrequency ablation of the genicular nerve branches was performed with significant-complete pain relief achieved that lasted at least 6 months. Bisphosphonate infusions were instituted to address the underlying osteoporosis detected by a dual energy X-ray absorptiometry (DEXA) scan. Clinical performance after the radiofrequency ablations was followed with clinically validated surveys (The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)/Knee Injury and Osteoarthritis Outcome Score (KOOS)) at 2 weeks, 1, 3, and 6 months. Patient was also asked to follow a restricted-modified weight-bearing plan for 3 months followed by physical therapy. Eight weeks apart of bisphosphonate infusions were delivered after proper administration of vitamin D. There was resolution of the insufficiency fracture at the medial femoral condyle between the magnetic resonance imaging exams within 4.5 months apart treated with restricted weight-bearing regimen. Pain resolution, significant improved function, and range of motion were the end results of our instituted treatment plan. This case reports presents an alternate pathway for the treatment of this condition especially when there is lack of consensus among physicians in how to best address this condition.
Keywords: Knee, SIFK, MRI, Bisphosphonate, Ablations
Introduction
Subchondral insufficiency fractures of the knee (SIFK) are painful, nontraumatic fractures that occur predominantly in the medial femoral condyle of postmenopausal osteoporotic women in their fifth and sixth decades of life. SIFK typically presents with acute knee pain localized to the area of the subchondral fracture [1,2]. These fractures can be recognized radiologically by the presence of a linear subchondral T1-T2 hypointense defect usually located underneath the articular cartilage on magnetic resonance imaging (MRI) with surrounding marrow and soft tissue edema [3]. Other articular pathology such as posterior root medial meniscus tears and resultant meniscal extrusion may be seen on imaging [4]. A previously used term of spontaneous osteonecrosis of the knee is now considered a misnomer given that histologically, osteonecrosis is absent in this setting. Disease progression has been attributed to lesion size and continued weight bearing following the initial fracture [2, 5]. For this reason, immobilization and restricted weight bearing with physical therapy have been proposed as a way to manage the low-grade lesions that will most likely resolve [6]. Other conservative measures such as teriparatide supplementation and bisphosphonates have been employed in treatment of SIFK, though the true benefit of these modalities has been a source of debate [7], [8], [9], [10], [11]. For patients who are unable to tolerate physical therapy and desire definitive treatment, arthroplasty has been shown to be an effective treatment option [12], [13], [14]. However, a conservative treatment regimen that provides adequate pain relief to allow for long-term rehabilitation and recovery has not previously been described.
Given the reported success of nerve ablations in treatment of chronic pain we suggest that radiofrequency ablation of the genicular nerve may be a viable minimally invasive treatment option for management of patients with symptomatic SIFK [15]. Here we report a positive outcome in the case of SIFK in a woman who was managed conservatively with radiofrequency ablations of the genicular nerves and a bisphosphonate regimen, leading to ultimate resolution of her symptoms and complete healing of her necrotic lesion.
Case report
A 66-year-old female presented for evaluation of left knee pain developed without any trauma. The discomfort was located in the medial and anterior aspects of the left knee and driving or standing up from the seated position worsened her pain. She sought orthopedic care and was treated with an anesthetic-corticosteroid injection. Although the injection provided symptomatic pain relief, she also developed palpitations, malaise, and insomnia and was therefore deemed unfit for further corticosteroid injections by her cardiologist. She continued to complain of severe left knee pain as well as decreasing walking tolerance. A DEXA scan demonstrated osteoporosis (T < -2.5) and an MRI of the left knee showed a degenerative tear involving the posterior horn, root attachment, and body of the medial meniscus with patellofemoral articular cartilage degeneration and medial femoral condyle marrow edema (Fig. 1B-1D). A total knee replacement was offered; however, the patient was interested in conservative treatment, so she was referred to interventional radiology for consideration of a genicular nerve block.
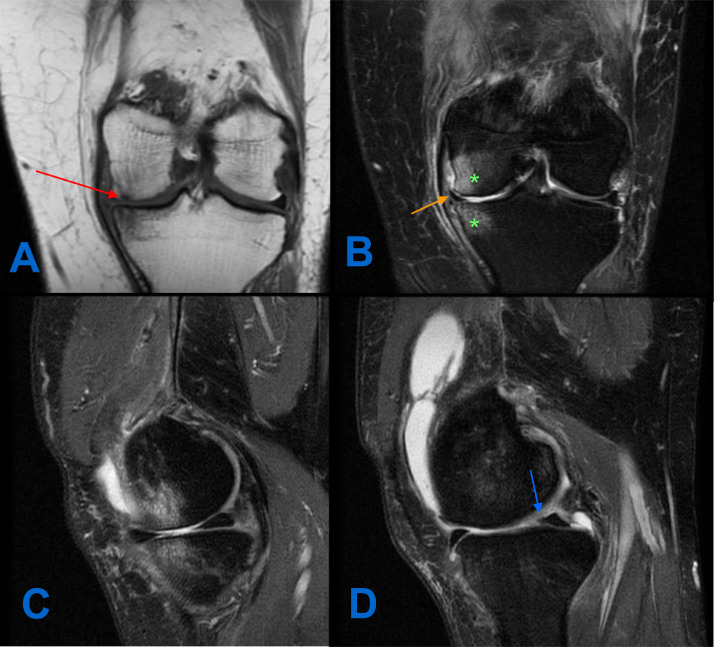
Fig. 1.
Preablation MRI of the left knee: coronal T1-w (A) images demonstrating the T1 hypointense subchondral insufficiency fracture line within the medial aspect of the medial femoral condyle measuring 7mm (red arrow). (B and C) Coronal proton density fat saturation (PD FS) and Sagittal PD FS images at the same level demonstrating the reciprocal bone marrow edema in the medial femoral condyle and medial tibial plateau (asterisk), as well as a tear of the medial meniscal body (orange arrow). Sagittal PD FS image at the level of the posterior horn/root junction of the medial meniscus demonstrating blunting of the medial meniscus compatible with free edge radial tear (blue arrow).
She was seen in our clinic and reported total modification of her lifestyle to avoid aggravating her knee pain. Her left knee remained her primary concern. She reported pain at rest that was 5/10 in severity and worsened to 9/10 with activity. She maintained full range of motion. On further review of her prior MRI, a small subchondral insufficiency fracture along the medial aspect of the left medial femoral condyle measuring 7 × 8 mm was accompanied by adjacent subchondral marrow edema and a complex meniscal tear (Fig. 1A). She was deemed to be an appropriate candidate for a left knee genicular nerve block procedure and pending relief with the nerve block of at least 50%, subsequent genicular nerve ablation utilizing cooled radiofrequency ablation technique. The patient agreed and underwent the nerve block 10 days later. She reported immediate improvement, stating her pain improved to 2 to 3/10 in severity for a few weeks afterward.
Diagnostic genicular nerve block procedure
The patient was first placed supine on the fluoroscopy table with feet and ankles secured to the fluoroscopy table with sturdy tape to assure leg immobility during the procedure. Skin wheal was first made utilizing 1 to 2 mL of 1% lidocaine for superficial local anesthesia in order to avoid involvement of the genicular nerves. Needle placement was confirmed in both anterior to posterior (A-P) and lateral planes with extra care to ensure that the condyles of the femur were superimposed over one another on the lateral imaging to ensure needle placement accuracy (Fig. 4). At each needle site, 1.0 mL of 2% lidocaine was injected without complications.
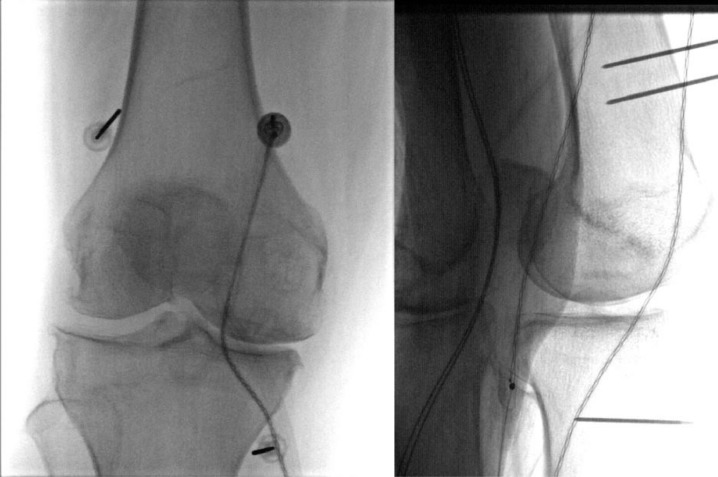
Fig. 4.
Frontal and lateral views of a knee demonstrating proper needle placement.
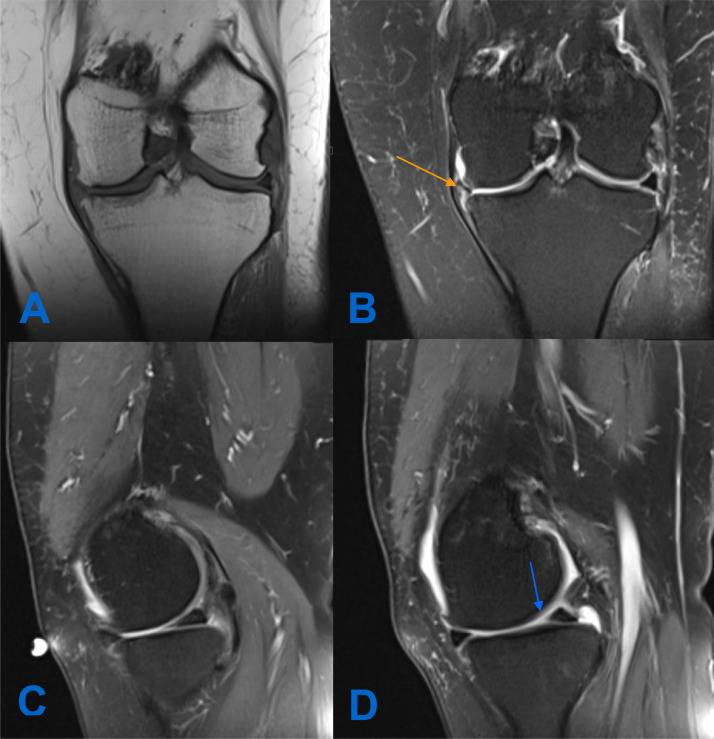
Cooled radiofrequency ablations of the genicular nerves were therefore performed 2 weeks later without any complications. Patient experienced pain relief within two weeks after the ablations that lasted for at least 6 months. After the ablations, she was started on weekly high-dose vitamin D (20,000 IU) for 4 months in preparation for bisphosphate therapy. This was followed by 2 infusions of ibandronate 8 weeks apart. She was restricted to touch down weight bearing for 3 months following the procedure, after which she was advanced by physical therapy. There was marked, progressive improvement in the patient's pain and functional status during her rehabilitation and treatment (Fig. 2). At her 8-week follow-up, she denied pain entirely while at rest and reported slight discomfort (1-2/10) with limited activity. MRI of the left knee performed at 4.5 months post-op demonstrated decreasing joint effusion and resolution of the subchondral marrow edema with slight progression of the medial meniscus tear (Fig. 3).
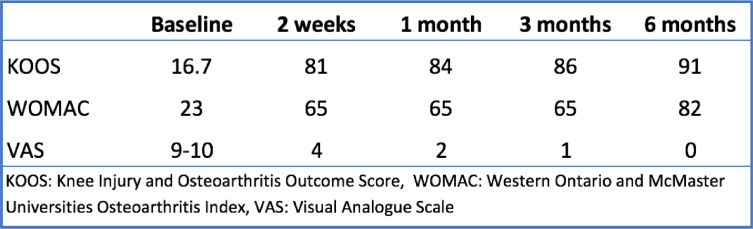
Fig. 2.
Functional outcome scores after radiofrequency ablation compared to baseline.
Fig. 3.
Postablation MRI of the left knee: coronal T1-w and PD FS images (A) of the left knee post ablation demonstrating resolution of the previous subchondral insufficiency fracture within the medial femoral condyle. Coronal and Sagittal PD FS (B and C) at the same level also showing complete resolution of the previously seen bone marrow edema, as well as progression of the medial meniscal tear (orange arrow). Sagittal PD FS image at the level of the medial meniscus posterior horn/root junction also showing further blunting of the posterior horn when compared to Fig. 1 (blue arrow).
Genicular nerve radiofrequency ablation procedure
Similar steps were followed as during the diagnostic block procedures. Conscious sedation (midazolam 1-2 mg IV and/or fentanyl 25-100 mcg IV) and supplemental nasal cannula oxygen were given. Skin and soft tissues were anesthetized with 1 to 2 mL of 1% lidocaine at each of the three anatomic sites for RFA. Seventy-five millimeters 17-gauge introducer needle was placed in the 3 locations abovementioned. Once the introducer needle was placed, the 18 g internally cooled, 4 mm active tip-RFA electrode (Coolief, Halyard Health, Alpharetta, GA, USA) was placed into the introducer needle, and positioning was verified with A-P and lateral fluoroscopic views. Testing at 2 Hertz at 1 mA was performed to test for motor nerve activity. Then 1 mL of 2% lidocaine was injected through the introducer needles. Each target was sequentially treated for 2 minutes and 30 seconds at a set temperature of 60°C, which a tissue temperature of 77°C to 80°C surrounding the electrode [15]. Electrode position is shown in Fig. 4.
Discussion
Given the relative infrequency with which subchondral insufficiency fractures of the knee are diagnosed, a consensus regarding classification and management does not currently exist. Outcomes vary widely even among patients who are managed with similar protocols, suggesting that treatment algorithms may benefit from further classification of these fractures based on prognosis. We previously proposed a SIFK grading system based on lesion size and associated pathology as viewed on MRI [6]. The size of SIFK lesions appears to be a valid indicator of outcome, with large size [mean sum of dimensions ≥26 mm; A-P mean values of 16.78 ± 7.88 and TR (transverse) dimensions of 13.14 ±3.13] portending irreversibility with conservative management (sensitivity of 91%). Arthroplasty and joint-preserving procedures may be better reserved for these fractures.
Conservative management of patients with smaller lesions or those who opt against surgery is more challenging. Barriers to recovery include the severe pain typically associated with these fractures as well as a slow rate of healing, often requiring extensive periods of nonweight bearing or invasive procedures. Bisphosphonates have been proposed as an adjunct therapy to aid in healing and prevent subchondral collapse [8,9]. Pain-management strategies to date have included oral and topical analgesics, immobilization, and physical therapy. However, these modalities in many cases are insufficient to control symptoms for the long duration of rehabilitation. Radiofrequency ablation of the genicular nerve has previously been shown to be effective in other chronic pain disorders of the knee, though to our knowledge it has never used in symptomatic management of SIFK. In our case, this was offered to a patient with a debilitating low-grade SIFK who was undesiring of surgery.
Conclusion
Our patient, a middle-aged, osteoporotic woman with a subchondral insufficiency fracture of the medial femoral condyle and medial meniscus tears with extrusion, is the classic presentation of SIFK. Her fracture dimensions totaled 15 mm and therefore she was deemed a good candidate for nonoperative management. Cooled radiofrequency ablation of the genicular nerve provided sufficient pain relief to allow our patient to tolerate physical therapy after a prolonged nonweight-bearing protocol. Supplementation with vitamin D and ibandronate were used to improve bone density during rehabilitation. She had eventual resolution of her fracture within 4.5 months and had subsequent return to baseline activity without limitation. We therefore submit this report to raise the possibility of cooled radiofrequency ablation as a conservative therapy to provide symptomatic relief for low-grade SIFK lesions. Larger studies with additional subjects would be an important next step in elucidating the role of nerve blocks in management of these fractures.
Consent was also from the patient prior to considering the case for publication.
Declarations
-
•
Ethics approval and consent to participate was obtained from our institution IRB committee prior to submission of this case.
-
•
Consent for publication was obtained from the coauthors prior to submission of this case.
-
•
Availability of data and materials: The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Footnotes
Declaration of competing interest: None.
Funding: None.
Authors’ contributions: All authors contributed to the different sections for publication satisfying the STARD guidelines for authorship. Dr Gonzalez, Dr Reimer, and Dr Phil were involved in the planning, conduct, reporting, conception, and design of this work. The remaining authors were involved in the acquisition of data or analysis and interpretation of the data.
Acknowledgment: None.
References
- 1.Wilmot AS, Ruutiainen AT, Bakhru PT, Schweitzer ME, Shabshin N. Subchondral insufficiency fracture of the knee: a recognizable associated soft tissue edema pattern and a similar distribution among men and women. Eur J Radiol. 2016;85(11):2096–2103. doi: 10.1016/j.ejrad.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 2.Yamamoto T, Bullough PG. Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. JBJS. 2000;82(6):858. doi: 10.2106/00004623-200006000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Zywiel MG, McGrath MS, Seyler TM, Marker DR, Bonutti PM, Mont MA. Osteonecrosis of the knee: a review of three disorders. Orthopedic Clin North Am. 2009;40(2):193–211. doi: 10.1016/j.ocl.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Yamagami R, Taketomi S, Inui H, Tahara K, Tanaka S. The role of medial meniscus posterior root tear and proximal tibial morphology in the development of spontaneous osteonecrosis and osteoarthritis of the knee. The Knee. 2017;24(2):390–395. doi: 10.1016/j.knee.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Zanetti M, Romero J, Dambacher MA, Hodler J. Osteonecrosis diagnosed on MR images of the knee: relationship to reduced bone mineral density determined by high resolution peripheral quantitative CT. Acta Radiologica. 2003;44(5):525–531. doi: 10.1080/j.1600-0455.2003.00108.x. [DOI] [PubMed] [Google Scholar]
- 6.Sayyid S, Younan Y, Sharma G, Singer A, Morrison W, Zoga A. Subchondral insufficiency fracture of the knee: grading, risk factors, and outcome. Skeletal Radiol. 2019;48(12):1961–1974. doi: 10.1007/s00256-019-03245-6. [DOI] [PubMed] [Google Scholar]
- 7.Gourlay ML, Renner JB, Spang JT, Rubin JE. Subchondral insufficiency fracture of the knee: a non-traumatic injury with prolonged recovery time. BMJ Case Rep. 2015 doi: 10.1136/bcr-2015-209399. bcr2015209399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraenzlin ME, Graf C, Meier C, Kraenzlin C, Friedrich NF. Possible beneficial effect of bisphosphonates in osteonecrosis of the knee. Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1638–1644. doi: 10.1007/s00167-010-1106-4. [DOI] [PubMed] [Google Scholar]
- 9.Meier C, Kraenzlin C, Friederich NF, Wischer T, Grize L, Meier CR. Effect of ibandronate on spontaneous osteonecrosis of the knee: a randomized, double-blind, placebo-controlled trial. Osteoporos Int. 2014;25(1):359–366. doi: 10.1007/s00198-013-2581-5. [DOI] [PubMed] [Google Scholar]
- 10.An VV, Van Den Broek M, Oussedik S. Subchondral insufficiency fracture in the lateral compartment of the knee in a 64-year-old Marathon runner. Knee Surg Relat Res. 2017;29(4):325. doi: 10.5792/ksrr.17.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jureus J, Lindstrand A, Geijer M, Roberts D, Tägil M. Treatment of spontaneous osteonecrosis of the knee (SPONK) by a bisphosphonate: A prospective case series with 17 patients. Acta Orthopaedica. 2012;83(5):511–514. doi: 10.3109/17453674.2012.729184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mont MA, Rifai A, Baumgarten KM, Sheldon M, Hungerford DS. Total knee arthroplasty for osteonecrosis. JBJS. 2002;84(4):599–603. doi: 10.2106/00004623-200204000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Radke S, Wollmerstedt N, Bischoff A, Eulert J. Knee arthroplasty for spontaneous osteonecrosis of the knee: unicompartimental vs bicompartimental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2005;13(3):158–162. doi: 10.1007/s00167-004-0551-3. [DOI] [PubMed] [Google Scholar]
- 14.Myers TG, Cui Q, Kuskowski M, Mihalko WM, Saleh KJ. Outcomes of total and unicompartmental knee arthroplasty for secondary and spontaneous osteonecrosis of the knee. JBJS. 2006;88(3):76–82. doi: 10.2106/JBJS.F.00568. [DOI] [PubMed] [Google Scholar]
- 15.Jamison DE, Cohen SP. Radiofrequency techniques to treat chronic knee pain: a comprehensive review of anatomy, effectiveness, treatment parameters, and patient selection. J Pain Res. 2018;11:1879. doi: 10.2147/JPR.S144633. [DOI] [PMC free article] [PubMed] [Google Scholar]