Abstract
Background
High-flow nasal cannula (HFNC) oxygen therapy is widely applied in idiopathic pulmonary fibrosis (IPF) patients with acute respiratory failure (ARF); however, its advantages over mechanical ventilation (MV) remain unclear. We aimed to compare the clinical outcomes of HFNC oxygen therapy and MV in IPF patients with respiratory failure.
Methods
A retrospective descriptive study of patients with IPF admitted between January 2015 and December 2017 who underwent HFNC oxygen therapy or MV during hospitalization was conducted. The primary outcome was the comparison of in-hospital mortality among HFNC only group, MV with prior HFNC group, and MV only group.
Results
A total of 61 patients with IPF and ARF were included in the current study. Forty-five patients received HFNC oxygen therapy without endotracheal intubation and 16 received MV. The overall hospital mortality rate was 59.0%, of which 53.3% was for HFNC oxygen therapy and 55.6% (5/9) for MV only group (P=1.000). Although no significant difference in the mortality rate was observed among three groups, that of MV with prior HFNC oxygen therapy (n=7) was 100% (P=0.064). Additionally, the HFNC oxygen therapy group showed shorter length of hospital and ICU stay than the MV group (P<0.001).
Conclusions
Patients with IPF and ARF who received MV with prior HFNC oxygen therapy showed increased mortality rate than those who received HFNC only oxygen therapy or MV. Considering the complication rate of MV, need for lung transplantation, and the will to undergo end-of-life care, a proper transition from HFNC oxygen therapy to MV should be planned cautiously.
Keywords: Idiopathic pulmonary fibrosis (IPF), high flow nasal cannula (HFNC), mechanical ventilation (MV)
Introduction
Idiopathic pulmonary fibrosis (IPF) is a serious disease that causes respiratory failure by progressive lung fibrosis. Studies have reported an increase in the incidence of IPF and the resultant deaths (1,2). In recent years, although nintedanib and pirfenidone have been shown to be effective disease-modifying agents, their beneficial effect on the prognosis of patients with IPF has been limited. Lung transplantation is the only definitive therapy in pharmacologically refractory IPF; however, only a small proportion of patients undergo the procedure due to insufficient supply of donor organs, technical challenges associated with the transplantation, or peri-operative conditioning (3). In the United States, the median period of survival of patients with IPF aged 65 years and older is only 3.8 years (4). In particular, the prognosis is extremely poor in IPF patients experiencing acute respiratory failure (ARF), the in-hospital mortality reaching almost 85%. Moreover, mechanical ventilation (MV) does not have a significant therapeutic effect on the survival, unlike in ARF caused by other etiologies (5). Impaired gas exchange and reduced pulmonary compliance lead to high peak airway pressure, tidal volume, and fraction of inspired oxygen (FiO2). These traumatic components could accelerate progression of the disease (6).
High-flow nasal cannula (HFNC) oxygen therapy is a technique that can deliver a FiO2 up to 1.0 by supplying warm, humidified oxygen through a nasal cannula. Recently, various attempts have been made to apply HFNC oxygen therapy to patients with ARF. Although the technique does not reduce the need for endotracheal intubation or mortality compared to conventional oxygen therapy or non-invasive ventilation (NIV), it has advantages such as patient comfort and tolerability (7). We reported that delayed intubation in the late HFNC oxygen therapy failure group increases the mortality rate (8). Because we included various etiologies of respiratory failure for analysis in this study, the outcome of HFNC oxygen therapy in IPF patients with the high mortality rate associated with MV may be different (9). The current study compared the clinical outcomes of HFNC oxygen therapy and MV in IPF patients admitted due to ARF.
Methods
Patients and study design
The institutional review board of Asan Medical Center (IRB No. 2019-0222) approved the current study. Informed consent was waived owing to the retrospective design of the study based on medical records.
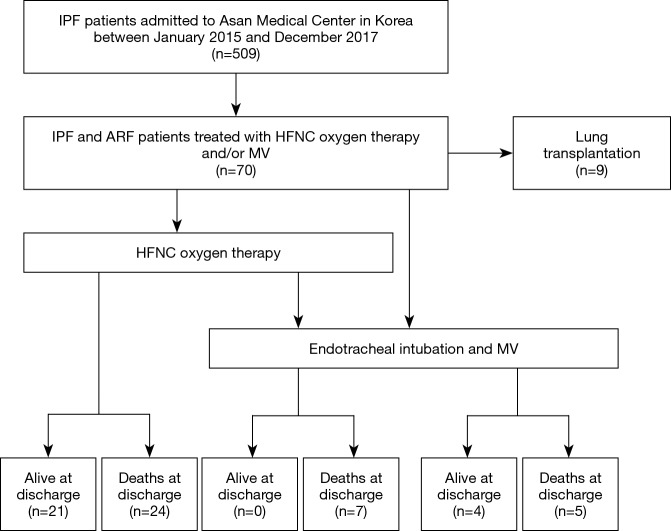
This retrospective descriptive study was conducted on patients with IPF who were admitted to the Asan Medical Center, Seoul, Korea, from January 2015 to December 2017 and underwent HFNC oxygen therapy or MV during hospitalization (Figure 1). Patients were divided into three groups (HFNC only group, MV with prior HFNC group and MV only group). The study subjects were limited to those who had an established diagnosis of IPF according to the statement of the American Thoracic Society (ATS)/European Respiratory Society (ERS)/Japanese Respiratory Society (JRS)/Latin American Thoracic Association (ALAT) (10), and who were followed up at this hospital.
Figure 1.
Distribution of the study population according to therapy and outcome. IPF, idiopathic pulmonary fibrosis; ARF, acute respiratory failure; HFNC, High-flow nasal cannula; MV, mechanical ventilation.
Data collection
The demographic factors and clinical parameters of the patients were reviewed from the electronic medical records. The results of the most recent (within six months) spirometry and diffusing capacity of the lung for carbon monoxide (DLCO) were retrieved to assess the severity of IPF before admission and the GAP index (11) and du Bois score (12) were calculated based on this information. Status of the patients at the time of admission was confirmed by vital signs and arterial blood gas analysis (ABGA).
Study outcomes
The primary outcome measure was in-hospital mortality, which was compared among HFNC only group, MV with prior HFNC group, and MV only group. Other pre-specified outcome measures were length of hospital stay, length of intensive care unit (ICU) stay, and the proportion of do-not-resuscitate (DNR) consent status. The vital signs were evaluated in patients who underwent HFNC oxygen therapy before the initiation of treatment and after 8 hours of treatment to indirectly assess respiratory distress. Ventilator-associated complications were reviewed in patients who underwent MV. Possible ventilator-associated pneumonia (PVAP) was defined based on the ventilator-associated event (VAE) surveillance algorithm definition by the Centers for Disease Control and Prevention (CDC) National Health Safety Network (13).
Statistical analyses
The results are represented as mean values and standard deviations (SD) or median and interquartile range (IQR) for continuous variables and numbers and percentages for categorical data. Group comparisons were based on the Fisher’s exact test or χ2 test for categorical data, and Kruskal-Wallis test for continuous data. All statistical results were evaluated using SPSS for Windows (Version 21.0, IBM Corporation, Chicago, IL, USA).
Results
Patient characteristics
A total of 61 patients with IPF and ARF were included in the current study. There were a higher number of male patients (n=48, 78.7%), and the mean age was 70.8 years. No significant difference was observed among three groups, except the baseline history of coronary artery disease. Most patients had advanced IPF (Table 1). GAP index stage III was the most common and the mean du Bois score was 42.8. The vital signs and ABGA results of the patients were not significantly different between the groups at the time of admission (Table 2).
Table 1. Baseline characteristics of study patients.
| Characteristics | HFNC only group (n=45) | MV with prior HFNC (n=7) | MV only group (n=9) | P value† |
|---|---|---|---|---|
| Male sex, n (%) | 35 (77.8) | 5 (71.4) | 8 (88.9) | 0.670 |
| Age, years | 71.0±7.6 | 69.9±8.8 | 70.4±9.1 | 0.974 |
| BMI (kg/m2) | 23.8±3.2 | 25.3±4.0 | 22.8±2.9 | 0.523 |
| TLC, % predicted* | 43.0±22.7 | 49.6±9.9 | 50.1±21.1 | 0.602 |
| FVC, % predicted* | 47.1±10.1 | 43.6±8.7 | 52.3±11.9 | 0.312 |
| FEV1, % predicted* | 56.6±12.0 | 52.1±11.4 | 63.7±13.2 | 0.208 |
| DLCO, % predicted* | 23.6±14.5 | 24.3±6.1 | 23.6±22.7 | 0.981 |
| Home oxygen therapy, n (%) | 34 (75.6) | 4 (57.1) | 6 (66.7) | 0.555 |
| IPF treatment, n (%) | 0.232 | |||
| Nintedanib | 8 (17.8) | 2 (28.6) | 0 (0.0) | |
| Pirfenidone | 6 (13.3) | 1 (14.3) | 0 (0.0) | |
| Glucocorticoids | 21 (46.7) | 3 (42.9) | 3 (33.3) | |
| Other | 2 (4.4) | 0 (0.0) | 2 (22.2) | |
| Treatment interruptions | 8 (17.8) | 1 (14.3) | 4 (44.4) | |
| GAP index stage, n (%) | 0.750 | |||
| II | 13 (28.9) | 3 (42.9) | 3 (33.3) | |
| III | 32 (71.1) | 4 (57.1) | 6 (66.7) | |
| du Bois score | 42.4±12.3 | 50.9±10.3 | 41.6±16.7 | 0.261 |
| Underlying disease, n (%) | ||||
| Diabetes | 16 (35.6) | 3 (42.9) | 6 (66.7) | 0.222 |
| Hypertension | 16 (35.6) | 2 (28.6) | 5 (55.6) | 0.459 |
| Solid malignancies | 17 (37.8) | 1 (14.3) | 3 (33.3) | 0.476 |
| Liver disease | 3 (6.7) | 0 (0.0) | 0 (0.0) | 0.571 |
| Coronary artery disease | 0 (0.0) | 2 (28.6) | 2 (22.2) | 0.002 |
| Pulmonary hypertension | 28 (62.2) | 3 (42.9) | 5 (55.6) | 0.609 |
HFNC, high flow nasal cannula; BMI, body mass index; TLC, total lung capacity; FVC, forced vital capacity; DLCO, carbon monoxide diffusing capacity; GAP, gender, age, and physiology. *Spirometry and DLCO values are based on the most recent values within 6 months before admission. †P value <0.05 among HFNC group, MV with prior HFNC, and MV only group.
Table 2. Physiologic and laboratory data of patients at hospital admission.
| Parameters | HFNC only group (n=45) | MV with prior HFNC (n=7) | MV only group (n=9) | P value† |
|---|---|---|---|---|
| Systolic blood pressure (mmHg) | 122.7±20.2 | 121.7±16.0 | 120.1±27.8 | 0.975 |
| Diastolic blood pressure (mmHg) | 76.7±15.2 | 75.9±15.4 | 68.9±20.1 | 0.512 |
| Pulse rate (beats/min) | 109.7±21.1 | 113.1±20.3 | 120.0±28.7 | 0.819 |
| Respiratory rate (breaths/min) | 30.1±8.2 | 22.6±3.2 | 28.9±4.8 | 0.010 |
| Body temperature (°C) | 36.9±0.7 | 37.1±0.9 | 37.1±0.6 | 0.562 |
| Arterial pH | 7.45±0.06 | 7.45±0.06 | 7.39±0.06 | 0.056 |
| PaCO2 (mmHg) | 37.1±6.6 | 39.3±12.0 | 42.4±7.1 | 0.130 |
| PaO2 (mmHg) | 82.9±47.7 | 87.9±44.0 | 97.6±42.0 | 0.366 |
| Bicarbonate (mmHg) | 25.8±4.1 | 26.9±6.2 | 25.8±3.3 | 0.910 |
| PaO2/FiO2 (mmHg) | 202.9±124.8 | 197.7±82.0 | 196.8±97.3 | 0.927 |
†P value <0.05 among HFNC group, MV with prior HFNC, and MV only group. HFNC, high flow nasal cannula; MV, mechanical ventilation.
Clinical course and outcome
With the worsening of oxygenation, 45 patients received HFNC oxygen therapy without endotracheal intubation and 16 patients underwent MV. None of the subjects applied NIV during their hospital stay. Seven patients who received MV underwent endotracheal intubation for clinical progression such as hypoxemia and respiratory distress during HFNC oxygen therapy and nine patients received MV without prior application of HFNC oxygen therapy. In the HFNC only group, the average time from the admission to the appliance was 3.0 days and the PF ratio was 155.6±65.2 mmHg. The initial settings of HFNC oxygen therapy were a median flow rate of 35 L/min (IQR 35 to 40) and FiO2 of 0.60 (IQR 0.50 to 0.80). Respiratory and pulse rate decreased at eight hours after application of HFNC oxygen therapy from 28.9 to 24.5 breaths/min and from 103.9 to 90.5 beats/min, respectively (Table 3).
Table 3. Changes in vital sign after application of HFNC.
| Parameters | Pre-HFNC application | Post-HFNC application | P value |
|---|---|---|---|
| Systolic blood pressure (mmHg) | 120.3±21.6 | 118.4±18.4 | 0.925 |
| Diastolic blood pressure (mmHg) | 74.1±13.5 | 74.3±11.8 | 0.785 |
| Pulse rate (beats/min) | 103.9±17.1 | 90.5±16.7 | <0.001 |
| Respiratory rate (breaths/min) | 28.9±6.0 | 24.5±3.6 | <0.001 |
HFNC, high flow nasal cannula.
The PF ratio before intubation in the MV only group was 143.4±75.5 mmHg. In the MV with prior HFNC oxygen therapy group, the average time from application of HFNC oxygen therapy to MV was 5 (3–5.5) days and the PF ratio was 120.4±55.9 mmHg at intubation. In patients who underwent MV, PVAP occurred in five of 16 patients (31.2%), and barotrauma (e.g., pneumomediastinum or pneumothorax) occurred in two patients (12.5%) during the procedure.
The hospital mortality rate of the study subjects was 59.0% (36/61), 53.3% (24/45) of which was for HFNC oxygen therapy only group and 55.6% (5/9) for MV only group (P=1.000). Although no difference in mortality was observed among the three groups, the mortality rate of patients who underwent MV with prior HFNC oxygen therapy was 100% (P=0.064). The 87.5% (21/24) of non-survivors in the HFNC only group was with their family during the end of life. Significant difference was observed between the groups in terms of the lengths of hospital and ICU stays (P<0.001 each) (Table 4).
Table 4. Clinical outcomes.
| Parameters | HFNC only group (n=45) | MV with prior HFNC (n=7) | MV only group (n=9) | P value† |
|---|---|---|---|---|
| Hospital mortality, n (%) | 24 (53.3) | 7 (100.0) | 5 (55.6) | 0.064 |
| Deaths in ICU, n (%) | 3 (6.7) | 7 (100.0) | 5 (55.6) | <0.001 |
| Length of hospital stay, days | 13 (7–18) | 19 (11–38.5) | 24 (12–31) | 0.134 |
| Length of ICU stay, days | 0 (0–0)‡ | 14 (8–24.5) | 7 (6–15) | <0.001 |
| DNR consent, n (%) | 30 (66.7) | 3 (42.9) | 4 (44.4) | 0.272 |
| Death without DNR consent, n (%) | 0 (0.0) | 4 (57.1) | 1 (11.1) | 0.001 |
| Time to death after DNR consent, days | 1 (0–4) | 0 (0–1) | 0 (0–1) | 0.563 |
HFNC, high flow nasal cannula; MV, mechanical ventilation; DNR, do-not-resuscitate. †P value <0.05 among HFNC group, MV with prior HFNC, and MV only group. ‡Only three died in ICU and the lengths of ICU stay were 1, 3 and 3 days, respectively.
Discussion
The current study retrospectively reviewed the clinical outcomes of advanced IPF patients with respiratory failure who required HFNC oxygen therapy or MV. The proportion of HFNC oxygen therapy was higher than MV in IPF patients with ARF. Most patients in the HFNC oxygen therapy group stayed with their family in the general ward, and non-survivors of this group received end-of-life care under DNR state. Although no significant difference in the in-hospital mortality rate was observed between the HFNC oxygen therapy and MV groups, the mortality rate of patients in the HFNC oxygen therapy failure group who were transitioned to MV was extremely high.
Respiratory failure in patients with IPF patients carries a miserable outcome, and no effective treatment is present to reverse progression of the condition (14). More than half of the patients in the current study died in the hospital, regardless of application of HFNC oxygen therapy or MV. In addition to not being able to reverse the course of the disease, the choice of MV could cause patient discomfort, increased requirement for sedation and ventilator-associated pneumonia. Particularly, the lung is vulnerable to the stress of MV due to progression of fibrosis. In the current study, complications related to MV occurred in many patients in the MV group. When considering the distinct characteristics of the disease, endotracheal intubation in acute respiratory failure in patients with advanced IPF is controversial. Nevertheless, according to a recent report, approximately 10% of IPF patients continue to receive MV, and is associated with increased admission cost and mortality (9).
HFNC can deliver a high concentration of humidified oxygen at a fraction of inspired oxygen of 1.0 (100%). The high flow rates of the nasal cannula generate a low level of positive pressure in the upper airway and lighten the work of breathing by reducing the physiologic dead space (15). HFNC oxygen therapy has gained popularity and is routinely used for the treatment of hypoxemic respiratory failure. Synthetically, HFNC oxygen therapy has the advantages of convenience and patient comfort when compared to invasive MV. Owing to its advantages, an expansion in the scope of application of HFNC oxygen therapy is being observed, both before and after intubation and end-of-life care, in addition to acute respiratory failure. Peters et al. have proposed HFNC oxygen therapy as an effective respiratory support for patients with respiratory failure in do-not-intubate status (16). HFNC oxygen therapy demonstrated palliative benefit, such as improved patient oxygenation and decreased respiratory rate, and was well tolerated. Similarly, reduction in the respiratory frequency and pulse rate of patients was observed after HFNC oxygen therapy in the current study. These findings suggest that HFNC oxygen therapy may be an effective adjunctive therapy for IPF patients with respiratory failure. However, in the current study, higher mortality was observed following the application of MV in cases of failure of HFNC oxygen therapy compared with other studies. In a previous study, high rate of mortality was observed when intubation was delayed due to failure of HFNC oxygen therapy (8), and mechanical ventilation may not have an additional therapeutic benefit because the cause of respiratory failure is not well corrected in patients with IPF with a pre-existing fibrotic component. Ventilator support can be used only as a bridge to lung transplant in cases of failure of HFNC oxygen therapy (17).
Early integrated palliative care is essential for patients with advanced IPF due to limited life expectancy and the heavy burden of symptoms. Despite recommendations for palliative care, the majority of IPF patients continue to receive life-prolonging procedures such as non-invasive ventilation, and end-of-life decisions are often delayed (18). Decision to refrain from intubation usually depends on the assessment of futility of care, wishes of the patient, and high probability of poor quality of life in the future (19). In the current study, non-survivors in the MV group showed lower agreement on the DNR order, which was very late, i.e., average 2 days prior to death. This may be associated with the low awareness of end-of-life care in patients with advanced IPF. In addition, patients with IPF receiving MV are referred to palliative care in a minority of cases (20). Therefore, in instances of no further treatment plan such as lung transplantation, the decision to perform invasive ventilation should be made in a discrete manner. HFNC oxygen therapy is advantageous in patients with advanced IPF in that they can make end-of-life decisions on their own until the last minute of consciousness, as patients are able to communicate unlike endotracheal intubation. HFNC oxygen therapy also plays a role in palliative care because symptoms such as shortness of breath can be relieved, and consumption of food and drink is facilitated. Therefore, in cases of patients with advanced IPF who are hospitalized with acute respiratory failure, wherein active integrated palliative care and end-of-life decisions are required, HFNC oxygen therapy may be the most appropriate modality for respiratory support.
The current study has several limitations. First, a single center, retrospective study might be associated with selection bias of patients. The application of the HFNC oxygen therapy or MV was based on the clinical decision of the physician. Although the baseline characteristics such age, pulmonary functions, and severity were compared, the sicker patient might have included in the MV group. However, a randomized trial is difficult due to the poor outcome of MV and routine application of HFNC oxygen therapy. Second, too few patients were included to analyze the statistical meaningful difference. Third, intubation was an inevitable step when patients and families disagreed for DNR despite the clinician recognizing the poor prognosis of the disease.
Conclusions
In the current retrospective study, the HFNC group showed shorter duration of stay in the hospital and ICU without difference in mortality. However, the application of MV in the HFNC oxygen therapy failure group showed extremely higher mortality. Considering the complications of MV and the end-of-life care, the further study for the guideline of the transition to MV are needed.
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The institutional review board of Asan Medical Center (IRB No. 2019-0222) approved the current study. Informed consent was waived owing to the retrospective design of the study based on medical records.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Hutchinson J, Fogarty A, Hubbard R, et al. Global incidence and mortality of idiopathic pulmonary fibrosis: a systematic review. Eur Respir J 2015;46:795-806. 10.1183/09031936.00185114 [DOI] [PubMed] [Google Scholar]
- 2.Hutchinson JP, McKeever TM, Fogarty AW, et al. Increasing global mortality from idiopathic pulmonary fibrosis in the twenty-first century. Ann Am Thorac Soc 2014;11:1176-85. 10.1513/AnnalsATS.201404-145OC [DOI] [PubMed] [Google Scholar]
- 3.Kistler KD, Nalysnyk L, Rotella P, et al. Lung transplantation in idiopathic pulmonary fibrosis: a systematic review of the literature. BMC Pulm Med 2014;14:139. 10.1186/1471-2466-14-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raghu G, Chen SY, Yeh WS, et al. Idiopathic pulmonary fibrosis in US Medicare beneficiaries aged 65 years and older: incidence, prevalence, and survival, 2001-11. Lancet Respir Med 2014;2:566-72. 10.1016/S2213-2600(14)70101-8 [DOI] [PubMed] [Google Scholar]
- 5.Stern JB, Mal H, Groussard O, et al. Prognosis of patients with advanced idiopathic pulmonary fibrosis requiring mechanical ventilation for acute respiratory failure. Chest 2001;120:213-9. 10.1378/chest.120.1.213 [DOI] [PubMed] [Google Scholar]
- 6.Anzueto A, Frutos-Vivar F, Esteban A, et al. Incidence, risk factors and outcome of barotrauma in mechanically ventilated patients. Intensive Care Med 2004;30:612-9. 10.1007/s00134-004-2187-7 [DOI] [PubMed] [Google Scholar]
- 7.Monro-Somerville T, Sim M, Ruddy J, et al. The Effect of High-Flow Nasal Cannula Oxygen Therapy on Mortality and Intubation Rate in Acute Respiratory Failure: A Systematic Review and Meta-Analysis. Crit Care Med 2017;45:e449-56. 10.1097/CCM.0000000000002091 [DOI] [PubMed] [Google Scholar]
- 8.Kang BJ, Koh Y, Lim CM, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med 2015;41:623-32. 10.1007/s00134-015-3693-5 [DOI] [PubMed] [Google Scholar]
- 9.Mooney JJ, Raimundo K, Chang E, et al. Mechanical ventilation in idiopathic pulmonary fibrosis: a nationwide analysis of ventilator use, outcomes, and resource burden. BMC Pulm Med 2017;17:84. 10.1186/s12890-017-0426-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011;183:788-824. 10.1164/rccm.2009-040GL [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ley B, Ryerson CJ, Vittinghoff E, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med 2012;156:684-91. 10.7326/0003-4819-156-10-201205150-00004 [DOI] [PubMed] [Google Scholar]
- 12.du Bois RM, Weycker D, Albera C, et al. Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011;184:459-66. 10.1164/rccm.201011-1790OC [DOI] [PubMed] [Google Scholar]
- 13.Magill SS, Klompas M, Balk R, et al. Developing a new, national approach to surveillance for ventilator-associated events: executive summary. Chest 2013;144:1448-52. 10.1378/chest.13-1640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blivet S, Philit F, Sab JM, et al. Outcome of patients with idiopathic pulmonary fibrosis admitted to the ICU for respiratory failure. Chest 2001;120:209-12. 10.1378/chest.120.1.209 [DOI] [PubMed] [Google Scholar]
- 15.Delorme M, Bouchard PA, Simon M, et al. Effects of High-Flow Nasal Cannula on the Work of Breathing in Patients Recovering From Acute Respiratory Failure. Crit Care Med 2017;45:1981-8. 10.1097/CCM.0000000000002693 [DOI] [PubMed] [Google Scholar]
- 16.Peters SG, Holets SR, Gay PC. High-flow nasal cannula therapy in do-not-intubate patients with hypoxemic respiratory distress. Respir Care 2013;58:597-600. [DOI] [PubMed] [Google Scholar]
- 17.Weill D, Benden C, Corris PA, et al. A consensus document for the selection of lung transplant candidates: 2014--an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant 2015;34:1-15. 10.1016/j.healun.2014.06.014 [DOI] [PubMed] [Google Scholar]
- 18.Rajala K, Lehto JT, Saarinen M, et al. End-of-life care of patients with idiopathic pulmonary fibrosis. BMC Palliat Care 2016;15:85. 10.1186/s12904-016-0158-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mallick S. Outcome of patients with idiopathic pulmonary fibrosis (IPF) ventilated in intensive care unit. Respir Med 2008;102:1355-9. 10.1016/j.rmed.2008.06.003 [DOI] [PubMed] [Google Scholar]
- 20.Rush B, Berger L, Anthony Celi L. Access to Palliative Care for Patients Undergoing Mechanical Ventilation With Idiopathic Pulmonary Fibrosis in the United States. Am J Hosp Palliat Care 2018;35:492-6. 10.1177/1049909117713990 [DOI] [PubMed] [Google Scholar]