Abstract
Background
In urbanized, low-income cities with high rates of congestion, delivery of antiepileptic drugs (AEDs) by unmanned aerial vehicles (drones) to people with epilepsy for both emergency and non-urgent distribution may prove beneficial.
Methods
Conakry is the capital of the Republic of Guinea, a low-income sub-Saharan African country (2018 per capita gross national income US$830). We computed the number of drones and delivery times to distribute AEDs from a main urban hospital to 27 pre-identified gas stations, mosques and pharmacies and compared these to the delivery times of a personal vehicle.
Results
We predict that a single drone could serve all pre-identified delivery locations in Conakry within a 20.4-h period. In an emergency case of status epilepticus, 8, 20 and 24 of the 27 pre-identified destinations can be reached from the hub within 5, 10 and 15 min, respectively. Compared with the use of a personal vehicle, the response time for a drone is reduced by an average of 78.8% across all times of the day.
Conclusions
Drones can dramatically reduce the response time for both emergency and routine delivery of lifesaving medicines. We discuss the advantages and disadvantages of such a drone delivery model with relevance to epilepsy. However, the commissioning of a trial of drones for drug delivery in related diseases and geographies is justified.
Keywords: epilepsy, healthcare delivery, remote medicine, unmanned aerial vehicle
Introduction
In response to inadequacies in medical service response times, computational and practical studies have examined the use of unmanned aerial vehicles (UAVs), commonly known as drones, to deliver emergency medical supplies.1–3 These studies have focused on the delivery of automatic external defibrillators, blood, laboratory samples and vaccines,3 often in economically prosperous developed areas such as Canada or Sweden.2–4 Drones are currently in use in Rwanda to deliver emergency blood supplies to rural areas.5 In Malawi, Madagascar and Senegal, pioneer projects for bidirectional delivery of specimens and delivery of tuberculosis and lifesaving maternal health needs have been implemented.6 To our knowledge, no computational or feasibility studies focusing on drone delivery for the treatment of brain disorders have been completed for a lower-income country. Brain disorders have some similarities with the implemented studies but differ in their chronicity, stigma and that there are fewer skilled providers available in low-income settings.
We developed a computational model for the use of drones to deliver antiepileptic drugs (AEDs) via a hub-and-spoke system in Conakry, the capital of the Republic of Guinea. Conakry was chosen because of the confluence of poor urban planning, congestion of traffic and the high need for access to AEDs among people with epilepsy (PWE). In the Conakry-based hub-and-spoke model, the central hub is the Ignace Deen Hospital (IDH), a large, academic referral hospital located near the Atlantic Ocean and along one of the city’s major thoroughfares.
Materials and methods
Setting
The Republic of Guinea is an impoverished West African country that recently experienced an Ebola epidemic and ranks 175th of 189 countries on the United Nation’s Human Development Index.7 In 2018, Guinea had a per capita gross national income of US$830.8 Conakry, home to 1.8 million people, is the epicentre for many populous suburbs. The eastern and western edges of Conakry are connected by only three major arteries—including one highway, the N1—that are traversed by relatively few roads.9,10 Roads that cross the city are in a state of extreme disrepair, which impedes the speedy flow of emergency vehicles.9 Public transport is limited to buses, although motorcycles, vans and sedan taxis are popular.9 As of 2011, the most recently reported data available, there were approximately 34 000 registered passenger vehicles in Guinea.11
Evidence of need
Epilepsy is more common in lower-income settings and the prevalence of poorly controlled epilepsy is generally higher. Mortality from status epilepticus ranges from 10 to 27%.12 It is imperative to emergently stop prolonged seizures, which can be accomplished by laypeople through the administration of AEDs that are most often given sublingually and require minimal to no training to administer. PWE infrequently own a means of transportation and are unable to independently and safely operate vehicles, particularly when their seizures are frequent and generalized.
In a convenience sample of 296 PWE, based on our data from a free clinic at IDH collected prior to this computational study, 89 (30%) owned a bicycle, 106 (36%) owned a motorcycle and 139 (47%) owned a car. They spent approximately 20% of their personal income on transportation.8 Only half (n=162 [55%]) reported regularly using an AED. Of 165 children enrolled in this prior study, 112 (68%) had a seizure lasting >5 min at least once. Others in sub-Saharan Africa have reported rates of status epilepticus two to five times higher than in Western populations.13 Given the high levels of congestion in Conakry, we believe drones would be able to reach almost all cases prior to emergency medical services (EMS) arrival, with the exception of cases that occur adjacent to clinics or hospitals.
Locations
IDH was chosen as the storage and dissemination centre for both the UAVs and AEDs. Mosques, pharmacies and gas stations were chosen as spokes because they are attended most hours of the day, represent centres of socialization or commerce, are accessible to most citizens and are distributed relatively evenly in the city (Figure 1). We applied our model to a scenario of regular medication delivery of standard AEDs to prevent seizures as well as delivery of emergency AEDs if needed (i.e. benzodiazepines). In this model we assume that there will be trained responders at each delivery location that will be able to retrieve AEDs from the drone and administer the drugs directly to the patient. Upon drone landing, trained responders at each delivery location will approach the drone and retrieve the AEDs from the payload area of the drone. They will then return to the patient and directly administer the drugs to the patient. We aimed to determine the number of depots that could be served by one, two, three and four drones within an 8-, 12-, 24- and 40-h period.
Figure 1.

Location of proposed drone depots and central hub in Conakry, Guinea.
Drone specifications
The technical specifications were based on the current capabilities of drones and parameters in the literature on drone deliveries for medical purposes.4Table 1 lists commercially available drones as of November 2019 that fit the model’s specifications. Ascent and descent times were set to 10 s with simultaneous horizontal acceleration and deceleration,14,15 allowing drones to reach a cruising altitude of 60 m, which is within legal flying heights in Canada and the United States.4,16,17 The top speed was set at 27.8 m/s.18 Drones are assumed to be flown to destination sites by pilots stationed at the drone base location. There is a one-way delivery to the spokes. On-scene delivery time was assumed to be 3 min, serving as the upper limit for the time required for personnel at the delivery site to retrieve the payload. On-scene delivery of supplies requires landing on predetermined open areas such as roofs or clearings, similar to helipads. The precise location of these open areas is dependent on the characteristics of each delivery location. This model assumes that staff at each location are trained to respond to the arrival of drones, which includes ensuring that the landing site is clear, obtaining medication from the drone’s payload area and providing the necessary clearance to the drone operator for the drone to return to base. Post-delivery maintenance time, which would likely include recharging of batteries and servicing, was set at 30 min. Since we are comparing the means of transport for medications to reach a patient, we assume that non-travel response delays (i.e. delays in calls for help, delays in calls from dispatch) up to the arrival of medication at the delivery location are identical for drones vs traditional (EMS and regular) delivery of medicines.
Table 1.
Existing drone models (as of November 2019) that meet the criteria for the transport and delivery of antiepileptic drugs in Conakry, Republic of Guinea
| Model | Existing delivery applications |
|---|---|
| Winga | • Consumer products in the United States, Australia and Finland |
| • Courier packages in the United States | |
| Ziplineb | • Medical supplies in Rwanda and Ghana |
| Wingcopterc | • Medical supplies and laboratory samples in Tanzania |
| Matternet M2d | • Courier packages in the United States |
| • Medical supplies in Switzerland | |
| Workhorse Horseflye | • Consumer products in the United States |
| • Courier packages in the United States |
Costs
Drone costs vary greatly by size, speed and battery capacity.19 Prices range from US$150 to US$1500 for the highest-end commercial drones, which we employ in this model. Industrial drones, used in technical applications such as construction management, film making and mine operations, range from US$5000 to >US$30 000.20–22
Analyses and calculations
Several assumptions were made. First, that only one delivery of AEDs would be made per round trip. While multistop delivery routes can be computed, the drone technology to make such deliveries is cost prohibitive. Second, that drones would fly a straight-line path between the base hub and destination spokes, ignoring any terrain and weather constraints that may affect drone flight, such as wind speeds, ambient temperature, precipitation and other aircraft. Third, that travel time is identical to and from the spoke at all times of the day. Finally, that drones would not be subject to failures that would result in additional downtime.
The time required for a single round-trip delivery from IDH to each of 27 possible destinations across the three prespecified categories (gas stations, pharmacies, mosques) including the time for ascent, cruising, descent, on-scene time, return and maintenance was calculated.
We calculated the total time required to make all trips to each destination category as well as the total time for all trips across all three categories. We then performed a sensitivity analysis, repeating for varying amounts of on-scene and maintenance time and tailoring our parameters to specific commercially available drone models. We also determined the set of destinations that were within 5, 10 and 15 min of one-way travel time to identify which destinations would be suitable for drone-based response to an emergency call for status epilepticus. Data were collected in Excel spreadsheets (Microsoft, Redmond, WA, USA). Distances were computed using the Haversine formula.
Drone response times were compared with response times to each destination using a personal vehicle (cars, trucks and other street-bound vehicles) over three distinct time snapshots on a weekday (daytime: noon, evening: 8:00 p.m., overnight: 4:00 a.m.) to determine differences in response time between the modes of transport. Personal vehicle travel time estimates were obtained from Google Maps (maps.google.com).
The number of deliveries that could be made to each destination (categorized by location type as well as across all types) with varying fleet sizes (between one and four drones) across 8-, 12-, 24- and 40-h time periods was computed.
Results
Based on a 3-min on-scene time, a single drone would be able to serve all spoke locations in Conakry once in 20.41 h of operation. All mosques and gas station locations could be served once in 5.63 and 6.60 h, respectively, whereas all pharmacy locations could be served by a single drone in 8.18 h.
With a fleet size of four drones, we determined that every destination location could be served a minimum of seven times within a 40-h period. There can be up to 28 deliveries per 40-h period if only considering mosques as destinations. Table 2 shows the number of feasible deliveries to each destination category (as well as across all categories) given varying numbers of drones in the fleet.
Table 2.
Number of possible deliveries to all destinations of each location type with varying time horizons and fleet size
| Time period (hours) | Fleet size | Pharmacies only | Mosques only | Gas stations only | All location types |
|---|---|---|---|---|---|
| 8 | 1 drone | 0.98 | 1.42 | 1.21 | 0.39 |
| 2 drones | 1.96 | 2.84 | 2.42 | 0.78 | |
| 3 drones | 2.93 | 4.27 | 3.63 | 1.18 | |
| 4 drones | 3.91 | 5.69 | 4.85 | 1.57 | |
| 12 | 1 drone | 1.47 | 2.13 | 1.82 | 0.59 |
| 2 drones | 2.93 | 4.27 | 3.63 | 1.18 | |
| 3 drones | 4.40 | 6.40 | 5.45 | 1.76 | |
| 4 drones | 5.87 | 8.53 | 7.27 | 2.35 | |
| 24 | 1 drone | 2.93 | 4.27 | 3.63 | 1.18 |
| 2 drones | 5.87 | 8.53 | 7.27 | 2.35 | |
| 3 drones | 8.80 | 12.80 | 10.90 | 3.53 | |
| 4 drones | 11.73 | 17.07 | 14.54 | 4.70 | |
| 40 | 1 drone | 4.89 | 7.11 | 6.06 | 1.96 |
| 2 drones | 9.78 | 14.22 | 12.12 | 3.92 | |
| 3 drones | 14.67 | 21.33 | 18.17 | 5.88 | |
| 4 drones | 19.56 | 28.44 | 24.23 | 7.84 |
In comparing response times across modes of transport, drones would be able to reduce response times by an average of 78.8% across all times of the day, ranging from a 75.1% reduction overnight to 82.3% during the evening. A drone network would reduce the median response time from 35–46 min via a personal vehicle to 7.5 min and reduce the 90th percentile response time from 53–80 min to 14.7 min (Figure 2).
Figure 2.
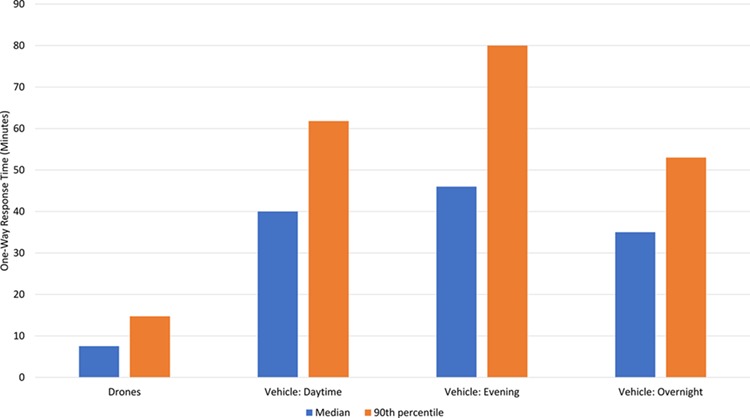
Response times via drone vs personal vehicle at different times of day.
In response to potential cases of status epilepticus, it is possible to reach 24 of 27 depot locations within 15 min of launch from the central hub and 20 of 27 within 10 min of launch (Table 3). In contrast, personal vehicles would only be able to reach 3–5 of 27 locations within 15 min of dispatch from the central hub and 1–2 locations within 10 min.
Table 3.
Emergency response times to medicine depots for a drone launched from Ignace Deen Hospital
| Location | Latitude | Longitude | Type | Arrive in 5 min. | Arrive in 10 min. | Arrive in 15 min. |
|---|---|---|---|---|---|---|
| Ignace Deen Hospital | 9.50694 | −13.70484 | Base | NA | NA | NA |
| Pharmacie Nouni | 9.59855 | −13.65337 | Pharmacy | No | Yes | Yes |
| Pharmacie Cimenterie | 9.68145 | −13.53357 | Pharmacy | No | No | No |
| Pharmacie Centrale de Guinee | 9.54602 | −13.67134 | Pharmacy | Yes | Yes | Yes |
| Pharmacie Garaya | 9.60846 | −13.61381 | Pharmacy | No | Yes | Yes |
| Manize Kolie | 9.54918 | −13.67462 | Pharmacy | Yes | Yes | Yes |
| Pharmacie Manque Pas | 9.50891 | −13.71105 | Pharmacy | Yes | Yes | Yes |
| Pharma+ | 9.63925 | −13.61647 | Pharmacy | No | No | Yes |
| Pharmacie Mbambe | 9.61681 | −13.60823 | Pharmacy | No | No | Yes |
| Pharmacie Wassalla Yimbabou | 9.5941 | −13.61971 | Pharmacy | No | Yes | Yes |
| BISS Pharmacie | 9.61291 | −13.61301 | Pharmacy | No | Yes | Yes |
| Grande Mosquée de Conakry | 9.53337 | −13.68439 | Mosque | Yes | Yes | Yes |
| Dixinn Mosquée | 9.54985 | −13.67062 | Mosque | Yes | Yes | Yes |
| Mosquée Kenien Rails | 9.55487 | −13.65524 | Mosque | Yes | Yes | Yes |
| Grande Mosquée du Cite de Francony | 9.55541 | −13.64036 | Mosque | No | Yes | Yes |
| Mosquée Petit Simbaya 3 | 9.61989 | −13.61955 | Mosque | No | Yes | Yes |
| Mosquée de Kobaya | 9.65246 | −13.59853 | Mosque | No | No | Yes |
| Mosquée de Foula Madina | 9.67372 | −13.57975 | Mosque | No | No | Yes |
| Station Total | 9.6084 | −13.6483 | Gas station | No | Yes | Yes |
| Station Shell | 9.68414 | −13.51386 | Gas station | No | No | No |
| Station Shell | 9.5283 | −13.68307 | Gas station | Yes | Yes | Yes |
| Station Shell | 9.58634 | −13.65822 | Gas station | No | Yes | Yes |
| Gas Station Shell | 9.58285 | −13.62703 | Gas station | No | Yes | Yes |
| Station Shell | 9.67169 | −13.55409 | Gas station | No | No | No |
| Station Total | 9.57745 | −13.65327 | Gas station | No | Yes | Yes |
| Station Total Coléah Domino | 9.53454 | −13.6784 | Gas station | Yes | Yes | Yes |
NA: not applicable.
Discussion
Drone delivery could be used to distribute AEDs, both to treat chronic, poorly controlled epilepsy and to respond to emergent situations. A relatively small drone fleet (n=4) would be able to adequately service a well-dispersed series of 27 spokes throughout Conakry from the central hospital hub. A significant reduction in response times compared with personal vehicles is apparent. Even in the emergency case of status epilepticus, we demonstrate that a drone would be able to quickly reach most destinations.
Several key factors would need to be considered to ensure full operation of our proposed drone delivery system in Conakry. First, education and appropriate training of personnel would be required. Pilots and/or service staff at the hub would need instruction to ensure proper maintenance of the drones, including servicing and replacement of parts, as well as monitoring in-flight performance and responding accordingly to unexpected events such as equipment failures or collisions.
Lay staff at each spoke destination would require training on how to make orders for AEDs, especially in the event of unscheduled orders for status epilepticus; maintain safe landing zones for drones; provide necessary clearances for drone departure and obtain and administer AEDs from a drone upon arrival. Engagement of community leaders and development of centralized protocols are necessary, especially in a country with few practicing neurologists.
Second, public awareness campaigns would need to be considered so that residents are aware of drones flying overhead, reducing the risk of unintentional or intentional damage to the vehicles.
Third, regulatory constraints would need to be addressed. Low-income countries are well poised to ‘leapfrog’ over wealthier countries because of the lack of competition from old technologies and systems. Currently Guinea has no legislation on the operation of commercially operated drones.22 Other countries that do, such as Canada and the United States, require special flight operations certificates in order to fly drones out of a visual line of sight, which would be required for deliveries to destinations that are beyond the horizon, and also require human supervision of all flights at all times,23 which would result in greater staffing requirements and accordingly higher costs of operation. Although Guinea currently has no regulations on drone use, this should not be a deterrent to the implementation of drone-delivered medicines in the country. Rather, successful implementation will require cooperation with government entities to establish standard operating guidelines and legislation, as has already been done in other African countries. Rwanda, Tanzania, and Ghana already have remotely operated drone delivery systems in place.
Other more pragmatic issues must also be considered before implementation of our model. The most obvious of these issues includes payment and costing of such a model of drone delivery for an economically disadvantaged patient group. It is possible that such a delivery system is cost effective given the heavy burden of seizures and status epilepticus on PWE throughout their lives. Education of healthcare workers and laypeople also requires some form of funding, even if donated by experts and supported by philanthropy, since the human resources require capacity building. However, education will have many benefits to PWE beyond the use of drones and may save lives, reduce stigma and enhance access to skilled care.
Another issue may be the use of controlled substances, such as benzodiazepines, which are extremely effective for stopping seizures but may lead to addiction, overdose and other forms of misuse. In this setting, the careful logging and entry of distributed medications and their doses would be a best practice. In Guinea, benzodiazepines are not controlled or scheduled and can be bought directly by patients, therefore our model remains feasible.
Recently a study of the impact of drone transportation on the quality of medicines was reported in the case of insulin.24 The authors recommended five tests be performed for implementation of a drone model: safe flight time and range, quality of medicines post-flight, on-board conditions experienced by the medicine, security of the drone supply chain and the effect of drone failure on both the medicine and environment. The same could be used for AEDs. Diazepam is the benzodiazepine that is usually available in Guinea. According to its package insert, the storage temperature of diazepam has an acceptable range of 15–30°C and it should be delivered in tight, light-resistant materials.25 Pre-hospital storage of diazepam must be replaced depending on its storage temperature, although this has been studied best in the intravenous formulation of the drug.26
Other pathways forward, which we did not explore in detail here, could easily include a combined approach with other non-communicable disease medications, including cardiac medications, insulin and medications for other brain disorders. In such a model, the recipients at the spokes may require more skills and diagnostic information than would be necessary for a generalized tonic clonic seizure in a patient with known epilepsy.
We believe the drone model, with government and community buy-in, is implementable in poor, highly urbanized cities. Our modelling exercise has implications across disease states and geographies. It serves as a predictive study for the amount of influence a currently available off-the-shelf technology could have for patients with an undertreated disorder. The computations here support the commissioning and trialling of a drone network in Conakry and similar locations. Such a cutting-edge health delivery system could also improve public awareness and engagement in the management and destigmatization of epilepsy.
Acknowledgements
None.
Authors’ contributions
FJM conceived the study. FJM, KHBL, ACV, AFC and TCYC implemented the study. ACV performed data collection on drone specifications and spoke locations in Guinea. FJM, KHBL and TCYC analysed and interpreted data on drone flights and response times. FJM and ACV drafted the manuscript. FJM, KHBL, ACV, AFC and TCYC revised the manuscript for intellectual content. All authors read and approved the final manuscript. FJM and ACV are the guarantors of the paper.
Funding
This work was not specifically funded. The Guinea Epilepsy Project is funded by the National Institutes of Health (R21NS098886) and Fondation Pierre Fabre.
Competing interests
None declared.
Ethical approval
Not required.
References
- 1. Baehr A. Optimizing a drone network to deliver automated external defibrillators. J Emerg Med. 2017;53(3):445–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Claesson A, Bäckman A, Ringh M et al. Time to delivery of an automated external defibrillator using a drone for simulated out-of-hospital cardiac arrests vs emergency medical services. JAMA. 2017;317(22):2332–2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rosser JC, Vignesh V, Terwilliger BA et al. Surgical and medical applications of drones: a comprehensive review. JSLS. 2018;22(3):e2018.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boutilier JJ, Brooks SC, Janmohamed A et al. Optimizing a drone network to deliver automated external defibrillators. Circulation. 2017;135(25):2454–2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Baker A. The American drones saving lives in Rwanda. Time Available from: https://time.com/rwanda-drones-zipline/ (accessed 18 October 2019).
- 6. Knobluach AM, Rosa S, Sherman J et al. Bi-directional drones to strengthen healthcare provision: Experiences and lessons from Madagascar, Malawi, and Senegal. BMJ Glob Health. 2019;4(4):e001541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. United Nations Development Programme. Human development data (1990–2018). Available from: http://hdr.undp.org/en/data (accessed 18 October 2019).
- 8. World Bank. GNI per capita , Atlas method (current US$) – Guinea. Available from: https://data.worldbank.org/indicator/NY.GNP.PCAP.CD?locations=GN (accessed 18 October 2019).
- 9. Sub-Saharan Africa Transport Policy Program Poverty and urban mobility in Conakry. Report 09/04/CKR. Available from: https://www.ssatp.org/sites/ssatp/files/publications/PapersNotes/Conakry_en.pdf (accessed 18 October 2019).
- 10. Atlassian. 2.3 Guinea Road Network Available from: https://dlca.logcluster.org/display/public/DLCA/2.3+Guinea+Road+Network (accessed 18 October 2019).
- 11. World Health Organization. Global Health Observatory data repository. Registered vehicles data by country Available from: http://apps.who.int/gho/data/node.main.A995?lang=en (accessed 1 July 2019).
- 12. Claassen J, Goldstein JN. Emergency neurological life support: status epilepticus. Neurocrit Care. 2017;27(Suppl 1):152–158. [DOI] [PubMed] [Google Scholar]
- 13. Newton CR, Kariuki SM. Status epilepticus in sub-Saharan Africa: new findings. Epilepsia. 2013;54(Suppl 6):50–53. [DOI] [PubMed] [Google Scholar]
- 14. Schollig A, Hehn M, Lupashin S et al. Feasibility of motion primitives for choreographed quadrocopter flight. In: Proceedings of the 2011 American Control Conference. New York: IEEE; 2011;3843–3849. [Google Scholar]
- 15. Kumar V, Michael N. Opportunities and challenges with autonomous micro aerial vehicles. Int J Rob Res. 2012;31(11):1279–1291. [Google Scholar]
- 16. Transport Canada Flying your drone safely and legally. Available from: https://www.tc.gc.ca/en/services/aviation/drone-safety/flying-drone-safely-legally.html (accessed 18 October 2019).
- 17. Federal Aviation Administration Fact sheet – small unmanned aircraft regulations (part 107). Available from: https://www.faa.gov/news/fact_sheets/news_story.cfm?newsId=22615 (accessed 18 October 2019).
- 17. Delft University of Technology TU Delft’s ambulance drone drastically increases chances of survival of cardiac arrest patients. Available from: https://www.tudelft.nl/en/2014/tu-delft/tu-delfts-ambulance-drone-drastically-increases-chances-of-survival-of-cardiac-arrest-patients/.
- 18. Sørensen LY, Jacobsen LT, Hansen JP. Low cost and flexible UAV deployment of sensors. Sensors (Basel) 2017;17(1):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Freefly Systems. Freefly ALTA 8 Available from: https://store.freeflysystems.com/products/freefly-alta8 .
- 20. QUESTUAV. Factory Built DATAhawk II Complete UAS Available from: https://shop.questuav.com/product/factory-built-datahawk-ii-complete-uas/.
- 21. B&H Photo. xFold rigs Dragon X12 U11 Drone with 3-axis gimbal for DSLR/cinema cameras (RTF) Available from: https://www.bhphotovideo.com/c/product/1239699-REG/xfold_rigs_dragon_12urtf_dragon_x12_u11_drone.html (accessed 18 October 2019).
- 22. Technical Centre for Agricultural and Rural Cooperation Drone governance: a scan of policies, laws and regulations governing the use of unmanned aerial vehicles (UAVs) in 79 ACP countries. CTA Working Paper 16/12. Wageningen, The Netherlands: Technical Centre for Agricultural and Rural Cooperation; 2016.
- 23. Jones T. International commercial drone regulation and drone delivery services. RR-1718/3-RC. Santa Monica, CA: RAND; 2017.
- 24. Hii MSY, Courtney P, Royall PG. An evaluation of the delivery of medicines using drones. Drones. 2019;3(3):52. [Google Scholar]
- 25. Roche. Product description. Valium brand of diazepam tablets . Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/013263s094lbl.pdf (accessed 18 October 2019).
- 26. Gottwald MD, Akers LC, Liu PK et al. Prehospital stability of diazepam and lorazepam. Am J Emerg Med. 1999;17(4):333–337. [DOI] [PubMed] [Google Scholar]


