Abstract
Objective: The study aims to describe the experiences of older persons in seeking health care in a private hospital in urban India. Methods: Semi-structured interviews were conducted with 50 older persons admitted in or visiting a private hospital in Hyderabad city in India between the period November 2017 and April 2018. The data were analyzed using Content Analysis. Results: Dimensions related to payment mechanisms, quality of health care staff, and hospital quality were reported to be important for the older persons. Payment mechanisms were related to discounts, insurance support, and reducing out-of-pocket expenditure. Quality of care was related to optimizing hospital operational processes like discharge time, standard of treatment, and trustworthiness of the medical staff. Discussion: Payment mechanism can be made friendly for the older persons. Quality of hospital including its staff can be enhanced by developing geriatric-specific competencies which can help them to understand and treat complex health problems specific for the older population.
Keywords: health-care-seeking behavior, older persons, payment mechanism, hospital quality, staff quality
Introduction
Demographics of Aging in India
The number of older persons in the world has increased in the recent years, and the growth is projected to accelerate in the coming decades. There were 901 million people aged 60 years or above in 2015, an increase of 48% over the 607 million older persons globally in 2000. By 2030, the number of people in the world aged 60 years or above is projected to grow by 56%, to 1.4 billion, and by 2050, the global population of older persons is projected to more than double its size in 2015, reaching nearly 2.1 billion (United Nations, 2017).
According to Population Census in 2011, there are nearly 104 million older persons in India with approximately equal distribution between men and women. The older population has increased from 5.6% of the total population in 1961 to 8.6% in 2011. It is projected to rise to 12.4% (173 million) of the total population by 2026 and 20% (350 million) by 2050 (Central Statistics Office, 2011; Subaiya & Bansod, 2014).
Common Health Problems of the Older Persons
Older persons suffer from physical and mental problems and acute and chronic diseases with different manifestations. They have a range of noncommunicable diseases like diabetes, hypertension, heart disease, cholesterol disorders, stroke, osteoarthritis, osteoporosis, dementia, cancer, gait disorders/falls, hearing loss, urinary incontinence, depression, delirium, and vision problems like cataract (Cybulski et al., 2016; Salagre, 2013; Thakur et al., 2013).
The Status of Elderly report 2014 by Helpage India mentions body pain (55%), eye-related problems (50%), hypertension (32%) followed by Asthma (25%), Arthritis (22%), and diabetes (19%) as the most prevalent diseases in the older population in India (Khurana et al., 2015).
Downstream and Upstream Factors Influencing Seeking Health Care by Older People
A systematic review found that health-care-seeking behavior of rural older women in low-, middle-, and high-income countries was influenced by downstream factors such as health literacy and education, passive health-care-seeking behavior, and lack of health care support (Hamiduzzaman et al., 2017). The reported upstream factors were financial constraints, transportation difficulties, relationship matters, and a culture of restriction. A study done in Jamaica concluded that older men have poor health-seeking behavior due to low health literacy (Bourne, 2010).
Research shows that there are financial determinants in seeking health-care-like sources of income after retirement, pension to support themselves, and look after their health care, shelter, and nutritional requirements. Physical and mental stress arising out of illness, isolation, and coping mechanisms affect health-care-seeking behavior (Shrivastava et al., 2013).
Financial Considerations
Health-care-seeking practice of older persons is influenced by the socioeconomic capacity of the individual. The socioeconomic factors of the older population in rural Bangladesh determine health care seeking over age, gender, health care expenditure, and type of diseases they suffer (Ahmed et al., 2005). Getting older, poor socioeconomic status, and poor access to health care in Kenya contributed to poor health care seeking in the older people (Waweru et al., 2003). Financial constraints impacted health care seeking in urban poor older community in Pakistan (Ladha et al., 2009). Similarly, in an urban community in Nepal, the health care seeking by older persons was based on the economic status of the family and cost of treatment (D. Adhikari & Rijal, 2010). Socioeconomic status, health expenditure, and perception of the severity of the disease were important determinants for health-seeking behavior over-riding age, gender, and ethnicity in a study done in the outpatient department of a public hospital in Karachi (Habibullah & Afsar, 2013).
Health care Facilities and Providers
Health care seeking is influenced by the availability of the health care facilities and health care providers.
Seeking health care by older persons is reported to depend upon access, type, cost of, and relationship with the health care providers (Biswas et al., 2006). Even the form of payment accepted by the health care providers, flexibility in terms of payment, and the different forms of medicine followed are influencing factors. The type of practitioners, whether allopathic or traditional, was contributory factors in seeking health care (Ahmed, 2005). A community-based study in an urban area in India concluded that half the older persons preferred allopathy and one-fifth of them chose self-medication. The health-seeking behavior of the older persons was influenced by age, level of education, and poverty (Patle & Khakse, 2015). A study has concluded that factors like early age between 60 and 65 years, formal education, family support during illness, knowledge when to visit health facility, and accessibility to health facility were predictors of health-care-seeking behaviors of older persons in Southern Ethiopia (Falaha et al., 2016). Availability of equipment and drugs, services, distance to the facility, type of the facility, and perception of health care services influenced health care seeking among the older persons in Nairobi (Judy et al., 2015).
The general adult population (aged 18–59 years) seeks care for their health problems in various health care facilities. There are hospitals which are specialized for children, women, and adults and cater to various specialties like neurology, pediatrics, orthopedics, and cardiology. The older population defined here as a population aged 60 years and older also seek health care as a part of the general population and have to see the same set of health care providers and access the same set of health care resources in the hospital (Verma & Khanna, 2013).
This can be compared to a children’s hospital where children access health care providers like a pediatrician and super-specialists based on their needs and there is a separate workflow for them. Similarly, there is a need to have a separate subsystem within the hospital system to segregate the older persons from the so-called adult population, which can range from above 18 years to as much as 100 years and above (P. Adhikari, 2017).
The need arises not only from the increasing population of the older persons but also from the different manifestation of the diseases they face and the need to address their issues in a focused manner. A simple fever in the older person can be a serious issue for them as the body immunity is lower and it can lead to more complications as compared to a normal adult male or female. Clubbing the younger adult population with the older persons and providing them with the same service will not help the older persons and the hospital in the long run (Tripathy, 2014).
Therefore, there was a need to delve deeper into the needs of the older persons and understand their health-care-seeking experiences. A micro-, meso-, and macro-level approach to the care of the older persons could make it friendlier and synergize the same with existing health care services. A study mentioned that special outpatient departments in the hospital can ease access for the older persons (de Carvalho et al., 2017; Jain et al., 2016).
Research Objective
The objective of the study is to describe the experiences of older persons in seeking health care in a private hospital in urban India. Specifically, experiences of reaching the hospital, interaction with health care providers and customer services at the hospital, and follow-up after leaving the hospital were explored.
Method
Setting
The study was conducted in a private hospital in the city of Hyderabad, India which lies in the State of Telangana. The location was selected as the city is a major health care hub with a wide range of private and public health care providers in India. Hyderabad has 50 government hospitals including 5,749 beds, 4,000 clinics and nursing homes, 500 diagnostic centers, and 165 private hospitals providing a total of 12,000 beds catering to the population of around 7 million in the city. Rapid urbanization in the city has led to exponential growth in private health care due to accessibility, reduced waiting time, and better quality of care (Healthcare Scenario of Hyderabad, n.d.). The private hospital was chosen as it is one of the major hospitals in the city and had started a geriatric care center which is the focus area in this study.
Sampling
Using purposive sampling, 50 older persons visiting the geriatric care outpatient and inpatient care departments of the hospital were interviewed. The purposive sampling was done by following the list shared by the nursing team for the day for the inpatients admitted to the Inpatient wards. The list had patients of all age groups. The list was followed from the top to the bottom to identify the patients who were 60 years and above. Of the selected patients, those who gave their informed consent were interviewed. They were older persons suffering from common identified diseases namely diabetes, hypertension/cardiac problems, joint disorders, and respiratory disorders. They were new inpatients and inpatients who returned to the hospital for their follow-up or a re-admission or after discharge. Those who had severe depression, were emotionally disturbed, or suffered from end-stage diseases were excluded from the study. The study was conducted with qualitative research methods using content analysis. Content analysis is described as a method to classify written or oral materials into identified categories of similar meanings (Elo & Kyngäs, 2008).
Data Collection
The data were collected with the help of an interview guide and the interviews were recorded using a recorder. The interviews in English and Hindi lasted around 30 to 45 min each and were conducted in the hospital in the inpatient and outpatient departments. The study period was between November 2017 and April 2018. Data collection was stopped when data saturation was reached.
The topics covered during the interviews of the older persons explored their experiences before reaching the hospital and the logistical challenges in reaching the hospital. It also focused on the interaction in the hospital with various service delivery points like doctors and medical teams and the various services such as lab testing, operational processes, and discharge. It also looked at operational processes of billing and customer care. The questions also enquired about the kind of financial and family support they received during their health-care-seeking journey.
Data Analysis
The data were analyzed using content analysis (Elo & Kyngäs, 2008). The interviews were transcribed verbatim. The transcripts were read thoroughly, and parts or sentences of the transcripts were extracted for which codes were assigned. Similar codes were grouped under 19 sub-categories which were then grouped under seven generic categories. The generic categories were further grouped together to form the three main categories.
Results
The following main categories were identified through the analysis of the data:
Payment mechanisms for health care services by older persons.
Hospital quality.
Staff quality.
Payment Mechanisms for Health care Services by the Older Persons
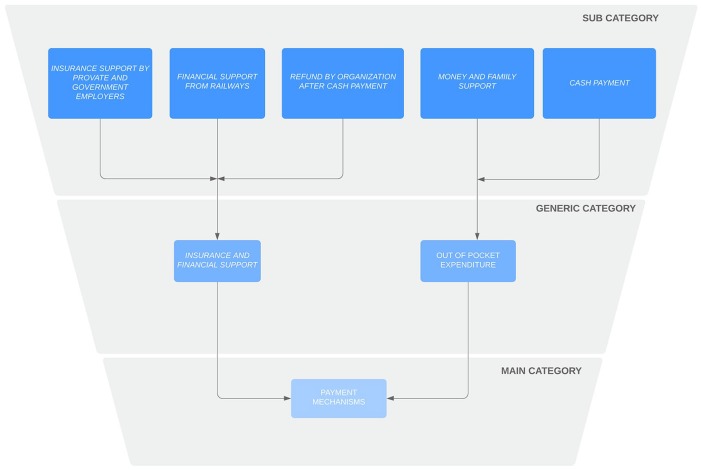
This main category addressed the way older persons paid for their treatment at the hospital during various stages. They used insurance, used family support, and made cash payments for their treatment alone or in combination (Figure 1). The older persons had to manage their expenses in the hospital based on factors like diagnosis and duration of stay, insurance provisions, and out-of-pocket expenditure. Payment mechanisms were mentioned to be important as this helped them access care in the hospital and continue or discontinue their care in the hospital based on their financial status.
Figure 1.
Payment mechanisms.
Insurance support
Older persons paid for the treatment through insurance support from their former employers or through private insurance taken. The employers were government or private organizations where they had worked for a number of years. A couple of older persons said that they got reimbursed for their treatment through the insurance done by the railways as they were former employees of the railways. A majority of them got support from their companies where they have worked for paying the money through insurance. They directly got reimbursed by their employers through their network tie up with the hospitals and insurance. They reported it as an important source of support for their payments:
Money, I don’t have problem since I have insurance. Everybody cannot access hospital as it is expensive. Since we worked and have insurance, we can access the hospital. I worked for 40 years. (65 years, man)
In a few cases, they had to pay the cash first and get reimbursed later from the insurance firm. They found the treatment to be expensive and needed insurance support or a discount in the treatment. One of the older persons who had taken his own private insurance said that there was need for monetary support for the older people from the government. The coverage provided by private insurance needed to be complemented with a discount from the hospital and government support. This would help them in seeking health care and provide financial support. There was a need to have adequate insurance for the older people as they faced health issues to a great extent:
I am paying Rs. 6000 yearly to United India Insurance and have a 4-lakh limit. Government should help. Hospitals also should give a discount. They can extend some more help for the older people in monetary terms. If I exceed 4 lakhs, it becomes a problem. (75 years, man)
As all older persons have health issues, they should have insurance private or government. Hospitals can charge based on financial position. They should not deny treatment for first time in emergency. (73 years, man)
There was also a need to continue the health insurance services for older persons in the cashless format as it facilitates health care seeking. There was payment done in cash before, and then, the family had to wait for a period to get the amount reimbursed which added to the financial burden in times of distress:
My husband is a government employee and we have EHS (Employee Health Scheme). Earlier we could use EHS for chemotherapy. Now they are not accepting at the hospital. We are paying and later getting reimbursed. I would suggest if we could remove the EHS problem. (65 years, woman)
Family support and out-of-pocket expenditure for payments
Some older persons were supported by their families who paid through their pockets and made cash payments but did not have insurance or company support to reimburse their payments. They had not taken any insurance on their own to cushion the expenses. An older woman mentioned that she got financial and physical support from her children. She said that there should be grading of financial charges for older persons by age and that would help the older individual in paying for their care more easily. Higher the age lesser should be the charges as the financial independence or sustainability decreases as one grows older. One of the older persons equated the money paid and health outcomes and said that every penny was worth it if paid in cash if they felt better at the end of the treatment. In absence of a regular source of income, family support physically and financially was of great support to the older persons in paying for the services. Family and support from relatives were mentioned to be a big source of support for the older persons so that they were not left alone to fend for themselves in their times of need:
Since I am a pension holder my son is a big support for me as a large sum of amount is difficult to procure. So, we are afraid of sickness. I think grading of financial charges as per age needs to be done. (61 years, woman)
An older person’s family was ready to spend money as they were traveling from a considerably distant geographic area. They were ready to pay as a family and expected good outcomes for the patient.
A person who was admitted for a kidney problem said,
“Money goes ok, outcome should be patient safety.” (Old man)
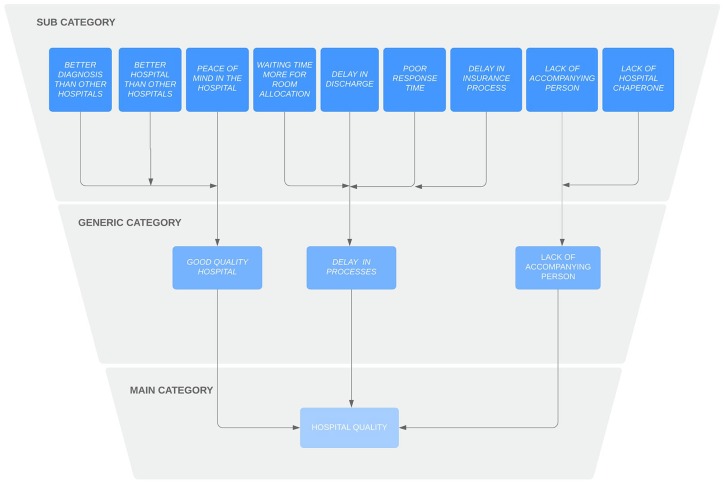
Hospital Quality
Hospital Quality was a main category which was identified as a factor in seeking health care by the older persons (Figure 2).
Figure 2.
Hospital quality.
Clinical outcomes/quality
This generic category focused on the quality of the hospital. The older persons had sought health care at various hospitals and had come to the hospital to get relief and good treatment after not getting proper diagnosis elsewhere. The patients mentioned that they came to the hospital as they expected to get the best diagnosis. They said that it was better than most of the hospitals in the city. The older persons said that they did not get good quality diagnosis in their own areas of residence and the clinical quality of the hospital was not up to the mark:
I think we have come here as we get the best diagnosis at the hospital and things get resolved. We have suffered a lot of misdiagnosis in our country. (69 years, man)
One of the patients mentioned that they sought health care at the particular hospital as it was 90% better than other hospitals. One person mentioned that he got peace of mind once they came to the hospital. Another older patient felt comfortable in the hospital. The older person made the decision to visit the hospital expecting a good clinical outcome after treatment:
It is 90% better than other hospitals. Here they want to treat the patient and not for money’s sake. (73 years, man)
We are lucky that we are in Hyderabad and we have the Hospital here. I am comfortable and all in respects it is comfortable. (84 years, man)
Hospital operations
This generic category encompassed the experiences of the various processes during different stages of seeking health care by the older persons. These centered around delay in operational processes and facilities like room allocation and room sharing with loss of privacy. There was a significant delay in processes like discharge and admissions which caused distress to the patients and their families:
The only thing is that discharge takes a lot of time, wait and wait and run around for the discharge process. It takes one day, and nobody bothers. (65 years, man)
One of the respondents said that the waiting time for room allocation was high. Another experienced a delay in the insurance authorization process. The emergency services were slow and patients had to wait. Sometimes the housekeeping and nursing staff attending the patients in the inpatient wards did not respond quickly leading to irritation for the patient and the family members. There was a delay in the discharge process and in the response time:
The emergency physicians make too much of delay. One or one and half hours. We come from far away/ we will have to wait for some time. There is a pre-authorization for insurance. There is too much delay. They take more than one and half hour. After that getting a room is also too much. Shifting will also take too much time. The Housekeeping staff is not punctual. (62 years, man)
Lack of accompanying person
This category described additional facilities which could improve the experience of the older patients while seeking health care. There was a need for people to accompany the older persons to the hospital:
We saw in Australia that a person comes to the older person’s place and arranges to take them to the hospital. Here we have to make our own arrangements. If my son is not here who will take care of us? We have to call a taxi or something. Who will do it for us? That much time should be there. (67 years, man)
An older woman who had come from the North East of India mentioned the need of a guide or a chaperone within the hospital to assist the older persons. These facilities for the older persons could help them navigate the hospital and make it more convenient:
There should be a guide for outsiders who could help us around in the hospital as I had to spend some time trying to find out my way. Sometimes we get lost. There is a need for guidance as we are not from this place. Somebody to guide around to go around counter to counter. (73 years, woman)
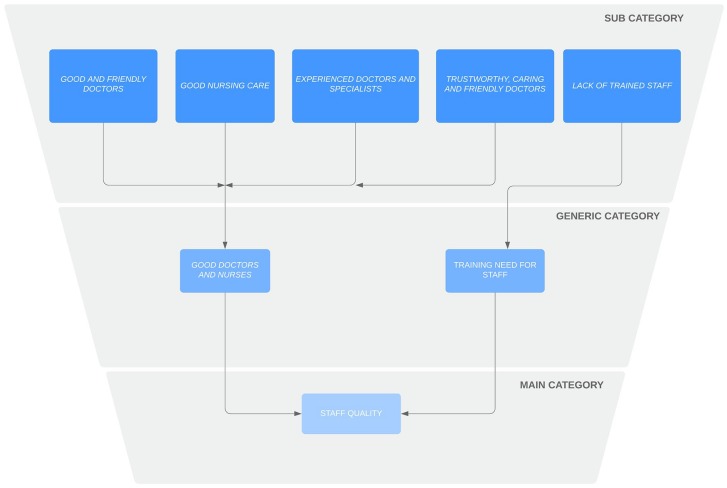
Quality of Staff
Quality of staff at the hospital was identified as one of the main categories when the older persons shared their experience of seeking health care (Figure 3).
Figure 3.
Staff quality.
Good doctors and nurses
This generic category describes about the quality of doctors and nurses in the hospital. A lot of older persons spoke about the quality of health care providers which included doctors and nurses in the hospital. They were happy with the doctors and the nurses and the treatment provided:
The medical and doctor part is very good at the hospital. Doctors are fantastic here in the hospital. Half my illness goes away with them. (woman)
The doctors and nurses had good skills, were courteous, were available for treating the older patients, and were able to communicate the problem, treatment regimen, and the costs in a better manner than other hospitals in the city. The treatment given by them was good, exceptional, and prompt in their words. This had helped the recover quickly from their health problems under their care. The doctor’s presence also helped in reducing their illness even before the treatment started, and fear and anxiety disappeared and underlined the mental comfort the doctors brought to the patients:
I have a good experience and doctors give good treatment. The people are very prompt. The care is exceptional here. It is very prompt. All treatment and costs are explained well. (60 years, woman)
I got perfect treatment here. I am being treated by Drs.—. Dr—.is looking after kidney and following up on creatinine. I had high fever and had a shrinkage of kidney and got good treatment at the hospital. As soon as we enter hospital, we feel less scared and all our tension dissolves. All our good treatment has happened here. (65 years, woman)
A respondent said that the specialist care delivered was very good and the hospital had a good panel of specialists available. They did not need to keep searching for specialist care in the hospital and a team helped address the disease in a better manner compared to other hospitals in the city. The interviewed older patients mentioned that the doctors at the specific hospital were better compared to those outside. They mentioned that the best doctors in the country were available here and they treated their entire families over a long time building a strong bond and hence they had come back to them. They mentioned about trust and care as the key factors for seeking health care at the hospital:
The positive thing about the hospital is that we don’t need to tell them about the problem. As soon as we tell them they say that they will get a specialist doctor for you. We don’t have to run around. They have a good bunch of doctors who are specialized. If they have a problem, they call the specialist. We trusted only the doctor as he is experienced and nice. We are here only because of him. (75 years, man)
Based on my experience, it is the best hospital. I have not gone to many hospitals, but it is best, serving people, doctors come on time and examine the patient and give importance to medicine. They keep coming and asking whether there is improvement or not and what else does the patent wants. (84 years, man)
Lack of trained staff
Lack of trained staff was mentioned by some of the respondents. There was a need for proper training for the nursing staff and to improve their skills in procedures like cannulation. They mentioned that they overlooked this and mainly came for the doctors and the care provided by him or her:
Staff is not much qualified and trained. Yesterday the nurses were putting a cannula and there was bleeding. One drop of blood matters a lot for dialysis patient. They won’t understand. They are pricking twice or thrice. They used to block the vein. Very difficult to get the veins. Because of doctor we are adjusting to the difficulties. (62 years, man)
Discussion
This study aimed to describe the experiences of older persons seeking health care at a hospital in urban India. According to the respondents, paying capacity and mode of payment, good doctors, nurses, and hospital quality were important factors while seeking care at the hospital.
One of the main findings of the study was the use of employer-supported insurance as a paying mechanism for the medical costs of the older patients. The insurance supported payments during the hospital stay, but there is also a need to support care after discharge and long-term medical care. Payment mechanisms such as out-of-pocket expenditure, insurance coverage, and support from family and friends are important considerations for older persons. This happens at various stages of illness as indicated by the health-seeking behavior model by Igun (1979). Such consideration is also necessary during the treatment stage as the older patient might need to reassess the costs of the treatment as the disease course is long (Dey et al., 2012).
The older patients in the current study were able to pay for their care through cash and with support from their children and relatives in a few cases. The cash payments were necessary as they did not have insurance, or their insurance schemes required them to first pay in cash and get the amount reimbursed later. Those older persons who had insurance coverage due to their previous employment at government or private organizations could claim the insurance and mentioned that their payment process was much easier and it removed much of the financial burden over their families. The insurance support helped them in reimbursing for the health care costs at the hospital.
A report on Aging in Asia (Dey et al., 2012) highlights the challenges of financial protection in India where the out-of-pocket expenditure is 100 Rupees for every 125 Rupees per capita expenditure on health. There is increase in spending on health care by 1.5 times more for individuals above 65 years compared to those between 60 and 64 years, and there is a chance that those who are insured also fall under poverty from the catastrophic spending. In India, there is low insurance penetration and insurance premiums can be paid only by those in formal employment in public and private organizations. Thus, a large section of population and older persons who are financially vulnerable do not get coverage under the insurance system of the country which is fragmented and underserved. Research from Japan and South Korea reports that their insurance systems cover the costs related to medical care and long-term care of older persons (Akiyama et al., 2018; Jeon & Kwon, 2017).
The older patients in the current study assessed the evaluation of the effects of the treatment stage with respect to whether they were feeling better or not after the treatment. The stage of recovery and rehabilitation is especially important as an older individual requires long follow-up time and a well-structured rehabilitation process with respect to the health conditions and procedures done (Intiso et al., 2012; Young et al., 1998). In case the recovery and rehabilitation process are not followed up well, the older persons can get readmitted in the hospital leading to poor outcomes as reported in a study on recovery from dementia and hip fracture (McFarlane et al., 2017). Hence, it is important to consider the payment process across various stages of seeking health care. This is more pertinent for those older persons who travel long distances to seek health care and will incur travel costs in addition to the cost of health care.
Another important aspect which influenced health care seeking for older persons in the current study was quality of doctors and staff, especially nurses. Well-trained and qualified staff is one of the important factors for older people to seek health care from a hospital. This impacts on the outcomes, specialized treatment, and continuity of care in terms of follow-up after discharge to ensure complete recovery. Therefore, older persons need well-trained and qualified staff specific to geriatric needs across the stages of health care seeking (Rowe & Stone, 2016). Geriatric care requires health to be addressed holistically namely for social, financial and emotional aspects and not only biological aspects (Bennett & Flaherty-Robb, 2003). The older persons in the current study mentioned that they did not have qualified doctors or hospitals in their own areas and had to either travel within the city or from out of the region to seek care at a specialized hospital. The older persons need the comfort of well-coordinated specialist care for multiple conditions and good treatment (Oliver et al., 2014) and well-trained human resources for geriatric care (Gutiérrez Robledo et al., 2012). A study in Nepal reporting perspectives of older persons indicate that the physical environment and human resource need to be improved to create older people friendly hospitals (Karki et al., 2015).
Importance of quality of the hospital services was another important finding of the current study. It related to hospital operational processes such as optimal response time, seamless coordination, and concierge support to navigate the system before admission till discharge. A study in North India on quality of medical and nonmedical services for older persons in a tertiary-care hospital suggested separate queues for older people and reduced waiting times (Shivendra et al., 2014). Quality of hospital service, service efficiency, and affordability were important factors for health care seeking for older persons in China (Lu et al., 2017). A systematic review on quality systems suggests the need to build quality indicators for nonclinical aspects of care for older persons (Joling et al., 2018). The use of information technology is reported to improve capabilities and quality to deliver older person’s care in Lebanese public hospitals (Badr et al., 2017). An integrated literature review in Norway suggested complementing the in-house visits of older persons with virtual home visits to address the complex health care needs of the older persons (Husebø & Storm, 2014). This can be a step to continue health care support after the hospital visit and it stressed on guiding older persons in managing their medications. Structured goal setting in acute care for older people during discharge planning can decrease readmissions of older persons, improve hospital quality, and reduce costs in health care (Docker et al., 2015).
Methodological Considerations
The strength of the study lies in gathering in-depth qualitative experiences of the older people seeking health care at a hospital in urban India. A limitation of the study is that it focused on one private hospital in the city of Hyderabad. There are other government and semi-autonomous institutes in the city where older persons access for treatment and specialized centers of care for specific ailments such as oncology.
The study was conducted in one hospital; hence, transferability of the findings is limited. The hospital selected for the study could be accessed by those older patients in India who had coverage by an insurance scheme, whether private or government health. Hence, a lot of older persons who were interviewed came from the insurance network supported by the hospital. This might have led to the exclusion of older persons who could not afford immediate out-of-pocket expenditure. Those older individuals who could not travel to the hospital due to long distance or restricted due to severe illness were also excluded from the study.
Conclusion
Older person’s health-care-seeking experience depends upon individual financial mechanisms, quality of medical staff and services in hospitals, and infrastructural facilities of the hospital. Insurance support from hospitals and employers, cash discounts, and universal health coverage for older persons will improve access and affordability for older persons. Quality of staff can be enhanced by geriatric-specific competencies to address multiple and complex morbidities of the older population. Improving operational processes at the hospital and facilitating geriatric care can enable older persons to access health care more efficiently.
Acknowledgments
This is to thank all the research participants in sharing their experiences and the staff of the hospital for the support in conducting the research.
Footnotes
Authors’ Note: S.G., Z.N.K., N.R., and H.T. designed the study. S.G. was involved in data collection. S.G., Z.N.K., N.R., and H.T. prepared the draft manuscript. All authors reviewed the manuscript and approved the final version.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Considerations: Ethical approval for the study was granted by the Ethical Board, Tata Institute of Social Sciences, Mumbai, India and the hospital ethics committee. Informed consent was taken from the participants during the study. Confidentiality and privacy of the data provided by them was ensured. The respondents were told that they could withdraw from the study at any point of time. It was explained to the participants that the study would not disturb the treatment or health services they are seeking in the health care organization. In case permission from the relatives was needed, it was taken and only then the interview was conducted.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Sachin Ganorkar  https://orcid.org/0000-0002-9409-6642
https://orcid.org/0000-0002-9409-6642
References
- Adhikari D., Rijal D. P. (2010). Factors affecting health seeking behavior of senior citizens of Dharan. Journal of Nobel Medical College, 3(1), 50–57. 10.3126/jonmc.v3i1.10055 [DOI] [Google Scholar]
- Adhikari P. (2017). Geriatric health care in India—Unmet needs and the way forward. Archives of Medicine & Health Sciences, 5(1), 112–114. 10.4103/2321-4848.208215 [DOI] [Google Scholar]
- Ahmed S. M. (2005). Exploring health-seeking behavior of disadvantaged populations in rural Bangladesh. Karolinska Institutet University Press; 10.1007/s11098-017-0904-7 [DOI] [Google Scholar]
- Ahmed S. M., Tomson G., Kabir Z. N. (2005). Socio economic status overrides age and gender in determining health seeking behaviour in rural Bangladesh. Bulletin of the World Health Organization, 83, 109–117. 10.1590/S0042-96862005000200011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akiyama N., Shiroiwa T., Fukuda T., Murashima S., Hayashida K. (2018). Healthcare costs for the elderly in Japan: Analysis of medical care and long-term care claim records. PLoS ONE, 13(5), 1–15. 10.1371/journal.pone.0190392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badr N. G., Chedrawi C., Arida J. (2017). ICT and ageing in Lebanese public hospitals a resource based view perspective on capabilities [Conference]. Proceedings of the 10th International Joint Conference on Biomedical Engineering Systems and Technologies–Volume 5: HEALTHINF, 205-212, 2017, Porto, Portugal: http://www.scitepress.org/DigitalLibrary/Link.aspx?doi=10.5220/0006096102050212 [Google Scholar]
- Bennett J. A., Flaherty-Robb M. K. (2003). Issues affecting the health of older citizens: Meeting the challenge. Online Journal of Issues in Nursing, 8(2), 2 http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12795628 [PubMed] [Google Scholar]
- Biswas P., Kabir Z. N., Nilsson J., Zaman S. (2006). Dynamics of health care seeking behaviour of elderly people in rural Bangladesh. International Journal of Ageing and Later Life, 1(1), 69–89. 10.3384/ijal.1652-8670.061169 [DOI] [Google Scholar]
- Bourne P. (2010). Health literacy and health seeking behavior among older men in a middle-income nation. Patient Related Outcome Measures, 2010, 39–49. 10.2147/prom.s11141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Central Statistics Office. (2011, June). Situation analysis of the elderly in India central statistics office ministry of statistics & programme implementation government of India. http://mospi.nic.in/sites/default/files/publication_reports/elderly_in_india.pdf [Google Scholar]
- Cybulski M., Krajewska-Kułak E., Sowa P., Shpakau A., Theodosopoulou E., Chadzopulu A. (2016). Most common health problems of elderly in the opinion of health sciences students in Poland, Belarus and Greece. Progress in Health Sciences, 6(2), 39–45. 10.5604/01.3001.0009.5027 [DOI] [Google Scholar]
- de Carvalho I. A., Epping-jordan J., Pot A. M., Kelley E., Toro N., Thiyagarajan J. A., . . . Beard J. R. (2017, October). Organizing health-care services to meet older people’s needs. https://www.semanticscholar.org/paper/Organizing-health-care-services-to-meet-older-%E2%80%99-s-Carvalho-Epping-Jordan/67dfe4ef05cc7c6c8fba6333c63aa9f81e4edd9b [DOI] [PMC free article] [PubMed]
- Dey S., Nambiar D., Lakshmi J., Sheikh K., Reddy K. (2012). Health of the elderly in India: Challenges of access and affordability. In Smith J. P., Majmundar M. (Eds.), Aging in Asia: Findings from new and emerging data initiatives, (pp. 371-386). Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Docker M., Prof A., Mackenzie L. (2015, November). Goal setting with older people in acute care before and after discharge: Occupational therapists perspectives. https://www.semanticscholar.org/paper/Goal-setting-with-older-people-in-acute-care-before-Docker-Mackenzie/8db15482c570dcafa28e6c17d4c3839b46b48164
- Elo S., Kyngäs H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Falaha T., Worku A., Meskele M. (2016). Health care seeking behaviour of elderly people in rural part of Wolaita Zone, Southern Ethiopia. Health Science Journal, 10, Article 4. 10.1093/ndt/gfq722 [DOI] [Google Scholar]
- Gutiérrez Robledo L. M., López Ortega M., Arango Lopera V. E. (2012). The state of elder care in Mexico. Current Geriatrics Reports, 1(4), 183–189. 10.1007/s13670-012-0028-z [DOI] [Google Scholar]
- Habibullah S., Afsar S. (2013). Health seeking behavior of adult patients attending OPDs of public sector hospitals in Karachi. Pakistan Journal of Medical Research, 52(3), 80–83. [Google Scholar]
- Hamiduzzaman M., De Bellis A., Abigail W., Kalaitzidis E. (2017). The social determinants of healthcare access for rural elderly women—A systematic review of quantitative studies. The Open Public Health Journal, 10(1), 244–266. 10.2174/1874944501710010244 [DOI] [Google Scholar]
- Healthcare Scenario of Hyderabad. (n.d.). https://hhbc.in/healthcare-scenario-of-hyderabad
- Husebø A. M. L., Storm M. (2014). Virtual visits in home health care for older adults. Scientific World Journal, 2014, Article 689873. 10.1155/2014/689873 [DOI] [PMC free article] [PubMed]
- Igun U. A. (1979). Stages in health-seeking: A descriptive model. Social Science & Medicine. Part A: Medical Psychology & Medical Sociology, 13, 445–456. 10.1016/0271-7123(79)90079-8 [DOI] [PubMed] [Google Scholar]
- Intiso D., Di Rienzo F., Russo M., Pazienza L., Tolfa M., Iarossi A., Maruzzi G. (2012). Rehabilitation strategy in the elderly. Journal of Nephrology, 25(Suppl. 19), 1–6. 10.5301/jn.5000138 [DOI] [PubMed] [Google Scholar]
- Jain N., Koolwal A., Goel A. (2016). Ageing in India. Journal of Community Medicine & Health Education, 6(1), Article 692. 10.4172/2161-0711.1000392 [DOI] [Google Scholar]
- Jeon B., Kwon S. (2017). Health and long-term care systems for older people in the republic of Korea: Policy challenges and lessons. Health Systems and Reform, 3(3), 214–223. 10.1080/23288604.2017.1345052 [DOI] [PubMed] [Google Scholar]
- Joling K. J., van Eenoo L., Vetrano D. L., Smaardijk V. R., Declercq A., Onder G., . . . van der Roest H. G. (2018). Quality indicators for community care for older people: A systematic review. PLoS ONE, 13(1), Article e0190298. 10.1371/journal.pone.0190298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judy W. W., Solomon C. K., George O., John O. (2015). Understanding the context of healthcare access among the elderly in informal settlement Kibera, Nairobi, Kenya. International Journal of Health Sciences and Research, 2595(11), 259–269. [Google Scholar]
- Karki S., Bhatta D. N., Aryal U. R. (2015). Older people’s perspectives on an elderly-friendly hospital environment: An exploratory study. Risk Management and Healthcare Policy, 8, 81–89. 10.2147/RMHP.S83008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana M., Sarma J. K., Sharma S., Datta A. (2015). State of elderly in India (The State of Elderly in India Report 2014). 10.1007/978-94-011-5854-1-3 [DOI]
- Ladha A., Khan R. S., Malik A. A., Khan S. F., Khan B., Khan I. N., Saleem S. (2009). The health seeking behaviour of elderly population in a poor-urban community of Karachi, Pakistan. Journal of the Pakistan Medical Association, 59(2), 89–92. [PubMed] [Google Scholar]
- Lu H., Wang W., Xu L., Li Z., Ding Y., Zhang J., Yan F. (2017). Healthcare seeking behaviour among Chinese elderly. International Journal of Health Care Quality Assurance, 30(3), 248–259. 10.1108/IJHCQA-10-2015-0132 [DOI] [PubMed] [Google Scholar]
- McFarlane R. A., Isbel S. T., Jamieson M. I. (2017). Factors determining eligibility and access to subacute rehabilitation for elderly people with dementia and hip fracture. Dementia, 16(4), 413–423. 10.1177/1471301215599704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver D., Foot C., Humphries R. (2014). Making our health and care systems fit for an ageing population. King’s Fund, 43(5), Article 731. 10.1093/ageing/afu105 [DOI] [PubMed] [Google Scholar]
- Patle R. A., Khakse G. M. (2015). Health-seeking behaviour of elderly individuals: A community-based cross-sectional study. The National Medical Journal of India, 28(4), http://archive.nmji.in/archives/Volume-28/Issue-4/Original-Article-III.pdf [PubMed] [Google Scholar]
- Rowe J. W., Stone R. (2016). Preparing for better health and health care for an aging population a vital direction for health and health care about the vital directions for health and health care series. 10.1109/IEMBS.2006.260188 [DOI]
- Salagre S. B. (2013). Health issues in geriatrics. Geriatrics, 177(26), 767–768. [Google Scholar]
- Shivendra S., Abhishek G., Manish M. K., Pallavi S., Rahul C. (2014). Quality of services in a tertiary care hospital of Northern India: Geriatric patient perspective. International Journal of Interdisciplinary and Multidisciplinary Studies, 1(5), 234–241. [Google Scholar]
- Shrivastava S. R. B. L., Shrivastava P. S., Ramasamy J. (2013). Health-care of elderly: Determinants, needs and services. International Journal of Preventive Medicine, 4, 1224–1225. [PMC free article] [PubMed] [Google Scholar]
- Subaiya L., Bansod D. (2014). Demographics of population ageing in India. 10.1017/CCO9781139683456.003 [DOI]
- Thakur R., Banerjee A., Nikumb V. (2013). Health problems among the elderly: A cross-sectional study. Annals of Medical and Health Sciences Research, 3(1), 19–25. 10.4103/2141-9248.109466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripathy J. P. (2014). Geriatric care in India: A long way to go. Journal of Mid-Life Health, 5(4), 205–206. 10.4103/0976-7800.145176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations. (2017). World population ageing [highlights]. 10.1007/s10916-012-9888-1 [DOI]
- Verma R., Khanna P. (2013). National program of health-care for the elderly in India: A hope for healthy ageing. International Journal of Preventive Medicine, 4(10), 1103–1107. https://www.ncbi.nlm.nih.gov/pubmed/24319548 [PMC free article] [PubMed] [Google Scholar]
- Waweru L. M., Kabiru E. W., Mbithi J. N., Some E. S. (2003). Health status and health seeking behaviour of the elderly persons in Dagoretti Division, Nairobi. East African Medical Journal, 80(2), 63–67. 10.1093/mnras/sts666 [DOI] [PubMed] [Google Scholar]
- Young J., Robinson J., Dickinson E. (1998). Rehabilitation for older people (Clinical Research Ed.). British Medical Journal, 316(7138), 1108–1109. 10.1136/bmj.316.7138.1108 [DOI] [PMC free article] [PubMed] [Google Scholar]