Abstract
Background:
CrossFit is a conditioning program involving high-intensity exercises performed in rapid, successive repetitions with limited or no recovery time. The shoulder girdle is highly involved in most basic CrossFit training programs.
Hypothesis:
CrossFit athletes affected by rotator cuff tear may be successfully treated with arthroscopic surgery with a high rate of early return to CrossFit activities.
Study Design:
Case series; Level of evidence, 4.
Methods:
Included in this study were athletes participating regularly in CrossFit training who had undergone arthroscopic rotator cuff repair. At a minimum follow-up of 24 months, we compared pre- and postoperative clinical outcome scores, including the Constant Score (CS), the American Shoulder and Elbow Surgeons (ASES) score, and a visual analog scale (VAS) for pain, as well as imaging results. Participants completed a return-to-CrossFit questionnaire at the final follow-up, and changes in laboratory blood test results from preoperative to final follow-up were evaluated for association with outcomes and questionnaire responses.
Results:
A total of 22 CrossFit athletes (23 shoulders) completed the 24-month follow-up evaluation. Each athlete had undergone single-row rotator cuff tendon repair with additional procedures such as biceps tenodesis. All (100%) athletes returned to intensive CrossFit training at a mean 8.7 ± 3.4 months after surgery (range, 6-15 months). CS and ASES scores improved between preoperative and final follow-up from 73 to 92 (P = .037) and from 71 to 95 (P = .035), respectively; VAS pain score improved from 7.2 preoperatively to 0.8 at final follow-up (P < .001). Imaging evaluation of the repaired rotator cuff tendon showed complete healing in 18 cases (78%) and incomplete healing in 5 (22%). Of the 5 patients with incomplete healing, 2 had lower clinical scores at follow-up. In their questionnaire responses, 13 (59%) participants indicated return to a higher level of fitness, 7 (32%) returned to the same level, and 2 (9%) returned to a lower level. We found a significant association between patients who indicated return to a higher level of CrossFit fitness and higher levels of creatine phosphokinase and testosterone from preoperative to final follow-up (P = .029 and .023).
Conclusion:
Arthroscopic repair of rotator cuff tendons led to 100% return to CrossFit participation at approximately 9 months of follow-up. All athletes had returned to sport by the final follow-up. Nevertheless, 2 patients reported a lower level of performance and showed scapular dyskinesis.
Keywords: CrossFit, cuff repair, return to sports, anabolic androgenic steroids
Founded in 2000 in the United States, CrossFit currently has more than 10,000 affiliates worldwide.22 CrossFit is a conditioning program involving high-intensity exercises such as Olympic lifting (snatch, clean, and jerk), powerlifting (squat, deadlift, press/push press, and bench press), and gymnastic movements (pull-ups, toes-to-bar, knees-to-elbows, lunges, muscle-ups, burpees, dips, push-ups, and rope climbs).3 These exercises are combined into high-intensity workouts that are performed in rapid, successive repetition with limited or no recovery time. This modality of high-intensity interval training improves muscle development, body composition, and maximal aerobic capacity.4
Recently, literature has focused on the possible role of CrossFit training as a cause of tendon and joint injuries.5 Although such intense training could logically lead to a high incidence of injuries, the literature has shown that no difference emerged with respect to Olympic weight lifting and gym training, distance running, military conditioning, or gymnastics.10 Injury rates are reported to be much higher in contact sports, such as soccer and basketball.18
The shoulder girdle is highly involved in most of the exercises composing the basic training and the “workout of the day” in CrossFit. CrossFit athletes have been shown to differ from athletes in gymnastics and other sports in terms of body composition, age, and the number of rest days they take. In the literature, only 1 cross-sectional study (which was developed through an electronic survey) has determined the training characteristics and prevalence of shoulder injuries in CrossFit athletes.24 The results of that study emerged from a self-reported questionnaire where the term injury encompassed any new musculoskeletal pain or sensation resulting from a CrossFit workout. In that series, only 1 individual reported surgical intervention for the injury, described by a sports medicine physician as a labral tear.24 CrossFit athletes may develop rotator cuff lesions because of the multitude of activities that entail abduction and forward elevation with external rotation under load-bearing conditions. The purpose of the current study was to evaluate the results of arthroscopic rotator cuff repair in a consecutive series of athletes and their consequent return to CrossFit activities. Our hypothesis was that arthroscopic surgery for rotator cuff lesions will lead to early return to CrossFit training and that athletes are able to return to their preinjury level of CrossFit performance.
Methods
The institutional review board at our clinic provided approval for this study. Clinical data were prospectively collected for athletes regularly participating in CrossFit training who had undergone arthroscopic rotator cuff repair by a single shoulder fellowship–trained surgeon (S.C.) between April 2013 and January 2017. Indications for surgery were a CrossFit-related shoulder injury with subsequent clinical and magnetic resonance imaging (MRI) diagnosis of rotator cuff tear.
Inclusion criteria were as follows:
Athletes participating in CrossFit training for a minimum of 1 year and at least 4 times a week preoperatively
No previous upper limb injury or surgery, including cervical spine injury
A maximum of 6 months from injury to surgery
Clinical signs of rotator cuff tear, with possible involvement of the biceps tendon
MRI scan showing partial-thickness (>50% of the width of the tendon) or full-thickness cuff tear, including biceps injury (degeneration, inflammation, and partial or full tear)
Athletes who complied with the postoperative restrictions, including the rehabilitation protocol and time of return to CrossFit training
A minimum 24-month follow-up with a complete clinical and ultrasound (US)/MRI follow-up.
Exclusion criteria were as follows:
Pre- and intraoperative assessment of glenohumeral arthritis
Concomitant medical or orthopaedic condition that would compromise return to CrossFit training
Overall, 22 CrossFit athletes (23 shoulders) who had rotator cuff repair were included in the study and submitted to statistical analysis at the final follow-up (24 months postoperatively) (Figure 1). All participants provided written informed consent and were extensively informed about the purpose of the study. All rights of the enrolled participants in the present study were protected. The study was carried out in accordance with the World Medical Association Declaration of Helsinki.
Figure 1.
Flowchart of study inclusion. SLAP, superior labrum anterior and posterior.
Operative Technique
All arthroscopic procedures were performed with the patient in the beach-chair position, under brachial plexus block, with the arm draped with 5 pounds of traction. Cefazolin 2 g was administered both 30 minutes before the procedure and 12 hours after the procedure; no adrenaline was added to the arthroscopic saline solution. The scope was inserted through a posterolateral approach; a standard anterior portal was used for inspection of the intra-articular structures, while additional portals were added depending on the location and size of tendon tear. The first surgical phase was assessment of biceps using a probe both for the labrum and tendon groove inspection, as suggested by Motley et al.17 In case of inflammation, degeneration, or partial tear of the biceps tendon, or if a superior labrum anterior and posterior lesion of type 2 or higher was found, we performed a tenotomy/tenodesis in the bicipital groove using a 4.5-mm titanium double-loaded Healix TI BR (DePuy Synthes) suture anchor, with 2 suture lasso knots—1 knot crossing and 1 knot passing into the biceps tendon. In case of complete rupture of the biceps during CrossFit training with a positive Popeye sign, a mini-open tenodesis as described by Tangari et al23 was performed after rotator cuff repair. Then, depending on the side and location of the cuff tear, additional portals were created. Partial lesions of more than 50% of the tendon width were completed; debridement of the tendon stump and shaving of the native footprint were systematically performed.
All lesions were repaired through use of a 4.5-mm titanium double- or triple-loaded Healix TI BR suture anchor. Finally, anterior acromioplasty with coplaning of the acromion-clavicular joint was performed. In case of a symptomatic acromioclavicular joint, the arthroscopic Mumford procedure was performed.
Rehabilitation
The arm was immobilized in a neutral rotation sling with 20° of abduction (IMB 800 Multisas; FGP Srl) for 3 or 4 weeks depending on the size of the cuff tear. Removal of the sling was allowed for early elbow mobilization and pendulum exercises starting at 1 week postoperatively. After sling removal, rehabilitation consisted of a 1-hour session under the supervision of a physical therapist, 3 times a week, with the patient using oral pain medications such as paracetamol 1 g before the session if needed. The first month of rehabilitation consisted of physical techniques to manage pain (icing, massaging of the cervical area, local electrotherapy) and therapist-assisted recovery of passive motion; mobilization was stopped when the maximum bearable range of motion was reached with a visual analog scale (VAS) pain score of less than 5. In this period, after sling removal, CrossFit training was not allowed, but constant-intensity jogging, treadmill, and cycling were allowed. Starting in the fifth postoperative week, with a frequency of 3 times a week, rehabilitation included recovery of active range of motion in addition to anti-inflammatory electrotherapy and massaging of the cervical area. Individuals were allowed to resume CrossFit Olympic lifting (snatch, clean, and jerk) and powerlifting movements (squat, deadlift, press/push press, and bench press) using plastic bars but no weights or barbells. The exercises were performed under the supervision of a qualified CrossFit trainer, and participants faced a mirror so they could monitor their form. For fitness improvement, participants performed high-intensity training with rapid succession of jogging, treadmill, and cycling in addition to exercises for the abdominal muscles. Participants began constant-intensity training with low resistance using Assault Bike and Concept 2 Rower devices. In the fourth postoperative month, a specific program for scapular motion was added,1 and participants were allowed to use weights equaling 10% of their body weight. Progressively, depending on the athlete’s condition, heavier weights were allowed, but gymnastic movements were forbidden until 6 months after surgery.
Clinical Outcomes
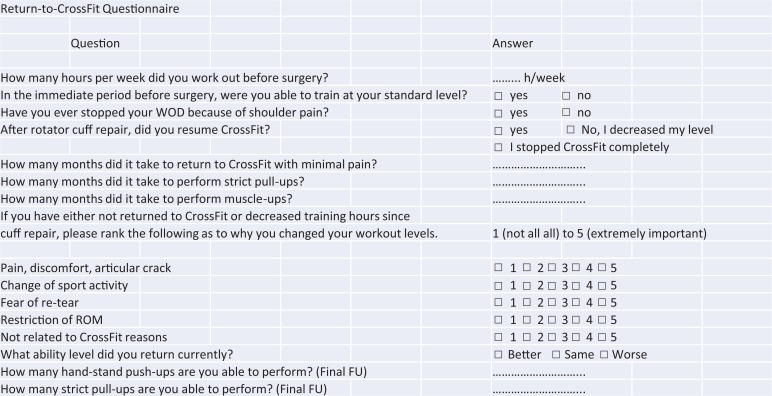
Clinical outcomes were assessed preoperatively and at final follow-up. The Constant Score (CS)2 and the American Shoulder and Elbow Surgeons (ASES) score were used for evaluation of the shoulder joint. At final follow-up, a customized return-to-CrossFit questionnaire was administered to patients (prospectively) (Figure 2). Scapular position and motion were evaluated according to Kibler et al.12 Finally, VAS pain scores were recorded. Some return-to-CrossFit outcomes were recorded at the final follow-up: hours of postoperative participation, length of time CrossFit was discontinued before surgery (days), length of time to resume CrossFit after surgery (months), return level of fitness (higher, same, lower), and last CrossFit exercise resumed.
Figure 2.
Return-to-CrossFit questionnaire. FU, follow-up; ROM, range of motion; WOD, workout of the day.
Imaging Outcomes
At the final 24-month follow-up, US evaluation of the repaired tendons was consistently performed by an expert musculoskeletal radiologist who was blinded to the operative report. A standard high-frequency musculoskeletal transducer was used. Routine static grayscale images as well as dynamic images were obtained during shoulder elevation with the transducer placed parallel to the fibers of the deltoid and the lateral acromion (Imagic Agile; Esaote Medical). The radiologist evaluated the repaired tendons as healed, incompletely healed, or retorn. In case of uncertain repair integrity evaluation, an MRI was obtained. Blinded to the operative protocol and the US images, the radiologist applied the Sugaya repair integrity classification (type 1, sufficient thickness with homogeneously low intensity; type 2, sufficient thickness with partial high intensity; type 3, insufficient thickness without discontinuity; type 4, presence of a minor discontinuity; and type 5, presence of a major discontinuity).21 Position of the suture anchors and arthritic changes of the glenohumeral joint were evaluated on a 2-plane radiograph (anteroposterior and axillary views).
Laboratory Test Results
All athletes were submitted to routine and sport-specific blood laboratory examinations the day before surgery and at the final follow-up. Hemoglobin, creatine phosphokinase (CPK), liver enzymes (aspartate aminotransferase, alanine aminotransferase), baseline lipid profile (high-density lipoprotein cholesterol [HDL-C], low-density lipoprotein cholesterol [LDL-C], triglycerides), and testosterone levels were studied for the purpose of determining whether these factors had a relationship to return to CrossFit (level of fitness declared).
Statistical Analysis
Patient data were analyzed through use of SPSS Version 23 (IBM Corp). Patient demographics were presented as means and standard deviations or frequencies and percentages. Categorical variables were presented as frequencies and percentages and were compared via the Pearson chi-square test. Return-to-CrossFit variables were reported as continuous data for hours spent weekly practicing CrossFit before and after surgery, the length of time that patients discontinued or decreased CrossFit preoperatively, the time elapsed from injury, and the time to return to CrossFit postoperatively. Continuous variables were compared using the Wilcoxon signed rank test. To determine the predictors of early return to CrossFit, a logistic regression model was used for multivariate analysis; considered variables were sport-specific blood laboratory examinations. Statistical significance was set at P < .05. From a difference in total ASES score of 15 ± 8 at follow-up, assuming a 2-tailed α = .05 (sensitivity, 95%) and a β = 0.95 (study power, 95%), we determined that at least 21 patients were required at the follow-up evaluation (G*Power 3 power analysis program).
Results
Patient Characteristics
Patient characteristics are presented in Table 1.
TABLE 1.
Characteristics of the Study Patientsa
| Characteristic | Value |
|---|---|
| Sex, n (%) | |
| Male | 20 (90) |
| Female | 2 (10) |
| Age, y | 40.5 ± 8.8 (29-52) |
| Body mass index, kg/m2 | 27.04 ± 3.6 (20-33) |
| Fat percentage | 10.9 ± 4 (6-17) |
| Shoulder side, n (%) | |
| Left | 12 (52) |
| Right | 11 (48) |
| Preinjury CrossFit participation, h/wk | 15.2 ± 3 (10-18) |
| Presurgery CrossFit participation, n (%) | |
| Maintained baseline routine | 10 (45) |
| Scaled back CrossFit involvement | 11 (50) |
| Stopped CrossFit | 1 (5) |
aN = 22 patients, 23 shoulders. Values are expressed as mean ± SD (range) unless otherwise noted.
Surgical Arthroscopic Procedures
Shoulder arthroscopic procedures (Table 2) consisted of synovectomy, biceps tenotomy/tenodesis or tenodesis alone if torn, subscapularis single-row repair, bursectomy, posterosuperior cuff repair with shaving of the greater tuberosity, acromioplasty, coplaning, and/or Mumford procedure of the acromioclavicular joint. Cuff tears were classified as follows: 1 (4%) massive, 4 (17%) large, 10 (43%) small, and 8 (35%) partial (>50% of the width of the tendon). A mean of 1.3 (range, 1-3) triple-loaded suture anchors were used. No surgical intraoperative complication was recorded.
TABLE 2.
Diagnoses and Surgical Arthroscopic Procedures (23 Shoulders)a
| n (%) | |
|---|---|
| Diagnoses | |
| SLAP ≥2 | 4 (17) |
| Biceps severe inflammation (no instability) | 7 (30) |
| Complete biceps tear | 2 (8.7) |
| Synovitis | 5 (21) |
| Subscapularis (isolated) tear | 5 (21) |
| Bursitis | 16 (70) |
| Supraspinatus (isolated) tear | 7 (30) |
| Supraspinatus/infraspinatus tear | 6 (26) |
| Supraspinatus/subscapularis tear | 5 (21) |
| Subacromial spoor | 6 (26) |
| Acromioclavicular spoor | 4 (17) |
| Surgical arthroscopic procedures | |
| Biceps tenotomy/tenodesis | 13 (56) |
| Biceps tenodesis (if torn) | 2 (8.7) |
| Synovectomy | 5 (21) |
| Anterosuperior cuff single-row repair | 10 (42) |
| Posterosuperior cuff single-row repair | 13 (56) |
| Anterior acromioplasty | 18 (79) |
| Acromioclavicular joint coplaning | 12 (52) |
| Arthroscopic Mumford | 4 (17) |
aSLAP, superior labrum anterior and posterior.
Clinical Outcomes
At 24-month follow-up, each of the 22 athletes showed significant improvement in the CS and ASES scores as well as VAS pain score when compared with preoperative scores (P < .05 for all) (Table 3).
TABLE 3.
Clinical Results Before Surgery and at 24-Month Follow-upa
| Clinical Outcome | Before Surgery | 24-Month Follow-up | P |
|---|---|---|---|
| Constant score | 73 ± 6 (66-80) | 92 ± 4 (88-100) | .037 |
| ASES score | 71 ± 8 (65-80) | 95 ± 3 (90-100) | .035 |
| VAS pain | 7.2 ± 1.2 | 0.8 ± 0.5 | <.001 |
aValues are expressed as mean ± SD (range). ASES, American Shoulder and Elbow Surgeons; VAS, visual analog scale.
Return-to-CrossFit Results
We found that 100% of athletes (22 patients; 23 shoulders) returned to complete CrossFit training after a mean 8.7 ± 3.4 months after surgery (range, 6-15 months) (Table 4). No statistically significant difference in weekly CrossFit training was found between preinjury and postoperative timepoints (15.2 ± 3 vs 14.8 ± 2.9 hours per week, respectively; P = .76). Postoperatively, 13 participants (59%) indicated return to a higher level of fitness, 7 (32%) returned to the same level, and 2 (9%) returned to a lower level. The 2 athletes with a lower level of fitness declared loss of control in overhead weight lifting (snatch, push-press, and thrusters) and partial inability to reach maximal external rotation with the arms in complete forward flexion (final phase of snatch). These 2 athletes were the only participants who showed scapular dyskinesis, with a prominence of the entire medial border (type 2 dyskinesis). No difference emerged in return-to-CrossFit between men and women (P = .8). Return to CrossFit was not significantly related to the time elapsed from injury (for all athletes, maximum 6 months) (P = .095). At the final follow-up, athletes reported that they were able to perform 11 ± 6 (range, 5-20) strict pull-ups and 40 ± 15 (range, 19-67) chest-to-ground push-ups.
TABLE 4.
Results of the Return-to-CrossFit Questionnairea
| Return-to-CrossFit Outcomes | Value |
|---|---|
| Postoperative participation, h/wk | 14.8 ± 2.9 |
| Length of time CrossFit was discontinued before surgery, d | 45 ± 23 |
| Length of time to resume CrossFit after surgery, mo | 8.7 ± 3.4 |
| Return level of fitness, n (%) | |
| Higher | 13 (59) |
| Same | 7 (32) |
| Lower | 2 (9) |
| Last exercise resumed, n (%) | |
| Snatch | 10 (45) |
| Muscle-ups | 7 (32) |
| Rope climb | 2 (9) |
| Others | 3 (13) |
aValues are expressed as mean ± SD unless otherwise noted.
Imaging Outcomes
US evaluation of the repairs showed complete healing in 18 cases (78%) and incomplete healing in 5 cases (21%). The final 5 cases were submitted to MRI examination, and the radiologist found two type 2 and three type 3 repair integrity categories according to the Sugaya classification. Of these, the 2 athletes with a type 2 repair reported that they returned to their preinjury level of performance. Of the 3 patients showing a type 3 repair integrity category, 2 patients reported a lower level of performance and 1 patient reported returning to the same preinjury level. The 2-plane radiographs showed no case of suture anchor mobilization and 2 cases (out of 23 shoulders; 8.7%) of low-grade glenohumeral arthritis (Hamada grade 2). The 2 cases showing Hamada grade 2 arthritis did not show any statistical difference in the final results or in return to CrossFit (P > .08).
Laboratory Results Outcomes
The logistic regression model revealed a significant association between higher levels of CPK and testosterone and return to a higher level of CrossFit at the final follow-up (P = .029 and .023, respectively), whereas no association was found with CS and ASES score. The 2 variables that changed significantly between the preoperative assessment and final follow-up were CPK (P = .031) and testosterone (P = .027); other variables did not show any significant difference.
Discussion
This study showed that arthroscopic repair of rotator cuff tendons led to 100% return to sport for CrossFit athletes at about 9 months of follow-up (range, 6-15 months), although some CrossFit skills such as snatch (Figure 3) and muscle-ups (Figure 4) were resumed later due to the high stresses on shoulder tendons. Most of the athletes (91%) returned to the same preinjury level or higher, with comparable preinjury and final follow-up hours of involvement in CrossFit.
Figure 3.
The snatch Olympic weight-lifting exercise: (A) initial, (B) midterm, and (C) final phase.
Figure 4.
The muscle-up (ring-dip) exercise: (A) initial, (B) midterm, and (C) final phase.
In every workout, CrossFit athletes perform weight lifting exercises, gymnastics, and high-intensity endurance, such as running, Assault Bike, and indoor rowing, with very limited recovery time. Body composition of such athletes is similar to that of body builders, with a body mass index of 25 kg/m2 and very low percentages of body fat (around 10%). Because CrossFit athletes can have high body weights for their heights (eg, 220 pounds for a 6-foot-tall athlete), their tendons have to support tremendous stresses for up to 7 training sessions per week, 2 to 3 hours a day. Nevertheless, the rate of shoulder injuries does not differ from the rate in other sports.24 The weight-training focus of CrossFit is likely the reason for such low injury rates as opposed to contact sports.11 This prospective study provides no data about the epidemiological patterns of CrossFit shoulder injuries; our only aim was to report the results of rotator cuff repair in competitive CrossFit athletes.
Up to 70% of the athletes had biceps abnormality. This very high percentage of biceps abnormality may be secondary to the execution of some exercises such as ring dips and muscle-ups, where the shoulder is positioned in maximum extension with the elbow in full flexion under the body weight. The susceptibility of the shoulder to weight-training injury is partially due to the high compressive loads that these exercises apply to a traditionally nonweightbearing joint14 (Figure 5) (see the online Video Supplement for this technique).
Figure 5.

The supraspinatus articular-side tear consequent with the injury shown in the video.
During strenuous workouts, the rotator cuff and other muscle-tendon units may sustain chronic overuse and acute injuries, as acute tear6 and rhabdomyolysis.20 A mixture of abduction-adduction and external rotation during resisted contraction with the hand fixed in a position may be the cause of the high incidence of biceps injury. The mean age of our study group was only 40 years, but the group had a considerable incidence (20%) of large and massive tears, with small tear of the supraspinatus as the most common injury. This is in line with observations in the gymnastic shoulder, where young male athletes develop lesions of the biceps and supraspinatus.7
Unfortunately, we do not have data to compare return to CrossFit after rotator cuff surgery. A recent review of the literature found that most recreational athletes returned to sports at the same level of play as before the rotator cuff injury, but only half of professional and competitive athletes returned to an equivalent level of play.13 Rossi et al19 reported an 87% rate of return to sports in athletes with a mean age of 42 years after arthroscopic repair of a partial-thickness cuff tear with a minimum of 2 years of follow-up. The reasons our group had 100% return to sports may lie in the early and successful treatment of the injury and the high psychological involvement and discipline of CrossFit athletes, all of whom strictly followed the rehabilitation program. The 2 athletes (9%) who reported loss of performance had type 2 scapular dyskinesis, with prominence of the entire medial border. The rest of the study group did not show any scapular abnormalities. This type of dyskinesia is often related to anterior shoulder instability.12 In these 2 athletes, pain in the posterior area of the scapula and of the cervical area interfered with the execution of the scapular rehabilitation program.
Each patient underwent dynamic sonographic evaluation of repair integrity by an expert radiologist blinded to the operative report. US imaging has been demonstrated to be highly sensitive and specific for the detection of recurrent rotator cuff tears, even partial tears.9 In addition, MRI was performed when US images were not definitive, and the MRI scans revealed two type 2 and three type 3 repair integrity categories according to the Sugaya classification.21 Although pre- and intraoperative factors affecting rotator cuff retear have been studied,15 information is lacking for the late postoperative periods, and therefore we do not know whether specific sports predispose to cuff retear. It is plausible that such intense training could compromise the tendons over the years, yet 2 years of follow-up is a reasonable time to evaluate retear and the results of arthroscopic repair.
Athletes underwent laboratory blood examinations at preoperative and final follow-up points to determine whether any of the laboratory values could be related to return to sport and/or higher CS and ASES scores. At the final follow-up, high values of CPK and testosterone seemed to positively influence return to sport. The high motivation of CrossFit athletes may explain the result; in fact, harder training causes secondary muscle fatigue and damage and an increase of CPK levels. CPK is released in blood after high-intensity training, with some cases of rhabdomyolysis reported.16,20 This condition is usually benign, but in very extreme training, it may lead to renal failure. Some athletes showed supraphysiological levels of testosterone in addition to other blood parameters as decreased HDL-C, increased LDL-C, and higher levels of hemoglobin and hepatic enzymes. These athletes admitted to use of anabolic androgenic steroids, so their sport performance was enhanced by these drugs. The possible role of anabolic androgenic steroids in tendon degeneration is unclear; recent experimental studies in sheep have shown a positive role of nandrolone in the prevention of muscle atrophy and fatty degeneration.8
Limitations
This study has several limitations, including the relatively short follow-up and the limited number of patients. The a posteriori power analysis showed adequate power to assess changes in the ASES score but not in the other variables, so many of the comparisons are underpowered; furthermore, the customized return-to-CrossFit questionnaire has not been previously validated. The high prevalence of biceps abnormality could have contributed to preoperative symptoms and limitations, the treatment of which could have confounded assessments of cuff repair. To detect later retears and development of osteoarthritis, a longer follow-up is necessary. The lack of a comparison group treated differently does not allow us to say whether the technique we used (arthroscopic single-row repair) is the best and whether CrossFit predisposes patients to retears more than other sports. Finally, the results may not be reproducible in the general orthopaedic community, because surgical procedures were performed by a single, high-volume, fellowship-trained shoulder surgeon.
Conclusion
In this prospective series, arthroscopic repair of cuff tendons was associated with 100% return to CrossFit training after about 9 months of follow-up. All athletes returned to CrossFit training at the final follow-up, with only 2 athletes reporting return to a lower level of participation and showing scapular dyskinesis.
A Video Supplement for this article is available online at http://journals.sagepub.com/doi/suppl/10.1177/2325967120911039.
Footnotes
Final revision submitted December 8, 2019; accepted December 17, 2019.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the ethics committee of Clinica San Felicano, Rome, Italy.
References
- 1. Carbone S, Postacchini R, Gumina S. Scapular dyskinesis and SICK syndrome in patients with a chronic type III acromioclavicular dislocation: results of rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):1473–1480. [DOI] [PubMed] [Google Scholar]
- 2. Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 3. CrossFit. The CrossFit training guide. https://www.crossfit.com/cf-seminars/CertRefs/CF_Manual_v4.pdf. Accessed April 5, 2016.
- 4. Eather N, Morgan PJ, Lubans DR. Improving health-related fitness in adolescents: the CrossFit Teens randomised controlled trial. J Sports Sci. 2015;34(3):1–15. [DOI] [PubMed] [Google Scholar]
- 5. Fisker FY, Kildegaard S, Thygesen M, Grosen K, Pfeiffer-Jensen M. Acute tendon changes in intense CrossFit workout: an observational cohort study. Scand J Med Sci Sports. 2017;27(11):1258–1262. [DOI] [PubMed] [Google Scholar]
- 6. Friedman MV, Stensby JD, Hillen TJ, Demertzis JL, Keener JD. Traumatic tear of the latissimus dorsi myotendinous junction: case report of a CrossFit-related injury. Sports Health. 2015;7(6):548–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gerhardt C, Doyscher R, Boschert HP, Scheibel M. The gymnastics shoulder. Orthopade. 2014;43(3):230–235. [DOI] [PubMed] [Google Scholar]
- 8. Gerber C, Meyer DC, Fluück M, Benn MC, von Rechenberg B, Wieser K. Anabolic steroids reduce muscle degeneration associated with rotator cuff tendon release in sheep. Am J Sports Med. 2015;43(10):2393–2400. [DOI] [PubMed] [Google Scholar]
- 9. Gilat R, Atoun E, Cohen O, et al. Recurrent rotator cuff tear: is ultrasound imaging reliable? J Shoulder Elbow Surg. 2018;27(7):1263–1267. [DOI] [PubMed] [Google Scholar]
- 10. Hak P, Hodzovic E, Hickey B. The nature and prevalence of injury during CrossFit training [published online November 22, 2013]. J Strength Cond Res. doi:10.1519/JSC.0000000000000318 [DOI] [PubMed] [Google Scholar]
- 11. Keog JWL, Winwood PW. The epidemiology of injuries across the weight-training sports. Sports Med. 2017;47:479–501. [DOI] [PubMed] [Google Scholar]
- 12. Kibler WB, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg. 2012;20(6):364–372. [DOI] [PubMed] [Google Scholar]
- 13. Klouche S, Lefevre N, Herman S, Gerometta A, Bohu Y. Return to sport after rotator cuff tear repair: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1877–1887. [DOI] [PubMed] [Google Scholar]
- 14. Kolber MJ, Beekhuizen KS, Cheng MS, et al. Shoulder injuries attributed to resistance training: a brief review. J Strength Cond Res. 2010;24(6):1696–1704. [DOI] [PubMed] [Google Scholar]
- 15. Lee YS, Jeong JY, Park CD, Kang SG, Yoo JC. Evaluation of the risk factors for a rotator cuff retear after repair surgery. Am J Sports Med. 2017;45(8):1755–1761. [DOI] [PubMed] [Google Scholar]
- 16. Meyer M, Sundaram S, Schafhalter-Zoppoth I. Exertional and CrossFit-induced rhabdomyolysis. Clin J Sport Med. 2018;28(6):e92–e94. [DOI] [PubMed] [Google Scholar]
- 17. Motley GS, Guengerich B, Schuller T, Turbyfill A. The ramp test: an arthroscopic technique for confirming intra-articular subluxation and instability of the long head of the biceps tendon within the shoulder. Arthrosc Tech. 2018;7(4):e327–e330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Parkkari J, Kannus P, Natri A, et al. Active living and injury risk. Int J Sports Med. 2004;25:209–216. [DOI] [PubMed] [Google Scholar]
- 19. Rossi LA, Atala N, Bertona A, et al. Return to sports after in situ arthroscopic repair of partial rotator cuff tears. Arthroscopy. 2019;35(1):32–37. [DOI] [PubMed] [Google Scholar]
- 20. Routman HD, Triplet JJ, Kurowicki J, Singh N. Isolated rhabdomyolysis of the infraspinatus muscle following the CrossFit “sissy test”: a report of two cases. JBJS Case Connect. 2018;8:e2. [DOI] [PubMed] [Google Scholar]
- 21. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am. 2007;89(5):953–960. [DOI] [PubMed] [Google Scholar]
- 22. Summitt RJ, Cotton RA, Kays AC, Slaven EJ. Shoulder injuries in individuals who participate in CrossFit training. Sports Health. 2016;8(6):541–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tangari M, Carbone S, Gallo M, Campi A. Long head of the biceps tendon rupture in professional wrestlers: treatment with a mini-open tenodesis. J Shoulder Elbow Surg. 2011;20(3):409–413. [DOI] [PubMed] [Google Scholar]
- 24. Weisenthal BM, Beck CA, Maloney MD, DeHave KE, Giordano BD. Injury rate and patterns among CrossFit athletes. Orthop J Sports Med. 2014;2(4):2325967114531177. [DOI] [PMC free article] [PubMed] [Google Scholar]