Abstract
Background:
The operative treatment of Achilles tendon ruptures has been associated with lower rerupture rates and better function but also a risk of surgery-related complications compared with nonoperative treatment, which may provide improved outcomes with accelerated rehabilitation protocols. However, economic decision analyses integrating the updated costs of both treatment options are limited in the literature.
Purpose:
To compare the cost-effectiveness of operative and nonoperative treatment of acute Achilles tendon tears.
Study Design:
Economic and decision analysis; Level of evidence, 2.
Methods:
An economic decision model was built to assess the cost-utility ratio (CUR) of open primary repair versus nonoperative treatment for acute Achilles tendon ruptures, based on direct costs from the practices of sports medicine and foot and ankle surgeons at a single tertiary academic center, with published outcome probabilities and patient utility data. Multiway sensitivity analyses were performed to reflect the range of data.
Results:
Nonoperative treatment was more cost-effective in the average scenario (nonoperative CUR, US$520; operative CUR, US$1995), but crossover occurred during the sensitivity analysis (nonoperative CUR range, US$224-US$2079; operative CUR range, US$789-US$8380). Operative treatment cost an extra average marginal CUR of US$1475 compared with nonoperative treatment, assuming uneventful healing in both treatment arms. The sensitivity analysis demonstrated a decreased marginal CUR of operative treatment when the outcome utility was maximized, and rerupture rates were minimized compared with nonoperative treatment.
Conclusion:
Nonoperative treatment was more cost-effective in average scenarios. Crossover indicated that open primary repair would be favorable for maximized outcome utility, such as that for young athletes or heavy laborers. The treatment decision for acute Achilles tendon ruptures should be individualized. These pilot results provide inferences for further longitudinal analyses incorporating future clinical evidence.
Keywords: Achilles tendon, decision analysis, cost-effectiveness
The optimal treatment approach for acute Achilles tendon ruptures is evolving and controversial.9,22 Common measures to assess the effectiveness of treatment include rerupture rate, posttreatment complications, subjective and objective outcome measurements, and time to return to play or work.7,9,19,21,29 Open surgical repair has traditionally been considered the gold standard for active patients.6 Nonoperative treatment has demonstrated comparable rerupture rates and similar functional recovery when incorporating accelerated functional rehabilitation protocols that allow earlier weightbearing and more aggressive progression in ankle range of motion.1,2,19,23,29,30
Quantitative decision analyses can be used to assess medical decision making through a decision tree that integrates variables such as the outcome utility, costs, and probabilities of events for each treatment arm. Expected utility value analyses can predict the utility values for each arm as the proxy for its effectiveness, which can serve as the basis for cost-effectiveness analyses to assess the economic impact of treatment. There are limited decision analysis reports in the current literature for the management of acute Achilles tendon ruptures. A recent study slightly supported the cost-effectiveness of surgical treatment according to data prospectively collected at a single institution in Sweden,27 while another study based on a claims database in the United States (US) showed a lower cost of nonoperative treatment from the payer’s perspective.20 The most recent expected value decision analysis based on data in the US, published in 2002, concluded that open surgical repair may be the preferred treatment option because of its superior patient outcome utility value.11
In light of new evidence comparing operative and nonoperative treatment and the relative paucity of studies on the cost-effectiveness of treating Achilles tendon ruptures, the purpose of the present study was to compare the cost-effectiveness of open surgical repair and nonoperative treatment of acute Achilles tendon ruptures.
Methods
Study Design
This study was an economic decision analysis with multiway sensitivity analyses based on actual direct cost data, expected utility values from a previously published decision analysis,11 and outcome probabilities from a recent level 1 systematic review.28 In short, utility values serve as a surrogate for patient-reported satisfaction with the treatment results. Probabilities reflect how likely each treatment result will ensue.
The analytical model was built on a decision tree. The initial binary decision node led to 2 arms of treatment, represented by 2 chance nodes: (1) operative (OP; open surgical repair) and (2) nonoperative (NOP). Subsequent terminal events in each treatment arm were represented by 5 terminal nodes—(1) well-being, (2) rerupture of the Achilles tendon, (3) major complication, (4) moderate complication, and (5) minor complication—similar to the algorithm as previously described11 (Figure 1A).
Figure 1.
The (A) decision tree and (B) foldback analysis for the clinical decision scenario of an acute Achilles tendon rupture. □: decision node; ˆ: chance node; ▵: terminal node. The probability and utility values shown at the terminal nodes were average values, with the ultimate utility values from the foldback analysis shown at the chance nodes, together with the average and range of direct costs.
Definition of Events and Variables
The 5 terminal events were defined as previously described in a high-quality systematic review28 and a decision analysis.11 Major complications were defined as one of the following: deep vein thrombosis or pulmonary embolism either after OP or NOP treatment or a deep infection that required a surgical intervention. Moderate complications were defined as one of the following: a superficial infection or wound dehiscence that did not require a surgical intervention or sural nerve disturbance (after either OP or NOP treatment). Minor complications were defined as skin adhesion at the rupture site (after either OP or NOP treatment) and noncosmetic scarring. Each of these 3 terminal events as well as the other 2 events (well-being and reruptures) was associated with 3 key variables in the analytical model:
Probability (P; unitless): the probability of the occurrence of each of the terminal events after either OP or NOP treatment
Utility (U; unitless; range, 0-10): subjective outcome measurement from the patients’ perspective
Direct cost (C; US$): cost of each treatment arm from the payers’ perspective
The detailed methods can be found in the Appendix.
Probability Data Acquisition
Probabilities (P) were populated from a level 1 systematic review comparing primary open repair versus nonoperative treatment for acute Achilles tendon ruptures.28 The reported pooled rate of reruptures was assigned as POP-rerupavg and PNOP-rerupavg to represent the average probability for the terminal node of reruptures in the OP and NOP arms, respectively. The range of rerupture probabilities for each arm was represented by POP-rerupmin and POP-rerupmax as well as PNOP-rerupmin and PNOP-rerupmax as the minimal and maximal probabilities for the OP and NOP arms, respectively. These were determined by the minimal and maximal rates among the 7 individual publications4,13,14,16,17,21,29 assessed in the systematic review.
The pooled rates as well as the minimal and maximal rates of all the complications reported in the systematic review28 were categorized under the 3 terminal nodes of major complications, moderate complications, and minor complications and were then summed to represent the average and range of probabilities for each arm. The remaining probability values outside of the rerupture and complication rates were then assigned to the terminal node of well-being of each treatment arm.
Outcome Utility Data Acquisition
The outcome utility (U) was represented as a unitless, continuous visual analog scale score from 0 to 10, with 0 being the worst and 10 being the best possible subjective outcome. The utility value for each of the 5 terminal events was assigned as previously described in a study assessing expected values for primary open repair versus nonoperative treatment.11 In short, a group of patients were asked to complete a questionnaire that simulates the life scenarios of the 5 terminal events for the OP and NOP treatment arms. The average and range of utility values were then determined by the mean value (and the span of 1 standard deviation above and below such a value) reported in the study.
Cost Data Acquisition
Cost data (C) were obtained from the billing department of a major tertiary care university medical center. The data were pooled from the practices of 8 fellowship-trained sports medicine and foot and ankle orthopaedic surgeons over 2 years. The present study utilized the direct costs from the payers’ perspective.
The cost of the OP treatment arm was the sum of payments for surgeon’s fees, hospital fees, anesthesiologist’s fees, physical therapy, and outpatient clinic visits outside of the 90-day global period as well as associated medical devices. The cost of the NOP treatment arm was the sum of payments for physical therapy and outpatient clinic visits as well as associated medical devices. The cost for 1 outpatient clinic visit was on par with that for 1 outpatient physical therapy visit. The average costs for OP and NOP treatment were represented by COPavg and CNOPavg, respectively.
Both the OP and NOP arms were assumed to undergo accelerated rehabilitation protocols, as previously described.29 The total numbers of outpatient physical therapy and clinic visits were similar between the 2 arms.
Foldback Analysis for Expected Utility Values
A foldback analysis was performed to determine the ultimate utility values for the OP and NOP treatment arms. For either treatment arm, the contribution of each of the 5 terminal events to the utility values was determined by the product of U and P and was subsequently summed to reach the ultimate utility value for OP (UOPSUM) and NOP (UNOPSUM):
Cost-Utility Analysis
The average cost-utility ratio (CUR) was determined by normalizing the ultimate cost to the ultimate utility value, designated as CUROPavg and CURNOPavg, respectively, for the OP and NOP arms to reflect the cost to gain 1 unit of utility:
Multiway Sensitivity Analyses for Boundary Conditions
The possible range of utility values, probabilities of events, and direct costs was included in the analytical model to account for the variability of such data. The highest possible CUR was determined by implementing the highest possible ultimate utility value and lowest possible cost, and vice versa. The highest possible ultimate utility value was computed by maximizing the probability of well-being, minimizing the probabilities of the other 4 events, and implementing the maximal utility value for each event. The range of CURs for the OP and NOP arms was determined accordingly.
Multiway Sensitivity Analyses for Marginal Cost per Utility
The marginal cost per utility indicated the extra cost that the payers needed to pay for OP treatment as opposed to NOP treatment for 1 unit of utility, defined as “marginal CUR”: ΔCUR = CUROP − CURNOP. The sensitivity analyses assessed the effect of the (1) marginal utility of well-being and (2) marginal rate of reruptures on ΔCUR.
The marginal utility was defined as the assumptive gap of (UOP-Well − UNOP-Well) in a spectrum of 0 to 9.8, respectively, corresponding to UOP-Wellavg, UOP-Wellmin, and UOP-Wellmax. Such an analysis evaluated the assumptive scenario when OP treatment resulted in better than average outcomes for higher demanding patients (higher marginal utility) or else equal outcomes as compared with NOP treatment for lower demanding patients (marginal utility = 0).
The marginal rate of reruptures was defined as the assumptive gap of (PNOP-rerup − POP-rerup) in a spectrum of 0% to 20%, respectively, corresponding to PNOP-rerupavg, PNOP-rerupmin, and PNOP-rerupmax. Such an analysis evaluated the assumptive scenario when NOP treatment resulted in higher than average or equal rerupture rates as compared with OP treatment (marginal rerupture rate = 0).
Results
Acquired Data for Probability, Outcome Utility, and Cost
The pooled average probabilities for reruptures were 3.6% and 8.8%, respectively, for the OP and NOP treatment arms. The average probabilities for the OP versus NOP arms of major, moderate, and minor complications were 9.4% versus 10.2%, 8.8% versus 0.8%, and 13.1% versus 0.6%, respectively, resulting in average well-being probabilities of 65.1% versus 79.6%, respectively (Table 1).
Table 1.
Probability and Outcome Utility Data for the 5 Major Eventsa
| Probability, % | Outcome Utility | |||||
|---|---|---|---|---|---|---|
| Average | Minimum | Maximum | Average | Minimum | Maximum | |
| Well-being | (Maximum) | (Minimum) | ||||
| OP | 65.10 | 95.10 | 14.66 | 7.9 | 6.0 | 9.8 |
| NOP | 79.56 | 95.50 | 31.22 | 7.0 | 5.0 | 9.0 |
| Reruptures | ||||||
| OP | 3.60 | 1.70 | 10.00 | 2.6 | 0.4 | 4.8 |
| NOP | 8.80 | 4.50 | 20.80 | 2.6 | 0.4 | 4.8 |
| Major complications | ||||||
| OP | 9.44 | 0.00 | 9.44 | 1.0 | 0.0 | 2.6 |
| NOP | 10.24 | 0.00 | 10.24 | 1.0 | 0.0 | 2.6 |
| Moderate complications | ||||||
| OP | 8.76 | 0.00 | 45.45 | 3.5 | 1.4 | 5.6 |
| NOP | 0.78 | 0.00 | 34.14 | 3.5 | 1.4 | 5.6 |
| Minor complications | ||||||
| OP | 13.10 | 3.20 | 20.45 | 4.7 | 2.5 | 6.9 |
| NOP | 0.62 | 0.00 | 3.60 | 4.7 | 2.5 | 6.9 |
aNOP, nonoperative; OP, operative.
The average outcome utility of well-being for the OP arm was 7.9, compared with 7.0 for the NOP arm. The average and range of utilities for reruptures as well as major, moderate, and minor complications were identical for both treatment arms (Table 1). The average cost for OP treatment (in US$) was $12,477 (range, $7594-$17,323) versus $3100 (range, $1975-$4600) for NOP treatment (Table 2).
Table 2.
Direct Cost of OP Versus NOP Treatmenta
| Average | Minimum | Maximum | |
|---|---|---|---|
| OP (open repair) | |||
| Surgeon’s fee | 1468 | 157 | 1783 |
| Anesthesia fee | 1200 | 1200 | 1200 |
| Hospital fee | 7209 | 4762 | 10,240 |
| Outpatient visitb | 2250 | 1125 | 3750 |
| Associated medical devicec | 350 | 350 | 350 |
| Total | 12,477 | 7594 | 17,323 |
| NOP | |||
| Outpatient visitb | 2250 | 1125 | 3750 |
| Associated medical devicec | 850 | 850 | 850 |
| Total | 3100 | 1975 | 4600 |
aData are reported as US dollars. NOP, nonoperative; OP, operative.
bOutpatient visits included clinic visits and physical therapy sessions, which were estimated as an average of 22.5 visits (range, 15 to 30 visits) in total for both OP and NOP treatment, with the average direct cost of $100 (range, $75-$125).
cOne boot and 1 set of crutches were included for both OP and NOP treatment; an additional cost of short leg casting was applied to NOP treatment.
Foldback and Cost-Utility Analyses for Boundary Conditions
The foldback analysis revealed that the average ultimate utility value for OP treatment was 6.3 versus 6.0 for NOP treatment (Figure 1B). The average cost to gain 1 unit of utility for the OP arm was approximately 3 times more than that for the NOP arm (CUROPavg: $1995; CURNOPavg: $520). Multiway sensitivity analyses for boundary conditions showed crossover of the 2 treatment arms in which the CUROPmin could be as low as $789 and the CURNOPmax could be as high as $2079 (Figure 2). This indicated that in certain scenarios, OP treatment can be more cost-effective than NOP treatment.
Figure 2.
Sensitivity analyses for boundary conditions for operative (OP) versus nonoperative treatment, showing a crossover in the range between the lowest and highest possible cost-utility ratios (CURs). The numbers for each bar represent the minimum (left), average (middle), and maximum (right) values.
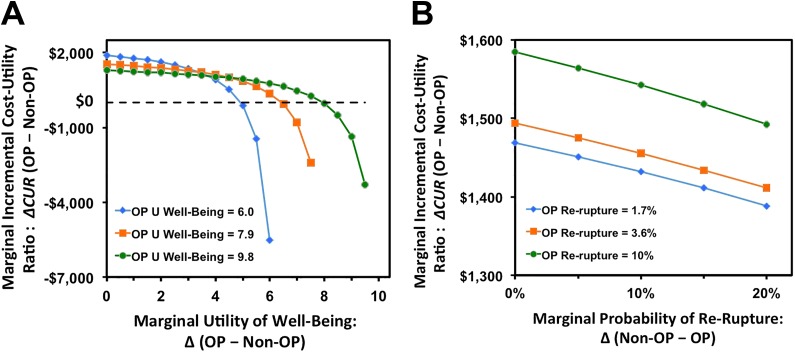
Multiway Sensitivity Analyses for Marginal Cost per Utility
OP treatment cost an extra marginal CUR of $1475, assuming the utility of well-being at the average values of 7.9 and 7.0, respectively, for OP and NOP treatment. The marginal CUR decreased as the marginal utility of well-being increased. If such a utility value for OP treatment reached its maximum of 9.8 and that for NOP treatment was 7.8 (marginal utility of well-being of 2.0), OP treatment cost an extra marginal CUR of $1196 (Figure 3A).
Figure 3.
Sensitivity analyses for marginal cost-utility ratio (ΔCUR) of operative (OP) treatment as opposed to nonoperative (Non-OP) treatment, implicating that OP treatment becomes increasingly cost-effective as its utility of well-being further exceeds Non-OP treatment and its rerupture rate minimizes, which could be the scenario of treating certain young, active athletes. (A) ΔCUR decreases as the utility of Non-OP treatment falls further behind OP treatment. (B) Decrease of ΔCUR as a function of increasing rerupture probability of Non-OP treatment compared with OP treatment. Note that in most scenarios, Non-OP treatment is still more cost-effective than OP treatment.
OP treatment cost an extra marginal CUR of $1475, assuming the probability of reruptures at the average values of 3.6% and 8.8%, respectively, for OP and NOP treatment. Sensitivity analyses, allowing for a greater advantage to OP treatment with regard to rerupture rates, decreased the marginal CUR. Even in the most favorable case, assuming a rerupture rate of 1.7% for OP treatment and 21.7% for NOP treatment, however, the marginal CUR was still $1388 (Figure 3B).
Discussion
This pilot analysis revealed that operative treatment of acute Achilles tendon ruptures had a higher incremental cost per utility gained but also higher expected utility value upon uneventful healing compared with nonoperative treatment. On average, nonoperative treatment was more cost-effective. Operative treatment became increasingly cost-effective as the utility of well-being increased: for example, with high-demand patients, such as athletes, or those in physically demanding occupations who prefer the highest possible functional outcome as early as possible.
Our study sought to provide novel information by incorporating actual cost data and updated outcome data into the decision analysis model. While the basic structure of the decision tree is similar to previous analyses,11 the probabilities of each outcome are expected to change over time because of advancement in either treatment option. In addition to the expected utility value alone, we integrated direct cost data with sensitivity analyses, accounting for potential heterogeneity among various patient populations and the associated variables.
Primary open repair for acute Achilles tendon ruptures may lead to favorable muscle strength in the first year after surgery16 and fewer days to return to sports4 or work.19 These benefits may not be supported by other reports, as some factors were measured differently in various sources in the literature and are thus difficult to compare. Primary open repair results in lower rates of reruptures, as reflected by the pooled rerupture rate in the most recent Cochrane review10 and by a level 1 systematic review.28 This may be of critical concern for active patients who need high athletic performance or a return to physically demanding occupations. Accordingly, operative treatment may reduce the societal costs resulting from underperformance or loss of work days.7
Nonoperative treatment is a cost-effective option and could be especially suitable for the general population that is not that active. Accelerated rehabilitation protocols with early weightbearing and range of motion progression can lead to decreased rerupture rates and similar objective outcomes as operative treatment.16,21,29 The complications associated with surgery become much less likely, as shown in the pooled probabilities of moderate and minor complications in the present study. The probability of certain major complications such as deep vein thrombosis remains similar. The advantage of avoiding wound complications may be offset in the near future by the advancement of percutaneous repair techniques13 that are relatively novel with emerging evidence to support promising midterm to long-term outcomes.5,12 A recent retrospective cohort analysis demonstrated that percutaneous repair could be more cost-effective than open repair,3 although more high-level analyses of its effectiveness, cost, and utility are needed.
Sensitivity analyses reflecting lower rerupture rates after primary surgical repair and higher rerupture rates after nonoperative treatment narrowed the cost advantage for nonoperative treatment, but only slightly, as shown in Figure 3B. Even under the scenario of a 20% higher rerupture rate after nonoperative treatment compared with primary surgical repair, operative treatment was still more expensive. However, while there is still variation regarding the rerupture rates of either treatment option in the literature, the difference in rerupture rates may be particularly important to certain patients depending on their lifestyle and expectations. In addition, the costs of managing reruptures after initial treatment, be it operative or nonoperative, can affect the overall cost-effectiveness should these costs be included in future analyses. Therefore, one should use caution in the interpretation of the results.
Surgical treatment for acute Achilles tendon ruptures was found to be cost-effective in a prospective randomized cohort study from Sweden.27 Using quality-adjusted life years (QALYs) as the measure for the effectiveness of treatment, the incremental cost-effectiveness ratio was €45,885 per QALY, resulting in a 57% likelihood for surgical treatment to be cost-effective based on the €50,000 threshold of willingness to pay for 1 QALY. The rerupture rate was 10% and 2.3% in their cohort, as opposed to 8.8% and 3.6% in the present study, for nonoperative and operative treatment, respectively. Further, the costs and health care infrastructure are distinct in different countries and may thus affect the cost-effectiveness of a variety of treatment strategies.
Nonoperative treatment may be favorable for cost minimization from the payer’s perspective based on a claims database in the US.20 The rates and associated costs of managing complications did not significantly differ between operative and nonoperative treatment. Based on claims data, there appeared to be a trend toward treating more of these Achilles tendon ruptures nonoperatively, whereas younger patients were more likely treated with surgery. These findings, although largely based on the claims that the payers processed and focused on costs only, resonated with our results, which were drawn from actual cost data integrated with utility scores for cost-effectiveness analyses.
Both QALY and utility values are common proxies to quantify the effectiveness of treatment in cost-effectiveness analyses. Because Achilles tendon ruptures do not directly affect life expectancy, using QALY requires the collection of subjective patient-reported outcomes, which may be essentially on par with the acquisition of utility values. The use of US$50,000 per QALY as the willingness-to-pay threshold in the US can be traced back to discussions in the 1970s on Medicare coverage for patients with end-stage renal disease.8 Revising such a threshold has been proposed to better reflect the current health care system and the needs of modern society.15 Further justification is needed for its use in orthopaedic surgical procedures, particularly when patients’ willingness to pay may widely vary based on their expected functional outcome, which is paramount in the practice of sports medicine as well as foot and ankle surgery.
The scenario of chronic Achilles tendon ruptures was not analyzed in the present study. These patients commonly require more complex procedures such as soft tissue flaps, tendon transfer or augmentation, or bridging materials.18,24–26 The cost of such procedures is presumably higher, and the outcome may be suboptimal compared with the treatment of acute ruptures. The cost-effectiveness of various treatment options in such a scenario may be difficult to assess because of a lack of sufficient case volume and homogeneity in the published literature.
Limitations
As a pilot investigation, the present study did have several limitations. First, the data of costs, utilities, and probabilities were not acquired from exactly the same patient population. Second, we assessed only the direct costs from the payers’ perspective and did not consider the societal costs attributed to loss of work days and school days alike. The outcome utility was populated from subjective patient reports and did not include quantitative measurements such as ankle push-off strength, which may affect athletic patients’ performance and thus place more emphasis on utility. Also, the cost data were from a single academic institution.
In addition, our decision model did not account for the full time horizon of each treatment arm, which may introduce additional costs resulting from further management of reruptures and other complications. The potential costs associated with complication management could be substantial, depending on the type of complication, the expected outcome, and the underlying medical condition of each patient. To date, there is insufficient high-level evidence to support secondary analyses assessing the cost-effectiveness of these complications. The results could differ if such costs were incorporated in the future.
Despite these limitations, we optimized the validity of this pilot study by incorporating data from the best available level 1 evidence as well as by performing multiway sensitivity analyses.
Future Directions
This analysis can serve as a foundation for future investigation. The decision tree could further expand based on this economic decision model, as more high-level evidence becomes available regarding the cost and utility of complication management as well as percutaneous Achilles tendon repair procedures.
Conclusion
While practicing cost-effective medicine, optimizing outcomes as they relate to patients’ expectations for their work and life should remain the surgeon’s top priority. In the current study, nonoperative treatment was cost-effective for the average patient population. This remained true when the expected utility value decreased, as in patients with lower physical demands, as well as when the surgical complication rates increased, as in patients with medical comorbidities. Primary open repair was less cost-effective in the average scenario. However, its cost-effectiveness increased when a higher utility value was expected, as in young athletes or patients with higher physical demands.
APPENDIX
Probability Data Acquisition
POP-wellavg and PNOP-wellavg, which represented the average probabilities of the well-being terminal node for the OP and NOP arms, respectively, were determined by the following:
The minimal probabilities of well-being, POP-wellmin and PNOP-wellmin, were determined by the “maximal” probabilities of the other 4 terminal nodes and vice versa:
Utility Data Acquisition
The average utility values for the OP and NOP arms were designated as UOP-wellavg, UOP-rerupavg, UOP-maavgj, UOP-modavg, and UOP-mnravg, respectively, and UNOP-wellavg, UNOP-rerupavg, UNOP-majavg, UNOP-modavg, and UNOP-mnravg, respectively. The range of such utility values was designated as UOP-wellmin, UOP-rerupmin, UOP-majmin, UOP-modmin, UOP-mnrmin, UOP-wellmax, UOP-rerupmax, UOP-majmax, UOP-modmax, and UOP-mnrmax, respectively, and UNOP-wellmin, UNOP-rerupmin, UNOP-majmin, UNOP-modmin, UNOP-mnrmin, UNOP-wellmax, UNOP-rerupmax, UNOP-majmax, UNOP-modmax, and UNOP-mnrmax, respectively, for the OP and NOP arms.
Cost Data Acquisition
The average and range of direct costs of OP and NOP treatment were represented by COPavg, COPmin, and COPmax as well as CNOPavg, CNOPmin, and CNOPmax, respectively.
Multiway Sensitivity Analyses for Boundary Conditions
For example, the highest possible CUR for OP treatment was determined as follows:
The range of CURs for the OP and NOP arms was then determined accordingly.
Footnotes
Final revision submitted October 27, 2019; accepted December 17, 2019.
One or more of the authors has declared the following potential conflict of interest or source of funding: L.B. has received educational support from Elite Orthopaedics and hospitality payments from Arthrex and Smith & Nephew. J.J. has received educational support from Arthrex, consulting fees from Tornier and Wright Medical, speaking fees from Arthrex, royalties from Tornier and Wright Medical, and hospitality payments from Stryker. M.J.M. has received educational support from Arthrex, Breg, and Elite Orthopaedics; consulting fees from Arthrex, Heron Therapeutics, Pacira, and Schwartz Biomedical; and speaking fees from Arthrex. J.M. has received educational support from Elite Orthopaedics, consulting fees from Wright Medical, and speaking fees from Arthrex and Wright Medical. M.V.S. has received educational support from Elite Orthopaedics, consulting fees from Arthrex and Flexion Therapeutics, and speaking fees from Arthrex. R.W.W. has received royalties from Responsive Arthroscopy. R.H.B. has received educational support from Arthrex and Elite Orthopaedics; consulting fees from Arthrex, ISTO Technologies, and Sanofi-Aventis; and speaking fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Washington University in St Louis (No. 201610143).
References
- 1. Barfod KW, Bencke J, Lauridsen HB, Ban I, Ebskov L, Troelsen A. Nonoperative dynamic treatment of acute Achilles tendon rupture: the influence of early weight-bearing on clinical outcome. A blinded, randomized controlled trial. J Bone Joint Surg Am. 2014;96(18):1497–1503. [DOI] [PubMed] [Google Scholar]
- 2. Brumann M, Baumbach SF, Mutschler W, Polzer H. Accelerated rehabilitation following Achilles tendon repair after acute rupture: development of an evidence-based treatment protocol. Injury. 2014;45(11):1782–1790. [DOI] [PubMed] [Google Scholar]
- 3. Carmont MR, Heaver C, Pradhan A, Mei-Dan O, Gravare Silbernagel K. Surgical repair of the ruptured Achilles tendon: the cost-effectiveness of open versus percutaneous repair. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1361–1368. [DOI] [PubMed] [Google Scholar]
- 4. Cetti R, Christensen SE, Ejsted R, Jensen NM, Jorgensen U. Operative versus nonoperative treatment of Achilles-tendon rupture: a prospective randomized study and review of the literature. Am J Sports Med. 1993;21(6):791–799. [DOI] [PubMed] [Google Scholar]
- 5. Cretnik A, Kosanovic M, Kosir R. Long-term results with the use of modified percutaneous repair of the ruptured Achilles tendon under local anaesthesia (15-year analysis with 270 cases). J Foot Ankle Surg. 2019;58(5):828–836. [DOI] [PubMed] [Google Scholar]
- 6. Erickson BJ, Cvetanovich GL, Nwachukwu BU, et al. Trends in the management of Achilles tendon ruptures in the United States Medicare population, 2005-2011. Orthop J Sports Med. 2014;2(9):2325967114549948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Erickson BJ, Mascarenhas R, Saltzman BM, et al. Is operative treatment of Achilles tendon ruptures superior to nonoperative treatment? A systematic review of overlapping meta-analyses. Orthop J Sports Med. 2015;3(4):2325967115579188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grosse SD. Assessing cost-effectiveness in healthcare: history of the $50,000 per QALY threshold. Expert Rev Pharmacoecon Outcomes Res. 2008;8(2):165–178. [DOI] [PubMed] [Google Scholar]
- 9. Guss D, Smith JT, Chiodo CP. Acute Achilles tendon rupture: a critical analysis review. JBJS Rev. 2015;3(4):e2. [DOI] [PubMed] [Google Scholar]
- 10. Jones MP, Khan RJ, Carey Smith RL. Surgical interventions for treating acute Achilles tendon rupture: key findings from a recent Cochrane review. J Bone Joint Surg Am. 2012;94(12):e88. [DOI] [PubMed] [Google Scholar]
- 11. Kocher MS, Bishop J, Marshall R, Briggs KK, Hawkins RJ. Operative versus nonoperative management of acute Achilles tendon rupture: expected-value decision analysis. Am J Sports Med. 2002;30(6):783–790. [DOI] [PubMed] [Google Scholar]
- 12. Makulavicius A, Mazarevicius G, Klinga M, et al. Outcomes of open “crown” type v. percutaneous Bunnell type repair of acute Achilles tendon ruptures: randomized control study [published online August 3, 2019]. Foot Ankle Surg. doi:10.1016/j.fas.2019.07.011 [DOI] [PubMed] [Google Scholar]
- 13. Metz R, Verleisdonk EJMM, van der Heijden GJMG, et al. Acute Achilles tendon rupture: minimally invasive surgery versus nonoperative treatment with immediate full weightbearing. A randomized controlled trial. Am J Sports Med. 2008;36(9):1688–1694. [DOI] [PubMed] [Google Scholar]
- 14. Möller M, Movin T, Granhed H, Lind K, Faxen E, Karlsson J. Acute rupture of tendon Achillis: a prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Joint Surg Br. 2001;83(6):843–848. [DOI] [PubMed] [Google Scholar]
- 15. Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness: the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–797. [DOI] [PubMed] [Google Scholar]
- 16. Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. Acute Achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38(11):2186–2193. [DOI] [PubMed] [Google Scholar]
- 17. Nistor L. Surgical and non-surgical treatment of Achilles tendon rupture: a prospective randomized study. J Bone Joint Surg Am. 1981;63(3):394–399. [PubMed] [Google Scholar]
- 18. Porter MD, Shadbolt B. Randomized controlled trial of accelerated rehabilitation versus standard protocol following surgical repair of ruptured Achilles tendon. ANZ J Surg. 2015;85(5):373–377. [DOI] [PubMed] [Google Scholar]
- 19. Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2012;94(23):2136–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Truntzer JN, Triana B, Harris AHS, Baker L, Chou L, Kamal RN. Cost-minimization analysis of the management of acute Achilles tendon rupture. J Am Acad Orthop Surg. 2017;25(6):449–457. [DOI] [PubMed] [Google Scholar]
- 21. Twaddle BC, Poon P. Early motion for Achilles tendon ruptures: is surgery important? A randomized, prospective study. Am J Sports Med. 2007;35(12):2033–2038. [DOI] [PubMed] [Google Scholar]
- 22. Uquillas CA, Guss MS, Ryan DJ, Jazrawi LM, Strauss EJ. Everything Achilles: knowledge update and current concepts in management. AAOS Exhibit Selection. J Bone Joint Surg Am. 2015;97(14):1187–1195. [DOI] [PubMed] [Google Scholar]
- 23. Valkering KP, Aufwerber S, Ranuccio F, Lunini E, Edman G, Ackermann PW. Functional weight-bearing mobilization after Achilles tendon rupture enhances early healing response: a single-blinded randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1807–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Villarreal AD, Andersen CR, Panchbhavi VK. A survey on management of chronic Achilles tendon ruptures. Am J Orthop (Belle Mead NJ). 2012;41(3):126–131. [PubMed] [Google Scholar]
- 25. Wapner KL, Hecht PJ, Mills RH., Jr Reconstruction of neglected Achilles tendon injury. Orthop Clin North Am. 1995;26(2):249–263. [PubMed] [Google Scholar]
- 26. Wapner KL, Pavlock GS, Hecht PJ, Naselli F, Walther R. Repair of chronic Achilles tendon rupture with flexor hallucis longus tendon transfer. Foot Ankle. 1993;14(8):443–449. [DOI] [PubMed] [Google Scholar]
- 27. Westin O, Svensson M, Nilsson Helander K, et al. Cost-effectiveness analysis of surgical versus non-surgical management of acute Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):3074–3082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wilkins R, Bisson LJ. Operative versus nonoperative management of acute Achilles tendon ruptures: a quantitative systematic review of randomized controlled trials. Am J Sports Med. 2012;40(9):2154–2160. [DOI] [PubMed] [Google Scholar]
- 29. Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92(17):2767–2775. [DOI] [PubMed] [Google Scholar]
- 30. Young SW, Patel A, Zhu M, et al. Weight-bearing in the nonoperative treatment of acute Achilles tendon ruptures: a randomized controlled trial. J Bone Joint Surg Am. 2014;96(13):1073–1079. [DOI] [PubMed] [Google Scholar]