Since December 2019, an outbreak of 2019 coronavirus disease (COVID-19) in Wuhan, Hubei Province, China has raised worldwide concern as it spiraled into a pandemic [1]. By Feb 29, 2020, there were more than 75,000 confirmed cases of COVID-19 in China [2]. The Fifth Affiliated Hospital of Sun Yat-sen University, as one of the biggest tertiary hospital serving for millions people, set up COVID-19-associated departments which were consisted of a 24-h fever clinic, a number of isolation wards as well as one Intensive Care Unit (ICU) for suspected infection patient and confirmed cases and undertook nearly 100 cases in Guangdong Province, a province whose cases numbered second only to Hubei Province in China.
Confronted this sudden public health crisis, Chinese doctors and nurses were under considerable psychological pressure. Mental health of the medical staff was assessed at the Fifth Affiliated Hospital of Sun Yat-sen University using Zung's self-rating depression scale (SDS) and Zung's self-rating anxiety scale (SAS).
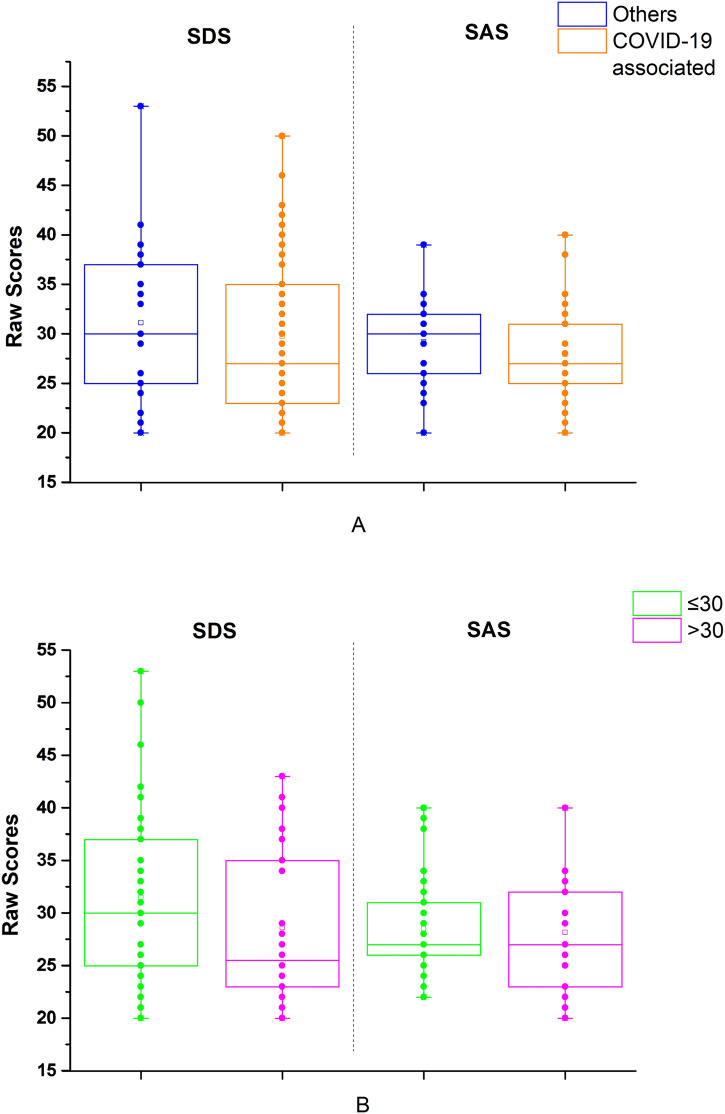
Our study was approved by the Research Ethics Committee of the Fifth Affiliated Hospital of Sun Yat-sen University (approve number K17–1). All participants provided written informed consent. We analyzed SDS and SAS raw scores of 23 doctors and 36 nurses from COVID-19-associated departments (38 participants) and others (21 participants), including Department of Pulmonary and Critical Care Medicine (PCCM), Department of Cardiology and General ICU, from 3 to 21, February 2020 (Fig. 1 ). As illustrated, several staff were experiencing clinically signficiant depressive symptoms according to established thresholds [3]. There were no significant differences in scores between staff in COVID-19-associated andother departments (Fig. 1A, t-test, tSDS = 0.77, dfSDS = 95, P SDS = 0.44; t-test, tSAS = 1.03, dfSAS = 95, P SAS = 0.31). Younger (age ≤ 30) medical staff had higher SDS scores than older staff but this difference was not statistically signficant. (Fig. 1 B, t-test, tSDS = 1.64, dfSDS = 83, P SDS = 0.11; t-test, tSAS = 0.31, dfSAS = 83, P SAS = 0.76). (Table 1 ).
Fig. 1.
Raw scores of various departments or ages. (A) Orange is the medical staffs of COVID-19-associated departments and the blue represents other departments. Dots represents each doctor or nurse raw score. SDS raw scores are on the left of the dashed line and the SAS scores are on the right. (B) Green is medical staffs under 30 years old and the magenta represents over 30 years old. Dots represents each doctor or nurse raw score. SDS raw scores are on the left of the dashed line and the SAS scores are on the right. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Table 1.
Average SDS and SAS raw scores.
| Age | Raw score | COVID-19 associated department (n = 38) | Other departments (n = 21) | t-test (t, df, P) |
|---|---|---|---|---|
| ≤30 (n = 33) |
SDS | 30.05 ± 8.16 | 34.09 ± 8.97 | 1.30, 31, 0.21 |
| SAS | 28.09 ± 4.98 | 29.36 ± 4.46 | 0.76, 31, 0.46 | |
| >30 (n = 26) | SDS | 29.06 ± 7.87 | 27.9 ± 5.86 | 0.40,24, 0.69 |
| SAS | 27.63 ± 6.34 | 29 ± 4.5 | 0.60, 24. 0.56 | |
| t-test (t, df, P) | SDS | 0.37, 36, 0.71 | 1.85, 19, 0.08 | – |
| SAS | 0.26, 36, 0.79 | 0.19, 19, 0.85 | – |
Raw score were present as mean ± standard deviation.
Our results are a reminder not to neglect the mental health of the other medical department staff during the pandemic, including younger medical staff. Intervention including daily living supplies, pre-job training, leisure activities and psychological counseling like the Second Xiangya Hospital of Central South University advised, were also ongoing in our hospital [4]. Reasonable resting for medical staff may also help relieve stress according to our experience. It's essential for medical staff to keep physical and psychological health during our struggle of COVID-19. SDS and SAS were simple = tools to monitoring the self-mental health [5].
Disclosure
The authors report no conflicts of interest in this work. All authors have read and approved the manuscript.
Acknowledgments
Acknowledgement
This work was supported by the Emergency project of clinical research on the prevention and treatment of COVID-19 with traditional Chinese medicine from Guangdong provincial bureau of traditional Chinese medicine, China (grant numbers 2020ZYYJ16).
References
- 1.Wang C., Horby P.W., Hayden F.G. A novel coronavirus outbreak of global health concern. Lancet. 2020 doi: 10.1016/S0140-6736(20)30185-9. (published online Jan 24) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Health Commission of the People'’s Republic of China By 24:00 on 9 February, The Latest Situation of New Coronavirus Pneumonia. 2020. http://www.nhc.gov.cn/xcs/yqtb/202002/543cc508978a48d2b9322bdc83daa6fd.shtml (accessed Feb 22, 2020)
- 3.Zung W.W.K. From art to science: the diagnosis and treatment of depression. Arch. Gen. Psychiatry. 1973;29:328–337. doi: 10.1001/archpsyc.1973.04200030026004. [DOI] [PubMed] [Google Scholar]
- 4.Chen Qiongni, Liang Mining, Li Yamin. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30078-X. published Online February 18, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zung W.W.K. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]