Abstract
Despite considerable advancements in medicine, the optimal treatment for chronic kidney disease (CKD), especially diabetic kidney disease (DKD), remains a major challenge. More patients with DKD succumb to death due to cardiovascular events than due to progression to end-stage renal disease (ESRD). Moreover, patients with DKD and ESRD have remarkably poor prognosis. Current studies have appreciated the contribution of inflammation and inflammatory mediators, such as tumor necrosis factor (TNF)-related biomarkers, on the development/progression of DKD. The present review focuses on molecular roles, serum concentrations of TNF receptors (TNFRs), and their association with increased albuminuria, eGFR decline, and all-cause mortality in diabetes. Experimental studies have suggested that DKD progression occurs through the TNFα–TNFR2 inflammatory pathway. Moreover, serum TNFR levels were positively associated with albuminuria and negatively associated with estimated glomerular filtration rate (eGFR), while circulating levels of TNFRs exhibited an independent effect on all-cause mortality and eGFR decline, including ESRD, even after adjusting for existing risk factors. However, their precise function has yet to be elucidated and requires further studies.
Keywords: TNFα, TNF receptor, biomarker, diabetic kidney disease
1. Introduction
A total of 850 million individuals suffer from kidney disease worldwide, with one in 10 adults possibly being at risk. Diabetic kidney disease can progress to end-stage renal disease (ESRD), a condition necessitating renal replacement therapy. Diabetic kidney disease (DKD) has been one of the most significant diseases given its relationship with both progression to ESRD and morbidity and mortality from cardiovascular diseases [1]. To prevent ESRD, identifying patients at high risk for progression of DKD at an early stage and providing intensive treatment are imperative. Highly sensitive biomarkers are required to identify such patients. In classical diabetic nephropathy, the earliest clinical sign is moderately increased albuminuria (microalbuminuria: 30–300 mg/g creatinine). However, albuminuria may be a less accurate predictor of nephropathy risk than initially thought [2]. In addition, some patients with diabetes have reduced kidney function while maintaining normo- or microalbuminuria [3].
Recently, growing evidence has highlighted the importance of inflammation in the development and progression of DKD [4]. Accordingly, increased expression of cell adhesion molecules, chemokines, and inflammatory cytokines have been observed in the kidneys of patients with diabetes. Moreover, studies have determined that tumor necrosis factor alpha (TNFα) is a well-known inflammatory cytokine associated with the progression of kidney disease [5]. Two types of TNF receptors (TNFRs) exist, TNFR1 and TNFR2, both of which have cleaved and solubilized extracellular domains (soluble TNFR1 (sTNFR1) and sTNFR2) [6]. sTNFR1 and sTNFR2 are not deviating enzymes appearing after cytolysis but rather appear in the blood at the initial stage of inflammation.
The present review therefore describes the role of chronic inflammation in the pathogenesis of DKD, focuses on the relationship between TNF–TNFR signaling and DKD progression, and highlights the utility of TNFRs as a biomarker.
2. Inflammation and Diabetic Kidney Disease
Studies have shown that hyperglycemia, oxidative stress, glycation end products, glomerular hypertension, and chronic inflammation are associated with DKD progression [7,8]. Given that the inflammation observed with DKD has been considered quite mild compared to that with classic inflammatory diseases, it has been referred to as “microinflammation” in order to distinguish it from the other classic inflammation [9].
Inflammation involves a myriad of factors, including inflammatory cytokines, chemokines, adhesion molecules, innate immunity, and transcription factors. Inflammatory cytokines, such as interleukin (IL) -1, IL-6, IL-18, and TNFα, have been associated with DKD through recruitment of inflammatory cells, such as monocytes and macrophages [10]. Monocyte chemoattractant protein-1 acts on monocyte–macrophage receptors to aggregate monocytes in tissues. They subsequently adhere to endothelial cells through intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 and then infiltrate into the tissues [11]. Macrophage infiltration into the glomerulus and tubulointerstitium causes chronic inflammation and fibrosis. In addition to these mechanisms, hyperglycemia activates many transcription factors, including nuclear factor-κB (NF-κB), which is involved in chronic inflammation [12]. As such, aggravated microinflammation in the kidney causes expansion into the mesangial and tubulointerstitial lesion with extracellular matrix accumulation [13].
Numerous inflammatory mediators have been investigated to assess their potential utility as biomarkers and/or molecular targets for DKD [9]. Although TNFα has been implicated in the pathogenesis of DKD, recent clinical observational studies have suggested that TNFRs were better biomarkers of renal function decline compared to TNFα [14].
3. Expression and Signaling Pathway of Tumor Necrosis Factor Alpha and Tumor Necrosis Factor Receptors
TNFα is a type II transmembrane protein that exists mainly in membrane-bound form (mTNFα) with a relative molecular weight of 26 kDa [15]. It is cleaved by disintegrin and metalloprotease protein 17 (ADAM-17), also called TNFα converting enzyme (TACE), releasing a functional soluble form (17 kDa) into the circulation [16]. This cleaved and solubilized TNFα is called soluble TNFα (sTNFα), while that measured in circulating plasma is referred to as circulating sTNFα [17,18]. Both sTNFα and mTNFα are active as non-covalently bound homotrimers.
TNFα has been known to have two different receptors, TNFR1 (TNFRSF1A, CD120a, p55) and TNFR2 (TNFRSF1B, CD120b, p75), with molecular weights of 55 and 75 kDa, respectively. These two receptors are typical representatives of the TNFR superfamily (TNFRSF). The TNFRSF falls into death receptors, decoy receptors, and activating receptors. Death receptors activate the caspase cascade via the death domain (DD)-initiating extrinsic apoptotic pathway. Most activating receptors mediate intracellular signals through TNF receptor-related factors (TRAFs) [19]. TNFR1 and TNFR2 are type I transmembrane proteins characterized by cysteine-rich motifs in the extracellular domain [20]. The intracellular segments of TNFR1 and TNFR2 have no homologous sequences and activate distinct signaling pathways [15,21].
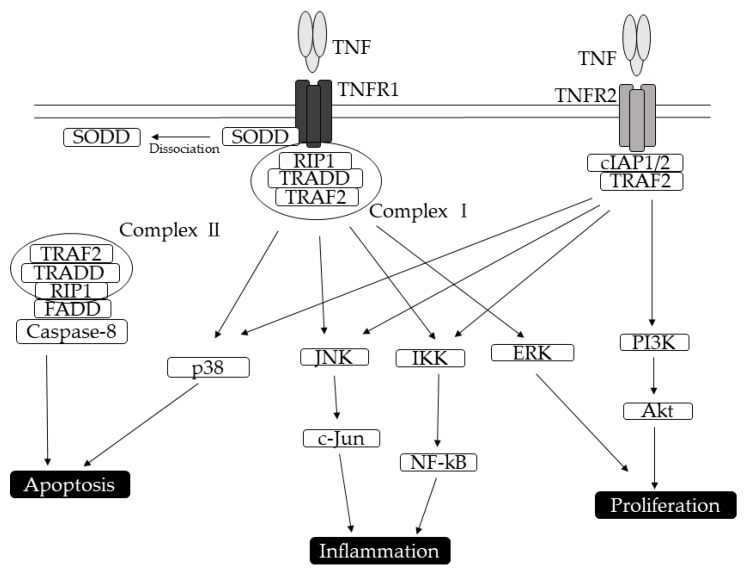
TNFR1 is ubiquitously expressed on almost all cell types [22]. In the kidneys, TNFR1 is mainly present in glomerular and tubular endothelial cells. The binding of TNFα to TNFR1 has been widely known to activate two different signaling pathways, mediate apoptosis, and regulate inflammation (Figure 1). TNFR1, which can be activated by both mTNFα and sTNFα, contains a homologous cytoplasmic region called DD. In the absence of a ligand, TNFR1 can interact with a cytoplasmic protein-containing DD domain called the silencer of death domain (SODD) [23,24]. The ligand-bound TNFR1 preferentially interacts with the DD-containing adaptor protein called the TNFR-associated death domain (TRADD) [25], which can replace the SODD. TRADD binds the Ser/Thr kinase receptor-interacting protein 1 and TRAF-2, forming complex I [26]. Complex I can trigger the activation of NF-κB, which functions as a transcription factor, as well as activate stress-activated MAP kinase (MAPK), p38, c-Jun N-terminal kinase, extracellular signal-regulated kinase, and other transcription factors via the MAPK3 signaling pathway [27,28,29]. Given that complex I formation is temporary, TRADD dissociates from TNFR1 and associates with the Fas-associated DD protein and caspase-8 to form complex II for caspase activation [30,31].
Figure 1.
Pathways induced by tumor necrosis factor receptors (TNFRs). TNFR1 and TNFR2 activate shared and divergent signaling pathways and downstream cellular responses that lead to apoptosis, proliferation, and inflammatory mediators. The initial step in TNF-TNFR1 signaling involves the release of the inhibitory protein silencer of death domains (SODD) from TNFR1 intracellular domain. Subsequently, TNFR1 recruits distinct adaptor molecules TNFR-associated death domain (TRADD), TNFR-associated factor 2 (TRAF-2), receptor-interacting protein (RIP) at the intracellular death domain, thereby activating NF-κB-signaling, MAPK/c-Jun-signaling, and caspase-signaling. After binding of TNFα, TNFR2 intracellular domains recruit existing cytoplasmic TRAF2–cIAP1–cIAP2 complexes. TNFR2 activation leads to PI3K/Akt and NF-κB activation.
TNFR2, the expression of which is mainly restricted to immune and endothelial cells [32], is not usually present in the kidneys of healthy subjects [6,33]. Moreover, TNFR2 has a high affinity for membrane-bound forms of cytokines. Unlike TNFR1, TNFR2 does not have a DD in the intracellular region, suggesting the activation of a different downstream transduction pathway [34]. TNFR2 lacks the ability to recruit TRADD but can interact directly with TRAF [35]. When TNFα binds to TNFR2, the intracellular domain recruits the existing cytoplasmic TRAF-2–cIAP-1–cIAP-2 complex [15,36]. cIAPs exert ubiquitin ligase activity and can inhibit caspases and other apoptosis-inducing factors, leading to the initiation of NF-κB activation [26,36,37]. Considering that both TNFR1 and TNFR2 signals activate NF-κB, they may not be distinguished through NF-κB activation. The interaction between TNFα and TNFR2 also activates the reciprocal PI3K–Akt pathway.
As mentioned above, both TNFR1 and TNFR2 membrane receptors can also be converted to soluble forms (sTNFR1 and sTNFR2) through TACE activity [13,15]. sTNFRs inhibit TNFα by competing with cellular receptors for TNFα binding and perhaps also by acting as dominant-negative molecules. While low concentrations of sTNFRs enhanced TNFα action, higher concentrations abrogated the effects of TNFα [38]. Given that serum TNFR levels are 100–500 times higher than serum TNFα levels, circulating TNFRs might have additional functions aside from being a TNFα-binding protein.
4. Circulating Tumor Necrosis Factor Receptors: Predictive Biomarker for Diabetic Kidney Disease Progression among Patients with Diabetes
Companion studies published in 2012 by Krolewski et al. in the Journal of the American Society of Nephrology had been the first to show that circulating soluble TNFR levels predicted future renal function decline among patients with both types of diabetes over a wide variety of stages [39,40]. Patients with type 1 diabetes whose circulating TNFR2 levels were in the highest quartile had a 55% cumulative incidence of reaching stage 3 CKD, whereas those with TNFR2 levels in the lower three quartiles had a 15% cumulative incidence after 12 years of follow-up in the early stages of DKD (normal renal function and normo- or microalbuminuria). Furthermore, another study comprising patients with type 2 diabetes, including advanced DKD (stage 3 CKD and/or macroalbuminuria), showed that patients with TNFR1 levels in the highest quartile had a nearly 80% cumulative incidence of progressing to ESRD after 12 years of follow-up, whereas those with TNFR1 levels in the lowest three quartiles had <20% cumulative incidence. Thus, circulating TNFRs levels have been considered useful predictors for renal function decline after adjusting for relevant factors, such as baseline estimated glomerular filtration rate (eGFR), albuminuria, and hemoglobin A1c. Although circulating TNFRs levels also predicted cardiovascular and all-cause mortality, its predictive ability for such conditions was weaker than that for ESRD. The same study group showed that circulating TNFR2 levels also predicted the risk for ESRD among patients with type 1 diabetes and macroalbuminuria [41]. The rate of eGFR loss was especially steep among patients with increased TNFR2 and hemoglobin A1c levels.
Among patients with classical type 1 diabetes, elevated albuminuria (macroalbuminuria) has been considered to precede the development of decreased GFR (i.e., the onset of microalbuminuria leads to macroalbuminuria, followed by progressive GFR decline, and eventually ESRD). However, one study first explicated the novel model that significant GFR decline precedes the stage of microalbuminuria (n = 86, 35%) or had already started from the stage of normoalbuminuria (n = 28, 10%) in the subset of patients with type 1 diabetes (normoalbuminuria: n = 286, microalbuminuria: n = 248) within 4–10 years of follow-up [42]. Among such patients, who were called early progressive decliners, circulating TNFRs levels were associated with early progressive renal decline (eGFRcr-cys loss ≥ 3.3%/year).
Pavkov et al. presented further evidence on the utility of circulating TNFRs by investigating the association between TNFRs levels and ESRD using a very unique cohort of American Indians (Pima Indians) with type 2 diabetes [43]. Notably, the GFR used in the aforementioned study was estimated using the urinary clearance of iothalamate and not a serum creatinine-based predictive equation. The study comprised patients with relatively good renal function (median measured GFR of 120 mL/min/1.73 m2, with 89% of the patients having normal renal function). However, 32% of the patients developed ESRD within a relatively short period (a median follow-up of 9.5 years), indicating the considerably high risk for progression to ESRD among such cohort. Nevertheless, both TNFR levels predicted the development of ESRD in patients with type 2 diabetes, most of whom were able to preserve renal function. Furthermore, the aforementioned study showed that elevated TNFRs levels were associated with decreased percentage of normal a endothelial cell fenestration and increased mesangial fractional volume in Pima Indians with type 2 diabetes and normal renal function, suggesting that TNFRs might be associated with early glomerular lesion in diabetes [44].
Niewczas et al. [45] recently published a study regarding TNFR, wherein they measured 194 circulating inflammatory proteins using aptamer-based proteomics analysis (Slow Off-rate Modified Aptamer scan) in multiple cohorts consisting of a discovery (advanced stage of type 1 diabetes Joslin cohort), validation (advanced stage of type 2 diabetes Joslin cohort), and replication cohort (early stage of type 2 diabetes Pima Indians cohort). Accordingly, they found that 12% of the 194 measured proteins were TNFR superfamily-related proteins. Moreover, they showed that six TNFR superfamily-related proteins, including TNFR1 and TNFR2, were strong predictors of early and late renal function, leading to ESRD, in both types of diabetes.
A number of similar studies from many reputable institutions around the world have based their study on the publication by the Joslin Diabetes Center (Table 1). Overall, the measurement of circulating TNFRs has been proven to be highly effective for predicting progression to renal function decline or ESRD among patients with diabetes. The results of a recent meta-analysis also showed a substantial relation between elevated TNFRs levels and DKD progression in more than 5000 patients with diabetes [46].
Table 1.
Characteristics of clinical studies, diabetic kidney disease-related outcome, and circulating tumor necrosis factor receptor levels in patients with type 1 and type 2 diabetes.
| Outcome | References | Type | n | Included Study Patients | ACR or AER | GFR (mL/min/1.73 m2) | Follow Up (Year) | Findings (HR (95%CI), C Index, AUC) |
|---|---|---|---|---|---|---|---|---|
| ESRD | Niewczas et al. [40] | 2 | 410 | eGFR >30 mL/min/1.73 m2 Normo, Micro, Macro |
NA | eGFR >30 | 8–12 | TNFR1: 9.4 (2.8–31.6) TNFR2: 7.6 (2.7–21.6) Per increase of interquartile range |
| ESRD | Forsblom et al. [47] | 1 | 429 | eGFR <60 mL/min/1.73 m2: 54% Macro (100%) |
NA | NA | 9.4 | GFR+HbA1c+DM duration (Model 1): 0.72, 0.63 Model 1+TNFR1: 0.86, 0.81 C index and AUC, respectively |
| ESRD | Pavkov et al. [43] | 2 | 193 | eGFR >60 mL/min/1.73 m2: 89% Normo (32%), Micro (37%), Macro (31%) |
72 (19, 493) mg/g | 120 (88, 149) | 9.5 | TNFR1: 1.6 (1.1–2.2) TNFR2: 1.7 (1.2–2.3) Per increase of interquartile range |
| Time to ESRD | Skupien et al. [41] | 1 | 349 | eGFR > 30 mL/min/1.73 m2 Macro (100%) |
771 (471, 1377) mg/g | 81 (55, 104) | 5–18 | TNFR2: −34.6% Per increase of interquartile range |
| eGFR loss >3.3%/year | Krolewski et al. [42] | 1 | 534 | eGFR > 60 mL/min/1.73 m2 Normo (n = 286) Micro (n = 248) |
Normo: 16 (12–22) mg/min Micro: 65 (44–116) mg/min |
Normo: 113 (102, 123) Micro: 112 (96, 122) |
4–10 | TNFR1: 2.9 (1.9–4.5) Per 200 pg/mL increase in biomarker |
| eGFR of >40% from baseline eGFR | Saulnier et al. [48] | 2 | 1135 | eGFR > 30 mL/min/1.73 m2 Normo (45%), Micro (36%), Macro (19%) |
3 (1–10) mg/mmol | 76 ± 21 | 4.3 | TNFR1: 1.69 (1.47–1.95) Per 1 SD increase in biomarker |
| eGFR of >40% from baseline eGFR | Coca et al. [49] | 2 | 380 | eGFR > 60 mL/min/1.73 m2 Case (50%), Control (50%) |
Case: 21 (8, 66) mg/g Control: 20 (8, 102) mg/g |
Case: 87 (77, 94) Control: 90 (79, 95) |
5 | TNFR1: 2.4 (1.5–4.0) TNFR2: 3.2 (1.7–6.1) Per doubling in biomarker |
| Composite renal outcome 1 | Coca et al. [49] | 2 | 1156 | eGFR 30–89.9 mL/min/1.73 m2 Macro (100%) |
NA | NA | 2.2 | TNFR1: 2.4 (1.7–3.3) TNFR2: 2.0 (1.4–2.8) Per doubling in biomarker |
| Composite renal outcome 2 | Barr et al. [50] | 2 | 194 | eGFR > 15 mL/min/1.73 m2 | NA | NA | 3 | TNFR1: 3.8 (1.1–12.8) Per doubling in biomarker |
| Stage 3 CKD | Gohda et al. [39] | 1 | 628 | eGFR > 60 mL/min/1.73 m2 Micro (n = 275) Normo + Micro (n = 353) |
Micro: 56 (37, 101) mg/mL Normo + Micro: 41 (24, 79) mg/mL |
Micro: 133 ± 30 Normo + Micro: 129 ± 30 |
Micro: 10–12 Normo + Micro: 5–7 |
TNFR1: 2.5 (1.4–4.7) TNFR2: 3.0 (1.7–5.5) Quartile 4 versus Quartiles 1–3 |
| Mortality | Niewczas et al. [40] | 2 | 410 | eGFR > 30 mL/min/1.73 m2 Normo, Micro, Macro |
NA | eGFR >30 | 8–12 | TNFR1: 1.6 (1.2–2.1) TNFR2: 1.6 (1.3–2.0) Per increase of interquartile range |
| Mortality | Saulnier et al. [51] | 2 | 522 | eGFR < 60 mL/min/1.73 m2, Micro, or Macro | 29 (111) mg/mmol* | 49 ± 23 | 4 | TNFR1: 3.0 (1.7–5.2) Quartile 4 versus Quartile 1 |
| Mortality | Carlsson et al. [52] | 2 | 607 | eGFR < 60 mL/min/1.73 m2: 10% Micro (10%) |
0.6 (0.5–0.7) g/mol** | 77 (75–78)** | 7.6 | TNFR1: 1.8 (1.4–2.1) TNFR1: 1.5 (1.1–1.9) Per 1 SD increase in biomarker |
Data are presented as mean ± standard deviation (SD), median (quartiles or interquartile range* or Bonett–Price 95% confidence intervals**); n, Number of patients. ACR, albumin/creatinine ratio; AER, albumin excretion rate; AUC, area under the ROC curve; CKD, chronic kidney disease; CI, confidence interval; ESRD, end-stage renal disease; GFR, glomerular filtration rate; HR, hazard ratio; Macro, macroalbuminuria; Micro, microalbuminuria; Normo, normoalbuminuria; NA, not applicable; ROC, receiver operating characteristic curve. Composite renal outcome 1: eGFR of >40% from baseline eGFR or an absolute decrease of >30 mL/min/1.73 m2 if the eGFR was <60 mL/min/ 1.73 m2 at randomization. Composite renal outcome 2: initial >30% decline in eGFR with a follow-up eGFR of <60 mL/min/1.73 m2, progression to renal replacement therapy, or renal death.
5. Circulating Tumor Necrosis Factor Receptors: A Predictive Biomarker for All-Cause Mortality among Patients with Diabetes or Undergoing Hemodialysis
Saulnier et al. [51] examined the association between circulating TNFR1 levels and all-cause mortality in 522 patients with type 2 diabetes and DKD (eGFR < 60 mL/min/1.73 m2 and/or albumin/creatinine 30 mg/mmol) using a follow-up study of Survie, Diabete de type 2 et Genetique (SURDIAGENE). Accordingly, they demonstrated that patients with TNFR1 levels in the highest quartile (15.9% patient-years) had around three times higher incidence of mortality compared to those with TNFR1 levels in the lowest quartile (4.7% patient-years) after 4 years of follow-up. Compared to the Joslin Study of the Genetics of Type 2 Diabetes and Kidney Complications, the SURDIAGENE study had a much higher incidence of mortality (Table 2), which might be attributed in part to clinical characteristics (SURDIAGENE patients were older and had lower eGFR compared to Joslin patients), although the impact of circulating TNFR1 levels on ESRD was extremely similar with both studies.
Table 2.
Incidence rate of end-stage renal disease and all-cause mortality among patients with type 2 diabetes in the Joslin and SURDIAGENE study [40,51].
| Joslin | SURDIAGENE | Joslin | SURDIAGENE | ||
|---|---|---|---|---|---|
| n = 410 | n = 500 | n = 410 | n = 522 | ||
| Outcome | ESRD | Mortality | |||
| TNFR1 | Q1 | 0 | 0 | 12 | 47 |
| Q2 | 0 | 4 | 13 | 77 | |
| Q3 | 6 | 10 | 26 | 93 | |
| Q4 | 84 | 89 | 49 | 159 | |
| 15 (59) | 18 (39) | 24 (84) | 89 (196) | ||
Per 1000 person years, (.) number of events. Inclusion criteria: Joslin eGFR > 30, SURDIAGENE: eGFR < 60 and/or ACR > 30 mg/mol. Mean observation time: Joslin 12 years SURDIAGENE 4 years; ESRD, end-stage renal disease; eGFR, estimated glomerular filtration rate; ACR, albumin/creatinine ratio; Q1–Q4, quartiles 1 to 4.
We had previously reported that elevated circulating TNFRs levels were associated with the risk for all-cause mortality among 319 Japanese patients undergoing hemodialysis [53]. Sensitivity analysis revealed no significant interaction regardless of the presence or absence of diabetes. Interestingly, patients with decreased renal function had three- to five-fold higher median circulating TNFRs levels than those with preserved renal function, suggesting that circulating TNFRs accumulate with decreased renal function. On the other hand, Carlsson et al. reported that circulating TNFRs levels did not predict all-cause mortality among 207 Caucasian patients undergoing hemodialysis [54]. As such, more large-scale studies are needed to clarify such conflicting results regarding the international difference in mortality among hemodialysis patients.
6. Circulating Tumor Necrosis Factor Receptor Levels among Patients with Diabetes from Different Races
Circulating TNFRs levels might differ among patients with diabetes from different races. Such differences in measured values may generally be attributed to differences in measurement method. Therefore, we compared TNFRs levels among previously published studies that used the ELISA kit from the R&D system (TNFR1: DRT100, TNFR2: DRT200). Given that circulating TNFRs levels have been reported to be associated with several factors, such as age, body mass index, albuminuria, and GFR, comparing them has been difficult. However, as shown in Table 3, circulating TNFRs levels in between Caucasian and Asian patients with diabetes do not seem to be extremely different. Moreover, studies have shown that TNFR levels were quite similar among patients with diabetes and IgA nephropathy who had comparable eGFR levels [55,56]. On the other hand, Pima Indians seem to have much higher TNFR levels than other races considering their GFR and albuminuria [43]. Obesity might be partly associated with increased TNFR levels, while Pima Indians might have had naturally high TNFR levels. Further studies are required to reveal the normal range.
Table 3.
Circulating tumor necrosis factor receptor levels among patients with diabetes and IgA nephropathy.
| References | n | Type | GFR (mL/min/1.73 m2) | GFR Estimated Method | ACR (AER) or PCR | ACR Level | TNFR1 (pg/mL) | TNFR2 (pg/mL) | Race, Patients, Cohort |
|---|---|---|---|---|---|---|---|---|---|
| Pavkov et al. [43] | 193 | 2 | 120 (88–149) |
Urinary clearance of iothalamate | 72 (19–493) |
Normo (32%) Micro (37%) Macro (31%) |
2833 (2081, 4092) |
4835 (3875, 6997) |
Pima Indian |
| Pavkov et al. [44] | 83 | 2 | 119 (94, 155) |
Urinary clearance of iothalamate | 26 (12, 127) |
Normo (52%) Micro (29%) Macro (19%) |
1500 (1205, 1960) |
3283 (2670, 4151) |
Pima Indian |
| Gohda et al. [39] | 353 | 1 | 129 ± 30 | Cyctatin C based GFR | 41* (24, 79) |
High normo (>15) Micro |
1382 (1180, 1709) |
2230 (1869, 2695) |
Caucasian (94%) Second Joslin Kidney Study |
| Gohda et al. [39] | 275 | 1 | 133 ± 30 | Cyctatin C based GFR | 56* (37, 101) |
Micro | 1345 (1156, 1598) |
2161 (1732, 2673) |
Caucasian (94%) First Joslin Kidney Study |
| Skupien et al. [41] | 349 | 1 | 81 (55, 104) |
CKD-EPI | 771 (471, 1377) |
Macro | NA | 4415 (3497, 5777) |
Caucasian Joslin Proteinuria Cohort |
| Kamei et al. [57] | 334 | 2 | 72 (61, 86) |
IDMS-traceable MDRD | 10 (6, 17) |
Normo | 1401 (1175, 1725) |
3036 (2558, 3828) |
Asian (Japanese) |
| Kamei et al. [57] | 171 | 2 | 69 (53, 85) |
IDMS-traceable MDRD | 79 (40, 152) |
Micro | 1630 (1418, 2092) |
3522 (2841, 4570) |
Asian (Japanese) |
| Kamei et al. [57] | 89 | 2 | 55 (44, 70) |
IDMS-traceable MDRD | 690 (449, 1487) |
Macro | 2229 (1751, 2811) |
4370 (3610, 5645) |
Asian (Japanese) |
| Sonoda et al. [55] | 106 | NA | 79 (60, 100) |
IDMS-traceable MDRD | 0.4** (0.2, 1.0) |
NA | 1412 (1264, 1807) |
2963 (2483, 3758) |
Asian (Japanese) IgA nephropathy |
| Murakoshi et al. [56] | 223 | NA | 83 ± 29 | IDMS-traceable MDRD | 0.4** (0.2, 1.0) |
NA | 1491 (1248, 1915) |
3083 (2598, 3822) |
Asian (Japanese) IgA nephropathy |
Data are presented as mean ± standard deviation (SD), median (quartiles). n, Number of patients; ACR (mg/g), albumin/creatinine ratio; *, AER (mg/min), albumin excretion rate; **, PCR (g/g), protein/creatinine ratio; IDMS, isotope dilution mass spectrometry; MDRD, modification of diet in renal disease; CKD-EPI, chronic kidney disease epidemiology collaboration; GFR (mL/min/1.73 m2), glomerular filtration rate; NA, not applicable
7. Contributions of TNFR1 and TNFR2 to Diabetic Kidney Disease and Other Kidney Diseases in Animal Models
Evidence for the involvement of TNFα and its receptors in the progression of DKD comes primarily from studies on the streptozotocin (STZ)-induced rat DKD model [58]. TNFR:Fc is a sTNFα antagonist consisting of two TNFR2 extracellular domains fused to the Fc portion of human IgG1, which binds to sTNFα and prevents TNFα from interacting with its cognate cell surface receptors. Administration of TNFR:Fc fusion protein to STZ-induced diabetic rats reduced urinary TNFα excretion and sodium retention and ameliorated renal hypertrophy without affecting the metabolic profile. This action might be important because sodium retention and renal hypertrophy precede the onset of albuminuria in this model. They also showed that TNFα stimulated sodium uptake in distal tubule cells isolated from diabetic rats. The expressions of both TNFR1 and TNFR2 were observed in distal tubule cells. Inhibiting the TNF–TNFR signaling may limit DKD progression by preventing sodium retention. Similarly, TNFα inhibition with infliximab, a chimeric monoclonal antibody directed against TNFα, significantly reduced both albuminuria and urinary TNFα excretion in STZ-induced diabetic rats [59]. We also reported that soluble TNFR2 fusion protein, Etanercept (ETN), significantly improved kidney injury in spontaneous DKD (KK-Ay) mice. Renal mRNA and/or TNFα and TNFR1 protein levels did not differ between DKD mice with and without ETN, although those of TNFR2 improved dramatically. Moreover, ETN treatment decreased serum sTNFR2 levels but not serum sTNFR1 levels. These results suggested that the TNF–TNFR2 pathway, but not sTNFR1, may function during kidney injury in this mouse model [60]. Few studies have utilized the mouse genetic approach to understand the role of TNFα and TNFR in the DKD animal model.
However, several reports have been available concerning TNFRs in other kidney disease models (Table 4). In a rat experimental model of anti-GBM nephritis, sTNFR1 was effective in preventing acute glomerular inflammation and crescent formation both before and after establishment of nephritis [61]. Another group reported that TNFR2-deficient mice with anti-GBM nephritis did not exhibit increased albuminuria throughout the study period [62]. On the other hand, TNFR1-deficient mice exhibited albuminuria that was largely comparable to that in wild-type mice at the end of the day despite the initial delayed onset of nephritis. This study suggested that therapeutic blockade of TNFR2 may be a promising strategy for the treatment of anti-GBM nephritis. One study using a cisplatin-induced acute kidney injury model showed that TNFR2-deficient mice had milder kidney injury compared to TNFR1-deficient mice after cisplatin treatment [63] Moreover, another study has found that among unilateral ureteral obstruction (UUO) mice, TNFR1 knockout mice had less severe renal lesions, such as collagen IV deposition, α-smooth muscle actin (α-SMA) matrix score, and NF-κB activity, than TNFR2 knockout mice [64]. Thus, it remains unclear which among TNFR, TNFR1, or TNFR2, is strongly associated with the development and/or progression of kidney injury.
Table 4.
Inhibitory effects of tumor necrosis factor signal in animal models.
| Model Used | Methods of TNFα Antagonism | Effect of TNFα Inhibition | References |
|---|---|---|---|
| Anti-GBM nephritis rat | Soluble TNFR1 | sTNFR1 prevented acute glomerular inflammation and crescent formation | [61] |
| Anti-GBM nephritis rat | Rat TNFα monoclonal antibody | TNF antibody reduced glomerular inflammation, crescent formation, and tubulointerstitial scarring, with preservation of renal function | [65] |
| Anti-GBM nephritis mice | TNFR1 or TNFR2 KO mice | TNFR1-deficient mice: less proteinuria and glomerular injury only at the early stages TNFR2-deficient mice: completely protected from glomerulonephritis at all stages |
[62] |
| TNF administration in SLE-prone mice | TNFR1 and/or TNFR2 KO mice | TNFR1/TNFR2-double deficient mice exhibited accelerated pathological and clinical nephritis | [66] |
| STZ-induced diabetic rat | TNFR:Fc | TNFR:Fc reduced urinary TNF excretion, sodium retention, and attenuated renal hypertrophy | [58] |
| STZ-induced diabetic rat | Infliximab | Infliximab ameliorated urinary albumin and TNFα excretion | [59] |
| Spontaneous DKD mice | Etanercept | Etanercept improved albuminuria and decreased serum sTNFR2 levels | [60] |
| UUO mice | TNFR1 or TNFR2 KO mice | TNFR1 or TNFR2 deficiency resulted in significantly less NF-κB activation compared with the wild type, with TNFR1 being less than TNFR2 knockout | [64] |
| UUO rat | Soluble TNFR1 (PEG-sTNFR1) | PEG-sTNFR1 significantly reduced tubulointerstitial fibrosis and a progressive renal function decline | [67] |
| Cisplatin-induced renal injury mice | TNFR1 or TNFR2 KO mice | TNFR1 or TNFR2 deficiency protects mice from cisplatin-induced AKI. TNFR2-deficient mice developed less severe renal dysfunction compared with either TNFR1-deficient or wild-type mice |
[63] |
TNF, tumor necrosis factor; KO, knockout; STZ, streptozotocin; UUO, unilateral ureteral obstruction; AKI, acute kidney injury
8. Conclusions
Considering that DKD has been a leading cause of ESRD, identifying new clinical biomarkers and therapeutic targets to effectively prevent the progression of complications is imperative. A number of studies have indicated that inflammation plays a major role in the pathogenesis of DKD, while TNF-α and its receptors, TNFR1 and TNFR2, contribute significantly to the progression of DKD. In addition, results from previous studies have provided sufficient evidence to suggest that TNFRs can be a prognostic biomarker for DKD. Further research is nonetheless needed to clarify the prognostic and therapeutic roles of TNFR in DKD.
Acknowledgments
This work was partially supported by Grant-in-Aid for Scientific Research (C) No. 17K09711 to T.G. This work was financially supported by Suzuken Memorial Foundation to M.M.
Abbreviations
| CKD | Chronic kidney disease |
| DKD | Diabetic kidney disease |
| ESRD | End-stage renal disease |
| TNFα | Tumor necrosis factor alpha |
| TNFR | TNF receptor |
Author Contributions
Writing—Original draft preparation, M.M.; writing—Original draft preparation, review and editing, T.G.; supervision, Y.S. All authors have read and agreed on the published version of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Association A.D. Improving Care and Promoting Health in Populations: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43:S7–S13. doi: 10.2337/dc20-S001. [DOI] [PubMed] [Google Scholar]
- 2.Lambers Heerspink H.J., de Zeeuw D. Debate: PRO position. Should microalbuminuria ever be considered as a renal endpoint in any clinical trial? Am. J. Nephrol. 2010;31:458–461. doi: 10.1159/000292501. [DOI] [PubMed] [Google Scholar]
- 3.Macisaac R.J., Jerums G. Diabetic kidney disease with and without albuminuria. Curr. Opin. Nephrol. Hypertens. 2011;20:246–257. doi: 10.1097/MNH.0b013e3283456546. [DOI] [PubMed] [Google Scholar]
- 4.Gohda T., Murakoshi M., Koshida T., Ichikawa S., Li Z., Adachi E., Sakuma H., Hagiwara s., Funabiki K., Suzuki Y. Concept of Diabetic Kidney Disease - Paradigm Shift from Albuminuria - Based to GFR - Based Kidney Disease. Juntendo Med J. 2019;65:510–516. doi: 10.14789/jmj.2019.65.JMJ19-R16. [DOI] [Google Scholar]
- 5.Ramseyer V.D., Garvin J.L. Tumor necrosis factor-alpha: Regulation of renal function and blood pressure. Am. J. Physiol. Renal. Physiol. 2013;304:F1231–F1242. doi: 10.1152/ajprenal.00557.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Speeckaert M.M., Speeckaert R., Laute M., Vanholder R., Delanghe J.R. Tumor necrosis factor receptors: Biology and therapeutic potential in kidney diseases. Am. J. Nephrol. 2012;36:261–270. doi: 10.1159/000342333. [DOI] [PubMed] [Google Scholar]
- 7.Gohda T., Kamei N., Koshida T., Kubota M., Tanaka K., Yamashita Y., Adachi E., Ichikawa S., Murakoshi M., Ueda S., et al. Circulating kidney injury molecule-1 as a biomarker of renal parameters in diabetic kidney disease. J. diabetes Investig. 2019 doi: 10.1111/jdi.13139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gohda T., Nishizaki Y., Murakoshi M., Nojiri S., Yanagisawa N., Shibata T., Yamashita M., Tanaka K., Yamashita Y., Suzuki Y., et al. Clinical predictive biomarkers for normoalbuminuric diabetic kidney disease. Diabetes Res. Clin. Pract. 2018;141:62–68. doi: 10.1016/j.diabres.2018.04.026. [DOI] [PubMed] [Google Scholar]
- 9.Barutta F., Bruno G., Grimaldi S., Gruden G. Inflammation in diabetic nephropathy: Moving toward clinical biomarkers and targets for treatment. Endocrine. 2015;48:730–742. doi: 10.1007/s12020-014-0437-1. [DOI] [PubMed] [Google Scholar]
- 10.Wada J., Makino H. Inflammation and the pathogenesis of diabetic nephropathy. Clin. Sci. (Lond.) 2013;124:139–152. doi: 10.1042/CS20120198. [DOI] [PubMed] [Google Scholar]
- 11.Seok S.J., Lee E.S., Kim G.T., Hyun M., Lee J.H., Chen S., Choi R., Kim H.M., Lee E.Y., Chung C.H. Blockade of CCL2/CCR2 signalling ameliorates diabetic nephropathy in db/db mice. Nephrol. Dial. Transplant. 2013;28:1700–1710. doi: 10.1093/ndt/gfs555. [DOI] [PubMed] [Google Scholar]
- 12.Liu R., Zhong Y., Li X., Chen H., Jim B., Zhou M.M., Chuang P.Y., He J.C. Role of transcription factor acetylation in diabetic kidney disease. Diabetes. 2014;63:2440–2453. doi: 10.2337/db13-1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sugimoto H., Shikata K., Hirata K., Akiyama K., Matsuda M., Kushiro M., Shikata Y., Miyatake N., Miyasaka M., Makino H. Increased expression of intercellular adhesion molecule-1 (ICAM-1) in diabetic rat glomeruli: Glomerular hyperfiltration is a potential mechanism of ICAM-1 upregulation. Diabetes. 1997;46:2075–2081. doi: 10.2337/diab.46.12.2075. [DOI] [PubMed] [Google Scholar]
- 14.Gohda T., Tomino Y. Novel biomarkers for the progression of diabetic nephropathy: Soluble TNF receptors. Curr. Diab. Rep. 2013;13:560–566. doi: 10.1007/s11892-013-0385-9. [DOI] [PubMed] [Google Scholar]
- 15.Yang S., Wang J., Brand D.D., Zheng S.G. Role of TNF-TNF Receptor 2 Signal in Regulatory T Cells and Its Therapeutic Implications. Front. Immunol. 2018;9:784. doi: 10.3389/fimmu.2018.00784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schlondorff J., Blobel C.P. Metalloprotease-disintegrins: Modular proteins capable of promoting cell-cell interactions and triggering signals by protein-ectodomain shedding. J. Cell Sci. 1999;112:3603–3617. doi: 10.1242/jcs.112.21.3603. [DOI] [PubMed] [Google Scholar]
- 17.Luettig B., Decker T., Lohmann-Matthes M.L. Evidence for the existence of two forms of membrane tumor necrosis factor: An integral protein and a molecule attached to its receptor. J. Immunol. 1989;143:4034–4038. [PubMed] [Google Scholar]
- 18.Moss M.L., Jin S.L., Milla M.E., Bickett D.M., Burkhart W., Carter H.L., Chen W.J., Clay W.C., Didsbury J.R., Hassler D., et al. Cloning of a disintegrin metalloproteinase that processes precursor tumour-necrosis factor-alpha. Nature. 1997;385:733–736. doi: 10.1038/385733a0. [DOI] [PubMed] [Google Scholar]
- 19.Puigserver P. Signaling Transduction and Metabolomics. In: Hoffman R., editor. Hematology. 7th ed. Elsevier; Amsterdam, The Netherlands: 2018. pp. 663–672. [Google Scholar]
- 20.Bodmer J.L., Schneider P., Tschopp J. The molecular architecture of the TNF superfamily. Trends Biochem. Sci. 2002;27:19–26. doi: 10.1016/S0968-0004(01)01995-8. [DOI] [PubMed] [Google Scholar]
- 21.Ihnatko R., Kubes M. TNF signaling: Early events and phosphorylation. Gen. Physiol. Biophys. 2007;26:159–167. [PubMed] [Google Scholar]
- 22.Cabal-Hierro L., Lazo P.S. Signal transduction by tumor necrosis factor receptors. Cell Signal. 2012;24:1297–1305. doi: 10.1016/j.cellsig.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Jiang Y., Woronicz J.D., Liu W., Goeddel D.V. Prevention of constitutive TNF receptor 1 signaling by silencer of death domains. Science. 1999;283:543–546. doi: 10.1126/science.283.5401.543. [DOI] [PubMed] [Google Scholar]
- 24.Al-Lamki R.S., Mayadas T.N. TNF receptors: Signaling pathways and contribution to renal dysfunction. Kidney Int. 2015;87:281–296. doi: 10.1038/ki.2014.285. [DOI] [PubMed] [Google Scholar]
- 25.Hsu H., Shu H.B., Pan M.G., Goeddel D.V. TRADD-TRAF2 and TRADD-FADD interactions define two distinct TNF receptor 1 signal transduction pathways. Cell. 1996;84:299–308. doi: 10.1016/S0092-8674(00)80984-8. [DOI] [PubMed] [Google Scholar]
- 26.Bradley J.R. TNF-mediated inflammatory disease. J. Pathol. 2008;214:149–160. doi: 10.1002/path.2287. [DOI] [PubMed] [Google Scholar]
- 27.Sabio G., Davis R.J. TNF and MAP kinase signalling pathways. Semin. Immunol. 2014;26:237–245. doi: 10.1016/j.smim.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guma M., Firestein G.S. c-Jun N-Terminal Kinase in Inflammation and Rheumatic Diseases. Open Rheumatol. J. 2012;6:220–231. doi: 10.2174/1874312901206010220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang Y., Kim S.C., Yu T., Yi Y.S., Rhee M.H., Sung G.H., Yoo B.C., Cho J.Y. Functional roles of p38 mitogen-activated protein kinase in macrophage-mediated inflammatory responses. Mediators Inflamm. 2014;2014:352371. doi: 10.1155/2014/352371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson N.S., Dixit V., Ashkenazi A. Death receptor signal transducers: Nodes of coordination in immune signaling networks. Nat. Immunol. 2009;10:348–355. doi: 10.1038/ni.1714. [DOI] [PubMed] [Google Scholar]
- 31.Blackwell K., Zhang L., Thomas G.S., Sun S., Nakano H., Habelhah H. TRAF2 phosphorylation modulates tumor necrosis factor alpha-induced gene expression and cell resistance to apoptosis. Mol. Cell. Biol. 2009;29:303–314. doi: 10.1128/MCB.00699-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Faustman D., Davis M. TNF receptor 2 pathway: Drug target for autoimmune diseases. Nat. Rev. Drug Discov. 2010;9:482–493. doi: 10.1038/nrd3030. [DOI] [PubMed] [Google Scholar]
- 33.Venkatesh D., Ernandez T., Rosetti F., Batal I., Cullere X., Luscinskas F.W., Zhang Y., Stavrakis G., García-Cardeña G., Horwitz B.H., et al. Endothelial TNF receptor 2 induces IRF1 transcription factor-dependent interferon-β autocrine signaling to promote monocyte recruitment. Immunity. 2013;38:1025–1037. doi: 10.1016/j.immuni.2013.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sakimoto T., Ohnishi T., Ishimori A. Significance of ectodomain shedding of TNF receptor 1 in ocular surface. Investig. Ophthalmol. Vis. Sci. 2014;55:2419–2423. doi: 10.1167/iovs.13-13265. [DOI] [PubMed] [Google Scholar]
- 35.Aggarwal B.B. Signalling pathways of the TNF superfamily: A double-edged sword. Nat. Rev. Immunol. 2003;3:745–756. doi: 10.1038/nri1184. [DOI] [PubMed] [Google Scholar]
- 36.Naude P.J., den Boer J.A., Luiten P.G., Eisel U.L. Tumor necrosis factor receptor cross-talk. Febs. J. 2011;278:888–898. doi: 10.1111/j.1742-4658.2011.08017.x. [DOI] [PubMed] [Google Scholar]
- 37.Sun S.C., Ley S.C. New insights into NF-kappaB regulation and function. Trends Immunol. 2008;29:469–478. doi: 10.1016/j.it.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aderka D., Engelmann H., Maor Y., Brakebusch C., Wallach D. Stabilization of the bioactivity of tumor necrosis factor by its soluble receptors. J. Exp. Med. 1992;175:323–329. doi: 10.1084/jem.175.2.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gohda T., Niewczas M.A., Ficociello L.H., Walker W.H., Skupien J., Rosetti F., Cullere X., Johnson A.C., Crabtree G., Smiles A.M., et al. Circulating TNF receptors 1 and 2 predict stage 3 CKD in type 1 diabetes. J. Am. Soc. Nephrol. 2012;23:516–524. doi: 10.1681/ASN.2011060628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Niewczas M.A., Gohda T., Skupien J., Smiles A.M., Walker W.H., Rosetti F., Cullere X., Eckfeldt J.H., Doria A., Mayadas T.N., et al. Circulating TNF receptors 1 and 2 predict ESRD in type 2 diabetes. J. Am. Soc. Nephrol. 2012;23:507–515. doi: 10.1681/ASN.2011060627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Skupien J., Warram J.H., Niewczas M.A., Gohda T., Malecki M., Mychaleckyj J.C., Galecki A.T., Krolewski A.S. Synergism between circulating tumor necrosis factor receptor 2 and HbA(1c) in determining renal decline during 5-18 years of follow-up in patients with type 1 diabetes and proteinuria. Diabetes Care. 2014;37:2601–2608. doi: 10.2337/dc13-1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Krolewski A.S., Niewczas M.A., Skupien J., Gohda T., Smiles A., Eckfeldt J.H., Doria A., Warram J.H. Early progressive renal decline precedes the onset of microalbuminuria and its progression to macroalbuminuria. Diabetes Care. 2014;37:226–234. doi: 10.2337/dc13-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pavkov M.E., Nelson R.G., Knowler W.C., Cheng Y., Krolewski A.S., Niewczas M.A. Elevation of circulating TNF receptors 1 and 2 increases the risk of end-stage renal disease in American Indians with type 2 diabetes. Kidney Int. 2015;87:812–819. doi: 10.1038/ki.2014.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pavkov M.E., Weil E.J., Fufaa G.D., Nelson R.G., Lemley K.V., Knowler W.C., Niewczas M.A., Krolewski A.S. Tumor necrosis factor receptors 1 and 2 are associated with early glomerular lesions in type 2 diabetes. Kidney Int. 2016;89:226–234. doi: 10.1038/ki.2015.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Niewczas M.A., Pavkov M.E., Skupien J., Smiles A., Md Dom Z.I., Wilson J.M., Park J., Nair V., Schlafly A., Saulnier P.J., et al. A signature of circulating inflammatory proteins and development of end-stage renal disease in diabetes. Nat. Med. 2019;25:805–813. doi: 10.1038/s41591-019-0415-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ye X., Luo T., Wang K., Wang Y., Yang S., Li Q., Hu J. Circulating TNF receptors 1 and 2 predict progression of diabetic kidney disease: A meta-analysis. Diabetes Metab. Res. Rev. 2019;35:e3195. doi: 10.1002/dmrr.3195. [DOI] [PubMed] [Google Scholar]
- 47.Forsblom C., Moran J., Harjutsalo V., Loughman T., Waden J., Tolonen N., Thorn L., Saraheimo M., Gordin D., Groop P.H., et al. Added value of soluble tumor necrosis factor-alpha receptor 1 as a biomarker of ESRD risk in patients with type 1 diabetes. Diabetes Care. 2014;37:2334–2342. doi: 10.2337/dc14-0225. [DOI] [PubMed] [Google Scholar]
- 48.Saulnier P.J., Gand E., Velho G., Mohammedi K., Zaoui P., Fraty M., Halimi J.M., Roussel R., Ragot S., Hadjadj S. Association of Circulating Biomarkers (Adrenomedullin, TNFR1, and NT-proBNP) With Renal Function Decline in Patients With Type 2 Diabetes: A French Prospective Cohort. Diabetes Care. 2017;40:367–374. doi: 10.2337/dc16-1571. [DOI] [PubMed] [Google Scholar]
- 49.Coca S.G., Nadkarni G.N., Huang Y., Moledina D.G., Rao V., Zhang J., Ferket B., Crowley S.T., Fried L.F., Parikh C.R. Plasma Biomarkers and Kidney Function Decline in Early and Established Diabetic Kidney Disease. J. Am. Soc. Nephrol. 2017;28:2786–2793. doi: 10.1681/ASN.2016101101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barr E.L.M., Barzi F., Hughes J.T., Jerums G., Hoy W.E., O’Dea K., Jones G.R.D., Lawton P.D., Brown A.D.H., Thomas M., et al. High Baseline Levels of Tumor Necrosis Factor Receptor 1 Are Associated With Progression of Kidney Disease in Indigenous Australians With Diabetes: The eGFR Follow-up Study. Diabetes Care. 2018;41:739–747. doi: 10.2337/dc17-1919. [DOI] [PubMed] [Google Scholar]
- 51.Saulnier P.J., Gand E., Ragot S., Ducrocq G., Halimi J.M., Hulin-Delmotte C., Llaty P., Montaigne D., Rigalleau V., Roussel R., et al. Association of serum concentration of TNFR1 with all-cause mortality in patients with type 2 diabetes and chronic kidney disease: Follow-up of the SURDIAGENE Cohort. Diabetes Care. 2014;37:1425–1431. doi: 10.2337/dc13-2580. [DOI] [PubMed] [Google Scholar]
- 52.Carlsson A.C., Ostgren C.J., Nystrom F.H., Lanne T., Jennersjo P., Larsson A., Arnlov J. Association of soluble tumor necrosis factor receptors 1 and 2 with nephropathy, cardiovascular events, and total mortality in type 2 diabetes. Cardiovasc. Diabetol. 2016;15:40. doi: 10.1186/s12933-016-0359-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gohda T., Maruyama S., Kamei N., Yamaguchi S., Shibata T., Murakoshi M., Horikoshi S., Tomino Y., Ohsawa I., Gotoh H., et al. Circulating TNF Receptors 1 and 2 Predict Mortality in Patients with End-stage Renal Disease Undergoing Dialysis. Sci. Rep. 2017;7:43520. doi: 10.1038/srep43520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carlsson A.C., Carrero J.J., Stenvinkel P., Bottai M., Barany P., Larsson A., Arnlov J. High levels of soluble tumor necrosis factor receptors 1 and 2 and their association with mortality in patients undergoing hemodialysis. Cardiorenal. Med. 2015;5:89–95. doi: 10.1159/000371661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sonoda Y., Gohda T., Suzuki Y., Omote K., Ishizaka M., Matsuoka J., Tomino Y. Circulating TNF receptors 1 and 2 are associated with the severity of renal interstitial fibrosis in IgA nephropathy. PLoS ONE. 2015;10:e0122212. doi: 10.1371/journal.pone.0122212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Murakoshi M., Gohda T., Sonoda Y., Suzuki H., Tomino Y., Horikoshi S., Suzuki Y. Effect of tonsillectomy with steroid pulse therapy on circulating tumor necrosis factor receptors 1 and 2 in IgA nephropathy. Clin. Exp. Nephrol. 2017;21:1068–1074. doi: 10.1007/s10157-017-1408-7. [DOI] [PubMed] [Google Scholar]
- 57.Kamei N., Yamashita M., Nishizaki Y., Yanagisawa N., Nojiri S., Tanaka K., Yamashita Y., Shibata T., Murakoshi M., Suzuki Y., et al. Association between circulating tumor necrosis factor-related biomarkers and estimated glomerular filtration rate in type 2 diabetes. Sci. Rep. 2018;8:15302. doi: 10.1038/s41598-018-33590-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.DiPetrillo K., Coutermarsh B., Gesek F.A. Urinary tumor necrosis factor contributes to sodium retention and renal hypertrophy during diabetes. Am. J. Physiol. Renal. Physiol. 2003;284:F113–F121. doi: 10.1152/ajprenal.00026.2002. [DOI] [PubMed] [Google Scholar]
- 59.Moriwaki Y., Inokuchi T., Yamamoto A., Ka T., Tsutsumi Z., Takahashi S., Yamamoto T. Effect of TNF-alpha inhibition on urinary albumin excretion in experimental diabetic rats. Acta Diabetol. 2007;44:215–218. doi: 10.1007/s00592-007-0007-6. [DOI] [PubMed] [Google Scholar]
- 60.Omote K., Gohda T., Murakoshi M., Sasaki Y., Kazuno S., Fujimura T., Ishizaka M., Sonoda Y., Tomino Y. Role of the TNF pathway in the progression of diabetic nephropathy in KK-A(y) mice. Am. J. Physiol. Renal. Physiol. 2014;306:F1335–F1347. doi: 10.1152/ajprenal.00509.2013. [DOI] [PubMed] [Google Scholar]
- 61.Karkar A.M., Smith J., Pusey C.D. Prevention and treatment of experimental crescentic glomerulonephritis by blocking tumour necrosis factor-alpha. Nephrol. Dial. Transplant. 2001;16:518–524. doi: 10.1093/ndt/16.3.518. [DOI] [PubMed] [Google Scholar]
- 62.Vielhauer V., Stavrakis G., Mayadas T.N. Renal cell-expressed TNF receptor 2, not receptor 1, is essential for the development of glomerulonephritis. J. Clin. Investig. 2005;115:1199–1209. doi: 10.1172/JCI200523348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ramesh G., Reeves W.B. TNFR2-mediated apoptosis and necrosis in cisplatin-induced acute renal failure. Am. J. Physiol. Renal Physiol. 2003;285:F610–F618. doi: 10.1152/ajprenal.00101.2003. [DOI] [PubMed] [Google Scholar]
- 64.Guo G., Morrissey J., McCracken R., Tolley T., Klahr S. Role of TNFR1 and TNFR2 receptors in tubulointerstitial fibrosis of obstructive nephropathy. Am. J. Physiol. 1999;277:F766–F772. doi: 10.1152/ajprenal.1999.277.5.F766. [DOI] [PubMed] [Google Scholar]
- 65.Khan S.B., Cook H.T., Bhangal G., Smith J., Tam F.W., Pusey C.D. Antibody blockade of TNF-alpha reduces inflammation and scarring in experimental crescentic glomerulonephritis. Kidney Int. 2005;67:1812–1820. doi: 10.1111/j.1523-1755.2005.00279.x. [DOI] [PubMed] [Google Scholar]
- 66.Jacob N., Yang H., Pricop L., Liu Y., Gao X., Zheng S.G., Wang J., Gao H.X., Putterman C., Koss M.N., et al. Accelerated pathological and clinical nephritis in systemic lupus erythematosus-prone New Zealand Mixed 2328 mice doubly deficient in TNF receptor 1 and TNF receptor 2 via a Th17-associated pathway. J. Immunol. 2009;182:2532–2541. doi: 10.4049/jimmunol.0802948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Meldrum K.K., Misseri R., Metcalfe P., Dinarello C.A., Hile K.L., Meldrum D.R. TNF-alpha neutralization ameliorates obstruction-induced renal fibrosis and dysfunction. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007;292:R1456–R1464. doi: 10.1152/ajpregu.00620.2005. [DOI] [PubMed] [Google Scholar]