Abstract
A 65-year-old male who presented with dizziness, dysarthria, and disability of his left hand was admitted to our hospital. Magnetic resonance imaging of the head revealed cerebral infarction and enhanced computed tomography revealed a suspicious thrombus in the ascending aorta. He did not have a coagulation disorder. We performed ascending aortic replacement and removed the thrombus with the aortic wall in order to avoid any recurrences. Here we report the successful treatment of the case from clinical and pathological points of view with some findings.
Keywords: thrombus, aorta, graft-replacement
Introduction
A floating thrombus in the aorta is relatively rare and usually only discovered due to embolism symptoms or by chance in echography, computed tomography, or magnetic resonance imaging scans. Patients with a thrombus tend to have tumors or coagulopathy, and patients without these diseases are very rare. Several treatments for thrombus in the aorta have been reported, including anticoagulant therapy and surgical treatments such as thrombectomy, endarterectomy, and graft replacement.
Case Report
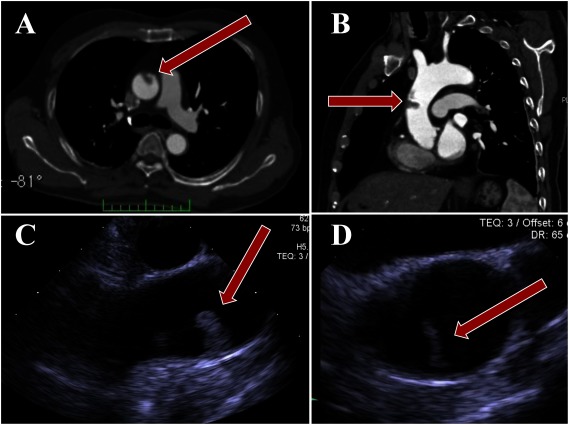
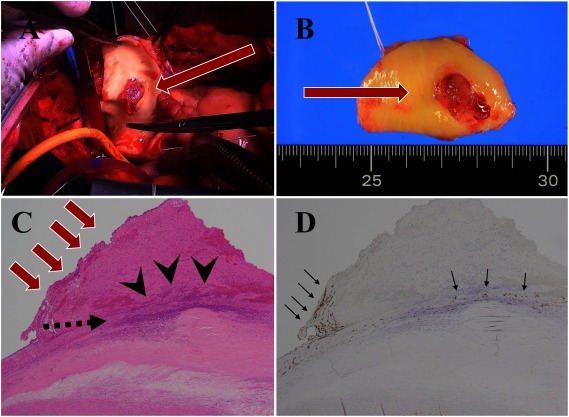
A 65-year-old male who presented with dizziness, dysarthria, and disability of his left hand was admitted to our hospital. He was a smoker with a past history of dyslipidosis and benign prostatic hyperplasia. Magnetic resonance imaging of the head revealed cerebral infarction and enhanced computed tomography revealed a suspicious thrombus in the ascending aorta (Figs. 1A and 1B). An electrocardiogram showed that the patient had sinus rhythm and no abnormal shunts, such as an atrial septal defect, patent foramen ovale, or ventricular septal defect, were detected in transthoracic echocardiography (Figs. 1C and 1D). The platelet count was 35.5×104/µL and the fibrinogen level was 333 mg/dL. C and S protein activities were within the normal range and the result for lupus anticoagulant was negative. Cholesterol values were also within the normal range. Cerebral infarction might have occurred due to a suspicious thrombus in the ascending aorta, so surgical treatment with a graft replacement was performed. A cardiopulmonary bypass (CPB) was established between right femoral artery and the right atrium to lessen the risk of the thrombus being broken by the blood flow of CPB and of another embolism. During CPB, the mass was strictly observed using transesophageal echocardiography. After circulatory arrest was achieved under hypothermia, the ascending aorta was cut open and the suspicious thrombus with the ascending aorta was successfully removed with the aortic wall. Then, the ascending aorta was replaced by an artificial vascular graft (Figs. 2A and 2B). The postoperative course was uneventful and the patient was discharged 15 days after surgery. Postoperative pathological findings revealed a fibrous cap, which had ruptured with the thrombus on it, of atherosclerotic plaque in the ascending aorta (Fig. 2C). It consisted of a platelet-rich thrombus. A specialized immunostaining for CD34 showed the regenerated CD34-positive endothelial cells that gathered on the intimal erosion and on the surface of the thrombus.
Fig. 1 (A) Axial and (B) left anterior oblique view of the ascending aorta by computed tomography (CT). (C) Long axial and (D) short axial view of the ascending aorta in transesophageal echocardiogram (TEE); the mobile thrombus was shown in CT and TEE (red arrows).
Fig. 2 (A) Intraoperative finding. The thrombus was attached to the ascending aorta (red arrow). (B) Resection of ascending aorta with thrombus (red arrow). (C) Hematoxylin & eosin stain of the resected ascending aorta with thrombus (×40); red arrows show thrombus attached to atherosclerosis plaque in the aorta. There was (not were) an intimal erosion and a ruptured fibrous cap of atherosclerotic plaque (black arrowheads), and the thrombus was on it. (D) Immunostaining for CD34 (×40); CD34-positive regenerated endothelial cells were on the intimal erosion and the thrombus (black arrow).
Discussion
Several cases of thrombus in the ascending aorta were reported in the literature, but treatment for this differed case by case. Jaworski et al. reported a replacement of aorta with a vascular prosthesis.1) Haida et al. reported a successful thrombectomy with no recurrence within 12 months,2) otherwise recurrence of thrombus in the case of thrombectomy was reported.3) A case of sarcoma in the ascending aorta was reported.4,5) Sometimes it was difficult to distinguish tumor from thrombus during surgery.6) For these reasons, we thought the removal of thrombus with aortic wall might be better for this suspicious thrombus. In removing the mass with the aortic wall, we can repair the aorta using patch repair or tube graft. Both of them need to use CPB and probably with circulatory arrest, which depends on the site where the mass is attached and might carry similar outcomes such as the risk of recurrence. We are used to performing tube graft replacement and have no hesitations to do it, so we thought that tube graft replacement was simpler and safer than patch repair in our institution. The appropriate timing for surgery is debatable. In case of infectious endocarditis or thrombus in the left ventricular and left atrium, early surgery is preferred to avoid another embolism, but heart surgery with heparin after cerebral infarction has a risk of cerebral bleeding. For this reason, if a patient has a high surgical risk when using CPB, an alternative treatment such as anticoagulant therapy or thrombolytic therapy should be considered.
The pathological testing revealed an intimal erosion, and immunostaining for CD34 revealed the existence of CD34-positive endothelial cells around the erosion and on the thrombus. CD34-positive endothelial cells are reported to have an important role in forming thrombi in the aorta. These cells gather at the area of the erosion to repair the injured intima. After the thrombus is formed, regeneration occurs on the surface of the thrombus and this supports the thrombus with a high blood flow of the aorta.7)
Conclusion
A mobile thrombus in the ascending aorta could associate with atherosclerotic intima and a ruptured fibrous cap. The mobile thrombus should be removed with the wall attached to lessen the risk of recurrence.
Ethical Statement
This study follows the ethical policy of Ashikaga Red Cross Hospital and does not require the approval of the ethical committees.
Disclosure Statement
All authors have no conflict of interest.
Author Contributions
Study conception: YK, KK, HS
Data collection: KK, TI, MI
Writing: YK
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
References
- 1.Jaworski L, Fijalkowski M, Rogowski J. Giant thrombus in ascending aorta and aortic arch. J Thorac Cardiovasc Surg 2013; 145: 1668-9. [DOI] [PubMed] [Google Scholar]
- 2.Haida H, Inoue Y, Kawajiri H, et al. Rod-shaped giant floating thrombus in a normal ascending aorta. Eur J Cardiothorac Surg 2015; 47: 582. [DOI] [PubMed] [Google Scholar]
- 3.Fayad ZY, Semaan E, Fahoum B, et al. Aortic mural thrombus in the normal or minimally atherosclerotic aorta. Ann Vasc Surg 2013; 27: 282-90. [DOI] [PubMed] [Google Scholar]
- 4.Shimizu H, Tanibuchi A, Akaishi M, et al. Stroke due to undifferentiated aortic intimal sarcoma with disseminated metastatic lesions. Circulation 2009; 120: e290-2. [DOI] [PubMed] [Google Scholar]
- 5.Rhee MY, Myong NH, Park YB. Primary intimal sarcoma of the aorta: role of transesophageal echocardiography. Circ J 2002; 66: 111-3. [DOI] [PubMed] [Google Scholar]
- 6.Wright EP, Glick AD, Virmani R, et al. Aortic intimal sarcoma with embolic metastases. Am J Surg Pathol 1985; 9: 890-7. [DOI] [PubMed] [Google Scholar]
- 7.Nishizaki F, Tomita H, Abe N, et al. Acute myocardial infarction caused by a floating thrombus in the ascending aorta: a role of CD34-positive endothelial cells. J Cardiol Cases 2013; 8: e88-90. [DOI] [PMC free article] [PubMed] [Google Scholar]