Abstract
Objective: We aimed to determine predictors of poor long term quality of life, using the VEINES Quality of Life (QOL) questionnaire, in patients with lower limb deep venous thrombosis (DVT).
Material and Methods: This study included adult patients with primary lower limb DVT between January 2007 and December 2017. Post thrombotic syndrome (PTS) was assessed using the Villalta score and Quality of Life (QoL) by the VEINES quality of life questionnaire.
Results: Our study included 125 patients, 57 (45.6%) of whom were males. The patient population’s median age was 41 years (IQR: 34–47 years). The median follow up was 450 days (IQR: 390–1020 days). PTS occurred in 49 (39.2%) patients. Independent predictors of poor quality of life post DVT were progression to PTS, complete occlusion of vein, proximal (Ileofemoral) DVT, poor control of INR, poor compliance with compression stockings, severity of PTS, ileofemoral DVT and poor control of therapeutic anticoagulation.
Conclusion: Predictors who are independently associated with poor quality of life post DVT are PTS, inability to maintain therapeutic anticoagulation and ileofemoral DVT.
Keywords: quality of life, deep vein thrombosis, VEINES-QOL, predictors, post thrombotic syndrome
Introduction
Deep vein thrombosis (DVT) is a long term, debilitating condition that usually involves the lower extremities. Around 460,000 in Europe and 300,000 people in North America are affected by DVT each year.1) DVT occurs as an acute condition, but its sequel can be very troublesome, ranging from massive venous thromboembolism to venous congestion in the extremity, leading to skin changes and ulcerations. Of these, venous thromboembolism (VTE) can be life threatening, with reported incidence of VTE-associated mortality is 19%2) in literature. The natural course of DVT is an acute event, which is associated with an episode of massive limb swelling and pain. This gradually settles down in weeks to months’ time, but one third of the population affected by DVT do not recover completely, continuing to suffer from chronic longstanding complications after the event.3) A constellation of symptoms takes place in this one third of population, which include generalised limb oedema, usually not associated with pain, leg discomfort, fatigue and skin-associated changed (excoriation and ulcerations). This condition is referred to as post thrombotic syndrome (PTS) and has an incidence of 25–50% in a population who previously had DVT in their lives.4–6) PTS is manageable, to some extent, with conservative measures like compression stockings until the involvement of skin. Once ulcers develop in PTS, the patient’s quality of life is seriously affected because of obstacles to daily, routine activities and increased cost of treatment. Taking care of the treatment cost in our patient population, or any patient population, from a developing nation is essential as there is no concept of health insurance and most patients are self-payers. There are several studies from Western and developed nations which report impaired quality of life in patients with PTS and skin ulceration. Different tools were used to measure quality of life in these studies, like Short Form Health Survey 36 (SF 36), DVTQOL, EQ-5D and VEINES Quality of Life (QOL).7,8) Also, post DVT quality of life is comparable to the quality of life after other serious ailments, like congestive heart failure, chronic obstructive pulmonary disease and diabetes (DM).7) There is minimal post DVT quality of life data available from the developing world. As mentioned earlier, we assume quality of life is affected more seriously in this population due to low income and higher out-of-pocket costs for treatment. More information about various factors linked to poor quality of life in post DVT patients will help further define ways to avoid those factors and design strategies to improve quality of life. Therefore, we intended to find out the predictors of poor quality of life after lower limb DVT using the VEINES QOL questionnaire.
Materials and Methods
We conducted a retrospective cohort study in section of Vascular Surgery, Department of Surgery, Aga Khan University Hospital Karachi. This included all adult patients, aged 16 and above, admitted to our hospital with primary lower limb DVT between January 2007 and December 2017. We excluded patients who had incomplete records, missing files, issues with obtaining informed consent, and patients having stroke, malignancy, and paraplegia. After identifying patients via hospital medical record systems and the International Classification of Disease (ICD-9) coding, patients were reached by phone. Patients were seen during free follow up, where they provided informed consent. Predefined questionnaire included details of demographics and other clinical details which were filled in the clinic. Patients were specifically asked for the duration of post DVT compression therapy, and the threshold to compression compliance was taken as compression used for eight hours per day for at least four days per week. This initial detail was followed by a physical examination, carried out by both the principal investigator and a Vascular Consultant to avoid inter-observer bias. PTS severity was assessed using the Villalta score, and the VEINES QOL questionnaire was used to assess the degree of impairment in quality of life. The VEINES QOL consists of 26 variables and includes details regarding symptoms, daily activity limitations, and psychological impact. These scores cover the disease related variable, and it also has good psychometric properties.
Data was analysed using the Statistical Package for Social Science (SPSS), v.20. Frequency tables were used to describe the patients’ demographics and clinical details. Frequencies and percentages were used for qualitative variables, and medians with interquartile ranges (IQR) were used for quantitative variables due to non-normal distribution. Univariate analysis was conducted to assess the association of different variables with poor quality of life. The Mann–Whitney U test was applied to assess qualitative variable association with quality of life. Spearman’s correlation coefficients were used to assess the association of quantitative variable with quality of life. Multiple linear regression analysis was done to look for independent predictors for impaired quality of life. A P value of less than 0.05 was considered significant.
Results
Of the 569 patients who presented to our hospital with diagnoses of DVT, 258 were enrolled in the study according to the inclusion criteria. We were able to reach 200 patients through telephone; of these 200, only 125 visited the clinic and participated in the study. The patients’ median age was 41 years (IQR: 34–47 years); 57(45.6%) of the participants were males, and the median follow up time period was 450 days (IQR: 390–1020 days). Most DVT cases (79, or 63.2%) involved the left lower limb. Only three patients (2.4%) had bilateral lower limb DVT, 26 (20.8%) patients presented with proximal (ileofemoral) DVT, and 48 (38.4%) patients experienced complete vein occlusion. PTS occurred in 49 patients (39.2%). Table 1 provides further demographic data. These patients had a median VEINES QOL score of 51 (IQR: 39–58).
Table 1 Demographic characteristics and disease related measures.
| Variables | Categories | Median (IQR) or N (%) |
|---|---|---|
| Age (Years) | 41 (34–47) | |
| Sex | Male | 57 (45.6%) |
| Follow up duration (Days) | 450 (390–1020) | |
| Location | Ileo-femoral | 26 (20.8%) |
| Other | 99 (79.2%) | |
| Extent of obstruction | Complete | 48 (38.4%) |
| Partial | 77 (61.6%) | |
| Obesity | BMI ≥30 | 62 (49.6%) |
| Recent surgery | 51 (40.8%) | |
| Family history of DVT | 30 (24%) | |
| Smoking | Current smoker | 26 (20.8%) |
| Past smoker | 9 (7.2%) | |
| Never smoker | 90 (72%) | |
| Compression therapy | 122 (97.6) | |
| Use of compression therapy as recommended | > 4 times per week and >8 h/week | 27 (21.6%) |
| Use of compression therapy | Less than 8 h | 89 (71.2%) |
| 8–16 h | 36 (28.8%) | |
| Compliance of compression therapy | Less than 4 times/week | 50 (40%) |
| More than 4 times/week | 60 (48%) | |
| Hypercoagulable state | 64 (51.2%) | |
| Range of INR | Stable | 80 (64%) |
| Not stable | 45 (36%) | |
| Post thrombotic syndrome | None | 76 (60.8%) |
| Mild | 29 (23.2%) | |
| Moderate | 10 (8%) | |
| Severe | 3 (2.4%) | |
| Severe+ulcer | 7 (5.6%) |
IQR: interquartile range; BMI: body mass index; DVT: deep venous thrombosis; INR: international normalised ratio
A univariate analysis revealed the variable that had the worst association with the post DVT quality of life was proximal DVT location, complete vein obstruction on ultrasound, presence of PTS, obesity, inappropriate anticoagulation management on follow up, and inappropriate use of compression stockings (both duration and compliance), as shown in Tables 2 and 3, respectively. Forward, stepwise, multivariate linear regression analysis was done to determine independent predictors of poor quality of life. The P value, at the univariate level of less than 0.1, was taken as a cut off value for the variable to be included in multivariate analysis. So variables like obesity, DVT location, extent of obstruction on ultrasound, compression therapy duration, compliance with compression therapy, age, time of follow up, range of INR, and Villalta score were included in multivariate analysis. Ileofemoral DVT, unstable INR range on follow up, and the Villalta score turned out to be the only independent predictors of poor quality of life. The multivariable regression analysis results are shown in Table 4.
Table 2 Relationship of various binomial categorical predictor variables with Quality of Life after DVT using the Mann–Whitney U test.
| Variables | Categories | Means +/− SDs of VEINES-QOL score | P Values |
|---|---|---|---|
| Gender | Male | 55 (40–58) | 0.188 |
| Female | 49 (39–57) | ||
| Obesity | Yes | 40 (39–49) | 0.018 |
| No | 55 (42–58) | ||
| Recent surgery | Yes | 50 (44–56) | 0.627 |
| No | 55 (39–58) | ||
| Location of DVT | Ileofemoral DVT | 33 (29–46) | <0.001 |
| Others | 55 (44–58) | ||
| Obstruction on U/S | Complete | 45 (32.5–57) | 0.025 |
| Partial | 53 (44–58) | ||
| IVC filter placed | Yes | 54.5 (37.5–57) | 0.848 |
| No | 50 (40–58) | ||
| PTS | Yes | 42 (34–47) | <0.001 |
| No | 57 (50–58) | ||
| PE on CTscan | Yes | 46.5 (34.5–58.5) | 0.832 |
| No | 49 (44–57) | ||
| Range of INR | Stable | 55.5 (44.5–58) | <0.001 |
| Not stable | 44 (29–53) | ||
| Hypercoaguble state | Present | 47.5 (39–57.5) | 0.174 |
| Absent | 55 (40–58) | ||
| Duration of compression | Less than 8 h/day | 48 (39–56) | <0.001 |
| 8–16 h/day | 57.5 (50–59) | ||
| Compliance of compression | Less than 4 times/week | 46.5 (40–55) | <0.001 |
| More than 4 times/week | 56 (42.5–59) |
DVT: deep venous thrombosis; SD: standard deviation; U/S: ultrasound; IVC: inferior vena cava; PTS: post thrombotic syndrome; PE: pulmonary embolism; CT: computed tomography; INR: international normalised ratio
Table 3 Correlation of various continuous predictors with Quality of Life after DVT using Spearman’s Correlation.
| Variable | Spearman’s Rho | P value |
|---|---|---|
| Age | 0.212 | 0.018 |
| Villalta score | −0.617 | <0.001 |
Table 4 Multivariable linear regression analysis. Dependent variable being VEINES QOL score. Only predictor variables that remained significant are shown.
| Model | Unstandardized coefficients | Standardized coefficients | T-statistic | P value | Odds ratio | |
|---|---|---|---|---|---|---|
| B | Std. error | Beta coefficient | ||||
| (Constant) | 47.284 | 4.152 | 11.388 | <0.001 | ||
| Villalta score | −.796 | .125 | −.445 | −6.379 | <0.001 | 0.474 |
| Range of INR | −5.754 | 1.474 | −.261 | −3.903 | <0.001 | 0.004 |
| Ileofemoral DVT | 7.077 | 1.802 | .271 | 3.927 | <0.001 | 0.001 |
QOL: quality of life; INR: international normalised ratio; DVT: deep venous thrombosis
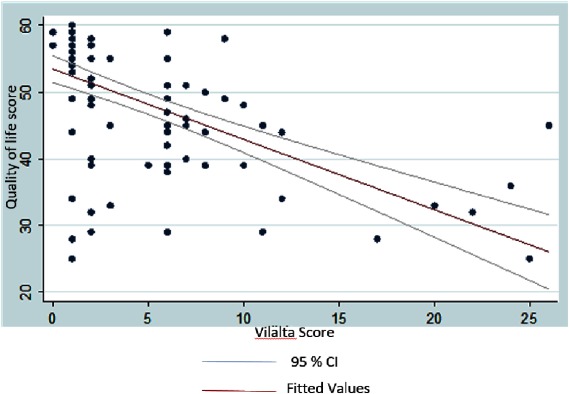
Figure 1 illustrates the relationship of the Villalta score with quality of life. It shows an inverse relationship of VEINES quality of life score with Villalta score. Increased severity of post-thrombotic syndrome is related to poorer quality of life.
Fig. 1 Scatter plot of Quality of Life score over the Villalta score with fitted values and 95% confidence interval limits.
Discussion
This study shows the association of poor quality of life scores in patients with DVT. We found that PTS is a commonly occurring phenomenon after a DVT episode, which sometimes presents as a disabling complication of a DVT. The median age of our population was 41 years; the average life expectancy in our country, as of 2016, is 66.8 years,9) which shows the significance of this condition. In our study, the Villalta score showed that PTS severity is an independent predictor of worse quality of life. In our study sample, PTS was seen in 40% of patients which indicates the disease’s hidden burden. This finding is also comparable to other reports in the literature which determined the predictors of poor quality of life. A report by Roberts LN et al. identified similar findings of PTS as an independent predictor of poor quality of life.10) Another report claims that worsening PTS severity is directly proportional to the worse quality of life post DVT.11) Measures to avoid this PTS severity are also highlighted in a few studies; using elastic compression stockings is and good compliance can prevent PTS development/progression.12,13)
Our study also associated proximal (Ileofemoral) DVT with poor quality of life, which is comparable to previous studies reported in the literature. A review article by Khan SR et al, also emphasised the association of proximal (Ileofemoral) DVT with greater PTS occurrence.14) Although the exact mechanism of this association is not clear, the authors state that, in proximal (Ileofemoral) DVT, the obstruction of the extremity veins are proximal to point where the profunda femoral veins enters. As a result, there is a decrease in the formation of collaterals and a higher chance of PTS than the distal (popliteal) DVT concomitantly.14) Another highlight of our study is the association of poor control of therapeutic range of INR and worse quality of life, which emphasises the importance of monitoring anticoagulation closely during DVT treatment. This was also emphasised in a report from Dongen CJ et al., which stated that maintaining appropriate therapeutic anticoagulation further helps develop PTS.15) To make our findings more objective, the post DVT QOL measurement was confirmed by disease-specific tools, such as the VEIINES QOL questionnaire. Various generic and disease-specific tools are available in the literature, but studies have proven that a disease-specific tool like VEINES QOL correlates better than generic tools like SF-36.16)
A major limitation of our study was its retrospective nature with small sample size. No baseline or pre DVT quality of life score was available for comparison, which made seeing the actual difference in quality of life difficult. Despite these limitations, our study’s greatest strength is the first of its kind to be reported from this region of the world, addressing post DVT quality of life and an effort to establish prognostic risk factors for poor quality of life. Another strength of the study is post DVT patient follow up; we made sure that each participant was followed for at least one year. We managed all of our patients with conservative measures (anticoagulation and compression) and not by thrombolysis; this further highlights the facts about PTS in a patient population which was managed conservatively. This study’s results can be used further in comparing quality of life predictors in conservative versus thrombolysis DVT management. We would certainly have difficulty in conducting such a comparison because of cost issues in thrombolysis, as patients are self-payers and opt for conservative management. Limitations of our study includes retrospective review, loss to follow up and people unwilling to participate in the study.
Conclusion
Predictors that are independently associated with poor quality of life post DVT are PTS, inability to maintain therapeutic anticoagulation and ileofemoral DVT. This can be avoided in proper counselling of patients to comply with measures like compression stockings to avoid developing PTS and also educating on maintaining therapeutic anticoagulation.
Disclosure Statement
The authors declare no conflict of interest.
Author Contributions
Study conception: FAS, NAS, ZS
Data collection: SN, MAM
Analysis: NS, MAM
Investigation: NS
Writing: MAM, FAS, NAS
Funding: None
Critical review and revision: All authors
Final approval: All authors
Accountability for all aspects of work: All authors
References
- 1.Cohen AT, Agnelli G, Anderson FA, et al. Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb Haemost 2007; 98: 756-64. [DOI] [PubMed] [Google Scholar]
- 2.Rosencher N, Vielpeau C, Emmerich J, et al. Venous thromboembolism and mortality after hip fracture surgery: the ESCORTE study. J Thromb Haemost 2005; 3: 2006-14. [DOI] [PubMed] [Google Scholar]
- 3.Kahn SR, Lamping DL, Ducruet T, et al. VEINES-QOL/Sym questionnaire was a reliable and valid disease-specific quality of life measure for deep venous thrombosis. J Clin Epidemiol 2006; 59: 1049-56. [DOI] [PubMed] [Google Scholar]
- 4.Kahn SR. The post-thrombotic syndrome: progress and pitfalls. Br J Haematol 2006; 134: 357-65. [DOI] [PubMed] [Google Scholar]
- 5.Prandoni P, Lensing AW, Prins MR. Long-term outcomes after deep venous thrombosis of the lower extremities. Vasc Med 1998; 3: 57-60. [DOI] [PubMed] [Google Scholar]
- 6.ten Cate-Hoek AJ, Henke PK, Wakefield TW. The post thrombotic syndrome: ignore it and it will come back to bite you. Blood Rev 2016; 30: 131-7. [DOI] [PubMed] [Google Scholar]
- 7.Kahn SR, Shbaklo H, Lamping DL, et al. Determinants of health-related quality of life during the 2 years following deep vein thrombosis. J Thromb Haemost 2008; 6: 1105-12. [DOI] [PubMed] [Google Scholar]
- 8.Hedner E, Carlsson J, Kulich KR, et al. An instrument for measuring health-related quality of life in patients with Deep Venous Thrombosis (DVT): development and validation of Deep Venous Thrombosis Quality of Life (DVTQOL) questionnaire. Health Qual Life Outcomes 2004; 2: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Life Expectancy in Pakistan. World Life Expectancy. 2020. [cited 14 January 2020]. Available from: https://www.worldlifeexpectancy.com/pakistan-life-expectancy
- 10.Roberts LN, Patel RK, Donaldson N, et al. Post-thrombotic syndrome is an independent determinant of health-related quality of life following both first proximal and distal deep vein thrombosis. Haematologica 2014; 99: e41-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahn SR, Hirsch A, Shrier I. Effect of postthrombotic syndrome on health-related quality of life after deep venous thrombosis. Arch Intern Med 2002; 162: 1144-8. [DOI] [PubMed] [Google Scholar]
- 12.Prandoni P, Lensing AWA, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med 2004; 141: 249-56. [DOI] [PubMed] [Google Scholar]
- 13.Appelen D, van Loo E, Prins MH, et al. Compression therapy for prevention of post-thrombotic syndrome. Cochrane Database Syst Rev 2017; 9: CD004174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kahn SR, Ginsberg JS. Relationship between deep venous thrombosis and the postthrombotic syndrome. Arch Intern Med 2004; 164: 17-26. [DOI] [PubMed] [Google Scholar]
- 15.Van Dongen CJ, Prandoni P, Frulla M, et al. Relation between quality of anticoagulant treatment and the development of the postthrombotic syndrome. J Thromb Haemost 2005; 3: 939-42. [DOI] [PubMed] [Google Scholar]
- 16.Garratt AM, Ruta DA, Abdalla MI, et al. Responsiveness of the SF-36 and a condition-specific measure of health for patients with varicose veins. Qual Life Res 1996; 5: 223-34. [DOI] [PubMed] [Google Scholar]