Short abstract
Background
The infraorbital nerve (ION) and its canal are important landmarks during surgical approaches to the orbital floor and pterygopalatine fossa. However, variations in the anatomy of the infraorbital canal and its corresponding neurovascular bundle may impact the access.
Objective
To investigate anatomic variants of the infraorbital canal from a prelacrimal endoscopic perspective and to explore the impact of these variants on exposing the lateral orbital floor.
Methods
Ten cadaveric specimens (20 sides) were dissected through an endonasal prelacrimal approach. Anatomic variants of the ION including location, branching pattern, and relationship to the infraorbital artery were assessed. The need for ION transposition to increase exposure of the lateral orbital floor was also investigated.
Results
Incidence of previously described Types 1, 2, and 3 ION variants were 30.0%, 60.0%, and 10.0%, respectively. Although the orbital floor could be directly accessed in Type 1 and Type 3 IONs, transposition of the ION was necessary to expose the lateral orbital floor in 5 of 12 sides (42%) for Type 2 ION. Bony dehiscence of the orbital floor was identified in 8 of 20 sides (40%) and branching of the ION in 2 of 20 sides (10%).
Conclusion
Anatomic variations of the infraorbital canal impact surgical exposure of the orbital floor via a prelacrimal approach. Type 1 and Type 3 ION variants allow a direct exposure of the entire orbital floor. A Type 2 ION may require transposition of the nerve to adequately expose the lateral orbital floor.
Keywords: infraorbital nerve, infraorbital canal, orbital floor, prelacrimal approach, bone dehiscence, nerve branch, maxillary sinus, transposition
Introduction
Following the development of novel techniques and instrumentation, endonasal endoscopic approaches gained popularity for the surgical management of benign lesions of the maxillary sinus, orbital floor, and medial orbit.1–3 Infectious, traumatic, and neoplastic processes are common conditions affecting the maxillary sinus and orbital floor.4–7 Although the infraorbital canal and lateral orbital floor can be viewed with an angled endoscope through a maxillary antrostomy, it is difficult to manage lesions affecting these areas without resecting the lateral nasal wall (ie, medial maxillectomy).8–10 Therefore, multiple modifications of endoscopic transmaxillary approaches have been proposed to address lesions involving the orbital floor.7–10 Modified medial maxillectomy approaches have also been used to approach the infraorbital nerve (ION) and orbital floor.8,10–12 The ION is an important landmark during these and other approaches to the orbital floor, pterygopalatine fossa, infratemporal fossa, and anterolateral skull base.13–15 Its anatomical relationship with the orbital floor may impact its identification and the effectiveness of certain surgical approaches.
Ference et al. have reported 3 variants of the infraorbital canal from a radiographic perspective.16 Type 1 is defined as a canal that does not bulge into the maxillary sinus, while in Type 3, the infraorbital canal hangs in the maxillary sinus. Type 2 is an intermediate variant between these 2 Types. Although the importance of the ION as a surgical landmark has been described by multiple authors,8,17 a description of anatomic variants of the infraorbital canal from an endoscopic perspective has not been previously reported. Moreover, the variants of the ION and its canal may obstruct the endoscopic visualization of the lateral orbital floor as well as impact the degree of access.
As an anterior endoscopic approach, the prelacrimal approach was designed by Zhou et al. to address lesions in the prelacrimal recess of the maxillary sinus while preserving the lateral nasal wall and nasolacrimal duct.18 Using this approach, the entire maxillary sinus including the orbital floor is directly visualized. The similar technique for the management of lesions in the maxillary sinus and inferior orbit via endonasal approach was also reported by Sieskiewicz et al.19 This study aimed to investigate the endoscopic morphology of the infraorbital canal considering its anatomic variants and to explore the correlation between the location of infraorbital canal and exposure of the lateral orbital floor through an endonasal prelacrimal approach.
Methods
This study was conducted at the Anatomy Laboratory Toward Visuospatial Surgical Innovations in Otolaryngology and Neurosurgery (ALT-VISION) at the Wexner Medical Center of The Ohio State University. ALT-VISION and all coauthors to perform this study have been certified by regulatory agencies dealing with the use of human tissues and cadaveric studies in The Ohio State University. An endoscopic prelacrimal approach to the ION and orbital floor was performed in 10 injected adult cadaveric specimens (20 sides). All specimens were fresh and had undergone an intravascular injection of blue and red latex to highlight the vasculature. After thawing, they were preserved in 70% alcohol.
Visualization was achieved using rigid rod-lens endoscopes (4-mm diameter, 18-cm length) with 0°, 30°, and 45° scopes (Karl Storz Endoscopy; Karl Storz, Tuttlingen, Germany), coupled to a high-definition camera and video monitor. Both video and standard digital images were recorded during dissections using the AIDA recording system (Karl Storz Endoscopy; Karl Storz). A high-resolution computed tomography scan was performed before the dissection, and the digital data were exported to a navigational system (Stryker, Kalamazoo, MI).
Steps for an endonasal prelacrimal approach include
First, a vertical incision is made in the mucoperiosteum of the lateral wall of the nasal cavity, between the pyriform aperture and anterior portion of the inferior turbinate, extending inferiorly to the floor of the nose.
Remove the bony attachment of the inferior turbinate with a high-speed drill to expose the nasolacrimal duct and enter the maxillary sinus.
Partial removal of the medial and anterior walls of the maxillary sinus and displace the nasolacrimal duct medially to increase instrument maneuverability.
Under endoscopic visualization, the ION was classified according to their relationship to the orbital floor following Ference’s radiologic description16: Type 1, the ION was completely located in the infraorbital groove with no bulging into the maxillary sinus; Type 2, the ION was partially protruded into the maxillary sinus; and Type 3, the ION hanged in the maxillary sinus with no attachment to the orbital floor. Parameters including the type of ION, extent of the orbital floor exposure, bony deficiency of the orbital floor, relative location of the infraorbital artery to the ION, and the requirement of ION transposition to expose the lateral orbital floor were recorded.
Results
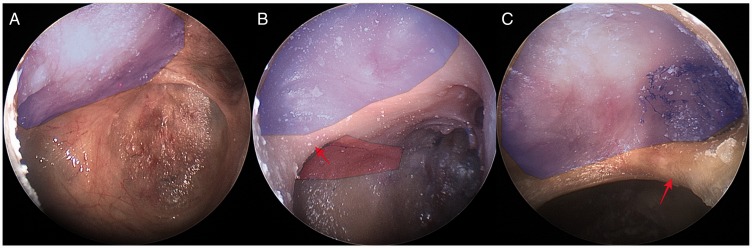
In this study sample, all 3 types of infraorbital canal variants were identified (Figure 1). Type 1, Type 2, and Type 3 IONs were found in 30.0% (6 of 20 sides), 60.0% (12 of 20 sides) and 10.0% (2 of 20 sides), respectively. Orbital floors with Type 1 and Type 3 ION variants could be directly exposed with a 0° scope. In addition, there were some relevant observations:
Figure 1.
Representative images demonstrating 3 types of infraorbital canal (arrows in B and C) as seen through an endonasal prelacrimal approach. A, Type 1 (right maxillary sinus). B, Type 2 (right maxillary sinus). C, Type 3 (left maxillary sinus). The highlighted portions in (A) and (C) show the entire orbital floor; the blue highlighted portion in (B) represents medial orbital floor, the red represents the lateral orbital floor.
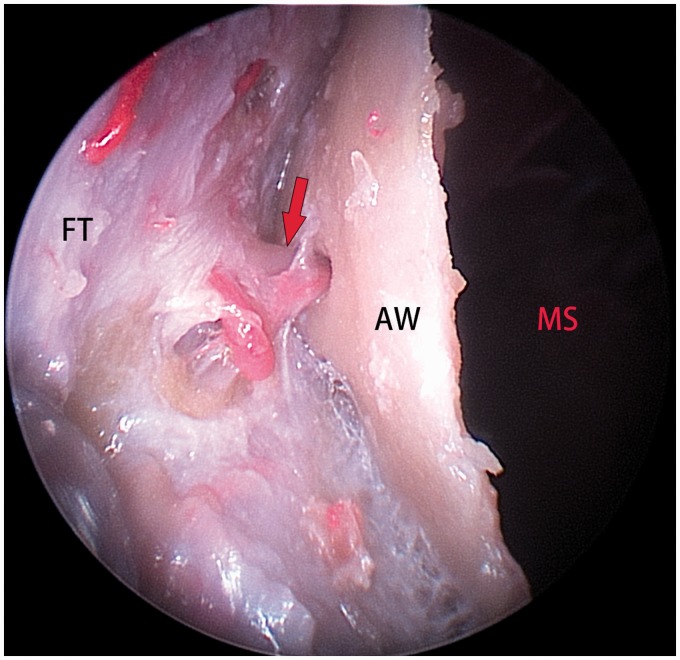
In Type 1, the infraorbital canal does not bulge into the maxillary sinus; therefore, the infraorbital foramen through the anterior wall of maxillary sinus could be used for identification of the ION (Figure 2).
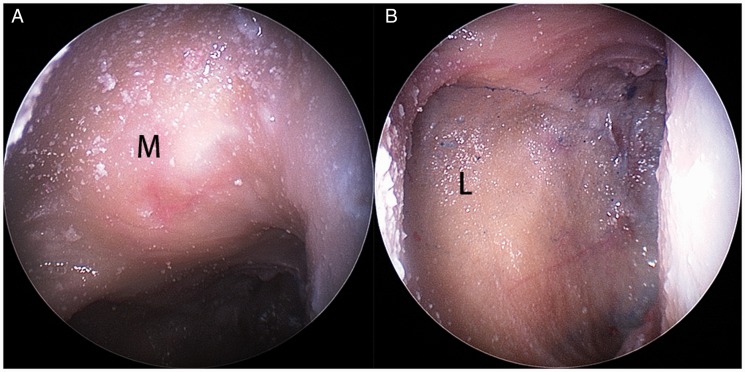
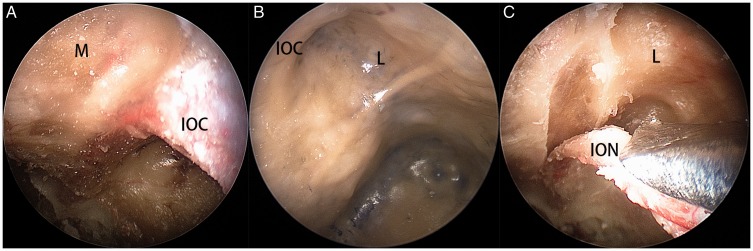
In Type 2, the infraorbital canal divided the orbital floor into medial and lateral aspects (Figure 3). In 5 of 12 sides, a direct view of the lateral orbital floor through a prelacrimal approach was obscured by the infraorbital canal (Figure 4(A)), and an angled endoscope (Figure 4(B)) or transposition of the ION was required (Figure 4(C)) to expose the lateral orbital floor.
In Type 3, the infraorbital canal hangs in the maxillary sinus and the entire orbital floor lying above the infraorbital canal (Figure 1(C)).
Figure 2.
In Type 1, no bulge of the canal could be identified in the orbital floor, and the infraorbital foramen (arrow) could be used to identify the infraorbital nerve. AW, anterior wall of maxillary sinus; FT, facial tissue; MS, maxillary sinus (right side).
Figure 3.
In Type 2, the orbital floor is divided into medial (A) and lateral (B) aspects by infraorbital canal. L, lateral; M, medial.
Figure 4.
In 5 sides of specimens with Type 2 ION, the direct view of lateral orbital floor was obscured by infraorbital canal (A), it could be inspected with angled endoscope (B), or the infraorbital nerve was inferiorly transposed for direct exposure (C). IOC, infraorbital canal; ION, infraorbital nerve; L, lateral orbital floor; M, medial orbital floor.
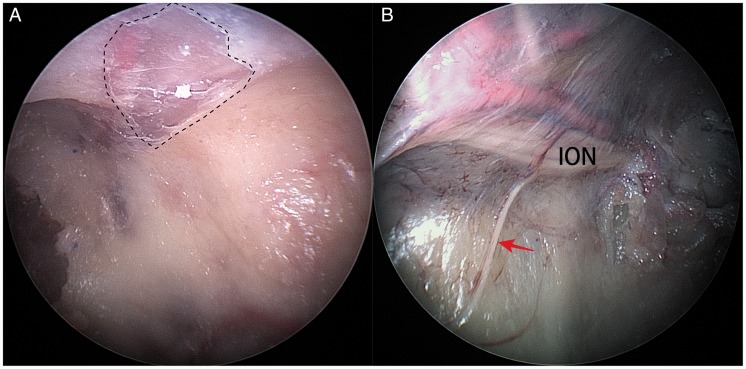
Other variants including bony dehiscence (Figure 5(A)) and branching from the ION (Figure 5(B)) were also observed. Bony dehiscence of the orbital floor was found in 8 of 20 sides (40%) and mainly occurred in Type 2 and Type 3 ION variants. In 2 of 20 sides (10%) of all specimens, a branch of the ION could be identified in the maxillary sinus.
Figure 5.
The bony dehiscence of the orbital floor (A, enclosed portion) and branch from the infraorbital nerve into the maxillary sinus could also be detected (B, arrow). ION, infraorbital nerve.
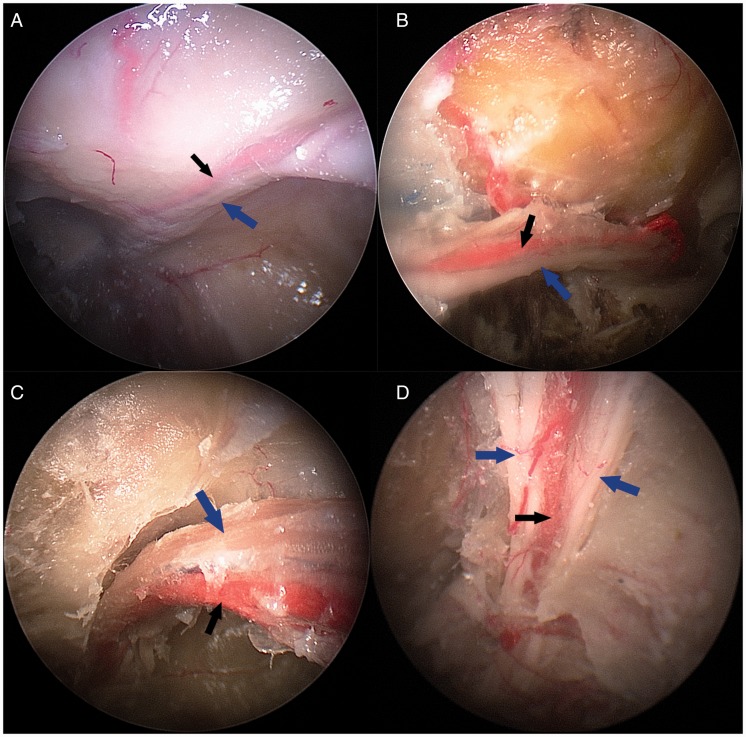
The infraorbital artery was located medial, superior, inferior, or between the branches of the ION (Figure 6). However, the artery was most frequently located medial to the ION (15 of 20).
Figure 6.
Correlation between the infraorbital artery (black arrows) and infraorbital nerve (blue arrows): (A) medial, (B) above, (C) inferior, and (D) between the branches of ION. A, C, and D, Left maxillary sinus. B, Right maxillary sinus (For interpretation of the references to colours in this figure legend, refer to the online version of this article).
One of the 20 sides (5%) showed hypoplasia of maxillary sinus. Although the orbital floor could be exposed, the maneuverability within the sinus through an endonasal prelacrimal approach was limited.
Discussion
The orbital floor lateral to the ION is difficult to access through a mid-meatal antrostomy.6 As opposed to extended medial maxillectomy, the prelacrimal approach adopted in this study preserves the inferior turbinate and the nasolacrimal duct, which may aid in preservation of postoperative nasal and lacrimal functions.20 Exposure of the orbital floor via an endonasal prelacrimal approach was feasible in 19 of 20 sides. However, it was not suitable in one side with hypoplasia of maxillary sinus. Moreover, the prelacrimal approach also provides an alternative to avoid a sublabial incision and its related postoperative complications.21
This study differed from previous reports regarding the incidence of anatomical variants of the infraorbital canal.16 Ference’s radiographic study showed an incidence of Type 1, Type 2, and Type 3 infraorbital canal of 60.5%, 27%, and 12.5%, respectively.16 However, in this anatomical study, the incidence of Type 1, Type 2, and Type 3 was 30.0%, 60.0%, and 10.0%, respectively. The main differences in these 2 studies corresponded to the incidences of IONs Type 1 and Type 2. However, one should note that the sample size in this study was significantly smaller than Ference’s (200 sides), and that the ION canal was examined through an endoscopic approach as opposed to a radiologic assessment.
From a practical standpoint, a Type 1 infraorbital canal implies that it does not bulge into the maxillary sinus; thus, the roof of the antrum will be easily visualized including the lateral orbital floor. In a Type 3 variant, the entire orbital floor is located above the level of the ION; thus, it is also easily exposed with a 0° scope. Conversely, the lateral orbital floor could not be directly accessed in 42% of Type 2 ION variants. In this setting, an inferiorly transposition of ION is helpful to expose the lateral orbital wall directly with a 0° scope. Alternatively, the lateral orbital floor could be exposed using angled endoscopes and instruments. In our opinion, however, direct exposure potentially facilitates the visualization and management in complex situations such as residual or recurrent tumor, foreign body, and fracture located at the lateral aspect of the canal.10 Furthermore, manipulation of the ION rarely leads to significant morbidity.5
The ION may be used as a landmark to identify V2 and provides an important landmark in surgeries of the pterygopalatine fossa and infratemporal fossa.15 However, it may be difficult to discern when its canal does not bulge into the maxillary sinus (Type 1).6 In this situation, a surgical navigation device can help to locate the ION in the orbital floor or one can use the infraorbital foramen at the anterior wall of maxillary sinus to identify the ION as one dissects posteriorly.
Another surgical consideration is the location of the infraorbital artery reported by Kazkayasi et al. to be always located in the superomedial location to the ION.22 In this study, the artery location was variable, running medial, superior, inferior, or between the branches of ION. Among these, the medial location was most common, which is consistent with a previous report.22 No artery, however, was identified lateral to the ION. The infraorbital artery may therefore not be a reliable landmark to identify the ION in surgery.
In this study, 8 of 20 sides (40%) of the specimens demonstrated a bony dehiscence of the orbital floor. These mostly occurred in the inferior wall of infraorbital canal in Type 2 and Type 3 ION variants. Bony dehiscence of the orbital floor might provide pathways for tumor extension22 or spread of infection23 from the maxillary sinus to the orbit.
Maxillary sinus surgeries may lead to postoperative facial hypesthesia.24,25 Interestingly, branches of the ION in the posterolateral wall of the maxillary sinus could be identified in 2 of 20 sides. These branches of the ION were covered by mucosa, but no bone, and were located in the middle to inferior part of the maxillary sinus. We considered that the small branches of ION may not have been previously appreciated, as inflammation or polyps may impede visualization of these variants. Damage to these branches may potentially contribute to the postoperative hypesthesia in some settings.24
This study comprises several limitations that need to be considered:
It is a cadaveric study, and its applications in live surgery still need to be evaluated.
The prelacrimal approach offers limited space for instrumentation. It is not wide enough to use a 4-mm endoscope and 2 instruments simultaneously; therefore, it is challenging for 4-hand technique. For management of complex situations in the lateral orbital floor, the approach may be extended laterally incorporating the anterior maxillary wall. Alternatively, the prelacrimal approach may be complemented with an endonasal mid-meatal maxillary window.
The morbidity related to transposition of the ION still requires clinical validation.
Conclusion
Variations of the infraorbital canal impact the exposure of the orbital floor via an endonasal approach. For Type 1 and Type 3 IONs, the entire orbital floor could be exposed directly. Transposition of the Type 2 ION increases the exposure to the lateral orbital floor, when the infraorbital canal blocked direct access. Bony dehiscence of the orbital floor and branches of the ION into the maxillary sinus might correlate with spread of infection or tumor from the maxillary sinus to the orbit and postoperative facial hypesthesia, respectively.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Kennedy DW, Goodstein ML, Miller NR, Zinreich SJ. Endoscopic transnasal orbital decompression. Arch Otolaryngol Head Neck Surg. 1990; 116:275–282. [DOI] [PubMed] [Google Scholar]
- 2.Herman P, Lot G, Silhouette B, et al. Transnasal endoscopic removal of an orbital cavernoma. Ann Otol Rhinol Laryngol. 1999; 108:147–150. [DOI] [PubMed] [Google Scholar]
- 3.Michel O. Transnasal surgery of the orbita. Review of current indications and techniques. HNO. 2000; 48:4–17. [DOI] [PubMed] [Google Scholar]
- 4.Ikeda K, Oshima T, Suzuki H, Kikuchi T, Suzuki M, Kobayashi T. Surgical treatment of subperiosteal abscess of the orbit: Sendai’s ten-year experience. Auris Nasus Larynx. 2003; 30:259–262. [DOI] [PubMed] [Google Scholar]
- 5.He S, Bakst RL, Guo T, Sun J. A combination of modified transnasal endoscopic maxillectomy via transnasal prelacrimal recess approach with or without radiotherapy for selected sinonasal malignancies. Eur Arch Otorhinolaryngol. 2015; 272:2933–2938. [DOI] [PubMed] [Google Scholar]
- 6.Nam Y, Bahk S, Eo S. Anatomical study of the infraorbital nerve and surrounding structures for the surgery of orbital floor fractures. J Craniofac Surg. 2017; 28:1099–1104. [DOI] [PubMed] [Google Scholar]
- 7.Ali MJ, Murphy J, James CL, Wormald PJ. Perineural squamous cell carcinoma infiltration of infraorbital nerve treated with endoscopic nerve resection up to foramen rotundum. Clin Exp Ophthalmol. 2015; 43:288–290. [DOI] [PubMed] [Google Scholar]
- 8.Kasemsiri P, Solares CA, Carrau RL, et al. Endoscopic endonasal transpterygoid approaches: anatomical landmarks for planning the surgical corridor. Laryngoscope. 2013; 123:811–815. [DOI] [PubMed] [Google Scholar]
- 9.Salzano G, Turri-Zanoni M, Karligkiotis A, et al. Infraorbital nerve transposition to expand the endoscopic transnasal maxillectomy. Int Forum Allergy Rhinol. 2017; 7:149–153. [DOI] [PubMed] [Google Scholar]
- 10.Lyson T, Sieskiewicz A, Rogowski M, Mariak Z. The transmaxillary endoscopic approach to the inferior part of the orbit: how I do it. Acta Neurochir (Wien). 2015; 157:625–628. [DOI] [PubMed] [Google Scholar]
- 11.Schultheiss S, Petridis AK, El Habony R, Maurer P, Scholz M. The transmaxillary endoscopic approach to the orbit. Acta Neurochir (Wien). 2013; 155:87–97. [DOI] [PubMed] [Google Scholar]
- 12.Har-El G. Combined endoscopic transmaxillary-transnasal approach to the pterygoid region, lateral sphenoid sinus, and retrobulbar orbit. Ann Otol Rhinol Laryngol. 2005; 114:439–442. [DOI] [PubMed] [Google Scholar]
- 13.Gao L, Zhou L, Dai Z, Huang X. The endoscopic prelacrimal recess approach to the pterygopalatine fossa and infratemporal fossa. J Craniofac Surg. 2017; 28:1589–1593. [DOI] [PubMed] [Google Scholar]
- 14.Elhadi AM, Zaidi HA, Yagmurlu K, et al. Infraorbital nerve: a surgically relevant landmark for the pterygopalatine fossa, cavernous sinus, and anterolateral skull base in endoscopic transmaxillary approaches. J Neurosurg. 2016; 125:1460–1468. [DOI] [PubMed] [Google Scholar]
- 15.Alfieri A, Jho HD, Schettino R, Tschabitscher M. Endoscopic endonasal approach to the pterygopalatine fossa: anatomic study. Neurosurgery. 2003; 52:374–378; discussion 378–380. [DOI] [PubMed] [Google Scholar]
- 16.Ference EH, Smith SS, Conley D, Chandra RK. Surgical anatomy and variations of the infraorbital nerve. Laryngoscope. 2015; 125:1296–1300. [DOI] [PubMed] [Google Scholar]
- 17.Fyrmpas G, Konstantinidis I, Constantinidis J. Endoscopic treatment of juvenile nasopharyngeal angiofibromas: our experience and review of the literature. Eur Arch Otorhinolaryngol. 2012; 269:523–529. [DOI] [PubMed] [Google Scholar]
- 18.Zhou B, Han DM, Cui SJ, Huang Q, Wang CS. Intranasal endoscopic prelacrimal recess approach to maxillary sinus. Chin Med J (Engl). 2013; 126:1276–1280. [PubMed] [Google Scholar]
- 19.Sieskiewicz A, Piszczatowski B, Olszewska E, Lukasiewicz A, Tarasow E, Rogowski M. Minimally invasive transnasal medial maxillectomy for treatment of maxillary sinus and orbital pathologies. Acta Otolaryngol. 2014; 134:290–295. [DOI] [PubMed] [Google Scholar]
- 20.Zhou B, Huang Q, Shen PH, et al. The intranasal endoscopic removal of schwannoma of the pterygopalatine and infratemporal fossae via the prelacrimal recess approach. J Neurosurg. 2016; 124:1068–1073. [DOI] [PubMed] [Google Scholar]
- 21.Zhou B, Huang Q, Cui SJ, et al. Removal of schwannoma in the pterygopalatine and infratemporal fossa via endoscopic prelacrimal recess approach. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2013; 48:802–806. [PubMed] [Google Scholar]
- 22.Kazkayasi M, Ergin A, Ersoy M, Tekdemir I, Elhan A. Microscopic anatomy of the infraorbital canal, nerve, and foramen. Otolaryngol Head Neck Surg. 2003; 129:692–697. [DOI] [PubMed] [Google Scholar]
- 23.Erickson BP, Lee WW. Orbital cellulitis and subperiosteal abscess: a 5-year outcomes analysis. Orbit. 2015; 34:115–120. [DOI] [PubMed] [Google Scholar]
- 24.Robinson SR, Baird R, Le T, Wormald PJ. The incidence of complications after canine fossa puncture performed during endoscopic sinus surgery. Am J Rhinol. 2005; 19:203–206. [PubMed] [Google Scholar]
- 25.Cho SE, Shin HS, Tak MS, et al. A rare complication of infraorbital nerve hyperesthesia in surgically repaired orbital fracture patients. J Craniofac Surg. 2017; 28:e233–e234. [DOI] [PubMed] [Google Scholar]