Short abstract
Objective
Polymeric (Hem-o-lok) clips represent a novel technique with which to ligate the appendiceal stump following laparoscopic appendectomy. We compared the outcomes of using polymeric clips versus endostaplers for complicated and uncomplicated appendicitis.
Methods
Six hundred seventy-three consecutive patients undergoing laparoscopic appendectomy with polymeric clips or endostaplers for acute appendicitis were assessed. The primary outcome was the incidence of intra-abdominal abscesses. Predictors of postoperative intra-abdominal abscesses were calculated using univariate and multivariate analyses.
Results
Polymeric clips were used in 65% of patients and endostaplers were used in 35%. Hem-o-lok clips were not only applied in patients with uncomplicated appendicitis (83%), but also in those with complicated appendicitis (26%). The frequency of intra-abdominal abscesses using polymeric clips and endostaplers was similar in both patients with uncomplicated appendicitis (1% vs. 3%, respectively) and complicated appendicitis (2% vs. 6%, respectively). The univariate and multivariate analyses showed that the stump closure technique was not a risk factor for postoperative abscesses.
Conclusions
Closure of the appendiceal stump using the nonabsorbable Hem-o-lok ligation system in patients with both uncomplicated and complicated appendicitis is a safe alternative to the application of endostaplers.
Keywords: Abscess, appendectomy, clip, endostapler, appendiceal stump, appendicitis
Introduction
Laparoscopic appendectomy is the treatment of choice for acute appendicitis.1–4 Its advantages include a shorter hospital stay, earlier return to normal activity, and fewer wound infections. However, the increased incidence of intra-abdominal abscesses remains the “Achilles’ heel” of laparoscopic appendectomy. This complication can be seen in up to 5% of patients.3
The optimal technique of appendiceal stump closure is still under discussion because it is assumed to affect the occurrence of intra-abdominal abscesses. Endoloops and endostaplers are the most commonly applied techniques for laparoscopic appendectomy.3,5–9 We recently reported that closure of the appendiceal stump using polymeric clips instead of endoloops reduces the rate of intra-abdominal abscess formation.10 The use of polymeric clips, a Hem-o-lok ligation system, is relatively new in laparoscopic appendectomy.11–17 These clips are characterized by easy and safe handling and are considerably less expensive than endostaplers. Some surgical departments routinely use endostaplers for laparoscopic appendectomy.7 However, surgeons are increasingly preferring endostaplers to treat complicated appendicitis (inflamed appendix base or perforation).18 In particular, the use of polymeric clips has been described in the treatment of uncomplicated appendicitis with an unaffected appendix base, similarly to endoloops.10
We hypothesized that appendiceal stump closure using polymeric clips is not inferior to that using staplers in uncomplicated and complicated appendicitis. Therefore, in the present study, we assessed the outcomes following appendiceal stump closure with Hem-o-lok clips versus endostaplers.
Patients and methods
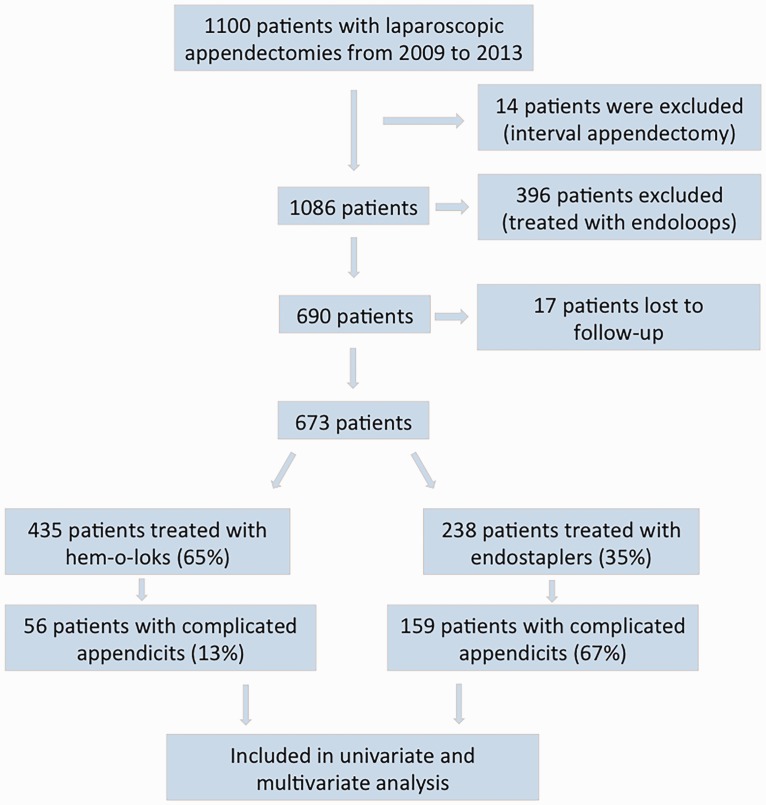
In this retrospective cohort study, we compared the outcomes of patients treated with staplers versus polymeric clips for appendicitis. Patients who underwent laparoscopic appendectomy from 2009 to 2013 were included in the present study. All consecutive patients treated with Hem-o-lok clips or endostaplers were included. Appendectomies were performed according to the surgeon’s preference. The patients were divided into two groups based on the method of securing the appendiceal stump (Hem-o-lok clips or endostaplers). The patients were further subgrouped into those with complicated and uncomplicated appendicitis. Complicated appendicitis was defined as perforation or necrosis of the appendix as well as inflammation at the base of the appendix or cecum. If postoperative antibiotics were administered, a combination of either amoxicillin/clavulanic acid or ceftriaxone/metronidazole was given. The exclusion criteria were application of endoloops, interval appendectomy, and open appendectomy (Figure 1).
Figure 1.
Flow chart of patients included in the study and multivariate analysis
The primary outcome was the incidence of postoperative intra-abdominal abscesses. The secondary outcomes were the readmission rate, reoperation rate, length of hospital stay, operative costs, and operation time.
The operation costs were calculated as follows: The price for one Hem-o-lok clip XL kit (Weck® Teleflex, Belp, Switzerland) containing five clips was EUR25. One endostapler (Multifire Endo GIA™ 30, 3.5 mm; Covidien, Wollerau, Switzerland) cost EUR360. The price of 1 minute in the operating room was EUR32; this included the costs for the staff, salaries, and general equipment.
This study was approved by the ethics committee of Zurich (KEK-ZH: 2013-0514) and conducted in accordance with the Swiss Human Research Act. Because of the retrospective nature of the study, written or verbal informed consent was not applicable or necessary.
Surgical procedure
Single-shot antibiotic prophylaxis was administered to all patients 30 to 60 minutes before surgery (amoxicillin/clavulanic acid at 2 g/200 mg for adults and 33 mg/3 mg/kg for children <40 kg or ceftriaxone/metronidazole at 2 g/1 g for adults and 50 mg/7.5 mg/kg for children <40 kg). An open technique (Hasson) was used to enter the abdomen under direct vision at the umbilicus. Three-port laparoscopic appendectomy was performed with a 10-mm camera (Karl Storz, Germany) port at the umbilicus and two working ports in the left lower quadrant (12 mm for stapled appendectomy and 10 mm for appendectomy using Hem-o-lok clips) and above the symphysis (5 mm), respectively. Pneumoperitoneum was set at a pressure of 12 mmHg. The mesoappendix was divided using bipolar diathermy (Karl Storz, Germany). For stapled appendectomy, a linear stapler (Multifire Endo GIA™ 30, 3.5 mm; Covidien) was used. In patients treated with polymeric clips (size XL; Weck® Teleflex), the appendix base was divided between the two proximal clips and one distal clip. The appendix was removed in an endo bag (Unimax Medical Systems, New Taipei City, Taiwan) via the paraumbilical incision.
Statistical analysis
Continuous variables are shown as median and interquartile range (IQR). Pearson’s χ2 test or Fisher’s exact test (dichotomous data) and the Mann–Whitney U test (categorical data) were applied. Univariate analysis was performed to identify clinical variables contributing to intra-abdominal abscess formation. Multiple logistic regression analysis was performed using variables from the univariate analysis with p < 0.200 and variables of special interest (technique of resection). Two-sided p values of <5% were regarded as significant. IBM SPSS Statistics for Windows, Version 21 (IBM Corp., Armonk, NY, USA) was used for analysis.
Results
In total, 673 patients were included in this study. The appendiceal stump was secured using Hem-o-lok clips in 435 (65%) patients and using endostaplers in 238 (35%) patients. Of the 673 patients, 215 had complicated appendicitis and 458 had uncomplicated appendicitis. The patients’ characteristics were similar between the Hem-o-lok and endostapler groups with regard to sex, American Society of Anesthesiologists grade, and preoperative white blood count (Table 1). The patients treated with staplers were older than those treated with clips (p < 0.001), and patients treated with staplers had a higher preoperative C-reactive protein level (p < 0.001), more often had perforated appendicitis (p < 0.001), and more often received postoperative antibiotics (p < 0.001) (Table 1).
Table 1.
Data of all patients.
| Hem-o-lok | Endostapler | p | |
|---|---|---|---|
| Patients | n = 435 | n = 238 | |
| Age, years | 27 (19–40) | 40 (25–56) | <0.001 |
| Age ≤16 years | n = 67 | n = 28 | 0.205 |
| Male/female | 233/202 (54%/46%) | 128/110 (54%/46%) | 1.000 |
| ASA grade I–II/III | 425/10 (98%/2%) | 230/8 (97%/3%) | 0.457 |
| WBC count ≥13 × 109/L | 13 (10–16) | 13 (11–16) | 0.760 |
| CRP ≥51 mg/L | 14 (4–45) | 48 (15–127) | <0.001 |
| Postoperative antibiotic treatment | 87 (20%) | 138 (58%) | <0.001 |
| Acute appendicitis (non-perforated) | 367 (84%) | 137 (58%) | <0.001 |
| Perforated appendicitis | 39 (9%) | 89 (37%) | <0.001 |
| No pathology | 15 (3%) | 4 (3%) | 0.229 |
| Other pathology | 11 (3%) | 8 (3%) | 0.627 |
Data are presented as median (interquartile range) or n (%) unless otherwise indicated.
ASA, American Society of Anesthesiologists; WBC, white blood cell; CRP, C-reactive protein.
Endostaplers were used in the majority of patients with complicated appendicitis (endostapler group, n = 159; Hem-o-lok group, n = 56). The patient demographics were similar between the two groups except that perforations occurred more frequently in the Hem-o-lok than endostapler group (70% vs. 56%, respectively; p = 0.024), while inflammation of the base of the appendix occurred more often in the endostapler than Hem-o-lok group (77% vs. 25%, respectively; p < 0.001) (Table 2).
Table 2.
Data of patients subgrouped into complicated and uncomplicated appendicitis.
| Complicated appendicitis |
Uncomplicated appendicitis |
|||||
|---|---|---|---|---|---|---|
| Hem-o-lok | Endostapler | p | Hem-o-lok | Endostapler | p | |
| Patients | n = 56 | n = 159 | n = 379 | n = 79 | ||
| Age ≥40 years | 28 (50%) | 93 (58%) | 0.278 | 84 (22%) | 28 (35%) | 0.015 |
| Age ≤16 years | 6 (10%) | 16 (10%) | 1.000 | 61 (16%) | 12 (15%) | 0.735 |
| Male/female | 36/20 (64%/36%) | 88/71 (55%/45%) | 0.273 | 197/182 (52%/48%) | 40/39 (51%/49%) | 0.902 |
| ASA grade I–II/III | 54/2 (96%/4%) | 152/7 (96%/4%) | 1.000 | 371/8 (98%/2%) | 78/1 (99%/1%) | 1.000 |
| WBC count ≥13 × 109/L | 27 (48%) | 87 (56%) | 0.438 | 177 (47%) | 31 (39%) | 0.264 |
| CRP ≥51 mg/L | 32 (57%) | 99 (62%) | 0.527 | 78 (21%) | 21 (27%) | 0.233 |
| Postoperative antibiotic treatment | 36 (64%) | 115 (72%) | 0.489 | 51 (13%) | 23 (29%) | 0.001 |
| Perforation | 39 (70%) | 89 (56%) | 0.024 | |||
| Perforation at the appendix base | 2 (4%) | 18 (11%) | 0.111 | |||
| Inflammation at the base of the appendix | 14 (25%) | 122 (77%) | <0.001 | |||
| Necrosis | 17 (30%) | 43 (27%) | 0.604 | |||
Data are presented as n (%) unless otherwise indicated.
ASA, American Society of Anesthesiologists; WBC, white blood cell; CRP, C-reactive protein.
In patients with uncomplicated appendicitis, the appendiceal stump was mainly closed using polymeric clips (Hem-o-lok group, n = 379; endostapler group, n = 79). More patients aged ≥40 years were treated with endostaplers (p = 0.015), and postoperative antibiotics were administered more often in the stapler group (29% vs. 13%; p = 0.001). The characteristics of the two groups were similar among patients with uncomplicated appendicitis (Table 2).
The median calculated operation cost using Hem-o-lok clips was EUR1993 (IQR, 1625–2553), and that using endostaplers was EUR2792 (IQR, 2280–3408; p < 0.0001).
In patients with complicated appendicitis, the incidence of postoperative abscesses and the readmission rate were higher following stapled appendectomy, but not significantly. The operation time was slightly and non-significantly longer in patients treated with staplers. The length of hospital stay was similar, and only three patients in total required a reoperation (two in the stapler group and one in the Hem-o-lok group).
Complications (intra-abdominal abscesses, readmissions, and reoperations) and the length of hospital stay were similar between the two groups among patients with uncomplicated appendicitis. The operation time was slightly longer (median, 7 minutes), but not significantly, following stapled appendectomy (Table 3).
Table 3.
Outcomes in patients with complicated and uncomplicated appendicitis.
| Complicated appendicitis |
Uncomplicated appendicitis |
|||||
|---|---|---|---|---|---|---|
| Hem-o-lok | Endostapler | p | Hem-o-lok | Endostapler | p | |
| Patients | n = 56 | n = 159 | n = 379 | n = 79 | ||
| Intra-abdominal abscesses | 1 (2%) | 10 (6%) | 0.295 | 4 (1%) | 2 (3%) | 0.277 |
| Readmissions | 1 (2%) | 11 (7%) | 0.192 | 15 (4%) | 3 (4%) | 1.000 |
| Reoperations | 1 (2%) | 2 (1%) | 0.932 | 3 (0.8%) | 1 (1%) | 1.000 |
| OR time, minutes | 73 (61–94) | 79 (62–100) | 0.188 | 59 (49–77) | 66 (53–83) | 0.068 |
| Hospital stay, days | 5 (3–6) | 5 (3–7) | 0.519 | 3 (3–4) | 3 (2–4) | 0.835 |
Data are presented as median (interquartile range) or n (%) unless otherwise indicated.
OR, operating room.
A univariate analysis was performed to assess risk factors for intra-abdominal abscess formation in patients with complicated appendicitis. Among the factors assessed, only perforation was correlated with intra-abdominal abscess formation (p = 0.031) (Table 4). Correspondingly, in the multivariate regression analysis, perforation of the appendix was the only independent predictor of postoperative intra-abdominal abscesses (p = 0.048).
Table 4.
Univariate analysis for postoperative intra-abdominal abscesses.
| Intra-abdominal abscess | Yes | No | p | ||
|---|---|---|---|---|---|
| Resection technique | |||||
| Hem-o-lok vs. | 1 | (9%) | 55 | (27%) | 0.295 |
| endostapler | 10 | (91%) | 149 | (73%) | |
| Age > 16 years | 9 | (82%) | 184 | (90%) | 0.313 |
| Age ≤ 16 years | 2 | (18%) | 20 | (10%) | |
| Age > 40 years | 5 | (45%) | 116 | (57%) | 0.540 |
| Age ≤ 40 years | 6 | (55%) | 88 | (43%) | |
| Male | 6 | (55%) | 118 | (58%) | 1.000 |
| Female | 5 | (45%) | 86 | (42%) | |
| ASA grade III | 2 | (18%) | 7 | (3%) | 0.070 |
| non-ASA grade III | 9 | (82%) | 197 | (97%) | |
| White blood cell count | |||||
| ≥13 × 109/L | 4 | (36%) | 110 | (54%) | 0.355 |
| ≤13 × 109/L | 7 | (64%) | 94 | (46%) | |
| Blood plasma level of CRP | |||||
| ≥51 mg/L | 5 | (45%) | 126 | (62%) | 0.346 |
| ≤51 mg/L | 6 | (55%) | 78 | (38%) | |
| Histology | |||||
| Perforated appendicitis | 10 | (91%) | 118 | (58%) | 0.031 |
| No perforation | 1 | (9%) | 86 | (42%) | |
| Antibiotic treatment | |||||
| Yes | 10 | (91%) | 141 | (69%) | 0.182 |
| No | 1 | (9%) | 63 | (31%) | |
| Operative duration | |||||
| ≤60 minutes | 3 | (27%) | 37 | (18%) | 0.433 |
| >60 minutes | 8 | (73%) | 167 | (82%) | |
Data are presented as n (%).
ASA, American Society of Anesthesiologists; CRP, C-reactive protein.
Discussion
The present study assessed the outcomes following appendiceal stump closure using polymeric (Hem-o-lok) clips versus staplers in patients with complicated and uncomplicated appendicitis. Among the outcomes assessed (incidence of postoperative intra-abdominal abscesses, readmission rate, reoperation rate, length of hospital stay, operative costs, and operation time), Hem-o-lok clips were non-inferior to staplers in both patients with complicated and uncomplicated appendicitis. More precisely, in patients with complicated appendicitis, the incidence of postoperative abscesses and the readmission rate were higher following stapled appendectomy, but not significantly. The operation time was slightly and non-significantly longer following stapled appendectomy in both patients with complicated and uncomplicated appendicitis, and the calculated operative costs were higher using a stapler. Among the risk factors assessed, only perforated appendicitis was correlated with intra-abdominal abscess formation.
Different methods are used to close the appendiceal stump, including endoloops, staplers, polymeric clips, and intracorporeal knots; among these, endoloops and staplers are the most commonly employed.19–22 Polymeric clips have primarily been used for vessel and tissue ligation and have been shown to be a safe alternative to endoloops in the treatment of uncomplicated appendicitis with a non-inflamed or only moderately inflamed appendix base measuring <10 mm.10,15,23,24 The handling of polymeric clips is technically easy, resulting in a shallow learning curve and short operation time.19,25 Unlike comparisons between polymeric clips and endoloops, studies assessing appendiceal stump closure with polymeric clips versus staplers are sparse in the literature.14,26,27 Only one such randomized controlled trial has been published; this trial included 30 patients treated with polymeric clips and 30 patients treated with staplers.26 To the best of our knowledge, the present study included the largest cohort of patients comparing polymeric clips and staplers. Our data suggest that polymeric clips are not inferior to staplers and may also be safely used in patients with perforated appendicitis. The non-inferiority corresponds to findings by other research groups. However, only a minor proportion of published appendiceal stump closures were performed in patients with perforated appendicitis, and no subgroup analysis of laparoscopic appendectomy using staplers versus polymeric clips in patients with perforated appendicitis has been published.14,26,27 Stapled appendectomy is expensive, fast, and reliable even in cases of inflammation at the base of the appendix.28 With the exception of an inflamed appendix base, staplers do not seem to be superior to endoloops or polymeric clips and are not recommended for use as standard treatment by many authors.27,29 Similarly, in our cohort of patients for whom the decision to use staplers versus clips was based on clinical findings, only a minor proportion was treated with polymeric clips when the appendix base was inflamed. Stapled appendectomy was more expensive then using polymeric clips in our patient cohort, which is not surprising given the higher price of a stapler than polymeric clips and the similar operation time. The operating room cost at our hospital is calculated at EUR32 (USD37) per minute, which is rather low when compared with the average in US hospitals (USD62/minute). A technique to reduce the operating time would therefore even more strongly impact the total costs in hospitals such as those in the US. In contrast to endostaplers, polymeric clips can leave protuberant mucosa near and around the locking device, which could be a source of postoperative abscesses. However, the present study showed no trend toward more postoperative abscesses following appendectomy using polymeric clips.
Although the present study accurately reflects the daily practice of treating acute appendicitis in our clinic, the study design is a limitation; i.e., this was a single-center, retrospective review in which the surgeon decided on the technique of appendiceal stump closure. The patients in the staple group were older and had a higher preoperative C-reactive protein level. Furthermore, patients with stapled appendectomy more often had perforated appendicitis and more often received postoperative antibiotics. To reduce these confounding factors, the patients were divided into two subgroups: those with uncomplicated and complicated appendicitis. In patients with complicated appendicitis, perforations occurred more frequently in the Hem-o-lok group, while inflammation of the base was seen more often in the endostapler group. In patients with uncomplicated appendicitis, more patients aged ≥40 years were treated with endostaplers, and postoperative antibiotics were administered more often after stapled appendectomy; this might have biased the present results. Because of the low incidence of complications such as intra-abdominal abscesses and of reoperations and readmissions, the true difference would not have been detected with the sample size used in the present study. More highly powered studies and/or meta-analyses will need to be performed to finally answer this question. A further limitation of the present study is that the term “complicated appendicitis” is not used consistently in the literature, which might make comparisons with other studies difficult. We defined complicated appendicitis as either appendicitis with perforation and/or necrosis of the appendix or as inflammation of the appendix base.
In conclusion, the present study has shown that polymeric clips are not inferior to staplers for appendiceal stump closure and that polymeric clips may be safely used to treat perforated appendicitis.
Acknowledgments
We thank Paloma Wyss for the initial data acquisition and Angela Munson for language editing.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Giesen LJ, van den Boom AL, van Rossem CC, et al. Retrospective multicenter study on risk factors for surgical site infections after appendectomy for acute appendicitis. Dig Surg 2016; 34: 103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horvath P, Lange J, Bachmann R, et al. Comparison of clinical outcome of laparoscopic versus open appendectomy for complicated appendicitis. Surg Endosc 2017; 31: 199–205. [DOI] [PubMed] [Google Scholar]
- 3.Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 2010; (10): CD001546. [DOI] [PubMed] [Google Scholar]
- 4.van Rossem CC, van Geloven AA, Schreinemacher MH, et al. Endoloops or endostapler use in laparoscopic appendectomy for acute uncomplicated and complicated appendicitis: no difference in infectious complications. Surg Endosc 2017; 31: 178–184. [DOI] [PubMed] [Google Scholar]
- 5.Beldi G, Vorburger SA, Bruegger LE, et al. Analysis of stapling versus endoloops in appendiceal stump closure. Br J Surg 2006; 93: 1390–1393. [DOI] [PubMed] [Google Scholar]
- 6.Kazemier G, de Zeeuw GR, Lange JF, et al. Laparoscopic vs open appendectomy. A randomized clinical trial. Surg Endosc 1997; 11: 336–340. [DOI] [PubMed] [Google Scholar]
- 7.Kazemier G, in't Hof KH, Saad S, et al. Securing the appendiceal stump in laparoscopic appendectomy: evidence for routine stapling? Surg Endosc 2006; 20: 1473–1476. [DOI] [PubMed] [Google Scholar]
- 8.Sahm M, Kube R, Schmidt S, et al. Current analysis of endoloops in appendiceal stump closure. Surg Endosc 2011; 25: 124–129. [DOI] [PubMed] [Google Scholar]
- 9.Swank HA, van Rossem CC, van Geloven AA, et al. Endostapler or endoloops for securing the appendiceal stump in laparoscopic appendectomy: a retrospective cohort study. Surg Endosc 2014; 28: 576–583. [DOI] [PubMed] [Google Scholar]
- 10.Soll C, Wyss P, Gelpke H, et al. Appendiceal stump closure using polymeric clips reduces intra-abdominal abscesses. Langenbecks Arch Surg 2016; 401: 661–666. [DOI] [PubMed] [Google Scholar]
- 11.Akkoyun I, Akbiyik F. Closing the appendicular stump with a polymeric clip in laparoscopic appendectomy: analysis of 121 pediatric patients. Eur J Pediatr Surg 2012; 22: 133–135. [DOI] [PubMed] [Google Scholar]
- 12.Colak E, Kement M, Ozlem N, et al. A comparison of nonabsorbable polymeric clips and endoloop ligatures for the closure of the appendicular stump in laparoscopic appendectomy: a prospective, randomized study. Surg Laparosc Endosc Percutan Tech 2013; 23: 255–258. [DOI] [PubMed] [Google Scholar]
- 13.Delibegovic S. The use of a single Hem-o-lok clip in securing the base of the appendix during laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A 2012; 22: 85–87. [DOI] [PubMed] [Google Scholar]
- 14.Hanssen A, Plotnikov S, Dubois R. Laparoscopic appendectomy using a polymeric clip to close the appendicular stump. JSLS 2007; 11: 59–62. [PMC free article] [PubMed] [Google Scholar]
- 15.Hue CS, Kim JS, Kim KH, et al. The usefulness and safety of Hem-o-lok clips for the closure of appendicular stump during laparoscopic appendectomy. J Korean Surg Soc 2013; 84: 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jenwitheesuk K, Chotikawanich E, Saeseow OT, et al. Laparoscopic appendectomy: results of a new technique for stump management. J Med Assoc Thai. 2012; 95: S7–S10. [PubMed] [Google Scholar]
- 17.Langer M, Safavi A, Skarsgard ED. Management of the base of the appendix in pediatric laparoscopic appendectomy: clip, ligate, or staple? Surg Technol Int 2013; 23: 81–83. [PubMed] [Google Scholar]
- 18.Gorter RR, Heij HA, Eker HH, et al. Laparoscopic appendectomy: state of the art. Tailored approach to the application of laparoscopic appendectomy? Best Pract Res Clin Gastroenterol 2014; 28: 211–224. [DOI] [PubMed] [Google Scholar]
- 19.Knight SR, Ibrahim A, Makaram N, et al. The use of polymeric clips in securing the appendiceal stump during laparoscopic appendicectomy: a systematic review. Eur J Trauma Emerg Surg 2019. doi: 10.1007/s00068-019-01105-5. [DOI] [PubMed] [Google Scholar]
- 20.Wilson MSJ, Knight SR, Vaughan-Shaw P, et al. Securing the appendiceal stump during emergency appendicectomy: options and influencing factors in current UK surgical practice. Surg Laparosc Endosc Percutan Tech 2018; 28: 209–213. [DOI] [PubMed] [Google Scholar]
- 21.Parlakgumus A, Ezer A. Polymeric clips for stump closure in laparoscopic appendectomy. J Coll Physicians Surg Pak 2017; 27: 660–662. [PubMed] [Google Scholar]
- 22.Obrist NM, Tschuor C, Breitenstein S, et al. Appendectomy in Switzerland: how is it done? Updates Surg 2019. doi: 10.1007/s13304-019-00654-z. [DOI] [PubMed] [Google Scholar]
- 23.Lucchi A, Berti P, Grassia M, et al. Laparoscopic appendectomy: Hem-o-lok versus Endoloop in stump closure. Updates Surg 2017; 69: 61–65. [DOI] [PubMed] [Google Scholar]
- 24.Wilson M, Maniam P, Ibrahim A, et al. Polymeric clips are a quicker and cheaper alternative to endoscopic ligatures for securing the appendiceal stump during laparoscopic appendicectomy. Ann R Coll Surg Engl 2018; 100: 454–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pogorelic Z, Kostovski B, Jeroncic A, et al. A comparison of endoloop ligatures and nonabsorbable polymeric clips for the closure of the appendicular stump during laparoscopic appendectomy in children. J Laparoendosc Adv Surg Tech A 2017; 27: 645–650. [DOI] [PubMed] [Google Scholar]
- 26.Delibegovic S, Mehmedovic Z. The influence of the different forms of appendix base closure on patient outcome in laparoscopic appendectomy: a randomized trial. Surg Endosc 2018; 32: 2295–2299. [DOI] [PubMed] [Google Scholar]
- 27.Partecke LI, Kessler W, von Bernstorff W, et al. Laparoscopic appendectomy using a single polymeric clip to close the appendicular stump. Langenbecks Arch Surg 2010; 395: 1077–1082. [DOI] [PubMed] [Google Scholar]
- 28.Parikh PP, Tashiro J, Wagenaar AE, et al. Looped suture versus stapler device in pediatric laparoscopic appendectomy: a comparative outcomes and intraoperative cost analysis. J Pediatr Surg 2018; 53: 616–619. [DOI] [PubMed] [Google Scholar]
- 29.Rakic M, Jukic M, Pogorelic Z, et al. Analysis of endoloops and endostaples for closing the appendiceal stump during laparoscopic appendectomy. Surg Today 2014; 44: 1716–1722. [DOI] [PubMed] [Google Scholar]