Abstract
The intestinal microbiota is one of the most rapidly evolving areas in biology and medicine. Extensive research in the last decade has escalated our understanding of the role of the microbiota in the pathogenesis of several intestinal and extra-intestinal disorders. Marked by high prevalence, substantial morbidity, and enormous costs, irritable bowel syndrome (IBS) is an important chronic gastrointestinal disorder that is widely encountered by gastroenterologists. Despite advances in our understanding of its pathophysiology, curative interventions have yet to be discovered, and therapeutic approaches remain symptom-driven. Recently, accumulating evidence has enlightened the possible impact of an imbalanced gut microbiome in the pathogenesis of IBS. In fact, several studies have documented altered microbiota in patients, while others have shown that IBS severity was associated with a distinct microbiota signature. These findings may pave the way for the use of microbiota manipulation strategies as an attractive option for IBS management, and may have an essential role in efforts to reduce the societal and economic effects of this ever-growing disorder. In this review, we have outlined the results of the latest research on the association between microbiota and IBS and their implications for the clinical management of affected patients.
Keywords: gut, microbiome, IBS
1. Introduction
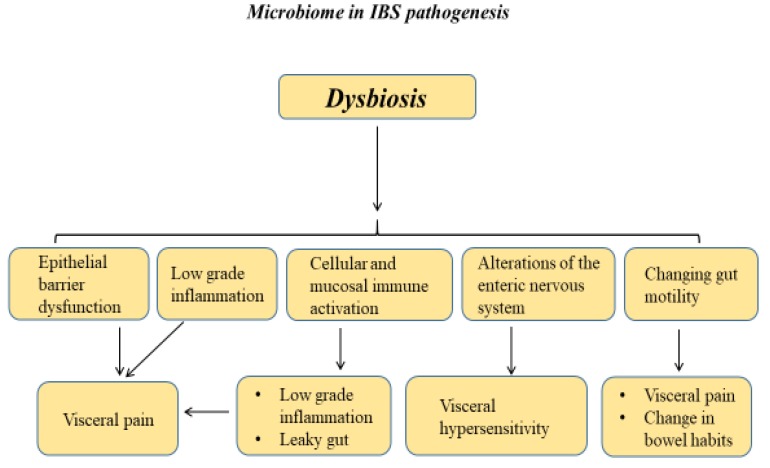
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder characterized by chronic recurrent abdominal pain, changes in bowel habits, and other symptoms such as bloating and flatulence. Based on the Rome IV criteria, four subtypes of IBS exist depending on the predominant stool pattern, including IBS with constipation (IBS-C), IBS with diarrhea (IBS-D), IBS with mixed bowel habits (IBS-M), and unclassified IBS [1,2]. IBS has a global prevalence of approximately 11% and is associated with several comorbidities, such as anxiety, depression, fibromyalgia, migraines, chronic pelvic pain, and others [3,4]. IBS is a major socioeconomic burden because affected patients utilize more healthcare resources with reduced work productivity when compared to the healthy population [5]. IBS is a complex heterogeneous condition with a multifactorial pathogenesis. Proposed mechanisms involved in the pathogenesis of IBS include visceral hypersensitivity, gut–brain axis alterations, disorders in the epithelial barrier integrity leading to abnormal mucosal intestinal permeability, changed intestinal motility, immune system activation, food intolerance, low-grade inflammation, altered enteroendocrine pathways signaling, genetic basis (e.g., mutation in the SC5NA gene encoding a sodium channel ion; a number of single-nucleotide polymorphism studies have also identified polymorphisms in genes associated with IBS pathogenesis including genes coding for serotonin signaling, immune regulation, and epithelial barrier function), and the evolving concept of dysbiosis in the gut microbiota (Figure 1) [6,7,8,9,10,11,12,13,14,15].
Figure 1.
Role of the microbiome in irritable bowel syndrome (IBS).
Gastrointestinal (GI) microbiota are the most relevant microbial community in the body and belong to the so-called microbiota which includes all microorganisms living in the human body. The intestinal microbiota includes bacteria, archaea, fungi, eukaryotes, and viruses. Most of the bacteria in the GI tract are represented in four main bacterial phyla: Firmicutes, Bacteroidetes, Proteobacteria, and Actinobacteria [16,17]. Trillions of microorganisms reside in the GI tract, with the highest density in the colon. However, most of them remain uncharacterized. Since this number is approximately equal to 10 times the total number of body cells, the interest in microbiota study for intestinal and extra-intestinal diseases is not surprising [18,19,20,21,22]. Advances in molecular biology techniques have significantly contributed to microbiome research. The most common technique to analyze the composition of the gut bacteria is marker gene sequencing, generally using the 16S rRNA gene [23,24,25]. Advantages of this method are related to its simplicity and low cost.
The aim of this review is to overview the most up-to-date literature about the evolving role of gut microbiome manipulation in IBS management, with a focus on probiotics, prebiotics, antibiotics, and fecal transplantation.
2. Methods
A search for studies published before January 2020 was performed in the PubMed and Embase databases. All authors participated in the search process. We looked for the terms “irritable bowel syndrome”, “microbiota”, “treatment”, “prebiotic”, “probiotic”, “synbiotic”, “FODMAP”, “meta-analysis”, “randomized”, “clinical”, “bifidobacteria”, “lactobacillus”, “firmicutes”, “bacteroidetes”, “methane”, “methanogen”, “diet”, “fecal transplantation”, “bacteriophage”, and “fungi”, mainly focusing on the literature that describes effects on microbiota, clinical studies, and therapeutic effects in IBS. The search was restricted to articles in the English language.
3. The Microbiome in IBS
A rash of research activity in this field from the last decade has led to the evidence that a disruption in the biodiversity, richness, and composition of the gut microbiota—a process named dysbiosis—plays a key function in the pathogenesis of IBS [26]. Dysbiosis can take place through several mechanisms: the overgrowth or vanishing of specific bacteria species, alterations in the relative richness of bacteria, and lastly, by mutation or gene transfer [27].
In IBS patients, GI dysbiosis has been associated with a visceral increased perception of pain and enhanced mucosal permeability that is provoked by the defective mucosal epithelial barrier, interfering with gut immune homeostasis and subsequently promoting gut inflammation and enhancing cellular and mucosal immune activation [28,29]. Moreover, it has also been associated with changing gut motility, low-grade chronic inflammation, alterations of the enteric nervous system, and vagal afferents neurons as well as brain functions [30,31,32]. In opposition, gut microbiota can be affected by the brain activity on intestinal motility, secretion, and immune function, generating the microbiota–gut–brain axis [12,33].
Microbiological and infectious bases of IBS pathogenesis have been previously established by several groups. Halvorson et al. reported a seven-fold increased risk of post-infectious IBS after acute infectious gastroenteritis [34]. Moreover, therapeutic interventions that manipulate the gut microbiota such as antibiotics, prebiotics, probiotics, and fecal microbial transplantation have been linked to improvements in IBS symptoms [35,36,37]. Several studies aiming to characterize and map the microbiome signature of IBS have shown divergent results. Nonetheless, data suggest that there is a relative richness of proinflammatory bacterial species containing Enterobacteriaceae, with a parallel decline in Lactobacillus and Bifidobacterium [38,39]. A decreased percentage of Lactobacillus and Bifidobacterium species has also been described in the IBS microbiota, leading to disturbances in short-chain fatty acid production and in immunologic and bactericidal activity, with a negative effect on microbiota function and stability [40,41,42,43,44,45,46]. Interestingly, the Firmicutes/Bacteroidetes ratio is a possible indicator of bacterial population shifts, and both high and low ratios of Firmicutes/Bacteroidetes have been reported in IBS patients [47,48,49,50]. These contrasts may be explained by differences in technical methods and subtypes of IBS, as well as the severity of IBS [38]. Several groups examined gut microbiota in different subtypes of IBS and compared the microbiota texture between different IBS subtypes as well as different IBS symptoms [48,51,52]. A study by Ringel-Kulka et al. using fecal samples from 60 patients with IBS and 20 healthy controls revealed major variances in the microbiota between the different subtypes of IBS based on clinical symptoms of abdominal bloating and bowel habits (IBS-D, IBS-C, or IBS-M type) [53]. A study examining both fecal and colonic mucosal microbiota in patients with chronic constipation found that their mucosal microbiota differed from those of the controls, with a higher abundance of Bacteroidetes species in the patients than in the controls. However, although the profile of the colonic mucosal microbiota discriminated between these two cohorts with a high level of accuracy, this finding was independent of colonic transit time. In contrast, the profile of the fecal microbiota was associated with colonic transit, but not with the clinical diagnosis of constipation [54]. Putting all of this together, numerous evidence is emerging regarding the link between microbiota and IBS pathogenesis, making microbiota manipulation strategies an attractive option for IBS management.
4. Therapeutic Interventions for Microbiome Manipulation in IBS
4.1. Probiotics
Historically, the theory of probiotics was described by Elie Metchnikoff in 1908, who observed that fermented foods—principally those fermented by lactic acid bacteria—had favorable effects on human wellbeing and longevity. According to the most updated definition based on the Food and Agriculture Organization as well as the World Health Organization, probiotics are defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host” [55]. Probiotics related to IBS pathogenesis are mainly those containing Lactobacillus and Bifidobacterium species [56]. Tentatively, probiotics may promote a favorable modulation of altered gut microbiota by several mechanisms: reducing the number of competing pathogens by both the production of antimicrobial substances and interfering in intestinal mucosal adhesion [57,58], modulating the metabolism of biliary salts [59], reducing low-grade inflammation [60], and regulating immune activation as well as gut motility [61]. Several meta-analyses of randomized controlled trials (RCTs) that assessed the effects of single probiotic strains, compared to a placebo in relieving IBS related symptoms [35,59,62], have concluded that probiotics are more efficient when compared to placebos in relieving global IBS symptoms including bloating abdominal pain. In safety terms, all studies have reported comparable rates of adverse events to the placebo arms. In an Iranian IBS cohort, Jafari and colleagues observed the effects of combinations of strains of Bifidobacterium, Lactobacillus, and Streptococcus genera [63]. The main finding was that 85% of patients in the probiotic group reported satisfactory relief of general symptoms compared with 47% in the control group (p < 0.01). In general terms, probiotics seem to have favorable effects on improving IBS symptoms, with an excellent safety profile. Nonetheless, more randomized controlled trials are warranted to better define some concerns such as treatment duration and optimal strain, and to better study personalized treatment.
4.2. Prebiotics
Since 2007, prebiotics have been defined as a “nonviable food component that confers a health benefit on the host associated with modulation of the microbiota” [64]. Prebiotics are basically classified as disaccharides or oligosaccharides and are resistant to enzymatic and chemical breakdown until they reach the colon, where they are fermented by colonic bacteria, stimulating the generation of microbial metabolic products such as short-chain fatty acids (acetate, butyrate, and propionate) [65]. Short-chain fatty acids give several benefits to the colonocytes, such as an energy source, regulation of electrolytes and water absorption, enhanced blood flow, and oxygenation [66]. Moreover, probiotics may promote host health and modulation of GI motility, reduction in visceral hypersensitivity, downregulation of low-grade mucosal immune activation, improvement of epithelial permeability, enhancement of gut–brain communication, and restoration of intestinal dysbiosis. Thus, these data provide a mechanistic rationale for a role of prebiotics in managing IBS symptoms. Indeed, several clinical studies have examined prebiotics’ performance in ameliorating symptoms of functional bowel disorders. A handful of RCTs evaluating the efficacy and safety of prebiotics in IBS [67,68] have been performed. In 1999, a small, double-blind crossover trial of oligofructose published by Hunter and colleagues [69] showed no therapeutic value in IBS patients. One year later, a randomized double-blind trial on almost 100 patients with IBS receiving either fructo-oligosaccharide or placebo for 12 weeks reported no statistically significant improvement in symptoms [70]. The first study to report a beneficial effect was a cross-over, single-blinded trial including 60 Rome II-defined IBS patients. Patients were randomized for four weeks to receive a low or high dose of trans-galacto-oligosaccharide or placebo. Both the low and high-dose arms experienced a significant improvement in stool consistency (p < 0.05), flatulence (p < 0.05), and bloating (p < 0.05) as well as a reduction in mean subjective global assessment (The subjective global assessment of relief was recorded at weekly intervals during the course of the study scored from 1–5. 1 = completely relieved, 2 = considerably relieved, 3 = somewhat relieved, 4 = unchanged, and 5 = worse) [71].
Interestingly, the prebiotic but not the placebo significantly enhanced fecal bifidobacteria [71]. A 12-week administration of partially hydrolyzed guar gum in a randomized, double-blind, placebo-controlled study led to a significant improvement in bloating and gasses scores with no effect on other reported IBS symptoms or quality of life scores, leading the authors to support its administration for IBS patients with an expected clinical effect on bloating and gasses [72]. In safety terms, all studies reported comparable rates of adverse events to the placebo arms. In conclusion, prebiotic use in IBS patients have yielded mixed to positive results, but further studies to address the combination, duration, and different aspects of effects on IBS are still warranted.
4.3. Non-Absorbable Antibiotics
Non-absorbable antibiotics, mainly rifaximin, have been shown to be safe and effective for the treatment of IBS with the diarrhea predominant type. Rifaximin, a rifamycin derivative, is a broad-spectrum, non-absorbable antibiotic which targets aerobic and anaerobic bacteria residing in the GI tract. Less than 1% of rifaximin is absorbed in the systemic circulation, making it very safe with extremely low toxicity and adverse events rates [73]. The proposed mechanisms of action of the non-absorbable antibiotics are the reduction of the amount of inhabitant GI bacteria, changes in bacterial structure, reduction of low-grade inflammation, and amelioration in gut permeability [74]. Rifaximin is the best-studied non-absorbable antibiotic for symptoms relief in IBS. The TARGET 1 and TARGET 2 trials, both designed as double-blinded, placebo-controlled, multi-center studies, have shown good efficacy of rifaximin for IBS symptoms relief [75]. In TARGET 1 and TARGET 2, a total number of 1258 patients with mild to moderate symptoms of IBS were randomized either to receive rifaximin 550 mg three times a day for 14 days or a placebo. Relief of IBS symptoms, after one month from the end of treatment, was reported more significantly among patients in the rifaximin group compared with those in the placebo group (40.7% vs. 31.7%, p < 0.001), with a comparable adverse events occurrence in both groups [75]. TARGET 3, a randomized, placebo-controlled study including 2579 patients with IBS, revealed that the durability of symptoms relief among patients with IBS-D responding to a 14-day course of rifaximin was reduced by 50% after 70 days from the end of treatment [76]. With a second treatment course, the most significant benefit was the relief of stool urgency and abdominal bloating [76].
4.4. Fecal Microbiota Transplantation
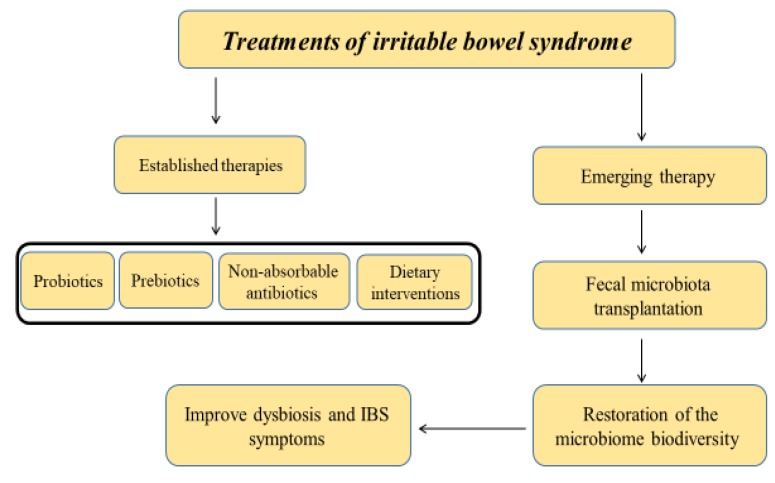
Fecal microbiota transplant (FMT), also known as a stool transplant, is the process of transplantation of fecal bacteria from a healthy individual into a recipient. FMT involves the restoration of the colonic microflora by introducing healthy bacterial flora through the infusion of stool (e.g., via colonoscopy, enema, rogastric tubeor by mouth in the form of a capsule containing freeze-dried material) obtained from a healthy donor. To date, FMT has been approved for the treatment of resistant Clostridium difficile infections [77,78], and in this context, it has been shown to be an effective therapy [79]. However, its therapeutic effect among IBS patients is still emerging. As reported above, in the last few years, several studies have underlined the role of dysbiosis among patients with IBS, with lower Lactobacillus spp. in IBS-D and increased loads of Veillonella spp., and genera Coprococcus, Collinsella, and Coprobacillus [42,80]. Other data revealed a decrease in the biodiversity of microbiota in the fecal composition of IBS-D patients [51]. Therefore, targeting the gut microbiota composition might be a promising therapy in IBS. However, among IBS patients, FMT has shown conflicting results. A previous randomized controlled study showed beneficial effects of FMT on IBS symptoms. In this study, 55 patients with IBS-D or IBS-M received 50–80 g of feces mixed with 200 mL of isotonic saline and 50 mL of 85% glycerol, administered to the cecum by colonoscopy, and were compared to 28 patients who received a placebo. Patients treated with FMT showed a significant clinical response at three months compared to those in the placebo group (65% vs. 43%, p = 0.049) [39]. These findings were further confirmed by other recent studies showing a positive effect on IBS symptoms after transplant, as 70–85% and 45–60% of patients reported symptomatic relief in the first three months and six months after FMT, respectively [81,82]. On the contrary, a recent study including 52 IBS adult patients who were randomized to either active FMT or placebo capsules administered for 12 months did not show beneficial effects favoring FMT at three months. In fact, a significant improvement in IBS symptom scores was observed at three months favoring the placebo (p = 0.012), and after three months, the results obtained by an IBS quality of life questionnaire were in favor of the placebo (p = 0.003) [83]. Moreover, a recent meta-analysis including eight single-arm trials (SATs) and 5 RCTs did not report beneficial effects of FMT among patients with IBS (relative risk = 0.93, 95%, confidence interval (CI (confidence interval) 0.50–1.75, p = 0.83 for RCT), while in the SAT 59.5% of patients (95% CI 49.1–69.3) showed a significant improvement [84]. Given the controversies regarding the published data, FMT-based treatments for IBS are still not widely accepted among gastroenterologists, as they are concerned about effectiveness and safety profile [85]. Therefore, the role of FMT must be further addressed by randomized, double-blind, placebo-controlled studies. Recent international consensus of stool banking for FMT have involved experts from Europe, North America, and Australia who proposed consensus guideline statements regarding several issues in stool banking, including the selection of donors and screening objectives, collection and processing of stool samples, monitoring of outcomes, ethical issues, and the evolving role of FMT in Clostridioides difficile infection and other diseases encountered in daily clinical practice [86]. Figure 2 demonstrates the established and evolving therapeutic options for IBS.
Figure 2.
Treatments of irritable bowel syndrome (IBS) by targeting the gut microbiome.
4.5. Dietary Intervention
Dietary modifications constitute one of the first choices of treatment for IBS patients [87]. Indeed, a careful history may reveal patterns of symptoms linked to specific food consumption. Although debatable, a high-fiber diet has traditionally been encouraged particularly in IBS-C patients, given the absence of serious side effects and its potential benefit [88,89]. In recent years, there has been a growing clinical and scientific interest in the use of a diet low in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) in IBS patients. Since its introduction, reports in the literature including several RCTs have reported the efficacy of a low-FODMAP diet in improving global IBS symptoms, visceral pain, bloating, and quality of life [90,91,92,93,94,95,96]. However, large and long-term RCTs are still lacking, and various concerns have been raised including diet complexity and cost, risk of nutritional deficiencies, and importantly, an unclear impact on gut microbiome [97,98,99].
A focus on the role of a gluten-free diet (GFD) in IBS has grown recently, with studies demonstrating the induction of symptoms following gluten consumption in IBS patients [100]. However, evidence to support gluten avoidance in IBS has been conflicting. Moreover, a recent report has suggested that fructans rather than gluten protein are responsible for the symptomatic improvement reported in a gluten-free diet [101]. Further studies are required to evaluate the effect of a GFD on nutritional status, gut microbiota, and long-term outcomes.
5. Conclusions
In conclusion, in the current review we have provided a focused summary of the latest literature on the potential role of gut dysbiosis in the pathogenesis of IBS and discussed the translation of microbiota-modifying strategies as a novel therapeutic option for this disorder (Figure 1). There is strong growing evidence supporting microbiome-based therapeutic approaches with dietary intervention, probiotics, prebiotics, non-absorbable antibiotics, and FMTs for the treatment of IBS (Table 1). Nonetheless, more knowledge is needed to better address the role of microbiome-based therapeutic interventions in the clinical management of IBS. Several future microbiome-based therapeutic options are being explored and investigated, including genetic engineering of bacteria, personalized microbiota manipulation, postbiotics, and bacteriophage therapy.
Table 1.
Summary of the meta-analysis studies reporting efficacy of therapeutic interventions in irritable bowel syndrome (IBS) based on overall global IBS symptoms.
| Meta-Analysis of RCT Studies of Probiotics vs. Placebo | |||||
| Reference | Number | Primary Endpoint as Dichotomous Variable (RR ± 95% CI) | p-Value | ||
| Studies | Patients | Clinical Improvement | Symptoms Persistence | ||
| Didari T., 2015 [59] | 15 | 1793 | 2.43 ± 1.13–5.21 | - | 0.02 |
| Zhang Y., 2016 [35] | 21 | 1639 | 1.82 ± 1.27–2.6 | - | <0.001 |
| Liang D., 2019 [102] | 14 | 1695 | 1.27 ± 1.13–1.44 | - | <0.001 |
| McFarland L.V., 2008 [103] | 23 | 1404 | 0.77 pooled ± 0.62–0.94 | - | <0.001 |
| Connell M., 2018 [104] | 5 | 243 | 1.39 ± 0.99–1.98 | - | 0.06 |
| Ford A.C., 2014 [63] | 23 | 2575 | - | 0.79 ± 0.7–0.89 | <0.0001 |
| Tiequn B., 2015 [105] | 6 | 273 167 |
17.62 pooled ± 5.12–60.65 for adults 3.71 pooled ± 1.05–13.11 for children |
- - |
<0.00001 0.04 |
| Ritchie M.L., 2012 [106] | 16 | - | 0.77 ± 0.65–0.92 | - | - |
| Horvath A., 2011 [107] | 3 | 167 | 1.7 ± 1.27–2.27 | - | 0.0004 |
| Hoveyda N., 2009 [108] | 7 | 425 | 1.6 ± 1.2–2.2 | - | 0.0007 |
| Moayyedi P., 2010 [109] | 10 | 918 | - | 0.71 ± 0.57–0.88 | 0.002 |
| Nikfar S., 2008 [110] | 8 | 1011 | 1.22 ± 1.07–1.4 | - | 0.004 |
| McFarland L.V., 2008 [103] | 20 | 1404 | 0.77 pooled ± 0.62–0.94 | - | <0.001 |
| Meta-Analysis of RCT Studies of Prebiotics vs. Placebo | |||||
| Wilson B., 2019 [67] | 11 | 729 | OR 0.62 ± 0.07–5.69 | - | 0.67 |
| Ford A.C., 2018 [68] | Trials for prebiotics were sparse and no definite conclusions could be drawn | ||||
| Ford A.C., 2014 [63] | |||||
| Meta-Analysis of RCT Studies of Fecal Microbiota Transplantation vs. Placebo | |||||
| Myneedu K., 2019 [84] | 5 | 262 | 0.93 ± 0.5–1.75 | - | 0.83 |
| Xu D., 2019 [111] | 4 | 254 | 0.93 ± 0.48–1.79 | - | 0.83 |
| Laniro G., 2019 [112] | 5 | 267 | - | 0.98 ± 0.58–1.66 | 0.94 |
| Meta-Analysis of RCT Studies of Non-Absorbable Antibiotics Rifaximin vs. Placebo | |||||
| Ford A.C., 2018 [68] | 5 | 3610 | - | 0.84 ± 0.79–0.9 | 0.0002 |
| Li J., 2016 [113] | 4 | 1803 | 1.19 ± 1.08–1.32 | - | 0.0008 |
| Menees S.B., 2012 [75] | 5 | 1803 | 1.57 ± 1.22–2.01 | - | <0.001 |
RCT: Randomized Controlled Trials; CI: Confidence Interval; pooled: Pooled RR.
Author Contributions
Conceptualization, A.M. and T.K.; methodology, A.M., F.A.B., M.M., W.S., T.K.; software, A.M., T.K.; validation, A.M., T.K. and M.M.; formal analysis, T.K., F.A.B.; investigation, A.M., T.K.; resources, A.M.; project administration, A.M. All authors have read and agreed to the published version of the manuscript.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare no conflicts of interest regarding this manuscript.
References
- 1.Mearin F., Lacy B.E., Chang L., Chey W.D., Lembo A.J., Simren M., Spiller R. Bowel Disorders. Gastroenterology. 2016 doi: 10.1053/j.gastro.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 2.Simren M., Palsson O.S., Whitehead W.E. Update on Rome IV Criteria for Colorectal Disorders: Implications for Clinical Practice. Curr. Gastroenterol. Rep. 2017;19:15. doi: 10.1007/s11894-017-0554-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canavan C., West J., Card T. The epidemiology of irritable bowel syndrome. Clin. Epidemiol. 2014;6:71–80. doi: 10.2147/CLEP.S40245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adriani A., Ribaldone D.G., Astegiano M., Durazzo M., Saracco G.M., Pellicano R. Irritable bowel syndrome: The clinical approach. Panminerva. Med. 2018;60:213–222. doi: 10.23736/S0031-0808.18.03541-3. [DOI] [PubMed] [Google Scholar]
- 5.Buono J.L., Mathur K., Averitt A.J., Andrae D.A. Economic Burden of Irritable Bowel Syndrome with Diarrhea: Retrospective Analysis of a U.S. Commercially Insured Population. J. Manag. Care Spec. Pharm. 2017;23:453–460. doi: 10.18553/jmcp.2016.16138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makker J., Chilimuri S., Bella J.N. Genetic epidemiology of irritable bowel syndrome. World J. Gastroenterol. 2015;21:11353–11361. doi: 10.3748/wjg.v21.i40.11353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Powell N., Walker M.M., Talley N.J. The mucosal immune system: Master regulator of bidirectional gut-brain communications. Nat. Rev. Gastroenterol. Hepatol. 2017;14:143–159. doi: 10.1038/nrgastro.2016.191. [DOI] [PubMed] [Google Scholar]
- 8.Pellissier S., Bonaz B. The Place of Stress and Emotions in the Irritable Bowel Syndrome. Vitam. Horm. 2017;103:327–354. doi: 10.1016/bs.vh.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Deiteren A., de Wit A., van der Linden L., De Man J.G., Pelckmans P.A., De Winter B.Y. Irritable bowel syndrome and visceral hypersensitivity: Risk factors and pathophysiological mechanisms. Acta Gastroenterol. Belg. 2016;79:29–38. [PubMed] [Google Scholar]
- 10.Mullin G.E., Shepherd S.J., Chander Roland B., Ireton-Jones C., Matarese L.E. Irritable bowel syndrome: Contemporary nutrition management strategies. JPEN J. Parenter. Enteral. Nutr. 2014;38:781–799. doi: 10.1177/0148607114545329. [DOI] [PubMed] [Google Scholar]
- 11.Sundin J., Ohman L., Simren M. Understanding the Gut Microbiota in Inflammatory and Functional Gastrointestinal Diseases. Psychosom. Med. 2017;79:857–867. doi: 10.1097/PSY.0000000000000470. [DOI] [PubMed] [Google Scholar]
- 12.Moloney R.D., Johnson A.C., O’Mahony S.M., Dinan T.G., Greenwood-Van Meerveld B., Cryan J.F. Stress and the Microbiota-Gut-Brain Axis in Visceral Pain: Relevance to Irritable Bowel Syndrome. CNS Neurosci. Ther. 2016;22:102–117. doi: 10.1111/cns.12490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quigley E.M.M. The Gut-Brain Axis and the Microbiome: Clues to Pathophysiology and Opportunities for Novel Management Strategies in Irritable Bowel Syndrome (IBS) J. Clin. Med. 2018;7:6. doi: 10.3390/jcm7010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fagoonee S., Pellicano R. Does the Microbiota Play a Pivotal Role in the Pathogenesis of Irritable Bowel Syndrome? J. Clin. Med. 2019;8:1808. doi: 10.3390/jcm8111808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gazouli M., Wouters M.M., Kapur-Pojskic L., Bengtson M.B., Friedman E., Nikcevic G., Demetriou C.A., Mulak A., Santos J., Niesler B. Lessons learned--resolving the enigma of genetic factors in IBS. Nat. Rev. Gastroenterol. Hepatol. 2016;13:77–87. doi: 10.1038/nrgastro.2015.206. [DOI] [PubMed] [Google Scholar]
- 16.Gill S.R., Pop M., Deboy R.T., Eckburg P.B., Turnbaugh P.J., Samuel B.S., Gordon J.I., Relman D.A., Fraser-Liggett C.M., Nelson K.E. Metagenomic analysis of the human distal gut microbiome. Science. 2006;312:1355–1359. doi: 10.1126/science.1124234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Backhed F., Fraser C.M., Ringel Y., Sanders M.E., Sartor R.B., Sherman P.M., Versalovic J., Young V., Finlay B.B. Defining a healthy human gut microbiome: Current concepts, future directions, and clinical applications. Cell Host. Microbe. 2012;12:611–622. doi: 10.1016/j.chom.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 18.Ribaldone D.G., Caviglia G.P., Abdulle A., Pellicano R., Ditto M.C., Morino M., Fusaro E., Saracco G.M., Bugianesi E., Astegiano M. Adalimumab Therapy Improves Intestinal Dysbiosis in Crohn’s Disease. J. Clin. Med. 2019;8:1646. doi: 10.3390/jcm8101646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masoodi I., Alshanqeeti A.S., Ahmad S., Alyamani E.J., Al-Lehibi A.A., Qutub A.N., Alsayari K.N., Alomair A.O. Microbial dysbiosis in inflammatory bowel diseases: Results of a metagenomic study in Saudi Arabia. Minerva. Gastroenterol. Dietol. 2019;65:177–186. doi: 10.23736/S1121-421X.19.02576-5. [DOI] [PubMed] [Google Scholar]
- 20.Bellocchi C., Fernandez-Ochoa A., Montanelli G., Vigone B., Santaniello A., Quirantes-Pine R., Borras-Linares I., Gerosa M., Artusi C., Gualtierotti R., et al. Identification of a Shared Microbiomic and Metabolomic Profile in Systemic Autoimmune Diseases. J. Clin. Med. 2019;8:1291. doi: 10.3390/jcm8091291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Korotkyi O.H., Vovk A.A., Dranitsina A.S., Falalyeyeva T.M., Dvorshchenko K.O., Fagoonee S., Ostapchenko L.I. The influence of probiotic diet and chondroitin sulfate administration on Ptgs2, Tgfb1 and Col2a1 expression in rat knee cartilage during monoiodoacetate-induced osteoarthritis. Minerva. Med. 2019;110:419–424. doi: 10.23736/S0026-4806.19.06063-4. [DOI] [PubMed] [Google Scholar]
- 22.Durazzo M., Ferro A., Gruden G. Gastrointestinal Microbiota and Type 1 Diabetes Mellitus: The State of Art. J. Clin. Med. 2019;8:1843. doi: 10.3390/jcm8111843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lloyd-Price J., Abu-Ali G., Huttenhower C. The healthy human microbiome. Genome Med. 2016;8:51. doi: 10.1186/s13073-016-0307-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim Y., Koh I., Rho M. Deciphering the human microbiome using next-generation sequencing data and bioinformatics approaches. Methods. 2015;79–80:52–59. doi: 10.1016/j.ymeth.2014.10.022. [DOI] [PubMed] [Google Scholar]
- 25.Kuczynski J., Lauber C.L., Walters W.A., Parfrey L.W., Clemente J.C., Gevers D., Knight R. Experimental and analytical tools for studying the human microbiome. Nat. Rev. Genet. 2011;13:47–58. doi: 10.1038/nrg3129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menees S., Chey W. The gut microbiome and irritable bowel syndrome. F1000Research. 2018;7 doi: 10.12688/f1000research.14592.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barbara G., Cremon C., Azpiroz F. Probiotics in irritable bowel syndrome: Where are we? Neurogastroenterol. Motil. 2018;30:e13513. doi: 10.1111/nmo.13513. [DOI] [PubMed] [Google Scholar]
- 28.Rea K., O’Mahony S.M., Dinan T.G., Cryan J.F. The Role of the Gastrointestinal Microbiota in Visceral Pain. Handb. Exp. Pharmacol. 2017;239:269–287. doi: 10.1007/164_2016_115. [DOI] [PubMed] [Google Scholar]
- 29.Fukui H. Increased Intestinal Permeability and Decreased Barrier Function: Does It Really Influence the Risk of Inflammation? Inflamm. Intest. Dis. 2016;1:135–145. doi: 10.1159/000447252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ohman L., Simren M. Pathogenesis of IBS: Role of inflammation, immunity and neuroimmune interactions. Nat. Rev. Gastroenterol. Hepatol. 2010;7:163–173. doi: 10.1038/nrgastro.2010.4. [DOI] [PubMed] [Google Scholar]
- 31.Shi N., Li N., Duan X., Niu H. Interaction between the gut microbiome and mucosal immune system. Mil. Med. Res. 2017;4:14. doi: 10.1186/s40779-017-0122-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Donnachie E., Schneider A., Mehring M., Enck P. Incidence of irritable bowel syndrome and chronic fatigue following GI infection: A population-level study using routinely collected claims data. Gut. 2018;67:1078–1086. doi: 10.1136/gutjnl-2017-313713. [DOI] [PubMed] [Google Scholar]
- 33.Kelly J.R., Kennedy P.J., Cryan J.F., Dinan T.G., Clarke G., Hyland N.P. Breaking down the barriers: The gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front. Cell. Neurosci. 2015;9:392. doi: 10.3389/fncel.2015.00392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Halvorson H.A., Schlett C.D., Riddle M.S. Postinfectious irritable bowel syndrome—A meta-analysis. Am. J. Gastroenterol. 2006;101:1894–1899. doi: 10.1111/j.1572-0241.2006.00654.x. [DOI] [PubMed] [Google Scholar]
- 35.Zhang Y., Li L., Guo C., Mu D., Feng B., Zuo X., Li Y. Effects of probiotic type, dose and treatment duration on irritable bowel syndrome diagnosed by Rome III criteria: A meta-analysis. BMC Gastroenterol. 2016;16:62. doi: 10.1186/s12876-016-0470-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valentin N., Camilleri M., Carlson P., Harrington S.C., Eckert D., O’Neill J., Burton D., Chen J., Shaw A.L., Acosta A. Potential mechanisms of effects of serum-derived bovine immunoglobulin/protein isolate therapy in patients with diarrhea-predominant irritable bowel syndrome. Physiol. Rep. 2017;5 doi: 10.14814/phy2.13170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.El-Salhy M., Mazzawi T. Fecal microbiota transplantation for managing irritable bowel syndrome. Expert. Rev. Gastroenterol. Hepatol. 2018;12:439–445. doi: 10.1080/17474124.2018.1447380. [DOI] [PubMed] [Google Scholar]
- 38.Rodino-Janeiro B.K., Vicario M., Alonso-Cotoner C., Pascua-Garcia R., Santos J. A Review of Microbiota and Irritable Bowel Syndrome: Future in Therapies. Adv. Ther. 2018;35:289–310. doi: 10.1007/s12325-018-0673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johnsen P.H., Hilpusch F., Cavanagh J.P., Leikanger I.S., Kolstad C., Valle P.C., Goll R. Faecal microbiota transplantation versus placebo for moderate-to-severe irritable bowel syndrome: A double-blind, randomised, placebo-controlled, parallel-group, single-centre trial. Lancet Gastroenterol. Hepatol. 2018;3:17–24. doi: 10.1016/S2468-1253(17)30338-2. [DOI] [PubMed] [Google Scholar]
- 40.Zhuang X., Xiong L., Li L., Li M., Chen M. Alterations of gut microbiota in patients with irritable bowel syndrome: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2017;32:28–38. doi: 10.1111/jgh.13471. [DOI] [PubMed] [Google Scholar]
- 41.Balsari A., Ceccarelli A., Dubini F., Fesce E., Poli G. The fecal microbial population in the irritable bowel syndrome. Microbiologica. 1982;5:185–194. [PubMed] [Google Scholar]
- 42.Malinen E., Rinttila T., Kajander K., Matto J., Kassinen A., Krogius L., Saarela M., Korpela R., Palva A. Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR. Am. J. Gastroenterol. 2005;100:373–382. doi: 10.1111/j.1572-0241.2005.40312.x. [DOI] [PubMed] [Google Scholar]
- 43.Carroll I.M., Chang Y.H., Park J., Sartor R.B., Ringel Y. Luminal and mucosal-associated intestinal microbiota in patients with diarrhea-predominant irritable bowel syndrome. Gut Pathog. 2010;2:19. doi: 10.1186/1757-4749-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kerckhoffs A.P., Samsom M., van der Rest M.E., de Vogel J., Knol J., Ben-Amor K., Akkermans L.M. Lower Bifidobacteria counts in both duodenal mucosa-associated and fecal microbiota in irritable bowel syndrome patients. World J. Gastroenterol. 2009;15:2887–2892. doi: 10.3748/wjg.15.2887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rajilic-Stojanovic M., Biagi E., Heilig H.G., Kajander K., Kekkonen R.A., Tims S., de Vos W.M. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology. 2011;141:1792–1801. doi: 10.1053/j.gastro.2011.07.043. [DOI] [PubMed] [Google Scholar]
- 46.Duboc H., Rainteau D., Rajca S., Humbert L., Farabos D., Maubert M., Grondin V., Jouet P., Bouhassira D., Seksik P., et al. Increase in fecal primary bile acids and dysbiosis in patients with diarrhea-predominant irritable bowel syndrome. Neurogastroenterol. Motil. 2012;24 doi: 10.1111/j.1365-2982.2012.01893.x. [DOI] [PubMed] [Google Scholar]
- 47.Tap J., Derrien M., Tornblom H., Brazeilles R., Cools-Portier S., Dore J., Storsrud S., Le Neve B., Ohman L., Simren M. Identification of an Intestinal Microbiota Signature Associated With Severity of Irritable Bowel Syndrome. Gastroenterology. 2017;152:111–123. doi: 10.1053/j.gastro.2016.09.049. [DOI] [PubMed] [Google Scholar]
- 48.Jeffery I.B., O’Toole P.W., Ohman L., Claesson M.J., Deane J., Quigley E.M., Simren M. An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota. Gut. 2012;61:997–1006. doi: 10.1136/gutjnl-2011-301501. [DOI] [PubMed] [Google Scholar]
- 49.Jalanka-Tuovinen J., Salojarvi J., Salonen A., Immonen O., Garsed K., Kelly F.M., Zaitoun A., Palva A., Spiller R.C., de Vos W.M. Faecal microbiota composition and host-microbe cross-talk following gastroenteritis and in postinfectious irritable bowel syndrome. Gut. 2014;63:1737–1745. doi: 10.1136/gutjnl-2013-305994. [DOI] [PubMed] [Google Scholar]
- 50.Lozupone C.A., Stombaugh J., Gonzalez A., Ackermann G., Wendel D., Vazquez-Baeza Y., Jansson J.K., Gordon J.I., Knight R. Meta-analyses of studies of the human microbiota. Genome Res. 2013;23:1704–1714. doi: 10.1101/gr.151803.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carroll I.M., Ringel-Kulka T., Keku T.O., Chang Y.H., Packey C.D., Sartor R.B., Ringel Y. Molecular analysis of the luminal- and mucosal-associated intestinal microbiota in diarrhea-predominant irritable bowel syndrome. Am. J. Physiol. Gastrointest. Liver Physiol. 2011;301:G799–G807. doi: 10.1152/ajpgi.00154.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carroll I.M., Ringel-Kulka T., Siddle J.P., Ringel Y. Alterations in composition and diversity of the intestinal microbiota in patients with diarrhea-predominant irritable bowel syndrome. Neurogastroenterol. Motil. 2012;24:521–530. doi: 10.1111/j.1365-2982.2012.01891.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ringel-Kulka T., Benson A.K., Carroll I.M., Kim J., Legge R.M., Ringel Y. Molecular characterization of the intestinal microbiota in patients with and without abdominal bloating. Am. J. Physiol. Gastrointest. Liver Physiol. 2016;310:G417–G426. doi: 10.1152/ajpgi.00044.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Parthasarathy G., Chen J., Chen X., Chia N., O’Connor H.M., Wolf P.G., Gaskins H.R., Bharucha A.E. Relationship Between Microbiota of the Colonic Mucosa vs. Feces and Symptoms, Colonic Transit, and Methane Production in Female Patients With Chronic Constipation. Gastroenterology. 2016;150:367–379. doi: 10.1053/j.gastro.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hill C., Guarner F., Reid G., Gibson G.R., Merenstein D.J., Pot B., Morelli L., Canani R.B., Flint H.J., Salminen S., et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014;11:506–514. doi: 10.1038/nrgastro.2014.66. [DOI] [PubMed] [Google Scholar]
- 56.Wrighton K.H. Mucosal immunology: Probiotic induction of tolerogenic T cells in the gut. Nat. Rev. Immunol. 2017;17:592. doi: 10.1038/nri.2017.110. [DOI] [PubMed] [Google Scholar]
- 57.Simren M., Barbara G., Flint H.J., Spiegel B.M., Spiller R.C., Vanner S., Verdu E.F., Whorwell P.J., Zoetendal E.G., Rome Foundation C. Intestinal microbiota in functional bowel disorders: A Rome foundation report. Gut. 2013;62:159–176. doi: 10.1136/gutjnl-2012-302167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mayer E.A., Savidge T., Shulman R.J. Brain-gut microbiome interactions and functional bowel disorders. Gastroenterology. 2014;146:1500–1512. doi: 10.1053/j.gastro.2014.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Didari T., Mozaffari S., Nikfar S., Abdollahi M. Effectiveness of probiotics in irritable bowel syndrome: Updated systematic review with meta-analysis. World J. Gastroenterol. 2015;21:3072–3084. doi: 10.3748/wjg.v21.i10.3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Joyce S.A., MacSharry J., Casey P.G., Kinsella M., Murphy E.F., Shanahan F., Hill C., Gahan C.G. Regulation of host weight gain and lipid metabolism by bacterial bile acid modification in the gut. Proc. Natl. Acad. Sci. USA. 2014;111:7421–7426. doi: 10.1073/pnas.1323599111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bermudez-Brito M., Plaza-Diaz J., Munoz-Quezada S., Gomez-Llorente C., Gil A. Probiotic mechanisms of action. Ann. Nutr. Metab. 2012;61:160–174. doi: 10.1159/000342079. [DOI] [PubMed] [Google Scholar]
- 62.Jafari E., Vahedi H., Merat S., Momtahen S., Riahi A. Therapeutic effects, tolerability and safety of a multi-strain probiotic in Iranian adults with irritable bowel syndrome and bloating. Arch. Iran. Med. 2014;17:466–470. [PubMed] [Google Scholar]
- 63.Ford A.C., Quigley E.M., Lacy B.E., Lembo A.J., Saito Y.A., Schiller L.R., Soffer E.E., Spiegel B.M., Moayyedi P. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: Systematic review and meta-analysis. Am. J. Gastroenterol. 2014;109:1547–1561. doi: 10.1038/ajg.2014.202. quiz 1546, 1562. [DOI] [PubMed] [Google Scholar]
- 64.Pineiro M., Asp N.G., Reid G., Macfarlane S., Morelli L., Brunser O., Tuohy K. FAO Technical meeting on prebiotics. J. Clin. Gastroenterol. 2008;42:S156–S159. doi: 10.1097/MCG.0b013e31817f184e. [DOI] [PubMed] [Google Scholar]
- 65.Alvarez-Curto E., Milligan G. Metabolism meets immunity: The role of free fatty acid receptors in the immune system. Biochem. Pharmacol. 2016;114:3–13. doi: 10.1016/j.bcp.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 66.Roberfroid M., Gibson G.R., Hoyles L., McCartney A.L., Rastall R., Rowland I., Wolvers D., Watzl B., Szajewska H., Stahl B., et al. Prebiotic effects: Metabolic and health benefits. Br. J. Nutr. 2010;104:S1–S63. doi: 10.1017/S0007114510003363. [DOI] [PubMed] [Google Scholar]
- 67.Wilson B., Rossi M., Dimidi E., Whelan K. Prebiotics in irritable bowel syndrome and other functional bowel disorders in adults: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2019;109:1098–1111. doi: 10.1093/ajcn/nqy376. [DOI] [PubMed] [Google Scholar]
- 68.Ford A.C., Harris L.A., Lacy B.E., Quigley E.M.M., Moayyedi P. Systematic review with meta-analysis: The efficacy of prebiotics, probiotics, synbiotics and antibiotics in irritable bowel syndrome. Aliment. Pharmacol. Ther. 2018;48:1044–1060. doi: 10.1111/apt.15001. [DOI] [PubMed] [Google Scholar]
- 69.Hunter J.O., Tuffnell Q., Lee A.J. Controlled trial of oligofructose in the management of irritable bowel syndrome. J. Nutr. 1999;129:1451S–1453S. doi: 10.1093/jn/129.7.1451S. [DOI] [PubMed] [Google Scholar]
- 70.Olesen M., Gudmand-Hoyer E. Efficacy, safety, and tolerability of fructooligosaccharides in the treatment of irritable bowel syndrome. Am. J. Clin. Nutr. 2000;72:1570–1575. doi: 10.1093/ajcn/72.6.1570. [DOI] [PubMed] [Google Scholar]
- 71.Silk D.B., Davis A., Vulevic J., Tzortzis G., Gibson G.R. Clinical trial: The effects of a trans-galactooligosaccharide prebiotic on faecal microbiota and symptoms in irritable bowel syndrome. Aliment. Pharmacol. Ther. 2009;29:508–518. doi: 10.1111/j.1365-2036.2008.03911.x. [DOI] [PubMed] [Google Scholar]
- 72.Niv E., Halak A., Tiommny E., Yanai H., Strul H., Naftali T., Vaisman N. Randomized clinical study: Partially hydrolyzed guar gum (PHGG) versus placebo in the treatment of patients with irritable bowel syndrome. Nutr. Metab. 2016;13:10. doi: 10.1186/s12986-016-0070-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saadi M., McCallum R.W. Rifaximin in irritable bowel syndrome: Rationale, evidence and clinical use. Ther. Adv. Chronic. Dis. 2013;4:71–75. doi: 10.1177/2040622312472008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Distrutti E., Monaldi L., Ricci P., Fiorucci S. Gut microbiota role in irritable bowel syndrome: New therapeutic strategies. World J. Gastroenterol. 2016;22:2219–2241. doi: 10.3748/wjg.v22.i7.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Menees S.B., Maneerattannaporn M., Kim H.M., Chey W.D. The efficacy and safety of rifaximin for the irritable bowel syndrome: A systematic review and meta-analysis. Am. J. Gastroenterol. 2012;107:28–35. doi: 10.1038/ajg.2011.355. [DOI] [PubMed] [Google Scholar]
- 76.Lembo A., Pimentel M., Rao S.S., Schoenfeld P., Cash B., Weinstock L.B., Paterson C., Bortey E., Forbes W.P. Repeat Treatment With Rifaximin Is Safe and Effective in Patients With Diarrhea-Predominant Irritable Bowel Syndrome. Gastroenterology. 2016;151:1113–1121. doi: 10.1053/j.gastro.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 77.Konig J., Siebenhaar A., Hogenauer C., Arkkila P., Nieuwdorp M., Noren T., Ponsioen C.Y., Rosien U., Rossen N.G., Satokari R., et al. Consensus report: Faecal microbiota transfer—Clinical applications and procedures. Aliment. Pharmacol. Ther. 2017;45:222–239. doi: 10.1111/apt.13868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Vaughn B.P., Rank K.M., Khoruts A. Fecal Microbiota Transplantation: Current Status in Treatment of GI and Liver Disease. Clin. Gastroenterol. Hepatol. 2019;17:353–361. doi: 10.1016/j.cgh.2018.07.026. [DOI] [PubMed] [Google Scholar]
- 79.Jiang Z.D., Ajami N.J., Petrosino J.F., Jun G., Hanis C.L., Shah M., Hochman L., Ankoma-Sey V., DuPont A.W., Wong M.C., et al. Randomised clinical trial: Faecal microbiota transplantation for recurrent Clostridum difficile infection—Fresh, or frozen, or lyophilised microbiota from a small pool of healthy donors delivered by colonoscopy. Aliment. Pharmacol. Ther. 2017;45:899–908. doi: 10.1111/apt.13969. [DOI] [PubMed] [Google Scholar]
- 80.Kassinen A., Krogius-Kurikka L., Makivuokko H., Rinttila T., Paulin L., Corander J., Malinen E., Apajalahti J., Palva A. The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology. 2007;133:24–33. doi: 10.1053/j.gastro.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 81.Holvoet T., Joossens M., Wang J., Boelens J., Verhasselt B., Laukens D., van Vlierberghe H., Hindryckx P., De Vos M., De Looze D., et al. Assessment of faecal microbial transfer in irritable bowel syndrome with severe bloating. Gut. 2017;66:980–982. doi: 10.1136/gutjnl-2016-312513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mazzawi T., Lied G.A., Sangnes D.A., El-Salhy M., Hov J.R., Gilja O.H., Hatlebakk J.G., Hausken T. The kinetics of gut microbial community composition in patients with irritable bowel syndrome following fecal microbiota transplantation. PLoS ONE. 2018;13:e0194904. doi: 10.1371/journal.pone.0194904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Halkjaer S.I., Christensen A.H., Lo B.Z.S., Browne P.D., Gunther S., Hansen L.H., Petersen A.M. Faecal microbiota transplantation alters gut microbiota in patients with irritable bowel syndrome: Results from a randomised, double-blind placebo-controlled study. Gut. 2018;67:2107–2115. doi: 10.1136/gutjnl-2018-316434. [DOI] [PubMed] [Google Scholar]
- 84.Myneedu K., Deoker A., Schmulson M.J., Bashashati M. Fecal microbiota transplantation in irritable bowel syndrome: A systematic review and meta-analysis. United Eur. Gastroenterol. J. 2019;7:1033–1041. doi: 10.1177/2050640619866990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Paramsothy S., Walsh A.J., Borody T., Samuel D., van den Bogaerde J., Leong R.W., Connor S., Ng W., Mitchell H.M., Kaakoush N.O., et al. Gastroenterologist perceptions of faecal microbiota transplantation. World J. Gastroenterol. 2015;21:10907–10914. doi: 10.3748/wjg.v21.i38.10907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cammarota G., Ianiro G., Kelly C.R., Mullish B.H., Allegretti J.R., Kassam Z., Putignani L., Fischer M., Keller J.J., Costello S.P., et al. International consensus conference on stool banking for faecal microbiota transplantation in clinical practice. Gut. 2019;68:2111–2121. doi: 10.1136/gutjnl-2019-319548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Clevers E., Tran M., Van Oudenhove L., Storsrud S., Bohn L., Tornblom H., Simren M. Adherence to diet low in fermentable carbohydrates and traditional diet for irritable bowel syndrome. Nutrition. 2020;73:110719. doi: 10.1016/j.nut.2020.110719. [DOI] [PubMed] [Google Scholar]
- 88.Harper A., Naghibi M.M., Garcha D. The Role of Bacteria, Probiotics and Diet in Irritable Bowel Syndrome. Foods. 2018;7:13. doi: 10.3390/foods7020013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rao S.S., Yu S., Fedewa A. Systematic review: Dietary fibre and FODMAP-restricted diet in the management of constipation and irritable bowel syndrome. Aliment. Pharmacol. Ther. 2015;41:1256–1270. doi: 10.1111/apt.13167. [DOI] [PubMed] [Google Scholar]
- 90.Eswaran S.L., Chey W.D., Han-Markey T., Ball S., Jackson K. A Randomized Controlled Trial Comparing the Low FODMAP Diet vs. Modified NICE Guidelines in US Adults with IBS-D. Am. J. Gastroenterol. 2016;111:1824–1832. doi: 10.1038/ajg.2016.434. [DOI] [PubMed] [Google Scholar]
- 91.Zahedi M.J., Behrouz V., Azimi M. Low fermentable oligo-di-mono-saccharides and polyols diet versus general dietary advice in patients with diarrhea-predominant irritable bowel syndrome: A randomized controlled trial. J. Gastroenterol. Hepatol. 2018;33:1192–1199. doi: 10.1111/jgh.14051. [DOI] [PubMed] [Google Scholar]
- 92.Schumann D., Langhorst J., Dobos G., Cramer H. Randomised clinical trial: Yoga vs. a low-FODMAP diet in patients with irritable bowel syndrome. Aliment. Pharmacol. Ther. 2018;47:203–211. doi: 10.1111/apt.14400. [DOI] [PubMed] [Google Scholar]
- 93.Eswaran S., Dolan R.D., Ball S.C., Jackson K., Chey W. The Impact of a 4-Week Low-FODMAP and mNICE Diet on Nutrient Intake in a Sample of US Adults with Irritable Bowel Syndrome with Diarrhea. J. Acad. Nutr. Diet. 2019 doi: 10.1016/j.jand.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 94.Dolan R., Chey W.D., Eswaran S. The role of diet in the management of irritable bowel syndrome: A focus on FODMAPs. Expert Rev. Gastroenterol. Hepatol. 2018;12:607–615. doi: 10.1080/17474124.2018.1476138. [DOI] [PubMed] [Google Scholar]
- 95.O’Keeffe M., Jansen C., Martin L., Williams M., Seamark L., Staudacher H.M., Irving P.M., Whelan K., Lomer M.C. Long-term impact of the low-FODMAP diet on gastrointestinal symptoms, dietary intake, patient acceptability, and healthcare utilization in irritable bowel syndrome. Neurogastroenterol. Motil. 2018;30 doi: 10.1111/nmo.13154. [DOI] [PubMed] [Google Scholar]
- 96.Staudacher H.M. Nutritional, microbiological and psychosocial implications of the low FODMAP diet. J. Gastroenterol. Hepatol. 2017;32:16–19. doi: 10.1111/jgh.13688. [DOI] [PubMed] [Google Scholar]
- 97.Singh R.K., Chang H.W., Yan D., Lee K.M., Ucmak D., Wong K., Abrouk M., Farahnik B., Nakamura M., Zhu T.H., et al. Influence of diet on the gut microbiome and implications for human health. J. Transl. Med. 2017;15:73. doi: 10.1186/s12967-017-1175-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Staudacher H.M., Whelan K. The low FODMAP diet: Recent advances in understanding its mechanisms and efficacy in IBS. Gut. 2017;66:1517–1527. doi: 10.1136/gutjnl-2017-313750. [DOI] [PubMed] [Google Scholar]
- 99.Biesiekierski J.R., Newnham E.D., Irving P.M., Barrett J.S., Haines M., Doecke J.D., Shepherd S.J., Muir J.G., Gibson P.R. Gluten causes gastrointestinal symptoms in subjects without celiac disease: A double-blind randomized placebo-controlled trial. Am. J. Gastroenterol. 2011;106:508–514. doi: 10.1038/ajg.2010.487. [DOI] [PubMed] [Google Scholar]
- 100.Rej A., Sanders D.S. Gluten-Free Diet and Its ‘Cousins’ in Irritable Bowel Syndrome. Nutrients. 2018;10:1727. doi: 10.3390/nu10111727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Skodje G.I., Sarna V.K., Minelle I.H., Rolfsen K.L., Muir J.G., Gibson P.R., Veierod M.B., Henriksen C., Lundin K.E. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology. 2018;154:529–539. doi: 10.1053/j.gastro.2017.10.040. [DOI] [PubMed] [Google Scholar]
- 102.Liang D., Longgui N., Guoqiang X. Efficacy of different probiotic protocols in irritable bowel syndrome: A network meta-analysis. Medicine. 2019;98:e16068. doi: 10.1097/MD.0000000000016068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.McFarland L.V., Dublin S. Meta-analysis of probiotics for the treatment of irritable bowel syndrome. World J. Gastroenterol. 2008;14:2650–2661. doi: 10.3748/wjg.14.2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Connell M., Shin A., James-Stevenson T., Xu H., Imperiale T.F., Herron J. Systematic review and meta-analysis: Efficacy of patented probiotic, VSL#3, in irritable bowel syndrome. Neurogastroenterol. Motil. 2018;30:e13427. doi: 10.1111/nmo.13427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tiequn B., Guanqun C., Shuo Z. Therapeutic effects of Lactobacillus in treating irritable bowel syndrome: A meta-analysis. Intern. Med. 2015;54:243–249. doi: 10.2169/internalmedicine.54.2710. [DOI] [PubMed] [Google Scholar]
- 106.Ritchie M.L., Romanuk T.N. A meta-analysis of probiotic efficacy for gastrointestinal diseases. PLoS ONE. 2012;7:e34938. doi: 10.1371/journal.pone.0034938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Horvath A., Dziechciarz P., Szajewska H. Meta-analysis: Lactobacillus rhamnosus GG for abdominal pain-related functional gastrointestinal disorders in childhood. Aliment. Pharmacol. Ther. 2011;33:1302–1310. doi: 10.1111/j.1365-2036.2011.04665.x. [DOI] [PubMed] [Google Scholar]
- 108.Hoveyda N., Heneghan C., Mahtani K.R., Perera R., Roberts N., Glasziou P. A systematic review and meta-analysis: Probiotics in the treatment of irritable bowel syndrome. BMC Gastroenterol. 2009;9:15. doi: 10.1186/1471-230X-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Moayyedi P., Ford A.C., Talley N.J., Cremonini F., Foxx-Orenstein A.E., Brandt L.J., Quigley E.M. The efficacy of probiotics in the treatment of irritable bowel syndrome: A systematic review. Gut. 2010;59:325–332. doi: 10.1136/gut.2008.167270. [DOI] [PubMed] [Google Scholar]
- 110.Nikfar S., Rahimi R., Rahimi F., Derakhshani S., Abdollahi M. Efficacy of probiotics in irritable bowel syndrome: A meta-analysis of randomized, controlled trials. Dis. Colon. Rectum. 2008;51:1775–1780. doi: 10.1007/s10350-008-9335-z. [DOI] [PubMed] [Google Scholar]
- 111.Xu D., Chen V.L., Steiner C.A., Berinstein J.A., Eswaran S., Waljee A.K., Higgins P.D.R., Owyang C. Efficacy of Fecal Microbiota Transplantation in Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis. Am. J. Gastroenterol. 2019;114:1043–1050. doi: 10.14309/ajg.0000000000000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ianiro G., Eusebi L.H., Black C.J., Gasbarrini A., Cammarota G., Ford A.C. Systematic review with meta-analysis: Efficacy of faecal microbiota transplantation for the treatment of irritable bowel syndrome. Aliment. Pharmacol. Ther. 2019;50:240–248. doi: 10.1111/apt.15330. [DOI] [PubMed] [Google Scholar]
- 113.Li J., Zhu W., Liu W., Wu Y., Wu B. Rifaximin for Irritable Bowel Syndrome: A Meta-Analysis of Randomized Placebo-Controlled Trials. Medicine. 2016;95:e2534. doi: 10.1097/MD.0000000000002534. [DOI] [PMC free article] [PubMed] [Google Scholar]