Abstract
Purpose of review:
Evaluating longer-term mortality, morbidity, and quality of life in survivors of critical illness is a research priority. This review details the challenges of long-term follow-up studies of critically ill patients and highlights recently proposed methodological solutions.
Recent findings:
Barriers to long-term follow-up studies of critical care survivors include high rates of study attrition due to death or loss to follow-up, data missingness from experienced morbidity, and lack of standardized outcome as well as reporting of key covariates. A number of recent methods have been proposed to reduce study subject attrition, including minimum data set selection and visits to transitional care or home settings, yet these have significant downsides as well. Conducting long-term follow-up even in the absence of such models carries a high expense, as personnel are very costly, and patients/families require reimbursement for their time and inconvenience.
Summary:
There is a reason why many research groups do not conduct long-term outcomes in critical care: it is very difficult. Challenges of long-term follow-up require careful consideration by study investigators to ensure our collective success in data integration and a better understanding of underlying mechanisms of mortality and morbidity seen in critical care survivorship.
Keywords: Mortality, Attrition, Loss to Follow-Up, Data Missingness, ICU survivors, Family
Introduction
As more patients survive critical illness, attention has shifted towards evaluating longer-term mortality, morbidity, and quality of life. However, this increased interest has shed light on many important methodological challenges of conducting this research (Figure 1). Important challenges facing investigators are how best to retain subjects in follow-up studies, reduce threats to both internal and external validity, and achieve sufficient statistical power, obtain external funding necessary to staff and conduct such research, and incorporation of family and loved ones by which to assess the full extent of the long-term burden of critical care. Further, greater attention has been given in recent years the best methods by which to perform analyses in long-term follow-up studies of ICU subjects when primary outcome measures are often truncated by death or other events. Lastly, having a core outcome set and uniformly reporting key covariates may facilitate the intersection of various dataset to answer complex questions, however such initiatives may inadvertently dampen innovation and creativity. This article provides a review of methodological challenges encountered in conducting long-term follow-up studies of critically ill patients and evolving solutions.
Figure 1.
A pictorial representation of challenges in conducting long-term outcomes studies. This list is not exhaustive but includes limits in estimating pre-morbid status, challenges in defining a study population of interest, delineating ICU-associated as compared to hospitalization-associated risk, establishing time to outcome assessment, and determination of which outcomes measures to assess.
Mortality
Survivors of critical illness have poor long-term survival. In a recent large cohort of ICU survivors from 21 ICUS in France and Belgium, 1-year mortality was 21% [1]. The need for mechanical ventilation portends a worse long-term prognosis, with an epidemiological study of over 35,000 Medicare patients having survived ICU admission demonstrating that mechanical ventilation was associated with a 58% risk of death at 3 years [2]. The need for greater in-ICU resource intensity has been shown to necessitate greater resource utilisation after discharge leading to greater likelihood of readmission [3]; as high as 84% of ICU survivors return to the emergency department with 65% requiring hospital readmission. The majority of rehospitalizations occur within the first year following discharge, a time period during which long-term follow-up in ICU survivorship trials is concentrated [3]. Beyond one year, 25% of ICU survivors are readmitted to the ICU during the 5 years following index hospitalization. Age and pre-existing chronic illnesses are the greatest influences on predicted risk of death, with overall 1-year survival for patients over the age of 80 years being reported as low as 42% [4]. Depending on the patient population (e.g. admitting diagnosis of sepsis or more aged patients) as well as the duration of follow-up (i.e. longer duration greater number of subjects likely to die before end of study) special consideration should be taken into the calculation of sample size to ensure there will be adequate number of subjects to assess at long-term follow-up. Achieving and maintaining adequate numbers of subjects is of increasing importance as the state of research shifts from primarily descriptive reviews of mortality and functional outcomes towards attempting to ascertain causal inference.
Loss to follow-up
Low follow-up rates are an important limitation in the interpretation of long-term ICU outcomes studies, especially because the patients lost to follow-up likely have important cognitive and/or physical deficits leading to their lack of retention. Researchers continue to debate the minimum participant retention rate acceptable to preserve study validity. The social science literature suggests a minimum rate of 70–80% [5]; no such guidelines exist for studies of ICU survivorship. It seems however that in both longitudinal cohorts and randomized controlled trials with long-term follow-up, investigators are achieving on average rates of 70–80%. For example, Herridge and colleagues in the Towards RECOVER study (n=391) evaluated 90% of subjects in hospital, and then 71%, 74% and 83% of eligible ICU survivors at 3-, 6- and 12-months respectively [6]. These follow-up rates were achieved by a well-experienced team with expertise in retention strategies for long-term follow-up. Comparing follow-up in the BRAIN-ICU [7] and COGWELL [8] studies both are studies of long-term cognition after ICU discharge one may get an idea of the size of team required to achieve such numbers (Figure 2). In the BRAIN-ICU study at 1-year follow-up, a large team of over 10 dedicated research personnel were able to achieve follow-up rates of 94%. In contrast, a single researcher and part-time research assistant in the COGWELL study achieved follow-up rates of only 73% (62% evaluated).
Figure 2.
Consort diagrams of two studies (A. BRAIN-ICU study [7] and B. COGWELL study [8] unpublished) of long-term cognitive follow-up of varying numbers of both participants and study personnel. All efforts should be made to limit study attrition from loss to follow-up to minimize bias, enhance generalizability as well as study validity. Strategies to mitigate loss to follow-up are heavily dependent on numbers of study personnel, dedicated time to allocate to retention strategies, and adequate funding to enact such aggressive strategies.
It is common to underestimate the number of study personnel required to ensure adequate follow-up, further, to misjudge the financial expense needed from external funding for such ventures. Strategies suggested for subject retention include using a systematic method for patient contact, scheduling, and cohort retention monitoring (e.g. obtaining multiple contacts for each participant, including two contacts not residing with the participant); minimizing participant burden through characteristics and procedures of follow-up study clinics (e.g. offering flexible clinic appointments); and, specifically training and managing study personnel (e.g. assigning one primary physician to each participant or hiring culturally sensitive staff with strong interpersonal skills) [9, 10], effective incorporation of these measures requires time, dedication, and training. Most importantly, adequate follow-up requires a large budget for adequate staffing and to allow staff the time to pursue these resource-intense endeavours to limit study attrition [11].
Expanding on the need to further understand and develop strategies to maximize subject retention, future strategies might include off-site or home visits, either in person or via available technologies. Waters and colleagues recently analyzed patient-related factors for requiring off-site or home visits in follow-up of subjects participating in either the Toronto 5-year Acute Respiratory Distress Syndrome (ARDS) outcomes study and RECOVER program [12]. Patients with the most significant functional dependency and medical complexity were more likely to require an off-site or home visit for follow-up [12]. Further study of the need for off-site or home visits may provide not only an opportunity to limit study attrition rates but might identify and therefore allow investigators to address issues that might prevent study follow-up, and possibly even readmission or death.
Although the current evidence supports the effectiveness of transitional care models in reducing hospital readmissions, the component of transitional care delivery from which patients are most likely to benefit has yet to be determined [13]. In a randomized controlled trial of elderly patients discharged from hospital, visits from an advanced practice nurse during the first four weeks after hospital discharge significantly delayed the time to first readmission and reduced the total number of multiple readmissions [14]. In a pair of studies of patients with chronic congestive heart failure, those patients who received home visits within 7 to 14 days after discharge had fewer unplanned readmissions and longer survival [15]. In a retrospective cohort of Medicaid recipients requiring complex care for their chronic conditions, home visits reduced the likelihood of a 30-day readmission by almost half, as compared to less intensive forms of nurse-led transitional care support [16]. Higher risk patients seemed to experience the greatest benefit in terms of number of inpatient admissions and total cost of care 6 months following discharge [16]. Outside of home visits, thinking of other solutions to meet the needs of follow-up subjects may need to be more creative. For example, a research study “car service” may facilitate one making in-person appointments. For an ICU survivor who lived 27 kilometres from the follow-up clinic and lacked the confidence in her own motor dexterity and response time to drive on the highway, our study team drove out to pick her up so that she could undergo a full cognitive evaluation and an electroencephalography study. By her second follow-up, her motor dexterity improved and as had her confidence, as a result she was enthusiastic to report that she was able to transport herself to clinic for her 12-months follow-up visit. Further study of the needs of patients unable to attend in-person follow-up is desperately needed to investigate the benefit of such a laborious endeavor for researchers and to minimize the inherent bias introduced by high rates of loss to follow-up.
Missing data points
Subjects who are not necessarily lost to follow-up but have missing data from incomplete study visits also contribute to decreased precision and statistical power, thus introducing selection bias. Many ICU survivors have poor baseline health and health related quality of life, and often face new or worse physical, psychological and cognitive morbidity after hospitalization [17]. These impairments may present difficulties for subjects to participate in longitudinal studies as follow-up assessments tend to be lengthy and involve multiple neuropsychological and physical surveys as well as performance-based tests [18–23]. As an example, to perform the minimum acceptable Core Outcome Measurement Set, comprising 42 questions, the estimated completion time is 12 minutes. Including the optional Montreal Cognitive Assessment instrument with the Short Form-36 raises the total number of questions to 91 and requires an estimated 26 minutes [21]. These times of course do not take into account initial time spent speaking with the subject, and possibly a family member or friend, about how things have been going since hospital discharge or the reassurance needed to complete the assessments if significant functional, cognitive or mood impairment.
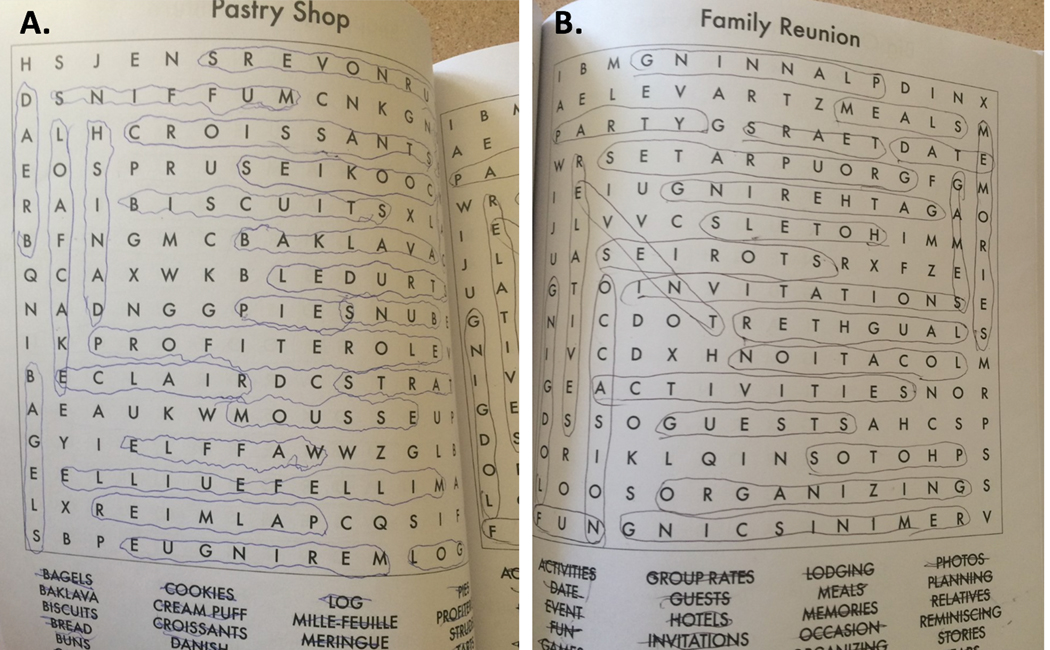
A real-world illustration of how morbidities experienced by this patient population may influence subject performance is shown in Figure 3. Although a minimum outcome dataset is an important initiative to help guide measurement selection, it may also be seen as a challenge in and of itself in this type of research. As investigators we need to maintain a degree of adaptability to meet the needs of our patients, while they are trying to provide us with the answers to ICU survivorship. We need to remain sensitive to the individual trajectories of disability and ensure that we don’t contribute to the frustrations that our patients face during recovery. Sensitivity to the needs of our patients should always supersede the need for a complete dataset. Further, one might argue that in many settings of long-term outcomes research, a minimum acceptable dataset may pose a very real set of problems that could stifle discovery through the restriction of research questions or possibly limitations in a more mechanistically driven sequence of measures. The focus of the Core Outcome Measurement Set is very heavy in functional measures and one might argue, giving an option for a cognitive screening tool where patients have made it clear that the maintenance of cognitive function after critical illness is a leading priority is in and of itself a limitation. We do however recognize the importance of standardization for making between study comparisons, however we caution investigators to use such measurement sets as a guide and to prioritize what is required in the interests of your patients and for answering the research question of interest.
Figure 3.
56-year-old university educated woman status post lung transplant. After hospital discharge, she reported difficulties with concentration and found reading to be overwhelming. She started to do word searches in the hopes that that would mediate some of her experienced symptoms. Shown on the left is a puzzle completed around her 6-months follow-up appointment; as can be seen her fine motor dexterity had not returned to her baseline at that time. Outside of this finding, her cognitive testing was within normal limits. Shown on the right is a puzzle she again completed but this time proximate to her 1-year follow-up. At this time, she not only subjectively felt that her concentration had improved but also her confidence in her daily activities, both of which seemed to lag behind her functional recovery.
A greater understanding of the barriers to complete data collection during follow-up visits may assist investigators in anticipating and tailoring their follow-up efforts. These factors are just starting to be elucidated. Recently, Heins and colleagues evaluated risk factors for missed assessments over a 6 to 24 months follow-up period in survivors of acute respiratory distress syndrome; number of dependencies in activities of daily living at hospital discharge was associated with higher odds of missed assessments at the initial visit of 3 months follow-up [24]. Variables associated with higher odds of missed assessments at subsequent visits were two or more dependencies of instrumental activities of daily living at hospital discharge and having missed assessments at the prior follow-up [24]. Just like adaptive trial design for mortality outcomes can reduce missing assessments, longitudinal clinical research studies may benefit from modifying parameters of follow-up based on subject performance. For example, if a subject has significant functional impairment at 3-months, future outcome measures might be modified such that those most important to the study are evaluated first; this then becomes the dataset carried through for that subject until the end of the trial.
Outcome measure selection across studies
Heterogeneity in the outcomes and measurement instruments used in ICU survivor studies has created a major barrier in synthesizing results. In a recent review by Turnbull et al., more than 300 original research publications on ICU survivors’ outcomes after hospital discharge since 2000 had highly variable time to follow-up and measures [25]. A further scoping review found that 250 unique measurement instruments were used between 1970 and 2013 to assess ICU survivors after hospital discharge [21]. As of May 2019, there are 16 projects registered with the Core Outcome Measures in Effectiveness Trials (COMET) Initiative (http://www.comet-initiative.org/).
Other than establishing a core set of outcomes and measurement instruments, work must also focus on standardizing definitions of clinically important difference. As an example of the difficulty in defining a clinically important difference, we can draw on our own experience in studying cognitive outcomes. Our attempt to compare rates of cognitive impairment across studies proved difficult as different batteries have been employed and widely divergent definitions of impairment used (Table 1). We found no consistency in the definitions used for impairment (e.g. 1 SD, 1.5 SDs or 2 SDs below the normative mean). Further, there was inconsistent reporting of whether cut-off scores for impairment were adjusted for age, education or premorbid ability.
Table 1.
Definitions used and covariates reported in studies of cognitive impairment after ICU discharge
| Study Dates | Study Design Population | Cognitive Test(s) | Definition of abnormality | Quality of outcome measured | Covariates reported in Table 1 |
|---|---|---|---|---|---|
| Ambrosino 2002 [31] January 1996 –December 1998 | Prospective; controlled; consecutive 63 COPD patients requiring MV; control group 34 stable COPD patient on LT oxygen therapy admitted to inpatient pulmonary rehabilitation program | Mini Mental Status Exam (MMSE) | MMSE < 24 | 2 (screening test) | Sex, age, BMI, PFTs, MIP/MEPs, PaCO2/PaO2 |
| Baumbach 2016 [32] September 2014 – March 2015 | Prospective cohort; self-selected by response to contact via mail 127 patients aged 18 to 85 years; mixed MSICU with minimum ICU LOS of 24 hrs | Functional Assessment of Cancer Therapy-Cognitive Function Adapted (FACT-Cogadapted) Informant Questionnaire of Cognitive Decline in the Elderly (IQCODE) | Likert scale; no clear definition of CI | 1 (self-reported) | Sex, age, education, employed (yes/no), APACHEII, hospital LOS, ICU LOS, days of MV, admission diagnosis |
| Bruck 2018 [33] January 2012 – February 2013 | Prospective cohort; patients with sepsis who were part of the PRE-DELIRIC study who responded to questionnaire 125 patients; mixed MSICU with minimum ICU LOS of 24 hrs | Cognitive Failures Questionnaire (CFQ) | Total CFQ score > 25 | 2 | Sex, age, history of cognitive impairment, alcohol use, drug use, diabetes, vascular disease, cardiac disease, APACHEII, type of ICU admission |
| Calsavara 2018 [34]-- | Prospective cohort; severe sepsis or septic shock during ICU stay 33 patients; 16 patients at 1 year | Consortium to Establish Registry for Alzheimer’s Disease (CERAD) battery | -- | 3 (Neuropsychological testing) | Sex, age, education, APACHEII, SOFA, ICU LOS, lab parameters (hemoglobin, Cr, lactate, CRP, glucose), site of infection, comorbidity index, IQCODE, cumulative doses of analgesia/sedatives/inotropes/pressors, steroid exposure, dialysis, days of MV |
| Christie 2006 [35]-- | 2 cross-sectional studies 1) 79 ARDS patients; internet ARDS support site 2) 34 ARDS patients discharged [in-person cognitive interviews] |
Neurobehavioral Cognitive Status Exam (NCSE): Judgment Wechsler Memory Scale )WMS)-III: Digit Span; Letter-Number Sequencing; Logical Memory I/II; Similarities Controlled Oral Word Association Hayling Sentence Completion Test | 2 test scores ≥1 SD or more below the population norm or a single test score ≥1.5 SDs below population norm | 3 | Sex, age, education, race, marital status, alcohol use, smoking status, comorbid conditions, prehospitalization function, prehospitalization cognition, prehospitalization depression |
| Chung 2017 [36] June 2014 – May 2015 | Retrospective; consecutive 30 patients from MICU, CCU and SICU | Mini-Cog test | Recall of 0 items or recall of 1–2 items with an abnormal clock face | 2 | Sex, age, high school graduate (yes/no), type of ICU, reason for admission, GCS at admission, SOFA, days of MV, days delirious, ICU LOS |
| Davydow 2013 [37] September 2010 – August 2011 | Prospective cohort; consecutive 150 nontrauma patients without cognitive impairment or dementia diagnosis who were admitted to an ICU for > 24 hrs; 120 patients completed FU |
Telephone Interview for Cognitive Status modified (TICSm) Mini International Neuropsychiatric Interview |
-- | 2 | Sex, age, education, |
| De Azevedo 2017 [38] March 2014 – February 2015 | Prospective cohort; consecutive 413 adult patients mechanically ventilated | Digit span forward and backward Rey Auditory Verbal Learning Test (RAVLT) Clock-drawing test Verbal fluency test MMSE | Mild or moderate impairment if 2 test scores 1.5 SDs below the mean or test scores 2 SDs below the mean; severe CI if ≥3 test scores 1.5 SD below the mean | 3 | Sex, age, education, APACHE IV, SOFA, days of MV, use of sedative agents, admission diagnosis, delirium (yes/no), ICU LOS |
| De Oliveira 2014 [39] February 2001 – March 2009 | Prospective cohort; consecutive 234 patients with severe TBI (GCS > or = 8); 46 were evaluated at 1 year | WMS-III Logical Memory First Recall; Logical Memory I/II; Visual Reproduction I/II/ III RVALT Total; Retention; Delayed Memory Wechsler Adult Intelligence Scale (WAIS)-III-Digit Span; Vocabulary; Similarities; Block Design; Letters Fluency; Category Fluency | -- | 3 | Sex, age, education, hand dominance, glucose, CT head characteristics, SAH (yes/no), multisystem trauma (yes/no), type of trauma, GCS, pupils |
| De Rooij 2008 [40] January 1997 – December 2002 | Retrospective; consecutive 164 patients >80 yrs; mixed MSICU who underwent elective surgery | IQCODE-SF Katz Activities of Daily Living(ADLs) EQ-5D | Score > 3.9 on IQCODE-SF severe CI; 3.1–3.8 mild-moderate CI | 2 | Sex, age, education, social status, cardiopulmonary resuscitation, GCS after 24 hrs, SAPS II, APACHE II, planned or unplanned admission, BMI, MV (%), ICU LOS |
| Duggan 2017 [41]-- | Prospective; consecutive 826 patients mixed MSICU population for respiratory failure, cardiogenic shock, or septic shock | Behavior Rating Inventory of Executive Function–Adult (BRIEF-A) Trail Making Test B Beck’s Depression Index (BDI)-II Short Form(SF)-36 ADLs Instrumental ADLs (IADLs) | BRIEF-A impairment defined as t-score ≥ 65; Trails B impairment is defined as t-score ≤ 35 | 3 | Sex, age, race, marital status, employment status, baseline clinical status, pre-existing CI, history of depression, history of nondepressive mental illness, comorbidity index, admit diagnosis, ICU type, SOFA, days of MV, septic (yes/no), stroke in hospital (yes/no), ICU LOS, discharge destination |
| Duning 2010 [42] January 2004 – December 2007 | Case-control 74 patients 18–80 yrs of age; 37 patients had at least one hypoglycemic event during SICU admission | MMSE Boston Naming Test Nuernberg Gerontopsychological Inventory Digit symbol substitution Color word interference tasks WMS (revised) Regensburg Word Fluency Test Trail Making test Rey-Osterrieth Complex FigureRAVLT Recognition | -- | 3 (compared to 2) | Matching criteria: sex, age, SAPS II, yr of ICU treatment; disease related criteria: type of OR, CP resuscitation, DM I or II, ICU LOS, mean am blood glucose, duration of sedation (<3 days, 3–7 days, 1–2 weeks, > 2 weeks), PF ratio, CV failure (pressors, MV assist device), renal failure, hepatic failure, medications (steroids, immunosuppressants) |
| Ehlenbach 2010 [43] 1994 – 1996 (2581 participants); 2000 – 2002 (additional 811 individuals) | Prospective; cohort Enrolled patients are evaluated q2yrs; 41 persons were hospitalized for critical illness | Cognitive Abilities Screening Instrument (CASI) | <86 prompted a full standardized clinical exam | 2 | Sex, age, race, education, CAD (yes/no), CV disease (yes/no), pulm dz (yes/no), D< (yes/no), renal dz, malignancy, follow-up time, study visits |
| Girard 2010 [44] October 2003 – March 2006 | Nested in RCT; prospective 76 MICU patients | MMSE Digit span Trail Making tests A and B Digit Symbol Coding Rey-Osterrieth Complex Figure RVALT | 2 cognitive test scores 1.5 SDs below the mean; one cognitive test score 2 SDs below the mean | 3 | Sex, age, education, APACHE II, admission diagnoses (sepsis, ARDS, MI/CHF, COPD/asthma, altered MS, hepatic or renal failure, malignancy, alcohol withdrawal, other), delirium in ICU (prevalence, duration), sedation exposure (benzos, opiates, propofol) |
| Girard 2018 [45] March 2007 - May 2010 | Multicenter; prospective; cohort 586 patients managed in a medical or surgical ICU with respiratory failure, septic or cardiogenic shock, or both | RBANS MMSE Trail Making Test B IQCODE | -- | 3 | Sex, age, race, education, short IQCODE, pre-existing CI, comorbidity index, admission diagnosis, APACHEII, SOFA, days of MV, dexamethasone/benzodiazepine/opioid/ propofol exposure, ICU LOS, hospital LOS, Framingham stroke risk profile, duration of severe sepsis, no. of 15 mins intervals with hypoxia |
| Godbolt 2012 [46] January 2010 – June 2011 | Multicenter; prospective; cohort 110 patients with severe TBI | Barrow Neurological Institute Screening of Cognitive function | Total score < 2 SD below the mean | 2 | -- |
| Guillamondegui 2011 [47] July 2006 – June 2007 | Prospective; cohort 108 patients with moderate-severe TBI; patients with hypoxemic event (SaO2 < 85%) within first 48 hrs of admission | Employment questions and battery of validated neuropsychological testing instruments | 2 test scores 1.5 SDs below the mean or 1 test score 2 SDs below the mean | 3 | Sex, age, ISS, ED GCS, ED pulse, ED SBP, transfusion, MV days, ICU LOS, SpO2 < 90% or 85% for > 5 mins; delirium (prevalence) |
| Hope 2013 [48] January 2003 - December 2007 | Prospective; consecutive; cohort 385 adults admitted to a respiratory care unit for treatment of chronic critical illness; undergone elective tracheostomy for weaning | Validated telephone version of the Confusion Assessment Method (CAM) | Three possible values: dead, alive with brain dysfunction, and alive without brain dysfunction | 2 | Sex, age, race, cognitive impairment at baseline, residence prior to hospitalization, FIM at admission, IADLs at admission, admission diagnosis, type of ICU, ICU LOS, APACHE II, APS, comorbidity index |
| Hopkins 1999 [49] February 1994 – July 1988 | Prospective; consecutive; cohort 67 ARDS survivors | WAIS-R WMS-R RAVLT Rey-Osterrieth Complex Figure Trail Making Tests A and B Verbal Fluency (verbal production) | 2 test scores > 1.5 SD or 1 test score > 2 SD below the normative population mean | 3 | Sex, age, education, ICU LOS, duration MV |
| Hopkins 2004 [50]-- | Prospective; consecutive; cohort 66 ARDS survivors | WAIS-R WMS-R RAVLT Rey-Osterrieth Complex Figure Trail Making Tests A and B Verbal Fluency (verbal production) | <80%, <85% or <90% (compared to normative data) | 3 | Sex, age, education, hospital LOS, ICU LOS, duration MV, APACHE II, mean MOF score, PF ratio, PaO2 at time of enrolment, mean PaO2, FiO2 at time of enrolment, days from ARDS onset to enrolment in 1 yr outcome study |
| Hopkins 2005 [51] February 1994 – December 1999 | Prospective; consecutive; cohort 66 ARDS survivors (low vs. high tidal volume ventilation study) | WAIS-R WMS-R RAVLT Rey-Osterrieth Complex Figure Trail Making Tests A and B Verbal Fluency (verbal production) | 2 or more test scores > 1.5 SDs or 1 test score > 2 SDs below normative population mean | 3 | Sex, age, education, race, number of ARDS RFs, duration MV, ICU LOS, hospital LOS, at study enrolment (APACHE II, MOF score, PF ratio, FiO2, PaO2); total ICU stay (mean MOF score, mean PF ratio, Mean FiO2, mean PaO2) |
| Hopkins 2005 [52]-- | Prospective; cohort 32 patients having received >5 days of MV | Neuropsychological testing-- | ≥2 test scores > 1.5 SDs or 1 test score > 2 SD below normative population mean | 3 | Sex, age, education, Charlson comorbidity index, number of ARDS RFs, duration MV, ICU LOS, hospital LOS, at study enrolment (APACHE II, MOF score, PF ratio, FiO2, PaO2); total ICU stay (mean MOF score, mean PF ratio, Mean FiO2, hrs oximetry SaO2 < 90%, hrs MBP < 60 mmHg, hrs MBP < 50 mmHg, days reciving either sedatives, narcotics or paralytics) |
| Hopkins 2010 [53] February 1994 – December 1999 | Prospective; consecutive; cohort 66 ARDS survivors (low vs. high tidal volume ventilation study) | WAIS-R WMS-R RAVLT Rey-Osterrieth Complex Figure Trail Making Tests A and B Verbal Fluency (verbal production) | 2 or more test scores > 1.5 SD or 1 test score > 2 SD below normative population mean using age, gender and education corrected t-scores | 3 | Sex, age, education, hospital LOS, DM I or II, total corticosteroid dose, at study enrolment (APACHE II, MOF score, PF ratio, FiO2, PaO2); total ICU stay (duration MV, ICU LOS, Mean FiO2, mean PaO2, hrs oximetry SaO2 < 90%, total insulin units/ICU hours, total potassium dose, mean blood glucose, lowest glucose, highest glucose) |
| Hughes 2017 [54] March 2007 - May 2010 | Multicentre; prospective; cohort 1040 patients with major noncardiac surgery during hospital admission and with nonsurgical medical illness | RBANS Trail Making Test B | -- | 3 | Sex, age, race, education, SES, IQCODE, clinical frailty score, functional activities questionnaire, comorbidity index, Framingham stroke risk profile, SOFA< APACHE II, sepsis in ICU, days of MV, ever delirious, coma, sedative or analgesia use, ICU LOS, hospital LOS |
| Hughes 2018 [55] | Multicentre; prospective; cohort 419 adults admitted to a MICU or SICU with respiratory failure and/or shock | RBANS Trail Making Test B Katz ADLs Functional activities questionnaire | -- | 3 | Sex, age, race, education, SES, IQCODE, clinical frailty score, functional activities questionnaire, comorbidity index, Framingham stroke risk profile, SOFA< APACHE II, sepsis in ICU, days of MV, ever delirious, coma, sedative or analgesia use, ICU LOS, hospital LOS |
| Iwashyna 2010 [56] 1998 – 2006 | Prospective; nonconsecutive; cohort Enrolled patients are evaluated q2yrs; survivors of severe sepsis | 35-point scale; tests of memory, serial 7 subtractions, naming and orientation ADLs IADLs | -- | 2 | Sex, age, education, race, LOS, required MV, required dialysis, used ICU, underwent major surgery, Charlson score, organ dysfunction score, acute conditions (CV dysfunction, neurologic dysfunction, hematologic dysfunction, hepatic dysfunction, renal/respiratory dysfunction), baseline cognitive impairment, baseline functional disability |
| Jackson 2003 [57] February 2000 – May 2001 | Prospective; cohort; consecutive 34 patients; MICU and CICU; requiring MV | Modified Blessed Dementia Rating Scale (mBDRS) MMSE Digit Symbol Coding Thurstone Word Fluency Letter Number Sequencing Sequencing Verbal Paired Associates Digit Symbol Paired Recall Recall (Faces) Rey-Osterrieth Complex Figure | 2 test scores > 2 SDs below the norm-referenced mean or 3 test scores ≥1.5 SD below norm-referenced mean | 3 | Sex, age, education, race, ADL, APACHE, Charlson, SOFA, Admission diagnosis |
| Jackson 2007 [58] January 2003 – December 2003 | Prospective; nonconsecutive; cohort 58 trauma patients without ICH or focal neurologic deficits or moderate to severe TBI | Digit span Digit symbol FAS IQCODE-SF MMSE RAVLT Rey-Osterrieth Complex Figure Trail Making Tests A and B Katz ADLs | ≥2 test scores > 1.5 SDs or 1 test score > 2 SDs below normative population | 3 (compared to 2) | Sex, age, education, race, ISS, type of trauma, mental health history, employment status |
| Jackson 2010 [22] October 2003 – March 2006 | Randomised controlled trial of SAT/SBT 80 patients requiring MV for > 72 hrs | Digit span Digit symbol IQCODE-SF MMSE RAVLT Rey-Osterrieth Complex Figure Trail Making Tests A and B Verbal Fluency test Katz ADLs | ≥1.5 SDs below the mean on ≥2 of the nine cognitive tests or scored ≥2 SDs below the mean on ≥1 of the nine cognitive tests | 3 | Sex, age, APACHE II, SOFA, Admission diagnosis, pre-existing cognitive impairment, baseline ADL, baseline IADL, pre-enrolment sedative exposure, sedative exposure, lorazepam equivalents, fentanyl equivalents, propofol |
| Jackson 2011 [59] July 2006 – June 2007 | Prospective; cohort 108 patients with moderate to severe trauma; no ICH | Digit span Digit symbol Verbal Fluency test (FAS) IQCODE-SF MMSE RAVLT Rey-Osterrieth Complex Figure Trail Making tests A and B | ≥2 test scores > 1.5 SDs or 1 test score > 2 SDs below normative population | 3 | Sex, age, education, race, ISS, admission GCS, long-bone fracture, concussion, ICU LOS, hospital LOS, MV status, duration of MV, CAM+ days, type of trauma |
| Juan 2018 [60] July 2012 - May 2015 | Prospective; cohort 50 survivors included from a prospective cohort of 138 patients admitted at the ICU for cardiopulmonary arrest | Naming subtest of the Lexis battery California Verbal Learning Test Doors and People test Digit span forward subtest of WAIS-IV Block tapping WMS-R Five-points test Digit-symbol subtest of the WAIS-IV Alert and Divided attention subtests of the Test battery Trail Making and Stroop tests from the GREFEX battery | z score less than or equal to –1.65 SDs of the mean | 3 | Sex, age, cardiac etiology arrest, out of hospital cardiac arrest, time to return of spontaneous circulation, first shockable rhythm, therapeutic hypothermia (yes/no) |
| Jones 2006 [61] March 2003 – November 2004 | Prospective; cohort 30 long-stay, MV patients | Cambridge Neuropsychological Test Automated Battery (CANTAB) | ≤25 percentile compared with an age-, sex-matched control population | 3 | Sex, age, APACHE II, ICU LOS, diagnostic groups (peritonitis, pneumonia, asthma/COPD, sepsis, ARDS, trauma) |
| Larson 2007 [62] February 1994 – December 1999 | Interventional trial; higher vs lower tidal volume ventilation strategy 66 ARDS survivors | WAIS-R (FSIQ; Vocabulary; Block Design) WMS-R (Attention Index; Verbal; RAVLT; Visual; Rey-Osterrieth Complex Figure) Trail Making Test B | ≥2 test scores > 1.5 SDs or 1 test score > 2 SDs below normative population mean values using age, gender and education | 3 | Sex, age, hospital LOS, ICU LOS, duration of MV, APACHE II, Charlson Comorbidity index, mean MOF score, mean PaO2, mean FiO2, PF ratio, days receiving sedatives/narcotics/paralytics |
| Lippert-Gruner 2006 [63] | Prospective; cohort 41 patients with severe TBI | Neurobehavioural Rating Scale | -- | 2 | Sex, age |
| Maley 2016 [64] January – May 2014 | Prospective; mixed-methods investigation 43 survivors from two MICUs | Health Utilities Index - 3 cognitive questions Hospital Anxiety and Depression Scale (HADS) Connor-Davidson Resilience Scale Life-Space Questionnaire | -- | 1 | Sex, age, race, marital status, no. of hospitalization in prior yr, comorbidity score, days of MV, sepsis LOS, shock LOS, ICU LOS, hospital LOS, disposition destination |
| Marquis 2000 [65] | Prospective; parallel controlled cohort 33 ARDS survivors; 24 critically ill controls | Trail Making Test B Symbol Digit Modalities test Test of Everyday Attention (Elevator Counting with Distraction) | -- | 3 | -- |
| Mikkelsen 2009 [66] | Cross-sectional 79 self-reported ARDS survivors | NCSE (Orientation, Judgment) WMS-III (Digit Span, Letter – Number Sequencing, Logical Memory, Similarities) Hayling Sentence Completion Test Controlled Oral Word Association Test | ≥2 test scores > 1 SD or 1 test score > 1.5 SDs below normative population | 3 | Sex, age, education, employment status, hospital LOS, precipitating factors (pneumonia, surgery, sepsis, trauma, other) |
| Mikkelsen 2012 [67] June 2000 – October 2005 | Prospective; multicenter; cohort 75 ALI survivors | Neuropsychological test battery (45–60 minutes); nil other specifics reported | 1 test score > 2 SDs below normative population | 3 | Sex, age, race, primary lung injury, coexisting conditions (none, DM, HIV/AIDS, cirrhosis, solid tumor, leukemia, lymphoma, immunosuppression), APACHE III, GCS, MAP, vasopressor use, PF ratio, conservative fluid strategy, PAC |
| Mitchell 2016 [68] November 2011 – December 2014 | Prospective; cohort 148 adult surgical, medical and trauma patients enrolled; 88 tested at 3-months and 79 tested at 6-months | RBANS Trail Making Test Part B MMSE | Classified as severely impaired if they scored 1.5 SDs below the mean on ≥3 of the index scores or 2 SDs below the mean on ≥2 of the index scores | 3 | Sex, age, education, admission diagnosis, APACHE II, APACHE III, ICU LOS, hospital LOS, Propofol/benzodiazepine/opioid dose, days of MV, delirium in ICU days |
| Needham 2013 [19] July 2008 – May 2012 | Multicentre; prospective; cohort 174 patients | Controlled oral word association (COWA) Digit span Hayling sentence completion Logical memory I/II Similarities | <1.5 SDs on any of tests | 3 | Sex, age, race, high school education (yes/no), BMI, steroids (yes/no), living independently at home prior to admission (yes/no), employed (yes/no), SF-36, functional performance inventory score, comorbidity score, comorbidities at admission, critical illness characteristics (pneumonia, sepsis, baseline shock, baseline PF ratio, APACHE II, days of MV, hypoglycemia, steroids, insulin, benzodiazepines, NMBs, narcotics, ever coma, ever delirious, ICU LOS, hospital LOS) |
| Pandharipande 2013 [7] March 2007 – May 2010 | Multicentre; prospective 467 adults admitted to a medical or surgical ICU with respiratory failure, cardiogenic shock, or septic shock | RBANS Trail Making Test B | 1.5 and 2 SDs below the population means | 3 | Sex, age, race, ICU type, education, short IQCODE, comorbidity score, APACHE II, SOFA, admission diagnosis, days of MV, days delirious, coma (yes/no), hospital LOS, use of sedatives/analgesia in ICU |
| Pasternak 2008 [69] February 2000 – April 2003 | Posthoc analysis of data from Intraoperative Hypothermia for Aneurysm Surgery Trial 878 patients with SAH; underwent aneurysm surgery | Benton Visual Retention test Controlled Oral Word Association Rey-Osterrieth Complex Figure Test Grooved Pegboard test Trail Making test Glasgow Outcome Score (GOS) | 1 test score > 2 SDs below normative population | 3 | Blood glucose at aneurysm clipping, age, sex, race, BMI, preoperative hx (DM, HTN, smoking, time from SAH to induction), WFNS, Fisher grade, NIHSS, preoperative Rankin score, hydrocephalus on initial CT |
| Pfoh 2015 [70] July 2008 – May 2012 | Cross-sectional secondary analysis of data from two prospective studies of acute respiratory failure patients requiring mechanical ventilation in an ICU | MMSE COWA Logical memory I/II Digit span total score, forward and backward | MMSE conservative cutoff score of <24 | 2 | Sex, age, education, employed, comorbidity score, psychiatric condition, severity illness score, days of MV, ICU LOS, hospital LOS |
| Pierrakos 2017 [71] January 2013 - January 2014 | Prospective; consecutive; cohort 28 patients with sepsis | MMSE IADLs | -- | 2 | Sex, age, APACHE II, IADL, pCO2, MAP, septic shock, days of MV, sedation, relapsing infection (yes/no), delirium (yes/no) |
| Rothenhausler 2001 [72] January 1985 – January 1995 | Prospective; consecutive; cohort 46 ARDS survivors | Short Cognitive Performance test (SKT) | SKT total scores (profound cognitive impairment: 24–27; severe: 19–23, moderate: 14–18, mild: 9–13; subthreshold: 5–8) | 2 | Sex, age, RF for ARDS (trauma, sepsis, pneumonia, other) |
| Sacanella 2011 [73] -- | Prospective; consecutive; Cohort 112 elderly patients electively admitted to MICU | MMSE IQCODE | MMSE < 24 | 2 | Sex, age, APACHE II, SOFA, ICU LOS, cardiac dx, respiratory dx, severe sepsis, CV dx, other medical dx, % MV, % RRT, OMEGA score, Charlson index |
| Sakuramoto 2015 [74] July – December 2009 | Prospective; consecutive; cohort 79 adults admitted to MICU or SICU | MMSE | MMSE < 24 | 2 | Sex, age, comorbidity score, vision deficits, hearing deficits, mBDRS score, APACHE, SOFA, days of MV, ICU LOS, hospital LOS, admission diagnosis |
| Schielke 2005 [75] January 1999 – June 1999 | Prospective; consecutive; cohort 27 patients treated for ischemic stroke requiring MV | MMSE National Institutes of Health Stroke Scale Barthel Index modified Rankin Scale | MMSE < 24 | 2 | -- |
| Semmler 2013 [76] January 2004 – August 2006 | Two center; prospective; non-consecutive; cohort 25 survivors of sepsis; 19 non-septic ICU survivors | Neuro Cognitive Effects (NeuroCogFx) Trail Making tests A and B Auditory Verbal Learning Test Rey-Osterrieth Complex Figure Test | > 1.5 SD from z differences scores | 3 | Age, estimate premorbid verbal ability, APACHE II, SOFA, ICU LOS, duration MV, electrolyte levels (Na and K), PF ratio (max), creatinine (max), HCT (max), MAP < 70 mmHg, ARDS %, surgery (emergent or elective), admission diagnosis, comorbid medical disorders (cardiac, respiratory, live, DM, immunosuppressed, cancer, renal dx, CV dx, GI dx, multiple disorders), drugs (sedatives, analgesics, vasopressor, other drug) |
| Suchyta 2004 [77] | Prospective; cohort 30 ARDS patients | -- | ≥2 test scores that were > 1 SD for mild, >1.5 SDs for moderate or ≥2 SDs for severe cognitive impairment | 3 | Sex, age, education, APACHE II, hospital LOS, PF ratio, RF for ARDS |
| Suchyta 2010 [78] July 2003 – June 2004 | Prospective; non-consecutive; cohort 46 MSICU patients | -- | -- | -- | Duration MV, ICU LOS, hospital LOS, APACHE II at ICU admission, % ARDS, admission diagnosis, co-morbid dx (cardiac, respiratory, liver, DM, immunosuppressed, cancer, renal dx, CV dx, GI dx, multiple disorders); hrs SpO2 < 90%, hrs MAP < 60 mmHg, sedatives (total dose ICU admission to scan) including lorazepam/fentanyl/morphine/midazolam/ propofol/hydromorphone, steroids |
| Sukantarat 2005 [79] April 2000 – March 2003 | Prospective; consecutive; cohort 51 MSICU patients | Hayling Sentence Completion test Modified Six Element test Raven’s Standard Progressive Matrices | Compared to percentiles of population norms | 3 | Sex, age, LOS, duration MV, APACHE II, TISS points |
| Teeters 2011 [80] 2004 – 2008 | Prospective; cohort 387 elderly patients admitted to ICU | Clinical Dementia Rating Scale FAQ Neurologic evaluation Neuropsychiatric testing | Expert consensus | 3 | Sex, age, APACHE III |
| Tembo 2012 [81] -- | Qualitative 12 MSICU patients | Face-to-face interviews | Self-reported | 2 | -- |
| Tobar 2009 [82] September 2008 – April 2009 | Prospective; cohort 8 MICU patients | MMSE MOCA | MMSE < 21 (norm for Chile) | 2 | Sex, age, APACHE II, SOFA, delirium days, duration MV, hospital LOS |
| Torgersen 2011 [83] January 2008 – February 2009 | Prospective; consecutive; cohort (parallel surgical cohort; not requiring ICU admission) 28 SICU patients; 24 surgical patients | CANTAB MMSE DMS (delayed matching to sample) Stocking of Cambridge Paired associate learning test SF-36 | MMSE < 24 Z-score below −2 SD on 2 or below 1.5 SDs on 3 out of 10 results reported by CANTAB | 3 | Sex, age, ICU LOS, duration MV, SAPS II, mac SOFA score, Charlson comorbidity index |
| Vitaz 2003 [84] October 1995 – March 1998 | Prospective; consecutive; cohort 56 patients with moderate TBI | Telephone interview; questions regarding ADLs and mental functioning | Self-report | 1 | Age, median 24-hr GCS, hospital LOS, ICU LOS, duration MV |
| Wolters 2017 [85] January 2011 – June 2013 | Prospective; consecutive; cohort 363 adult patients in mixed MSICU for > 48 hrs | Cognitive Failures Questionnaire (CFQ) | -- | 1 | Sex, age, comorbidity index, APACHE IV, SOFA, ICU LOS, admission type |
| Woon 2012 [86] August 2007 – December 2008 | Prospective; consecutive; cohort 53 patients MSICU | MMSE Mini-Cog WASI (full-scale, verbal, performance) Trail Making tests A and B Hayling Sentence Completion Test WASI-R (digit symbol) WMS-III (logical memory) California Verbal Learning Test-II Rey-Osterrieth Complex Figure Test Finger Tapping test Controlled Oral Word Association test Wide-Range Assessment test-3 (reading) Golden Stroop test (inference trial) | MMSE < 24 MiniCog considered impaired if recalled no words, or recalled 1 or 2 words with an abnormal clock drawing score NP testing: ≥2 or test scores > 1.5 SDs or 1 test score that was > 2 SDs below population norms | 3 | Sex, age, education, ICU LOS, hospital LOS, duration MV, max FiO2, Min PaO2, APACHE II, ICU admission diagnosis |
| Zhao 2017 [87] January 2013 to September 2013 | RCT 332 patients; 165 patients were included in the control group and 167 in the cognitive intervention group | Montreal Cognitive Assessment (MoCA) | < 26 was considered CI | 2 | Sex, age, education, ICU LOS, ICU type, comorbidity index, medications (steroids, analgesia, sedation) |
ARDS: acute respiratory distress syndrome; ALI: acute lung injury; COPD: chronic obstructive pulmonary disease; LT: long-term; MV: mechanical ventilation; LOS: length of stay; ICU: intensive care unit; MSICU: medical-surgical ICU; CCU: coronary care unit; SICU: surgical ICU; CICU: cardiac ICU; FU: follow-up; TBI: traumatic brain injury; GCS: Glasgow coma score; RCT: randomized controlled trial; SAT: spontaneous awakening trial; SBT: spontaneous breathing trial; ICH: intracerebral hemorrhage; SAH: subarachnoid hemorrhage
Reporting of key covariates
Interestingly, but not surprisingly, there is variable reporting of important covariates in studies of ICU survivors after hospital discharge. Again, using the example of long-term cognitive impairment, the most commonly reported covariates were age and sex in follow-up of ICU survivors; level of education was reported in only half of the studies (31/61; 51%). Severity of illness, duration of ICU or hospital stay, use of sedative agents, and incident delirium were also inconsistently reported. In order to inform a comprehensive understanding of outcomes after ICU, more uniform reporting of key covariates is necessary to synthesize the results of different cohorts. Such an understanding is essential for researchers and clinicians to advance research and enhance future care of ICU survivors.
Family and friends of ICU survivors
Physical, cognitive, emotional and social problems are common among ICU survivors. These wide-ranging issues are also seen frequently in family members and friends [26]. While many of these problems are new, unmasked, or exacerbated by acute illness, in-hospital events may also strip away compensatory strategies that had helped patients or their caregivers cope in the past. Social relationships have a two-way influence on health and well-being; social isolation in many disease processes is known to exacerbate conditions and predict mortality [27]. Conversely, social relationships are also known to have a protective impact on health, especially in disease processes such as cancer and depression [28, 29]. Therefore, understanding the emotional and social needs of not only our patients, but also their caregivers, will help improve our understanding of ICU survivorship. Given the key role of family members and friends in the lives of our patients, future research should include further understanding the relationship between survivors and their caregivers, including their respective social networks [30], to determine how acquired co-morbidities may be managed and mitigated.
Conclusions
Many methodological challenges face the researcher and clinician in understanding the long-term consequences of critical illness, such as high mortality rates in long-term follow-up. The current focus should be on ensuring adequate sample sizes, limiting attrition, standardizing outcome measures, and reporting key covariates to better understand the context of described outcomes. These challenges require diligent focus to enhance our collective ability to collect and integrate data, with the hope of creating a better understanding of the morbidity associated with ICU survival and life after hospital discharge.
Key Points.
Methodological consideration needs to be integrated in all stages of study design for long-term follow-up of ICU survivors after hospital discharge.
Heterogeneity in outcome definitions, measurement instruments and reported covariates used in studies of ICU survivors creates a major barrier in synthesizing the existing literature.
High financial burden of personnel as well as the reimbursement of subjects and family members for their time and inconvenience is an important limitation to many investigators and research groups.
Family members and friends are key contributors to understanding the landscape of ICU survivorship, and their knowledge and data should be included in the methodological design and outcomes assessments.
Acknowledgments
• Financial support and sponsorship – none
• Conflicts of interest - Dr. Ely reports grants from NIH, grants from VA, during the conduct of the study; personal fees from Orion Pharmaceuticals, personal fees from Pfizer Pharmaceuticals, personal fees from Köhler, personal fees from Masimo, outside the submitted work.
References
- 1.Gayat E, Cariou A, Deye N, et al. : Determinants of long-term outcome in ICU survivors: results from the FROG-ICU study. Crit Care 2018, 22(1):8.* Large multicenter cohort study of 1570 ICU survivors discharged from one of 21 medical, surgical or mixed ICUs conducted in France and Belgium that identified potentially actionable clinical and biological factors at ICU discharge (age, comorbidity, length of stay and clinical parameters including low systolic blood pressure, temperature, total protein, platelet and white cell count) associated with poor long-term outcome.
- 2.Wunsch H, Guerra C, Barnato AE, et al. : Three-year outcomes for Medicare beneficiaries who survive intensive care. Jama 2010, 303(9):849–856. [DOI] [PubMed] [Google Scholar]
- 3.Hill AD, Fowler RA, Pinto R, et al. : Long-term outcomes and healthcare utilization following critical illness--a population-based study. Crit Care 2016, 20:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andersen FH, Flaatten H, Klepstad P, Romild U, Kvale R: Long-term survival and quality of life after intensive care for patients 80 years of age or older. Ann Intensive Care 2015, 5(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desmond DP, Maddux JF, Johnson TH, et al. : Obtaining follow-up interviews for treatment evaluation. J Subst Abuse Treat 1995, 12(2) 95–102. [DOI] [PubMed] [Google Scholar]
- 6.Herridge MS, Chu LM, Matte A, et al. : The RECOVER Program: Disability Risk Groups and 1-Year Outcome after 7 or More Days of Mechanical Ventilation. Am J Respir Crit Care Med 2016, 194(7):831–844. [DOI] [PubMed] [Google Scholar]
- 7.Pandharipande PP, Girard TD, Jackson JC, et al. : Long-term cognitive impairment after critical illness. 2013, 1(14):1306–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilcox ME, Lim AS, McAndrews MP, et al. : A study protocol for an observational cohort investigating COGnitive outcomes and WELLness in survivors of critical illness: the COGWELL study. BMJ Open 2017, 7(7):e015600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teague S, Youssef GJ, Macdonald JA, et al. : Retention strategies in longitudinal cohort studies: a systematic review and meta-analysis. BMC Med Res Methodol 2018, 18(1):151.* Review of 95 participant retention strategies illustrating that those strategies aimed at reducing participant burden (e.g., flexibility in data collection methods) may be more than employing multiple strategies in maximising cohort retention.
- 10.Robinson KA, Dinglas VD, Sukrithan V, et al. : Updated systematic review identifies substantial number of retention strategies: using more strategies retains more study participants. J Clin Epidemiol 2015, 68(12):1481–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davies H, McKenzie N, Williams TA, et al. : Challenges during long-term follow-up of ICU patients with and without chronic disease. Aust Crit Care 2016, 29(1):27–34. [DOI] [PubMed] [Google Scholar]
- 12.Waters B, Matte A, Chu L, et al. : The Role for Off-Site/Home Visits in the Post ICU Care Continuum. Ann Am Thorac Soc 2019, S(D14):A5858. [Google Scholar]
- 13.Hansen LO, Young RS, Hinami K, et al. : Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med 2011, 155(8):520–528. [DOI] [PubMed] [Google Scholar]
- 14.Naylor MD, Brooten D, Campbell R, et al. : Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA 1999, 281(7):613–620. [DOI] [PubMed] [Google Scholar]
- 15.Stewart S, Horowitz JD: Home-based intervention in congestive heart failure: long-term implications on readmission and survival. Circulation 2002, 105(24):2861–2866. [DOI] [PubMed] [Google Scholar]
- 16.Jackson C, Kasper EW, Williams C, DuBard CA: Incremental Benefit of a Home Visit Following Discharge for Patients with Multiple Chronic Conditions Receiving Transitional Care. Popul Health Manag 2016, 19(3):163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Needham DM, Davidson J, Cohen H, et al. : Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med 2012, 40(2):502–509. [DOI] [PubMed] [Google Scholar]
- 18.Needham DM, Dennison CR, Dowdy DW, et al. : Study protocol: The Improving Care of Acute Lung Injury Patients (ICAP) study. Crit Care 2006, 10(1):R9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Needham DM, Dinglas VD, Bienvenu OJ, et al. : One year outcomes in patients with acute lung injury randomised to initial trophic or full enteral feeding: prospective follow-up of EDEN randomised trial. BMJ 2013, 346:f1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Needham DM, Dinglas VD, Morris PE, et al. : Physical and cognitive performance of patients with acute lung injury 1 year after initial trophic versus full enteral feeding. EDEN trial follow-up. Am J Respir Crit Care Med 2013, 188(5):567–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Needham DM, Sepulveda KA, Dinglas VD, et al. : Core Outcome Measures for Clinical Research in Acute Respiratory Failure Survivors. An International Modified Delphi Consensus Study. Am J Respir Crit Care Med 2017, 196(9):1122–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jackson JC, Girard TD, Gordon SM, et al. : Long-term cognitive and psychological outcomes in the awakening and breathing controlled trial. Am J Respir Crit Care Med 2010, 182(2):183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jackson JC, Pandharipande PP, Girard TD, et al. : Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med 2014, 2(5):369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heins SE, Wozniak AW, Colantuoni E, et al. : Factors associated with missed assessments in a 2-year longitudinal study of acute respiratory distress syndrome survivors. BMC Med Res Methodol 2018, 18(1):55.** Large mutlicenter study of ARDS survivors evaluating relevant sociodemographic, physical status, and mental health variables as risk factors for missed assessments of long-term follow-up. Dependencies in physical functioning (e.g. ADLs, IADLs) prior to hospitalization and at hospital discharge were associated with higher odds of missed assessments.
- 25.Turnbull AE, Sepulveda KA, Dinglas VD, et al. : Core Domains for Clinical Research in Acute Respiratory Failure Survivors: An International Modified Delphi Consensus Study. Crit Care Med 2017, 45(6):1001–1010.* First consensus-based list of core domains to be considered for assessment of all clinical research studies evaluating ARDS survivors in long-term follow-up.
- 26.Cameron JI, Chu LM, Matte A, et al. : One-Year Outcomes in Caregivers of Critically Ill Patients. 2016, 1(19):1831–1841. [DOI] [PubMed] [Google Scholar]
- 27.Boothroyd RI, Fisher EB: Peers for progress: promoting peer support for health around the world. Fam Pract 2010, 27 Suppl 1:i62–68. [DOI] [PubMed] [Google Scholar]
- 28.Stansfeld SA, Rael EG, Head J, Shipley M, Marmot M: Social support and psychiatric sickness absence: a prospective study of British civil servants. Psychol Med 1997, 27(1):35–48. [DOI] [PubMed] [Google Scholar]
- 29.Cameron LD, Booth RJ, Schlatter M, et al. : Changes in emotion regulation and psychological adjustment following use of a group psychosocial support program for women recently diagnosed with breast cancer. Psychooncology 2007, 16(3):171–180. [DOI] [PubMed] [Google Scholar]
- 30.McPeake J, Hirshberg EL, Christie LM, et al. : Models of Peer Support to Remediate Post-Intensive Care Syndrome: A Report Developed by the Society of Critical Care Medicine Thrive International Peer Support Collaborative. Crit Care Med 2019, 47(1):e21–e27.** Innovative initiative to categorize distinct models of peer support among participants of the Society of Critical Care Medicine Thrive Peer Support Collaborative; community based, psychologist-led outpatient, models-based within ICU follow-up clinics, online, groups based within ICU, and peer mentor models. Common barriers to implementation were recruitment to groups, training of personnel, funding, risk management, and measurement of model success.
- 31.Ambrosino N, Bruletti G, Scala V, et al. : Cognitive and perceived health status in patient with chronic obstructive pulmonary disease surviving acute on chronic respiratory failure: a controlled study. Intensive Care Medicine 2002, 28(2):170–177. [DOI] [PubMed] [Google Scholar]
- 32.Baumbach P, Meissner W, Guenther A, et al. : Perceived cognitive impairments after critical illness: a longitudinal study in survivors and family member controls. Acta Anaesthesiol Scand 2016, 60(8):1121–1130. [DOI] [PubMed] [Google Scholar]
- 33.Bruck E, Schandl A, Bottai M, Sackey P: The impact of sepsis, delirium, and psychological distress on self-rated cognitive function in ICU survivors-a prospective cohort study. J Intensive Care 2018, 6:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Calsavara AJC, Costa PA, Nobre V, Teixeira AL: Factors Associated With Short and Long Term Cognitive Changes in Patients With Sepsis. Sci 2018, 8(1):4509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Christie JD, Biester RCP, Taichman DB, et al. : Formation and validation of a telephone battery to assess cognitive function in acute respiratory distress syndrome survivors. Journal of Critical Care 2006, 21(2):125–132. [DOI] [PubMed] [Google Scholar]
- 36.Chung CR, Yoo HJ, Park J, Ryu S: Cognitive Impairment and Psychological Distress at Discharge from Intensive Care Unit. Psychiatry Investig 2017, 14(3):376–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davydow DS, Hough CL, Levine DA, et al. : Functional Disability, Cognitive Impairment, and Depression Following Hospitalization for Pneumonia. The American journal of medicine 2013, 126(7):615–624.e615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de Azevedo JR, Montenegro WS, Rodrigues DP, et al. : Long-term cognitive outcomes among unselected ventilated and non-ventilated ICU patients. J Intensive Care 2017, 5:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Oliveira Thais ME, Cavallazzi G, et al. : Limited predictive power of hospitalization variables for long-term cognitive prognosis in adult patients with severe traumatic brain injury. J 2014, 8(1):125–139. [DOI] [PubMed] [Google Scholar]
- 40.de Rooij SEJA Govers AC, Korevaar JC, et al. : Cognitive, functional, and quality-of-life outcomes of patients aged 80 and older who survived at least 1 year after planned or unplanned surgery or medical intensive care treatment. Journal of the American Geriatrics Society 2008, 56(5):816–822. [DOI] [PubMed] [Google Scholar]
- 41.Duggan MC, Wang L, Wilson JE, et al. : The relationship between executive dysfunction, depression, and mental health-related quality of life in survivors of critical illness: Results from the BRAIN-ICU investigation. Journal of Critical Care 2017, 37:72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duning T, van den Heuvel I, Dickmann A, et al. : Hypoglycemia aggravates critical illness-induced neurocognitive dysfunction. Diabetes Care 2010, 33(3):639–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ehlenbach WJ, Hough CL, Crane PK, et al. : Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA 2010, 303(8):763–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Girard TD, Jackson JC, Pandharipande PP, et al. : Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Critical Care Medicine 2010, 38(7):1513–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Girard TD, Thompson JL, Pandharipande PP, et al. : Clinical phenotypes of delirium during critical illness and severity of subsequent long-term cognitive impairment: a prospective cohort study. Lancet Respir Med 2018, 6(3):213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Godbolt A, Nygren-DeBoussard C, Stenberg M, et al. : Cognitive recovery in the first 3 months after severe traumatic brain injury: preliminary data from “PROBRAIN” study [abstract]. Brain Injury 2012, 26(4-5):639. [Google Scholar]
- 47.Guillamondegui OD, Richards JE, Ely EW, et al. : Does hypoxia affect intensive care unit delirium or long-term cognitive impairment after multiple trauma without intracranial hemorrhage?. Journal of Trauma-Injury Infection & Critical Care 2011, 70(4):910–915. [DOI] [PubMed] [Google Scholar]
- 48.Hope AA, Morrison RS, Du Q, et al. : Risk factors for long-term brain dysfunction after chronic critical illness. Ann Am Thorac Soc 2013, 10(4):315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hopkins RO, Weaver LK, Pope D, et al. : Neuropsychological sequelae and impaired health status in survivors of severe acute respiratory distress syndrome. American Journal of Respiratory & Critical Care Medicine 1999, 160(1):50–56. [DOI] [PubMed] [Google Scholar]
- 50.Hopkins RO, Weaver LK, Chan KJ, Orme JF, Jr.: Quality of life, emotional, and cognitive function following acute respiratory distress syndrome. Journal of the International Neuropsychological Society 2004, 10(7):1005–1017. [DOI] [PubMed] [Google Scholar]
- 51.Hopkins RO, Weaver LK, Collingridge D, et al. : Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. American Journal of Respiratory & Critical Care Medicine 2005, 171(4):340–347. [DOI] [PubMed] [Google Scholar]
- 52.Hopkins RO, Jackson JC, Wallace C: Neurocognitive Impairments in ICU Patients with Prolonged Mechanical Ventilation [abstract]. J Int Neuropsychol Soc 2005, 11:A60. [Google Scholar]
- 53.Hopkins RO, Key CW, Suchyta MR, et al. : Risk factors for depression and anxiety in survivors of acute respiratory distress syndrome. General Hospital Psychiatry 2010, 32(2):147–155. [DOI] [PubMed] [Google Scholar]
- 54.Hughes CG, Patel MB, Jackson JC, et al. : Surgery and anesthesia exposure is not a risk factor for cognitive impairment after major noncardiac surgery and critical illness. Annals of Surgery 2017, 265(6):1126–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hughes CG, Patel MB, Brummel NE, et al. : Relationships between markers of neurologic and endothelial injury during critical illness and long-term cognitive impairment and disability. Intensive Care Med 2018, 44(3):345–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Iwashyna TJ, Ely EW, Smith DM, Langa KM: Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 2010, 304(16):1787–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jackson JC, Hart RP, Gordon SM, Shintani A, et al. : Six-month neuropsychological outcome of medical intensive care unit patients. Critical Care Medicine 2003, 31(4):1226–1234. [DOI] [PubMed] [Google Scholar]
- 58.Jackson JC, Obremskey W, Bauer R, et al. : Long-term cognitive, emotional, and functional outcomes in trauma intensive care unit survivors without intracranial hemorrhage. Journal of Trauma-Injury Infection & Critical Care 2007, 62(1):80–88. [DOI] [PubMed] [Google Scholar]
- 59.Jackson JC, Archer KR, Bauer R, Abraham CM, et al. : A prospective investigation of long-term cognitive impairment and psychological distress in moderately versus severely injured trauma intensive care unit survivors without intracranial hemorrhage. Journal of Trauma-Injury Infection & Critical Care 2011, 71(4):860–866. [DOI] [PubMed] [Google Scholar]
- 60.Juan E, De Lucia M, Beaud V, et al. : How Do You Feel? Subjective Perception of Recovery as a Reliable Surrogate of Cognitive and Functional Outcome in Cardiac Arrest Survivors. Crit Care Med 2018, 46(4):e286–e293. [DOI] [PubMed] [Google Scholar]
- 61.Jones C, Griffiths RD, Slater T, et al. : Significant cognitive dysfunction in non-delirious patients identified during and persisting following critical illness. Intensive Care Medicine 2006, 32(6):923–926. [DOI] [PubMed] [Google Scholar]
- 62.Larson MJ, Weaver LK, Hopkins RO: Cognitive sequelae in acute respiratory distress syndrome patients with and without recall of the intensive care unit. Journal of the International Neuropsychological Society 2007, 13(4):595–605. [DOI] [PubMed] [Google Scholar]
- 63.Lippert-Gruner M, Kuchta J, et al. : Neurobehavioural deficits after severe traumatic brain injury (TBI). Brain Injury 2006, 20(6):569–574. [DOI] [PubMed] [Google Scholar]
- 64.Maley JH, Brewster I, Mayoral I, et al. : Resilience in survivors of critical illness in the context of the survivors’ experience and recovery. Ann Am Thorac Soc 2016, 13(8):1351–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marquis KA, Curtis JR, Caldwell ES, et al. : Neuropsychological Sequelae in Survivors of ARDS Compared with Critically Ill Control Patients. American Journal of Respiratory and Critical Care Medicine 2000, 161:A383. [Google Scholar]
- 66.Mikkelsen ME, Shull WH, Biester RC, et al. : Cognitive, mood and quality of life impairments in a select population of ARDS survivors. Respirology 2009, 14(1):76–82. [DOI] [PubMed] [Google Scholar]
- 67.Mikkelsen ME, Christie JD, Lanken PN, et al. : The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury. American Journal of Respiratory & Critical Care Medicine 2012, 185(12):1307–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mitchell M, Aitken L, Shum D, et al. : Long-term cognitive impairment and delirium in intensive care (logic): A prospective cohort study. Anaesthesia and Intensive Care 2016, 44 (2):311. [DOI] [PubMed] [Google Scholar]
- 69.Pasternak JJ, McGregor DG, Schroeder DR, et al. : Hyperglycemia in patients undergoing cerebral aneurysm surgery: its association with long-term gross neurologic and neuropsychological function. Mayo Clin Proc 2008, 83(4):406–417. [DOI] [PubMed] [Google Scholar]
- 70.Pfoh ER, Chan KS, Dinglas VD, et al. : Cognitive screening among acute respiratory failure survivors: a cross-sectional evaluation of the Mini-Mental State Examination. Crit Care 2015, 19:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pierrakos C, Attou R, Decorte L, et al. : Cerebral perfusion alterations and cognitive decline in critically ill sepsis survivors. Acta Clin Belg 2017, 72(1):39–44. [DOI] [PubMed] [Google Scholar]
- 72.Rothenhausler HB, Ehrentraut S, Stoll C, et al. : The relationship between cognitive performance and employment and health status in long-term survivors of the acute respiratory distress syndrome: results of an exploratory study. General Hospital Psychiatry 2001, 23(2):90–96. [DOI] [PubMed] [Google Scholar]
- 73.Sacanella E, Perez-Castejon JM, Nicolas JM, et al. : Functional status and quality of life 12 months after discharge from a medical ICU in healthy elderly patients: a prospective observational study. Critical Care (London, England) 2011, 15(2):R105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sakuramoto H, Subrina J, Unoki T, et al. : Severity of delirium in the ICU is associated with short term cognitive impairment. A prospective cohort study. Intensive Crit Care Nurs 2015, 31(4):250–257. [DOI] [PubMed] [Google Scholar]
- 75.Schielke E, Busch MA, Hildenhagen T, et al. : Functional, cognitive and emotional long-term outcome of patients with ischemic stroke requiring mechanical ventilation. J Neurol 2005, 252(6):648–654. [DOI] [PubMed] [Google Scholar]
- 76.Semmler A, Widmann CN, Okulla T, et al. : Persistent cognitive impairment, hippocampal atrophy and EEG changes in sepsis survivors. Journal of Neurology, Neurosurgery & Psychiatry 2013, 84(1):62–69. [DOI] [PubMed] [Google Scholar]
- 77.Suchyta MR, Hopkins RO, White J, Jephson A: The incidence of cognitive dysfunction after ARDS [abstract]. American Journal of Respiratory & Critical Care Medicine 2004, 169(7):A18. [Google Scholar]
- 78.Suchyta MR, Jephson A, Hopkins RO: Neurologic changes during critical illness: brain imaging findings and neurobehavioral outcomes. Brain Imaging & Behavior 2010, 4(1):22–34. [DOI] [PubMed] [Google Scholar]
- 79.Sukantarat KT, Burgess PW, Williamson RCN, Brett SJ: Prolonged cognitive dysfunction in survivors of critical illness. Anaesthesia 2005, 60(9):847–853. [DOI] [PubMed] [Google Scholar]
- 80.Teeters D, Moua T, Biehl M, et al. : The Incidence of Preexisting Cognitive Impairment Before ICU Admission: A Population Based Study [abstract]. Chest 2011, 140:A349. [Google Scholar]
- 81.Tembo AC, Higgins I, Parker V: Cognitive Impairment in Critical Illness Survivors - A Phenomenological Inquiry [abstract]. Neuroepidemiology 2012, 39:A159. [Google Scholar]
- 82.Tobar E, Galleguillos T, Delgado C, et al. : Hypoactive delirium in septic mechanically ventilated patient. Preliminary data of cognitive and psychiatric follow up [abstract]. Critical Care Medicine 2009, 37(12):A781. [Google Scholar]
- 83.Torgersen J, Hole JF, Kvale R, et al. : Cognitive impairments after critical illness. Acta Anaesthesiologica Scandinavica 2011, 55(9):1044–1051. [DOI] [PubMed] [Google Scholar]
- 84.Vitaz TW, Jenks J, Raque GH, Shields CB: Outcome following moderate traumatic brain injury. Surgical Neurology 2003, 60(4):285–291; discussion 291. [DOI] [PubMed] [Google Scholar]
- 85.Wolters AE, Peelen LM, Veldhuijzen DS, et al. : Long-Term Self-Reported Cognitive Problems After Delirium in the Intensive Care Unit and the Effect of Systemic Inflammation. J Am Geriatr Soc 2017, 65(4):786–791. [DOI] [PubMed] [Google Scholar]
- 86.Woon FL, Dunn CB, Hopkins RO: Predicting cognitive sequelae in survivors of critical illness with cognitive screening tests. American Journal of Respiratory & Critical Care Medicine 2012, 186(4):333–340. [DOI] [PubMed] [Google Scholar]
- 87.Zhao J, Yao L, Wang C, et al. : The effects of cognitive intervention on cognitive impairments after intensive care unit admission. Neuropsychol 2017, 27(3):301–317. [DOI] [PubMed] [Google Scholar]