Dear Editor,
Since December, 2019, an outbreak of a novel coronavirus pneumonia (COVID-19) occurred in Wuhan (Hubei, China).1 Recent papers in this journal also described the clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by COVID-19.2 During nearly two months of fighting against the epidemic, health workers were under great physiological and psychological pressure in China.3 For example, due to wearing protective clothing, many health workers avoided drinking water and wore adult diapers for a long time, so that some of them fainted under hypoxia and hypoglycaemia.4 Previous studies showed that stress could increase the risk of infection5 as well as induce ventricular arrhythmia, and thus sudden cardiac death.6 As a result, the medical staff in the front-line fighting against the novel coronary pneumonia were facing high risks of virus infection and sudden death. In 2003, more than 1,000 health workers were attacked by severe acute respiratory syndrome (SARS) and 124 deaths were observed in China. As of Mar 16, 2020, 24 health workers had died during the outbreak of COVID-19 infection in China.
We retrieved information on 24 cases of deceased health workers based on official reports from governmental institutes, as well as reports from news sites. Data available to the public included gender, age, cause of death, location city, date of disease onset, date of admission, date of death, and hospital levels they worked. We grouped cases into three groups based on the cause of death, which included COVID-19 infection, sudden death, and traffic accident groups. Mann-Whitney U test was applied to compare continuous variables because the data was non-normal distribution, and Fisher exact test was used for categorical variables because the data number was limited.
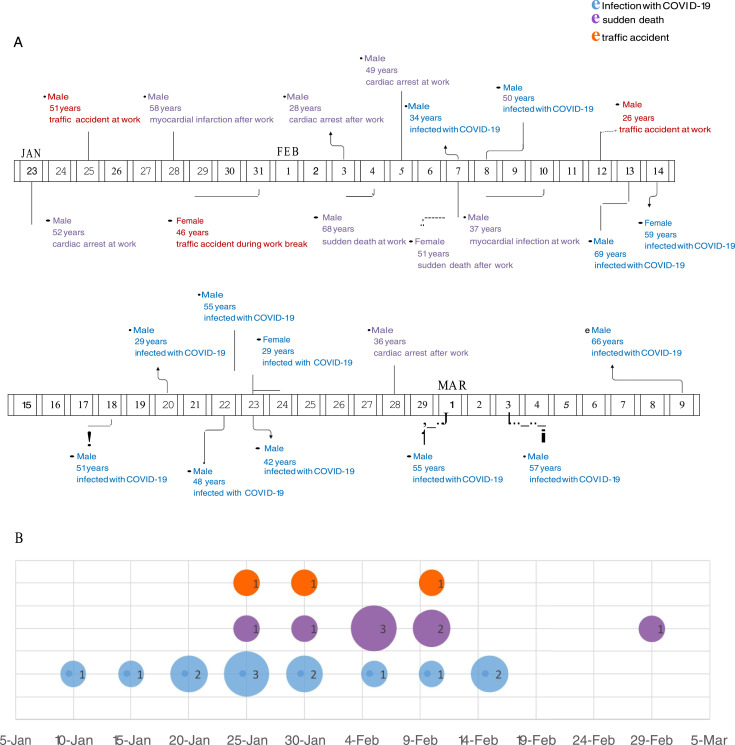
Thirteen (54.2%) cases died of COVID-19 infection, 8 (33.3%) suffered from sudden death including cardiac arrest, myocardial infarction, and other non-confirmed diseases, and 3 (12.5%) died in traffic accidents during work time or after work (Table 1 ). The basic information of all the deceased health workers was listed in Fig 1 A. The median age was 50.5 years (IQR: 36.25-56.5), ranging from 26 to 69 years. A total of 72,314 patient record showed that 81% of dead cases were aged 60 years or older and 12.7% were aged 50 to 59 years.7 The median age of deceased medical staff was obviously younger than that of the general population, because medical staff were mostly in employment who were younger than 60 years. Up to 83.3% of deceased medical workers were males and no sex differences existed among COVID-19 infection group, sudden death group, and traffic accident group. In the group of infection, 11 deceased cases (84.6%) were males. Zhang reported that the overall case fatality rate of male patients (rough estimate: 2.8%) was significantly higher than that of female patients (rough estimate: 1.7%).7 In the group of sudden death, 7 cases (87.5%) were males. Previous study revealed that, at 45 years of age, lifetime risks for sudden cardiac death were 10.9% for men and 2.8% for women,8 which was similar to the results in our study. The above data suggested that males had a higher risk of death due to COVID-19 infection and sudden death than females.
Table 1.
Demographics of deceased medical workers in China by Mar 16, 2020
| Characteristic | Total(n=24) | COVID-19 infection(n=13, 54.2%) | Sudden death(n=8, 33.3%) | Traffic accident(n=3, 12.5%) | Z/χ2(P /Fisher P) |
|---|---|---|---|---|---|
| Age, Median (IQR) -yrs | 50.5(36.25-56.5) | 51(38.0-58.0) | 50(36.25-56.5) | / | -0.399(0.690) |
| Male, No. (%) | 20(83.3) | 11(84.6) | 7(87.5) | 2(66.7) | 1.180(0.579) |
| Hubei resident, No. (%) | 11(45.8) | 11(84.6) | 0(0.0) | 0(0.0) | 17.293(0.000*) |
| Wuhan resident, No. (%) | 9(37.5) | 9(69.2) | 0(0.0) | 0(0.0) | 11.684(0.001*) |
| Community hospital, No. (%) | 11(45.8) | 3(23.1) | 5(62.5) | 3(100.0) | 6.644(0.022*) |
| Onset to admission, Median (IQR)-days | / | 2(1-5.5) (n=9) | / | / | / |
| Admission to death, Median (IQR)-days | / | 26(21.25-36.5) (n=12) | / | / | / |
| Onset to death, Median (IQR)-days | / | 30.5(25-35.25) (n=10) | / | / | / |
Fig. 1.
A) Death date, demographics, and death cause of medical workers in China by Mar 16, 2020. Infection with COVID-19 marked with blue, sudden death marked with purple, and traffic death marked with red. B) The new number of deceased medical workers with confirmed COVID-19 infection at admission per 5 days (marked with blue), new number of medical workers with sudden death per 5 days (marked with purple), and new number of medical workers with traffic accident per 5 days (marked with red).
Transmission of COVID-19 occurred in the hospital setting. In the group of COVID-19 infection, there were more medical staff working in Hubei province (84.6%) and Wuhan city (69.2%), which was consistent with the result of 63% of infected medical staffs in Wuhan in a recent report.9 Due to the severity of COVID-19 infection in Hubei, more nosocomial infections and deaths occurred in Hubei than other provinces. As of February 11, 2020, 3,019 cases have been observed among health workers, of whom there have been 1,716 confirmed cases. Among health workers infected, 14.8% of confirmed cases were classified as severe or critical, and 5 deaths were observed.9 Among all the deceased medical staff with COVID-19 infection, the median of period from disease onset to hospital admission was 2 days (IQR: 1-5.5), and the median of period from admission to death was 26 days (IQR: 21.25-36.5) (Table 1). Based on the admission date of staff with COVID-19 infection and the death date of staff with sudden death, the new number of deceased health workers per 5 days was listed in Fig 2. Attacked infection mostly occurred on January and sudden death mainly happened from Jan 23 to Feb 10, 2020.
Furthermore, there were more health workers who worked in community hospitals suffering from sudden death or traffic accident. Sudden death due to huge work and lack of rest happened since Jan 23, 2020, when comprehensive measures for epidemic prevention and control were taken nationwide. Large-scale work including temperature measurements, door to door visit, medicine delivery, patients transfer, disinfection, etc., had been completed by community or village medical workers. Some village doctors even lived and ate in the village clinics. On Feb 22,2020, the Chinese government took a series of measures to protect and support health workers in the front line, such as improving the quality of life, strengthening personal protection, arranging rest in turns, and relieving mental stress. Afterwards, the incidence of accidental death decreased significantly.
In summary, there were more males in the fatality of health workers, more sudden death happening to community health workers, and more death due to COVID-19 infection occurring in Hubei health workers during the outbreak of COVID-19 in China.
Declaration of Competing Interest
None
Acknowledgments
This research was funded by grants from Clinical research center project of Shanghai Mental Health Center (CRC2017ZD02), Western medical guidance project of Shanghai Science and Technology Commission (17411970100), and National Natural Science Foundation of China (81301139).
References
- 1.Chen Q., Liang M., Li Y. Mental health care for medical staff in China during the COVID-19 outbreak. The lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.YH X., JH D., WM A. Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2. The Journal of infection. 2020 doi: 10.1016/j.jinf.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu P., Fang Y., Guan Z. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeng Y., Zhen Y. Chinese medical staff request international medical assistance in fighting against COVID-19. The Lancet Global health. 2020 doi: 10.1016/S2214-109X(20)30065-6. [DOI] [PubMed] [Google Scholar]
- 5.Calefi A.S., de Queiroz Nunes C.A., da Silva Fonseca J.G., Quinteiro-Filho W.M., Ferreira A.J.P., Palermo-Neto J. Heat stress reduces Eimeria spp. infection and interferes with C. perfringens infection via activation of the hypothalamic-pituitary-adrenal axis. Research in veterinary science. 2019;123:273–280. doi: 10.1016/j.rvsc.2019.01.026. [DOI] [PubMed] [Google Scholar]
- 6.Scorza F.A., Albuquerque R., Arida R.M. What are the similarities between stress, sudden cardiac death in Gallus gallus and sudden unexpected death in people with epilepsy. Arquivos de neuro-psiquiatria. 2010;68(5):788–790. doi: 10.1590/s0004-282x2010000500022. [DOI] [PubMed] [Google Scholar]
- 7.Novel Coronavirus Pneumonia Emergency Response Epidemiology T. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China] Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145–151. [Google Scholar]
- 8.E M., A U.-E., K R. Sudden cardiac arrest during sports activity in middle age. Circulation. 2015;131(16):1384–1391. doi: 10.1161/CIRCULATIONAHA.114.011988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Z W., JM M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. Jama. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]