Abstract
The COVID-19 epidemic, which is caused by the novel coronavirus SARS-CoV-2, has spread rapidly to become a world-wide pandemic. Chest radiography and chest CT are frequently used to support the diagnosis of COVID-19 infection. However, multiple cases of COVID-19 transmission in radiology department have been reported. Here we summarize the lessons we learned and provide suggestions to improve the infection control and prevention practices of healthcare workers in departments of radiology.
Key Words: COVID-19, SARS-CoV-2, Infection control, Radiology department
Abbreviations: COVID-19, Coronavirus disease 2019; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2; APP, Application software; CT, Computed tomography; PACS, Picture Archiving and Communication Systems
BACKGROUND
Since the initial discovery in December 2019, the novel coronavirus SARS-CoV-2, which is causing the new coronavirus disease COVID-19, has spread across the world. Confirmed cases have surpassed 140,000 and are still climbing (1). Among these cases, are 1716 Chinese health care providers and sadly six of them have lost their lives, as of February 11, 2020 (2,3).
Since imaging is heavily relied upon in the diagnosis of patients suspected of COVID-19 infection, radiology personnel are at high risk of infection with COVID-19. Thus, it is of critical importance to scrutinize the current infection control and prevention practices of radiology departments to reduce cross-infection and protect medical professionals. Here, we analyze cases of health care-associated COVID-19 transmission to radiology personnel, summarize the lessons learned, and provide suggestions of improvement.
LACK OF KNOWLEDGE OF INFECTION CONTROL PRACTICES
One of the most common problems is lack of understanding among healthcare personnel about how the virus is transmitted. According to the reports of the health care-associated COVID-19 transmission in China, most of cases are due to the medical staff's lack of knowledge about the prevention and control of infectious diseases. A survey found that only 40% of radiology department professional staff have sufficient knowledge of infection control practice (4). Therefore, in addition to regular training, the radiology department should quickly reinforce the training of infection control practices during major infectious disease outbreaks like COVID-19.
LOOPHOLES IN THE PATIENT TRIAGE
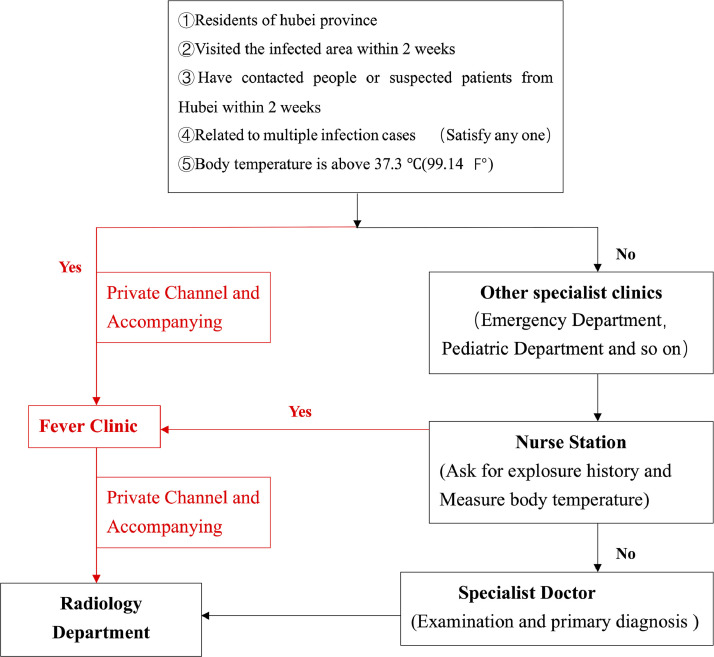
According to the diagnosis flow diagram of one hospital (Fig 1 ), outpatient physicians and nurses separate patients into those confirmed or suspected of COVID-19 infection from other patients based on the patient's temperature, symptoms, and exposure history (5). Those patients suspected of COVID-19 infection go to the fever clinic and are accompanied by a nurse to the radiology department for a chest CT examination. Those patients not suspected of COVID-19 infection are triaged to other departments. In terms of classification, epidemiological factors and fever are the most important criteria. Patients with fever only account for 43.8% of the confirmed cases in the early stage, and about 1.2%–6% of the asymptomatic patients were found to be able to spread the disease (6,7). This inconsistency creates a serious safety risk. Indeed, many reported hospital-acquired COVID-19 infections are related to either the misclassification of patients or asymptomatic patients with no known exposure history (8).
Figure 1.
Patient diagnosis and treatment flowchart. Red arrows indicate the dedicated passage. All patients are triaged at the triage desk near the hospital entrance. Patients who meet at least one of the epidemiological criteria or have a fever go through a dedicated passage to the fever clinic. Doctor collects detailed medical history and takes blood and throat swap samples. Patients then go through the dedicated passage to the radiology department for examination. Patients who are assigned to other departments have their temperature examined and report their exposure history again at the nurse station. Suspected patients identified at nurse station go through the dedicated passage to the fever clinic. (Color version of figure is available online.)
Thus, the classification of patients is critically important. Fever should not be overemphasized and the exposure history should focus on disease clusters (7). Patient classification is better when three categories are used: (1) highly suspected and confirmed cases (category A), (2) suspected cases (category B), and (3) confirmed negative cases (category C). The medical staff who come into contact with category B patients should adopt at least the WHO grade I protective criterion. This method can greatly reduce the risk of transmission of COVID-19.
RADIOLOGY DEPARTMENT LAYOUT AND ISOLATION STRATEGY
In the absence of specific drugs and vaccines, protection measures in radiology departments are focused primarily on controlling transmission routes such as droplet, contact surface, and aerosol transmissions. To handle patients of different categories, it is suggested that departments be divided into contaminated areas, suspected contaminated areas, transition areas, and clean areas to accommodate the three categories of patients. The contaminated area should be well ventilated, preferably with ventilation equipment. After the completion of the examination, the air and contact surface should be thoroughly sterilized. The next patient should be examined after more than 30 minutes, and the duration of the examination should be minimized as much as possible. Health workers in contaminated areas and suspected contaminated areas must be protected by at least WHO grade I and II protection measures, respectively.
In the reported cases of hospital-acquired infections, one hospital failed to isolate suspected patients from ordinary patients, leading to five radiology staff infected. Another hospital simply copied the previous isolation scheme and did not design a separate area for patients suspected of COVID-19 infection, resulting in unconfirmed COVID-19 patients in the examination room with only simple isolation. As a result, several radiology medical staff became infected (9).
The total number of patients admitted to our department from January 23 to March 12, 2020 was 8755. Among these, 1212 were in the highly suspected (category A), accounting for 13.8% of the total number, and the final confirmed cases were 15. Category B patients (5594) accounted for 63.9% of the total number, and 2 patients were finally confirmed. Category C patients (1949) comprised 22.2% of the total number of patients. The two confirmed category B patients had no clear exposure history and showed only mild respiratory symptoms. Fortunately, the medical personnel in the examination room of the suspected contamination area were well protected and no infection occurred.
POSTEXPOSURE MEASUREMENTS
Medical personnel likely to come into close physical contact with infected or suspected infected patients should strictly follow the standardized procedures to enter and leave contaminated and suspected contaminated areas. Once exposed, they must report the incident and are isolated immediately (Fig 2 ). In the Hubei province of China, several cases were not handled properly after exposure, resulting in the unnecessary spread of COVID-19 infection in these hospitals (10).
Figure 2.
The postexposure procedure of medical staff. Exposed medical staff report the incidence immediately and conduct isolation for 21 days. They are allowed to return to work only after cleaned of the possibility of infection. (exposed medical staff).
INCONSISTENCY BETWEEN RADIOLOGICAL EXAMINATION AND NUCLEIC ACID DETECTION
In the early stage of the outbreak, unenhanced high-resolution CT (HRCT) played an important role in screening patients suspected of COVID-19 infection. According to reports, the sensitivity of HRCT for COVID-19 infection was 73.6%, with the results available within minutes (11).
In contrast, it takes two days to obtain the results of the Reverse Transcription-Polymerase Chain Reaction test, which has a low sensitivity, and often must be repeated multiple tests to confirm one case. What is more problematic is that the nucleic acid detection reagent is often not immediately available. During the outbreak in Wuhan, physicians felt that CT should be used instead of nucleic acid detection and those patients with positive examinations must be properly isolated, otherwise many suspected patients could not be diagnosed in a timely manner, leading to further spread of the disease (12).
Patients with only mild disease are still at risk for poor outcomes. Thirteen percent of those who died were healthy people with no underlying disease (6). Mobile CT is recommended in isolation areas, intensive care units and emergency departments for the preliminary diagnosis of patients suspected of COVID-19 infection. However, not all patients can be diagnosed by HRCT. Among the 17 nucleic acid positive patients in our hospital, 2 showed negative HRCT results. Thus, patients with positive nucleic acid tests must be isolated regardless of whether the HRCT result is negative or positive.
PAPERLESS SYSTEMS REDUCE EXPOSURE RISK
Paperless systems minimize the risk of document-mediated transmission. Electronic examination application forms, informed consent for CT examination of patients, and imaging data can be viewed throughout the hospital without contact with physical documents. Radiologists can perform remote diagnosis and patients can use mobile APPs or patient portals to check their results. This paperless system contributes significantly to the lack of virus transmission within our institution.
CONCLUSIONS
The incidence of COVID-19 infection of radiology personnel is due in large part to a poor understanding of the newly emerged virus. The disease can better handled and the radiology staff can be better protected by improving the training, department design, patient triage, postexposure patient handling and the implement of paperless systems.
Acknowledgments
This article was countersigned by a “guarantor” Juan Yu–who is deemed to take overall responsibility for all aspects of the study (ethics, consent, data handling, and storage and all other aspects of Good Research Practice). I want to extend my heartfelt gratitude to the authors of this manuscript who gives me much help and advice. Special thanks to Dr. Ning Ding for native English polish.
Our institutional review board waived written informed consent for this retrospective cases that evaluated de-identified data and involved no potential risk to patients.
References
- 1.CDC. https://www.cdc.gov.
- 2.Wang Y., Wang Y., Chen Y. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures [published online ahead of print, 2020 Mar 5] J Med Virol. 2020 doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Y.C., Chen C.S., Chan Y.J. The outbreak of COVID-19: An overview. J Chin Med Assoc. 2020;83(3):217–220. doi: 10.1097/JCMA.0000000000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peng J., Ren N., Wang M. Practical experiences and suggestions on the eagle-eyed observer, a novel promising role for controlling nosocomial infection of the COVID-19 outbreak [published online ahead of print, 2020 Mar 3] J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.02.020. S0195-6701(20):30096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang H.W., Yu J., Xu H.J. Corona virus international public health emergencies: implications for radiology management. Acad Radiol. 2020;27(4):463–467. doi: 10.1016/j.acra.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Epidemiology Working Group for NCIP Epidemic Response The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin J Epidemiol. 2020;41(2):145–151. [Google Scholar]
- 7.W. Guan, Z. Ni, W. Liang, et al. Clinical characteristics of 2019 novel coronavirus infection in China. MedRxiv preprint. doi: https://doi.org/10.1101/2020.02.06.20020974.
- 8.Cao Y., Li Q., Chen J. Hospital emergency management plan during the COVID-19 epidemic [published online ahead of print, 2020 Mar 2] Acad Emerg Med. 2020 doi: 10.1111/acem.13951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.https://mp.weixin.qq.com/s/1P3nn0p_A3AqO-2NFmAGPw
- 10.Zhonghua Liu, Xing Bing, Za Zhi. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chinese Journal of Surgery. 2020;41(2):145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Xu X., Yu C., Qu J. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2 [published online ahead of print, 2020 Feb 28] Eur J Nucl Med Mol Imaging. 2020 doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai T.H.T., Tang E.W.H., Chau S.K.Y. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong [published online ahead of print, 2020 Mar 3] Graefes Arch Clin Exp Ophthalmol. 2020 doi: 10.1007/s00417-020-04641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]