Introduction
Up to March 31 2020, more than 800 000 cases of COVID-19 have been reported worldwide, and France has declared 50 000 patients and 3500 deaths. The COVID-19 epidemic is unique because of its scale, the speed of its spread, the lack of pre-existing scientific data and the importance of media coverage [1]. It impelled the hospitals taking charge of the cases to face the many new challenges associated with the outbreak [2]. However, the resilience of health systems in response to COVID-19—including those in high-income countries—is open to question [3,4]. Health-system resilience can be defined as the capacity of health actors, institutions, and populations to prepare for and effectively respond to crises, to maintain core functions when a crisis hits, and—informed by lessons learned during the crisis—to reorganize if conditions require it [5].
Bichat-Claude Bernard hospital is a 1000-bed university hospital in Paris belonging to the Assistance Publique–Hôpitaux de Paris (AP-HP), the largest hospital system in Europe employing more than 90 000 people in 39 hospitals. The hospital is one of the reference centres in France for patients with suspected or confirmed emerging infectious diseases, such as patients with Ebola or Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Bichat hospital managed the first three COVID-19 cases in Europe, diagnosed on January 24, 2020 [6], and has managed more than 400 COVID-19 patients since then. On March 31 2020 more than 280 patients with COVID-19 were hospitalized in the hospital, including 65 in intensive care units (ICUs). In order to provide data on the resilience of health systems during the COVID-19 pandemic, we describe, at the hospital level, the key elements of the response to COVID-19, including the challenges and issues to anticipate following the experience of our centre (Table 1 ).
Table 1.
Challenges encountered by the hospital and local solutions found
| Challenges | Local solutions |
|---|---|
| Management of suspected and confirmed patients with COVID-19 | |
| Preparedness |
|
| Adapting to a new microorganism |
|
| Biosafety level 3 (then 2) laboratory examinations |
|
| Anticipating the increase of cases |
|
| Logistical considerations | |
| Moving patients in the hospital for radiological examinations or surgery |
|
| Organizing the switchboard |
|
| Links with the pre-hospital care |
|
| Hazardous waste management |
|
| Managing and taking care of healthcare workers | |
| Healthcare workers' anxiety |
|
| Increased need for healthcare workers |
|
| Avoiding double standards between healthcare workers who take care of the suspected and confirmed cases and those who do not |
|
| Continuing usual care, research and teaching activities as long as possible | |
| Evaluating and anticipating collateral effects |
|
| Increasing the availability of beds |
|
| Organizing the development of research projects |
|
| Maintaining teaching activities |
|
ID, infectious diseases department; IPC, infection prevention and control; ICU, intensive care unit; ED, emergency department.
Establishing the clinical management of suspected or confirmed patients with COVID-19
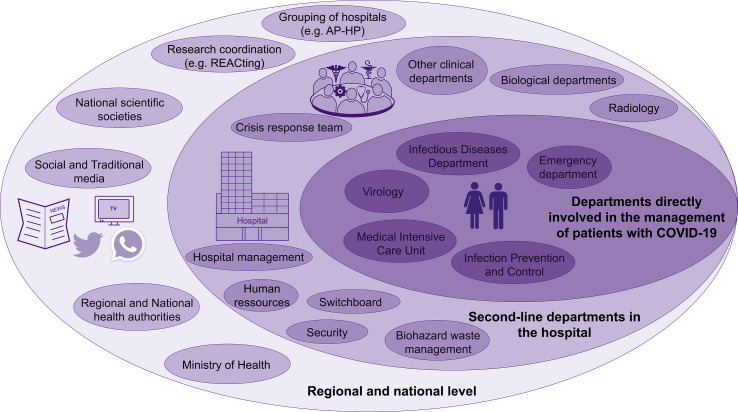
During epidemics, a coordinated and multidisciplinary management between specialists in infectious diseases (IDs), ICUs, and infection prevention and control (IPC), and also the hospital management, is of paramount importance to provide optimal care (Fig. 1 ). The management of the first infected patients was based on scientific data published since the start of the outbreak, as well as our experience from previous outbreaks (SARS and MERS-CoV). When the first patients arrived in January, we used the procedures for MERS-CoV [7] and also applied the principle of ‘supervision’, developed for Ebola, with four to six head nurses from the most involved units (ID, IPC, ICU) who are trained to manage all the aspects of caring for suspected or confirmed cases together with logistical matters. In a context of day-to-day evolution of scientific information, it was necessary to adapt in real time to new data, and new guidelines were produced at a rapid pace. Informing all the healthcare workers (HCWs) of the new guidelines is a challenge that we met with regular information meetings and with the use of the intranet of the hospital. Education, training and exercises have been regularly organized since the beginning of the outbreak for frontline HCWs to ensure that all HCWs caring for patients receive adequate information and training on personal protective equipment (PPE) and clinical management of the patients.
Fig. 1.
Key levels for outbreak management.
Anticipating the next steps of the epidemic
The ID department had a unit with seven bedrooms with negative air pressure and an anteroom. This unit was used first, but as more beds were needed we dedicated more and more units with a scale-up approach to the management of COVID-19 patients. On March 13 2020 the 59 beds of Bichat hospital and the 13 beds of the day hospital were exclusively dedicated to COVID-19, and the sexually transmitted infection (STI) screening centre was used for COVID-19 screening and the follow-up of discharged COVID-19 patients. On March 16 we added the 60 beds of the rehabilitation unit of Bichat for the management of hospitalized COVID-19 patients. On March 24 we had to use the internal medicine department (48 beds), then the pneumology department (28 beds), and on March 28 the cardiology department (27 beds). The ICU capacity increased up to 65 beds at the same time by mobilizing the three ICUs of our centre, as well as surgery theatres. We thus had to discharge or transfer to other hospitals all patients who were not infected with the SARS-CoV-2 virus. As previously reported by some Italian and Chinese colleagues, many activities that are not related to COVID-19 had to be stopped in the midst of the epidemic [8,9].
Despite this, medical staff in the ID department had to be doubled and then tripled night and day to cope with the increase in work, and three teams were created: one to manage external calls, one to organize the testing of cases, and one to take care of the infected patients. They first managed all the COVID-19 patients of the hospital, but then had to let the other departments take care of their infected patients under the supervision of the IPC team. At first, doctors from the emergency department managed the hospitalized patients with COVID-19 outside of the ICU at night, but a specific night duty service was soon needed, first with one ID resident and now with six residents and two senior consultants. Ventilatory support is critical, and efforts have been made to provide the highest number of ventilators available. To this aim, the decision was taken in France to delay all surgical interventions that were not urgent. Microbiology services had to develop and increase the capacities for SARS-CoV-2 detection and monitoring. All the biology departments had to organize the analysis of samples with biosafety level 2. Point-of-care testing was already available in the ICU in order to decrease the workload of biological departments, and was rapidly installed in the ID unit.
Involving and caring for the HCWs
HCWs are at the forefront of the epidemic response and they must be supported. The hospital had to call in temporary nurses to deal with COVID-19, but the epidemic arrived in a national context where public hospitals are at the centre of a protest movement due to, among other difficulties, the difficulty in recruiting HCWs and bed shortages. The existence of a large health system such as AP-HP was helpful in recruiting nurses and other HCWs from outside the hospital and to organize support between different hospitals when absenteeism was a problem. Vacations were put on hold, and many HCWs did extra hours for which the hospital and AP-HP management committed to pay. HCWs who developed COVID-19 were managed in the hospital if needed, or as outpatients, and were put on sick leave for at least 7 days and 2 days free of symptoms. From March 18 onward, all the HWCs were asked to always wear surgical masks in the hospital. Psychological support was offered to HCWs taking care of patients, but also to those who may have felt threatened or anxious. Media pressure about the COVID-19 epidemic has been felt at all levels [10]: rumours and global anxiety led to difficulties for the recruitment of temporary staff who sometimes refused to come to the hospital. The hospital management team had to reassure them and ensure that health care was not disrupted and that doctors were not distracted from their missions. Internal communication was addressed with conferences open to all the HCWs of the hospital and information was shared on the intranet on a daily basis.
Logistical matters
An unexpected difficulty was the management of hazardous waste; the service provider initially refused to come following the announcement of confirmed SARS-CoV-2 cases in the hospital. This problem was resolved through the involvement of the IPC team and the head of the administrative staff of the hospital. The severity of the disease among patients made it necessary to perform CT scans in dedicated CT scanners. The transport of the patients to other departments was found to be a critical point to anticipate. Patient movement circuits to avoid nosocomial spread had to be organized by the IPC team and forwarded to involved HCWs. The logistics services for medical equipment management had to adapt to a rapidly growing demand and provide the personnel with the necessary equipment for treatment. The security service was called upon to manage the arrival of journalists and the media, in particular to protect entry to the ID and ICU departments. They were also mobilized to secure the patient transport circuits. The hospital switchboard was a key department to handle external calls about COVID-19.
Ensuring the commitment of hospital management staff and health authorities
The elaboration of the hospital response was of course integrated at the level of the AP-HP as well as at the regional, national and international levels. The support of the hospital management staff and the AP-HP was necessary in order to supervise communication with multiple actors, notably high-level administrative and political decision-makers. This support was necessary, for example, to accelerate the transfer of patients from the hospital to rehabilitation units, including patients with highly resistant bacteria such as carbapenemase-producing bacteria of the Enterobacteriales. The hospital's communication unit was crucial in informing the media about the management of the epidemic. Video interviews were conducted with experts and recognized leaders from different departments and circulated via traditional and social media to inform about the risk posed by the epidemic and to limit rumours [11].
Concluding remarks
Many health structures will face an increasing number of patients with COVID-19 and have to anticipate the consequences, including the need for more beds, trained HCWs, and ventilators. In order to face the outbreak, hospitals have to anticipate the consequences of COVID-19 on all the departments, including indirect impact on non-infected patients, to ensure the commitment of hospital management staff and health authorities, to encourage effective leadership, to involve and care for all the HCWs, and to organize communication with the wider public.
Ethics approval
The study has obtained the approval of the Comité d’Ethique de Recherche en Maladies Infectieuses et Tropicales (CER-MIT) (Institutional Review Board N° IRB00011642).
Author contributions
Conceptualization: NP-S, J-CL, F-XL. Writing original draft: NP-S. Writing, review and editing: NP-S, J-CL, GB, LB, SG, CC, SJ, AK, DD, PM, J-FT, YY, F-XL.
Transparency declaration
The authors have no competing interests to disclose. No funding was received for this work.
Acknowledgements
We thank all the healthcare workers who are taking care of patients.
Editor: L. Leibovici
References
- 1.Shimizu K. 2019-nCoV, fake news, and racism. Lancet. 2020;395:685. doi: 10.1016/S0140-6736(20)30357-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heymann D.L., Shindo N. COVID-19: what is next for public health? Lancet. 2020;395:542–550. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diseases T.L.I. Challenges of coronavirus disease 2019. Lancet Infect Dis. 2020;20:261. doi: 10.1016/S1473-3099(20)30072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Legido-Quigley H., Asgari N., Teo Y.Y., Leung G.M., Oshitani H., Fukuda K. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. 2020;395:848–850. doi: 10.1016/S0140-6736(20)30551-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kruk M.E., Myers M., Varpilah S.T., Dahn B.T. What is a resilient health system? Lessons from Ebola. Lancet. 2015;385:1910–1912. doi: 10.1016/S0140-6736(15)60755-3. [DOI] [PubMed] [Google Scholar]
- 6.Lescure F.-X., Bouadma L., Nguyen D., Parisey M., Wicky P.-H., Behillil S. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30200-0. March. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bouadma L., Lescure F.-X., Lucet J.-C., Yazdanpanah Y., Timsit J.-F. Severe SARS-CoV-2 infections: practical considerations and management strategy for intensivists. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05967-x. February. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khan S., Nabi G., Han G., Siddique R., Lian S., Shi H. Novel coronavirus: how things are in Wuhan. Clin Microbiol Infect. 2020;26:399–400. doi: 10.1016/j.cmi.2020.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zarocostas J. How to fight an infodemic. Lancet. 2020;395:676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atlani-Duault L., Ward J.K., Roy M., Morin C., Wilson A. Tracking online heroisation and blame in epidemics. Lancet Pub Health. 2020;5:e137–e138. doi: 10.1016/S2468-2667(20)30033-5. [DOI] [PMC free article] [PubMed] [Google Scholar]