Abstract
As the global pandemic of coronavirus disease-19 (COVID-19) progresses, many physicians in a wide variety of specialties continue to play pivotal roles in diagnosis and management. In radiology, much of the literature to date has focused on chest CT manifestations of COVID-19 (Zhou et al. [1]; Chung et al. [2]). However, due to infection control issues related to patient transport to CT suites, the inefficiencies introduced in CT room decontamination, and lack of CT availability in parts of the world, portable chest radiography (CXR) will likely be the most commonly utilized modality for identification and follow up of lung abnormalities. In fact, the American College of Radiology (ACR) notes that CT decontamination required after scanning COVID-19 patients may disrupt radiological service availability and suggests that portable chest radiography may be considered to minimize the risk of cross-infection (American College of Radiology [3]). Furthermore, in cases of high clinical suspicion for COVID-19, a positive CXR may obviate the need for CT. Additionally, CXR utilization for early disease detection may also play a vital role in areas around the world with limited access to reliable real-time reverse transcription polymerase chain reaction (RT-PCR) COVID testing.
The purpose of this pictorial review article is to describe the most common manifestations and patterns of lung abnormality on CXR in COVID-19 in order to equip the medical community in its efforts to combat this pandemic.
Keywords: COVID-19, Coronavirus, Chest X-ray, Chest CT
Highlights
-
•
COVID-19 lung infection commonly produces ground glass and consolidative opacities with a bilateral, peripheral, and lower lung distribution.
-
•
Portable CXR will likely be the primary imaging modality used in diagnosis and management of COVID-19 patients.
-
•
With high clinical suspicion for COVID-19 infection, positive CXR findings can obviate the need for CT scanning.
-
•
Lung opacities can rapidly evolve into a diffuse pattern within weeks after symptom onset, often peaking at around 6-12 days.
1. Ground glass densities
CXR is a less sensitive modality in the detection of COVID-19 lung disease compared to CT, with a reported baseline CXR sensitivity of 69% [4]. The most common reported CXR and CT findings of COVID-19 include lung consolidation and ground glass opacities2.
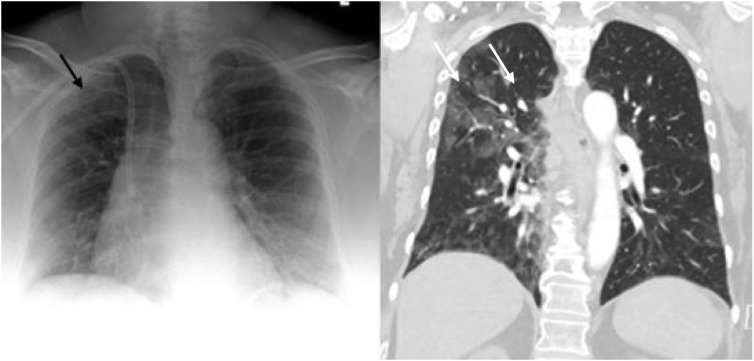
Ground glass densities observed on CT may often have a correlate that is extremely difficult to detect on CXR (Fig. 1, Fig. 2 ).
Fig. 1.
Portable CXR (left) with vague hazy densities in the right upper lobe (white arrow) which correspond to ground glass opacities (black arrow) on coronal image from contrast enhanced CT (right) performed the same day.
Fig. 2.
CXR (left) with patchy peripheral left mid to lower lung opacities (black arrow) corresponding to ground glass opacities (white arrow) on coronal image from contrast-enhanced the contemporaneous chest CT (right).
Often, reticular opacities accompanying regions of ground glass attenuation are more easily appreciable on standard CXR (Fig. 3 ).
Fig. 3.
CXR (left) with reticular and hazy left lower lobe opacities (black arrow) in a patient with COVID-19. Similar findings are present on the coronal CT from the same day (right).
The hazy pulmonary opacities on CXR can sometimes be diffuse making identification challenging in some instances (Fig. 4 ).
Fig. 4.
CXR (left) with subtle ill-defined hazy opacities in the right (black arrows) greater than left lungs in a patient with COVID-19. Findings are easier to appreciate on subsequent CT the same day (right).
2. Bilateral lower lobe consolidations
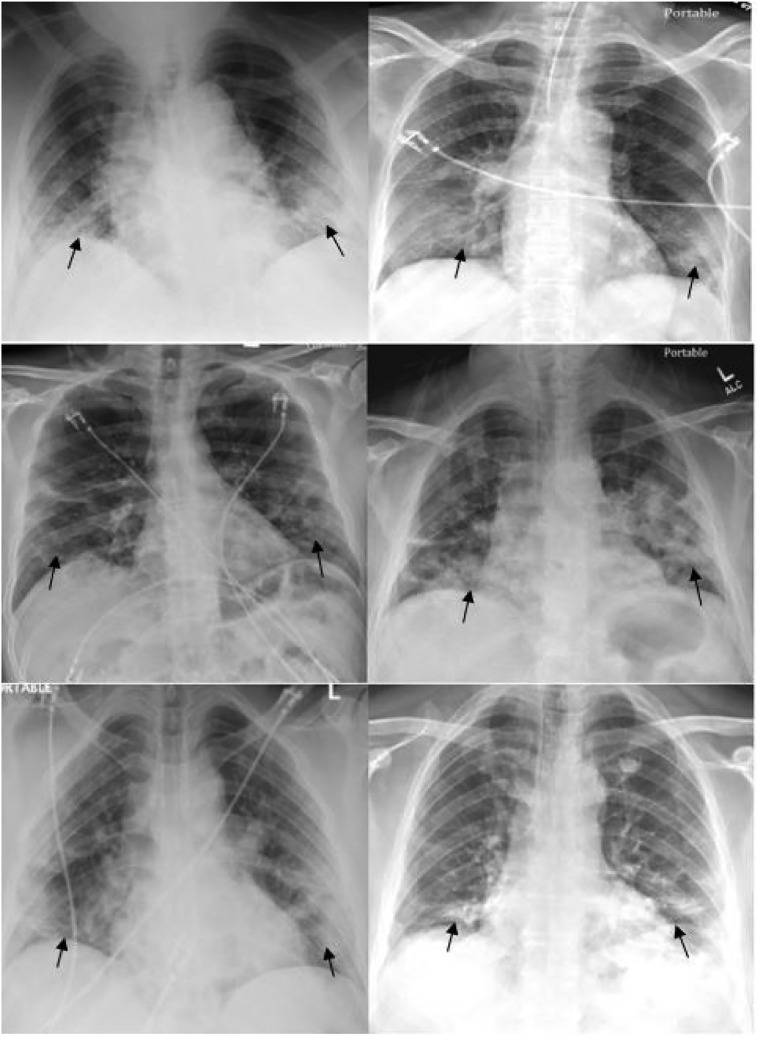
As opposed to community acquired bacterial pneumonia which tends to be unilateral and involving a single lobe [5], COVID-19 and other viral pneumonias typically produce lung opacities in more than one lobe. Identifying multifocal air-space disease on CXR can be a significant clue to COVID-19 pneumonia. Early COVID-19 investigators have noted that the air-space disease tends to have a lower lung distribution and is most frequently bilateral [4] (Fig. 5 ).
Fig. 5.
Six different patients with varying degrees of COVID-19 pneumonia predominantly involving the lower lung zones (black arrows) bilaterally on CXR.
3. Peripheral air space opacities
One of the most unique and somewhat specific features of COVID-19 pneumonia is the high frequency of peripheral lung involvement, often mirroring other inflammatory processes such as organizing pneumonia. Chung et al. reported that 33% of COVID-19 chest CTs had peripheral lung distribution [2] and Ng et al. reported an even greater incidence of up to 86% on chest CT [6]. Such peripheral lung opacities also tend to be multifocal, either patchy or confluent, and can be readily identified on CXR (Fig. 6 ).
Fig. 6.
Four different patients with varying degrees of COVID-19 pneumonia on CXR predominantly involving the peripheral lungs bilaterally (black arrows).
4. Diffuse air space disease
Diffuse lung opacities in patients with COVID-19 have a similar CXR pattern (Fig. 7 ) as other widespread infectious or inflammatory processes including acute respiratory distress syndrome (ARDS).
Fig. 7.
CXR (left) and subsequent coronal image from chest CT (right) performed in a patient with COVID-19 and diffuse ground glass and consolidative opacities throughout both lungs.
When lung disease involves the majority of the pulmonary parenchyma, patients are typically hypoxic and require intubation with mechanical intubation (Fig. 8 ).
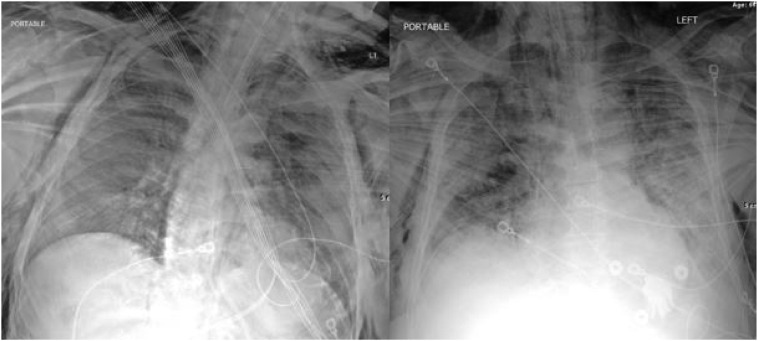
Fig. 8.
Two different intubated patients with COVID-19 infection and diffuse lung opacities.
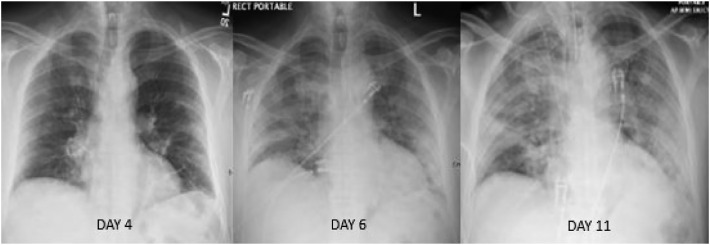
Lung opacities may rapidly evolve into a diffuse coalescent or consolidative pattern within 1–3 weeks of symptom onset [1,7], often peaking at around 6–12 days after initial clinical presentation (Fig. 9, Fig. 10 ).
Fig. 9.
Serial radiographs over 7 days in a patient with COVID-19 infection depicting progression of diffuse lung disease that ultimately required intubation.
Fig. 10.
Serial chest radiographs of a different patient with COVID-19 infection separated by 6 days depicting progression of diffuse lung disease requiring intubation.
5. Uncommon CXR findings
Pleural effusions have been reported as exceedingly rare on CXR and CT in COVID-19 infected patients, and when present are most often identified late in the disease course [8].
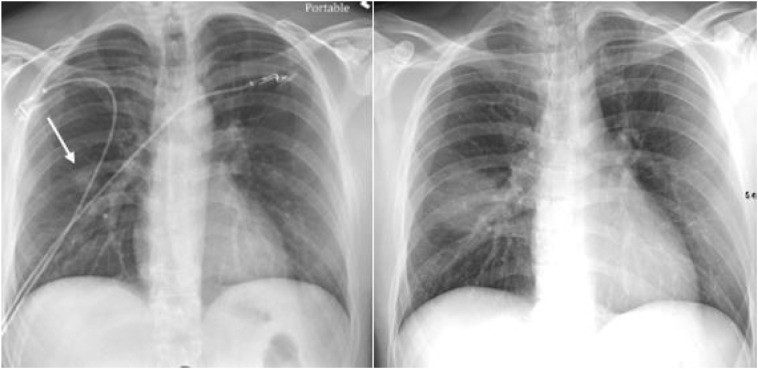
Lung cavitation and pneumothorax are also rare findings in COVID-19 patients [8] but can occur (Fig. 11 ).
Fig. 11.
Serial chest radiographs of a COVID-19 patient with diffuse lung opacities (left image) with interval cavitation (left image white arrows) and tension pneumothorax (right image black arrow). Successful chest tube placement was subsequently performed (not shown).
Localized large nodules have yet to be reported in the literature to this date (Fig. 12 ).
Fig. 12.
A unique case of a rapidly enlarging right lung nodule (left image, white arrow) over the course of 5 days. Subsequent bronchoscopy with tissue sampling revealed COVID-19 infection.
Diffuse chest wall subcutaneous emphysema and pneumomediastinum after intubation in the setting of COVID-19 infection has been described in one case report [9], as of the time of this writing. This phenomenon has also been reported previously in the setting of H1N1 viral infection [10].
Since the influx of cases began at our institution, we have noticed this to occur in several patients (Fig. 13 ). Potential mechanisms include alveolar rupture leading to interstitial emphysema from the currently recommended high positive end-expiratory pressure (PEEP) settings on COVID-19 ventilated patients according to the Macklin effect [11]. The diffuse alveolar damage in severe cases may also contribute to alveolar rupture. The exact mechanism requires additional investigation.
Fig. 13.
Two different intubated patients with COVID-19 and diffuse subcutaneous emphysema and pneumomediastinum identified on CXR. No pneumothorax was identified.
6. Conclusions
Patterns of COVID-19 lung disease can be identified on conventional chest radiography as well as chest CT. Typical verbiage when reporting patients with, or suspected COVID-19 on CXR include terms such as irregular, patchy, hazy, reticular, and widespread ground glass opacities. Grading disease severity based on total lung involvement is also important to relay to the clinicians. As the pandemic progresses, the medical community will frequently rely on portable CXR due to its widespread availability and reduced infection control issues that currently limit CT utilization.
Credit authorship contribution statement
Adam Jacobi:Conceptualization, Writing - original draft, Supervision.Michael Chung:Conceptualization, Writing - review & editing.Adam Bernheim:Writing - review & editing, Resources.Corey Eber:Writing - review & editing, Resources.
References
- 1.Zhou S., Wang Y., Zhu T., Xia L. CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, China. Am J Roentgenol. 2020:1–8. doi: 10.2214/AJR.20.22975. March. [DOI] [PubMed] [Google Scholar]
- 2.Chung M., Bernheim A., Mei X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. February 2020;200230 doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection|American College of Radiology. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Accessed March 22, 2020. Google Scholar 2020.
- 4.Wong H.Y.F., Lam H.Y.S., Fong A.H. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019:201160. doi: 10.1148/radiol.2020201160. Mar 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vilar J., Domingo M.L., Soto C. Radiology of bacterial pneumonia. J Eur J Radiol. 2004 Aug;51(2):102–113. doi: 10.1016/j.ejrad.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 6.Ng M.Y., Lee E., Yang J. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020;2(1) doi: 10.1148/ryct.2020200034. [Link, Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernheim A., Mei X., Huang M. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020:200463. doi: 10.1148/radiol.2020200463. Feb 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salehi S., Abedi A., Balakrishnan S. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020 Mar;14:1–7. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 9.Sun R., Liu H., Wang X. Mediastinal emphysema, Giant Bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol. 2020 Mar 20 doi: 10.3348/kjr.2020.0180. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gou H.H., Sweeney R.T., Regula D. Fatal 2009 influenza a (H1N1) infection, complicated by acute respiratory distress syndrome and pulmonary interstitial emphysema. Radiographics. 2010 Mar;30(2):327–333. doi: 10.1148/rg.302095213. [DOI] [PubMed] [Google Scholar]
- 11.Poston JT, Patel BK, Davis AM. Management of critically ill Adults with COVID-19. JAMA Clinical Guideline Synopsis. https://jamanetwork.com/journals/jama/fullarticle/2763879. Accessed March 26, 2020 2020. [DOI] [PubMed]